Abstract
Background
Odontogenic cutaneous fistula appears as dimpling or a nodule with purulent discharge, usually in the chin or jaw. Affected patients usually seek help from dermatologists or surgeons rather than from dentists. However, clinical symptoms of facial skin fistula without dental problems can lead to misdiagnosis.
Objective
The purpose of this study was to investigate the clinical characteristics of patients with odontogenic cutaneous fistulas.
Methods
This retrospective observational study was performed at Chungbuk National University Hospital by analyzing patients who visited from April 1994 to September 2014. Following clinical and radiographic examinations, the paths and origins of sinus fistulas were determined. Investigated factors were gender, age, morphology, location, originating tooth, time to evolution, recurrence, and treatment method.
Results
Thirty-three patients (22 males, 11 females; average age 49.2 years) were examined during the investigation period. Thirty-four fistulas were diagnosed as odontogenic cutaneous fistulas. The most common morphology was dimpling (n=14, 41.2%). The various locations observed were related to the originating tooth. The most common site was the mandibular body related to mandibular molars. The referral clinical diagnosis was of odontogenic origin in 6 cases (18.2%). The majority of patients had experienced recurrence after treatment in previous clinics that had failed to diagnose odontogenic cutaneous fistula. Surgical fistulectomy and/or tooth treatment were performed in all cases. All patients were followed-up for 1 year. None showed signs of recurrence.
Conclusion
Extraoral and dental examinations are required to make a diagnosis of odontogenic cutaneous fistula. Thus, cooperation between dermatologists and dentists is essential.
Keywords: Cutaneous, Fistula, Odontogenic, Tooth
INTRODUCTION
Odontogenic cutaneous fistula is caused by chronic dental infection. The fistula provides a path for pus drainage and infection of the facial area. In cases of dental infection, fistula openings are typically located in the intraoral gingival area, whereas extraoral openings usually arise as sequelae to bacterial invasion of dental pulp through a breach in the enamel and dentin caused by a carious lesion, trauma, or other causes1. If treatment is not initiated during the early inflammatory stage, the pulp becomes necrotic and infection spreads beyond the confines of the affected tooth into the periradicular area, where it causes apical lesions. Discharge of purulent exudate is usually associated with periapical radiolucent lesion, and this exudate flows through tissues and structures along paths of least resistance2. Although cutaneous fistulas of dental origin are rather common lesions, misdiagnosis and inappropriate treatment often occur. The reasons for misdiagnosis include varied morphologies and locations or asymptomatic chronic dental infections.
In the present study, we analyzed the clinical characteristics of odontogenic cutaneous fistulas. Our goal was to identify etiological factors important in ensuring correct treatment of facial cutaneous sinus fistulas.
MATERIALS AND METHODS
This retrospective study was carried out at the Departments of Oral and Maxillofacial Surgery, and Dermatology of Chungbuk National University Hospital (Cheongju, Korea) by analyzing patients who visited from April 1994 to September 2014. All patients had a clinical and radiological diagnosis of odontogenic cutaneous fistula. X-ray (panoramic view) and intraoral examinations were used for dental evaluations.
Thirty-three patients were enrolled in the study. Clinical data included gender, age, morphology, location, originating tooth, time to evolution, recurrence, and treatment method. All patients were followed up for at least 1 year after surgical fistulectomy and tooth treatment.
RESULTS
Thirty three patients were treated over a 21-year period. Thirty four fistulas were diagnosed as odontogenic cutaneous fistulas (one patient had two fistulas on both buccal cheeks) after clinical and radiologic evaluations. The patients consisted of 22 males and 11 females with an average age of 49.2 years (range 10~83 years) (Table 1). The most affected age group (13 patients, 39.4%) was ≥60 years of age.
Table 1. Number of patients in the different age groups, genders, and time to evolution.
| Age (yr) | Male | Female | Time to evolution (wk) | Total |
|---|---|---|---|---|
| ≤19 | 3 (9.1) | 2 (6.1) | 6.1 (1.5~12) | 5 (15.2) |
| 20~29 | 4 (12.1) | 1 (3.0) | 22.8 (2~44) | 5 (15.2) |
| 30~39 | 0 | 2 (6.1) | 25.5 (3~48) | 2 (6.1) |
| 40~49 | 4 (12.1) | 1 (3.0) | 20.8 (8~44) | 5 (15.2) |
| 50~59 | 2 (6.1) | 1 (3.0) | 18.4 (16~48) | 3 (9.1) |
| ≥60 | 9 (27.3) | 4 (12.1) | 37.0 (2~144) | 13 (39.4) |
| Total | 22 (66.7) | 11 (33.3) | 26.4 (1.5~144) | 33 (100) |
Values are presented as number (%) or mean (range).
Time to evolution was 1.5~144 weeks (mean; 26.4), and was greatest in those aged ≥60 years (Table 1).
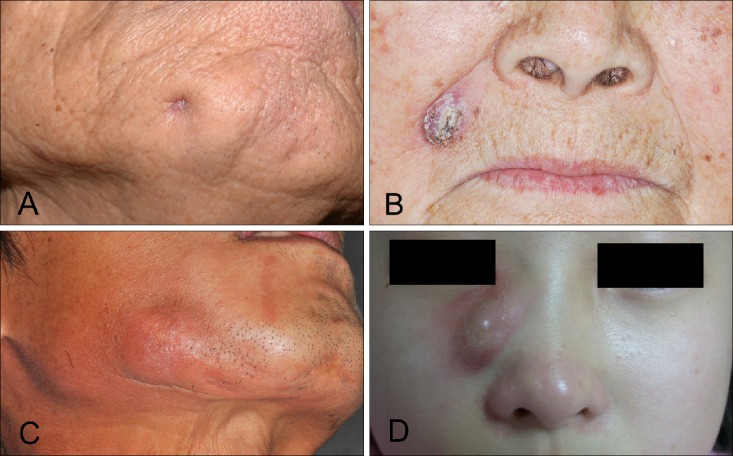
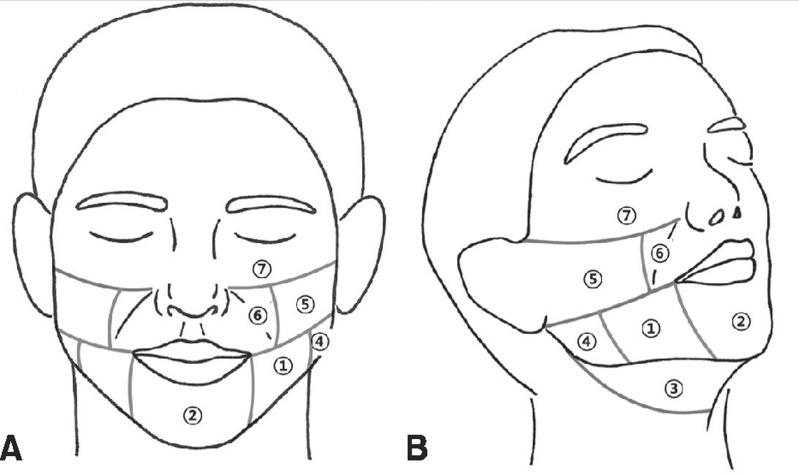
The predominant morphology was dimpling, which occurred in 14 fistulas (41.2%). Other morphologies were nodule, abscess, and cyst (Table 2, Fig. 1). The most frequent location was the mandibular body (11 fistulas, 32.4%). Other locations in decreasing order of occurrence were; the chin (mentum), buccal cheek, nasolabial fold (paranasal) region, submandibular region, infraorbital region, and mandibular angle (Table 3, Fig. 2). One patient had two fistulas on both buccal cheeks, thus the total number of fistulas was 34. Cutaneous lesions were adjacent to causative teeth in 32 patients (97.0%). Only one patient had a lesion at a distant site. This case involved a 13-year-old girl, in whom the right upper canine was affected, but the fistula was located in the right infraorbital region (Fig. 1D).
Table 2. Morphologies of the odontogenic cutaneous fistulas.
| Morphology | Fistula no. |
|---|---|
| Dimpling | 14 (41.2) |
| Nodule | 11 (32.4) |
| Abscess | 7 (20.6) |
| Cyst | 2 (5.9) |
| Total | 34 (100)* |
Values are presented as number (%). *Numbers of fistulas included two fistulas of one patient.
Fig. 1. Clinical photos showing the various morphologies of odontogenic cutaneous fistulas. (A) Dimpling, (B) nodule, (C) abscess, (D) cyst.
Table 3. Locations and affected teeth of the odontogenic cutaneous fistulas.
| Location | Right | Left | Midline | Total | Affected teeth | |
|---|---|---|---|---|---|---|
| Mandibular body | 5 | 6 | 0 | 11 (32.4) | Mn | Mn: 24 (70.6) |
| 1 | 0 | 0 | 1st, 2nd premolars | |||
| 2 | 6 | 0 | 1st, 2nd molars | |||
| 2 | 0 | 0 | Edentulous | |||
| Chin (mentum) | 3 | 5 | 1 | 9 (26.5) | Mn | |
| 0 | 4 | 1 | Incisors | |||
| 3 | 0 | 0 | Canine | |||
| 0 | 1 | 0 | Edentulous | |||
| Submandibular region | 3 | 0 | 0 | 3 (8.8) | Mn | |
| 2 | 0 | 0 | 1st, 2nd molars | |||
| 1 | 0 | 0 | Edentulous | |||
| Mandibular angle | 1 | 0 | 0 | 1 (2.9) | Mn: 3rd molar | |
| Buccal cheek | 4 | 1 | 0 | 5 (14.7) | Mx | Mx: 10 (29.4) |
| 0 | 1 | 0 | 1st, 2nd premolars | |||
| 4 | 0 | 0 | 1st, 2nd molars | |||
| Nasolabial fold | 1 | 3 | 0 | 4 (11.8) | Mx | |
| 0 | 2 | 0 | Incisors | |||
| 1 | 1 | 0 | Canine | |||
| Infraorbital region | 1 | 0 | 0 | 1 (2.9) | Mx: canine | |
| Total | 18 | 15 | 1 | 34 (100) | ||
Values are presented as number only or number (%). Mn: mandible, Mx: maxilla.
Fig. 2. Diagram showing the locations of odontogenic cutaneous fistulas. (A) Frontal view, (B) lateral view. ① Mandibular body (cheek), ② chin (mentum), ③ submandibular region, ④ mandibular angle, ⑤ buccal cheek, ⑥ nasolabial fold (paranasal), ⑦ infraorbital region.
To examine the affected teeth in each patient, a panoramic view X-ray was taken (Fig. 3). Of the 34 fistulas, 24 (70.6%) originated from a mandibular edentulous site or tooth, and the other 10 (29.4%) originated from a maxillary edentulous site or tooth (nine cases-10 fistulas). The teeth most frequently affected were molars (15 fistulas, 44.1%), followed by incisors (n=7, 20.6%), canines (cuspid; n=6, 17.6%), and premolars (n=2, 5.9%). Four fistulas (11.8%) affected edentulous sites. Relationships between locations and affected teeth are summarized in Table 3.
Fig. 3. Panoramic view. Radiolucent lesion of the periapical area of a mandibular molar (white arrow).
A clinical diagnosis of an odontogenic origin was made in six patients (18.2%). In two of these patients, fistulas were related to actinomycosis. One of the two patients developed an infection after bone grafting and miniplate fixation. In the other patient, the fistula was presumed to have been caused by osteoradionecrosis after radiation therapy for mandibular cancer.
The other 27 patients (81.8%) had been misdiagnosed in previous clinics, resulting in one or more recurrences. Initial misdiagnoses included epidermal cyst (8 cases, 24.2%), furuncle (7 cases, 21.2%), subcutaneous mycosis (5 cases, 15.2%), squamous cell carcinoma (3 cases, 9.1%), basal cell carcinoma (2 cases, 6.1%), and foreign body granuloma (2 cases, 6.1%).
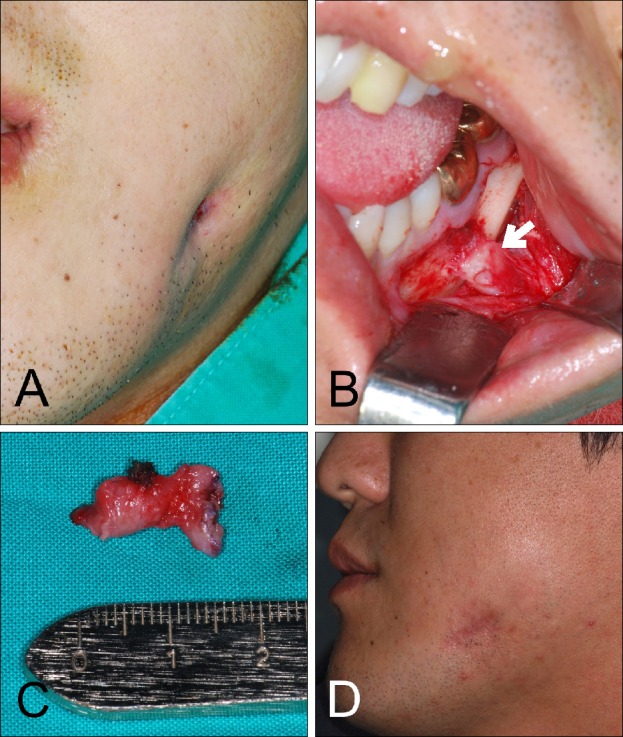
Cutaneous lesions and affected teeth were treated by fistulectomy and extraction or endodontic therapy with antibiotic therapy. All 33 patients were followed up for 1 year. No recurrence was encountered (Fig. 4).
Fig. 4. Odontogenic cutaneous fistula of the mandibular body region. (A) Extraoral photo; showing dimpling on the left mandibular body region. (B) The odontogenic cutaneous fistula was observed by orientating the root apex (#36; left mandibular first molar) to overlying cortical plates and muscular attachments. The fistula tract is indicated by a white arrow. (C) Resected fistula tract. (D) Postoperative photo showing diminished dimpling.
DISCUSSION
Odontogenic cutaneous fistula is characterized by the presence of a draining sinus fistula originating from a localized area with pus and surrounded by granulation tissue in alveolar bone of the affected tooth. Its main causes are pulpal degeneration due to a carious tooth, tooth fracture, remaining tooth (root rest), and periodontal infection3. The majority of odontogenic sinus fistulas have an intraoral opening4, but in cases of chronic dental infection, the local inflammatory destructive process progresses slowly as an alveolar bone abscess. Once the inflammation passes through cortical bone and periosteum, it may spread into the surrounding soft tissue, limited by muscle attachments and facial regions (Fig. 4)3.
The traditional consensus is that fistulas do not exhibit gender preference, with no significant relationship between prevalence and age4,5,6,7. However, in the present study, the 22 males seemed to be more affected than the 11 females. In addition, patients aged ≥60 years seemed to be most affected (Table 1). Older patients may present with no dental symptom because of the low-grade and insidious nature of the odontogenic infection. In terms of duration, time to evolution was shorter in younger patients (≤19 years of age) than in older patients (≥60). In these groups, mean time was 6.1 weeks (range 1.5~12 weeks) and 37.0 weeks (range 2~144 weeks), respectively. Symptom duration was greatest (144 weeks) in an elderly patient with a diagnosis of chronic osteomyelitis of the mandible.
Protracted evolution could also be due to a lack of diagnostic suspicion caused by the absence of significant dental symptoms in patients with a variety of clinical characteristics in skin8. This leads to misdiagnosis and unnecessary treatment.
The skin manifestations of odontogenic cutaneous fistulas are nonspecific and have rarely been mentioned in the literature. The orifice of a cutaneous sinus fistula can present as a dimpling, nodule, abscess, cyst, ulcer, draining lesion, or nodulocystic lesion with suppuration9. Samir et al.10 described a classic lesion as an erythematous nodule of diameter up to 20 mm with or without drainage presenting skin retraction secondary to healing. In our experience, dimpling was the most frequently encountered manifestation (14 fistulas, 41.2%), though nodules, abscesses, and cysts were also observed.
The variable location of odontogenic cutaneous fistula is the main cause of diagnostic confusion, although locations are related to affected teeth. In the present study, 24 fistulas (70.6%) of mandibular origin were located in the lower third of the face and 10 fistulas (29.4%) of maxillary origin were located in the middle third. The most common location was the mandibular body. Other sites were the chin (mentum), buccal cheek, nasolabial fold (paranasal) region, submandibular region, infraorbital region, and mandibular angle. Twenty odontogenic cutaneous fistulas (58.9%) were located on the mandibular body or chin and originated from a mandibular tooth (Table 3), similar to previous reports6,9. Further study is required to determine whether mandibular teeth tend to drain extra-orally more often than maxillary teeth. Notably, misdiagnoses have also been reported in edentulous patients with fistulas resulting from infected implants, bones, or bone grafts6.
Although the most common cause of an intermittently suppurating cutaneous sinus fistula of the face and neck area is chronic dental infection, these lesions present a diagnostic challenge1. Importantly, previous misdiagnosis and inappropriate medical treatment result in ineffective treatment and repeated recurrence. In the present study, 27 of 33 patients were transferred from general clinicians and had experience of one or more recurrence.
The differential diagnosis reported in previous studies includes subcutaneous mycosis and neoplastic processes, such as, squamous cell carcinoma, basal cell carcinoma, and pyogenic and foreign body granolumas9,11. Diagnostic errors lead to multiple trials of antibiotics and unnecessary repeat surgical procedures3. When a lesion develops, being unaware of its dental origin, patients seek treatment from dermatologists or surgeons. Lack of dental examination possibly leads to inappropriate treatments6. Intraoral and dental examination and panoramic view X-ray imaging are critical for diagnosis (Fig. 3)4. The guideline for achieving an accurate diagnosis is that focus should be placed on the accurate evaluation of involved teeth.
Permanent cure is obtained after proper dental treatment, such as, extraction or endodontic therapy, and appropriate treatment of the offending tooth can lead to lesion resolution12. Dimpling and hyperpigmentation of the skin usually diminishes slowly and sometimes, it remains in the face as a small dimple. Thus, surgical revision or fistulectomy may be needed in some cases for esthetic reasons3,12,13.
The variable characteristics of odontogenic cutaneous fistulas lead to diagnostic confusion. Odontogenic cutaneous fistulas should always be considered in the differential diagnosis of tumors and chronic facial lesions that recur despite treatment. Attending clinicians should carefully take patient history and examine the possibility of a potential odontogenic infection. The keys to making a correct diagnosis are chronicity (weeks, months, or even years) and the recognition that the facial lesion is related to a tooth by a sinus fistula. Extraoral and dental examinations are critically required to make a diagnosis of odontogenic cutaneous fistula, and thus, cooperation between dermatologists and dentists is essential.
References
- 1.Mittal N, Gupta P. Management of extra oral sinus cases: a clinical dilemma. J Endod. 2004;30:541–547. doi: 10.1097/00004770-200407000-00019. [DOI] [PubMed] [Google Scholar]
- 2.Pasternak-Júnior B, Teixeira CS, Silva-Sousa YT, Sousa-Neto MD. Diagnosis and treatment of odontogenic cutaneous sinus tracts of endodontic origin: three case studies. Int Endod J. 2009;42:271–276. doi: 10.1111/j.1365-2591.2008.01519.x. [DOI] [PubMed] [Google Scholar]
- 3.Kim SH, Park SJ, Oh JJ, Lee ES. A case of cutaneous sinus tract of dental origin. Ann Dermatol. 2002;14:235–238. [Google Scholar]
- 4.Barbosa CAM, Tancredo F, Fonseca CF, Pinho MAB. Diagnosis of cutaneous sinus tract in association with traumatic injuries to the teeth. Braz J Dent Traumatol. 2011;2:75–79. [Google Scholar]
- 5.Sadeghi S, Dibaei M. Prevalence of odontogenic sinus tracts in 728 endodontically treated teeth. Med Oral Patol Oral Cir Bucal. 2011;16:e296–e299. doi: 10.4317/medoral.16.e296. [DOI] [PubMed] [Google Scholar]
- 6.Chowdri NA, Sheikh S, Gagloo MA, Parray FQ, Sheikh MA, Khan FA. Clinicopathological profile and surgical results of nonhealing sinuses and fistulous tracts of the head and neck region. J Oral Maxillofac Surg. 2009;67:2332–2336. doi: 10.1016/j.joms.2008.06.084. [DOI] [PubMed] [Google Scholar]
- 7.Slutzky-Goldberg I, Tsesis I, Slutzky H, Heling I. Odontogenic sinus tracts: a cohort study. Quintessence Int. 2009;40:13–18. [PubMed] [Google Scholar]
- 8.Ghodsi SZ, Ghiasi M. Two unusual cases of dental (periapical) infection. Dermatol Online J. 2006;12:15. [PubMed] [Google Scholar]
- 9.Spear KL, Sheridan PJ, Perry HO. Sinus tracts to the chin and jaw of dental origin. J Am Acad Dermatol. 1983;8:486–492. doi: 10.1016/s0190-9622(83)70053-8. [DOI] [PubMed] [Google Scholar]
- 10.Samir N, Al-Mahrezi A, Al-Sudairy S. Odontogenic cutaneous fistula: report of two cases. Sultan Qaboos Univ Med J. 2011;11:115–118. [PMC free article] [PubMed] [Google Scholar]
- 11.Cohen PR, Eliezri YD. Cutaneous odontogenic sinus simulating a basal cell carcinoma: case report and literature review. Plast Reconstr Surg. 1990;86:123–127. doi: 10.1097/00006534-199007000-00020. [DOI] [PubMed] [Google Scholar]
- 12.Cioffi GA, Terezhalmy GT, Parlette HL. Cutaneous draining sinus tract: an odontogenic etiology. J Am Acad Dermatol. 1986;14:94–100. doi: 10.1016/s0190-9622(86)70012-1. [DOI] [PubMed] [Google Scholar]
- 13.Braun RJ, Lehman J., 3rd A dermatologic lesion resulting from a mandibular molar with periradicular pathosis. Oral Surg Oral Med Oral Pathol. 1981;52:210–212. doi: 10.1016/0030-4220(81)90321-2. [DOI] [PubMed] [Google Scholar]