Dear Editor:
Acral persistent papular mucinosis (APPM) is a rare subtype of localized lichen myxedematosus (LM)1 with unknown etiology. To our knowledge only six cases tried treatment1,2,3, and two cases showed family history1.
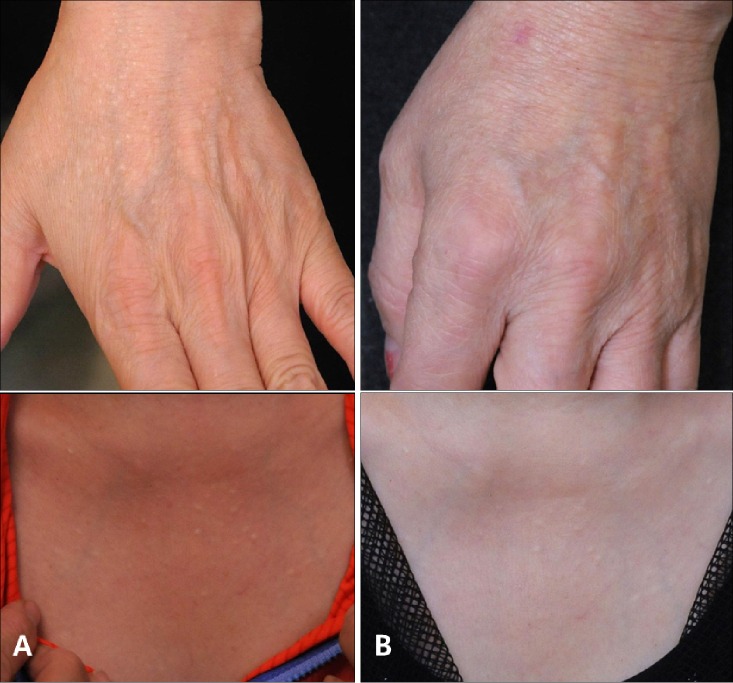
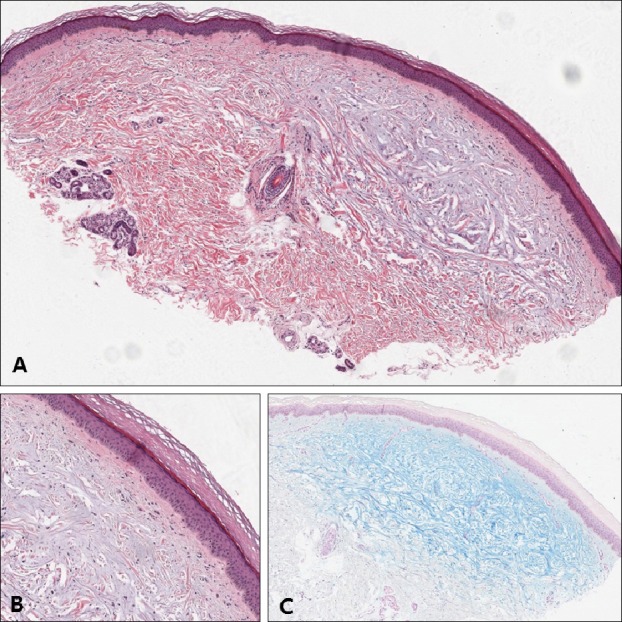
A 53-year-old woman presented with asymptomatic 1~3 mm flesh-colored papules symmetrically located on both dorsum of hands and wrists, and on anterior chest. It first appeared 7~8 years ago and did not disappear. She was previously healthy and no abnormalities were found in annual check-up. Her two brothers had same lesions on their dorsum of hands. Biopsy was done on the hand lesion and discrete mucin depositions in upper dermis with spared grenz zone confirmed the diagnosis of APPM (Fig. 1).
Fig. 1. (A) Epidermis is normal. Deposition of bluish material is seen at upper to mid dermis, fairly discrete (H&E, ×20). (B) Small grenz zone was spared. Fibroblasts were present among the deposition but not seem to be proliferated. Inflammatory cell infiltration in dermis is barely seen (H&E, ×100). (C) The bluish material was positive with alcian blue (Alcian blue pH 2.5, ×20).
Tacrolimus ointment 0.1% was applied once a day for 15 weeks but responded partially (Fig. 2).
Fig. 2. (A) Left dorsum of hand and anterior chest before treatment. (B) Left dorsum of hand and anterior chest after 15 weeks of tacrolimus ointment 0.1% application.
In our patient, anterior chest was also involved and differential diagnosis with discrete papular lichen myxedematosus (DPLM–other subtype of LM) was needed. In DPLM, papules may occur anywhere on the body, usually asymmetrically. Histologically, DPLM shows more diffuse deposition of mucin than APPM, which interspersed among large collagen bundles in the reticular dermis4. Our patient showed characteristic symmetric distribution of papules on the extensor side of distal upper extremities, and characteristic histologic features such as focal accumulation of mucin in upper dermis and spared grenz zone. These features fit well into the diagnostic criteria of APPM4, so we concluded the diagnosis was APPM. Since we didn't do biopsy on the chest lesion, we couldn't completely rule out the possibility of the chest lesion being DPLM accompanied with APPM of hands. But since there are no reported cases of two other types occurring at once, it is reasonable to think chest lesion was also APPM. There was a report of successful treatment of two DPLM cases with tacrolimus ointment5, but our case was the first reported case to apply tacrolimus in APPM. In contrast to DPLM, our patient showed only partial response despite fifteen weeks of long term application. This might imply that the pathogenesis of two diseases is different. It is known that tacrolimus inhibits tumor necrosis factor (TNF)-α secretion in human keratinocytes and transforming growth factor (TGF)-β-nduced collagen synthesis. TNF-α and TGF-β stimulate glycosaminoglycan synthesis from skin fibroblast, and Rongioletti et al.5 suggested that inhibiting these cytokines might be the mechanism of the tacrolimus on DPLM. The difference of the contributing proportion of these cytokines in DPLM and APPM might be the reason for different response to tacrolimus.
Although the etiology of APPM is yet unknown, our patient showed familial occurrence and it raises the possibility of the genetic role in APPM pathogenesis along with previous reports of familial occurrences1.
Our case gives some notable points on the pathophysiology of APPM, and we hope that this case may add to the growing body of literature of APPM.
References
- 1.Luo DQ, Wu LC, Liu JH, Zhang HY. Acral persistent papular mucinosis: a case report and literature review. J Dtsch Dermatol Ges. 2011;9:354–359. doi: 10.1111/j.1610-0387.2010.07594.x. [DOI] [PubMed] [Google Scholar]
- 2.André Jorge F, Mimura Cortez T, Guadalini Mendes F, Esther Alencar Marques M, Amante Miot H. Treatment of acral persistent papular mucinosis with electrocoagulation. J Cutan Med Surg. 2011;15:227–229. doi: 10.2310/7750.2011.10030. [DOI] [PubMed] [Google Scholar]
- 3.Kim HO, Song JY, Lee SW, Kim CW, Kim HO. A case of acral persistent papular mucinosis. Ann Dermatol. 2002;14:178–180. [Google Scholar]
- 4.Harris JE, Purcell SM, Griffin TD. Acral persistent papular mucinosis. J Am Acad Dermatol. 2004;51:982–988. doi: 10.1016/j.jaad.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 5.Rongioletti F, Zaccaria E, Cozzani E, Parodi A. Treatment of localized lichen myxedematosus of discrete type with tacrolimus ointment. J Am Acad Dermatol. 2008;58:530–532. doi: 10.1016/j.jaad.2006.10.021. [DOI] [PubMed] [Google Scholar]