Abstract
Purpose. Administration of supplemental oxygen is common in paediatric intensive care. We explored the current practice of oxygen administration using a case vignette in paediatric intensive care units (PICU) in the united kingdom. Methods. We conducted an online survey of Paediatric Intensive Care Society members in the UK. The survey outlined a clinical scenario followed by questions on oxygenation targets for 5 common diagnoses seen in critically ill children. Results. Fifty-three paediatric intensive care unit members from 10 institutions completed the survey. In a child with moderate ventilatory requirements, 21 respondents (42%) did not follow arterial partial pressure of oxygen (PaO2) targets. In acute respiratory distress syndrome, cardiac arrest, and sepsis, there was a trend to aim for lower PaO2 as the fraction of inspired oxygen (FiO2) increased. Conversely, in traumatic brain injury and pulmonary hypertension, respondents aimed for normal PaO2 even as the FiO2 increased. Conclusions. In this sample of clinicians PaO2 targets were not commonly used. Clinicians target lower PaO2 as FiO2 increases in acute respiratory distress syndrome, cardiac arrest, and sepsis whilst targeting normal range irrespective of FiO2 in traumatic brain injury and pulmonary hypertension.
1. Introduction
The administration of supplemental oxygen is common in the critically ill. The aim is to augment oxygen delivery to the tissues [1]. Hyperoxia can lead to production of reactive oxygen species and cell injury [2, 3]. Conversely, hypoxia causes cell death. The “ideal” PaO2 target range is unclear. Consequently clinical practice varies.
Eastwood et al. reported that 77% of intensivists in Australia and New Zealand prescribed oxygen saturation targets. Clinicians working in regional centers were less concerned with oxygen toxicity [4]. De Graaff et al. explored the response of Dutch clinicians to arterial blood gas values (ABG) in tertiary intensive care units. The FiO2 was reduced in only 25% of situations with a PaO2 > 16 kPa [5].
The etiology and evolution of paediatric critical illness are different to adults. Multiorgan failure (MOF) occurs early in children and they have better survival [6, 7]. Nonetheless, the duration of mechanical ventilation and length of stay in the paediatric intensive care unit is increasing [8]. This survey aimed to describe prevalent paediatric intensive care practice, existence of weaning protocols, and if a clinical equipoise exists between liberal and restrictive oxygenation targets.
2. Material and Methods
All the members of the Paediatric Intensive Care Society (PICS), UK, were requested to complete an online survey. PICS consists of nursing, medical, and allied health professionals working in paediatric intensive care units. The practitioners from the neonatal intensive care units in UK were not approached, as their patient profile is significantly different.
The survey was designed by the authors and published using a survey website (https://opinio.ucl.ac.uk). Demographic data including age, ICU type, their seniority, and years of practice were sought. The study was discussed with the chair of Bloomsbury Research and Ethics Committee (London, UK). We were advised that a formal ethics review was not required.
The survey outlined the following clinical scenario: a 1-year-old patient with no premorbid conditions is ventilated with peak inspiratory pressure of 28 cm H2O, positive end expiratory pressure of 6 cm H2O, respiratory rate of 20 breaths per min, and FiO2 of 0.8. His peripheral oxygen saturation (pulse oximetry), heart rate, blood pressure, and mean blood pressure are 94%, 125 beats per min, 85/56 mmHg, and 66 mmHg, respectively. He has bilaterally equal and reactive pupils measuring 3 mm. He is sedated on intravenous morphine and midazolam. He is not paralysed. Latest arterial blood gas values are as follows: pH: 7.32, PCO2: 6.2 kPa, PaO2: 10 kPa, BE: -ve 4, and lactate: 1.5 mmol/L. The PIM2 predicted risk of mortality is 8.8%. He has been ventilated for 2 days.
With the same clinical history, clinicians were asked to decide on the oxygenation targets when the potential diagnosis is ARDS, CA, Sepsis, TBI, or PHTN.
A further question explored if weaning protocols were in place in their units. The need for a randomised control trial (RCT) with tight arterial oxygenation targets was explored.
3. Results
Only 30% (53) of those whom were invited to participate in the online survey responded. The majority of respondents worked in moderate sized ICUs, with admission rates between 500 and 1000 patients per annum. The characteristics of the respondents are presented in Table 1.
Table 1.
Characteristics of respondents.
| Number of admissions/year to your intensive care unit | Number (%) |
|---|---|
| <500 | 9 (17.6) |
| 501–1000 | 24 (47) |
| 1001–1500 | 13 (25.5) |
| >1500 | 5 (9.8) |
| No response | 2 |
|
| |
| Cardiosurgical center | 33 (66) |
|
| |
| Neurosurgical center | 35 (67) |
|
| |
| Grade of respondent | |
|
| |
| Consultant | 25 (48) |
| Senior nurse | 10 (19.2) |
| Senior fellow | 12 (23) |
| Junior fellow | 5 (9.6) |
| No response | 1 |
|
| |
| Number of years of practice in intensive care | |
|
| |
| 2–5 years | 13 (25.5) |
| 5-6 years | 13 (25.5) |
| >10 years | 25 (49) |
| No response | 2 |
The majority of units (96%) had an alarm target on their oxygen saturation monitor. Thirty-eight respondents (73%) worked in units that did not have an oxygen weaning protocol for mechanically ventilated patients. The units with admissions more than 1500 were less likely to have a weaning protocol compared to those between 500 and 1500 admissions.
For the given clinical scenario, 21 respondents (42%) did not follow PaO2 targets. Of the rest, 21 clinicians (42%) targeted PaO2 between 8.1 and 10 kPa. Only 8 (16%) aimed for the normal range (10.1–13 kPa).
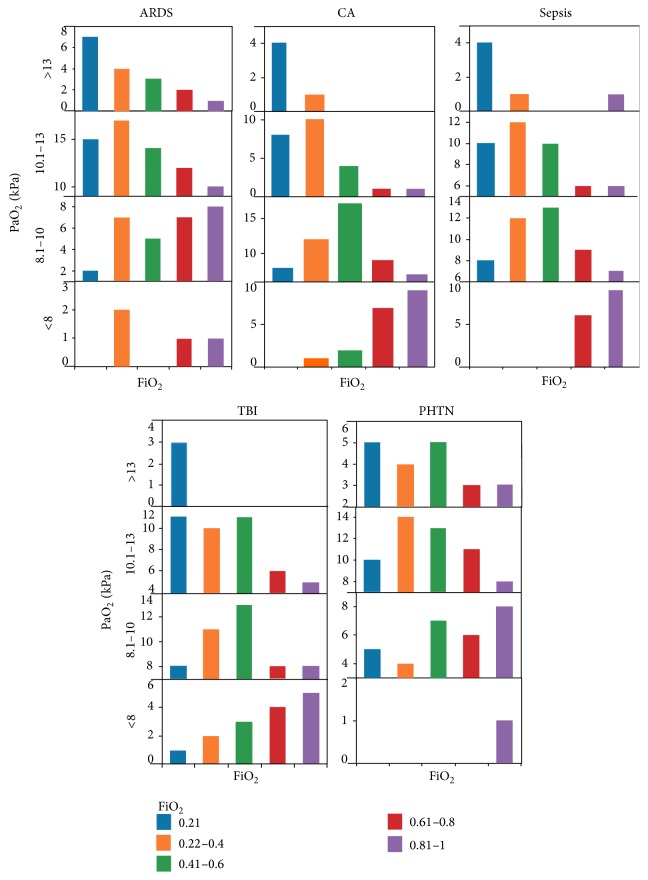
In ARDS, CA, and sepsis, there was a tendency to aim for lower PaO2 (<10 kPa) as the FiO2 increased. This was noticeable when the FiO2 was more than 0.4 (45%) which equates to a PaO2/FiO2 ratio of less than 200. Following TBI and in PHTN, there was a propensity to aim for normal PaO2 (10.1–13 kPa) even as the FiO2 rose (28–33% when FiO2 > 0.4). In TBI, the proportion of respondents targeting a lower PaO2 increased when the FiO2 was more than 0.8 (8%). A proportion of respondents targeted PaO2 ranges above normal (15%). In PHTN, normal range remained the preferred range throughout the range of FiO2 (Figure 1).
Figure 1.
The profile of PaO2 (y-axis) and FiO2 (x-axis) targeted in 5 clinical scenarios in a child with moderate ventilatory requirements. The PaO2 ranges from <8 kPa in the bottom panel to >13 kPa in the top panel within each scenario. FiO2 ranges from 0.21 (blue) through to 0.81–1 (purple). The three scenarios in the upper section show a pattern of more restrictive PaO2 targets with increasing FiO2. The 2 scenarios in the lower section show that higher normal PaO2 ranges are targeted irrespective of increasing FiO2.
The initial scenario was further extended as “no improvement after 24 hours of intensive care.” The management strategy did not change in this setting.
Thirty-nine percent considered it ethical to conduct a RCT with tight arterial oxygenation target whilst 11% did not. The remaining respondents were undecided.
4. Discussion
Our survey shows that, practice variation notwithstanding, there seems to be a general consensus to aim for lower PaO2 in the setting of ARDS, CA, and sepsis. The results are consistent with higher PaO2 targets being chosen in children following TBI and in PHTN. Only a small proportion of respondents felt a RCT with tight oxygenation target would be unethical.
Paediatric intensivists tolerate a low SpO2 target (88%) with a low tidal volume strategy for ARDS [9]. Our findings concur. A recent point prevalence study reported that adult intensive care practitioners aim to prevent low oxygen saturation (SpO2 < 90%) but fail to address high saturations [10]. This is in the face of mounting evidence of harm from hyperoxia [11]. Should we aim for a restrictive oxygenation target in critically ill patients? The “HOT or NOT” trial showed that separation between titrated oxygen target and standard target is possible in intensive care [12]. A recent multicenter study demonstrated no difference in 90-day mortality between mechanically ventilated patients randomised to a conservative (pulse oximetry: 88–92%) and liberal oxygenation targets (>96%) [13]. A larger randomised control trial is awaited.
The main limitation of this survey is the likely low response rate. At the time of the survey the membership of the society was not well defined. Responses were not sought beyond a single e-mail. The low number of respondents from junior staff perhaps suggests that considerable experience is needed to set distinct targets in these clinical scenarios. Despite this limitation, the results indicate that restrictive targets are aimed for in certain scenarios.
We had intended to analyse Cohen's kappa to look at interrater agreement. However, due to the small sample size a formal statistical analysis was not attempted.
5. Conclusions
In this study variability and lack of consensus are consistent with an assumption of clinical equipoise. Supplemental oxygen administration practices and oxygenation target practices vary. A majority of respondents worked in units with no oxygen weaning protocol. A proportion of clinicians do not follow PaO2 targets. Clinicians aim for lower PaO2 thresholds in ARDS, CA, and sepsis whilst aiming for the normal range in TBI and PHTN. The lack of consensus and the large variability in practice demonstrate equipoise. This should be addressed with a feasibility trial comparing restrictive to standard oxygenation targets in critically ill children to lead up to a future RCT.
Disclosure
Dr. Raman is a holder of HCA fellowship.
Competing Interests
The authors declare that they have no competing interests.
References
- 1.Treacher D. F., Leach R. M. ABC of oxygen: oxygen transport—1. Basic principles. British Medical Journal. 1998;317(7168):1302–1306. doi: 10.1136/bmj.317.7168.1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Helmerhorst H. J. F., Schultz M. J., van der Voort P. H. J., de Jonge E., van Westerloo D. J. Bench-to-bedside review: the effects of hyperoxia during critical illness. Critical Care. 2015;19, article 284 doi: 10.1186/s13054-015-0996-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Magder S. Reactive oxygen species: toxic molecules or spark of life? Critical Care. 2006;10(1, article 208):1–8. doi: 10.1186/cc3992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eastwood G. M., Reade M. C., Peck L., Jones D., Bellomo R. Intensivists' opinion and self-reported practice of oxygen therapy. Anaesthesia and Intensive Care. 2011;39(1):122–126. doi: 10.1177/0310057X1103900120. [DOI] [PubMed] [Google Scholar]
- 5.De Graaff A. E., Dongelmans D. A., Binnekade J. M., De Jonge E. Clinicians' response to hyperoxia in ventilated patients in a Dutch ICU depends on the level of FiO2 . Intensive Care Medicine. 2011;37(1):46–51. doi: 10.1007/s00134-010-2025-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vincent J.-L., Mendonça A. D., Cantraine F., et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Critical Care Medicine. 1998;26(11):1793–1800. doi: 10.1097/00003246-199811000-00016. [DOI] [PubMed] [Google Scholar]
- 7.Leteurtre S., Duhamel A., Grandbastien B., et al. Daily estimation of the severity of multiple organ dysfunction syndrome in critically ill children. Canadian Medical Association Journal. 2010;182(11):1181–1187. doi: 10.1503/cmaj.081715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Network PICA. PICANet Annual Report 2013. PICANet; 2013. [Google Scholar]
- 9.Santschi M., Randolph A. G., Rimensberger P. C., Jouvet P. Mechanical ventilation strategies in children with acute lung injury: a survey on stated practice pattern. Pediatric Critical Care Medicine. 2013;14(7):e332–e337. doi: 10.1097/pcc.0b013e31828a89a2. [DOI] [PubMed] [Google Scholar]
- 10.Young P. J., Beasley R. W., Capellier G., Eastwood G. M., Webb S. A. R. Oxygenation targets and monitoring in the critically ill: a point prevalence study of clinical practice in australia and New Zealand. Critical Care and Resuscitation. 2015;17(3):202–207. [PubMed] [Google Scholar]
- 11.Damiani E., Adrario E., Girardis M., et al. Arterial hyperoxia and mortality in critically ill patients: a systematic review and meta-analysis. Critical Care. 2014;18(1, article 711) doi: 10.1186/s13054-014-0711-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Young P., Bailey M., Bellomo R., et al. HyperOxic Therapy OR NormOxic Therapy after out-of-hospital cardiac arrest (HOT OR NOT): a randomised controlled feasibility trial. Resuscitation. 2014;85(12):1686–1691. doi: 10.1016/j.resuscitation.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 13.Panwar R., Hardie M., Bellomo R., et al. Conservative versus liberal oxygenation targets for mechanically ventilated patients—a pilot multicenter randomized controlled trial. American Journal of Respiratory and Critical Care Medicine. 2016;193(1):43–51. doi: 10.1164/rccm.201505-1019oc. [DOI] [PubMed] [Google Scholar]