Abstract
Hypertension is a major global health burden and a leading risk factor for cardiovascular diseases. Although its heritability has been documented previously, contributing loci identified to date account for only a small fraction of blood pressure (BP) variation, which strongly suggests the existence of undiscovered variants. To identify novel variants, we conducted a three staged genetic study in 21,990 hypertensive cases and normotensive controls. Four single nucleotide polymorphisms (SNPs) at three new genes (L3MBTL4 rs403814, Pmeta = 6.128 × 10−9; LOC729251, and TCEANC) and seven SNPs at five previously reported genes were identified as being significantly associated with hypertension. Through functional analysis, we found that L3MBTL4 is predominantly expressed in vascular smooth muscle cells and up-regulated in spontaneously hypertensive rats. Rats with ubiquitous over-expression of L3MBTL4 exhibited significantly elevated BP, increased thickness of the vascular media layer and cardiac hypertrophy. Mechanistically, L3MBTL4 over-expression could lead to down-regulation of latent transforming growth factor-β binding protein 1 (LTBP1), and phosphorylation activation of the mitogen-activated protein kinases (MAPK) signaling pathway, which is known to trigger the pathological progression of vascular remodeling and BP elevation. These findings pinpointed L3MBTL4 as a critical contributor to the development and progression of hypertension and uncovers a novel target for therapeutic intervention.
Due to its high prevalence, hypertension is a major global health burden and represents an increased risk for cardiovascular diseases and premature death1,2,3,4,5. Although lifestyle is known to influence blood pressure (BP) in previous studies6,7, a substantial contribution of genetic factors has been documented by a number of genome-wide association studies (GWASs)8,9. However, the contributing loci identified to date account for only a small fraction of BP variation in the population and point to the existence of additional susceptibility loci.
Therefore, we performed a GWAS and two-staged follow-up study to identify novel genetic variants contributing to essential hypertension in the Chinese population. We first report a genome-wide significant locus in L3MBTL4 gene (rs403814) and comprehensively illustrate its pathogenic effects and probable mechanisms as a potential inducer of hypertension. We estimated the expression level of L3MBTL4 in spontaneously hypertensive rats (SHRs) and Wistar-Kyoto rats (WKYs) and found that L3MBTL4 is predominantly expressed in vascular smooth muscle cells (SMCs) and upregulated in SHRs. Furthermore, rats over-expressing L3MBTL4 exhibited significantly elevated BP and cardiac hypertrophy. We observed phosphorylation activation of the mitogen-activated protein kinases (MAPK) signaling pathway in the L3MBTL4 over-expression model, which may be a trigger of vascular remodeling and BP elevation. A direct binding of L3MBTL4 with LTBP1 was also detected, leading to decrease of the target gene. Moreover, copy number variation (CNV) burden analysis suggested a pathogenic role of 16q24.2 for hypertension.
Results
GWAS of Hypertensive Cases and Normotensive Controls
In stage 1, a genome-wide association analysis was performed in 528 Chinese individuals (276 cases and 252 controls) to identify genomic loci associated with BP using an extreme case-control strategy (Supplementary Methods, Supplementary Fig. S1, and Supplementary Table S1)10. In this stage, hypertensive cases were defined as having SBP ≥150 mmHg and/or DBP ≥ 90 mmHg in untreated subjects with an age of onset of ≤50 years. Normotensive controls were defined as having SBP ≤ 125 mmHg and DBP ≤ 80 mmHg without antihypertensive treatment. All controls were ≥65 years of age. Following a clean-up of the data, 518 samples (271 cases and 247 controls) and 727,172 SNPs remained for subsequent analyses. From this filtered data set, we found the genomic inflation factor λ value to be 1.02, indicating the absence of systemic confounding factors across the GWAS samples (Supplementary Fig. S2). We set a threshold of P < 5 × 10−4 in this stage. The association of genomic loci with hypertension and/or SBP and DBP identified a total of 358 SNPs within 152 chromosome regions beyond the significance threshold (Supplementary Fig. S3).
Two Follow-up Studies and Combined Analyses
In stage 2, the 358 SNPs and 26 additional SNPs previously reported to be associated with SBP/DBP or hypertension8,9,11 were selected as candidate loci and genotyped in 4,608 Chinese individuals (2,044 cases and 2,564 controls) (Supplementary Methods). In this stage, hypertension and normotension were defined as described for stage 1, while the normotensive controls were ≥55 years of age. After data clean-up, 371 SNPs and 4,502 samples (1,994 cases and 2,508 controls) remained. We used a false discovery rate (FDR) threshold of 0.212,13 and therefore expected a maximum of only 20% of declared discoveries to be false. After adjustment for multiple testing with FDR, 18 SNPs reached the level of FDR < 0.2 and were selected for stage 3 (Supplementary Table S2). These loci identified by these 18 SNPs consisted of several previously reported genes including FGF5, ATP2B1, MTHFR, CASZ1, CYP11B2, CYP17A1, ADRB1, and HECTD48,9,11, as well as seven new genes (L3MBTL4, KIRREL, C9orf98, GALNT18, LOC729251, NLRP1 and TCEANC) that may be associated with hypertension. We also generated haplotype analysis in stage 2, and no haplotype was associated with hypertension (Supplementary Table S3).
In stage 3, 17,318 samples (7,796 cases and 9,522 controls) selected from three cohorts (Shantou, Shanghai, and Jidong) were genotyped for the 18 SNPs identified from stage 2 (Supplementary Methods). In this stage, hypertension and normotension were defined as described for stage 1 but without age limitation. Following data clean-up, 16,970 samples (7,639 cases and 9,331 controls) were retained. We next performed a combined analysis of data from stages 1 to 3 and thereby identified L3MBTL4 as a novel susceptibility gene significantly associated with hypertension (meta-analyses odds ratio (OR) = 1.15, 95% confidence interval (CI) = 1.07–1.23, Pmeta = 6.128 × 10−9). In addition, we identified three SNPs in two novel genes (LOC729251 and TCEANC) and seven SNPs in five previously reported genes (FGF5, ATP2B1, CYP17A1, MTHFR and CASZ1) nominally associated with hypertension (Pmeta < 0.05) (Table 1).
Table 1. Combined results of the 18 SNPs genotyped in stage 1, 2 and 3.
| chr | SNP ID | position | minor/major allele | gene | location | group | OR(95% CI) | P |
|---|---|---|---|---|---|---|---|---|
| 1 | rs12749808* | 158065762 | C/T | KIRREL | UTR | stage1 | 1.47 (1.15, 1.88) | 1.315 × 10−4 |
| stage2 | 1.09 (1.00, 1.18) | 0.004 | ||||||
| Jidong | 1.02 (0.93, 1.12) | 0.678 | ||||||
| Shanghai | 0.82 (0.69,1.02) | 0.541 | ||||||
| Shantou | 0.99 (0.92, 1.06) | 0.776 | ||||||
| meta | 1.03 (0.86, 1.20) | 0.687 | ||||||
| 1 | rs17367504 | 11862778 | G/A | MTHFR | INTRON | stage2 | 1.42 (1.20, 1.67) | 3.918 × 10−5 |
| Jidong | 1.20 (0.67, 2.17) | 0.197 | ||||||
| Shanghai | 1.05 (0.93, 1.20) | 0.404 | ||||||
| Shantou | 1.22 (1.03, 1.45) | 0.009 | ||||||
| meta | 1.21 (1.09, 1.30) | 3.810 × 10−4 | ||||||
| 1 | rs880315 | 10796866 | A/G | CASZ1 | INTRON | stage2 | 0.88 (0.80, 0.96) | 0.003 |
| Jidong | 0.98 (0.89, 1.08) | 0.771 | ||||||
| Shanghai | 0.93 (0.86, 0.99) | 0.009 | ||||||
| Shantou | 0.86 (0.80, 0.93) | 0.000924 | ||||||
| meta | 0.91 (0.86, 0.95) | 1.814 × 10−4 | ||||||
| 4 | rs1458038 | 81164723 | A/G | FGF5 | UTR | stage2 | 1.30 (1.20, 1.42) | 8.853 × 10−10 |
| Jidong | 0.96 (0.88, 1.06) | 0.524 | ||||||
| Shanghai | 1.12 (1.05, 1.20) | 0.005 | ||||||
| Shantou | 1.10 (1.03, 1.18) | 5.235 × 10−5 | ||||||
| meta | 1.12 (1.01, 1.24) | 0.037 | ||||||
| 4 | rs16998073 | 81184341 | A/T | FGF5 | UTR | stage2 | 1.32 (1.21, 1.44) | 1.799 × 10−10 |
| Jidong | 0.99 (0.90, 1.09) | 0.847 | ||||||
| Shanghai | 1.14 (1.06, 1.22) | 1.495 × 10−4 | ||||||
| Shantou | 1.12 (1.04, 1.20) | 3.182 × 10−5 | ||||||
| meta | 1.14 (1.03, 1.26) | 0.007 | ||||||
| 8 | rs1799998 | 143999600 | C/T | CYP11B2 | UTR | stage2 | 0.80 (0.73, 0.87) | 1.099 × 10−6 |
| Jidong | 1.04 (0.94, 1.16) | 0.418 | ||||||
| Shanghai | 0.93 (0.86, 1.00) | 0.048 | ||||||
| Shantou | 0.94 (0.87, 1.01) | 0.469 | ||||||
| meta | 0.92 (0.84, 1.02) | 0.166 | ||||||
| 9 | kgp9568150* | 66749500 | A/G | C9orf98 | INTRON | stage1 | 1.85 (1.31, 2.61) | 4.385 × 10−4 |
| stage2 | 0.82 (0.73, 0.92) | 5.812 × 10−4 | ||||||
| Jidong | 1.03 (0.91, 1.17) | 0.645 | ||||||
| Shanghai | 1.00 (0.91,1.10) | 0.127 | ||||||
| Shantou | 1.01 (0.92, 1.11) | 0.846 | ||||||
| meta | 1.03 (0.90, 1.18) | 0.714 | ||||||
| 10 | rs11191548 | 104846178 | C/T | CYP17A1 | UTR | stage2 | 0.85 (0.77, 0.93) | 5.388 × 10−4 |
| Jidong | 0.92 (0.83, 1.02) | 0.160 | ||||||
| Shanghai | 0.95 (0.87, 1.02) | 0.345 | ||||||
| Shantou | 0.92 (0.85, 0.99) | 0.027 | ||||||
| meta | 0.91 (0.85, 0.95) | 7.584 × 10−5 | ||||||
| 10 | rs1801253 | 115805056 | C/G | ADRB1 | CODING | stage2 | 0.89 (0.81, 0.98) | 0.008 |
| Jidong | 1.01 (0.91, 1.13) | 0.644 | ||||||
| Shanghai | 0.99 (0.91, 1.07) | 0.363 | ||||||
| Shantou | 0.99 (0.92, 1.07) | 0.564 | ||||||
| meta | 0.97 (0.92, 1.02) | 0.251 | ||||||
| 11 | rs12421938* | 11422750 | G/A | GALNT18 | INTRON | stage1 | 0.63 (0.42, 0.96) | 3.522 × 10−4 |
| stage2 | 0.81 (0.71, 0.93) | 0.002 | ||||||
| Jidong | 0.85 (0.73, 1.00) | 0.051 | ||||||
| Shanghai | 0.91 (0.81, 1.01) | 0.166 | ||||||
| Shantou | 1.12 (1.08, 1.23) | 0.034 | ||||||
| meta | 0.89 (0.77, 1.02) | 0.124 | ||||||
| 12 | rs17249754 | 90060586 | A/G | ATP2B1 | INTERGENIC | stage2 | 0.85 (0.78, 0.92) | 1.785 × 10−4 |
| Jidong | 0.99 (0.90, 1.10) | 0.967 | ||||||
| Shanghai | 0.94 (0.88, 1.01) | 0.139 | ||||||
| Shantou | 0.85 (0.79, 0.91) | 8.582 × 10−4 | ||||||
| meta | 0.90 (0.84, 0.97) | 0.007 | ||||||
| 12 | rs2681472 | 90008959 | C/T | ATP2B1 | INTRON | stage2 | 0.87 (0.80, 0.95) | 0.001 |
| Jidong | 1.01 (0.91, 1.11) | 0.950 | ||||||
| Shanghai | 0.94 (0.87, 1.01) | 0.157 | ||||||
| Shantou | 0.87 (0.81, 0.94) | 4.243 × 10−4 | ||||||
| meta | 0.91 (0.85, 0.98) | 1.443 × 10−5 | ||||||
| 12 | rs2074356 | 112645401 | T/C | HECTD4 | INTRON | stage2 | 0.78 (0.69, 0.89) | 1.632 × 10−4 |
| Jidong | 0.99 (0.86, 1.15) | 0.920 | ||||||
| Shanghai | 0.92 (0.83, 1.01) | 0.099 | ||||||
| Shantou | 1.03 (0.94, 1.13) | 0.224 | ||||||
| meta | 0.93 (0.83, 1.04) | 0.288 | ||||||
| 16 | rs4243170* | 79437209 | A/G | LOC729251 | INTERGENIC | stage1 | 0.59 (0.44, 0.78) | 2.782 × 10−4 |
| stage2 | 0.87 (0.79, 0.96) | 0.005 | ||||||
| Jidong | 0.95 (0.85, 1.06) | 0.379 | ||||||
| Shanghai | 0.95 (0.88, 1.03) | 0.199 | ||||||
| Shantou | 0.98 (0.91, 1.06) | 0.839 | ||||||
| meta | 0.88 (0.78, 1.00) | 0.029 | ||||||
| 17 | rs17225738* | 5861557 | A/G | NLRP1 | INTERGENIC | stage1 | 0.63 (0.49, 0.82) | 3.614 × 10−4 |
| stage2 | 0.89 (0.81, 0.97) | 0.008 | ||||||
| Jidong | 1.01 (0.91, 1.12) | 0.655 | ||||||
| Shanghai | 1.02 (0.95, 1.09) | 0.180 | ||||||
| Shantou | 0.99 (0.92, 1.06) | 0.561 | ||||||
| meta | 0.91 (0.81, 1.02) | 0.210 | ||||||
| 18 | rs403814* | 6282593 | G/T | L3MBTL4 | INTRON | stage1 | 1.39(1.01, 1.94) | 4.699 × 10−4 |
| stage2 | 1.24 (1.12, 1.36) | 1.321 × 10−5 | ||||||
| Jidong | 1.14 (1.01, 1.29) | 0.006 | ||||||
| Shanghai | 1.15 (1.06, 1.25) | 0.003 | ||||||
| Shantou | 1.06 (0.98, 1.14) | 0.177 | ||||||
| meta | 1.15 (1.07, 1.23) | 6.128 × 10−9 | ||||||
| 23 | rs2361159* | 13681115 | C/T | TCEANC | CODING | stage1 | 1.21 (1.12, 1.29) | 2.813 × 10−4 |
| stage2 | 1.10 (1.02, 1.15) | 0.008 | ||||||
| Jidong | 1.20 (0.89, 1.52) | 0.991 | ||||||
| Shanghai | 1.03 (1.01, 1.10) | 0.034 | ||||||
| Shantou | 1.04 (0.98, 1.14) | 0.383 | ||||||
| meta | 1.07 (1.02, 1.12) | 0.002 | ||||||
| 23 | rs5935649* | 13681638 | C/T | TCEANC | CODING | stage1 | 1.24 (1.10, 1.30) | 4.687 × 10−4 |
| stage2 | 1.11 (0.89, 1.09) | 0.006 | ||||||
| Jidong | 1.21 (1.04, 1.55) | 0.825 | ||||||
| Shanghai | 1.02 (1.00, 1.06) | 0.021 | ||||||
| Shantou | 1.06 (0.97, 1.15) | 0.226 | ||||||
| meta | 1.08 (1.03, 1.14) | 7.911 × 10−4 |
CHR, chromosome; OR, odds ratio; 95% CI, 95% confidence interval; stage 1, the genome-wide association study; stage 2, the follow-up study; stage 3, the replication study; meta, meta-analysis of stages 1, 2 and 3. SNPs with bold font are significantly associated with hypertension (P < 0.05). Newly identified loci are indicated by asterisks.
Basing on GWAS data of stage 1 control group, 5 SNPs on L3MBTL4 gene were genotyped in Shantou, Shanghai and Jidong cohort, which were in linkage disequilibrium with rs403815 (r2 > 0.5) and MAF > 0.05. Association analysis of each cohort and combined results implied these 5 SNPs did not associated with hypertension (Supplementary Table S4).
CNV Burden Analyses
The total CNV burden in hypertensive cases was significantly greater than that in controls (Supplementary Methods and Supplementary Table S5). Eleven CNV regions were implicated by PLINK 1.0714 and further validated across 989 cases and 1,022 controls randomly selected from stage 2 by multiplex ligation-dependent probe amplification (MLPA) (Supplementary Table S6 and Supplementary Table S7). Among these, only 16q24.2 emerged as having a statistically significant association with hypertension (P = 0.048) (Supplementary Table S8).
Functional Analyses of the L3MBTL4 Locus
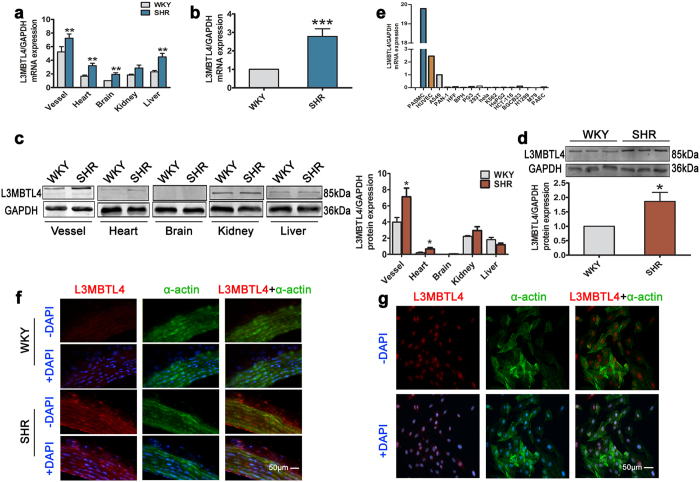
The newly identified SNP rs403814 is located in an intron of the L3MBTL4 gene at 18p11.31 (Supplementary Fig. S4). L3MBTL4 is known as lethal(3) malignant brain tumor-like protein 4. To determine the expression and distribution of L3MBTL4 in hypertension, we performed q-PCR and Western blotting, and compared L3MBTL4 mRNA and protein expression from different tissues of SHRs, the most widely-used animal model for hypertension, and WKYs, a normotensive reference group. We found more abundant L3MBTL4 mRNA and protein expression in the blood vessels of SHRs (Fig. 1a,c) and further validated the enhancement in vessels using another rats (Fig. 1b,d). In different human cell lines, we found L3MBTL4 to be highly expressed in SMCs and endothelial cells (Fig. 1e). Double immunofluorescence staining revealed co-localization of L3MBTL4 with α-actin, indicating that L3MBTL4 is predominant in the medial layer of the vasculature (Fig. 1f). Due to the limitation of frozen sections staining in clarity and the complex structure of aortic tissue, we are not sure about the subcellular localization of L3MBTL4, although L3MBTL4 mainly co-localized with α-actin, and distributed in the medial layer of the vasculature. To address this issue, further analysis was performed using vascular SMCs (Fig. 1g). According to our findings, the cellular localization of L3MBTL4 is mainly in nucleus, which is consistent with the product datasheet of L3MBTL4 antibody.
Figure 1. Expression and localization of L3MBTL4.
(a) Relative mRNA expression of L3MBTL4 in Wistar-Kyoto rats (WKYs) and spontaneously hypertensive rats (SHRs) (n = 8 each group). (b) Quantification of L3MBTL4 mRNA level in the blood vessels (n = 12 per group). (c) Western blot analysis of L3MBTL4 protein expression relative to GAPDH from tissues (n = 3–6 each group). (d) Increased protein levels of L3MBTL4 in the vessel from SHR are verified by western blot (n = 4 each group). (e) Expression of L3MBTL4 mRNA in different cell lines. (f–g) Representative immunofluorescence images of L3MBTL4 (red) and α-actin (green) in the vessels from WKY and SHR (f), as well as cultured vascular smooth muscle cells (g). Nuclei are stained with DAPI (blue). Scale bars are 50 μm. n = 3 independent experiments for (e–g), *p < 0.05, **p < 0.01, ***p < 0.001 compared to WKY. All data represent mean ± s.e.m.
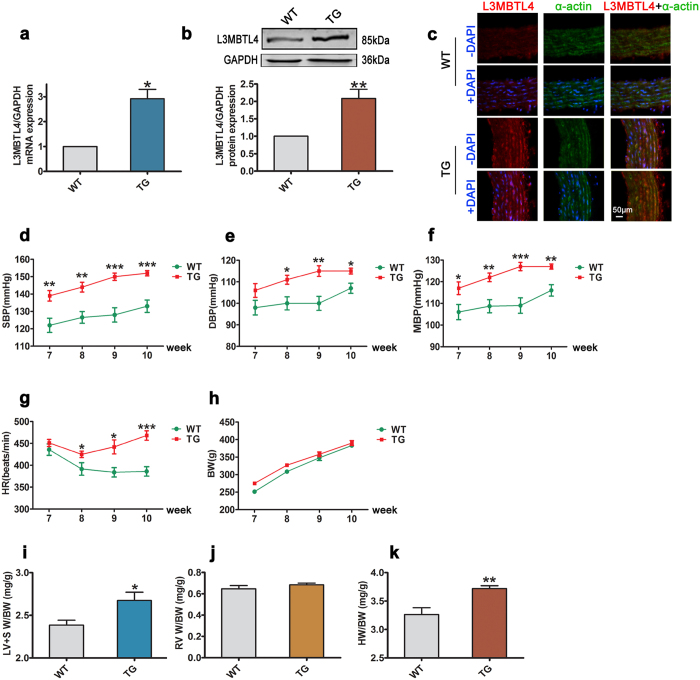
To investigate whether L3MBTL4 participates causally in the development of hypertension, we constructed L3MBTL4 transgenic rats (TGs) and confirmed increased L3MBTL4 expression, at both the mRNA and protein levels in the vasculature (Fig. 2a–c). When compared to wild-type rats (WTs), TGs had similar body weights (Fig. 2h) but higher SBP, DBP, MBP and HR (Fig. 2d–g). TGs also had higher left ventricle and septum weight/body weight ratios (LV + SW/BW) and heart weight/body weight ratios (HW/BW), but no substantial changes were observed in the right ventricle weight/body weight ratio (RVW/BW) (Fig. 2i–k). These findings suggest that L3MBTL4 might be an important inducer of elevated BP and cardiac hypertrophy. To explore the functional role of L3MBTL4 more specifically in the vasculature, we undertook a series of histological analyses. The results of these showed an increase in the thickness and area of the vasculature media layer in TGs compared to WTs, as well as a higher media/lumen area ratio in TGs, without any difference in vessel diameter or lumen area between TGs and WTs (Fig. 3a–f).
Figure 2. Blood pressure and cardiac parameters of L3MBTL4 transgenic rats.
(a) Relative mRNA expression of L3MBTL4 in the blood vessels from wild type rats (WTs) and transgenic rats (TGs) (n = 7 each group). (b) L3MBTL4 protein levels in the vasculature are measured by western blot analysis (n = 7 per group). (c) Representative immunofluorescence images of L3MBTL4 (red) and α-actin (green) in the vessels from WTs and TGs. Nuclei are stained with DAPI (blue). Scale bars are 50 μm. n = 3 independent experiments. (d–h) Systolic blood pressure (SBP), diastolic blood pressure (DBP), mean blood pressure (MBP), heart rate (HR) and body weight (BW) of WTs and TGs (n = 8 each group). (j,k) Quantitative analysis of left ventricle + septum weight/body weight (LV + SW/BW), right ventricle weight/body weight (RVW/BW) and heart weight/body weight (HW/BW) ratios between groups (n = 6 each group). *p < 0.05, **p < 0.01, ***p < 0.001 compared to WT. All data represent mean ± s.e.m.
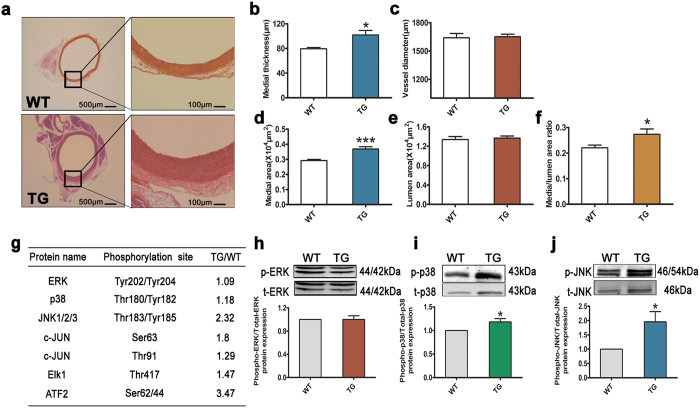
Figure 3. L3MBTL4 induces vascular remodeling via MAPK signaling pathway.
(a) Representative photomicrographs of hematoxylin-eosin staining in blood vessels from wild type rats (WTs) and transgenic rats (TGs) (n = 7 each group). (b–f) The media thickness, vessel diameter, media area, lumen area and media/lumen area ratio of aortas is quantified (n = 7 per group). Scale bars are 500 μm and 100 μm. (g) Changed phosphorylated proteins in the vessels of TGs compared to WTs are identified by phospho-antibody microarray. Listed are proteins in mitogen-activated protein kinases (MAPK) family. (h–j) Western Blot analysis validate the phosphorylation levels of extracellular signal-regulated kinase (ERK), p38MAPK and c-Jun N-terminal kinase (JNK) in the aortas from WTs and TGs; n = 7 per group for (h,j), n = 6 each group for (i). *p < 0.05, ***p < 0.001 compared to WT. All data represent mean ± s.e.m.
To identify the signaling pathways involved in vascular remodeling mediated by L3MBTL4, we performed high-throughput protein phosphorylation profiling on cell lysates from the aortas of WTs versus TGs using the phospho-antibody microarray. The spectrum of proteins whose phosphorylation levels were changed for more than 20% was shown in Supplementary Table S9. Extracellular signal-regulated kinase (ERK), p38MAPK and c-Jun N-terminal kinase (JNK) comprise three key families of MAPK, that play central roles in cellular growth and proliferation. We found the phosphorylation levels of p38MAPK and JNK to be upregulated in TGs compared to WTs, while phospho-ERK hardly differed between the two. Moreover, downstream transcription factors of p38MAPK and JNK, including c-JUN, Elk1, and ATF2 were phosphorylated by more than 20% in TG (Fig. 3g). We further confirmed that L3MBTL4 did affect the phosphorylation of p38MAPK and JNK, but not ERK (Fig. 3h–j). Together, these results led us to speculate that activation of the MAPK pathway may be a central mechanism by which L3MBTL4 affects vascular remodeling.
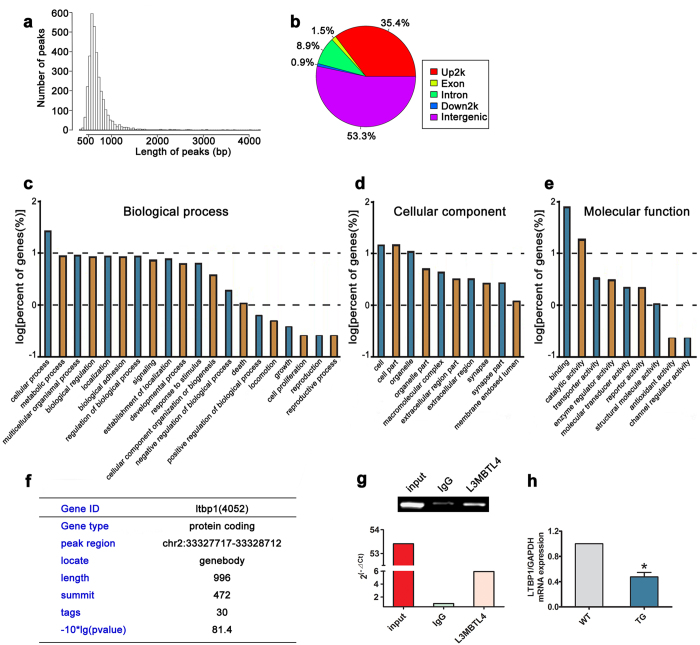
Chromatin DNA from human aortic smooth muscle cells (HASMCs) was immunoprecipitated with L3MBTL4 antibody and sequenced to search for downstream targets of L3MBTL4. 3,289 peaks were yielded and annotated using the UCSC database (University of California Santa Cruz), and 1362 of them were successfully located to a gene (Fig. 4a, Supplementary Table S10). Based on their location in genome elements, these peaks were classified into exon, intron, upstream, intergenic, and downstream regions (Fig. 4b). Gene Ontology analyses of genes mapping to the sequenced peaks indicated enrichment of genes playing crucial roles in biological processes, cellular components and molecular functions (Fig. 4c–e). Among the 1362 genes, we speculated that LTBP1 might participate in the effect of L3MBTL4 on vascular remodeling and hypertension, as there are evidence that anomalous expression of LTBP1 is detected in thoracic aortic aneurysm, and may promote the development of arterial diseases15,16, Therefore the protein coding gene LTBP1 (Gene ID 4052) was further focused (Fig. 4f). LTBP1 was validated for L3MBTL4 association, which showed higher abundance in immunoprecipitated samples compared to the control IgG (Fig. 4g). Repressed transcription activities of LTBP1 was confirmed in the blood vessels of TGs (Fig. 4h). Together, these results strongly suggest that L3MBTL4 directly targets to LTBP1.
Figure 4. ChIP sequencing data of DNA bound by L3MBTL4 in HASMCs.
(a) The distribution of peak length (bp) is indicated. (b) The location of ChIP-sequencing peaks in genome regions. (c–e) Gene Ontology categories of L3MBTL4 binding genes in biological process, cellular component and molecular function. (f) LTBP1 is a target gene interacting with L3MBTL4. (g) The enrichment of LTBP1 peak regions in immunoprecipitated DNA fragments were determined by q-PCR; “input” indicates total DNA, “IgG” represents DNA fragments binding with control IgG, “L3MBTL4” means DNA fragments binding with anti-L3MBTL4 antibody. Data shown are from three independent experiments. (h) Relative mRNA expression of LTBP1 in the vasculature of WTs and TGs (n = 7 for each group). *p < 0.05 compared to WT. All data represent mean ± s.e.m.
Given altered MAPK family upon LTBP2 knockdown17, we speculate the increased activity of MAPKs by L3MBTL4 is possibly due to the down-regulation of LTBP1. To further reveal the direct effects of LTBP1 on MAPKs activation, we inhibited the expression of LTBP1 by siRNA (Supplementary Fig. S5a). It was noted that siRNA target to LTBP1 conduced to a increase of p38MAPK and JNK phosphorylation (Supplementary Fig. S5b,c). Thus LTBP1 is responsible for the activation of MAPKs, and repressed LTBP1 may be a primary factor in the effect of L3MBTL4 on vascular remodeling and hypertension.
Discussion
By using an extreme case-control strategy in a three-staged genetic study of up to 21,990 individuals of Chinese population, we identified eleven loci associated with hypertension (P < 0.05). Seven of these loci in five genes, FGF5, ATP2B1, CYP17A1, MTHFR and CASZ1, were reported as having an association with SBP, DBP and/or hypertension in European populations9,11,17. Replication studies in Asians8,18,19,20 confirmed the relationship between SNPs and BP or hypertension.
In this study, we also identified four new hypertension-associated variants in three genes, LOC729251, L3MBTL4, and TCEANC. Distribution of SNP rs403814 in L3MBTL4 was significantly different between hypertensive participants and controls in the three stages and in the meta-analysis (Pmeta = 6.128 × 10−9, OR = 1.15, 95% CI = 1.07–1.23). SNP rs403814 lies within the intron of the conserved domain on L3MBTL4 gene. We did not find other SNPs on or near gene L3MBTL4 or haplotypes to be associated with hypertension, indicated the important role of rs403814. Moreover, SNP rs403814 in intron of L3MBTL4 might be a binding site for a repressor, and a C to A transition abrogates the interaction with the repressor and thus leads to an up-regulation of L3MBTL4 expression, illustrating the importance of rs403814 in regulation of the gene expression. The three other loci (rs4243170 of LOC729251 gene, rs2361159 and rs5935649 of TCEANC gene) nominally associated with hypertension (5 × 10−4 < Pmeta < 0.05). Larger cohort and more genetic studies are needed to identified the association of these three SNPs and hypertension.
Very few studies have investigated associations between CNVs and hypertension17. To address this question, we sought to identify loci with significant associations with hypertension using a CNV burden analysis. The locus we identified by this approach is 16q24.2. This region has been shown to be associated with a number of diseases21,22 and low HDL-C23, but potential associations with BP have not been uncovered. Chromosome region 16q24.2 includes 9 genes that had no relationship with hypertension or blood pressure were reported. Mechanism that locus on 16q24.2 modulates blood pressure and generation of hypertension is unclear. This novel result promises to shed new light on the association between CNVs and hypertension. Refined analysis and functional investigations are required to understand its role in hypertension.
Previous research has revealed associations of L3MBTL4 with several malignancies24,25,26. Recently, L3MBTL4 has been found to be decreased in breast tumors, suggesting that it may act as a tumor suppressor27. To further understand the biological and cellular functions of L3MBTL4, especially within the context of hypertension, we performed a number of functional studies. Our finding that L3MBTL4 over-expression results in increased BP and heart hypertrophy supports a pathogenic role for L3MBTL4 in the context of hypertension that extends beyond its putative function as a tumor suppressor.
L3MBTL4 over-expression was correlated with aorta thickening and activation of the MAPK signaling pathway. Alterations in the structure of blood vessels are thought to contribute to the development of hypertension by promoting increased vascular resistance28. In the present study, we found evidence of hypertrophic remodeling in the arterial structure, as indicated by an increased medial to lumen area ratio29. Activation of MAPK pathway components including p38MAPK, JNK and other downstream targets are known to drive cellular growth and proliferation, and several previously published studies support the association between activity of the MAPK signaling pathway and vascular remodeling30,31,32,33. These data propose a mechanistic model wherein L3MBTL4 activates the MAPK pathway, triggering vascular remodeling and the eventual development of hypertension. Further studies are still required to understand the contribution of the cell cycle- and cell adhesion-regulatory functions of L3MBTL434,35.
Moreover, the targeting of LTBP1 by L3MBTL4 was demonstrated in the current work. LTBP1 belongs to the fibrillin-LTBP superfamily36. There are evidence that anomalous expression of LTBP1 may promote the development of arterial diseases15. Decreased expression of LTBP1 is also detected in fibroblasts from thoracic aortic aneurysm16. In L3MBTL4 TGs, LTBP1 was significantly down-regulated whereas the activity of MAPK signaling was apparently up-regulated. Notably, the latest research findings identify altered MAPK family upon LTBP2 knockdown37. Consistently, siRNA specific to LTBP1 induced elevated phosphorylation of p38MAPK and JNK. Therefore, the mechanism underlying L3MBTL4-induced MAPKs activation is depending on depressed expression of LTBP1. LTBP1 may be a primary factor in the effect of L3MBTL4 on vascular remodeling and hypertension. Taken together, the underlying mechanism of L3MBTL4-induced hypertension was summarized in Supplementary Fig. S6. Our data indicated that L3MBTL4 targets the LTBP1 gene, and thereby represses its expression, which results in phosphorylation of p38MAPK and JNK, as well as their downstream factors. The activation of MAPK signaling is engaged in the progression of vascular remodeling associated with pathological hypertension.
In summary, the GWAS described in this paper, along with the two-staged follow-up study, identified L3MBTL4 as a novel susceptibility gene in hypertension. Through in vitro and in vivo experiments, we have shed further light on the biological function of L3MBTL4 and the molecular mechanisms underlying BP regulation. We have also identified the locus, 16q24.2, as a potential hypertension-modulating locus given its great CNV burden. These findings yield new insights into the genetic and biological basis of hypertension and offer potential targets for future antihypertensive therapies.
Methods
Supplementary methods (including complete methods for genetic study design, ethics and subjects, genotyping, quality control, imputation, SNP selection at each stage, CNV analyses and MLPA, statistical analyses, and functional study), Supplementary tables, and Supplementary figures are available in the on-line supplementary.
Ethics Statement
The study was approved by the Institutional Ethical Committee of each hospital and was performed according to the Declaration of Helsinki principles. Peripheral blood and clinical information were collected from subjects who provided written informed consent.
Subjects and BP Phenotyping
The study was designed in three stages using an extreme case-control strategy10. (Supplementary Methods and Supplementary Table S1). Five independent cohorts were recruited. In stage 1, Hypertensive cases were defined as having SBP ≥ 150 mmHg and/or DBP ≥ 90 mmHg in untreated subjects with an age of onset of ≤50 years. Normotensive controls were defined as having SBP ≤ 125 mmHg and DBP ≤ 80 mmHg without antihypertensive treatment. All controls were ≥65 years of age. In stage 2, hypertension and normotension were defined as described for stage 1, while the normotensive controls were ≥55 years of age. In stage 3, hypertension and normotension were defined as described for stage 1 but without age limitation. Individuals would be excluded who had secondary form of hypertension as evaluated by an extensive workup that included serum creatinine and electrolytes, urinalysis, and other hematologic screening tests (Supplementary Methods, Supplementary Fig. S1, and Supplementary Table S1).
Genotyping and Quality Control
Genomic DNA was extracted from peripheral blood samples using the QIAGEN QIAamp DNA Mini Blood Kit (Hilden, Germany). Genotyping was performed using the HumanOmniZhongHua-8 Beadchip (Illumina, San Diego, California, U.S.) in stage 1, the Illumina GoldenGate assay (custom, 384 SNPs) in stage 2 and the MassARRAY iPLEX (Sequenom, San Diego, California, U.S.) in stage 3. Quality control and data filtering were performed according to the call rate (CR), minor allele frequency (MAF), and Hardy-Weinberg equilibrium test (HWE) (Supplementary Methods).
CNV burden Analyses and MLPA
CNV burden was indicated by PLINK 1.0714 based on the genotyping results of stage 1 and then replicated in an additional cohort (989 cases and 1,022 controls randomly selected from stage 2) by multiplex ligation-dependent probe amplification (MLPA) method38 (Supplementary Methods and Supplementary Table S5–S9).
Statistics
The associations between SNPs and SBP, DBP as well as hypertension were assessed using the Cochran-Armitage trend test. Manhattan plots were generated using Haploview software (V4.2). METAL software39 was used for the meta-analyses. Heterogeneity was examined using Cochran’s Q and I2 statistics to assess diversity across different studies. A fixed-effects model was applied if Phet for Q was > 0.05; a random-effects model was adopted if Phet for Q was < 0.05. The significance threshold was set at P < 0.05. For quantitative trait analyses, the genetic effects estimated in each of the multistage panels were combined using the inverse variance method. Regional association plots were generated using Locus Zoom v1.340. Haplotypes were estimated using the software PLINK 1.0714. We used Pearson correlation to estimate the CNV rate differences between cases and controls. The significance threshold was set at P < 0.05. Details of statistics are showed in Supplementary Methods.
Gene Expression Analysis
Quantitative real-time PCR (q-PCR) and Western blotting were performed to estimate mRNA and protein concentrations of the susceptibility genes selected from this genetic study on tissues from spontaneously hypertensive rats (SHRs) and Wistar-Kyoto rats (WKYs). Double immunofluorescence staining was used to localize the protein encoded by susceptibility gene in vasculature and smooth muscle cells (SMCs) (Supplementary Methods).
Rats Model Construction and Phenotype Analysis
Transgenic rats were constructed to explore functional roles of susceptibility gene. Systolic BP (SBP), diastolic BP (DBP), mean BP (MBP) of rats were measured by no-invasive and invasive methods. Weight of different parts of heart were measured to estimate cardiac hypertrophy. Thickness and area of vasculature media layer were measured by histological analyses (Supplementary Methods).
Pathway Analysis and Target Gene Identification
Phospho-antibody microarray was used to analysis high-throughput protein phosphorylation profiling on cell lysates from the aortas and identify probable signaling pathways. Chromatin immunoprecipitation (ChIP) and Gene Ontology analyses were used to indicated downstream targets of susceptibility gene (Supplementary Methods, Supplementary Table S12 and Supplementary Table S13).
Additional Information
How to cite this article: Liu, X. et al. Genome Wide Association Study Identifies L3MBTL4 as a Novel Susceptibility Gene for Hypertension. Sci. Rep. 6, 30811; doi: 10.1038/srep30811 (2016).
Supplementary Material
Acknowledgments
The authors wish to thank the study subjects for their consent to participate in the current study. We also thank the research staff for their contributions and commitment to this project. This research was supported in part by the National Basic Research Program–2014CB542302, the International S&T Cooperation Program of China- 2013DFB30310, the Natural Science Foundation of China –811170244, 81222001, 81470541.
Footnotes
Author Contributions J.C., X.Y. and X.W. designed, analyzed and managed genotyping aspects of the study. J.C., M.B. and X.L. wrote the paper. J.L. and X.L. designed functional studies and contributed to manuscript preparation. Analysis of genome-wide association study and follow-up studies data was performed by X.L. and C.H. Biological samples was collected by X.R.T., Y.Z., Y.C., S.W., S.C., R.Z., F.J. and W.J. contributed to phenotypic and genetics analyses of the study.
References
- Ezzati M., Lopez A. D., Rodgers A., Vander Hoorn S. & Murray C. J. L. Selected major risk factors and global and regional burden of disease. The Lancet 360, 1347–1360, doi: 10.1016/s0140-6736(02)11403-6 (2002). [DOI] [PubMed] [Google Scholar]
- Lopez A. D., Mathers C. D., Ezzati M., Jamison D. T. & Murray C. J. L. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. The Lancet 367, 1747–1757, doi: 10.1016/s0140-6736(06)68770-9 (2006). [DOI] [PubMed] [Google Scholar]
- Lawes C. M. M., Hoorn S. V. & Rodgers A. Global burden of blood-pressure-related disease, 2001. The Lancet 371, 1513–1518, doi: 10.1016/s0140-6736(08)60655-8 (2008). [DOI] [PubMed] [Google Scholar]
- Kearney P. M. et al. Global burden of hypertension: analysis of worldwide data. The Lancet 365, 217–223, doi: 10.1016/s0140-6736(05)17741-1 (2005). [DOI] [PubMed] [Google Scholar]
- Li L. M. et al. [A description on the Chinese national nutrition and health survey in 2002]. Zhonghua liu xing bing xue za zhi=Zhonghua liuxingbingxue zazhi 26, 478–484 (2005). [PubMed] [Google Scholar]
- FJ H. & GA M. Effect of longer-term modest salt reduction on blood pressure. The Cochrane database of systematic reviews 4, (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- NA G., T H.-G. & G J. Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. The Cochrane database of systematic reviews 11 (2011). [DOI] [PubMed] [Google Scholar]
- Kato N. et al. Meta-analysis of genome-wide association studies identifies common variants associated with blood pressure variation in east Asians. Nature genetics 43, 531–538, doi: 10.1038/ng.834 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy D. et al. Genome-wide association study of blood pressure and hypertension. Nature genetics 41, 677–687, doi: 10.1038/ng.384 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padmanabhan S. et al. Genome-wide association study of blood pressure extremes identifies variant near UMOD associated with hypertension. PLoS genetics 6, e1001177, doi: 10.1371/journal.pgen.1001177 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho Y. S. et al. A large-scale genome-wide association study of Asian populations uncovers genetic factors influencing eight quantitative traits. Nature genetics 41, 527–534, doi: 10.1038/ng.357 (2009). [DOI] [PubMed] [Google Scholar]
- Smith N. L. et al. Association of genetic variations with nonfatal venous thrombosis in postmenopausal women. Jama 297, 489–498, doi: 10.1001/jama.297.5.489 (2007). [DOI] [PubMed] [Google Scholar]
- Benjamini Y. & Yekutieli D. Quantitative trait Loci analysis using the false discovery rate. Genetics 171, 783–790, doi: 10.1534/genetics.104.036699 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purcell S. et al. PLINK: a tool set for whole-genome association and population-based linkage analyses. American journal of human genetics 81, 559–575, doi: 10.1086/519795 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oklu R. & Hesketh R. The latent transforming growth factor beta binding protein (LTBP) family. The Biochemical journal 352 Pt 3, 601–610 (2000). [PMC free article] [PubMed] [Google Scholar]
- Jones J. A. et al. Cellular phenotype transformation occurs during thoracic aortic aneurysm development. The Journal of thoracic and cardiovascular surgery 140, 653–659, doi: 10.1016/j.jtcvs.2009.12.033 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marques F. Z. et al. Measurement of absolute copy number variation reveals association with essential hypertension. BMC medical genomics 7, 44, doi: 10.1186/1755-8794-7-44 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabara Y. et al. Common variants in the ATP2B1 gene are associated with susceptibility to hypertension: the Japanese Millennium Genome Project. Hypertension 56, 973–980, doi: 10.1161/hypertensionaha.110.153429 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C. et al. Common variants in or near FGF5, CYP17A1 and MTHFR genes are associated with blood pressure and hypertension in Chinese Hans. Journal of hypertension 29, 70–75, doi: 10.1097/HJH.0b013e32833f60ab (2011). [DOI] [PubMed] [Google Scholar]
- Lu X. et al. Genome-wideassociationstudyinChineseidentifies novel loci for blood pressure and hypertension. Human molecular genetics 24, 865–874, doi: 10.1093/hmg/ddu478 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause A. et al. Junctophilin 3 (JPH3) expansion mutations causing Huntington disease like 2 (HDL2) are common in South African patients with African ancestry and a Huntington disease phenotype. American journal of medical genetics. Part B, Neuropsychiatric genetics: the official publication of the International Society of Psychiatric Genetics, doi: 10.1002/ajmg.b.32332 (2015). [DOI] [PMC free article] [PubMed]
- Huang Y. et al. A novel human hydroxysteroid dehydrogenase like 1 gene (HSDL1) is highly expressed in reproductive tissues. Molecular biology reports 28, 185–191 (2001). [DOI] [PubMed] [Google Scholar]
- Soro A. et al. Genome scans provide evidence for low-HDL-C loci on chromosomes 8q23, 16q24.1-24.2, and 20q13.11 in Finnish families. American journal of human genetics 70, 1333–1340, doi: 10.1086/339988 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao H. & Brooks J. D. Selenomethionine induced transcriptional programs in human prostate cancer cells. The Journal of urology 177, 743–750, doi: 10.1016/j.juro.2006.09.071 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong W. et al. An analysis of the clinical and biologic significance of TP53 loss and the identification of potential novel transcriptional targets of TP53 in multiple myeloma. Blood 112, 4235–4246, doi: 10.1182/blood-2007-10-119123 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin N. R. et al. Overexpression of Snail is associated with lymph node metastasis and poor prognosis in patients with gastric cancer. BMC cancer 12, 521, doi: 10.1186/1471-2407-12-521 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addou-Klouche L. et al. Loss, mutation and deregulation of L3MBTL4 in breast cancers. Molecular cancer 9, 213, doi: 10.1186/1476-4598-9-213 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulvany M. J. Small artery remodelling in hypertension: causes, consequences and therapeutic implications. Medical & biological engineering & computing 46, 461–467, doi: 10.1007/s11517-008-0305-3 (2008). [DOI] [PubMed] [Google Scholar]
- Folkow B. Physiological aspects of primary hypertension. Physiological reviews 62, 347–504 (1982). [DOI] [PubMed] [Google Scholar]
- Cheng G. et al. IL-17 stimulates migration of carotid artery vascular smooth muscle cells in an MMP-9 dependent manner via p38 MAPK and ERK1/2-dependent NF-kappaB and AP-1 activation. Cellular and molecular neurobiology 29, 1161–1168, doi: 10.1007/s10571-009-9409-z (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usui T. et al. Death-associated protein kinase 3 mediates vascular structural remodelling via stimulating smooth muscle cell proliferation and migration. Clinical science 127, 539–548, doi: 10.1042/cs20130591 (2014). [DOI] [PubMed] [Google Scholar]
- Liu Y., Wen J. K., Dong L. H., Zheng B. & Han M. Kruppel-like factor (KLF) 5 mediates cyclin D1 expression and cell proliferation via interaction with c-Jun in Ang II-induced VSMCs. Acta pharmacologica Sinica 31, 10–18, doi: 10.1038/aps.2009.185 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godeny M. D. & Sayeski P. P. ERK1/2 regulates ANG II-dependent cell proliferation via cytoplasmic activation of RSK2 and nuclear activation of elk1. American journal of physiology. Cell physiology 291, C1308–C1317, doi: 10.1152/ajpcell.00618.2005 (2006). [DOI] [PubMed] [Google Scholar]
- Almon R. R. et al. Circadian variations in rat liver gene expression: relationships to drug actions. The Journal of pharmacology and experimental therapeutics 326, 700–716, doi: 10.1124/jpet.108.140186 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maurer-Morelli C. V. et al. A Locus Identified on Chromosome18P11.31 is Associated with Hippocampal Abnormalities in a Family with Mesial Temporal Lobe Epilepsy. Frontiers in neurology 3, 124, doi: 10.3389/fneur.2012.00124 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saharinen J., Hyytiainen M., Taipale J. & Keski-Oja J. Latent transforming growth factor-beta binding proteins (LTBPs)–structural extracellular matrix proteins for targeting TGF-beta action. Cytokine & growth factor reviews 10, 99–117 (1999). [DOI] [PubMed] [Google Scholar]
- Ren Y. et al. LTPB2 acts as a prognostic factor and promotes progression of cervical adenocarcinoma. American journal of translational research 7, 1095–1105 (2015). [PMC free article] [PubMed] [Google Scholar]
- Stuppia L., Antonucci I., Palka G. & Gatta V. Use of the MLPA Assay in the Molecular Diagnosis of Gene Copy Number Alterations in Human Genetic Diseases. International journal of molecular sciences 13, 3245–3276, doi: 10.3390/ijms13033245 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willer C. J., Li Y. & Abecasis G. R. METAL: fast and efficient meta-analysis of genomewide association scans. Bioinformatics (Oxford, England) 26, 2190–2191, doi: 10.1093/bioinformatics/btq340 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pruim R. J. et al. LocusZoom: regional visualization of genome-wide association scan results. Bioinformatics (Oxford, England) 26, 2336–2337, doi: 10.1093/bioinformatics/btq419 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.