Abstract
Mobile technologies are revolutionizing the field of mental health, and particular progress has been made in their application to addiction research and treatment. The use of smartphones and other mobile devices has been shown to be feasible with individuals addicted to any of a wide range of substances, with few biases being observed concerning the repeated monitoring of daily life experiences, craving, or substance use. From a methodological point of view, the use of mobile technologies overcomes longstanding limitations of traditional clinical research protocols, including the more accurate assessment of temporal relationships among variables, as well as the reduction in both contextual constraints and discipline-specific methodological isolation. The present article presents a conceptual review of these advances while using illustrations of research applications that are capable of overcoming specific methodological barriers. Finally, a brief review of both the benefits and risks of mobile technology use for the treatment of patients will be addressed.
Keywords: addiction, ecological momentary assessment, EMA, ESM, experience-sampling method, mobile technology, substance
Abstract
Las tecnologías móviles están revolucionando el campo de la salud mental y se ha realizado un especial progreso en sus aplicaciones a la investigación y tratamiento de las adicciones. Se ha demostrado que el empleo de teléfonos inteligentes y otros dispositivos móviles es factible en sujetos adictos a una amplia gama de sustancias, observándose pocos sesgos en relación con la supervisión repetida de experiencias de la vida diaria, el craving o el uso de sustancias. Desde un punto de vista metodológico el empleo de tecnologías móviles supera desde hace mucho tiempo las limitaciones de los protocolos de investigación clínica tradicional, incluyendo la evaluación precisa de las relaciones temporales entre las variables, como también la reducción en las limitaciones contextuales y en el aislamiento metodológico específico de la disciplina. El presente artículo presenta una revisión conceptual de estos avances utilizando ilustraciones de aplicaciones a la investigación que son capaces de superar barreras metodológicas específicas. Por último, en una revisión breve, se abordan los riesgos y beneficios del empleo de la tecnología móvil en el tratamiento de pacientes.
Abstract
Les technologies mobiles sont en train de révolutionner le domaine de la santé mentale, les progrès étant notables dans leur application à la recherche et au traitement des addictions. Il a été montré que les smart-phones et autres appareils mobiles peuvent être utilisés par les sujets dépendants, et ce pour une vaste gamme de substances, avec cependant quelques biais au niveau du suivi du vécu quotidien, du besoin irrépressible ou de la consommation de substances. D'un point de vue méthodologique, l'utilisation des technologies mobiles surmonte les limites des protocoles traditionnels de recherche clinique en rendant plus précise l'évaluation des relations temporelles entre variables et en diminuant les contraintes contextuelles et l'isolation méthodologique spécifique à chaque discipline. Cet article présente une mise au point conceptuelle de ces avancées en illustrant les applications de la recherche capables de surmonter les barrières méthodologiques spécifiques. Enfin, les bénéfices et risques de l'utilisation de la technologie mobile pour traiter les patients seront rapidement abordés.
Introduction
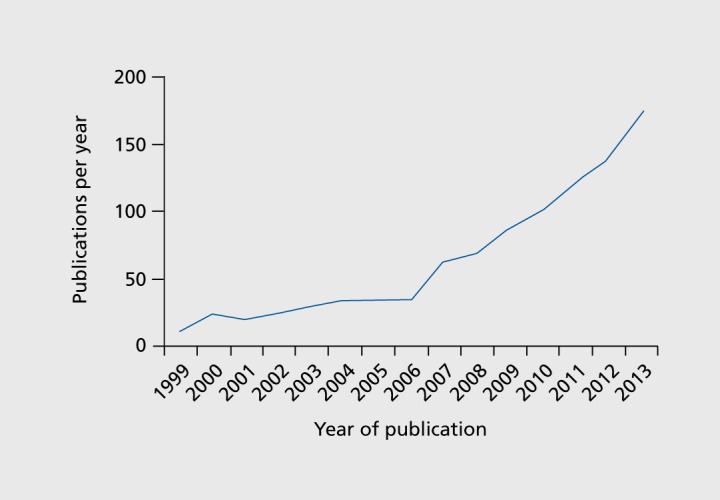
Considering the number of researchers around the world investigating mental disorders, it is surprising to note the enduring nature of many debates concerning models of etiology or comorbidity. The persistence of these questions over time is attributable to common methodological or conceptual barriers that have long been acknowledged in mental health research and treatment, but remain poorly mastered. Moreover, these limitations represent a major impediment to bridging laboratory-based research on genetic, biological, or cognitive vulnerabilities to field research that examines the conditions under which such vulnerabilities express themselves. The recent revolution in mobile technologies has had a major impact in all areas of mental health in particular due to the ability of these tools to overcome barriers and address both new and old questions with increased precision. It is therefore not surprising that the number of investigations applying mobile technologies in psychiatry has increased almost exponentially in recent years(Figure 1). What was once seen as a methodological novelty is now quickly becoming a standard tool for researchers, and its expansion to include treatment applications is likely to revolutionize the way clinicians interact with patients in the years to come.
Figure 1. Studies using mobile technologies in psychiatry. Source: PubMed search.
Although the contributions of mobile technologies are widespread, the present article addresses these advances specifically for substance use disorders. The following sections will first describe the manner in which mobile technologies are used in clinical research, including fundamental information concerning their feasibility, validity, and potential biases. The principal methodological impediments that characterize traditional clinical and epidemiologic research paradigms in the addiction field will then be described, each followed by illustrations of the advantages of mobile technology use. Finally, a brief review of both the benefits and risks of mobile technologies in the treatment of patients will be addressed.
Mobile technologies in mental health research
Although the term “mobile technologies” is currently associated with smartphones and connected devices, it is surprising to note that they have been applied in one form or another in psychiatry research for almost 30 years. Earlier applications have utilized mobile devices such as multi-alarm watches or beepers to alert individuals with regard to the time that they should complete paper-based assessments. The pioneers of research in this domain1-3 referred to this approach either as the experience-sampling method (ESM) or ecological momentary assessment (EMA), and the repeated data generated by each participant provided highly novel insights into daily life behaviors and experiences that were inaccessible to other research paradigms. The majority of the earliest studies were largely descriptive, such as providing “time budget” surveys of the frequency and distribution of daily life behaviors in different psychiatric populations. This initial series of mobile technology investigations in psychiatry was increasingly joined by hypothesis-driven research and tests of theoretical models of etiology. Although considerable variation between studies can be seen in the number of assessments administered each day, the number of days of participation, and the signaling parameters, these earlier studies quickly demonstrated the unique benefits of mobile technologies when applied to the investigation of mental health issues. However, the use of paper-based methods was labor-intensive due to the necessity of data transcription, and patients were often unable to provide accurate descriptions of the timing that daily life reports were completed.4 Beginning in the 1990s, the availability of programmable electronic devices, such as personal digital assistants and palm- top computers, greatly facilitated data collection while also reducing errors commonly associated with paper-based approaches. Thanks to this new wave of mobile research tools, and to their decreasing financial costs, a considerable expansion of ESM and EMA investigations was seen for a large number of mental disorders.
Common research strategies for the use of mobile technologies
The basic methodological approach of ESM and EMA studies consists of providing repeated but brief assessments of a range of daily life experiences, environmental contexts, emotional states, daily stressors, and specific thoughts, as well as a range of other variables associated with specific psychiatric conditions. For the field of addiction, most of these disorder-specific questions have focused on craving experience, cue exposure, and actual substance use.5 Perhaps the most novel contribution of such methods is their ability to provide prospective data that are able to identify predictors of craving or substance use in real time and over short time periods. The electronic time-stamps available for each interview also guarantee that assessments are completed at desired times throughout the day rather than being completed in mass at the end of the study period (as would be possible for paper-based methods). In addition, the analyses conducted in these investigations permit control for the status of the predicted variable at the time of the previous assessment (often spanning 2 to 4 hours, on average), thereby informing the researcher of the direction of relationships even among very highly correlated variables.
Despite these advances, electronic ambulatory monitoring remained the object of clinical skepticism, mainly reflecting doubts relative to the acceptability of these methods among certain psychiatric populations or because of concerns about the potential biases associated with their use. These fears were particularly present for substance use disorders, where clinicians were often skeptical of the feasibility of its use among individuals with illicit drug dependence or concerned that patients would sell the device in order to acquire substances. In response to these concerns, extensive validation studies have been conducted in diverse psychiatric populations over the years, including individuals with substance use disorders, in order to examine the potential limitations of this approach. Table I presents a summary of different psychiatric populations to have used the same methodologies for mobile technology use.6-9 Individuals with a substance use disorder were found to be no more likely than other populations to refuse participation or to lose the signaling device. Their average response rate to the multiple electronic interviews was also very high and comparable to healthy controls. Importantly, no fatigue effects were observed for the multiple daily electronic interviews per day (assessed by the rate of missing data observed by study day), and participants were able to respond more quickly to electronic interviews as the study progressed. More recent validation studies including patients with alcohol, tobacco, cannabis, and heroin addiction have observed lower initial study acceptance rates,10 but similarly high compliance with the multiple electronic interviews and the absence of fatigue effects.
Encouraging patient compliance
Although the use of mobile technologies among individuals with substance use disorders may therefore be considered both feasible and valid, it is important to note that such studies were often carefully designed to encourage compliance and patient investment in the procedures. For many of these studies, patients were paid for their participation, and a portion of studies increased payments as a function of the number of electronic interviews completed. Other techniques were used in some of these investigations, such as providing an extra bonus for returning the smartphone or other signaling device, and some have tried to reduce the street value of the device by blocking all functions with the exception of those necessary for the study. These procedures have most likely contributed to the high rates of participation and repeated-interview compliance, but they nonetheless show that patients with any form of substance dependence can participate in investigations of their daily life experiences using mobile technologies, without major biases, if the investigator understands the particular characteristics and risks of the study population.
Methodological impediments in addiction research
The demonstration of the feasibility and validity of mobile technologies in addiction research is a prerequisite for encouraging their wider diffusion in the field. However, the actual value of this approach depends on its ability to overcome specific methodological barriers that impede our understanding of various aspects of addiction etiology, chronicity, and treatment efficacy. These barriers are numerous and often interdependent, explaining why mobile technology use has often addressed several limitations simultaneously.
TABLE I. Feasibility and validity of mobile technologies in psychiatry.
| Feasibility | Reactivity | ||||
| Acceptability (%) | Material loss (%) | Response rate (%) | Fatigue effect, γ (SE) | Training effect, γ (SE) | |
| Healthy controls, n=280 | 93 | 2 | 83 | 0.03 (0.03) | -0.18 (0.03*) |
| Anxiety disorders, n=45 | 89 | 0 | 73 | 0.02 (0.05) | -0.28 (0.05*) |
| Schizophrenia, n=56 | 96 | 2 | 69 | -0.04 (0.05) | -0.31 (0.04*) |
| Mood disorders, n=42 | 90 | 0 | 86 | 0.01 (0.02) | 0.12 (0.02*) |
| Addiction, n=85 | 98 | 0 | 80 | 0.03 (0.03) | -0.13 (0.03*) |
| *P < 0.01; γ, mean γ distribution; SE, standard error |
Temporal barriers in addiction research
A first major impediment confronting researchers in the field of addiction concerns the important differences between the natural phenomena under study and the methods used in their investigation. In particular, this discrepancy is most visible concerning the assessment of temporal relationships among variables. In contrast to diagnostic criteria that are based in part on the importance of duration over time as a defining feature of disorder, the actual pathological mechanisms at the origin of a given syndrome are often highly dynamic. That is, the expression of many forms of addiction are characterized by a relatively short “life cycle” with regard to the period of time in which a given vulnerability or risk factor may influence the severity of craving or the use of substances. Such phenomena are observable over periods that are typically limited to a matter of minutes to hours, whereas most traditional methodologies apply retrospective, cross-sectional, or longitudinal assessments spanning weeks, months, or years.
A salient illustration of temporal barriers in traditional research paradigms is found in investigations of addiction comorbidity. For example, a large body of clinical and epidemiologic research has demonstrated the strong correlation between alcohol dependence and anxiety or mood disorders,11-17 with associations of essentially equal magnitude for both forms of comorbidity. The association for anxiety disorders, as one example, is noted by the left graph of Figure 1. Such correlations are generally highly significant across the diverse studies published over the past 30 years, and they have been replicated both in treatment-seeking samples and in community residents. Concerning the explanations for these associations, one of the most commonly cited models is that of ”self-medication,“ whereby the individual would use or abuse alcohol to assuage pre-existing anxiety (or depressive) states. The self-medication model would indeed have important treatment implications if it was able to accurately characterize the majority of cases of these forms of comorbidity, as it would suggest that comorbid disorders should be addressed before the treatment of alcohol dependence could be effective. However, the validity of tests of this hypothesis depends heavily on the nature of data collected in the samples studied.
Figure 2. Example of correlational studies of anxiety and alcohol use.
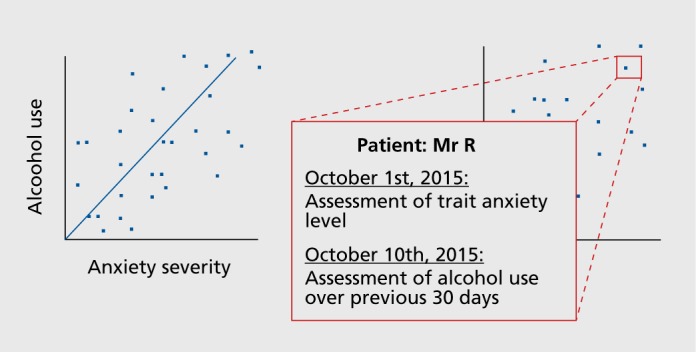
Using an example patient, the right graph of Figure 2 illustrates to what extent the existing data on this issue is typically based solely on assessments of the average severity of anxiety, depression, or alcohol-related syndromes (therefore showing little or no within-subject variation). As a result, at no point was the example investigation presented in Figure 2 able to demonstrate that “Mr R,” or anyone else in the sample, was more likely to consume alcohol when anxious. Logically, a person consuming alcohol to alleviate anxiety would be motivated to do so only if they were anxious at that particular moment and not because they were an anxious person “on average” or because they were anxious the week or month before. Self-medication is, therefore, a highly dynamic within-person phenomenon that can be accurately studied only over considerably shorter time frames. The phenomenon of interest was never studied directly in the great majority of epidemiologic and clinical research, thereby ignoring the potential underlying mechanisms and rendering the conclusions difficult to exploit on a practical level.
Among the first tests of the self -medication hypothesis that used mobile technologies, one study18 demonstrated highly different patterns of association between the different mood states and later alcohol use. In particular, alcohol was often used to assuage anxious moods, but no self-medication effect was found for depressed moods. This finding was in stark contrast to the conclusions of many epidemiologic or clinical investigations using traditional paradigms that assumed that the essentially equivalent associations between alcohol dependence and anxiety disorders or depression probably reflected the same underlying mechanism. In addition, this study's repeated assessments in daily life also allowed for two interesting qualifications of the selfmedication phenomenon: the motivation for alcohol consumption after increases in anxiety was significantly greater in males, and those with a family history of alcoholism required greater quantities of alcohol to achieve the same “anxiolytic” effects as participants without a family history of alcoholism. These findings provide potentially important insight into the strongly heritable nature of alcohol use disorders, notably by explaining why individuals (or families) might be more susceptible to use alcohol in greater quantities as a means of alleviating anxiety problems. A number of subsequent investigations have used mobile technologies to provide assessments of mood states and alcohol use several times per day and over periods spanning from 1 to several weeks.18-22 Similar to earlier research, each electronic assessment remained brief (1 to 3 minutes, on average), but their repetition on a daily basis allowed for these variables to be studied in a manner complementary to more traditional investigations, including real-time assessment in the natural contexts of daily life.
The barrier of context
A second major impediment to testing etiologic models of addiction pertains to the ecological validity of the existing literature. Although it remains possible for laboratory or clinic-based investigations to overcome some of the temporal constraints described previously, they remain limited to the study of artificially induced states or to assessments conducted within the same context (clinic or hospital). It is therefore difficult or impossible to determine how these variables will express themselves in naturalistic contexts. To again take the example of self-medication, alcohol consumption has been shown to immediately reduce the negative emotional states induced through certain laboratory-based experimental procedures.23 However, this paradigm cannot determine if subjects would actually choose to use alcohol as a means of assuaging negative affect outside of the laboratory. It is also impossible to determine the contexts in which the phenomenon of self -medication is most likely to express itself (for example, when the individual is alone versus accompanied, or when confronted with a specific form of stress). Therefore, through mobile technologies, a clearer description of the contexts in which these variables express themselves in vivo permits a better understanding of how diverse vulnerabilities for complex mental disorders such as addiction influence the emergence or exacerbation of symptoms.
The barrier of personalized medicine
In addition to the general issue of ecological validity, an important impediment in addiction research concerns the personal and unique significance of certain environments or stimuli that cannot be duplicated in the laboratory. For example, it has been repeatedly demonstrated that exposure to conditioned substance-related cues results in greater craving and psychophysiological reactivity.24-27 In general, these cues can in most instances be qualified as ”universal“ in that most patients addicted to that given substance would react to the given cue examined. Most patients addicted to heroin, for example, would show increased craving or physiological reactivity when exposed to a syringe, and most alcoholdependent patients would show increased craving or reactivity when exposed to a bottle, etc. However, each addicted individual can also be characterized by their own unique pattern of substance use, and therefore by person-specific cues that cannot be duplicated in the laboratory. A patient who is addicted to heroin may use this drug most often with a specific friend, or in the specific stairwell of their apartment building that has a particular odor. Such person-specific cues have been largely ignored in addiction research, because the methods used in this domain were not able to follow individuals into their intimate environments or to incorporate knowledge about personal risk factors of this type into laboratory-based protocols. By use of mobile technologies, a recent investigation was able to utilize information from individual interviews to assess both universal and personal cues and to program both sources of risk into mobile devices. In this way, individual-specific vulnerabilities for substance use were compared directly with ”universal“ or ”standard“ risk factors.28 This study found that the frequency of universal cue exposure in natural contexts tended to decrease over the course of treatment, but that personal cue frequency remained stable. In addition, the magnitude and duration of craving reactivity after exposure was greater for personal than for universal cues. These findings argue that what is most visible and most easily assessed in addiction research (in this example, universal cues) may represent only the tip of the iceberg in terms of relapse risk. It may therefore be for this reason that therapies based on classical conditioning and focused on exposure to substance-related paraphernalia have reported mixed results, as they have often ignored a number of powerful person-specific cues. Exposure to such personal risk factors would be difficult to accomplish through traditional laboratory investigations, yet these findings clearly demonstrate the importance of understanding addiction in natural environments and according to the trajectory and experiences of each individual.
The barriers of methodological isolation
Many of the major tools used in addiction research, and in clinical neuroscience more generally, have often been applied in isolation of other methods. It is obvious that state-of-the-art techniques in neuroimaging and genetics have made considerable progress in identifying diverse biological markers of addiction risk, as well as in understanding the pathophysiology of this disorder.29-33 However, when a given marker is found, it is often difficult to understand its full implications, such as the daily life changes associated with its presence, absence, or intensity. Mobile technologies hold promise for informing us of the full implications of markers identified through these techniques, and conversely, they provide information about the daily life mechanisms underlying addiction etiology or relapse risk that may in turn guide the identification of biomarkers.34 Examples include the degree to which a particular polymorphism may influence the strength of the association between cue exposure and subsequent craving or the degree to which brain networking connectivity may explain variance in fluctuations in craving and substance use. The response to these questions requires, almost by definition, the fusion of methods capable of bridging the body and brain with behavior and the environment.
The combination of methods not only provides complementary information necessary for understanding a wider spectrum of addiction risk factors and mechanisms, but it also provides for more comprehensive investigations of a single given construct. This point is perhaps best illustrated by neuropsychological testing of cognitive vulnerabilities to addiction. For example, decision making results from the integration of several executive functions necessary for the control and execution of complex tasks.35 Impairment in this cognitive function is observed in several psychiatric disorders, including addiction,36-40 and it leads to an inability to make profitable long-term decisions that incorporate expectations of future outcomes. With traditional cognitive testing, such functions are often measured by the Iowa Gambling Task (IGT), as it mimics the complexity of choices that individuals are confronted with in everyday life. Its design incorporates the unpredictability of the consequences of a choice, the need to weigh shortterm and long-term gains and losses, and the necessity to exert behavioral control to maximize gains in the long term. Patients suffering from addiction in which decision making is compromised typically persevere in their choice for the disadvantageous options that yield immediate large rewards, despite larger losses in the long term.
Despite the interest of the IGT, this test is administered at one point in time and therefore is adapted only to characterizing a general deficit in executive functioning. In reality, however, decision making and other cognitive functions are actually highly variable, with daily fluctuations in performance occurring frequently over time for any given individual. For this reason, the juxtaposition of mobile cognitive test performance with subsequent substance use, in real time, would move beyond simple correlations based on between-person variance and serve as clearer support for the role of executive dysfunction in subsequent symptom expression.41 The simultaneous use of both assessment strategies (the IGT and mobile tests) may also clarify the debate as to whether we should conceptualize cognitive functioning as a “state” or “trait,” or rather attempt to understand that these terms may simply reflect the manner in which a single given construct is measured.
Statistical issues in data analysis
Finally, the barrier of methodological isolation is reinforced by the fact that most traditional tools of clinical neuroscience are adapted to analyzing between-person variance, whereby each individual has a single score that represents a biomarker's presence or intensity. The current rarity of analyses in clinical neuroscience that take into account both between- and within-person variance is perhaps explained more by discipline-specific habits than by imperatives, but such a combination allows for the modeling of phenomenological experiences of the individual (collected by mobile technologies) by the diverse between-subject characteristics assessed through controlled laboratory procedures (genetics, biological assays, neuroimaging, neuropsychology). In this way, the repeated-measures data generated by mobile technologies can be combined with traditional neuroscience methods without the need of disaggregating to the level of individual assessments (which violates the assumption of independence of observations) and without requiring an average to be calculated across the diverse observations (which ignores the majority of the within subject variance).
Barriers to treatment
Although the majority of this article has focused on the benefits of mobile technologies for research purposes, a final consideration is how they may revolutionize treatment strategies. Even in the context of daily contact with a clinician or therapy group, patients are alone for the majority of the day to face the challenges of avoiding risk factors, managing craving, and remaining abstinent. In outpatient settings, it is also obvious that patients cannot be followed up continuously by the clinical team; therefore, mobile technologies may offer a logical solution to addressing this unmet need. Smartphone applications and other solutions have the capacity to reinforce abstinence and manage craving at the moments that they are most needed in daily life, and indeed hundreds of applications have been developed for this purpose and for a range of different substances.
Despite possibly being considered as treatment progress, it is nonetheless important to consider three potential limitations associated with the application of mobile technologies to addiction treatment. A first issue involves the uncontrolled proliferation of such applications and the diversity of content that may not always be adapted, and may even perhaps be dangerous, for specific individuals. For example, the risk of seizures following alcohol withdrawal is not taken into account by many applications, despite their encouragement of full abstinence. It is also unknown if the developers of such applications include clinicians trained in the treatment of addiction and who are aware of medical risks, as well as of the vulnerabilities of particular patient populations. Unfortunately, there is still no comprehensive regulatory system in the United States or in Europe for classifying smartphone (or other) applications as a medical device. Moreover, even if the US Food and Drug Administration (FDA) or other governmental organization were able to specify such criteria, individuals would still be confronted with the large diversity of options for smartphone applications available through Google, through the App Store, or through other general public sources. It therefore remains very difficult at present to imagine the control of patient safety for existing applications in the field of addiction. A second concern reflects our lack of knowledge about the unwanted consequences of smartphone applications relative to treatment seeking. Otherwise stated, it is currently unknown to what degree individuals who would normally have consulted directly with a clinician might not do so simply because they believe they have achieved some form of treatment through mobile technologies. An important debate therefore concerns the degree to which in-person treatment is superior to electronic treatment strategies and to what extent mobile technologies should be used in conjunction with clinician contact, in place of clinician contact, or only following direct clinician contact. A final issue involves the length of use of mobile treatment applications. Research studies may show benefits of mobile interventions, but they are typically limited to 12 or 15 weeks of treatment. Given that most smartphone users download applications that are used for a limited amount of time, it is unclear if individuals with addiction would use their mobile treatment programs over the longer term. The response to these issues requires carefully designed, prospective investigations in both clinical and control populations.
In any case, it is a reality that mobile technologies are among us, and their use — or abuse — must be dealt with by clinicians. Perhaps the wisest strategy for clinicians is to test demos of the applications themselves so that they can verify their content and only then direct patients to specific “verified” sites for downloading. It is also important that patients be clearly informed that a smartphone application or other program is meant only as a source of additional support and that direct contact with the clinician is always the first-line option. No computer-based option can respond in detail to questions from the patient as they evolve throughout therapy, and only the clinician can decide if treatment changes are necessary. A final issue in the education of patients pertains to data confidentiality, which is never fully guaranteed on electronic devices, both in terms of the curiosity of family or friends and also involving “big data” strategies that particular applications may include. In the absence of a clear strategy for the verification of applications by the health care sector or the government, clinicians and patients must work together to make the best choices.
Conclusion
In conclusion, there is no doubt that the revolution in mobile technologies has provided considerable advances for addiction research by overcoming several methodological barriers that characterize traditional research tools. These advances include solutions for temporal barriers, contextual constraints, and discipline-specific isolation. However, the application of mobile technologies as a means of clinical intervention is far less controlled and should remain a focus of both scientific and ethical debate in the years to come. One might conclude that the “future is now,” but the question remains if such a future has come too quickly, too suddenly, to fully understand and master the power of mobile technologies.
REFERENCES
- 1.Csikszentmihalyi M., Larson R. Validity and reliability of the experience-sampling method. J Nerv Ment Dis. 1987;175(9):526–536. doi: 10.1097/00005053-198709000-00004. [DOI] [PubMed] [Google Scholar]
- 2.De Vries M., Delespaul P., Dijkman C. Affect and anxiety in daily life. In: G. Racagni, Ed. Anxious Depression: Assessment and Treatment. New York, NY: Raven Press;1987;xx:21–32. [Google Scholar]
- 3.Stone AA., Shiftman S. Ecological momentary assessment (EMA) in behavioral medicine. Ann Behav Med. 1994;16(3):199–202. [Google Scholar]
- 4.Stone AA., Shiftman S., Schwartz JE., Broderick JE., Hufford MR. Patient compliance with paper and electronic diaries. Control Clin Trials. 2003;24(2):182–199. doi: 10.1016/s0197-2456(02)00320-3. [DOI] [PubMed] [Google Scholar]
- 5.Serre F., Fatseas M., Swendsen J., Auriacombe M. Ecological momentary assessment in the investigation of craving and substance use in daily life: a systematic review. Drug Alcohol Depend. 2015;148:1–20. doi: 10.1016/j.drugalcdep.2014.12.024. [DOI] [PubMed] [Google Scholar]
- 6.Granholm E., Loh C., Swendsen J. Feasibility and validity of computerized ecological momentary assessment in schizophrenia. Schizophr Bull. 2008;34(3):507–514. doi: 10.1093/schbul/sbm113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnson El., Barrault M., Nadeau L., Swendsen J. Feasibility and validity of computerized ambulatory monitoring in drug-dependent women. Drug Alcohol Depend. 2009;99(1-3):322–326. doi: 10.1016/j.drugalcdep.2008.06.010. [DOI] [PubMed] [Google Scholar]
- 8.Johnson El., Grondin O., Barrault M., et al Computerized ambulatory monitoring in psychiatry: a multi-site collaborative study of acceptability, compliance, and reactivity. IntJ Methods Psychiatr Res. 2009;18(1):48–57. doi: 10.1002/mpr.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Husky MM., Gindre C., Mazure CM., et al Computerized ambulatory monitoring in mood disorders: feasibility, compliance, and reactivity. Psychiatry Res. 2010;178(2):440–442. doi: 10.1016/j.psychres.2010.04.045. [DOI] [PubMed] [Google Scholar]
- 10.Serre F., Fatseas M., Debrabant R., Alexandre JM., Auriacombe M., Swendsen J. Ecological momentary assessment in alcohol, tobacco, cannabis and opiate dependence: a comparison of feasibility and validity. Drug Alcohol Depend. 2012;126(1-2):118–123. doi: 10.1016/j.drugalcdep.2012.04.025. [DOI] [PubMed] [Google Scholar]
- 11.Glantz MD., Anthony JC., Berglund PA., et al Mental disorders as risk factors for later substance dependence: estimates of optimal prevention and treatment benefits. Psychol Med. 2009;39(8):1365–1377. doi: 10.1017/S0033291708004510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grant BF., Goldstein RB., Saha TD., et al Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. WIJAMA Psychiatry. 2015;72(8):757–766. doi: 10.1001/jamapsychiatry.2015.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hasin DS., Stinson FS., Ogburn E., Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64(7):830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- 14.Helzer J., Pryzbeck T. The co-occurrence of alcoholism with other psychiatric disorders in the general population and its impact on treatment. J Stud Alcohol. 1988;49(3):219–224. doi: 10.15288/jsa.1988.49.219. [DOI] [PubMed] [Google Scholar]
- 15.Hesselbrock M., Meyer R., Keener J. Psychopathology in hospitalized alcoholics. Arch Gen Psychiatry. 1985;42(11):1050–1055. doi: 10.1001/archpsyc.1985.01790340028004. [DOI] [PubMed] [Google Scholar]
- 16.Merikangas K., Mehta R., Molnar B., et al Comorbidity of substance use disorders with mood and anxiety disorders: results of the International Consortium in Psychiatric Epidemiology. Addict Behav. 1998;23(6):893–907. doi: 10.1016/s0306-4603(98)00076-8. [DOI] [PubMed] [Google Scholar]
- 17.Swendsen J., Conway KP., Degenhardt L., et al Mental disorders as risk factors for substance use, abuse and dependence: results from the 10-year follow-up of the National Comorbidity Survey. Addiction. 2010;105(6):1117–1128. doi: 10.1111/j.1360-0443.2010.02902.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Swendsen J., Tennen H., Carney MA., Affleck G., Willard A., Hromi A. Mood and alcohol consumption: an experience sampling test of the selfmedication hypothesis. J Abnorm Psychol. 2000;109(2):198–204. [PubMed] [Google Scholar]
- 19.Crooke AH., Reid SC., Kauer SD., et al Temporal mood changes associated with different levels of adolescent drinking: using mobile phones and experience sampling methods to explore motivations for adolescent alcohol use. Drug Alcohol Rev. 2013;32(3):262–268. doi: 10.1111/dar.12034. [DOI] [PubMed] [Google Scholar]
- 20.Papp LM., Blumenstock SM. Momentary affect and risky behavior correlates of prescription drug misuse among young adult dating couples: an experience sampling study. Addict Behav. 2016;53:161–167. doi: 10.1016/j.addbeh.2015.10.016. [DOI] [PubMed] [Google Scholar]
- 21.Shadur JM., Hussong AM., Haroon M. Negative affect variability and adolescent self-medication: the role of the peer context. Drug Alcohol Rev. 2015;34(6):571–580. doi: 10.1111/dar.12260. [DOI] [PubMed] [Google Scholar]
- 22.Simons JS., Gaher RM., Oliver MN., Bush JA., Palmer MA. An experience sampling study of associations between affect and alcohol use and problems among college students. J Stud Alcohol. 2005;66(4):459–469. doi: 10.15288/jsa.2005.66.459. [DOI] [PubMed] [Google Scholar]
- 23.Kushner MG., Mackenzie TB., Fiszdon J., et al The effects of alcohol consumption on laboratory-induced panic and state anxiety. Arch Gen Psychiatry. 1996;53(3):264–270. doi: 10.1001/archpsyc.1996.01830030086013. [DOI] [PubMed] [Google Scholar]
- 24.Childress AR., McLellan AT., O'Brien CP. Conditioned responses in a methadone population: a comparison of laboratory, clinic, and natural settings. J SubstAbus Treat. 1986;3(3):173–179. doi: 10.1016/0740-5472(86)90018-8. [DOI] [PubMed] [Google Scholar]
- 25.Childress AR., McLellan AT., Natale M., O'Brien CP. Mood states can elicit conditioned withdrawal and craving in opiate abuse patients. NIDA ResMonogr. 1987;76:137–144. [PubMed] [Google Scholar]
- 26.Fatseas M., Denis C., Massida Z., Verger M., Franques-Reneric P., Auriacombe M. Cue-induced reactivity, Cortisol response and substance use outcome in treated heroin dependent individuals. Biol Psychiatry. 2011;70(8):720–727. doi: 10.1016/j.biopsych.2011.05.015. [DOI] [PubMed] [Google Scholar]
- 27.Yu J., Zhang S., Epstein DH., et al Gender and stimulus difference in cue-induced responses in abstinent heroin users. Pharmacol Biochem Behav. 2007;86(3):485–492. doi: 10.1016/j.pbb.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 28.Fatseas M., Serre F., Alexandre JM., Debrabant R., Auriacombe M., Swendsen J. Craving and substance use among patients with alcohol, tobacco, cannabis or heroin addiction: a comparison of substance- and person-specific cues. Addiction. 2015;110(6):1035–1042. doi: 10.1111/add.12882. [DOI] [PubMed] [Google Scholar]
- 29.Hart AB., Kranzler HR. Alcohol dependence genetics: lessons learned from genome-wide association studies (GWAS) and post-GWAS analyses. Alcohol Clin Exp Res. 2015;39(8):1312–1327. doi: 10.1111/acer.12792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jasinska AJ., Stein EA., Kaiser J., Naumer MJ., Yalachkov Y. Factors modulating neural reactivity to drug cues in addiction: a survey of human neuroimaging studies. Neurosci Biobehav Rev. 2014;38:1–16. doi: 10.1016/j.neubiorev.2013.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McClure SM., Bickel WK. A dual-systems perspective on addiction: contributions from neuroimaging and cognitive training. Ann N Y Acad Sci. 2014;1327:62–78. doi: 10.1111/nyas.12561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Parsons LH., Hurd YL. Endocannabinoid signalling in reward and addiction. Nat Rev Neurosci. 2015;16(10):579–594. doi: 10.1038/nrn4004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Volkow ND., Koob G., Baler R. Biomarkers in substance use disorders. ACS Chem Neurosci. 2015;6(4):522–525. doi: 10.1021/acschemneuro.5b00067. [DOI] [PubMed] [Google Scholar]
- 34.Lagadec S., Allard M., Dilharreguy B., Schweitzer P., Swendsen J., Sibon I. Linking imaging data to daily life: the example of post-stroke depression. Neurology. 2012;78(5):322–325. doi: 10.1212/WNL.0b013e31824528b2. [DOI] [PubMed] [Google Scholar]
- 35.Ernst M., Paulus MP. Neurobiology of decision making: a selective review from a neurocognitive and clinical perspective. Biol Psychiatry. 2005;58(8):597–604. doi: 10.1016/j.biopsych.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 36.Grant S., Contoreggi C., London ED. Drug abusers show impaired performance in a laboratory test of decision making. Neuropsychologic . 2000;38(8):1180–1187. doi: 10.1016/s0028-3932(99)00158-x. [DOI] [PubMed] [Google Scholar]
- 37.Bechara A., Damasio H. Decision-making and addiction (part I): impaired activation of somatic states in substance dependent individuals when pondering decisions with negative future consequences. Neuropsychology. 2002;40:1675–1689. doi: 10.1016/s0028-3932(02)00015-5. [DOI] [PubMed] [Google Scholar]
- 38.Bechara A., Dolan S., Hindes A. Decision-making and addiction (part II): myopia for the future or hypersensitivity to reward? Neuropsychoiogia. 2002;40(10):1690–1705. doi: 10.1016/s0028-3932(02)00016-7. [DOI] [PubMed] [Google Scholar]
- 39.Ernst M., Grant SJ., London ED., Contoreggi CS., Kimes AS., Spurgeon L. Decision making in adolescents with behavior disorders and adults with substance abuse. Am J Psychiatry. 2003;160(1):33–40. doi: 10.1176/appi.ajp.160.1.33. [DOI] [PubMed] [Google Scholar]
- 40.Dom G., De Wilde B., Hulstijn W., Van Den Brink W., Sabbe B. Decision-making deficits in alcohol-dependent patients with and without comorbid personality disorder. Alcohol Clin Exp Res. 2006;30(10):1670–1677. doi: 10.1111/j.1530-0277.2006.00202.x. [DOI] [PubMed] [Google Scholar]
- 41.Swendsen J., Palmier-Claus J., Nezlek J., D'Argel A., Leboyer M. Mobile and connected technologies in psychiatry state-of-the-art and future directions. Paper presented at 23rd European Psychiatry Association Conference March 12-15, 2015 Vienna, Austria. [Google Scholar]


