Abstract
A 68‐year‐old woman with interstitial lung disease related to dermatomyositis and systemic scleroderma was admitted to our hospital with fever and dyspnoea. Although the fever was reduced after antibiotic therapy, a left pneumothorax suddenly occurred on day 27 after admission. A continuous air leak persisted despite chest drainage with three tubes and repeated pleurodesis. Chest computed tomography (CT) images showed a cavitary lesion with a pinhole in the left upper division, which was suspected to be the affected lesion with the air leak. Virtual bronchoscopic navigation images were constructed from CT data. Bronchial occlusion with Endobronchial Watanabe Spigots (EWSs) was performed on day 52. Two medium‐sized EWSs were inserted into the left B1 + 2a and B1 + 2b, and the air leak stopped immediately. No procedure‐related adverse events occurred. All three chest tubes were successfully removed by day 60. This case demonstrates that virtual bronchoscopic navigation can improve bronchial occlusion procedures using EWSs.
Keywords: Bronchial occlusion, bronchopleural fistula, Endobronchial Watanabe Spigot, pneumothorax, virtual bronchoscopic navigation
Introduction
Bronchopleural and alveolar‐pleural fistulas with persistent air leaks can cause significant morbidity and increase the risk of mortality. Fistulas are commonly related to underlying pulmonary diseases, including bullous emphysema, interstitial lung disease, and necrotizing pneumonia. Surgical interventions are often inappropriate because of the patients' poor performance status.
Bronchial occlusion with silicone spigots (Endobronchial Watanabe Spigot [EWS]) is a useful alternative for patients who are not candidates for surgical intervention 1. During the bronchial occlusion procedure, a balloon catheter is generally used to identify the affected bronchus. Speedy identification of the affected bronchus is necessary for the patient's comfort and safety; thus, accurate prediction of the affected bronchus is necessary before the procedure.
A virtual bronchoscopic navigation (VBN) system supports the diagnosis of peripheral pulmonary lesions by identifying bronchi reaching the lesions 2. However, there have been no reports of its successful use for bronchial occlusion. We, herein, report a case of a persistent air leak successfully treated using bronchial occlusion with EWSs under VBN.
Case Report
The patient was a 68‐year‐old woman with interstitial lung disease related to dermatomyositis and systemic scleroderma who was receiving long‐term oxygen therapy and oral prednisolone (20 mg per day) and azathioprine (50 mg per day). She was admitted to our hospital with fever and dyspnoea. The fever was reduced after intravenous antibiotic therapy (meropenem 3 g/day) for 10 days. However, sudden respiratory deterioration occurred on day 27 after admission. Chest X‐ray revealed left pneumothorax, and chest drainage was started immediately. However, a continuous air leak persisted despite chest drainage with three tubes and repeated autologous blood patch pleurodesis. Respiratory failure during exercise (Peripheral capillary oxygen saturation (SpO2) of 96% with oxygen supplied at 4 L/min) persisted and severe pneumoderma (subcutaneous emphysema) rapidly progressed. Therefore, a multidisciplinary team in our hospital concluded that endoscopic bronchial occlusion with EWS should be performed.
Chest computed tomography (CT) images before bronchoscopy showed a cavitary lesion with a pinhole in the left upper division, which was suspected to be the affected lesion. VBN images were constructed by a computer‐assisted VBN system (LungPoint®, Bronchus Ltd.) 3, and a bronchial route to the left B1 + 2a was indicated for the cavitary lesion (Fig. 1).
Figure 1.
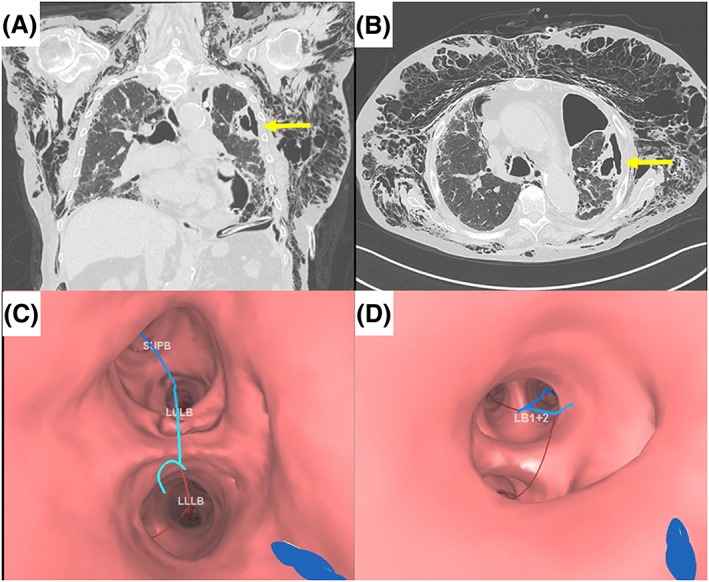
(A, B) Chest computed tomography images on day 48 show severe pneumoderma and a cavitary lesion with a pinhole on the left S1 + 2 (arrows). (C, D) Virtual bronchoscopic navigation images on LungPoint® indicate a bronchial route to the left B1 + 2a to the cavitary lesion.
On day 52, endobronchial occlusion was performed using two bronchoscopes (BF‐1 T260 and BF‐P260, Olympus Ltd.) under local anesthesia with intravenous administration of midazolam for mild sedation. Complete termination of the air leak was confirmed when a balloon catheter was inserted into the left B1 + 2. Two medium‐sized EWSs (6 mm diameter) were inserted into the left B1 + 2a and B1 + 2b, and the air leak stopped immediately (Fig. 2). Removal of the EWSs was not planned due to the risk of pneumothorax recurrence. No procedure‐related adverse events occurred. The severe pneumoderma gradually disappeared, and all three chest tubes were successfully removed by day 60.
Figure 2.
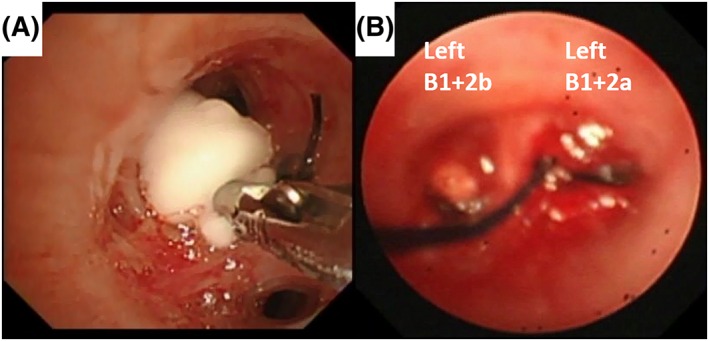
Bronchial occlusion with Endobronchial Watanabe Spigots (EWSs). (A) A medium‐sized EWS is guided in the direction of the left B1 + 2 with a grasping forceps. (B) Two medium‐sized EWSs are inserted into the left B1 + 2a and B1 + 2b. The EWSs are sutured with nylon threads so they can be easily grasped with forceps if they drop off.
Discussion
We report a case of a bronchopleural fistula successfully infilled by EWSs based on a VBN pathway. Bronchial occlusion with EWS is a useful and safe strategy for patients with severe underlying pulmonary diseases. Sasada et al. previously reported that EWS usage successfully eliminated or reduced air leaks in 79.2% of 24 patients, including four patients requiring mechanical ventilation. In their report, however, balloon occlusion tests revealed the affected bronchi in 10 of 23 patients 4. Patients with severe disease, such as the patient in this case report, cannot tolerate prolonged bronchoscopic procedures; therefore, it is important to determine the affected bronchi based on the chest CT images before the procedure. In this case, we accurately identified the affected bronchi before the procedure and successfully inserted EWSs based on the VBN images.
Although endobronchial occlusion with EWS is a simple procedure using grasping forceps, a certain training period is required for successful EWS insertion. In addition to prior training on a bronchial model, three‐dimensional image training using VBN can be useful for technical improvement. For the diagnosis of peripheral pulmonary lesions, VBN images are associated with better diagnostic performance and a shorter procedure time 2. In this case, the image simulation before the procedure using the VBN images was helpful both for the detection of the affected bronchi by the balloon occlusion test and for smooth insertion of EWSs; therefore, we successfully performed the procedure with minimal patient discomfort.
A practical problem with this technique is that a computer‐based VBN system has a high additional cost. However, a recent report suggests that a VBN constructed by a CT workstation was useful for the diagnosis of peripheral pulmonary lesions 5. No additional cost is required to create VBN images with a multidetector‐row CT workstation, and thus, VBN images can be available for many types of bronchoscopic interventions in many hospitals. A limitation of this technique is that VBN can possibly be of help only when there is a focal abnormality on the CT images, as in this case.
In conclusion, VBN can be a supportive tool for endobronchial occlusion with EWS. A careful simulation using three dimensional VBN images should be performed before the procedure to maximize the patient's safety and comfort.
Disclosure Statements
No conflict of interest declared.
Appropriate written informed consent was obtained for publication of this case report and the accompanying images.
Hayama, M. , Sato, S. , Shiroyama, T. , Nishida, T. , Nishihara, T. , and Okamoto, N. (2016) Endoscopic bronchial occlusion with silicone spigots under virtual bronchoscopic navigation. Respirology Case Reports, 4 (4), e00157. doi: 10.1002/rcr2.157.
References
- 1. Watanabe Y, Matsuo K, Tamaoki A, et al. 2003. Bronchial occlusion with Endobronchial Watanabe Spigot. J. Bronchol. 10:264–267. [Google Scholar]
- 2. Ishida T, Asano F, Yamazaki K, et al. 2011. Virtual bronchoscopic navigation combined with endobronchial ultrasound to diagnose small peripheral pulmonary lesions: a randomised trial. Thorax 66:1072–1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tamiya M, Okamoto N, Sasada S, et al. 2013. Diagnostic yield of combined bronchoscopy and endobronchial ultrasonography, under LungPoint guidance for small peripheral pulmonary lesions. Respirology 18:834–839. [DOI] [PubMed] [Google Scholar]
- 4. Sasada S, Tamura K, Chang YS, et al. 2011. Clinical evaluation of endoscopic bronchial occlusion with silicone spigots for the management of persistent pulmonary air leaks. Intern. Med. (Tokyo, Japan) 50:1169–1173. [DOI] [PubMed] [Google Scholar]
- 5. Matsumoto Y, Izumo T, Sasada S, et al. 2015. Diagnostic utility of endobronchial ultrasound with a guide sheath under the computed tomography workstation (ziostation) for small peripheral pulmonary lesions. Clin. Respir. J. DOI:10.1111/crj.12321. [DOI] [PubMed] [Google Scholar]


