Abstract
Introduction:
It is believed that the outcomes of robotic surgery depends not only on the experience of the console surgeon but also the patient-side assistant. However, objective data supporting it is lacking. The aim of this study was to objectively determine change in operative outcomes with increasing experience of patient-side assistant.
Materials and Methods:
We performed a retrospective analysis of 222 urologic robotic procedures performed by two teams of surgeon-assistant and split the data into two chronological halves according to date of surgery. We considered that the assistant was inexperienced in the 1st half and had become experienced by the 2nd half, and we compared mean operative time and blood loss between these two halves of his experience.
Results:
We observed that with increasing experience of the assistant, the mean operative time reduced from 138.06 to 124.32 min (P = 0.001) and mean blood loss decreased from 191.93 to 187.61 ml (P = 0.57). On subset analysis, a consistent trend of reduction in the mean operative time was noted for both the assistants separately and for all surgical procedures included in the analysis. Maximum reduction was noted for pyeloplasty which was the most commonly performed surgery. The mean blood loss had a varied relation to the experience of the assistant and did not reach statistical significance in either direction.
Conclusions:
With increasing experience of the patient-side surgeon, the mean operative time for all robotic procedures showed a consistent trend of reduction across all types of surgery with greater reduction for commonly performed procedures.
Key words: Outcomes of robotic surgery, robotic surgery, scrubbed surgeon, surgical robot
INTRODUCTION
The surgical da Vinci® robot revolutionized laparoscopic surgery, especially urologic and pelvic surgery, ever since its inception at the beginning of this century. However, at the same time, it shifted the main surgeon away from the patient cart, with no direct control at the tableside. As a result, it necessarily mandated the presence of another surgeon who would scrub and stand as assistant by the patient's side. This assistant must be skilled enough in technical work associated with the robotic patient-side cart and also provide pure laparoscopic assistance. This makes the role of the assistant surgeon even more important than in pure laparoscopy. It has been felt that a trained patient-side surgeon who can skillfully accomplish his/her role during the procedure is most important for establishment of a successful robotic program.[1] Even though literature exists with regard to impact on outcomes with the experience of the main surgeon, there is no existing objective evidence regarding the impact on outcomes with the experience of the assistant surgeon in robot-assisted surgery. The goal of this study was to objectively verify the hypothesis that the experience of patient-side assistant in robotic surgery affects intraoperative outcomes.
MATERIALS AND METHODS
This retrospective analysis was based on robotic surgeries performed at a single tertiary care center from July 2006 to June 2013. We analyzed all our data and selected two most frequent robotic patient-side assistants (assistant 1 [A1] and assistant 2 [A2]). Cases assisted by these selected assistants to a single surgeon were included for analysis: A1-assisted surgeon 1 (S1) and A2-assisted surgeon 2 (S2). Each of these selected surgeons was amply experienced and had already completed > 50 robotic procedures. Only five most commonly performed robotic surgeries were considered (radical prostatectomy, pyeloplasty, ureterolithotomy, radical cystectomy, and partial nephrectomy). A total of 222 cases were thus included for analysis (70 by A1-S1 and 152 by A2-S2). For each assistant, the cases he assisted were split into two halves (if the total number was odd, the median case was excluded). It was assumed that the particular assistant was inexperienced in the 1st half and more experienced in the latter half. Outcomes in terms of intraoperative measures such as total operative time, blood loss, and complications were compared between the first and second halves of the assistant's experience. Analysis was first done for pooled data and then for each assistant separately. Comparison was also made between the 1st and 2nd halves of experience for each separate surgery type.
All the data were analyzed with SPSS 20.0 (SPSS Inc., Chicago, IL, USA) and nonparametric test (Wilcoxon signed rank test) was used, and P < 0.05 was considered statistically significant. Linear regression was used to assess the possible cutoff level for the learning curve in terms of reduction in operative time for the assistants. Mean operative time of five consecutive cases was plotted and the line of best fit was drawn. Linear regression model was used to calculate the reduction in operative time with increasing experience of the assistant.
RESULTS
A total of 222 cases were analyzed, the mean age of study population was 47.3 years, and 186 (87.3%) were males. On comparing intraoperative outcomes between the 1st and 2nd halves according to the assistants experience, the mean operative time reduced from 138.06 min to 124.32 min (P = 0.001) and mean blood loss decreased from 191.93 mL to 187.61 mL (P = 0.57).
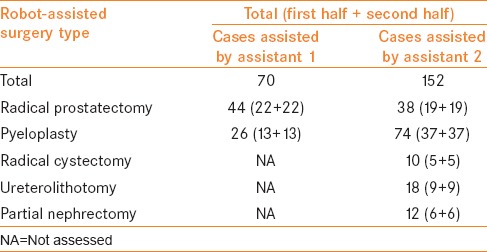
The data were then further subdivided based on assistant and surgery type [Table 1]. Seventy cases were assisted by A1 and 152 by A2. On comparing intraoperative outcomes between the 1st and 2nd halves of A1's experience, the mean operative time reduced from 152.1 min to 150.2 min (P = 0.76) and mean blood loss decreased from 235.7 ml to 145.5 ml (P = 0.02). For A2, with his increasing experience, the mean operative time reduced from 131.5 min to 112.69 min (P = 0.001) and mean blood loss increased from 171.7 ml to 208.2 ml (P = 0.31).
Table 1.
Number of cases included in study classified according to assistant and the surgery type
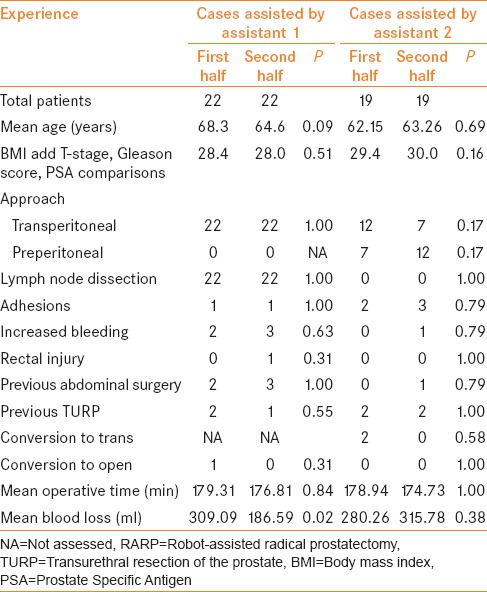
On dividing data according to the type of surgery assisted, a total of 82 cases of robot-assisted radical prostatectomy (RARP) were analyzed. On comparing outcomes between the 1st and 2nd halves of the assistant experience in RARP, the mean operative time reduced from 179.1 min to 175.8 min (P = 0.89) and mean blood loss decreased from 295.7 ml to 246.4 ml (P = 0.37). Of the total 82 cases of RARP, A1 assisted 44 cases and A2 assisted 38 cases. A1-S1 used a transperitoneal approach with bilateral pelvic lymph node dissection in all of 44 patients. One case in the 1st half of their experience was converted to open due to dense adhesion, and another one had rectal injury requiring open repair after the procedure. A2-S2 used transperitoneal approach in 19 and preperitoneal in 19 of their 38 cases. No patient underwent pelvic lymph node dissection. No conversion to open or rectal injury was noted. Two patients were converted to transperitoneal in their 1st half of experience because of inadequate space (1 case) and peritoneal breach (1 case). Patient profile and intraoperative outcomes are presented in Table 2. The mean blood loss of A1-S1 reduced from 309.09 ml to 186.59 ml (P = 0.02) with increasing experience of A1. An insignificant reduction was also noted in operative time of A1-S1 (179.31 min to 176.81 min, P = 0.84) and A2-S2 (178.94 min to 174.73 min, P = 1.0). However, an insignificant increase was noted in blood loss for A2-S2 (280.26 ml to 315.78 ml, P = 0.38) with the increasing experience of assistant.
Table 2.
Patient profile and intraoperative outcomes of those who underwent robot-assisted radical prostatectomy
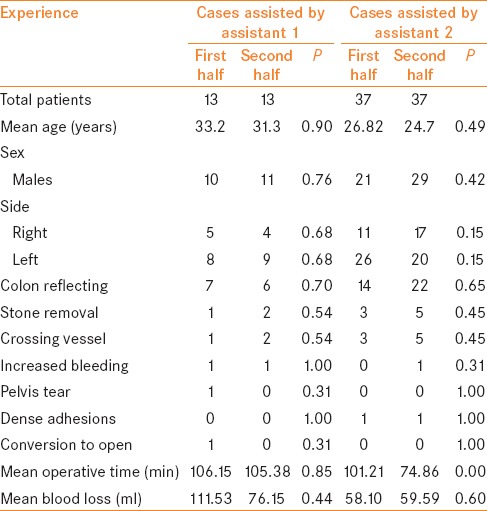
A total of 100 cases of robot-assisted laparoscopic pyeloplasty were analyzed and on comparing outcomes between the 1st and 2nd halves of the assistant experience, the mean operative time reduced from 102.50 min to 82.80 min (P = 0.001) and mean blood loss reduced from 72.00 ml to 63.90 ml (P = 0.91). Of these 100 cases, A1 assisted 26 cases and all of these were transperitoneal Anderson–Hynes dismembered type. One case was converted to open in the 1st half of their experience as ureter could not be identified. The remaining 74 cases were assisted by A2; all were transperitoneal Anderson–Hynes dismembered type except one in which Foleys' Y-V plasty was done for high insertion of ureter. No conversions or major complications were noted. Patient profile and intraoperative outcomes are shown in Table 3. There was an insignificant reduction in mean operative time (106.15 min to 105.38 min, P = 0.85) and mean blood loss (111.53 ml to 76.15 ml, P = 0.44) for A1, with increasing experience of the assistant. For A2, a significant reduction was noted in mean operative time (101.21 min to 74.86 min, P = 0.00) with no change in mean blood loss (58.10 ml to 59.59 ml; P = 0.60).
Table 3.
Patient profile and intraoperative outcomes of those who underwent robotic pyeloplasty
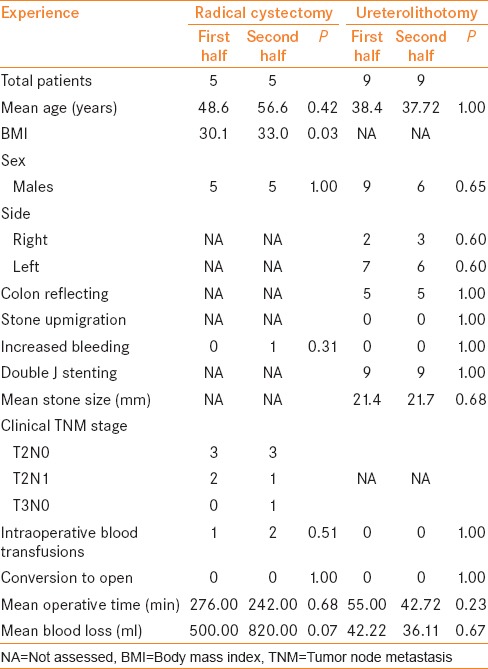
Only 10 patients underwent robotic radical cystectomy with bilateral pelvic lymph node dissection and extracorporeal ileal conduit in all. All cases were assisted by A2. The patient profile and intraoperative outcomes are presented in Table 4. The mean operative time reduced from 276 min to 242 min (P = 0.68) but an insignificant increase in mean blood loss was noted from 500 ml to 820 ml (P = 0.07). All the 18 cases of uretrolithotomy were assisted by A2, done via transperitoneal route and all were stented antegradely. There was difficulty in identifying ureter in one patient in the 1st half of experience of the team. One patient had retroperitoneal hematoma due to Veress needle insertion in latter part of A2's experience. The patient profile and intraoperative characteristics are shown in Table 4. With increasing experience of the first assistant, an insignificant decrease in mean operative time (55.00 min to 42.77 min, P = 0.23) and mean blood loss (42.22 ml to 36.11 ml, P = 0.67) was noted.
Table 4.
Patient profile and intraoperative outcomes in patients who underwent robotic radical cystectomy and ureterolithotomy assisted by assistant 2
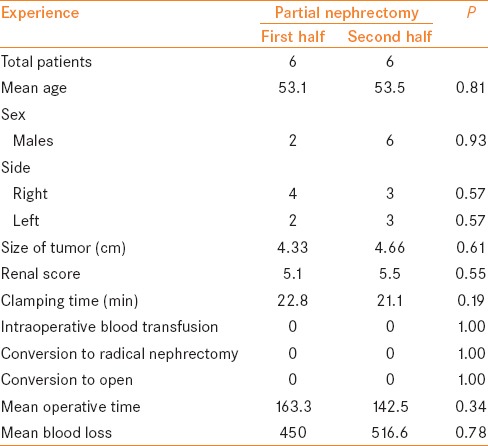
A2 assisted robotic partial nephrectomy on 12 patients, all by transperitoneal route. There were no conversions to either radical nephrectomy or open surgery. The patient profile and intraoperative outcomes are presented in Table 5. The mean operative time insignificantly reduced from 163.3 min to 142.5 min (P = 0.34), but we noticed an insignificant increase in blood loss from 450 ml to 516.6 ml (P = 0.78).
Table 5.
Patient profile and intraoperative outcomes in patients who underwent robotic partial nephrectomy assisted by assistant 2
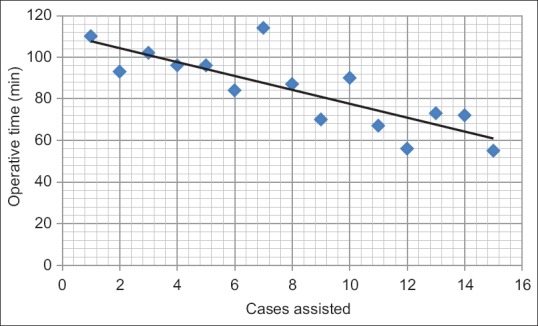
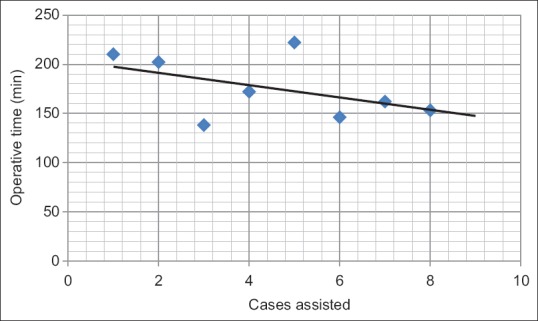
Mean of operative time for five sequential cases was calculated and plotted to see the line of best fit to depict the trend over increasing experience of a single assistant [Figures 1–4]. Using the linear regression model for prostatectomy, we found that after every five cases assisted by A1, there is a reduction of 0.33 min in the mean operative time for next five cases he assisted. Similarly, for A2, with every five cases assisted, there is a reduction of 6.25 min in the mean operative time for next five cases. Thus, as the assistant is gaining experience, the procedure is taking less time. Similarly, using linear regression model for pyeloplasty, with every five cases assisted, there is a reduction of 1.42 min in mean operative time of next five cases for A1 and 3.5 min for A2.
Figure 1.
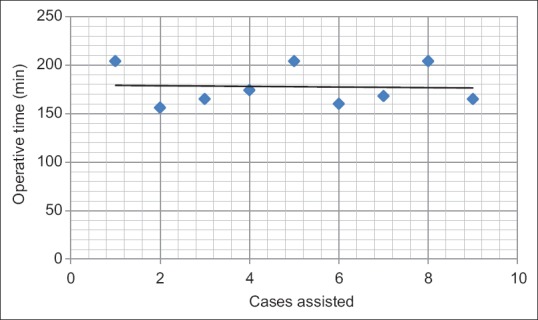
Linear regression model for operative time for assistant 1 for radical prostatectomy. Each point represents mean operative time of five sequential cases
Figure 4.
Linear regression model for operative time for assistant 2 for pyeloplasty. Each point represents mean operative time of five sequential cases
Figure 2.
Linear regression model for operative time for assistant 2 for radical prostatectomy. Each point represents mean operative time of five sequential cases
Figure 3.
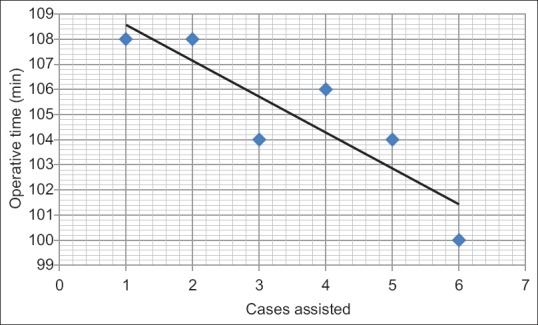
Linear regression model for operative time for assistant 1 for pyeloplasty. Each point represents mean operative time of five sequential cases
DISCUSSION
The robot may make a technically difficult and demanding procedure look easy but it cannot function without a skilled assistant. The literature on robotic surgery is mostly concerned about feasibility, surgical outcomes, and experience or learning curve of the main console surgeon.[2] Some studies do mention the need for a well-trained team, but very few studies objectively determine the importance of skilled assistance. A prospective study showed that in nonurologic robotic surgery a more trained assistant is quicker and accurate.[2] Another retrospective analysis had shown that for robotic partial nephrectomy, an experienced assistant is more likely to assist in more complex cases but the perioperative outcomes were same.[3] The importance of tableside assistance is indirectly illustrated by studies that recommend use of fourth arm or robotic bulldog clamps to increase console surgeons independence.[4] However, the independence can never be complete and all these studies are either nonurologic or limited to a particular set of surgery. To our knowledge, this is the first study to have objectively analyzed the impact of experience of assistant surgeon on outcomes in robotic surgery.
While the impact of main surgeon's experience can never be completely undone, our methodology tended to minimize its impact. First 50 cases of each main console surgeon were excluded from the analysis. Further, the main console surgeon continued to gain experience with other assistants as well. Thus, even though the impact of main surgeon's increasing experience was minimized, the results obtained in the study still represent those of a fixed surgical team than an individual assistant. Other operative room staff had been effectively consistent and unchanged during the entire study period. This included a dedicated robot technician who confirms the working condition of the robot and instruments before each case and a technical assistant who scrubs along with another nurse for each case. Availability of a consistent paramedical team in our study helped minimize the possible confounding effect on operative time from factors other than the assistant or main surgeon. In addition, ours being a teaching hospital, 4th arm had been very sparingly used in our series. This again limits the confounding effect on assistant's work. At our center, the first assistant is usually a second or final year resident with basic laparoscopic training and no formal training in robotic surgery. No simulation facility is available for learning robotic surgery. Over their residency, the residents learn laparoscopic and robotic techniques by observation and practice exercises and then play the role of patient-side assistants.
We found that with increasing experience of tableside assistant, the mean operative time reduced by 13.7 min (range 1.9 to 26.1 min). Given the retrospective nature of study, it is not possible for us to suggest which part of operative time (port placement, docking, or surgery itself) showed maximum reduction. However, we noted a consistent trend of reduction in mean operative time for both the assistants and for all surgical types included in the analysis. On stratifying the data according to the surgery performed, a mean reduction of 3.29 min for radical prostatectomy, 19.7 min for pyeloplasty, 34 min for radical cystectomy, 12.3 min for ureterolithotomy, and 20.8 min for partial nephrectomy was observed. A significant reduction in mean operative time was seen in pyeloplasty cases assisted by A2. S2-A2 performed 74 cases together, which provided adequate exposure and understanding of surgical steps, thus making the team more efficient in terms of assistant's port placement, self-anticipation of surgical steps and time saved in instrument exchanges and various laparoscopic steps during the procedure.
The relationship of mean blood loss and experience of assistant was more varied. It decreased with increasing experience of A1 but increased with A2. For type of surgery, an insignificant reduction was noted for all types except in radical cystectomy where there was a significant increase and in RARP and pyeloplasty assisted by A2, where there was insignificant increase. A nonsignificant reduction was seen in all other cases. In radical cystectomy, the significant increase in blood loss can be attributed to heavy bleeding in one patient with advanced disease that skewed our data. If we exclude the skewer, mean blood loss during latter half of experience reduces from 820 ml to 650 ml, and difference between the 1st and latter half of experience becomes insignificant (P = 0.14). In addition, the body mass index of patients operated in the latter half of experience was higher which could have resulted in this insignificant increase in blood loss. For all other surgeries, this varied presentation can be explained by fact that although clip application is assistants' domain (as we do not have robotic clip applicator), primary hemostasis is done by monopolar or bipolar cautery, both of which are in console surgeons' control. In addition, the changes in blood loss may be more apparent for cases with inherently more blood loss such as cystectomy or partial nephrectomy, which did not form a major percentage of cases in our series.
Assistance in robotic surgeries is a complex issue. A skilled assistant can actively participate in complex maneuvers easing the console surgeon provided following points are remembered by both the console surgeon and the assistant. (a) Vision for assistant is two-dimensional in nature, different in angle, and the field of view is slightly less than what is visible to the main surgeon as he gets vision only from one eye of the surgeon. (b) Ports available to the assistant are limited in number and significantly restricted in available angle of working because the he has access to only one side of the patient, the other side being precluded by the bulk of robotic arms. (c) Assistant works with pure laparoscopic instruments. (d) Introduction of assistant's instruments are seldom camera guided and risks organ injury at every exchange. (e) The robotic instruments are thicker (8 mm each) and with their 7° movement, they tend to occupy majority of already limited working area. Because of their bulk and degrees of freedom of movement, the surgeon's movements tend to move or nudge the assistant's instruments especially when the assistant is needed to work closely with main surgeon's field. (f) Unlike pure laparoscopy, the projecting robotic arms necessitate the assistant to stand far from table and work with stretched arms. This negatively impacts the dexterity and also increases the ergonomic load on the assistant. (g) The space crunch inherently associated with extraperitoneal approach leads to placement of assistant ports near to the robotic ports which significantly reduces the spatial freelance and may make some parts of the operative field inaccessible to the assistant. (h) Sudden movement of the robotic arms outside may hit the assistant with punishing force and also have the potential to move the assistant's instrument risking injury to the patient.
Considering all above limitations, it is imperative on both the surgeon and the assistant to understand and respect each other's limitations and work out coordinated surgical movements to help each other. At times, the operator may have to proactively make space for the assistant and make maneuvers for obtaining good assistance. This is even more important when the surgical field is bloody or in critical situations such as vascular control or vigorous bleed.
Our study has some limitations. First, this is a retrospective study and depends on accurate documentation of blood loss and operative time in surgical notes. Second with increasing experience, the surgeon keeps on improving with time (even though the change/improvement is small and difficult to quantify) that may account for some reduction in intraoperative parameters measured. Third, although we divided each assistant's robotic experience into two halves, the learning curve of the assistant may not have been reached by the time he has assisted half of his cases. Fourth, we only considered the robotic training and have not included the laparoscopic training the residents were undergoing side by side that may affect their overall laparoscopic skills. Finally, the number of cases of cystectomy and partial nephrectomy were limited. These are demanding surgeries with inherent more blood loss, time of surgery, and possibility of complications and thus these would tend to project the role of assistant more prominently. However, the strength of our results is fortified by having evaluated the data for two different assistants for evaluating the same hypothesis and evaluating the results for each individual procedure type.
CONCLUSIONS
We found that with increasing experience of patient-side surgeon and associated console surgeon, who form a consistent surgical team, the mean operative time for all robotic procedures shows a consistent trend of reduction across all surgical types and the reduction is highest for most commonly performed procedure.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kumar R, Hemal AK. The ‘scrubbed surgeon’ in robotic surgery. World J Urol. 2006;24:144–7. doi: 10.1007/s00345-006-0068-0. [DOI] [PubMed] [Google Scholar]
- 2.Sgarbura O, Vasilescu C. The decisive role of the patient-side surgeon in robotic surgery. Surg Endosc. 2010;24:3149–55. doi: 10.1007/s00464-010-1108-9. [DOI] [PubMed] [Google Scholar]
- 3.Jeong W, Sammon J, Petros F, Dusik S, Rogers C. V769 the role of the bedside assistant in robotic partial nephrectomy. J Urol. 2010;183:E301. [Google Scholar]
- 4.Rogers CG, Laungani R, Bhandari A, Krane LS, Eun D, Patel MN, et al. Maximizing console surgeon independence during robot-assisted renal surgery by using the fourth arm and TilePro. J Endourol. 2009;23:115–21. doi: 10.1089/end.2008.0416. [DOI] [PubMed] [Google Scholar]


