Abstract
Introduction:
Clavien–Dindo classification system is used for grading complications of various oncological, renal, and endourological procedures. We applied this system for grading the severity of perioperative complications in patients undergoing transurethral resection of bladder tumor (TURBT) and identify parameters predicting these complications.
Materials and Methods:
Data of 984 patients who underwent TURBT from 2006 to 2014 were included in this study. All data was retrospectively collected and analyzed for complications occurring within the first postoperative month. All complications were classified according to the five grades of modified CCS (.Clavien classification system).
Results:
A total of 172 complications were observed in 138 patients. Majority were low grade complications (Grade 1 [77.3%] and Grade 2 [12.7%]). Higher grade complications were rare (Grade 3 [6.4%] and Grade 4 [3.0%]). There was one death (Grade 5 0.6%), with an overall mortality rate of 0.1%. The incidence of complications was significantly greater for age >60 years, baseline serum creatinine >1.4 mg/dl, size of tumor >4 cm, tumor located at dome, resection time >60 min, incomplete resection and if surgery performed by a resident urologist.
Conclusions:
Clavien–Dindo classification system can be easily applied to grade the complications of TURBT, and it is easily reproducible. We observed that TURBT was a safe procedure. Majority of complications were Grade 1–2 (90%) and Grade 3–5 were rare (10%). Postoperative bleeding is the most common complication. A greater rate of complications of TURBT was associated with patient age, size of tumor, location of tumor, surgeon experience, resection time, and completion of tumor resection.
Key words: Bladder tumor, Clavien–Dindo, complications, transurethral resection
INTRODUCTION
Bladder cancer is the seventh most common malignancy in men and the seventeenth most common malignancy in women. Transurethral resection of the bladder tumor (TURBT) is the main procedure in the diagnostic evaluation and treatment of bladder cancer.[1,2] Postoperative morbidity after TURBT ranges from 5.1% to 43.3%.[3,4,5,6,7,8] Variable reporting methods made it difficult to compare complications of TURBT between different studies.[9]
In 1992, the Clavien classification system (CCS) was developed for grading surgical complications, which was modified later by Dindo et al. in 2004 and validated as Clavien–Dindo classification of surgical complications.[10,11]
This classification system has been used for grading complications in oncological procedures such as radical cystourethrectomy[12] and radical prostatectomy;[13] laparoscopic procedures such as pyeloplasty[14] and live donor nephrectomy;[15] endourological procedures such as transurethral resection of prostate,[16] percutaneous nephrolithotomy,[17] and semi-rigid ureteroscopy.[18] However, the modified CCS has been less frequently used for TURBT. We aimed to apply the modified CCS in grading and reporting the severity of perioperative complications in patients who underwent TURBT at our center and assess parameters that may predict the occurrence of these complications.
MATERIALS AND METHODS
Patients admitted with the diagnosis of bladder tumor who underwent TURBT from January 2006 to July 2014 in a tertiary care center of North India were included in this study. Informed consent for the procedure was taken from all patients and the ethics board approved the study. The data were retrospectively collected, reviewed, and assessed for complications occurring within the first postoperative month. Exclusion criteria included a history of previous TURBT, prostate cancer, and associated urethral stricture disease. Baseline parameters were recorded which included age, gender, body mass index, the presence of comorbidities, baseline creatinine, hemoglobin level, and America Association of Anesthesiology score.
Surgical technique
All operations were performed using monopolar electrosurgical system and 24 Fr resectoscope (Karl-Storz). The procedure was performed by the consultant urologists or trainee urology residents. The coagulation and cutting settings were 80 and 120 W, respectively. 1.5% Glycine solution was used as irrigation fluid intraoperatively. After complete resection of bladder tumor, 22 Fr three-way catheter was placed, and continuous irrigation with normal saline was started in the operating room. Postoperatively, intravesical Mitomycin C (MMC) was used according to the European Association of Urology guidelines.[9] Irrigation was continued for 6–8 h postoperatively. Catheter was removed on postoperative day 2 and the patient was discharged after passing clear urine.
Perioperative data was recorded included size of tumor, number of tumorsn, location of tumor, operating time, duration of hospital stay, decline in hemoglobin postoperatively. Histopathology of all patients was evaluated according to tumor-node-metastasis staging system 2010.[19] All complications, which occurred within 30 days of procedures were recorded and classified into five grades of postoperative complications as per modified CCS criteria. Fever was defined as a temperature of more than 100°F. Hematuria that persisted for more than 6 h and had resolved spontaneously by 48 h was defined as “transient hematuria.” Deranged renal function was described as serum creatinine more than 1.4 mg/dl. Prolonged operative time was defined as more than 60 min. The operating time was generally limited to 90 min as per hospital protocol.
RESULTS
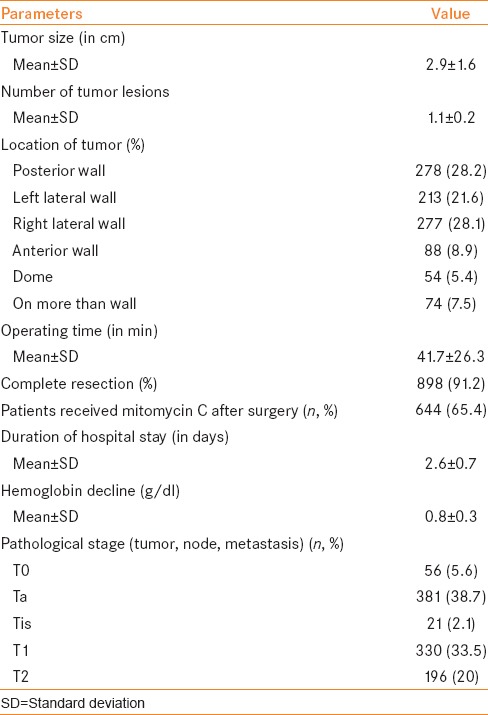
A total of 1186 patients underwent TURBT during the study period. A total of 202 patients were excluded from the study (history of previous TURBT in 164, associated urethral stricture disease in 27, and history of prostate cancer in 11). Finally, 984 patients were enrolled in this study. Baseline preoperative data of all patients is summarized in Table 1. Mean age of study group was 53.8 ± 24.7 years. 82.1% patients were male, and the rest were female. History of smoking was present in 56.8% (n = 559). 23.9% of patients (n = 226) had catheter inserted preoperatively due to urinary retention. Tumor characteristics and perioperative parameters are summarized in Table 2. Mean tumor size was 2.9 ± 1.6 cm. Mean number of tumor lesions was 1.1 ± 0.2. Tumor was located on lateral, posterior, anterior wall, dome, and on more than one wall in 49.7% (n = 490), 28.2% (n = 278), 8.9% (n = 88), 5.4% (n = 54), and 7.5% (n = 74), respectively. Mean operative time was 41.7 ± 26.3 min; duration of hospital stay was 2.6 ± 0.7 days. 65.4% patients (n = 644) received intravesical MMC perioperatively. T stage on histopathology was T0, Ta, Tis, T1, and T2 in 5.6%, 38.7%, 2.1%, 33.5%, and 20%, respectively.
Table 1.
Baseline preoperative data of 984 patients who underwent transurethral resection of bladder tumor
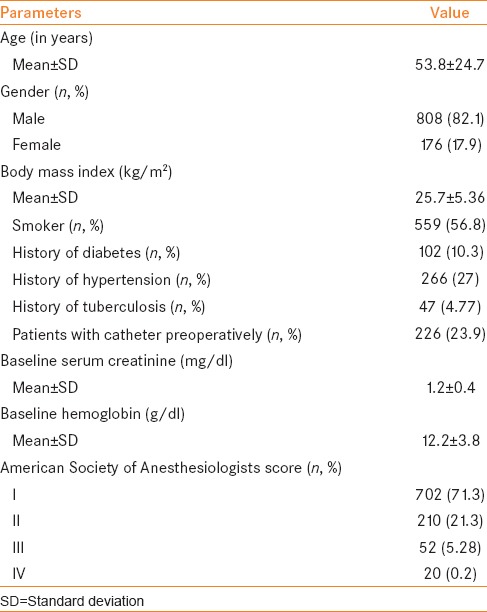
Table 2.
Perioperative data of 984 patients who underwent transurethral resection of bladder tumor
A total of 172 complications were observed in 138 patients with 14% incidence of postoperative complications. All complications were categorized according to five grades of CCS and summarized in Table 3. Majority were low grade complications (Grade 1: 77.3% [n = 133] and Grade 2 in 12.7% [n = 22], respectively). Higher grade complications were rare (Grade 3: 6.4% [n = 11] and Grade 4: 3.0% [n = 5], respectively). There was one death (Grade 5: 0.6%) due to acute myocardial infarction (overall mortality rate: 0.1%).
Table 3.
Complications of transurethral resection of bladder tumor classified according to Clavien-Dindo classification
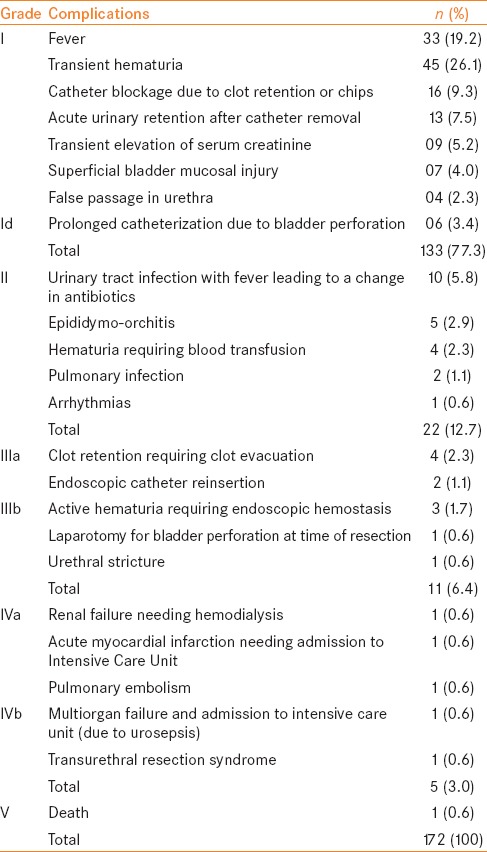
Clavien Grade 4 occurred in five patients who developed life-threatening complications and were admitted to intensive care unit (renal failure requiring haemodialysis-1, acute myocardial infarction-1, pulmonary embolism-1, multiorgan failure due to urosepsis-1, and transurethral resection syndrome-1).
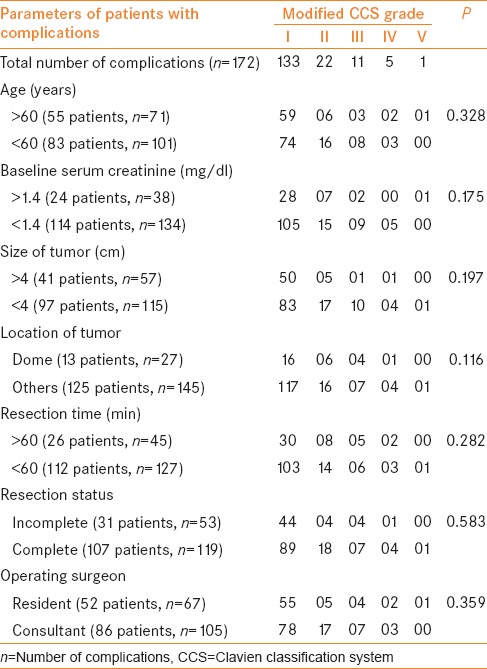
Comparative data between patients with (n = 138) and without complications (n = 846) are listed in Table 4. Table 5 compares the grades of complications according to various parameters. The incidence of complications was significantly greater for age >60 years (P = 0.29), baseline serum creatinine >1.4 mg/dl (P = 0.029), size of tumor >4 cm (P = 0.048), tumor located at dome (P = 0.041), resection time >60 min (P = 0.016), incomplete resection versus complete resection (P = 0.009), and resident urologist versus consultant (P = 0.035). However, these differences were not statistically significant.
Table 4.
Comparison of descriptive data between those with and without complications
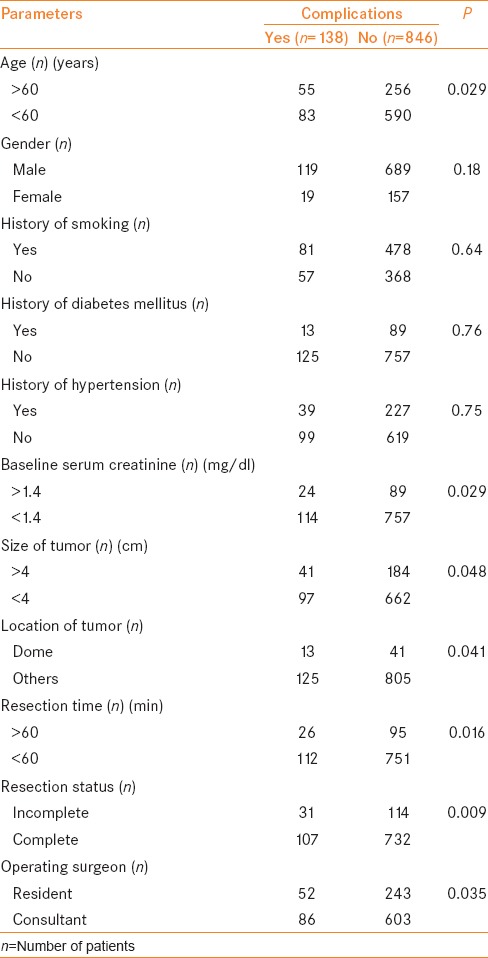
Table 5.
Comparison of grades of complications according to various parameters predicting them
DISCUSSION
This study aimed at using the modified CCS in grading and reporting severity of perioperative complications in patients who underwent TURBT.[3,4,5,6,7,8] To report complications, the modified CCS has been proposed as a standard tool. For the classification of peri- or post-operative complications, Clavien et al. described a four-tiered classification system in 1992.[11] Grade 1 complications include alterations from the ideal postoperative course (nonlife-threatening, and with no lasting disability). Grade 2 includes potentially life-threatening complications but without residual disability (which were further subdivided into IIa and IIb according to the requirement of invasive procedures). Grade 3 is associated with residual disability or persistence of life-threatening conditions. Grade 4 includes death due to complication.
In 2004, Dindo et al. revised this system and divided the complications into five grades (Grade 3 and 4 were further split into “a” and “b”).[10] This classification is proclaimed as Clavien–Dindo classification or modified CCS. According to the authors, this classification is unequivocal and represents a compelling tool regarding the assessment of surgical outcomes.
Clavien Grade 1 and 2 are minor complications but Grade 3–5 are the major complications when compared with other classification system. Modified CCS grants comparison of various studies and their results and being more reproducible, is an imperative tool for quality assessment of surgical outcomes. Competency of a patient to give informed consent is also hampered by the unavailability of standardized tool for reporting their peri- and post-operative complications. Recently, this classification system has been adopted by several urologists and is currently being used for various oncological, renal, and endourological procedures.[12,13,14,15,16,17,18] However, there is a paucity of literature on stratification of complications following TURBT using the Clavien–Dindo system.
TURBT is the cornerstone of diagnosis, and it is the gold standard treatment for patients with nonmuscle invasive bladder cancer. Our study stratifies the complications of TURBT using Clavien–Dindo system. In our study, the overall complication rate of TURBT was 14% with 0.1% mortality rate. This was comparable to 16% morbidity rate with zero mortality in a study done by De Nunzio et al., in Italian cohort, who also graded complications of TURBT in 275 patients according to modified Clavien system.[20]
A total of 172 complications were seen in 138 patients, and most of them (155/172; 90%) were low grade (CCS ≤ II) according to the CCS. The most common complication in this group were transient hematuria (26.1%, n = 45) and fever (19.2%, n = 45). Bladder perforation occurred in 0.71% patients (n = 7/984) with extraperitoneal perforation in 6 patients (managed conservatively with prolonged catheterization) and intraperitoneal perforation in 1 patient (requiring laparotomy). Nearly, 1.72% of patients (17/984) had high-grade complications (CCS ≥ 3). The rate of reintervention was 1.1% (11/984). The indication of reintervention was clot retention requiring clot evacuation in 4, endoscopic catheter insertion due to false passage in the urethra in 2, significant hematuria requiring endoscopic hemostasis in 3, laparotomy for bladder perforation in 1, and urethral stricture requiring internal urethrotomy in 1.
There is limited data in the literature regarding complications and morbidity of TURBT. Nieder et al. prospectively evaluated 173 patients of TURBT and reported complications, i.e. bladder perforation in 3.5% and postoperative bleeding requiring blood transfusion in 2.3% of patients (overall 5.8%).[3] Collado et al. retrospectively reviewed 2821 patients who underwent TURBT and concluded that most common complication was bleeding (2.8%) and bladder perforation (1.3%).[7] Kondás et al. reported that most common complication of TURBT are bladder wall perforation, prostatitis, and bleeding with overall complication and mortality rate of 9.9% and 0.8%, respectively.[8] Dick et al. reviewed data of 373 patients who underwent TURBT and reported that most common complications were urinary tract infection (24%), hemorrhage requiring transfusion (13%), and bladder perforation (5%) with overall mortality of 1.3%.[5] Pycha et al. reported overall complication rate of 16% in 417 patients who underwent TURBT, which includes postoperative bleeding in 8% of patients.[6] However, above studies did not find any parameters which predict complications, nor apply any special criteria for grading and reporting postoperative complications as there was a scarcity of a systematic way for reporting surgical complications.
This is an important obstacle in comparing the related literature, and there is need of a standardized system for reporting complications that can be reproduced easily among researchers and surgeons. Modified CCS is easily reproducible and will help the surgeons worldwide in comparing their experiences. Because of reasonably high incidence of complications reported through this classification system, it may appear stunning at the first look. However, the person who is familiar with this system will observe that most of the complications are minor and are difficult to report with a nonstandardized reporting system.[21]
This modified CCS classification system has been in demand in the recent time as evident by its increased utilization in reporting surgical outcomes from 21% in 2010 to 50% in 2012 according to Yoon et al., who analyzed all published papers in five major journals of urology from 2010 to 2012.[22] Mitropoulos et al. did a systematic review of papers which reports the complications related to urologic procedures, published in 1999–2000 and 2009–2010 in renowned urology journals and purposed that Clavien–Dindo classification is “highly recommended” for reporting urological complications.[23]
However, this system has its own flaws. It has been adversely affected by the incongruity in reporting negative surgical outcomes. Constantinides et al. highlighted that this system lacks the ability to assess the patient's quality of life and does not take into account the comorbidities which have a strong impact on early complications.[24] Moreover, the system does not take into account the surgical skills and technique, which has long-term effects on the patient's quality of life. Complications related to anesthesia such as respiratory and cardiac complications may also adversely affect the surgical outcomes and therefore should be incorporated in the future classification systems. To best of our knowledge, this is the first study that applied modified CCS for evaluating complications of TURBT on a large number of patients in an Indian cohort and identified the parameters, which predict these complications.
CONCLUSION
Clavien–Dindo classification system can be easily applied by an urologist to grade the complications of various procedures. We observed that TURBT is a safe procedure with a low morbidity rate according to CCS system. Majority of complications were Grade 1–2 (90%) and Grade 3–5 were rare (10%). Postoperative bleeding in the form of transient hematuria is the most common complication. A greater rate of complications of TURBT was associated with patient age, baseline serum creatinine, size of tumor, location of tumor, surgeon experience, resection time, and completion of tumor resection.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
I acknowledge the residents of the Urology Department of King George Medical University.
REFERENCES
- 1.Colombel M, Soloway M, Akaza H, Bṏhle A, Palou J, Buckley R, et al. Epidemiology, staging, grading, and risk stratification of bladder cancer. Eur Urol Suppl. 2008;7:618–26. [Google Scholar]
- 2.Traxer O, Pasqui F, Gattegno B, Pearle MS. Technique and complications of transurethral surgery for bladder tumours. BJU Int. 2004;94:492–6. doi: 10.1111/j.1464-410X.2004.04990.x. [DOI] [PubMed] [Google Scholar]
- 3.Nieder AM, Meinbach DS, Kim SS, Soloway MS. Transurethral bladder tumor resection: Intraoperative and postoperative complications in a residency setting. J Urol. 2005;174:2307–9. doi: 10.1097/01.ju.0000181797.19395.03. [DOI] [PubMed] [Google Scholar]
- 4.Babjuk M. Transurethral resection of non-muscle invasive bladder cancer. Eur Urol Suppl. 2009;8:542–8. [Google Scholar]
- 5.Dick A, Barnes R, Hadley H, Bergman RT, Ninan CA. Complications of transurethral resection of bladder tumors: Prevention, recognition and treatment. J Urol. 1980;124:810–1. doi: 10.1016/s0022-5347(17)55677-3. [DOI] [PubMed] [Google Scholar]
- 6.Pycha A, Lodde M, Lusuardi L, Palermo S, Signorello D, Galantini A, et al. Teaching transurethral resection of the bladder: Still a challenge? Urology. 2003;62:46–8. doi: 10.1016/s0090-4295(03)00128-6. [DOI] [PubMed] [Google Scholar]
- 7.Collado A, Chéchile GE, Salvador J, Vicente J. Early complications of endoscopic treatment for superficial bladder tumors. J Urol. 2000;164:1529–32. [PubMed] [Google Scholar]
- 8.Kondás J, Szentgyörgyi E. Transurethral resection of 1250 bladder tumours. Int Urol Nephrol. 1992;24:35–42. doi: 10.1007/BF02552115. [DOI] [PubMed] [Google Scholar]
- 9.Babjuk M, Oosterlinck W, Sylvester R, Kaasinen E, Böhle A, Palou-Redorta J, et al. EAU guidelines on non-muscle-invasive urothelial carcinoma of the bladder, the 2011 update. Eur Urol. 2011;59:997–1008. doi: 10.1016/j.eururo.2011.03.017. [DOI] [PubMed] [Google Scholar]
- 10.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clavien PA, Sanabria JR, Strasberg SM. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery. 1992;111:518–26. [PubMed] [Google Scholar]
- 12.Elshal AM, Barakat TS, Mosbah A, Abdel-Latif M, Abol-Enein H. Complications of radical cysto-urethrectomy using modified Clavien grading system: Prepubic versus perineal urethrectomy. BJU Int. 2011;108:1297–300. doi: 10.1111/j.1464-410X.2010.09987.x. [DOI] [PubMed] [Google Scholar]
- 13.Rabbani F, Yunis LH, Pinochet R, Nogueira L, Vora KC, Eastham JA, et al. Comprehensive standardized report of complications of retropubic and laparoscopic radical prostatectomy. Eur Urol. 2010;57:371–86. doi: 10.1016/j.eururo.2009.11.034. [DOI] [PubMed] [Google Scholar]
- 14.Szydelko T, Kasprzak J, Apoznanski W, Tupikowski K, Pupka A, Janczak D, et al. Clavien classification of complications after 150 laparoscopic pyeloplasties. Urology. 2011;77:1359–64. doi: 10.1016/j.urology.2010.12.025. [DOI] [PubMed] [Google Scholar]
- 15.Ramasamy R, Afaneh C, Katz M, Chen X, Aull MJ, Leeser DB, et al. Comparison of complications of laparoscopic versus laparoendoscopic single site donor nephrectomy using the modified Clavien grading system. J Urol. 2011;186:1386–90. doi: 10.1016/j.juro.2011.05.053. [DOI] [PubMed] [Google Scholar]
- 16.Mamoulakis C, Efthimiou I, Kazoulis S, Christoulakis I, Sofras F. The modified Clavien classification system: A standardized platform for reporting complications in transurethral resection of the prostate. World J Urol. 2011;29:205–10. doi: 10.1007/s00345-010-0566-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mandal S, Goel A, Kathpalia R, Sankhwar S, Singh V, Sinha RJ, et al. Prospective evaluation of complications using the modified Clavien grading system and success rates of percutaneous nephrolithotomy using guy's stone score: A single center experience. Indian J Urol. 2011;28:392–8. doi: 10.4103/0970-1591.105749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mandal S, Goel A, Singh MK, Kathpalia R, Nagathan DS, Sankhwar SN, et al. Clavien classification of semirigid ureteroscopy complications: A prospective study. Urology. 2012;80:995–1001. doi: 10.1016/j.urology.2012.05.047. [DOI] [PubMed] [Google Scholar]
- 19.Sobin LH, Gospodarowicz MK, Wittekind C. TNM Classification of Malignant Tumours. 7th ed. Hoboken, NJ: Wiley-Blackwell; 2010. International union against cancer. [Google Scholar]
- 20.De Nunzio C, Franco G, Cindolo L, Autorino R, Cicione A, Perdonà S, et al. Transuretral resection of the bladder (TURB): Analysis of complications using a modified Clavien system in an Italian real life cohort. Eur J Surg Oncol. 2014;40:90–5. doi: 10.1016/j.ejso.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 21.Graefen M. The modified Clavien system: A plea for a standardized reporting system for surgical complications. Eur Urol. 2010;57:387–9. doi: 10.1016/j.eururo.2009.12.020. [DOI] [PubMed] [Google Scholar]
- 22.Yoon PD, Chalasani V, Woo HH. Use of Clavien-Dindo classification in reporting and grading complications after urological surgical procedures: Analysis of 2010 to 2012. J Urol. 2013;190:1271–4. doi: 10.1016/j.juro.2013.04.025. [DOI] [PubMed] [Google Scholar]
- 23.Mitropoulos D, Artibani W, Graefen M, Remzi M, Rouprêt M, Truss M. European Association of Urology Guidelines Panel. Reporting and grading of complications after urologic surgical procedures: An ad hoc EAU guidelines panel assessment and recommendations. Eur Urol. 2012;61:341–9. doi: 10.1016/j.eururo.2011.10.033. [DOI] [PubMed] [Google Scholar]
- 24.Constantinides CA, Tyritzis SI, Skolarikos A, Liatsikos E, Zervas A, Deliveliotis C. Short- and long-term complications of open radical prostatectomy according to the Clavien classification system. BJU Int. 2009;103:336–40. doi: 10.1111/j.1464-410X.2008.08080.x. [DOI] [PubMed] [Google Scholar]


