Abstract
Four patients diagnosed with chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS), met criteria for National Institute of Health (NIH) Category III prostatitis, failed multiple medicinal treatments and underwent robotic radical prostatectomy (RRP). Median operative time (range): 157 (127–259) min. Validated functional questionnaires responses and NIH CP symptom index (NIH-CPSI) score were collected for each patient's status at different time points pre- and post-operatively. Median decreases (range) were: International Prostate Symptom Score – 14 (1–19); Sexual Health Inventory for Men – 6 (−14–22); and NIH-CPSI total – 23.5 (13–33). Median length of follow-up (range) was 34 (24–43) months. RRP appears to be an option for carefully selected patients with medication-refractory CP/CPPS who understand that baseline sexual function may not be restored postoperatively.
Key words: Chronic pelvic pain syndrome, chronic prostatitis, chronic prostatitis/chronic pelvic pain syndrome, robotic radical prostatectomy
INTRODUCTION
National Institute of Health (NIH) Category III prostatitis or chronic pelvic pain syndrome (CPPS) is characterized by chronic pelvic pain symptoms and possible voiding symptoms in the absence of a urinary tract infection or demonstrable bacterial infection. Chronic prostatitis/CPPS (CP/CPPS) can be a debilitating condition that can affect men of all ages and can even diminish a patient's quality of life. Unfortunately, studies have shown that medical management is ineffective in many patients.[1]
Surgery and minimally invasive therapy as a treatment for CP/CPPS have been previously utilized. Mixed results were found following “radical” transurethral resection of the prostate, which is no longer advocated.[2] Frazier and colleagues reported a series of five men that underwent prostatovesiculectomy for debilitating perineal pain, with three patients experiencing complete relief of pain.[3] Krongrad et al. reported the initial experience with six men undergoing laparoscopic prostatectomy for severe prostatitis as part of an ongoing Phase II clinical trial.[4] All patients experienced resolution of symptoms measured using the CP symptom index (CPSI). Herein, we report the application of robotic radical prostatectomy (RRP) as a treatment option for patients with CP/CPPS refractory to medical intervention.
CASE REPORT
Four patients meeting criteria for NIH Class III CP/CPPS refractory to multimodal medical management strategies underwent RRP by a single surgeon from July 2011 to March 2013. Patients' data were retrospectively gathered by chart review, follow-up clinical visits, and telephone interview. The NIH-CPSI, International Prostate Symptom Score (IPSS) and Sexual Health Inventory for Men (SHIM) questionnaires were collected for each patient's status at different time points pre- and post-operative.
The median duration of CP/CPPS symptoms until RRP reported by the patient cohort was 7.5 years (range 6–20 years). Medications tried unsuccesfully before surgery included finasteride, pentosan polysulfate, antibiotics, various analgesics, tamsulosin, and alprazolam among others. Three patients underwent preoperative transrectal ultrasound-guided 12-core biopsy. One patient was found to have low volume Gleason 6 prostate cancer (3 + 3 in <5% of 1 core), and the other two patients' biopsies were negative. All patients displayed significant symptoms for CP/CPPS. They were counseled thoroughly before RRP about potential other therapeutic options, both medicinal and surgical, for their condition. Informed consent in all patients consisted of a discussion of the material risks, benefits, and alternatives to RRP, with a specific focus on highlighting that this is not standard of care, that there is limited data for CP/CPPS and that there may be complications related to continence and erectile function without alleviating pelvic pain. To optimize the consent process, all patients were referred for second opinions to academic urologists that offer other modalities for refractory CP/CPPS. After deliberation, each patient elected to undergo RRP.
All patients underwent our standard five-port placement configuration RRP successfully. Since the etiology of the condition was benign, a maximal nerve-sparing technique was utilized. Each patient received a bilateral, intrafascial nerve-sparing approach. In addition, we also utilize a pre-prostatectomy program at our institution to instruct men on Kegel exercises. This is subsequently reinforced after the Foley catheter is removed, by both the surgeon as well as through a dedicated physiotherapist who focuses on pelvic floor exercises. Our dissection technique to optimize continence consists of meticulous, atraumatic handling of levator fibers at the prostatic apex, and optimization of urethral length. In addition, urethropexy is performed to bring the anterior bladder neck in close approximation to the pubic symphysis using a 2-0 vicryl® on a CT-1 needle, Figure 8 stitch.
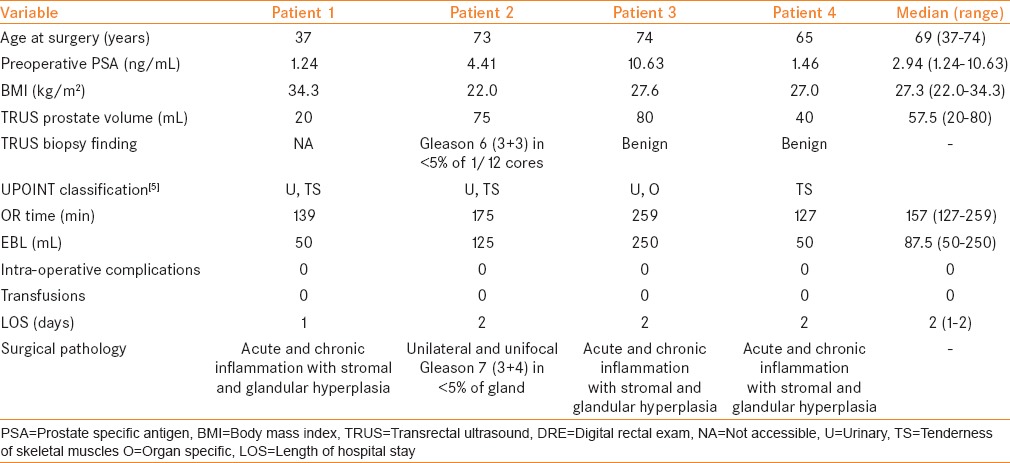
Table 1 provides demographical and perioperative findings. Median operative time (range) was 157 (127–259) minutes without any significant intraoperative or 30-day postoperative complications. Patient #3 had a prolonged surgery due to a concomitant procedure. For Patient #2, the findings from the preoperative biopsy combined with intraoperative findings deemed it necessary for the surgeon to perform a bilateral pelvic lymph node dissection; no metastasis was found on pathology. In all cases, there were no extraordinary intraoperative observations related to scarring or inflammation related to the diagnosis of CP/CPPS.
Table 1.
Patient information
Within the initial 6-month postoperative period, Patient #4 developed meatal stenosis that was treated initially with urethral dilatation and eventually urethral meatoplasty. The patient reports to be doing well to date regarding this complication. Three months before RRP, Patient #1 underwent a cystocopy and since that procedure suffered from urinary retention and required an indwelling catheter until RRP. The patient did not try a voiding trial or medical intervention to treat the retention between his cystoscopy and RRP. Postoperatively, this patient was rendered catheter-free and was able to void without difficulty.
In three patients, the postoperative final pathology revealed evidence of acute and chronic inflammation with stromal and glandular hyperplasia. For Patient #2, final pathology showed unilateral, unifocal Gleason 7 (3 + 4) prostatic adenocarcinoma in <5% of the gland. All lymph nodes were found to be benign.
Table 2 reports on patient outcomes through response to questionnaires. Median follow-up was 34 (24–43) months. Postoperatively, all patients regained full continence within 6 months (defined as no pads or one pad for security). Patient #3 was not evaluable for IPSS due to preoperative catheter use.
Table 2.
Questionnaire response
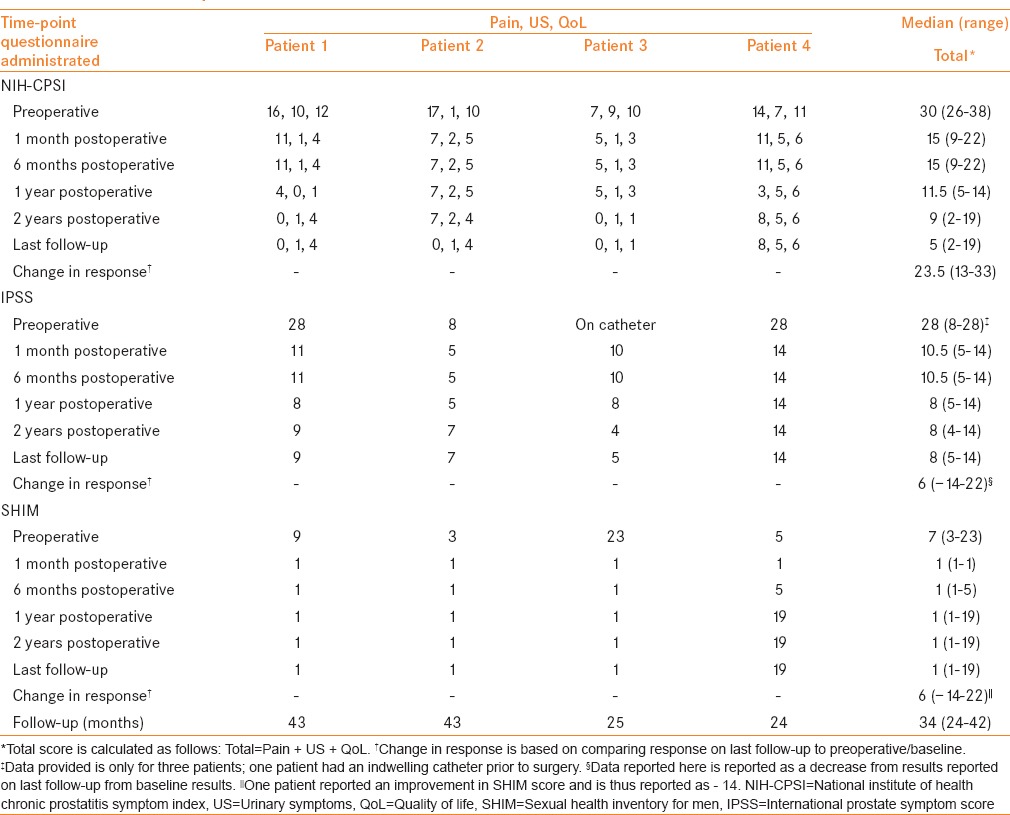
Three patients report very low confidence to achieve a spontaneous erection to date, although none of these men are currently sexually active. One patient did demonstrate an improvement from a preoperative SHIM score of 5 to a score of 19 on last follow-up of 24 months since surgery. All patients report to be doing well to date and report no concerns with their prostate-specific antigen levels from their local physician. Despite a majority of patients being impotent, all patients report to be pleased with the outcome of the procedure as their main complaint was treated.
DISCUSSION
The etiology of CP/CPPS remains uncertain, and while treatment often requires multimodal therapy, it may be refractory with significant detriment to quality of life. RRP may be a viable treatment option in select patients that have failed medical therapies. As the putative etiologies and exacerbating factors in CP/CPPS suggest a complex interplay of psychosocial, psychological, neurological, inflammatory, and infectious factors, a phenotype-directed evidence-based approach should be exhausted before offering surgery.[5] Careful patient counseling and selection remains imperative. Shoskes and Nickel have created the UPOINT phenotypic system for CPPS, where each letter represents a domain that is diagnosed clinically and associated with specific therapies. While this is an attractive approach that simplifies treatment in patients with this challenging diagnosis, it does not address the treatment strategy for patients with medication-refractory CP/CPPS or those patients where none of these therapies successfully alleviate their symptoms.[5]
In our study, the use of RRP for CP/CPPS was able to effectively treat all four patients for their main complaint of lower urinary tract symptoms and pelvic/perineal pain. Each patient exhausted all medical treatment modalities. After appropriate counseling of other available treatment options, each patient sought radical prostatectomy for treatment, thereby representing the utility of RRP in the context of medication treatment failure for CP/CPPS. In our experience, while the motivating rationale for some patients to undertake RRP was to eliminate pelvic/perineal pain, the potential morbidity of RRP was regarded as an acceptable risk. Our study demonstrates the potential utility of contemporary RRP for CP/CPPS.
Ultimately, despite our encouraging results, this study is a small pilot feasibility evaluation, and a prospective multi-institutional study is warranted before RRP can be recommended for widespread uptake for medication refractory CP/CPPS. In addition, the etiology of the patients' complaints may have been entirely psychological, and the belief that removal of the prostate provided an improvement in morbidity, despite not actually providing any evaluable improvement in morbidity other than patient feedback. Nonetheless, in the interim, we advocate careful patient selection and thorough counseling to set reasonable expectations, including a discussion that RRP may potentially worsen pelvic pain and may be associated with permanent impotence. Furthermore, the time interval studied is relatively short and may not capture the risk of long-term return of symptoms or patient regret. Studies demonstrating a longer follow-up period are required to adequately access the outcomes of such treatment.
RRP appears to be a feasible treatment option for a very selective group of patients with medication-refractory CP/CPPS. RRP may be judiciously offered to alleviate the symptoms of CP/CPPS in patients that have exhausted other options of medical management who understand that there is a high potential for loss of sexual function based on our initial results.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Schaeffer AJ. Clinical practice. Chronic prostatitis and the chronic pelvic pain syndrome. N Engl J Med. 2006;355:1690–8. doi: 10.1056/NEJMcp060423. [DOI] [PubMed] [Google Scholar]
- 2.Barnes RW, Hadley HL, O'Donoghue EP. Transurethral resection of the prostate for chronic bacterial prostatitis. Prostate. 1982;3:215–9. doi: 10.1002/pros.2990030303. [DOI] [PubMed] [Google Scholar]
- 3.Frazier HA, Spalding TH, Paulson DF. Total prostatoseminal vesiculectomy in the treatment of debilitating perineal pain. J Urol. 1992;148(2 Pt 1):409–11. doi: 10.1016/s0022-5347(17)36615-6. [DOI] [PubMed] [Google Scholar]
- 4.Krongrad A, Shenghan L. Laparoscopic prostatectomy for severely symptomatic treatment-refractory chronic prostatitis: Preliminary observations from an ongoing phase II clinical trial. UroToday Int J. 2011;4:1944–5784. [Google Scholar]
- 5.Shoskes DA, Nickel JC. Classification and treatment of men with chronic prostatitis/chronic pelvic pain syndrome using the UPOINT system. World J Urol. 2013;31:755–60. doi: 10.1007/s00345-013-1075-6. [DOI] [PubMed] [Google Scholar]


