Abstract
Background
Pain associated with coxarthrosis, typically occurring in middle-aged and elderly patients, very commonly causes considerable limitation of motor fitness and dependence on pharmacotherapy. This article provides an assessment of a rehabilitation program with tailored water exercises in patients with osteoarthritis before and after total hip replacement.
Material/Methods
A total of 192 patients (the mean age 61.03±10.89) suffering from hip osteoarthritis (OA) were evaluated before and after total hip replacement (THR). The clinical study covered measurements of hip active ranges of motion (HAROM) and the forces generated by pelvis stabilizer muscles. Pain intensity was assessed according to analogue-visual scale of pain (VAS) and according to the Modified Laitinen Questionnaire. The patients were divided into 6 groups (4 treatment and 2 control). We compared 2 rehabilitation programs using kinesitherapy and low-frequency magnetic field. One of them also had specially designed exercises in the water. Statistical analysis was carried out at the significance level α=0.05. This was a cross-sectional study.
Results
A positive effect of water exercises on a number of parameters was found in patients with OA both before and after total hip replacement surgery. We noted a significant reduction of pain (p<0.001), increased ranges of motion and muscle strength, and reduced use of medicines (NASAIDs) (p<0.001). A correlation was found between the degree of degenerative deforming lesions and the effects of the treatment process (p<0.01).
Conclusions
1. The rehabilitation program including water exercises most significantly reduced pain in patients with OA before and after total hip replacement surgery. 2. Inclusion of water exercises in a rehabilitation program can reduce the use of medicines in patient with OA and after THR.
MeSH Keywords: Arthroplasty, Replacement, Hip; Osteoarthritis, Hip; Rehabilitation; Water Purification
Background
The development of civilization is connected not only with tremendous improvement of the quality of people’s everyday life, but also with increased risk of injuries. A growing number of people suffer from degenerative lesions due to overload of joints, which are particularly sensitive elements of the locomotor system. Hip joints are especially susceptible to injuries and overload, which can lead to degenerative-deforming lesions. The morbidity of osteoarthritis is disturbing, and hip and knee OA affect many people in different countries [1,2]. The disease progressively reduces ability to engage in activities. Physical activity of these persons is estimated to be considerably lower than in the general population [2]. Various forms of therapy are used in the rehabilitation of patients with hip OA, but new effective procedures are sought [3–14]. Pharmacological therapy and frequent use of NASIDs currently predominate [15].
The aquatic environment has specific properties, in particular, mechanical and thermal properties, that exert a beneficial effect on the musculoskeletal system, which creates favorable conditions for conducting therapy. Exercises in a rehabilitation pool at about 34–35°C can cause myorelaxation, increase the pain threshold, give a sense of greater protection against falls and injury, and facilitate the re-education of gait. The beneficial effects on the psyche of the patient are also very important [12,16]. In this connection, an aquatic environment can play a significant role in rehabilitation of patients with degenerative-deforming lesions and after total hip replacement (THR) surgery. Various studies have explained the therapeutic effects of exercise in water, but there is still a need to confirm it in larger samples of patients with OA [11,12,16,17–23]. The purpose of this study was to assess the effectiveness of physiotherapy combined with treatment in a water environment in patients suffering from hip degenerative-deforming lesions before and after THR.
Material and Methods
The study was conducted at the Center of Treatment, Rehabilitation, and Occupational Medicine “ATTIS” in Warsaw. A total of 192 patients were studied, including 136 women and 56 men, ages 48–82 (61.03± 8.23 years).
96 patients were suffering from degenerative-deforming lesions of the hip joint (the mean age 59.7±9.24). The degenerative lesions were diagnosed as first degree lesions in 25 patients including 18 women, as second degree lesions in 42 patients including 33 women, and as third degree lesions in 29 patients including 17 women. A relevant assessment was conducted according to the 4-degree Altman scale [24].
96-patients were after hip joint replacement (mean age 62.32±11,39), including 46 patients with cemented and 50 patients with uncemented prostheses. The average time between the surgery and the study was 14.8 (min.2–max.18) months.
Average BMIs of the patients were 27.32 in the patients with degenerative lesions and 27.34 in the group of patients after the THR. Detailed data are presented in Table 1.
Table 1.
Age, BMI, and Altman Scale in each research group.
| Group I N-32 |
Group II N-32 |
Group III N-32 |
Group IV N-32 |
Group V N-32 |
Group VI N-32 |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| χ̄ | SD | χ̄ | SD | χ̄ | SD | χ̄ | SD | χ̄ | SD | χ̄ | SD | |
| Age | 59.84 | 6.00 | 63.46 | 9.99 | 58.47 | 5.79 | 60.53 | 8.28 | 63.66 | 9.79 | 60.19 | 7.82 |
| BMI | 27.72 | 5.10 | 27.12 | 4.62 | 26.20 | 4.50 | 27.51 | 5.27 | 27.18 | 4.58 | 27.03 | 5.22 |
| Altman S. | – | – | – | – | 2.00 | 0.76 | 2.06 | 0.72 | – | – | 2.06 | 0.80 |
Analysis of variance (ANOVA) with LSD post hoc tests revealed that the above characteristics did not differ significantly between the groups.
The effectiveness of the therapy involving exercises in a rehabilitation pool applied in the patients suffering from degenerative-deforming lesions and the patients after THR was assessed based on objective and subjective functional parameters. Pain intensity was assessed according to the Visual Analogue Scale (VAS) and Laitinen Scale. Other measures included hip active ranges of motion (HAROM) and measurements of the strength of hip abductors and hip extensors. In all cases, measurements were made by the same physiotherapist and in the same measurement conditions.
HAROMs in horizontal, sagittal, and frontal planes were measured with a manual goniometer (made by MSD Europe bvba in Londerzeel, Belgium) in a patient supine (abduction-adduction), seated (internal-external rotation), and lying on the side (flexion-extension) with trunk and pelvis stabilized. The highest angle value out of 3 consecutive measurements in each plane was noted. Results of measurements in 3 planes were added for each hip, and averaged for each group.
For strength measurement, we used a manual dynamometer CL 162z made by Precision Measurement Systems in Warsaw, Poland. For the hip abduction measurement a patient was placed in supine position with hip and knee extended. The lever of the dynamometer was applied at the level of the lateral femoral epicondyle and the patient was asked to abduct the leg with maximal strength. For the hip extension measurement, a patient was placed in prone position with pelvis and a trunk supported on a couch, with lower extremities extended, flexed to 90 degrees. The measurement was performed with the knee flexed to 90 degrees and the opposite foot stabilized on the ground. The lever of the dynamometer was applied at the level of the femoral epicondyle. For each dynamometric measurement, 3 trials were performed and the highest strength was noted. Results of extensors and abductors measurements were added for each hip, and subsequently averaged for each group.
The patients were randomly assigned to 6 groups (4 therapeutic and 2 control):
Group I comprised patients after THR, undergoing kinesitherapy, low-frequency magnetic field and water exercises;
Group II comprised patients after THR, undergoing kinesitherapy and low-frequency magnetic field, without water exercises;
Group III comprised patients with degenerative-deforming lesions of the hip joint who were subjected to kinesitherapy, low-frequency magnetic field, and water exercises;
Group IV comprised patients with degenerative-deforming lesions of the hip joint undergoing kinesitherapy and low-frequency magnetic field, without water exercises;
Group V first control group comprising patients after THR and awaiting rehabilitation. They were recommended not to perform activities that might aggravate their pain;
Group VI second control group comprising patients suffering from degenerative-deforming lesions of the hip joint and awaiting rehabilitation. They were recommended not to perform activities that might aggravate their pain.
Treatment protocol
Low-frequency magnetic field (the same parameters) was applied in all therapeutic groups (I–IV) (field shape – rectangular – bipolar, frequency – 40 Hz, intensity – 6 mT, treatment time – 20 min) within 20 days together with kinesitherapy. Kinesitherapy of patients with OA (groups III and IV) included hip joint axial traction, non-weight bearing active exercises, free active exercises, and non-weight bearing active exercises with resistance. Kinesitherapy of patients after THR (groups I and II) included the same exercises excluding load-relieving axial traction. Two of the therapeutic groups (I and III) additionally performed exercises in the rehabilitation pool.
Exercises in water were organized in a rehabilitation pool sized 3×10 meters and 1.3 meter deep. The patients performed exercises daily, within 20 days including weekend breaks; each session lasted 30 min. Water temperature was 34°C. Hydrotherapy groups comprised 6 patients. Patients performed about 25 exercises for 1–1.5 min each. These exercises strengthen the extensors muscles and hip abductors (muscle groups weakened in osteoarthritis and after THR) and exercises to increase range of motion in the hip and knee joints.
The hydrotherapeutic session consisted of: warm-up (vigorous forward and sideway walking through water reaching the chest, cycling lower limb exercises with hands on handrails, climbing up the pool wall with knees and hips flexed), main phase (pulling the knees towards the chest, hip abduction with extended hips and knees using buoyant wheels around ankles, hip circular exercises and knee flexion-extension exercises, knee flexion-extension exercises and pulling knees towards the chest using polystyrene flippers on feet, performed in supine position holding a handrail; flexion-extension exercises of hips and knees performed in prone position holding a handrail; pulling knees towards the chest while standing facing the pool wall with flippers on, hip abduction while standing sideways to the pool wall with flippers on; hip flexion-extension while standing sideways to the pool wall with flippers on and buoyant band around ankles); and relaxing phase (slow walk forward and sideway and cycling lower limb exercises with hands on handrails).
The patients from the control groups (V and VI) were examined to be qualified for rehabilitation treatment. As the waiting time that preceded treatment was 6–10 months, they were re-examined after 4 weeks.
The study was conducted with consent of the Management of the Department of Rehabilitation Centre ATTIS in Warsaw and we obtained written consent of patients.
Statistical methods
The Statistica software package was used for statistical calculations. Some of the analyses and diagrams presented in this article were produced using Excel spreadsheet. The subjects were randomly assigned to groups using the random selection function in the Excel program. The agreement between the statistical distribution and normal distribution was assessed using the Shapiro-Wilk test. Significance of the differences between the mean values was determined using analysis of variance for repeated measurements (ANOVA). The Newman-Keuls test was applied for post hoc comparisons in the analysis of variance. For detailed comparisons, the Wilcoxon test (dependent data) or the Mann-Whitney U test (for independent data) was used. Statistical analysis was carried out at the significance level α=0.05.
Results
Treatment methods applied in the study resulted in most cases in positive changes of parameters. Figure 1 presents results of the pain intensity assessment using VAS before and at completion of the treatment. Each individual group subjected to examination showed different levels of pain reduction (Wilcoxon’s test). Specifically, for each group the following statistics were observed: Group I: Z=−4.861, p<0.001, Group II: Z=−4.939, p<0.001, Group III: Z=−4.938, p<0.001, Group IV: Z=−4.940, p<0.001, Group V: Z=−4.242, p<0.01, and Group VI: Z=−2.715, p=0.07. The highest reduction of pain was noted in the patients who performed exercises in the rehabilitation pool (Figure 1).
Figure 1.
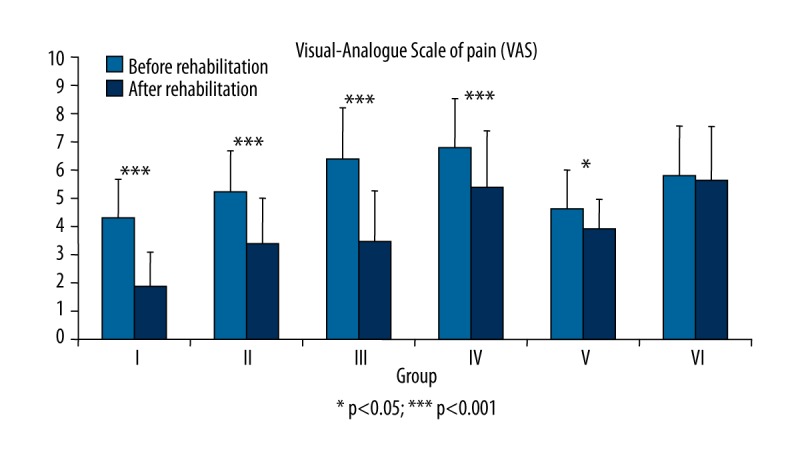
Assessment of pain intensity in the Visual-Analogue Scale of pain (VAS) carried out before and after rehabilitation treatment in each evaluated groups
Figure 2 presents the intensity of pain, which was assessed using the Modified Laitinen Questionnaire. With this method, no significant change of pain intensity perception was noticed in the control groups. Specifically, for each group the following statistics were used: Group I: Z=−4.244, p<0.001, Group II: Z=−3.742, p<0.001, Group III: Z=−5.002, p<0.001, Group IV: Z=−3.464, p=0.001, Group V: Z=−0.577, p=0.564, and Group VI: Z=0.000, p=1.000. The most substantial reduction of pain intensity occurred in patients who exercised in water, similar to the VAS-based assessment (Figure 2).
Figure 2.
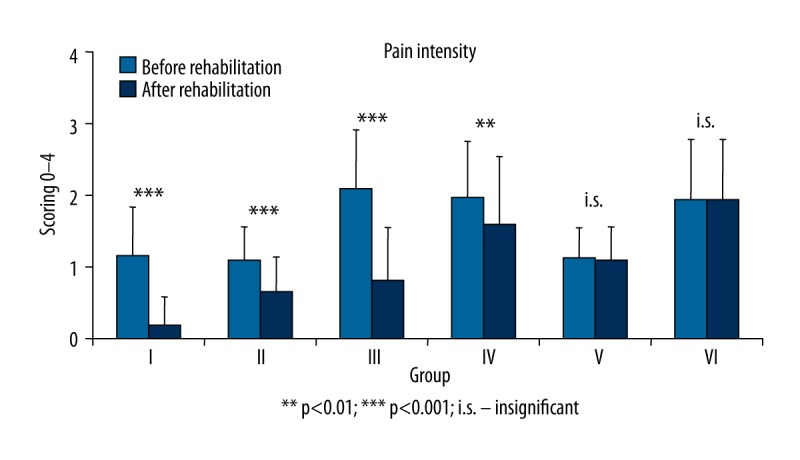
Assessment of pain intensity in the five-degree Laitinen Scale carried out before and after rehabilitation in each evaluated groups.
Figure 3 illustrates the need for medicines (taking into account NASAIDs) declared by the patients before rehabilitation, at the beginning, and at completion of the rehabilitation. This parameter was determined quantitatively using the Modified Laitinen Questionnaire. As with pain intensity, only the control group had no significant changes noted, while especially marked changes were observed in patients who exercised in the pool. Specifically, for each group the following statistics were observed: Group I: Z=−3.839, p<0.001, Group II: Z=−3.606, p<0.001, Group III: Z=−4.434, p<0.001, Group IV: Z=−3.742, p=0.001, Group V: Z=0.000, p=1.000, and Group VI: Z=−1.000, p=0.317 (Figure 3).
Figure 3.
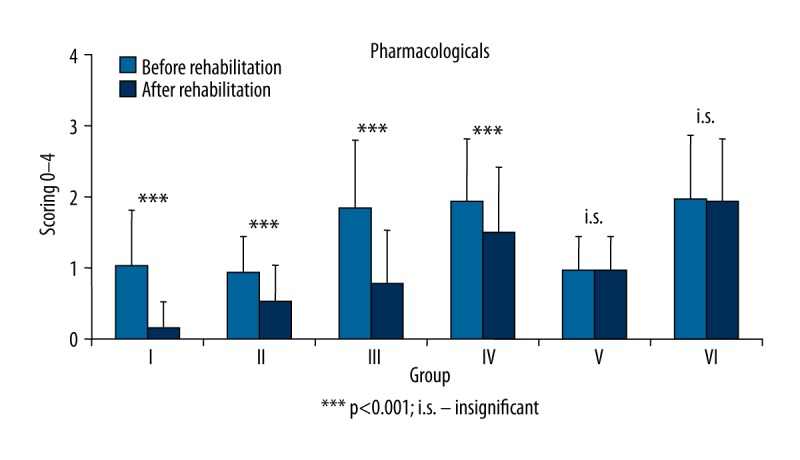
Need to take pharmacological agents before and after treatments in each evaluated group.
The two-factor analysis of variance considering assignment to groups I, II, V (assessment according to kind of prosthesis) and groups III, IV,VI (assessment according to Altman scale (I°, II°, III°); repeated measurements before and after the therapy (BEFORE-AFTER) were taken into account.
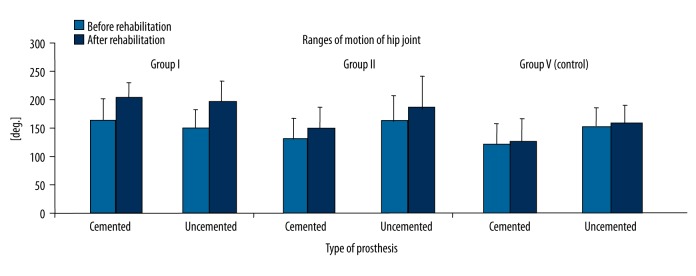
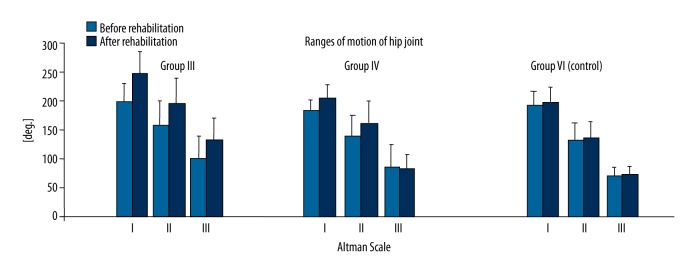
We found that the ranges of motion (ROM) were significantly increased as a result of rehabilitation (F1.87=143.9; p<0.001). The changes depended both on the examined group (F2.87=46.4; p<0.001) and on the degree of degenerative lesions (F2.87=6.80; p<0.01). Determination of the effect of the type of prosthesis on the study outcome showed no positive result (F2.87=0.20; p ins.) (Figure 4).
Figure 4.
The sum of ranges of motion (HAROM) before and after the treatment in groups I, II, and V (after THR) taking into account the kind of prosthesis.
The greatest improvement was noted in the groups that performed exercises in the pool and the smallest improvement was found in the remaining groups, particularly in the subjects with the most advanced degenerative changes (Figure 5).
Figure 5.
The sum of range of movements (HAROM) before and after the treatment in groups III, IV, and VI with OA, according to Altman Scale.
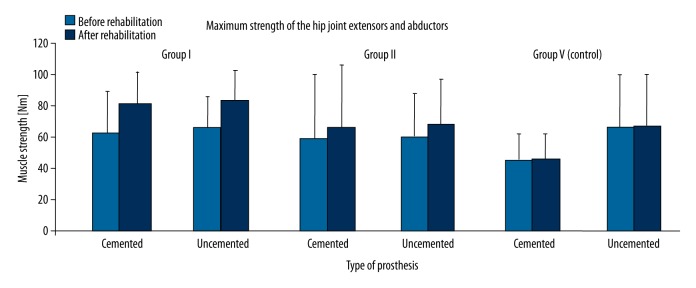
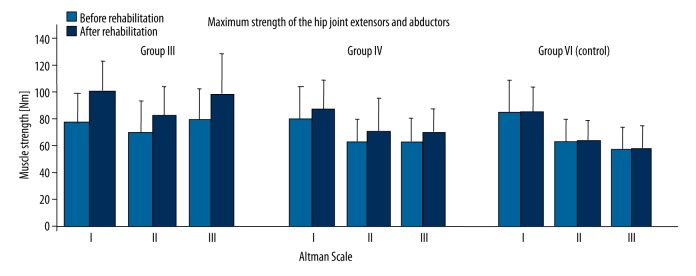
Similar to the former cases, some significant differences were observed in terms of the mean values, both before and after the treatment (F1.87=179.1; p<0.001), in maximum strength of the hip joint. The increase in muscle power depended on the type of rehabilitation treatment conducted (assignment to the particular group) (F2.87=63.5; p<0.001). The most substantial increase in muscle strength was noted in the group of patients with OA and THR, whose rehabilitation was combined exercises in water (Figures 6, 7), but the results showing no effect regarding to the type of prosthesis (F2.87=1.58; p ins.) (Figure 6).
Figure 6.
The sum of strength moments in the hip joint extensor and abductor muscles before and after the treatment in groups I, II, and V (after THR), considering the type of prosthesis.
Figure 7.
The sum of strength moments in the hip joint extensor and abductor muscles before and after the treatment in groups III, IV, and VI with OA, according to Altman Scale.
In the group of patients with OA, it was shown that the increase in muscular strength depended on the degree of degenerative lesions. Higher increases were observed in the group of patients with less pronounced degenerative lesions (Figure 7).
Discussion
The main aim of present study was to assess a rehabilitation program using water exercises in osteoarthritis patients. The results showed that water exercises are effective and worth using in the process of rehabilitation of patients with OA and after THR.
Treatment of degenerative-deforming changes in joints is a serious problem, both medical and economic [2,10]. Most often these are chronic diseases that are accompanied by pain and patients often have to wait for targeted rehabilitation for weeks, which can also affect their mental condition and quality of life [25–28]. Authors present different approaches to treating degenerative-deforming changes in the hip joint [29]. There are some papers on pharmacological treatment of such changes using hyaluronic acid, corticosteroids, or botulinum toxin Type A, and commonly NASAIDs [15,30,31]. There are also interesting papers presenting the results of treatment using different forms of rehabilitation and their therapeutic efficacy [2–4,6–8,32,33]. Additionally, some of them discuss the significance of rehabilitation when preparing the patient for endoprosthesis replacement and during the postoperative period [5,9].
According to prevalent and general opinions of many people related to therapeutic treatment, the positive effect of water exercises on many chronic illnesses is obvious [11,12,18,20,34]. The authors discussing this matter indicate that water supports hastening of the therapeutic effects. The results presented in this paper indicated that the level of pain according to VAS and Laitinen Scale was reduced in all treatment groups. The most substantial reductions were found in patients who exercised in water. Analyzing the increases in the range of motion and maximum strength of hip joints after rehabilitation showed that greatest changes were obtained after water exercises (p<0.001). The kind of prosthesis (cemented/uncemented) did not affect the treatment outcome in patients with THR, but the degree of degeneration of articular cartilage had significant effects in patients with OA. Using the degree of degenerative-deforming lesions assessed according to Altman Scale, we found that more severe degenerative changes were associated with worse treatment outcomes. In the literature there few studies that corroborate the presented results.
Foley et al. found a positive effect of water exercises on degenerative-deforming changes in hip joints. They found that 105 patients who were treated with water exercises obtained better results than the patients who were not treated that way. The group that exercised in the pool showed a statistically significant increase in the forces generated by extensors and abductors, combined with the increased range of motion of the hip joint, as confirmed by our study. No statistically significant changes were noted in terms of the need for pharmacotherapy [19]. Belz et al. reported the effects of exercises in a rehabilitation pool on gait efficiency of the treated patients. The results obtained from 249 patients after a 20-week rehabilitation treatment program in water (2 times a week) clearly indicate that this particular type of kinesitherapy is effective in the treatment of degenerative lesions of the hip joint. The patients who exercised in water obtained significantly better results than the control group [17]. Lin et al. discussed a positive therapeutic effect in 106 patients treated with aquatic exercise kinesitherapy. Based on assessment of pain in the Visual-Analogue Scale and according to assessment of the range of motion, they noticed statistically significant changes in the groups that exercised in water [35]. Siu Am et al. obtained better results in patients who exercised in water, using the same criteria as those in the study of Li Sy et al. [36]. Suomi et al. found, based on results of treatment combined with exercises in water, no benefits from kinesitherapy in that environment [37] and they did not find any statistically significant changes across treated groups in muscle strength and functions of the lower limbs.
Although there is little relevant data in the literature, water exercises seem to be a valuable and effective complement to rehabilitation programs in patients with OA and after THR. More reliable research on this topic should be conducted because of the possibilities of using this environment to treat the patients. Future studies more advanced methods to measure treatment effects of aquatic exercises.
Conclusions
Rehabilitation program including water exercises most significantly influenced the reduction of pain in patients with degenerative-deforming lesions and after total hip replacement surgery.
Inclusion of water exercises in a rehabilitation program can reduce the use of analgesics in patients with OA.
Footnotes
Source of support: Departmental sources
References
- 1.Zhang Y, Jordan JM. Epidemiology of osteoarthritis. Clin Geriatr Med. 2010;3:355–69. doi: 10.1016/j.cger.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kloek CJ, Bossen D, Veenhof C, et al. Effectiveness and cost-effectiveness of a blended exercise intervention for patients with hip and/or knee osteoarthritis: Study protocol of a randomized controlled trial. BMC Musculoskelet Disord. 2014;15:269. doi: 10.1186/1471-2474-15-269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bennell KL, Hinman RS. A review of the clinical evidence for exercise in osteoarthritis of the hip and knee. J Sci Med Sport. 2011;14(1):4–9. doi: 10.1016/j.jsams.2010.08.002. [DOI] [PubMed] [Google Scholar]
- 4.Bennell KL, Egerton T, Pua YH, et al. Efficacy of a multimodal physiotherapy treatment program for hip osteoarthritis: A randomised placebo-controlled trial protocol. BMC Musculoskelet Disord. 2010;11:238. doi: 10.1186/1471-2474-11-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hoogeboom TJ, Dronkers JJ, van den Ende CH, et al. Preoperative therapeutic exercise in frail elderly scheduled for total hip replacement: A randomized pilot trial. Clin Rehabil. 2010;24(10):901–10. doi: 10.1177/0269215510371427. [DOI] [PubMed] [Google Scholar]
- 6.Hoogeboom TJ, Stukstette MJ, de Bie RA, et al. Non-pharmacological care for patients with generalized osteoarthritis: Design of a randomized clinical trial. BMC Musculoskelet Disord. 2010;11:142. doi: 10.1186/1471-2474-11-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Juhakoski R, Tenhonen S, Malmivaara A, et al. A pragmatic randomized controlled study of the effectiveness and cost consequences of exercise therapy in hip osteoarthritis. Clin Rehabil. 2011;25(4):370–83. doi: 10.1177/0269215510388313. [DOI] [PubMed] [Google Scholar]
- 8.McNair PJ, Simmonds MA, Boocock MG, Larmer PJ. Exercise therapy for the management of osteoarthritis of the hip joint: A systematic review. Arthritis Res Ther. 2009;11(3):R98. doi: 10.1186/ar2743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Minns Lowe CJ, Barker KL, Dewey ME, Sackley CM. Effectiveness of physiotherapy exercise following hip arthroplasty for osteoarthritis: A systematic review of clinical trials. BMC Musculoskelet Disord. 2009;10:98. doi: 10.1186/1471-2474-10-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moe RH, Uhlig T, Kjeken I, et al. Multidisciplinary and multifaceted outpatient management of patients with osteoarthritis: Protocol for a randomised, controlled trial. BMC Musculoskelet Disord. 2010;11:253. doi: 10.1186/1471-2474-11-253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Paans N, van den Akker-Scheek I, van der Meer K, et al. 20 Aquatic exercise for the treatment of knee and hip osteoarthritis. BMC Musculoskelet Disord. 2009;10:24. doi: 10.1186/1471-2474-10-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schencking M, Otto A, Deutsch T, Sandholzer H. A comparison of Kneipp hydrotherapy with conventional physiotherapy in the treatment of osteoarthritis of the hip or knee: Protocol of a prospective randomised controlled clinical trial. BMC Musculoskelet Disord. 2009;10:104. doi: 10.1186/1471-2474-10-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Di Monaco M, Castiglioni C. Which type of exercise therapy is effective after hip arthroplasty? A systematic review of randomized controlled trials. Eur J Phys Rehabil Med. 2013;49(6):893–907. [PubMed] [Google Scholar]
- 14.Minns Lowe CJ, Davies L, Sackley CM, Barker KL. Effectiveness of land-based physiotherapy exercise following hospital discharge following hip arthroplasty for osteoarthritis: An updated systematic review. Physiotherapy. 2015;101(3):252–65. doi: 10.1016/j.physio.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 15.Pope JE, McCrea K, Stevens A, Ouimet J. The relationship between NSAID use and osteoarthritis (OA) severity in patients with hip and knee OA: Results of a case control study of NSAID use comparing those requiring hip and knee replacements to those in whom surgery was not recommended. Med Sci Monit. 2008;14(12):604–10. [PubMed] [Google Scholar]
- 16.Ahlqvist J. Hydrotherapy has had and has a rationale. Rheumatology. 2002;41:1070–71. doi: 10.1093/rheumatology/41.9.1070. [DOI] [PubMed] [Google Scholar]
- 17.Belza B, Topolski T, Kinne S, et al. Does adherence make a difference? Results from a community-based aquatic exercise program. Nurs Res. 2002;51(5):285–91. doi: 10.1097/00006199-200209000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Bilberg A, Ahlmen M, Mannerkorpi K. Moderately intensive exercise in a temperature pool for patients with rheumatoid arthritis: A randomized controlled study. Rheumatology. 2005;44(4):502–8. doi: 10.1093/rheumatology/keh528. [DOI] [PubMed] [Google Scholar]
- 19.Foley A, Halbert J, Hewitt T, Crotty M. Does hydrotherapy improve strength and physical function in patients with osteoarthritis – a randomised controlled trial comparing a gym based and a hydrotherapy based strengthening programme. Ann Rheum Dis. 2003;62:1162–67. doi: 10.1136/ard.2002.005272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang TJ, Belza B, Elaine Thompson F, et al. Effects of aquatic exercise on flexibility, strength and aerobic fitness in adults with osteoarthritis of the hip or knee. J AdvNurs. 2007;57(2):141–52. doi: 10.1111/j.1365-2648.2006.04102.x. [DOI] [PubMed] [Google Scholar]
- 21.Gibson AJ, Shields N. Effects of aquatic therapy and land-based therapy versus land-based therapy alone on range of motion, edema and function after hip or knee replacement: A systematic review and meta-analysis. Physiother Can. 2015;67(2):133–41. doi: 10.3138/ptc.2014-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liebs TR, Herzberg W, Rüther W, et al. Multicenter randomized controlled trial comparing early versus late aquatic therapy after total hip or kneearthroplasty. Arch Phys Med Rehabil. 2012;93(2):192–99. doi: 10.1016/j.apmr.2011.09.011. [DOI] [PubMed] [Google Scholar]
- 23.Bartels EM, Lund H, Hagen KB, et al. Aquatic exercise for the treatment of knee and hip osteoarthritis. Cochrane Database Syst Rev. 2007;(4):CD005523. doi: 10.1002/14651858.CD005523.pub2. [DOI] [PubMed] [Google Scholar]
- 24.Altman R, Alarcon G, Appelrouth D, et al. The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum. 1991;34:505–14. doi: 10.1002/art.1780340502. [DOI] [PubMed] [Google Scholar]
- 25.Cabak A, Dąbrowska-Zimakowska A, Tomaszewski P, et al. Selected aspects of mental health of elderly patients with chronic back pain treated in primary care center. Med Sci Monit. 2015;21:3327–33. doi: 10.12659/MSM.894333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cabak A, Dąbrowska-Zimakowska A, Truszczyńska A, et al. Strategies for coping with chronic lower back pain in patients with long physiotherapy wait time. Med Sci Monit. 2015;21:3913–20. doi: 10.12659/MSM.894743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Janikowska-Hołoweńko D, Zaborowska-Sapeta K, Bidzan I. The level of anxiety and the subjective assessment of the quality of life in patients post hip replacement after primary and secondary rehabilitation. Acta Neuropsycholog. 2014;12(2):143–44. [Google Scholar]
- 28.Tomaszewski W, Kotela I, Kawik L, et al. Quality of live of patients in the evaluation of outcomes of short stem hip arthroplasty for hip osteoarthritis. Ortop Traumatol Rehabil. 2013;15(5):439–57. doi: 10.5604/15093492.1084359. [DOI] [PubMed] [Google Scholar]
- 29.Veenhof C, Dekker J, Bijjlssmma JW, Van den Ende CH. Influence of various recruitment strategies on the study population and outcome of a randomized controlled trial involving patients with osteoarthritis of the hip or knee. Arthritis Rheum. 2005;53(3):375–82. doi: 10.1002/art.21171. [DOI] [PubMed] [Google Scholar]
- 30.Colen S, van den Bekerom MP, Bellemans J, Mulier M. Comparison of intra-articular injections of Hyaluronic Acid and Corticosteroid in the treatment of Osteoarthritis of the hip in comparison with intra-articular injections of Bupivacaine. Design of a prospective, randomized, controlled study with blinding of the patients and outcome assessors. BMC Musculoskelet Disord. 2010;11:264. doi: 10.1186/1471-2474-11-264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Marchini C, Acler M, Bolognari MA, et al. Efficacy of botulinum toxin type A treatment of functional impairment of degenerative hip joint: Preliminary results. Rehabil Med. 2010;42(7):691–93. doi: 10.2340/16501977-0546. [DOI] [PubMed] [Google Scholar]
- 32.Rroddy E, Zhang W, Doherty M, et al. Evidence-based recommendations for the role of exercise in the management of osteoarthritis of the hip or knee-the MOVE consssensuss. Rheumatology. 2005;44(1):5–6. doi: 10.1093/rheumatology/keh399. [DOI] [PubMed] [Google Scholar]
- 33.Tak E, Staats P, Van Hespen A, Hopman-Rock M. The effects of an exercise program for older adults with osteoarthritis of the hip. J Rheumatol. 2005;32(6):1106–13. [PubMed] [Google Scholar]
- 34.Weigl M, Angst F, Stucki G, et al. Inpatient rehabilitation for hip or knee osteoarthritis: 2 year follow up study. Ann Rheum Dis. 2004;63:360–68. doi: 10.1136/ard.2003.011601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lin Sy, Davey RC, Cochrane TL. Community rehabilitation for older adults with osteoarthritis of the lower limb: A controlled clinical trial. Clin Rehabil. 2004;18(1):92–101. doi: 10.1191/0269215504cr706oa. [DOI] [PubMed] [Google Scholar]
- 36.Siu A, Chui D. Evaluation of a community rehabilitation services for people with rheumatoid arthritis. Patient Educations. 2004;55(1):62–69. doi: 10.1016/j.pec.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 37.Suomi R, Collier D. Effects of arthritis exercise programs on functional fitness and perceived activates of daily living measures in older adults with arthritis. Arch Phys Med Rehabil. 2003;84(11):1589–94. doi: 10.1053/s0003-9993(03)00278-8. [DOI] [PubMed] [Google Scholar]