Abstract
Alveolar echinococcosis is a chronic and serious, even lethal, parasitic infection caused by the helminth Echinococcus multilocularis. The involvement of Central Nervous System is reported to be 1–3% in literature. Brain involvement is considered a sign of the terminal phase of alveolar echinococcosis. We here in reported a 67-year-old female who had liver alveolar hydatid disease with brain and spinal intradural metastases.
Keywords: Alveolar echinococcosis, cerebral cystic lesions, head-ache, spinal
Öz
Alveolar ekinokokozis ölümcül olabilen kronik ve ciddi bir hastalıktır. Ekinokokus multilokülaris helmiti nedeniyle oluşan parazitik bir enfeksiyondur. Santal sinir sistemi tutulumu literatürde %1–3 olarak raporlanmıştır. Beyin tutulumu alveolar ekinokokozisin terminal fazının bir bulgusu olarak düşünülür. Bu makalede biz beyin ve spinal intradural metastazı olan karaciğer alveolar hidatid hastalığı olan 67 yaşında bir kadın hastayı sunduk.
Introduction
Alveolar echinococcosis is a chronic and serious, even lethal, parasitic infection caused by helminth Echinococcus multilocularis [1]. The disease initially localized in the liver, whereas in the later stages might appear with lung, heart, brain, bone tissue and ligament involvements. We herein reported a 67-year-old female, who had liver alveolar hydatid disease with brain and spinal intradural metastases.
Case Report
A 67-year-old female patient, who was a shepherd, was admitted to the emergency room due to suffering from headache, lower limb weakness and mental confusion. She had a medical history of a liver surgery 3 months prior to arrival. The patient or her family did not have a history of cancer. Patient’s symptoms appeared 1 month after the operation and gradually increased in intensity.
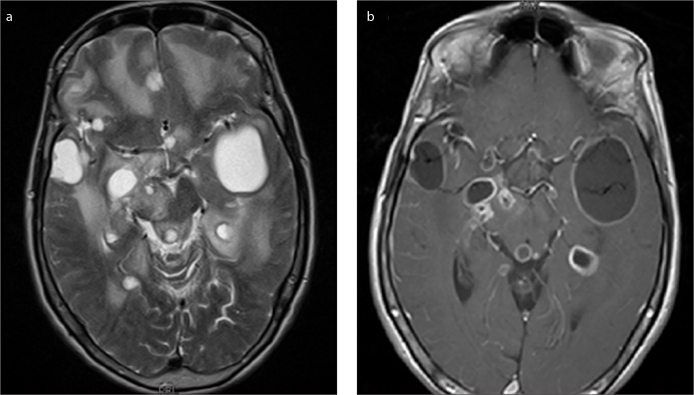
Due to the neurological symptoms of the patient and pre-diagnosis of Guillain Barre Syndrome, a contrast-enhanced cranial and spinal MRI was performed with the approval of the relatives of patients (Siemens MAGNETOM Avanto, Siemens, Erlangen, Germany). In the cranial MRI examination, multiple cystic lesions were observed in the subarachnoid space and subpial area in the supratentorial and infratentorial area, largest size reaching 55x33 mm at the left temporal lobe, showing occasional levelling, hypointense on T1-weighted images, hyperintense on T2-weighted images and intermediate-signal-intensity on FLAIR images. Besides, signal increases due to the oedema around the lesions were observed on T2-weighted images (Figure 1a). On postcontrast images, there were rim-like contrast enhancements on the lesion walls (Figure 1b). However, mural nodule contrasts were also observed on cyst walls in some cystic lesions.
Figure 1. a, b.
T2-weighted image shows multiple cystic lesions with oedema in the subarachnoid space and subpial area (a). Postcontrast T1-weighted image shows rim-like contrast enhancement on the lesion walls, however, mural nodule contrasts are also observed on cyst walls in some cystic lesions (b).
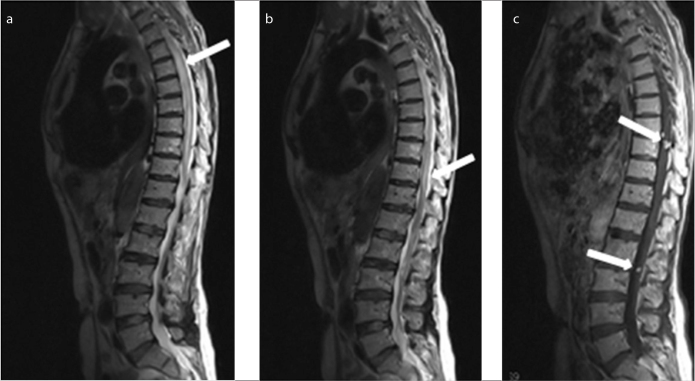
In the contrast-enhanced spinal MRI examination, a slight expansion in the entire spinal cord and all cauda equine fibres with a signal increase in T2-weighted images and occasional nodule contrasts mimicking drop metastases on postcontrast images were observed in the intradural area (Figure 2). Initially, the symptoms were considered to confirm the colloidal vesicular phase of the neurocysticercosis. The results of biochemical studies for neurocysticercosis in blood were negative. The indirect hemaglutination test of the patient for the detection of echinococcosis was positive. When the operation of the patient was scrutinized, it was learned that the pathologic diagnosis was alveolar echinococcosis. The symptoms and findings confirmed the alveolar echinococcosis. The patient began the treatment with albendazole and a surgery was scheduled. However, the patient died of resistant refractory hypernatremia and acute respiratory distress syndrome (ARDS).
Figure 2. a–c.
T2-weighted images show a slight expansion in the entire spinal cord and all cauda equine fibres with a signal increase (arrows) (a, b). On postcontrast images, several nodule contrasts mimicking drop metastases are observed in the intradural area (arrows) (c).
Discussion
Echinococcus multilocularis is considered to be the most potentially lethal parasitic zoonosis in non-tropical areas in the Northern Hemisphere [1]. Eastern Anatolia Region is the highest and largest geographical region in Turkey [2]. The disease caused by echinococcus multilocularis initially localized in the liver, whereas in later stages might appear in lung, heart, brain, bone tissue and ligament involvements. The involvement of Central Nervous System is reported to be 1–3% in the literature [1]. Brain involvement is considered a sign of the terminal phase of alveolar echinococcosis [3]. Clinical symptoms of cerebral involvement in alveolar echinococcosis depend on the extent of central nervous system lesions; increased intracranial pressure, epilepsy, neurologic disturbances (e.g., dysarthria, hemiparesis), skull deformity and cranial nerve palsy have been reported [4]. Cerebral dissemination of primary hepatic lesions is often multifocal [5]. There may be vascular or lymphatic migration of a fertile cell from the hepatic focus. On CT and MR, cerebral alveolar echinococcosis lesion appears as a solid, semisolid or multilocular cystic mass with definite margins. Calcification and surrounding oedema are common. Contrast enhancement occurs within the region of inflammatory reaction around the cysts [6, 7]. Our patient also has had similar cerebral neural parenchymal involvement.
Echinococcosis affecting the spine is rare in rural areas where echinococcosis is endemic [8, 9]. Generally, spinal hydatid disease presents with a radicular symptom of cord compression. In the literature, it is mentioned that spinal cord invasion usually occurs after the local invasion and compression made by the spinal invasion. However, in our case, slight cord expansion with diffuse intramedullary signal increased and intradural extramedullary nodular solid contrasted focuses due to the drop metastasis were present different than the other cases. This situation is a good example for alveolar echinococcosis spread through cerebrospinal fluid (CSF). In the English literature, we did not come across spinal cord invasion of alveolar echinococcosis and drop metastasis like this one.
The differential diagnosis for these lesions include Taenia cestode (for a single large mass in the brain without other organ involvement), cysticercosis (for multiple small cysts in various locations in the brain and muscles, or clustered racemose lesions in the cisternae), paragonimiasis, toxoplasmosis, tuberculosis, bacterial abscess, glioma and cerebral metastasis from malignant neoplasms in other sites [10].
Surgery is the radical solution for the accessible lesions; but the patients are generally admitted at a later stage. Surgical treatment should be considered with chemotherapy instead of only medication in appropriate patients.
Diagnosis of alveolar echinococcus should be considered during the differential diagnosis of the multiple cystic lesions, which were accompanied with oedema around and contrasted in intracranial regions in a patient dealing with animal husbandry or with a medical history of prior hepatic operation. It should be kept in mind that alveolar echinococcosis can spread through CSF and can make diffuse intramedullary T2 SI changes.
Footnotes
Informed Consent: Written informed consent was obtained from the relatives of the patient who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - G.A., A.K.S.; Design - A.K.S.; Supervision - G.S.; Resources - G.A., A.K.S., M.Ç.; Materials - A.K.S., B.S.; Data Collection and/or Processing - A.K.S., B.S.; Analysis and/or Interpretation - A.K.S., G.A.; Literature Search - A.K.S., B.S.; Writing Manuscript - A.K.S.; Critical Review -G.A., A.K.S.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Kern P, Bardonnet K, Renner E, et al. European echinococcosis registry: human alveolar echinococcosis, Europe, 1982–2000. Emerg Infect Dis. 2003;9:343–9. doi: 10.3201/eid0903.020341. http://dx.doi.org/10.3201/eid0903.020341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aydinli B, Aydin U, Yazici P, Oztürk G, Onbaş O, Polat KY. 2008. Alveolar echinococcosis of liver presenting with neurological symptoms due to brain metastases with simultaneous lung metastasis: a case report. Turkiye Parazitol Derg. 2008;32:371–4. [PubMed] [Google Scholar]
- 3.Bresson-Hadni S, Delabrousse E, Blagosklonov O, et al. Imaging aspects and non-surgical interventional treatment in human alveolar echinococcosis. Parasitol Int. 2006;55(Suppl):267–72. doi: 10.1016/j.parint.2005.11.053. http://dx.doi.org/10.1016/j.parint.2005.11.053. [DOI] [PubMed] [Google Scholar]
- 4.Algros MP, Majo F, Bresson-Hadni S, et al. 2003. Intracerebral alveolar echinococcosis. Infection. 2003;31:63–5. doi: 10.1007/s15010-002-2178-y. http://dx.doi.org/10.1007/s15010-002-2178-y. [DOI] [PubMed] [Google Scholar]
- 5.Kantarci M, Bayraktutan U, Karabulut N, et al. Alveolar echinococcosis: spectrum of findings at cross-sectional imaging. Radiographics. 2012;32:2053–70. doi: 10.1148/rg.327125708. http://dx.doi.org/10.1148/rg.327125708. [DOI] [PubMed] [Google Scholar]
- 6.Reittner P, Szolar DH, Schmid M. Systemic manifestation of echinococcus alveolaris infection. J Comput Assisted Tomogr. 1996;20:1030–2. doi: 10.1097/00004728-199611000-00033. http://dx.doi.org/10.1097/00004728-199611000-00033. [DOI] [PubMed] [Google Scholar]
- 7.Bensaid AH, Dietemann JL, de la Palavesa MM, et al. Intracranial alveolar echinococcosis: CT and MRI. Neuroradiology. 1994;36:289–91. doi: 10.1007/BF00593262. http://dx.doi.org/10.1007/BF00593262. [DOI] [PubMed] [Google Scholar]
- 8.Basak M, Ozel A, Yildirim O, Erturk M. 2002. Relapsing hydatid disease involving the vertebral body and paravertebral soft tissues. Acta Radiol. 2002;43:192–3. doi: 10.1080/028418502127347745. http://dx.doi.org/10.1080/028418502127347745. [DOI] [PubMed] [Google Scholar]
- 9.Kadioglu H, Malcok UA, Sengul G, Aydin İH. Alveolar hydatid disease of the spine causing paraplegia. Neurosciences (Riyadh) 2005;10:180–2. [PubMed] [Google Scholar]
- 10.Tappe D, Weise D, Ziegler U, Müller A, Müllges W, Stich A. 2008. Brain and lung metastasis of alveolar echinococcosis in a refugee from a hyperendemic area. J Med Microbiol. 2008;57:1420–3. doi: 10.1099/jmm.0.2008/002816-0. http://dx.doi.org/10.1099/jmm.0.2008/002816-0. [DOI] [PubMed] [Google Scholar]