To the Editor:
Each year, 500,000 babies are born prematurely in the United States (1), and prematurity is now the largest single cause of death around the world in children before age 5 years (2). Premature infants have respiratory instability beyond term characterized by life-threatening episodes of apnea and hypoxemia that increase their morbidity and mortality risk (3, 4). Preterm birth interrupts the development and maturation of the autonomic nervous system (ANS), which regulates normal ventilatory drive and autoresuscitation responses during periods of apnea and hypoxemia (5, 6). Prior studies have confirmed that premature infants have ANS deficits (7), but a comprehensive assessment of the early trajectory of ANS dysfunction in prematurity and subsequent relationship to respiratory outcomes has not been undertaken. Here we present a computational analysis of ANS development in very premature infants, covering almost 2 months of continuous neonatal intensive care unit (NICU) cardiorespiratory monitor data. Our hypothesis was that premature infants requiring rehospitalization resulting from acute episodes of apnea and hypoxemia had distinctive ANS developmental signatures.
Methods
We conducted a retrospective analysis of heart rate variability (HRV), a widely used metric of ANS function (8, 9), in 73 infants born at less than 29 weeks gestational age discharged from our NICU in 2014. We only included subjects in which we could retrieve continuous NICU monitoring signals from 30 to 37 weeks postmenstrual age (PMA) and 4 or more months of outpatient electronic pulmonary or neonatology medical records. We excluded premature infants with any congenital condition associated with significantly increased cardiorespiratory morbidity during early life. To examine respiratory instability, we developed a stringent a priori definition of apparent life-threatening event (ALTE) limited to hospitalization within 3 months of NICU discharge resulting from an acute event of apnea with documented cyanosis or acute oxygen saturation as measured by pulse oximetry desaturation. Other respiratory hospitalizations (e.g., wheezing) or nonrespiratory concerns (e.g., lethargy) were not included. Comparison of HRV metrics between premature infants classified as ALTE cases versus controls without ALTE was conducted using NICU cardiorespiratory monitoring data and computational MATLAB processing (Mathworks, Natick, MA) (8). We calculated traditional HRV frequency and time-domain metrics including normalized low-frequency power and normalized high-frequency power (8). We also used detrended fluctuation analysis (9, 10), a nonlinear method in which the data trends (nonstationarities) are systematically eliminated to take into account the nonstationary nature of HRV time series (8–10). Detrended fluctuation analysis metrics included the variability at short (root mean square [RMS] short time scale, 15–50 beats) and long (RMS long time scale, 100–150 beats) time scales and the autocorrelations in the heart rate at short (detrended fluctuation analysis short α exponent [α-S], 15–30 beats) and long (detrended fluctuation analysis long α exponent [α-L], 35–150 beats) time scales (9). At the start of each postmenstrual week, each subject was assigned an HRV value (median of 10-min windows over the course of 24 h), and then weekly values were plotted. HR artifacts were detected using local maximum/immediate minimum thresholds and replaced with the median of the prior 10 values. Differences between groups were analyzed using χ2 test for proportions or unpaired t or Mann-Whitney U tests for continuous data (significance, P < 0.05).
Results
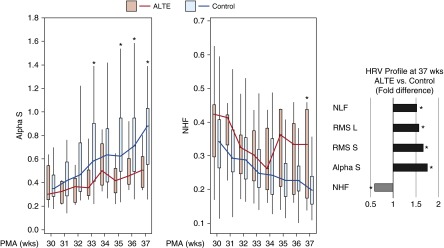
Baseline characteristics were comparable in subjects with ALTE (n = 7) versus in the control group without ALTE (n = 66) (Table 1). Bronchopulmonary dysplasia severity was similar in both study groups. All ALTE cases occurred within two months of NICU discharge, and none had a clear etiology determined beyond the association with prematurity. Our longitudinal high-resolution HRV analysis showed distinct developmental trajectories in premature infants who had ALTE after NICU discharge (Figure 1). With the exception of α-L, which had identical trajectory in both groups (data not shown), all the HRV markers of sympathetic tone (α-S, RMS-short, RMS-long, and normalized low-frequency power) were lower at each time point in the ALTE group, particularly after 34 weeks PMA. The lack of differences in α-L indicated similar autocorrelations at long time scales (35–150 beats) in both groups. At short time scales (15–30 beats), α-S was overall the best HRV parameter differentiating both trajectories; however, at 37 weeks PMA, all the sympathetic markers were more than 1.5-fold higher in control premature infants relative to the ALTE group. In contrast, normalized high-frequency power (marker of parasympathetic tone) had an increasing trend in the ALTE group becoming 1.4-fold higher at 37 weeks PMA relative to the control group (Figure 1).
Table 1.
Demographic Data and Baseline Characteristics of All Premature Infants
| Group | Control | ALTE | P Value | |
|---|---|---|---|---|
| N | 66 | 7 | ||
| Gestational age, wk, mean (SD) | 25.7 (1.8) | 25.9 (1.7) | 0.81 | |
| PMA at discharge, wk, mean (SD) | 40.6 (3.1) | 39.8 (3.4) | 0.58 | |
| Male, n (%) | 38 (57) | 4 (57) | 0.98 | |
| Birth weight, g, mean (SD) | 829 (257) | 767 (165) | 0.40 | |
| SGA, n (%) | 10 (15) | 1 (14) | 0.95 | |
| IUGR, n (%) | 9 (13) | 1 (13) | 0.96 | |
| Multiple births, n (%) | 16 (24) | 3 (42) | 0.34 | |
| Antenatal steroids, n (%) | 42 (66) | 6 (86) | 0.13 | |
| Systemic steroids in NICU, n (%) | 36 (55) | 4 (57) | 0.90 | |
| Surfactant, n (%) | 50 (76) | 6 (86) | 0.49 | |
| Caffeine therapy duration, wk, mean (SD) | 9.6 (3.4) | 9.5 (2.0) | 0.95 | |
| BPD severity | ||||
| Mild BPD, n (%) | 18 (27) | 1 (14) | 0.37 | |
| Moderate/severe BPD, n (%) | 44 (67) | 6 (86) | 0.63 | |
| PMA at ALTE hospitalization, wk, mean (range) | 42.8 (38–48) |
Definition of abbreviations: ALTE = apparent life-threatening event; BPD = bronchopulmonary dysplasia; IUGR = intrauterine growth restriction; NICU = neonatal intensive care unit; PMA = postmenstrual age; SGA = small for gestational age.
Control infants without an ALTE are compared to infants admitted after an ALTE at home. There are no group differences.
Figure 1.
Developmental trajectories of heart rate variability (HRV) in very premature infants. Data represent longitudinal HRV continuous measurements in premature infants born at less than 29 weeks gestational age (n = 73). HRV metrics included α-S (detrended fluctuation analysis short α exponent), normalized high frequency (NHF), normalized low frequency (NLF), and root mean square short and long time scales (RMS-S and RMS-L). In the box-and-whisker plots, the horizontal lines inside the boxes represent medians; the top and bottom of the boxes represent 75th and 25th percentiles, respectively; and the ends of the top and bottom whiskers represent maximum and minimum values, respectively. HRV fold differences are presented as ALTE/control ratios. *P < 0.05. ALTE = apparent life-threatening event; PMA = postmenstrual age.
Discussion
This is the first study to demonstrate that premature infants requiring rehospitalization for ALTE within 3 months of discharge had distinctive ANS developmental signatures during their NICU staying. Near discharge (37 weeks PMA), premature infants with ALTE episodes had reduced sympathetic tone and increased parasympathetic tone. This distinctive HRV profile is expected to increase the risk for cardiorespiratory collapse for two reasons. First, sympatho-adrenal activation is crucial for “autoresuscitation responses,” including centralization of blood flow to vital organs (heart and brain) and arousal from sleep (5, 6). These survival responses are triggered by life-threatening stressors such as hypoxemia and apnea (5, 6). Second, enhanced parasympathetic tone is expected to have the opposite effect, promoting “resting responses” during vagal stimulation (e.g., apnea/bradycardia during feeding). Collectively, our findings suggest that some premature infants have higher risk for ALTE episodes because of blunted sympathetic autoresuscitation and intrinsic vagal hypersensitivity.
Premature infants undergo major phases of their ANS maturation in an ex utero environment that is vastly different from the normal intrauterine milieu, with deprivation of maternoplacental support and exposure to iatrogenic toxicity. Using developmental ANS trajectories, we documented that premature infants requiring rehospitalization because of ALTE had a progressive reduction in HRV between 30 and 37 weeks PMA, a developmental window that coincides with a critical period of ANS maturation (5–7). There thus appears to be a critical window of opportunity to identify and prevent prematurity-related ANS dysfunction, which might lead to a significant reduction in subsequent ALTE risk. Given our small sample size, retrospective design, and lack of simultaneous respiratory signal monitoring, we could not examine the potentially modifiable prenatal and postnatal factors that contribute to the origin and persistence of autonomic respiratory instability in premature infants. Large longitudinal studies including cardiorespiratory monitoring data from NICU and subsequent hospitalizations would have high effect, enhancing our knowledge of the mechanisms contributing to respiratory instability in prematurity and providing novel diagnostic and treatment strategies to improve outcomes for this vulnerable population.
Supplementary Material
Footnotes
Work partially supported by NHLBI grant HL090020 (K12 Genomics of Lung), Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) grant HD001399 (K12 Child Health Research Career Development Award), National Center for Advancing Translational Sciences grant UL1TR000075, and NICHD Intellectual and Developmental Disabilities Research Center grant P30HD040677.
Author Contributions: Conception and design: G.N., R.B.G., C.E.H., and A.J.d.P.; data collection, analysis, and interpretation: G.N., R.B.G., T.A.-S, M.M., A.N.M., G.F.P., R.M., C.E.H., and A.J.d.-P.; drafting the manuscript for important intellectual content: G.N., R.B.G., and A.J.d.-P.
Author disclosures are available with the text of this letter at www.atsjournals.org.
References
- 1.Centers for Disease Control and PreventionAtlanta, GA: Centers for Disease Control and Prevention; 2012 [updated 2015 Dec 4; accessed 2015 Oct 10]. Available from: http://www.cdc.gov/reproductivehealth/MaternalInfantHealth/PretermBirth.htm
- 2.Liu L, Oza S, Hogan D, Perin J, Rudan I, Lawn JE, Cousens S, Mathers C, Black RE. Global, regional, and national causes of child mortality in 2000-13, with projections to inform post-2015 priorities: an updated systematic analysis. Lancet. 2015;385:430–440. doi: 10.1016/S0140-6736(14)61698-6. [DOI] [PubMed] [Google Scholar]
- 3.Eichenwald EC Committee on Fetus and Newborn. Apnea of Prematurity. Pediatrics. 2016;137:1–7. doi: 10.1542/peds.2015-3757. [DOI] [PubMed] [Google Scholar]
- 4.Eichenwald EC, Aina A, Stark AR. Apnea frequently persists beyond term gestation in infants delivered at 24 to 28 weeks. Pediatrics. 1997;100:354–359. doi: 10.1542/peds.100.3.354. [DOI] [PubMed] [Google Scholar]
- 5.Gershan WM, Jacobi MS, Thach BT. Maturation of cardiorespiratory interactions in spontaneous recovery from hypoxic apnea (autoresuscitation) Pediatr Res. 1990;28:87–93. doi: 10.1203/00006450-199008000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Fewell JE. Protective responses of the newborn to hypoxia. Respir Physiol Neurobiol. 2005;149:243–255. doi: 10.1016/j.resp.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 7.Yiallourou SR, Witcombe NB, Sands SA, Walker AM, Horne RS. The development of autonomic cardiovascular control is altered by preterm birth. Early Hum Dev. 2013;89:145–152. doi: 10.1016/j.earlhumdev.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 8.Govindan RB, Massaro AN, Niforatos N, du Plessis A. Mitigating the effect of non-stationarity in spectral analysis-an application to neonate heart rate analysis. Comput Biol Med. 2013;43:2001–2006. doi: 10.1016/j.compbiomed.2013.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Govindan RB, Massaro AN, Al-Shargabi T, Andescavage NN, Chang T, Glass P, du Plessis A. Detrended fluctuation analysis of non-stationary cardiac beat-to-beat interval of sick infants. Europhys Lett. 2014;108:40005. [Google Scholar]
- 10.Chiang JY, Huang JW, Lin LY, Chang CH, Chu FY, Lin YH, Wu CK, Lee JK, Hwang JJ, Lin JL, et al. Detrended fluctuation analysis of heart rate dynamics is an important prognostic factor in patients with end-stage renal disease receiving peritoneal dialysis. PLoS One. 2016;11:e0147282. doi: 10.1371/journal.pone.0147282. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.