Abstract
Biomarkers have become an essential component of Alzheimer disease (AD) research and because of the pervasiveness of AD pathology in the elderly, the same biomarkers are used in cognitive aging research. A number of current issues suggest that an unbiased descriptive classification scheme for these biomarkers would be useful. We propose the “A/T/N” system in which 7 major AD biomarkers are divided into 3 binary categories based on the nature of the pathophysiology that each measures. “A” refers to the value of a β-amyloid biomarker (amyloid PET or CSF Aβ42); “T,” the value of a tau biomarker (CSF phospho tau, or tau PET); and “N,” biomarkers of neurodegeneration or neuronal injury ([18F]-fluorodeoxyglucose–PET, structural MRI, or CSF total tau). Each biomarker category is rated as positive or negative. An individual score might appear as A+/T+/N−, or A+/T−/N−, etc. The A/T/N system includes the new modality tau PET. It is agnostic to the temporal ordering of mechanisms underlying AD pathogenesis. It includes all individuals in any population regardless of the mix of biomarker findings and therefore is suited to population studies of cognitive aging. It does not specify disease labels and thus is not a diagnostic classification system. It is a descriptive system for categorizing multidomain biomarker findings at the individual person level in a format that is easy to understand and use. Given the present lack of consensus among AD specialists on terminology across the clinically normal to dementia spectrum, a biomarker classification scheme will have broadest acceptance if it is independent from any one clinically defined diagnostic scheme.
By providing measures of relevant pathophysiology in living persons, biomarkers have become increasingly important to understanding the biology of Alzheimer disease (AD). Biomarkers are also used in all modern research diagnostic criteria across the AD clinical spectrum,1–6 in therapeutic trials, and by regulatory agencies.7 Because AD pathology is so frequent in the elderly, AD biomarkers are also commonly used in cognitive aging research. However, several current issues suggest that a different approach to biomarkers used in AD research might be useful.
First, available evidence points to recently developed tau PET tracers as useful measures of neurofibrillary tangles in AD, while utility in non-AD tauopathies has not yet been clarified.8,9 Elevated tau PET tracer signal, particularly in neocortical regions, is highly associated with the presence of positive amyloid PET scans as would be expected in a ligand that binds to the tau deposits in AD.10,11 Tau PET ligand binding correlates well with clinical impairment in individuals who lie along the AD clinical spectrum.10,11 When easily characterized off-target and nonspecific binding is accounted for, the topographic patterns of ligand uptake match quite well what is expected from Braak staging of neurofibrillary tangles.12 However, because of its recent introduction, tau PET is not yet integrated into any current AD diagnostic schemes.
Second, many details of AD pathogenesis remain uncertain.13,14 One of the most contentious issues, and one of the oldest, is which proteinopathy “causes” the disease in the elderly. Some propose that AD pathogenesis follows a specific cause and effect order of events, where β-amyloidosis potentiates the spread of tauopathy, tauopathy is associated with neurodegeneration, which is the immediate cause of clinical symptoms.15 Others argue for different, less β-amyloid (Aβ) centric pathways to clinically symptomatic AD.13,14,16 Interdependent pathways have also been proposed.17 A biomarker classification system will have the broadest use if it makes no assumptions about temporal ordering of biomarkers or their putative causal relationships.
Third, current biomarker classification systems are linked to disease or syndromic labels and are based on consensus diagnostic criteria rather than certainty of disease pathogenesis. The 2 major such diagnostic schema are those of the International Working Group (IWG),1,18 which first proposed the use of a common biomarker algorithm for all clinical stages of the disease, and the National Institute on Aging–Alzheimer's Association (NIA-AA).3–6 Although there are areas of agreement, important disagreements exist concerning staging, nomenclature, and interpretations of biomarker findings. We recognize that associating biomarkers with clinical findings is important. However, given the confusion that has arisen over the use of competing definitions of clinical impairment in the AD spectrum,19 a biomarker classification scheme will have broadest acceptance if it is independent from any one clinically operationalized diagnostic scheme. The biomarker classification scheme we propose is applicable across all clinical diagnostic states, and is thus independent of cognitive status.
Fourth, the prevalence of AD, non-AD, and mixed brain pathologies increases with age in both individuals who are clinically impaired and those nonimpaired.20 To be an effective tool in cognitive aging research, a biomarker classification system must include all possible biomarker profiles and all individuals in the population. For example, classification schemes that require Aβ positivity do not classify individuals who are Aβ negative but positive on tau or neurodegenerative biomarkers, yet the latter biomarker profile is common.21
The objective of this report is to propose an unbiased descriptive classification scheme for biomarkers commonly used in AD research that addresses each of these 4 issues.
AD BIOMARKERS
We propose that the major biomarkers used in AD research can be divided into 3 binary categories based on the nature of the underlying pathophysiology each measures. Biomarkers of fibrillary Aβ deposition are high ligand retention on amyloid PET22 or low CSF Aβ42.23–25 Biomarkers of tau pathology (neurofibrillary tangles) are elevated CSF phosphorylated tau (p-tau) and tau PET.24,26 Biomarkers of AD-like neurodegeneration or neuronal injury are CSF total tau (t-tau), [18F]-fluorodeoxyglucose (FDG)-PET hypometabolism, and atrophy on structural MRI in regions characteristic of AD.27
CSF biomarkers report a single absolute value reflecting degree of abnormality but that does not indicate topographic extent of pathology. In contrast, imaging biomarkers contain information about both the severity and topographic extent of the abnormality. Typical AD (i.e., amnestic multidomain dementia) is associated with a characteristic topographic pattern of FDG-PET hypometabolism that appears earliest and most severely in the medial parietal and lateral temporal-parietal isocortex (figure 1A).28 Typical AD likewise is associated with a pattern of atrophy on MRI that appears earliest and most severely in the medial temporal allocortex and the basal-lateral temporal isocortex (figure 1C).15 Aβ deposition on PET does not seem to follow a sequential topographic progression through the isocortex (figure 1E). Available evidence indicates that in the typical AD spectrum, tau PET captures the topography of tau spread as described at autopsy by Braak12—medial temporal to basal and lateral temporal, then to other isocortical areas (figure 2).
Figure 1. Images of clinically normal individuals and participants with AD.
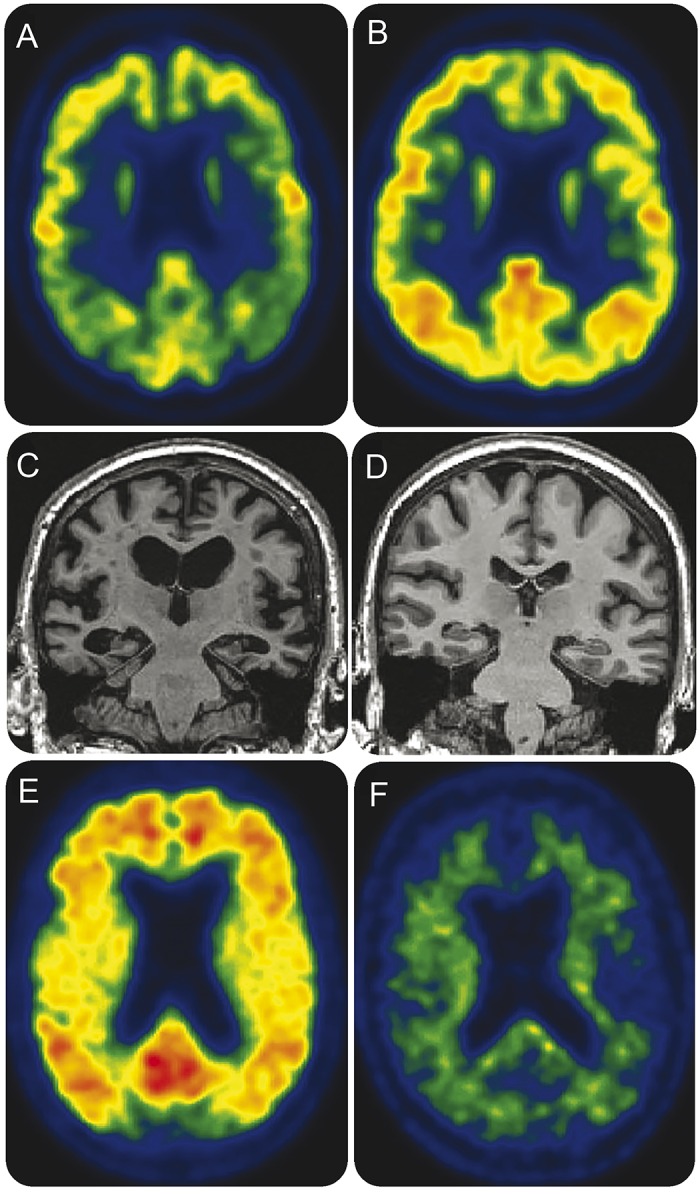
Individuals with AD dementia are clinically diagnosed participants in Mayo Alzheimer's Disease Research Center study while clinically normal individuals are participants in the Mayo Clinic Study of Aging. (A) FDG-PET of 75-year-old man with AD dementia. Hypometabolism in medial parietal and lateral temporal-parietal isocortex with relative preservation of frontal metabolism, which is characteristic of typical (multidomain amnestic) AD. (B) FDG-PET of clinically normal 71-year-old man. Uniform FDG uptake is present throughout the isocortex. (C) MRI of 71-year-old man with AD dementia. Atrophy is present in the medial temporal allocortex and the basal-lateral temporal isocortex, which is characteristic of typical (multidomain amnestic) AD. (D) MRI of clinically normal 71-year-old woman without atrophy. (E) Amyloid PET with Pittsburgh compound B of 71-year-old woman with AD dementia. Ligand uptake is seen throughout the isocortex. (F) Amyloid PET of clinically normal 93-year-old man showing no ligand uptake in the isocortex. AD = Alzheimer disease; FDG = [18F]-fluorodeoxyglucose.
Figure 2. Tau and amyloid PET imaging in AD.
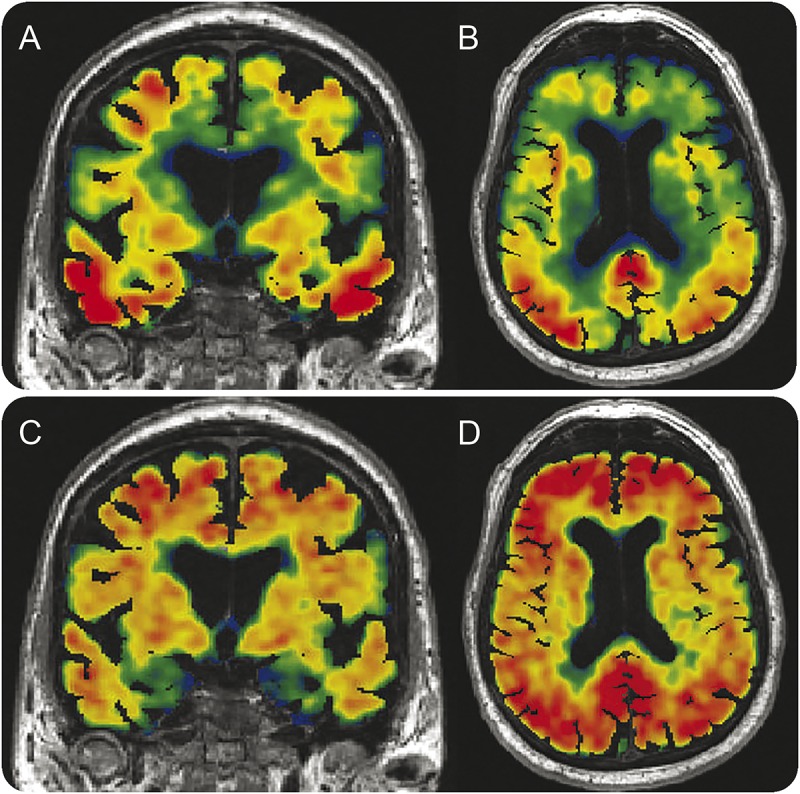
A 79-year-old man with a clinical diagnosis of AD dementia. He is a participant in the Mayo Alzheimer's Disease Research Center study. (A, B) Coronal and axial tau PET images (AV1451) superimposed on MRI. (C, D) Coronal and axial Pittsburgh compound B PET images superimposed on MRI. The tau PET images (top) illustrate extensive tracer uptake in basal lateral temporal, parietal, and frontal isocortex with sparing of sensory motor and primary visual cortices. Off-target binding is seen in the basal ganglia, which is characteristic of this tracer. Although areas of spatial overlap between the tau and amyloid tracers are present, abundant amyloid tracer uptake is seen in the frontal lobes, but not with the tau tracer. Conversely, abundant uptake is seen in the medial temporal lobes with the tau ligand but not with the amyloid ligand. AD = Alzheimer disease.
While each of the 7 commonly used core biomarkers is associated with AD, they are not equally specific. Biomarkers of β-amyloidosis are specific for AD pathology.29–31 However, amyloid PET tracers do bind to Aβ deposits in vessel walls, and increased tracer binding can be found following acute traumatic brain injury.32 CSF Aβ42 is decreased (i.e., abnormal) in some non-AD conditions such as HIV encephalitis33 and multiple system atrophy.34
Typical AD shows an increase in both t-tau and p-tau and a tight correlation between these biomarkers.35 Neither CSF t-tau nor p-tau shows any change in primary tauopathies such as frontotemporal dementia, progressive supranuclear palsy, or corticobasal degeneration.36,37 However, findings on CSF t-tau and p-tau diverge in conditions with acute brain damage. There is a marked temporary increase in t-tau with normal p-tau levels in traumatic brain injury and stroke that correlates with the severity of neuronal damage.38,39 It is the same for Creutzfeldt-Jakob disease, which shows a large increase in t-tau (reflecting rapid neurodegeneration) but normal p-tau since there are no neurofibrillary tangles in this condition.40,41 The CSF level of p-tau correlates with severity of tau pathology postmortem,30 and high p-tau has not been found in disorders other than AD. Taken together, these data indicate that CSF t-tau reflects the intensity of neuronal degeneration in AD at a specific point, while p-tau seems more specific for the burden of AD-type tau pathology accumulated over time.42 Tau PET is being actively investigated, but initial data indicate that tau PET ligands have high binding affinity for paired helical filament tau in AD but have much weaker affinity in non-AD tauopathies, especially those with straight filament tangles.9
Atrophy and hypometabolism involving AD-like regions occur in a variety of disorders and are the least specific for AD.43 Atrophy in the anterior/medial/basal temporal lobes occurs in a wide variety of pathologic conditions including AD but also cerebrovascular disease, epilepsy, anoxia, hippocampal sclerosis, TDP-43-opathy, primary age-related tauopathy,44 chronic traumatic encephalopathy, argyrophilic grain disease, and non-AD primary tauopathies such as progressive supranuclear palsy and Pick disease.43 Temporoparietal hypometabolism can be found in non-AD conditions, such as corticobasal degeneration, primary progressive aphasia,45 and cerebrovascular disease.46 This nonspecificity is the explanation for the frequent and consistently observed finding of abnormal FDG-PET and structural MRI (and CSF t-tau) in non-AD conditions—a state that has been labeled suspected non-Alzheimer pathophysiology (SNAP).21
Interpreting biomarker data is confounded by the common coexistence of AD pathology, and therefore positive AD biomarkers, with other age-related pathologies. Multidomain amnestic dementia and mild cognitive impairment (MCI) are most commonly associated with multiple pathology,20 especially with advancing age.
THE A/T/N CLASSIFICATION SYSTEM
In the proposed A/T/N classification system, the 7 major AD biomarkers are divided into 3 binary classes. “A” refers to the value of an Aβ biomarker (amyloid PET or CSF Aβ42); “T,” the value of a tau pathology biomarker (CSF p-tau or tau PET); and “N,” a quantitative or topographic biomarker of neurodegeneration or neuronal injury (CSF t-tau, FDG-PET, or structural MRI).
The A/T/N classification system is related to the biomarker classification proposed in recent consensus diagnostic criteria. In both IWG and NIA-AA diagnostic criteria, A refers to Aβ (PET or CSF Aβ). Segregation of MRI and FDG-PET from CSF tau biomarkers was proposed by the IWG (2014),1while in the NIA-AA criteria, MRI, FDG-PET, and CSF tau proteins were grouped together as biomarkers of neurodegeneration or neuronal injury. The rationale for grouping CSF tau, FDG-PET, and MRI atrophy into a single category in the NIA-AA criteria had strong support from numerous observations that the 3 behaved in a similar manner relative to clinical symptoms. More abnormal values in all 3 of these biomarkers are strongly associated with worse cognitive symptoms throughout the clinical spectrum, which is not the case for amyloid biomarkers.15 The topography of hypometabolism and atrophy maps well onto the expression of clinical symptoms, which is not the case for amyloid PET.47
We recognize that having both T and N categories adds complexity in comparison to simply grouping tau PET, FDG-PET, MRI atrophy, CSF t-tau, and p-tau into a single catch-all N category. However, the simpler approach would fail to take advantage of information that is available. Some (perhaps quite a bit) of the neuronal injury/neurodegeneration present in elderly individuals is related to non-AD etiologies. Separating biomarkers of neurofibrillary tangles (tau PET and CSF p-tau) from markers of neuronal injury/neurodegeneration might differentiate neuronal injury/neurodegeneration that is attributable to AD from non-AD causes.
In the A/T/N system, each biomarker is rated as positive or negative. An individual score might appear as A+/T+/N−, or A+/T−/N−, etc. In the event that a biomarker class was unavailable, it would be denoted “u.” Conflicting results within a category would be labeled “c.” For example, if an individual had conflicting results from amyloid PET and CSF Aβ, he or she might be labeled Ac. While we regard atrophy, hypometabolism, and total tau each as exemplars of neuronal injury/neurodegeneration, we do not believe these 3 measures should be equated. Analyses show that neurodegeneration biomarkers are only modestly correlated with one another.48 Therefore, if possible, within a given research study, the N category should be described by only one N marker, not either/or mixtures of the 3. Individuals can be fully classified by CSF alone, imaging alone, or combinations.
POSITIVE/NEGATIVE OR NORMAL/ABNORMAL BIOMARKER CUTPOINTS
Although every biomarker exists on a continuous scale, normal vs abnormal cutpoints exist in most disease categories to make diagnostic categorization of individuals practical and inform clinical decision-making. We recognize that cutpoints can be arbitrary, and many individuals will have biomarker values close to cutpoints. This is true for any disease and is not unique to biomarkers used in AD research. The presence of positive/negative cutpoints is not inherently problematic provided that values close to cutpoints are interpreted and used properly.
Amyloid biomarkers have been bimodally distributed in some research samples where participants are highly selected,49 while neurodegenerative biomarkers typically are not. This has led to the suggestion that cutpoints are not valid for neurodegenerative biomarkers. However, most physiologic measures are continuously, not bimodally, distributed—blood pressure, for example.50 This has not prevented medicine from identifying a cutpoint and designating those above hypertensive and those below normotensive. It seems illogical to treat AD differently from other diseases.
We emphasize that binary, +/− categorization does not imply that individuals who fall below the cutpoint for a particular biomarker have no pathology in the brain. For example, an individual designated as A may well have amyloid plaques in the brain, but not at a sufficient level to cross the in vivo detection threshold of amyloid PET. Current biomarker readouts are not sensitive to low but perhaps biologically important levels of early pathology.51,52 The +/− designation is a convenient shorthand to facilitate communication, ease of use, and understanding.
Several different approaches to selecting normal/abnormal cutpoints in the continuous range of biomarker values exist. These include selecting values that best separate clinically normal individuals from those with dementia, values that have predictive power for future clinical decline,53 or using autopsied individuals with antemortem biomarker studies to guide selection of cutpoints.51,52 In laboratory medicine, the 95th percentile based on a healthy control population is commonly used.54 A popular approach has been to select cutpoints based on the (most normal) 10th percentile of values seen in typical AD dementia.21,55 Validating specific cutpoints will be an ongoing exercise for research groups working in each separate modality.
Experience labeling tau PET scans positive vs negative is limited at this point. Tauopathy confined to the medial temporal lobes with minimal or no neocortical β-amyloidosis is very common at autopsy and whether this should be regarded as AD or simply an aging phenomenon is controversial.12,13,44 One possible approach to categorizing tau PET is to label scans that have tracer uptake exceeding an analytically determined threshold in AD-like isocortical areas as “AD positive” (figure 2). Where tau is located and its topographic progression over time will be important. But for purposes of labeling a scan abnormal, we provisionally propose that a scan with tracer uptake confined to the medial temporal lobes would not be considered positive44 but a scan with uptake in AD-like isocortical areas would.10
ALTERNATIVES TO POSITIVE/NEGATIVE SCORING OF BIOMARKERS
Advantages of binary, +/− categorization of each biomarker class include economy, conceptual clarity, and ease of use. Thus, we recommend binary, +/− categorization. Alternatives exist however and are briefly discussed for completeness. One alternative is to score the severity of each biomarker on a continuous or semicontinuous scale. An example of this, termed the centiloid scale,56 has been proposed for amyloid PET. The process requires empirically establishing reference values for the abnormal part of the distribution using individuals with AD dementia and for the normal part of the distribution using young, clinically normal individuals. Biomarker values are then scaled linearly from 0 (normal) to 100 (abnormal). The centiloid scale is related to but not identical to percentiles because centiloid values below 0 (i.e., below the mean for the normal group) and above 100 (i.e., above the mean for the abnormal group) are possible. An example of how this might appear is A80/T50/N20, where this individual ranks at the 80th centiloid for amyloid, 50th for tau, and 20th for neurodegeneration. This approach would require a 0 to 100 scale that was standardized across all biomarkers.
A second alternative to binary, +/− biomarker scoring is topographic staging. This approach would only be applicable to imaging and might best apply to tau PET. Topographic tau PET staging would mirror pathologic Braak neurofibrillary tangle stage whereby individuals would be assigned to 1 of 3 stages based on anatomical locations of tracer uptake—i.e., stage 0, limbic stage, isocortical stage. Since cortical atrophy on MRI closely mirrors Braak stage and tau density in imaging–autopsy correlation studies,57 and the topographic spread of atrophy within individuals over time also mirrors progressive Braak stages, this Braak-like topographic staging approach might be valid for MRI as well.
Generalizability of AD biomarker categorization is dependent on standardization and reproducibility of the measures.58
ATYPICAL AD, CEREBROVASCULAR DISEASE, AND EXPANSION OF THE CORE A/T/N SYSTEM
The descriptions of FDG-PET, tau PET, and MRI topography outlined above reflect patterns of typical multidomain amnestic AD (figures 1 and 2). Because MRI, FDG, and tau PET topographic patterns map onto clinical phenotype, a different set of imaging signatures is needed to describe atypical variants of AD. Although not detailed in the present report, the A/T/N system is equally applicable to atypical AD variants by modifying the topographic search pattern. For example, pattern recognition algorithms could easily be modified to recognize atrophy, hypometabolism, and tau PET deposition in the frontal, dominant temporal lobe, or posterior cortical regions for atypical AD.
Our primary focus is the core A/T/N system, which addresses biomarkers of AD; however, biomarkers of other proteinopathies could be added if/when they become available. The category of synaptic dysfunction (S) may be a useful future addition and this might include FDG-PET, task-free functional MRI, EEG, MEG (magnetoencephalography), as well as synapse-specific proteins in CSF.59 However, if neurodegeneration is defined as progressive loss and shrinkage of neurons and processes with a corresponding impairment in neuronal function,15 then synaptic dysfunction is subsumed within the category of neurodegeneration.
The core A/T/N system could also be supplemented by adding a cerebrovascular disease category. A limitation is the absence of an agreed on pathologic summary scoring system for cerebrovascular disease on which to base an imaging counterpart. Nonetheless, systems in which the MRI findings of ischemic cerebrovascular disease are combined to form a vascular (V) summary score have been described.60 The A/T/N system would then be extended to A/T/N/V by compressing the vascular index into V+ or V−.
APPLICATION OF THE A/T/N SYSTEM IN COGNITIVE AGING AND DEMENTIA RESEARCH: A/T/N/C
The A/T/N system provides a common framework by which investigators can describe and communicate multidomain biomarker profiles at the individual person level. Application in cognitive aging and dementia research, however, will require the inclusion of clinical information about each individual. Clinical status (C) could be denoted in several possible ways resulting in A/T/N/C notation. Setting aside detailed syndromic descriptions, cognitive function can be thought of categorically or as a continuum. The cognitive/functional continuum could be divided into normal for age (n), mildly impaired (m), or demented (d), resulting in designations of A/T/N/Cn, A/T/N/Cm, or A/T/N/Cd. The cognitive continuum could also be expressed as a continuous variable on a 0 (normal) to 100 (abnormal) scale; individuals are assigned values along this 0 to 100 scale.
HOW DOES THE A/T/N SYSTEM RELATE TO EXISTING AD CLINICAL CLASSIFICATION SYSTEMS?
The IWG and NIA-AA criteria both integrate 5 biomarkers into the diagnostic classification process: CSF Aβ42 and tau proteins, amyloid PET, FDG-PET, and MRI. In the most recent version of the IWG criteria,1 CSF Aβ, tau, and amyloid PET are regarded as pathophysiologic biomarkers of AD while FDG-PET and MRI are considered topographic downstream biomarkers. Biomarker support for AD pathophysiology consists of a positive amyloid PET scan or both depressed Aβ42 and elevated t-tau or p-tau in CSF. In the NIA-AA criteria (2011), separate guidelines were outlined for 3 clinical phases—preclinical, MCI, and AD dementia.3–6 The NIA-AA preclinical AD criteria were predicated on the concept that AD biomarkers follow a specific temporal ordering where β-amyloidosis occurs before tau-related neurodegeneration, which in turn is the proximate correlate of clinical symptoms. By contrast, NIA-AA criteria for MCI and AD dementia attribute equal diagnostic weight to all AD biomarkers included in the criteria.
Tables 1 to 3 outline how the A/T/N system maps onto these 2 existing diagnostic classification systems. Conceptual differences both between and within these sets of diagnostic criteria are evident. For example, a clinically asymptomatic individual with a positive CSF Aβ42 and negative CSF tau profile is labeled preclinical AD stage 1 by the NIA-AA criteria but is classified as not being in the AD pathway by IWG. A clinically asymptomatic individual with positive CSF Aβ42 and tau is labeled preclinical AD stage 2 by the NIA-AA criteria and as “asymptomatic at risk for AD” by IWG. Disagreement in how these different diagnostic criteria treat biomarkers creates uncertainty for investigators, regulators, and pharmaceutical companies designing trials. Thus, there is a need for a unifying conceptual approach to biomarkers used in AD research.
Table 1.
Clinically normal individuals
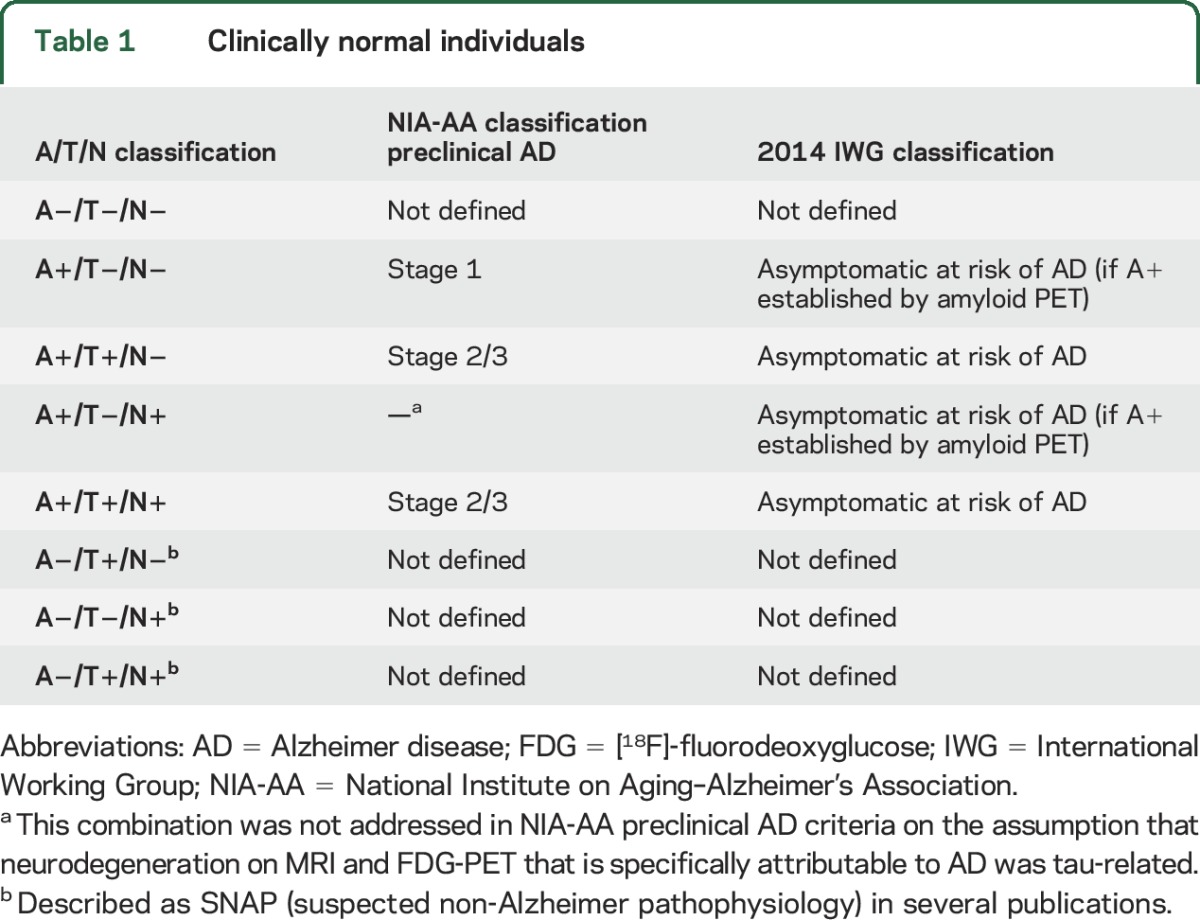
Table 2.
Individuals who meet clinical criteria for MCI
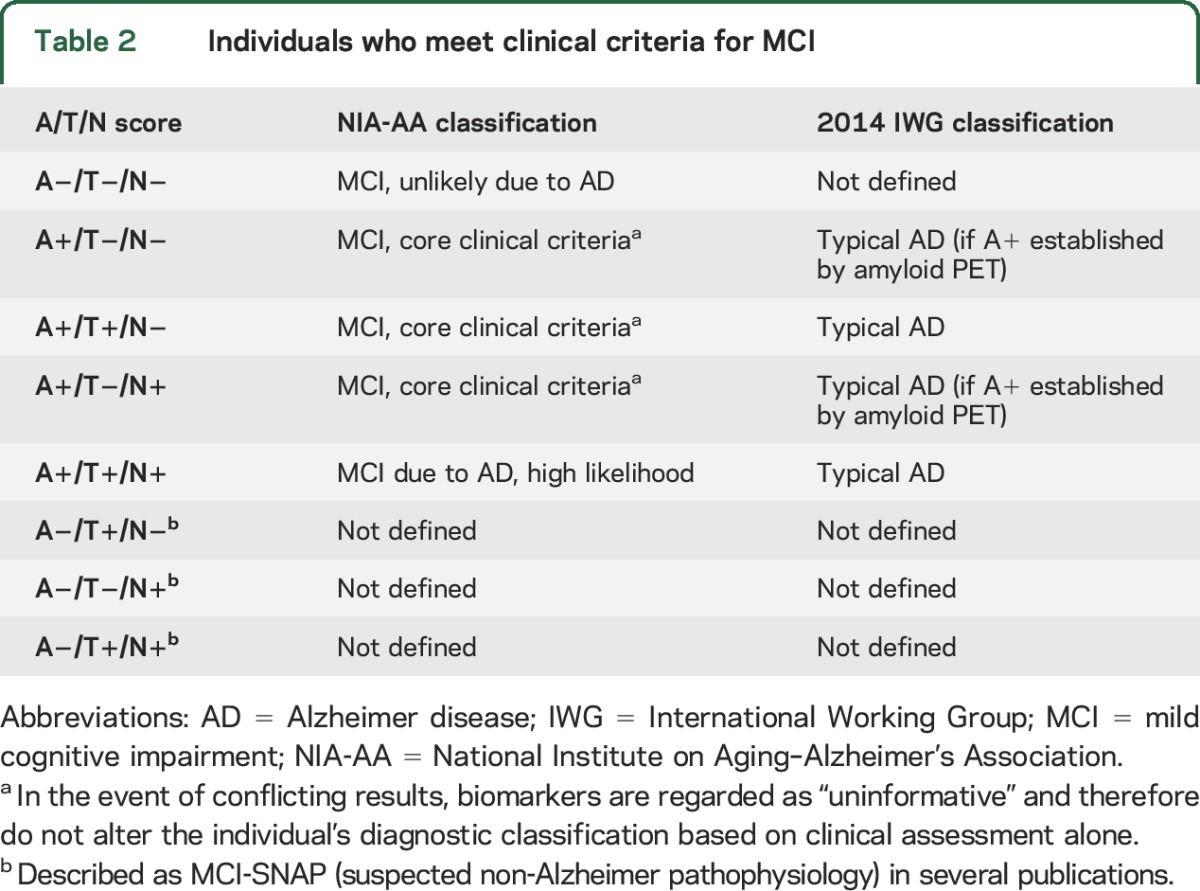
Table 3.
Individuals who meet clinical criteria for probable AD dementia

We recognize that the A/T/N biomarker system will almost always be used in conjunction with a complementary system to classify clinical impairment. By taking an unbiased descriptive approach and avoiding syndromic or disease labels, the A/T/N system can be used in any set of diagnostic criteria that exist currently or are developed in the future. In addition, the A/T/N system includes all individuals in any population and thus is suited to cognitive aging research where AD constitutes only part of the etiologic landscape. We leave it to expert panels such as the IWG and NIA-AA to decide what disease or syndromic labels (i.e., AD, not AD, SNAP, preclinical AD, at risk of AD, MCI due to AD, prodromal AD, etc.) should apply to individuals with varying clinical presentations who are classified into different biomarker states by this system.
Finally, while we anticipate N and T will often concur, i.e., either both will be positive or both negative, this will not always be the case and informative profiles will be identified that are not captured by either the NIA-AA or the IWG system. For example, an A−T−N+ profile would be expected with pathologies such as ischemic cerebrovascular disease or hippocampal sclerosis whereas an A−T+N+ profile would be expected with PART (primary age-related tauopathy).44 An A+T−N+ profile might indicate an individual in the earliest stage of preclinical AD (accounting for the A+T− status) who also has a non-AD pathology such as hippocampal sclerosis (accounting for the N+ status). Other informative profiles will emerge as the A/T/N system is applied empirically.
Supplementary Material
GLOSSARY
- Aβ
β-amyloid
- AD
Alzheimer disease
- FDG
[18F]-fluorodeoxyglucose
- IWG
International Working Group
- MCI
mild cognitive impairment
- NIA-AA
National Institute on Aging–Alzheimer's Association
- p-tau
phosphorylated tau
- SNAP
suspected non-Alzheimer pathophysiology
- t-tau
total tau
Footnotes
Editorial, page 456
AUTHOR CONTRIBUTIONS
Dr. Jack: study concept and design and critical revision of the manuscript for important intellectual content. Dr. Bennett: critical revision of the manuscript for important intellectual content. Dr. Blennow: critical revision of the manuscript for important intellectual content. Dr. Carrillo: critical revision of the manuscript for important intellectual content. Dr. Feldman: critical revision of the manuscript for important intellectual content. Dr. Frisoni: critical revision of the manuscript for important intellectual content. Dr. Hampel: critical revision of the manuscript for important intellectual content. Dr. Jagust: critical revision of the manuscript for important intellectual content. Dr. Johnson: critical revision of the manuscript for important intellectual content. Dr. Knopman: critical revision of the manuscript for important intellectual content. Dr. Petersen: critical revision of the manuscript for important intellectual content. Dr. Scheltens: critical revision of the manuscript for important intellectual content. Dr. Sperling: critical revision of the manuscript for important intellectual content. Dr. Dubois: critical revision of the manuscript for important intellectual content.
STUDY FUNDING
No targeted funding reported.
DISCLOSURE
C. Jack has provided consulting services for Eli Lilly Co. He receives research funding from the NIH (R01 AG011378, U01 HL096917, U01 AG024904, RO1 AG041851, R01 AG037551, R01 AG043392, U01 AG006786) and the Alexander Family Alzheimer's Disease Research Professorship of the Mayo Foundation. D. Bennett reports no disclosures relevant to the manuscript. K. Blennow has served as a consultant for Eli Lilly, Novartis, Roche Diagnostics, and Sanofi-Aventis and on advisory boards for Amgen and IBL International, and has given lectures for Fujirebio Europe and Lundbeck. Dr. Blennow's research team has received grants for collaborative research projects from Eli Lilly and Roche Diagnostics. M. Carrillo is a full time employee of the Alzheimer's Association. H. Feldman reports no disclosures relevant to the manuscript. G. Frisoni has served on advisory boards for Lilly, BMS, Bayer, Lundbeck, Elan, AstraZeneca, Pfizer, TauRx, Wyeth, GE, Baxter. He is a member of the editorial boards of Lancet Neurology, Aging Clinical & Experimental Research, Alzheimer's Diseases & Associated Disorders, and Neurodegenerative Diseases. He is imaging section editor of Neurobiology of Aging. Dr. Frisoni has received grants from Wyeth International, Lilly International, Lundbeck Italia, GE International, Avid/Lilly, Roche, Piramal, and the Alzheimer's Association. Research of industrial interest has touched: memantine, PET amyloid ligands, diagnostic and tracking Alzheimer's biomarkers. Lecture fees when speaking at the invitation of a commercial sponsor (in the past 2 years): Lundbeck, Piramal, and GE. H. Hampel serves as senior associate editor for the journal Alzheimer's & Dementia; he is a scientific advisor/consultant for Axovant, Anavex, Eli Lilly and Company, GE Healthcare, Cytox, Jung Diagnostics, Roche, Biogen, Takeda-Zinfandel, Oryzon; and receives research support from the Alzheimer Foundation (Paris), Pierre and Marie Curie University, Pfizer, Avid; and has (partly pending) patent applications, but receives no royalties. W. Jagust is a consultant to BioClinica, Banner Alzheimer's Institute–Genentech, and Novartis. K. Johnson has consulted for Novartis, AbbVie, Janssen, GEHC, Avid/Lilly, Piramal, Roche, and Isis Pharmaceuticals, is an investigator in clinical trials sponsored by Biogen, Merck, Janssen, Eisai, Navidea, Avid/Lilly, and receives research support from the NIH, Fidelity Biosciences, and the Alzheimer's Association. D. Knopman serves as deputy editor for Neurology®; serves on a data safety monitoring board for Lundbeck Pharmaceuticals and for the DIAN Study; is an investigator in clinical trials sponsored by TauRX Pharmaceuticals, Lilly Pharmaceuticals, and the Alzheimer's Disease Cooperative Study; and receives research support from the NIH. R. Petersen is the chair of the data monitoring committee for Pfizer, Inc., and Janssen Alzheimer Immunotherapy, consultant for Hoffmann-La Roche, Inc., Merck, Inc., Genentech, Inc., Biogen, Inc., and Eli Lilly & Co. He receives royalties from Oxford University Press for Mild Cognitive Impairment. P. Scheltens has received grant support (for the institution) from GE Healthcare, Danone Research, Piramal, and Merck. In the past 2 years he has received consultancy/speaker fees (paid to the institution) from Lilly, GE Healthcare, Novartis, Forum, Sanofi, Nutricia, Probiodrug, and EIP Pharma. R. Sperling has been a consultant for Janssen Eisai, Lundbeck, Isis, Boehringer Ingelheim, Roche, and Genentech; and receives research support from the Alzheimer's Association, Fidelity Biosciences, Janssen, BrightFocus Foundation, and the National Institute on Aging. B. Dubois has received consulting fees from Eli Lilly and Pfizer grant support from industry in 2012. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Dubois B, Feldman HH, Jacova C, et al. Advancing research diagnostic criteria for Alzheimer's disease: the IWG-2 criteria. Lancet Neurol 2014;13:614–629. [DOI] [PubMed] [Google Scholar]
- 2.Dubois B, Feldman HH, Jacova C, et al. Research criteria for the diagnosis of Alzheimer's disease: revising the NINCDS-ADRDA criteria. Lancet Neurol 2007;6:734–746. [DOI] [PubMed] [Google Scholar]
- 3.Sperling RA, Aisen PS, Beckett LA, et al. Toward defining the preclinical stages of Alzheimer's disease: recommendations from the National Institute on Aging–Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement 2011;7:280–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Albert MS, DeKosky ST, Dickson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer's disease: recommendations from the National Institute on Aging and Alzheimer's Association Workgroup. Alzheimers Dement 2011;7:270–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer's disease: recommendations from the National Institute on Aging and the Alzheimer's Association Workgroup. Alzheimers Dement 2011;7:263–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jack CR Jr, Albert MS, Knopman DS, et al. Introduction to the recommendations from the National Institute on Aging–Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement 2011;7:257–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hampel H, Frank R, Broich K, et al. Biomarkers for Alzheimer's disease: academic, industry and regulatory perspectives. Nat Rev Drug Discov 2010;9:560–574. [DOI] [PubMed] [Google Scholar]
- 8.Villemagne VL, Fodero-Tavoletti MT, Masters CL, Rowe CC. Tau imaging: early progress and future directions. Lancet Neurol 2015;14:114–124. [DOI] [PubMed] [Google Scholar]
- 9.Marquie M, Normandin MD, Vanderburg CR, et al. Validating novel tau positron emission tomography tracer [F-18]-AV-1451 (T807) on postmortem brain tissue. Ann Neurol 2015;78:787–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johnson KA, Shultz A, Betensky RA, et al. Tau positron emission tomographic imaging in aging and early Alzheimer's disease. Ann Neurol 2016;79:110–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scholl M, Lockhart SN, Schonhaut DR, et al. PET Imaging of tau deposition in the aging human brain. Neuron 2016;89:971–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Braak H, Thal DR, Ghebremedhin E, Del Tredici K. Stages of the pathologic process in Alzheimer disease: age categories from 1 to 100 years. J Neuropathol Exp Neurol 2011;70:960–969. [DOI] [PubMed] [Google Scholar]
- 13.Duyckaerts C, Braak H, Brion JP, et al. PART is part of Alzheimer disease. Acta Neuropathol 2015;129:749–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Duyckaerts C. Tau pathology in children and young adults: can you still be unconditionally baptist?. Acta Neuropathol 2011;121:145–147. [DOI] [PubMed] [Google Scholar]
- 15.Jack CR Jr, Holtzman DM. Biomarker modeling of Alzheimer's disease. Neuron 2013;80:1347–1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chetelat G. Alzheimer disease: Abeta-independent processes—rethinking preclinical AD. Nat Rev Neurol 2013;9:123–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Small SA, Duff K. Linking Abeta and tau in late-onset Alzheimer's disease: a dual pathway hypothesis. Neuron 2008;60:534–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dubois B, Feldman HH, Jacova C, et al. Revising the definition of Alzheimer's disease: a new lexicon. Lancet Neurol 2010;9:1118–1127. [DOI] [PubMed] [Google Scholar]
- 19.Vos SJ, Verhey F, Frolich L, et al. Prevalence and prognosis of Alzheimer's disease at the mild cognitive impairment stage. Brain 2015;138:1327–1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schneider JA, Arvanitakis Z, Leurgans SE, Bennett DA. The neuropathology of probable Alzheimer disease and mild cognitive impairment. Ann Neurol 2009;66:200–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jack CR Jr, Knopman DS, Weigand SD, et al. An operational approach to NIA-AA criteria for preclinical Alzheimer's disease. Ann Neurol 2012;71:765–775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Klunk WE, Engler H, Nordberg A, et al. Imaging brain amyloid in Alzheimer's disease with Pittsburgh compound-B. Ann Neurol 2004;55:306–319. [DOI] [PubMed] [Google Scholar]
- 23.Fagan AM, Roe CM, Xiong C, Mintun MA, Morris JC, Holtzman DM. Cerebrospinal fluid tau/beta-amyloid(42) ratio as a prediction of cognitive decline in nondemented older adults. Arch Neurol 2007;64:343–349. [DOI] [PubMed] [Google Scholar]
- 24.Mattsson N, Zetterberg H, Hansson O, et al. CSF biomarkers and incipient Alzheimer disease in patients with mild cognitive impairment. JAMA 2009;302:385–393. [DOI] [PubMed] [Google Scholar]
- 25.Visser PJ, Verhey F, Knol DL, et al. Prevalence and prognostic value of CSF markers of Alzheimer's disease pathology in patients with subjective cognitive impairment or mild cognitive impairment in the DESCRIPA Study: a prospective cohort study. Lancet Neurol 2009;8:619–627. [DOI] [PubMed] [Google Scholar]
- 26.Buerger K, Ewers M, Pirttila T, et al. CSF phosphorylated tau protein correlates with neocortical neurofibrillary pathology in Alzheimer's disease. Brain 2006;129:3035–3041. [DOI] [PubMed] [Google Scholar]
- 27.Besson FL, La Joie R, Doeuvre L, et al. Cognitive and brain profiles associated with current neuroimaging biomarkers of preclinical Alzheimer's disease. J Neurosci 2015;35:10402–10411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jagust WJ, Landau SM, Shaw LM, et al. Relationships between biomarkers in aging and dementia. Neurology 2009;73:1193–1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Strozyk D, Blennow K, White LR, Launer LJ. CSF Abeta 42 levels correlate with amyloid-neuropathology in a population-based autopsy study. Neurology 2003;60:652–656. [DOI] [PubMed] [Google Scholar]
- 30.Tapiola T, Alafuzoff I, Herukka SK, et al. Cerebrospinal fluid {beta}-amyloid 42 and tau proteins as biomarkers of Alzheimer-type pathologic changes in the brain. Arch Neurol 2009;66:382–389. [DOI] [PubMed] [Google Scholar]
- 31.Ikonomovic MD, Klunk WE, Abrahamson EE, et al. Post-mortem correlates of in vivo PiB-PET amyloid imaging in a typical case of Alzheimer's disease. Brain 2008;131:1630–1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hong YT, Veenith T, Dewar D, et al. Amyloid imaging with carbon 11-labeled Pittsburgh compound B for traumatic brain injury. JAMA Neurol 2014;71:23–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Krut JJ, Zetterberg H, Blennow K, et al. Cerebrospinal fluid Alzheimer's biomarker profiles in CNS infections. J Neurol 2013;260:620–626. [DOI] [PubMed] [Google Scholar]
- 34.Holmberg B, Johnels B, Blennow K, Rosengren L. Cerebrospinal fluid Abeta42 is reduced in multiple system atrophy but normal in Parkinson's disease and progressive supranuclear palsy. Mov Disord 2003;18:186–190. [DOI] [PubMed] [Google Scholar]
- 35.Blennow K, Wallin A, Agren H, Spenger C, Siegfried J, Vanmechelen E. Tau protein in cerebrospinal fluid: a biochemical marker for axonal degeneration in Alzheimer disease? Mol Chem Neuropathol 1995;26:231–245. [DOI] [PubMed] [Google Scholar]
- 36.Olsson A, Vanderstichele H, Andreasen N, et al. Simultaneous measurement of beta-amyloid(1-42), total tau, and phosphorylated tau (Thr181) in cerebrospinal fluid by the xMAP technology. Clin Chem 2005;51:336–345. [DOI] [PubMed] [Google Scholar]
- 37.Hall S, Ohrfelt A, Constantinescu R, et al. Accuracy of a panel of 5 cerebrospinal fluid biomarkers in the differential diagnosis of patients with dementia and/or parkinsonian disorders. Arch Neurol 2012;69:1445–1452. [DOI] [PubMed] [Google Scholar]
- 38.Hesse C, Rosengren L, Andreasen N, et al. Transient increase in total tau but not phospho-tau in human cerebrospinal fluid after acute stroke. Neurosci Lett 2001;297:187–190. [DOI] [PubMed] [Google Scholar]
- 39.Ost M, Nylen K, Csajbok L, et al. Initial CSF total tau correlates with 1-year outcome in patients with traumatic brain injury. Neurology 2006;67:1600–1604. [DOI] [PubMed] [Google Scholar]
- 40.Skillback T, Rosen C, Asztely F, Mattsson N, Blennow K, Zetterberg H. Diagnostic performance of cerebrospinal fluid total tau and phosphorylated tau in Creutzfeldt-Jakob disease: results from the Swedish Mortality Registry. JAMA Neurol 2014;71:476–483. [DOI] [PubMed] [Google Scholar]
- 41.Buerger K, Otto M, Teipel SJ, et al. Dissociation between CSF total tau and tau protein phosphorylated at threonine 231 in Creutzfeldt-Jakob disease. Neurobiol Aging 2006;27:10–15. [DOI] [PubMed] [Google Scholar]
- 42.Blennow K, Hampel H. CSF markers for incipient Alzheimer's disease. Lancet Neurol 2003;2:605–613. [DOI] [PubMed] [Google Scholar]
- 43.Fotuhi M, Do D, Jack C. Modifiable factors that alter the size of the hippocampus with ageing. Nat Rev Neurol 2012;8:189–202. [DOI] [PubMed] [Google Scholar]
- 44.Crary JF, Trojanowski JQ, Schneider JA, et al. Primary age-related tauopathy (PART): a common pathology associated with human aging. Acta Neuropathol 2014;128:755–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Josephs KA, Duffy JR, Fossett TR, et al. Fluorodeoxyglucose F18 positron emission tomography in progressive apraxia of speech and primary progressive aphasia variants. Arch Neurol 2010;67:596–605. [DOI] [PubMed] [Google Scholar]
- 46.Wirth M, Villeneuve S, Haase CM, et al. Associations between Alzheimer disease biomarkers, neurodegeneration, and cognition in cognitively normal older people. JAMA Neurol 2013;70:1512–1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rabinovici GD, Jagust WJ, Furst AJ, et al. Abeta amyloid and glucose metabolism in three variants of primary progressive aphasia. Ann Neurol 2008;64:388–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Alexopoulos P, Kriett L, Haller B, et al. Limited agreement between biomarkers of neuronal injury at different stages of Alzheimer's disease. Alzheimers Dement 2014;10:684–689. [DOI] [PubMed] [Google Scholar]
- 49.De Meyer G, Shapiro F, Vanderstichele H, et al. Diagnosis-independent Alzheimer disease biomarker signature in cognitively normal elderly people. Arch Neurol 2010;67:949–956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Whitworth JA. 2003 World Health Organization (WHO)/International Society of hypertension (ISH) statement on management of hypertension. J Hypertens 2003;21:1983–1992. [DOI] [PubMed] [Google Scholar]
- 51.Murray ME, Lowe VJ, Graff-Radford NR, et al. Clinicopathologic and 11C-Pittsburgh compound B implications of Thal amyloid phase across the Alzheimer's disease spectrum. Brain 2015;138:1370–1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Thal DR, Beach TG, Zanette M, et al. [(18)F]flutemetamol amyloid positron emission tomography in preclinical and symptomatic Alzheimer's disease: specific detection of advanced phases of amyloid-beta pathology. Alzheimers Dement 2015;11:975–985. [DOI] [PubMed] [Google Scholar]
- 53.Wright JT Jr, Williamson JD, Whelton PK, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 2015;373:2103–2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Grasbeck R. The evolution of the reference value concept. Clin Chem Lab Med 2004;42:692–697. [DOI] [PubMed] [Google Scholar]
- 55.Knopman DS, Jack CR Jr, Wiste HJ, et al. Short-term clinical outcomes for stages of NIA-AA preclinical Alzheimer disease. Neurology 2012;78:1576–1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Klunk WE, Koeppe RA, Price JC, et al. The Centiloid Project: standardizing quantitative amyloid plaque estimation by PET. Alzheimers Dement 2015;11:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Whitwell JL, Josephs KA, Murray ME, et al. MRI correlates of neurofibrillary tangle pathology at autopsy: a voxel-based morphometry study. Neurology 2008;71:743–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hampel H, Schneider LS, Giacobini E, et al. Advances in the therapy of Alzheimer's disease: targeting amyloid beta and tau and perspectives for the future. Expert Rev Neurother 2015;15:83–105. [DOI] [PubMed] [Google Scholar]
- 59.Portelius E, Zetterberg H, Skillback T, et al. Cerebrospinal fluid neurogranin: relation to cognition and neurodegeneration in Alzheimer's disease. Brain 2015;138:3373–3385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Villeneuve S, Reed BR, Madison CM, et al. Vascular risk and Abeta interact to reduce cortical thickness in AD vulnerable brain regions. Neurology 2014;83:40–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


