Abstract
The recently released National Public Health Action Plan for the Detection, Prevention, and Management of Infertility calls for better access to high-quality infertility services and improved safety of fertility treatments. Both assisted reproductive technology (ART) and non-ART fertility treatments have allowed millions of patients worldwide to overcome infertility—a disease of the reproductive system and important public health issue. However, there are substantial disparities in access to effective treatments in the United States, largely attributable to high out-of-pocket costs, especially for ART. Moreover, the outcomes of fertility treatments are often complicated by the large proportion of multiple births with substantial health risks for both neonates and mothers. Prevention of multiple births is difficult during non-ART fertility treatments but can be effective with single-embryo transfer during ART. Several U.S. states have enacted legislative mandates that require private insurers to cover some portion of the costs associated with fertility treatments and thus reduce the financial pressure to transfer multiple embryos during ART. Although studies have shown that insurance coverage reduces per-cycle multiple births to a certain degree, states with insurance mandates have more ART-related multiple births attributable to substantially larger number of ART-conceived neonates. Experience from other countries shows that access to ART can be improved without concomitant increases in multiple births by providing reimbursement for ART in combination with restrictions on the number of embryos transferred per cycle. Such approaches may or may not be successful in the United States with its unique and complex health care system.
Infertility is a disease of the reproductive system and important public health issue.1 To better understand public health implications of infertility, the Centers for Disease Control and Prevention recently released its first National Public Health Action Plan for the Detection, Prevention, and Management of Infertility.1 In addition to promoting strategies for the prevention and early detection of infertility, the plan calls for eliminating disparities in access to high-quality infertility services and improving safety of fertility treatments. Assisted reproductive technology (ART) (defined as fertility treatments in which eggs or embryos are handled in the laboratory with the purpose of establishing a pregnancy, such as in vitro fertilization with or without intracytoplasmic sperm injection) and non-ART fertility treatments (defined as fertility drugs that induce or enhance ovulation in women and are used with timed intercourse or intrauterine insemination but with no intention of performing ART) have been used to help millions of people all over the world overcome infertility. Since the 1960s when non-ART fertility treatments were first introduced, and especially after the first ART birth in 1978, the field of fertility treatments has experienced unprecedented growth, which is expected to continue because of the increasing availability of these treatments and growing demand resulting from delayed childbearing in developed nations. As fertility treatments play a larger role in human reproduction, their effect on demographics and public health is likely to expand. In the United States, the effects of fertility treatments on public health are associated with several factors, including disparities in access to more effective treatment options and suboptimal maternal and child health outcomes, primarily related to the large proportion of multiple births.1
Although many non-ART fertility treatments are relatively affordable or covered by insurance, they often lead to multiple births resulting from the limited ability to predict or control the number of fertilized oocytes and inadequate use of strategies to minimize multiple births. Multiple births are especially common when gonadotropin preparations are used in non-ART cycles.2 On the other hand, ART is often associated with high out-of-pocket costs as a result of limited or lack of insurance coverage, which can make these treatments unaffordable for most U.S. couples affected by infertility. As such, treatment decisions can be influenced by financial incentives. For example, some couples may choose or be required to undergo multiple rounds of less costly non-ART fertility treatments. Likewise, couples may be motivated to transfer multiple embryos per ART cycle to maximize their chances of “success” and avoid another treatment. Notably, many also express a preference for twins, either underestimating or ignoring the higher risks.
Unlike all ART cycles that are annually reported to the Centers for Disease Control and Prevention’s National ART Surveillance System, there is no national reporting of non-ART fertility treatments. As estimated in a recent study, in 2011, ART and non-ART fertility treatments contributed to 36% of all twin births (17% and 19%, respectively) and 77% of all triplet and higher order multiple births in the United States (32% and 45%, respectively).3 Although non-ART treatments contribute to a larger proportion of multiple births in the United States than ART, the ability to prevent iatrogenic multiple births is much higher with ART, in which single-embryo transfer among eligible patients leaves almost no chance for multiple gestation.4,5
Access to ART varies around the globe and depends on many factors, including availability of services, religious or ethical considerations as well as affordability of treatment, which takes into account procedure cost, people’s disposable income, and level of subsidization. The average cost of one fresh ART cycle in the United States ($13,048 in 2006 U.S. dollars) can be more than 46% of annual disposable income, resulting in greater net cost for U.S. patients than patients in other developed countries.6 As a result, only people with high socioeconomic status or adequate insurance can afford the needed treatment, leading to substantial disparities in access to ART. According to the Centers for Disease Control and Prevention’s National Survey of Family Growth, non-Hispanic black women of reproductive age are more than 80% more likely to report infertility than non-Hispanic white women,7 but they are more than 20% less likely to ever receive any infertility services.8
Another consequence of the high out-of-pocket costs of ART is the financial incentive to transfer multiple embryos to increase the chance of live birth, a practice that increases multiple births with substantial risks for both neonates and their mothers. Regardless of the cause of multiple births, neonates born as multiples are more likely to be preterm and have low birth weight, and they are at higher risk for morbidity, including cerebral palsy and autism spectrum disorders. Twins have a 6-fold higher chance of neonatal death than singletons, and triplets have a 14-fold higher chance. Women carrying multiples are at higher risk for cesarean delivery, gestational hypertension, preeclampsia, gestational diabetes, hemorrhage, maternal hospital admission, and mental health dysfunctions. Because almost half of children conceived by ART in the United States are born in multiple gestations,9 overall health risks for these children and their mothers are substantially higher than among the general population. Although there is ongoing debate whether worse health outcomes of children conceived by ART result from underlying factors associated with parental infertility or treatment itself, iatrogenic multiple births resulting from the unnecessary transfer of more than one embryo undoubtedly play a major role.3
Because reduced financial pressure is thought to increase the practice of elective single-embryo transfer and, subsequently, lead to healthy singleton births, insurance coverage of ART has been touted as a mechanism to improve outcomes. In the United States, 15 states have enacted legislative mandates (the most recent one was enacted in Connecticut in 2005) with wide variations in restrictions and exceptions that require insurers to cover some portion of the costs associated with fertility treatments.9 Although studies have shown that insurance coverage for ART (currently mandated in eight states) is associated with fewer embryos transferred per cycle and reduces per-cycle multiple births to a certain degree,10–13 the expectation that insurance coverage will solve the problem of ART-related multiple births has not been realized. To the contrary, states with insurance mandates requiring ART coverage tend to have more ART-related multiple births than other states.9 The reason is that the modest increase in single-embryo transfers and corresponding decrease in multiple births are offset by a dramatic increase in ART use, because ART is more affordable in states with the most comprehensive insurance mandates. The substantially larger number of neonates conceived by ART in these states leads to more ART-related multiple births (Fig. 1). To the best of our knowledge, none of the states with mandated insurance coverage for ART linked such coverage with limits on the number of embryos transferred per cycle, although there is anecdotal evidence that some insurers have introduced their own restrictions on number of embryos transferred per cycle. In addition, because some mandates require a certain number of non-ART cycles before ART-related benefits can be accessed, states with insurance mandates may have a large number of multiple births after non-ART fertility treatments.
Fig. 1.
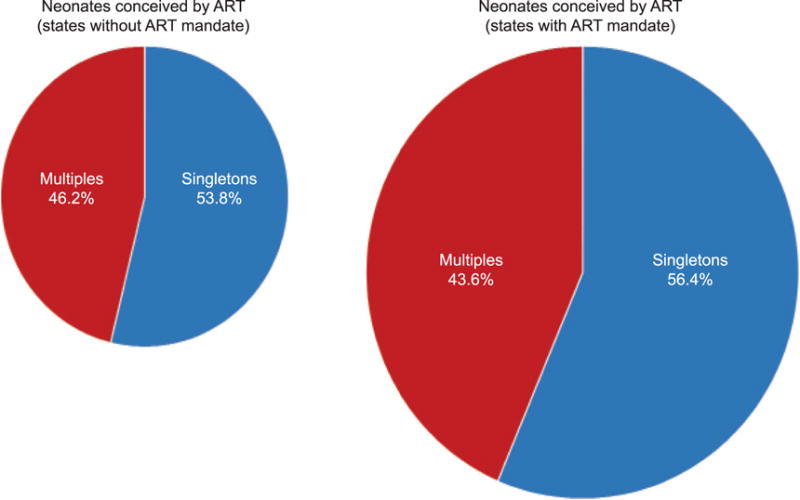
Proportion of singletons and multiples among neonates conceived by assisted reproductive technology (ART) and relative proportion of neonates conceived by ART among all neonates born, by ART insurance mandate status, United States, 2013. The proportion of multiples among ART-conceived neonates in states without an ART insurance mandate (46.2%) is approximately 6% higher than that in states with an ART insurance mandate (43.6%). The size of the pie charts shows the relative proportion of neonates conceived by ART among all neonates born. The proportion of ART-conceived neonates among all neonates born in states without an ART insurance mandate (1.3%) is 123% lower than that in states with an ART insurance mandate (2.9%). Data from National ART Surveillance System, 2013 (http://www.cdc.gov/art/index.html).
Kissin. Fertility Treatments and Public Health. Obstet Gynecol 2016.
What is the best way to balance expanded access to expensive but highly effective technology needed by thousands of couples affected by infertility in the United States with the need to promote the health of children conceived by ART? Experience from several countries shows that providing reimbursement for ART in combination with restrictions on the number of embryos transferred can address both issues without significant reductions in live birth rates.14–16 Policies where ART coverage is contingent on limitations on the number of transferred embryos have resulted in a dramatic increase in the proportion of ART cycles involving single embryos as well as a corresponding decrease in the proportion of multiple births: 54% reduction of multiple births in Australia (from 19% to 9%), 59% reduction in Belgium (from 27% to 11%), and 84% reduction in Sweden (from 35% to 6%). Whether these approaches will work in the United States, given the country’s unique and complex health care system, is unknown.
As more and more people are turning to fertility treatments to achieve their reproductive goals, it is important to ensure that such treatments are accessible and safe. In the context of non-ART fertility treatments, it has been suggested that low-dose gonadotropin protocols may reduce the risk of multiple births.17,18 For some patients, faster transition to more effective fertility treatment options such as ART may be beneficial because time to pregnancy is reduced and exposure to ovulation induction is minimized.18,19 However, because little is known about effectiveness or safety of non-ART fertility treatments, systematic collection of national data on the use and outcomes of ovulation induction and ovarian stimulation is an important first step that can lead to the development of better treatment practices and alleviate their adverse outcomes. More economic analyses are needed to show whether insurance coverage for ART, coupled with safer ART practices, can improve health equity and reduce health care costs associated with iatrogenic multiple births. Development of prediction models can help patients and health care providers to determine the best time for transitioning from one protocol to another and select the safest and most cost-effective treatment algorithms.20 The importance of new approaches to educate couples affected by infertility about the risks of multiple births and the benefits of building their families one newborn at a time cannot be overstated. Well-designed comparative studies that use data from countries with different ART policies may also be useful for studying the effect of these policies on access to ART and its outcomes. A U.S.-based study that assesses reproductive outcomes among women covered by health insurance plans that link reimbursement for ART with limitations on the number of embryos transferred would provide important information on the acceptability and feasibility of such an approach in this country. Such a study will require broad collaboration among federal and state public health agencies, professional societies, consumer groups, and insurance providers.
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Financial Disclosure
The authors did not report any potential conflicts of interest.
References
- 1.Centers for Disease Control and Prevention. National public health action plan for the detection, prevention, and management of infertility. Atlanta (GA): Centers for Disease Control and Prevention; 2014. [Google Scholar]
- 2.Diamond MP, Singh M. Use of gonadotropins for initiation of singleton gestations in non-assisted reproductive technology cycles. Fertil Steril. 2012;97:810–2. doi: 10.1016/j.fertnstert.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 3.Kulkarni AD, Jamieson DJ, Jones HW, Jr, Kissin DM, Gallo MF, Macaluso M, et al. Fertility treatments and multiple births in the United States. N Engl J Med. 2013;369:2218–25. doi: 10.1056/NEJMoa1301467. [DOI] [PubMed] [Google Scholar]
- 4.Kissin DM, Kulkarni AD, Mneimneh A, Warner L, Boulet SL, Crawford S, et al. Embryo transfer practices and multiple births resulting from assisted reproductive technology: an opportunity for prevention. Fertil Steril. 2015;103:954–61. doi: 10.1016/j.fertnstert.2014.12.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kanter JR, Boulet SL, Kawwass JF, Jamieson DJ, Kissin DM. Trends and correlates of monozygotic twinning after single embryo transfer. Obstet Gynecol. 2015;125:111–7. doi: 10.1097/AOG.0000000000000579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chambers GM, Hoang VP, Sullivan EA, Chapman MG, Ishihara O, Zegers-Hochschild F, et al. The impact of consumer affordability on access to assisted reproductive technologies and embryo transfer practices: an international analysis. Fertil Steril. 2014;101:191–8.e4. doi: 10.1016/j.fertnstert.2013.09.005. [DOI] [PubMed] [Google Scholar]
- 7.Chandra A, Copen CE, Stephen EH. Infertility and impaired fecundity in the United States, 1982–2010: data from the national Survey of family growth. Natl Health Stat Report. 2013:1–18. [PubMed] [Google Scholar]
- 8.Chandra A, Copen CE, Stephen EH. Infertility service use in the United States: data from the National Survey of Family Growth, 1982–2010. Natl Health Stat Report. 2014:1–21. [PubMed] [Google Scholar]
- 9.Sunderam S, Kissin DM, Crawford SB, Folger SG, Jamieson DJ, Warner L, et al. Assisted Reproductive Technology Surveillance—United States, 2013. MMWR Surveill Summ. 2015;64:1–25. doi: 10.15585/mmwr.ss6411a1. [DOI] [PubMed] [Google Scholar]
- 10.Boulet SL, Crawford S, Zhang Y, Sunderam S, Cohen B, Bernson D, et al. Embryo transfer practices and perinatal outcomes by insurance mandate status. Fertil Steril. 2015;104:403–9.e1. doi: 10.1016/j.fertnstert.2015.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jain T, Harlow BL, Hornstein MD. Insurance coverage and outcomes of in vitro fertilization. N Engl J Med. 2002;347:661–6. doi: 10.1056/NEJMsa013491. [DOI] [PubMed] [Google Scholar]
- 12.Martin JR, Bromer JG, Sakkas D, Patrizio P. Insurance coverage and in vitro fertilization outcomes: a U.S. perspective. Fertil Steril. 2011;95:964–9. doi: 10.1016/j.fertnstert.2010.06.030. [DOI] [PubMed] [Google Scholar]
- 13.Reynolds MA, Schieve LA, Jeng G, Peterson HB. Does insurance coverage decrease the risk for multiple births associated with assisted reproductive technology? Fertil Steril. 2003;80:16–23. doi: 10.1016/s0015-0282(03)00572-7. [DOI] [PubMed] [Google Scholar]
- 14.Chambers GM, Illingworth PJ, Sullivan EA. Assisted reproductive technology: public funding and the voluntary shift to single embryo transfer in Australia. Med J Aust. 2011;195:594–8. doi: 10.5694/mja10.11448. [DOI] [PubMed] [Google Scholar]
- 15.De Neubourg D, Bogaerts K, Wyns C, Albert A, Camus M, Candeur M, et al. The history of Belgian assisted reproduction technology cycle registration and control: a case study in reducing the incidence of multiple pregnancy. Hum Reprod. 2013;28:2709–19. doi: 10.1093/humrep/det269. [DOI] [PubMed] [Google Scholar]
- 16.Karlström PO, Bergh C. Reducing the number of embryos transferred in Sweden—impact on delivery and multiple birth rates. Hum Reprod. 2007;22:2202–7. doi: 10.1093/humrep/dem120. [DOI] [PubMed] [Google Scholar]
- 17.Cantineau AE, Cohlen BJ, Heineman MJ. Ovarian stimulation protocols (anti-oestrogens, gonadotrophins with and without GnRH agonists/antagonists) for intrauterine insemination (IUI) in women with subfertility. The Cochrane Database of Systematic Reviews. 2007;(2) doi: 10.1002/14651858.CD005356.pub2. Art. No.: CD005356. [DOI] [PubMed] [Google Scholar]
- 18.Practice Committee of American Society for Reproductive Medicine. Multiple gestation associated with infertility therapy: an American Society for Reproductive Medicine Practice Committee opinion. Fertil Steril. 2012;97:825–34. doi: 10.1016/j.fertnstert.2011.11.048. [DOI] [PubMed] [Google Scholar]
- 19.Reindollar RH, Regan MM, Neumann PJ, Levine BS, Thornton KL, Alper MM, et al. A randomized clinical trial to evaluate optimal treatment for unexplained infertility: the fast track and standard treatment (FASTT) trial. Fertil Steril. 2010;94:888–99. doi: 10.1016/j.fertnstert.2009.04.022. [DOI] [PubMed] [Google Scholar]
- 20.van Loendersloot L, Repping S, Bossuyt PM, van der Veen F, van Wely M. Prediction models in in vitro fertilization; where are we? A mini review. J Adv Res. 2014;5:295–301. doi: 10.1016/j.jare.2013.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]


