ABSTRACT
Background
Body armor is credited with increased survival rates in soldiers but the additional axial load may negatively impact the biomechanics of the spine resulting in low back pain. Multiple studies have found that lumbar stabilization programs are superior to generalized programs for patients with chronic low back pain. It is not known if such programs produce objective changes in trunk muscle function with wear of body armor.
Hypothesis/Purpose
An eight-week core stability exercise program would result in a larger improvement in physical endurance and abdominal muscle thickness than a control intervention. The purpose of this study was to assess the effectiveness of an eight-week core stability exercise program on physical endurance and abdominal muscle thickness with and without wear of body armor.
Study Design
Randomized controlled trial
Methods
Participants (N = 33) were randomized into either the core strengthening exercise group or the control group. Testing included ultrasound imaging of abdominal muscle thickness in hook-lying and standing with and without body armor and timed measures of endurance.
Results
There were statistically significant group by time interactions for transversus abdominis muscle contraction thickness during standing, both with (p = 0.018) and without body armor (p = 0.038). The main effect for hold-time during the horizontal side-support (p = 0.016) indicated improvement over time regardless of group. There was a significant group by time interaction (p = 0.014) for horizontal side-support hold-time when compliance with the exercise protocol was set at 85%, indicating more improvement in the core stabilization group than in the control group.
Conclusion
Performing an eight-week core stabilization exercise program significantly improves transversus abdominis muscle activation in standing and standing with body armor. When compliant with the exercises, such a program may increase trunk strength and muscle endurance.
Levels of Evidence
Therapy, Level 2b
Keywords: Body armor, lumbar stabilization, transversus abdominis
INTRODUCTION
Back pain is a significant concern in the military due to attrition from a unit during deployment or training as well as increased medical costs. Back pain has been identified as the leading non-battle injury that occurred in the theater of operations during Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF).1 Low back pain was the primary complaint of 53% of soldiers in OIF/OEF who presented to a military pain management center,1 a leading cause of medical evacuation in OIF/OEF,2 and the second most frequent reason for health care visits of active duty military personnel.3 From 2004 to 2007, only 13% of 1,410 consecutive soldiers medically evacuated to Germany for two weeks of rehabilitation for back pain returned to their deployed unit.4 Not just a condition affecting the U.S. military, the need for medical consultation and treatment due to low back pain was 2.4 times greater for men in the Finnish military than in age-matched controls not in the military.5
Deployed military personnel often carry more than 45 kg of gear and equipment while on foot patrols.6 The Kevlar® vest alone weighs 9.5 kg in its minimum configuration and 14 kg in its standard configuration.7 Body armor (Figure 1) is standard military issued equipment that is vital to the safety of personnel, however, it may cause increased pain and disability due to increased load carriage. There is a positive correlation between increased musculoskeletal pain and soldiers who wore body armor for more than four hours each day.8 Additionally, many soldiers reported that they attributed their back pain to wearing body armor rather than specific job-related tasks or physical training with their units.8 Reports of low back pain were also higher with loads of 45% body weight in active duty Marines.9 Wear of body armor and carrying a ruck sack, ammunition, and weapons can comprise such a load. Postural adaptations, such as increased trunk flexion and forward head posture, are contributing factors to back pain 8,10 and may be exacerbated by wearing body armor, especially if such postures are unable to be counteracted by adequate core stability.
Figure 1.
Participant wearing typical body armor (Point Blank Enterprises, Inc., Pompano Beach, FL) used by service members currently engaged in combat operations. From left to right: anterior, lateral, and posterior view.
There is evidence to suggest that the recurrence of back pain can be reduced with core stabilization exercise programs.11-15 Among individuals who had acute low back pain, those who performed multifidus-specific exercises had a 30% injury recurrence rate compared to the control group of 84% after one year.11 Additionally, improving core strength has been shown to help prevent injury among firefighters by 42% and reduced lost time from injuries by 62%.16 The ability to quantitatively measure muscle thickness under loading would be valuable to clinicians in order to assess the effectiveness of core stabilization treatment programs and could aid in return to work decisions as abdominal muscle thickness has been shown to correlate with strength.17 Ultrasound (US) imaging has been used to measure abdominal muscle thickness with subjects in multiple positions18 or with the muscles under load.19 Imaging the abdominal muscles with and without wear of body armor may provide the clinician with a greater understanding of how the core muscles perform under increasing functional demands.
There is limited available literature on core stabilization effects on muscle activation with wear of body armor in the military population. The purpose of this study was to assess the effectiveness of an eight-week core stability exercise program on physical endurance and abdominal muscle thickness with and without wear of body armor. It was hypothesized that there would be a difference in core muscle engagement when standing with body army as compared to lying supine or standing unloaded. Additionally, it was hypothesized that an eight-week core stability exercise program would result in a larger improvement in physical endurance and abdominal muscle thickness than a control intervention.
METHODS
Participants
Participants were all active duty U.S. service members who responded to recruiting advertisements in the Army Medical Department Center and School at Joint Base San Antonio, Texas. Study inclusion criteria consisted of greater than 18 years of age, able to perform standard physical training, and no conditions that may have affected standing balance. Exclusion criteria included presence of low back pain and inability to perform the prescribed core stability regimen. The study protocol was approved by the Institutional Review Board of Brooke Army Medical Center. All participants provided informed consent prior to study enrollment. Demographic characteristics for all participants are listed in Table 1.
TABLE 1.
Baseline demographics for the control and exercise groups
| Control Group | Exercise Group | |
|---|---|---|
| Sex | 8 Male, 10 Female | 8 Male, 8 Female |
| Age*, years | 27 ± 5 | 29 ± 5 |
| Weight*, kg | 70.53 ± 15.42 | 70.86 ± 10.83 |
| Height*, m | 1.73 ± 0.11 | 1.73 ± 0.12 |
| BMI*, kg/m2 | 23.27 ± 2.88 | 23.66 ± 2.59 |
Values are mean ± SD.
A parallel group, randomized controlled trial was conducted. It was determined that a sample size of 16 participants in each group (using an effect size of 45 seconds based on the extensor endurance test20) was needed to achieve 80% power with alpha set at 0.05. Allowing for attrition, thirty-six active duty men and women over the age of 18 were enrolled from July 2012 to February 2013.
Procedures
During the initial appointment, participants were screened for the absence of low back pain and to ensure they were otherwise physically appropriate to participate in the study. Lumbar range of motion was observed and a bilateral quadrant test21 was performed to ensure pain-free, active motion within a normal physiological range and with provocation (positioning into combined extension and rotation). Participants were randomized into either the core strengthening exercise group or the control group. The randomization process was performed using a random number generator and allocation concealment was preserved until the moment of group assignment.
Participants were evaluated initially and after eight weeks. Previous research has determined that initial changes in muscle strength are related to neural factors,22 such as increased neural innervation. After three to five weeks of strength training both increased neural innervation and hypertrophy of muscles account for strength gains, however, hypertrophic changes are the primary means of strength gains after that time.22 Therefore, the time frame of eight weeks was used to capture both neural and hypertrophic changes that could occur in muscle strength.
The measures during the pre- and post-intervention assessments included ultrasound imaging of abdominal muscle thickness with and without wear of body armor and timed physical endurance tests. Examiners were blind to the participants’ group assignment.
Ultrasound Imaging
Ultrasound imaging was used to measure the muscle thickness of the transversus abdominis (TrA) and internal oblique (IO) at rest and with the TrA preferentially contracted. The imaging took place at both the initial and final assessments. The subject's left side was imaged just superior to the iliac crest to standardize data collection. In order to measure the muscles consistently, the anterior fascia of the TrA was aligned with the edge of the US imaging screen. The US technician read directly from a script to ensure that all participants received standardized instructions. During imaging, the US technician cued the participant with one of three methods (the abdominal drawing in maneuver, cutting off the flow of urine, or closing the anal sphincter) in order to preferentially activate the TrA. The method that best activated the TrA was used for that participant at both initial and final assessments and was used while doing all of the prescribed exercises for participants in the core strengthening exercise group. Three trials of each position were imaged (hook-lying, standing, and standing with body armor) as previously described by Hoppes et al.23 This method has shown high intrarater reliability (ICC (3,3) = 0.90 to 0.98) but poor to fair interrater reliability (ICC (2,1) = 0.39 to 0.79) when measuring abdominal muscle thickness on the same day.23 The longitudinal reliability of this method is not known. Therefore, the same examiner, who had undergone approximately 3-4 hours of hands-on training with the US machine and protocol, performed all US imaging. The order of US imaging was randomized for each participant to prevent order effects such as fatigue.
In the hook-lying position, participants were supine with their knees bent and feet flat to minimize lordosis. In standing, participants lined up the base of each of their fifth metatarsals inside a 30 cm tile on the floor. The time from initiation of standing or standing with body armor until US imaging was approximately two minutes. The body armor used was the same model worn by service members currently engaged in combat operations (Point Blank Enterprises, Inc., Pompano Beach, FL). The manufacturer modified the body armor under the direction of the research team in order to allow access to the abdomen for US imaging while maintaining the structural integrity and weight distribution caused by the Ballistic Panels, Small Arms Protective Inserts, and Enhanced Small Arms Protective Inserts. All inserts were training grade but still possessed the same weight and size as the combat-grade inserts.
The percent change in thickness for each muscle was determined based on the average of three trials for each position according to the equation below and multiplied by 100%.
Preferential Activation Ratio,24 where t is the thickness:
This equation calculates the relative change in the proportion of the TrA relative to the total lateral abdominal muscle thickness, with higher values indicating more change in the TrA thickness and lower values indicating more change in IO and external oblique thickness.24
Physical Testing
Participants completed a series of three timed endurance tests; the order of which was randomized for each participant to prevent order effects. Examiners did not count aloud or provide verbal encouragement during the test. The three timed physical endurance tests were the horizontal side support, extensor endurance, and flexor endurance. The participants were asked to hold each static position until they were either too fatigued to continue or until 240 seconds had elapsed. A rest period of no less than two minutes was provided in between each endurance test.
The extensor endurance test was used to measure the endurance of the erector spinae muscle group, including the lumbar multifidus. This test, also known as the Biering-Sorenson test, has predictive and discriminative validity for nonspecific low back and has high reliability.25 During this test of extensor muscle endurance, participants were required to lie prone on a treatment table with the upper half of their body positioned off the edge and resting on the pull-out head rest while they were supported by straps in three locations (ankles, knees, and greater trochanters). The participants were instructed to hold their torso in neutral alignment, parallel to the floor, after the pull-out head rest was removed. If they deviated greater than ten degrees from neutral they received one verbal cue to realign, and if they faltered again, the test was terminated.
The horizontal side support, which purports to measure the endurance of the TrA muscle,26 started with the participant laying on their right side with legs extended and their feet stacked so their body was aligned. Participants were instructed to lift their hips from the ground and support themselves on their right elbow so that their body maintained a straight line. They were also instructed to hold their left arm across their chest with the left hand placed on the right shoulder. The same position was repeated on the left side. If this position could not be maintained, the participant was verbally prompted to maintain the position, if this could not be achieved, the test was terminated. The horizontal side support is known to have good to excellent interrater agreement for both the right (ICC 0.89-0.91) and left (ICC 0.82-0.91) sides.27 A minimal clinically important difference has not been established for the horizontal side support (or side bridge test), but McGill et al. have proposed ratios between extensor, flexor, and lateral flexor core muscle groups in healthy adults.20
The flexor endurance test measured abdominal muscle strength. This was a modification of a commonly performed exercise in Army physical training, known as the bent-leg raise.28 During this test, participants were supine and lifted both legs 15 cm off the surface of the table. If they deviated greater than 5 cm they were prompted to return to the original position. If they faltered again, the test was terminated.
Intervention
Upon completion of the initial assessment, the intervention group (N = 16) was assigned a core stabilization exercise regimen to perform five days per week for eight weeks. The core stabilization regimen used in this study was adapted from the Prevention of Low Back Pain in the Military (POLM) program.29 The regimen consisted of seven exercises, each performed for one minute (Appendix A). The program called for slow activation of the deep core muscles using the abdominal drawing-in or similar maneuver with little to no trunk movements. All exercises were performed with body weight and fewer repetitions than traditional exercise programs. At the initial session, the intervention group was given a pamphlet of detailed instructions, verbal and tactile feedback while first performing the exercises, and a DVD with a model performing the proper technique for each exercise. The pamphlet included a training log so the participants and examiners were able to track performance of the exercises. After four weeks, the core stabilization group was contacted by phone to determine compliance with the exercise program. At this time, participants were offered verbal reinforcement of the exercises if necessary. When the participants returned for the eight-week follow up, the US imaging and endurance tests were repeated. The training log was collected from each participant but the participants were allowed to keep the pamphlet and exercise DVD.
Upon completion of the initial assessment, the control group was instructed to continue their previous individual workout routines and to avoid starting any new exercise programs. They were not participating in organized physical training with their units and were not participating in the POLM program. At the eight-week follow up, the US imaging and endurance tests were repeated.
STATISTICAL METHODS
Descriptive statistics (mean and standard deviation) were calculated for demographic variables as well as US imaging and physical testing measurements. Six 2 x 2 mixed model analyses of variance were conducted on muscle thickness as a function of time and group using IBM SPSS Statistics 22 (Chicago, IL). The within-participants independent variable was time with two levels (baseline and after eight weeks). The between-participants independent variable was group with two levels (control and core strengthening exercise). The Greenhouse-Geiser test was interpreted as a safeguard against type I error. An intention to treat analysis was used, with baseline data on dropouts carried forward to estimate eight-week status.
RESULTS
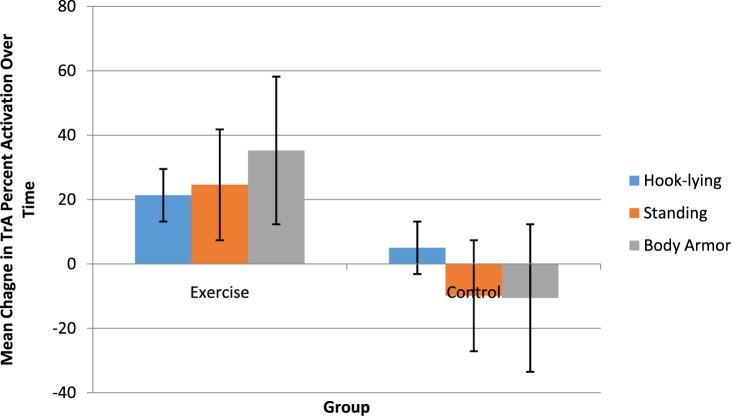
A total of 34 people were enrolled and 33 (17 men, 16 women; average age 28 ± 4.9 years) completed the study (Figure 2). A statistically significant group by time interaction for TrA activation was found during standing, both with (F(1,31) = 6.25, p = 0.02) and without body armor (F(1,31) = 4.70, p = 0.04). The change in thickness of the contracted TrA muscle in the exercise group while standing and standing with a load was significantly greater than the control group after the eight-week core stabilization program (Figure 3).
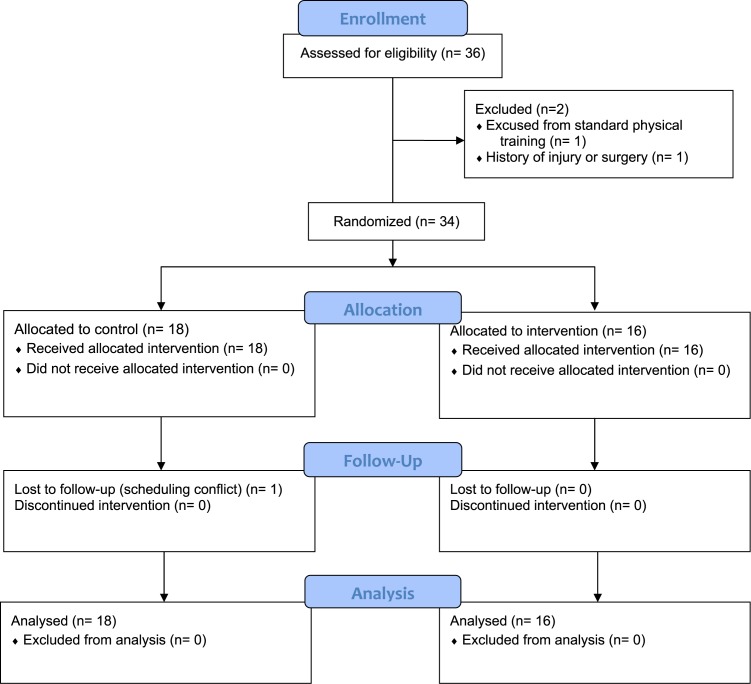
Figure 2.
CONSORT flow diagram.
Figure 3.
Difference in percent activation of the transversus abdominis (TrA) in three positions (hook-lying, standing, and standing with body armor) for the exercise group and the control group after 8 weeks.
The exercise group increased their TrA activation by an average of 24.6% while standing and 35.5% while standing with body armor (Table 2). Although the other muscle contraction thicknesses were not significantly different between the groups after eight weeks, the IO muscle showed a similar trend to the TrA.
Table 2.
Mean percent muscle activation with standard deviation during transversus abdominis (TrA) contraction at baseline and after eight weeks for the control and exercise groups.
| Control Group Initial | Control Group Final | Exercise Group Initial | Exercise Group Final | |
|---|---|---|---|---|
| TrA in Hook-lying | 83.16 (47.44) | 88.21 (52.97) | 69.68 (35.14) | 91.04 (45.12) |
| TrA in Standing | 57.44 (32.63) | 47.58 (36.86) | 42.15 (21.24) | 66.74 (39.43) |
| TrA in Body Armor | 73.74 (46.39) | 63.17 (38.87) | 45.45 (36.07) | 80.71 (46.06) |
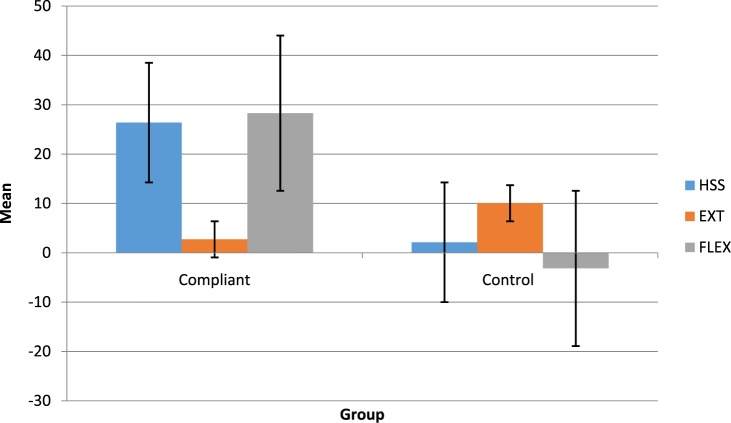
Time by group interactions for endurance hold-times were not statistically significantly different. However, there was a main effect for horizontal side-support (F(1,31) = 6.54, p = 0.02) which indicated an improvement in ability to hold the position regardless of group. Moreover, there was a significant group by time interaction (F(1,31) = 7.05, p = 0.01) for the horizontal side support hold-time when compliance with the exercise protocol was set at greater than 85% (Figure 4). Six subjects in the intervention group, or one-third, achieved 85% or greater compliance with the core stabilization exercise regimen. Those complaint with the exercise protocol increased their ability to hold the horizontal side support from 85.9 ± 41.9 to 112.3 ± 57.7 seconds (mean ± standard deviation).
Figure 4.
Average difference in endurance test hold-time for the compliant exercise group (greater than 85% adherence to the core strengthening regimen) and the control group. Horizontal side support (HSS), extensor endurance (EXT), and flexor endurance (FLEX).
DISCUSSION
The results of this study suggest that performing an eight-week core strengthening exercise program significantly improves TrA muscle activation, assessed by a change in muscle thickness in standing and standing with increased load. For the military population, the implication of this finding may be to offset the physical detriments caused by wearing body armor as activation of the core musculature may reduce excessive mobility and loading of the spine. This study was not designed to serially assess muscle thickness, so it is not known if muscle thickness varies with time in standing. Unpublished thesis work using surface electromyography of the internal and external oblique muscles found no change in muscle activation with 30 minutes of prolonged standing.30 Therefore, the authors do not think that standing would change the measures of muscle thickness over time and the overall implications of the current study.
Not only may an eight-week core stabilization program increase core muscle activation but such a program may also increase core muscle endurance. Although both the control and exercise groups showed significant improvement in performing the horizontal side support, the exercise group showed statistically greater improvements after eight weeks if the participants had higher compliance with the exercise program. Multiple studies have found that lumbar stabilization programs are superior to generalized programs for patients with chronic low back pain.12-15 The eight-week core stabilization program used in this study was found to have a positive effect, though limited, on core endurance. Future studies should explore if such changes in core endurance translate to decreasing the incidence of low back pain and injury related to wearing body armor in the military population.
One limitation of the current study was the compliance rate with the exercise program. Only one participant demonstrated 100% compliance with the exercise program. The lack of compliance by other participants with the prescribed exercises may have negatively affected the endurance test results. For example, when compliance was set at greater than 85%, the length of time the participants were able to hold the horizontal side support significantly increased for the exercise group after eight weeks. The increased endurance hold-time indicates more improvement in the core strengthening group than in the control group when the participants performed the stabilization program as indicated. It is possible that similar results would also occur with the other endurance tests if compliance was higher.
Additionally, there was variability in the measure of the mean percent muscle activation during TrA contraction at baseline and after an eight-weeks for the control and exercise groups, as evidenced by the standard deviations reported in Table 2. This variability may be due to consistency of US transducer placement between the pre- and post-intervention assessments. The authors attempted to limit systematic error by conducting US imaging training, using standardized protocols, and referencing anatomical landmarks. Measurement variability introduced by systematic error would certainly negatively impact the ability to record true changes in muscle activation over time. Figure 3 depicts the difference in percent activation of the TrA in three positions (hook-lying, standing, and standing with body armor) for the exercise group and the control group after 8 weeks. In this figure, the exercise group showed increased activation while the control group showed a trend toward decreased activation. This change in the control group may reflect measurement variability as discussed previously or it may reflect true change. As many of the participants were in academic training programs during the study, they may have become more sedentary over the 8 weeks. These changes were not statistically or clinically different than the baseline measurements.
A third limitation was that while all the participants were active duty personnel, most did not wear body armor regularly, which could limit generalization of the results to other types of U.S. military personnel. There was also no long term follow up with the participants, which would be helpful in determining if the exercise program has long term effects regarding injury prevention. Future studies should incorporate trials of the eight-week exercise program with soldiers who train with body armor regularly or who are deployed, and should include long-term outcome assessments regarding injury rates.
CONCLUSIONS
The results of the current study demonstrate an increase in core muscle activation while wearing body armor and a limited increase in core muscle endurance following an eight-week core stabilization exercise program. Future research is required to determine if this program could be used to decrease the low back pain and injury rates associated with wearing body armor in the military population, in turn leading to decreased attrition rates and medical costs.
APPENDIX A
| Core Stabilization Exercise | Instructions Provided to Participants |
|---|---|
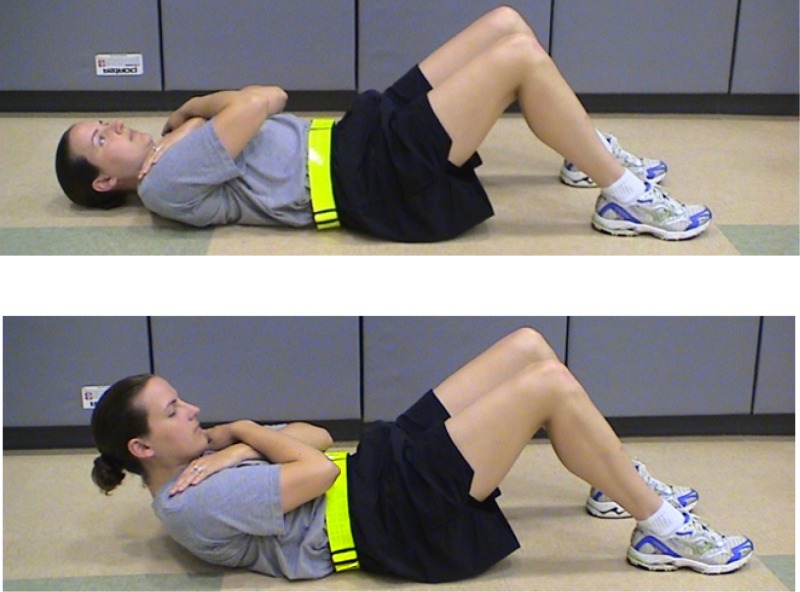 |
Abdominal Drawing-In Maneuver Crunch Start Position: Lie on back with arms crossed over chest. Movement: Pull lower abdominal muscles up and into spine. Slowly curl trunk off the ground until just the base of shoulder blades are touching ground, hold for 10 seconds and then slowly curl trunk back down. Perform 6 repetitions in 1 minute. |
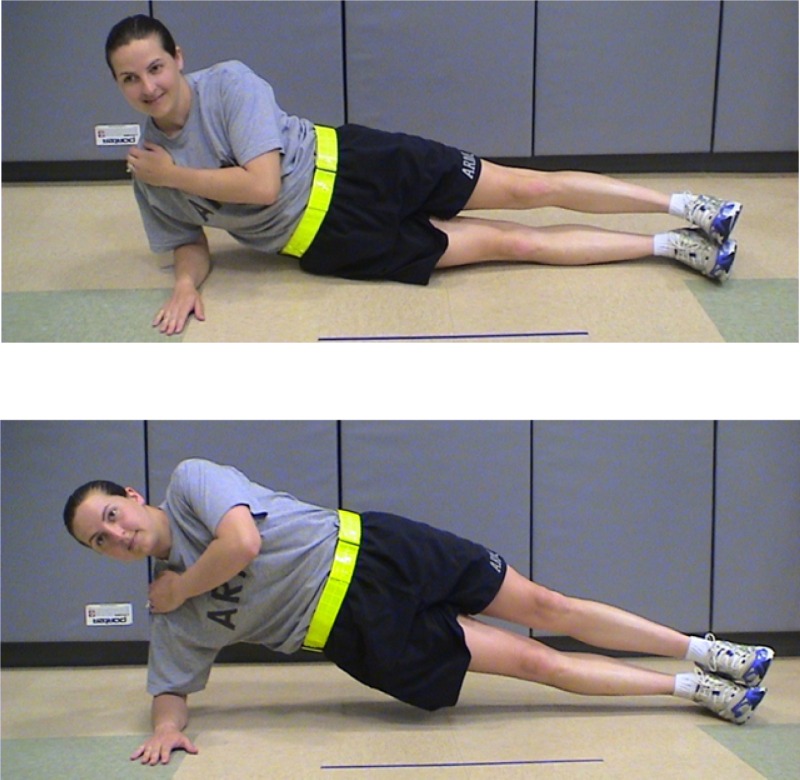 |
Right Horizontal Side Support Start Position: Lie on right side with legs straight and feet stacked. Upper body should be supported with right elbow; cross left arm across chest (left hand on right shoulder). Movement: Pull lower abdominal muscles up and into spine. Lift right side off the ground so body weight is supported through right elbow and feet. Go up in 5 counts and down in 5 counts. Perform 6 repetitions in 1 minute. |
 |
Left Horizontal Side Support Start Position: Lie on left side with legs straight and feet stacked. Upper body should be supported with left elbow; cross right arm across chest (right hand on left shoulder). Movement: Pull lower abdominal muscles up and into spine. Lift left side off the ground so body weight is supported through left elbow and feet. Go up in 5 counts and down in 5 counts. Perform 6 repetitions in 1 minute. |
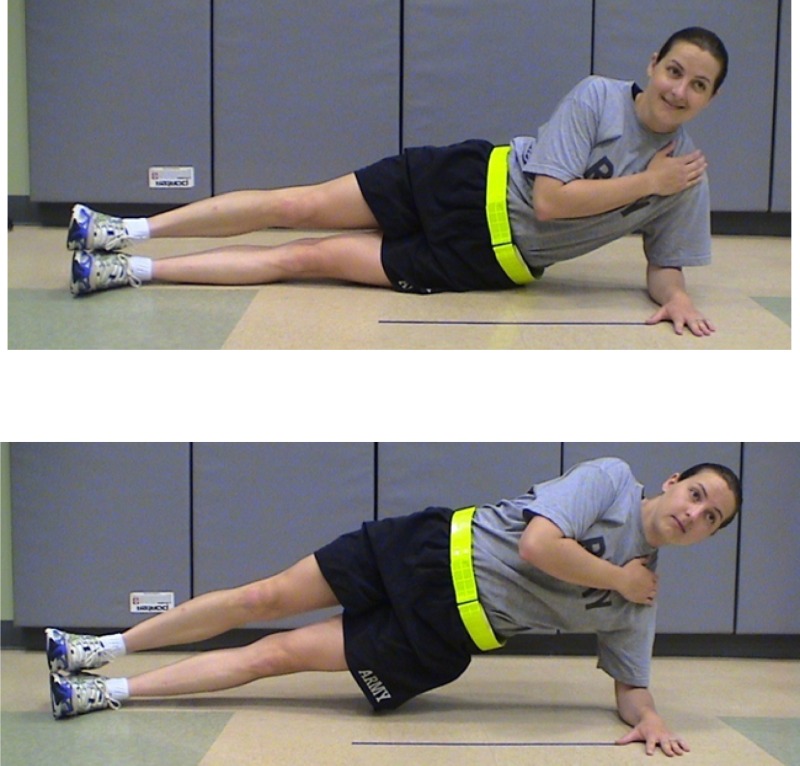
 |
Prone Plank Start Position: Lie on stomach with legs straight and feet together. Upper body should be supported with elbows and forearms. Movement: Pull lower abdominal muscles up and into spine. Lift entire body off the ground so body weight is supported through elbows/forearms and toes. Pull shoulders down and back (don't slump). Hold for 15 seconds in “up” position then slowly return to start. Perform 4 repetitions, 15 seconds each. |
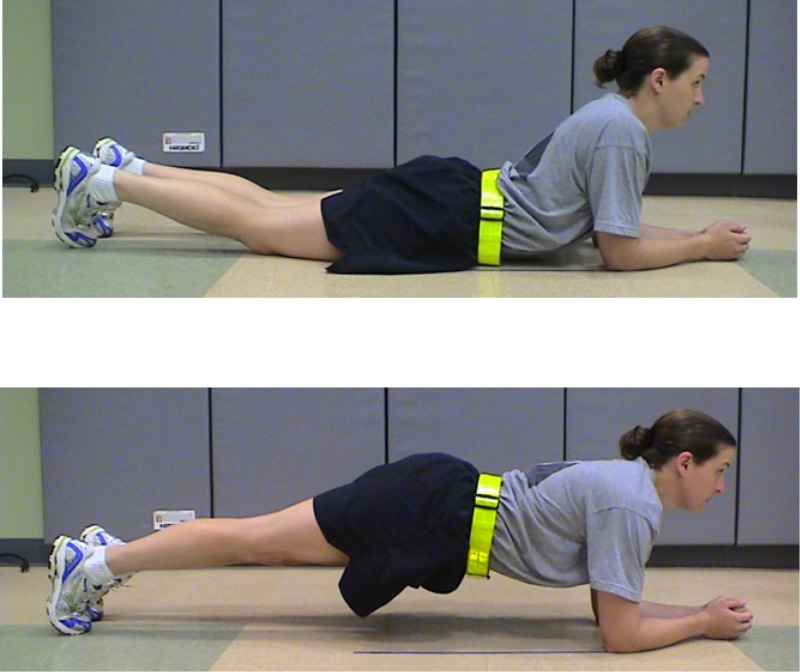
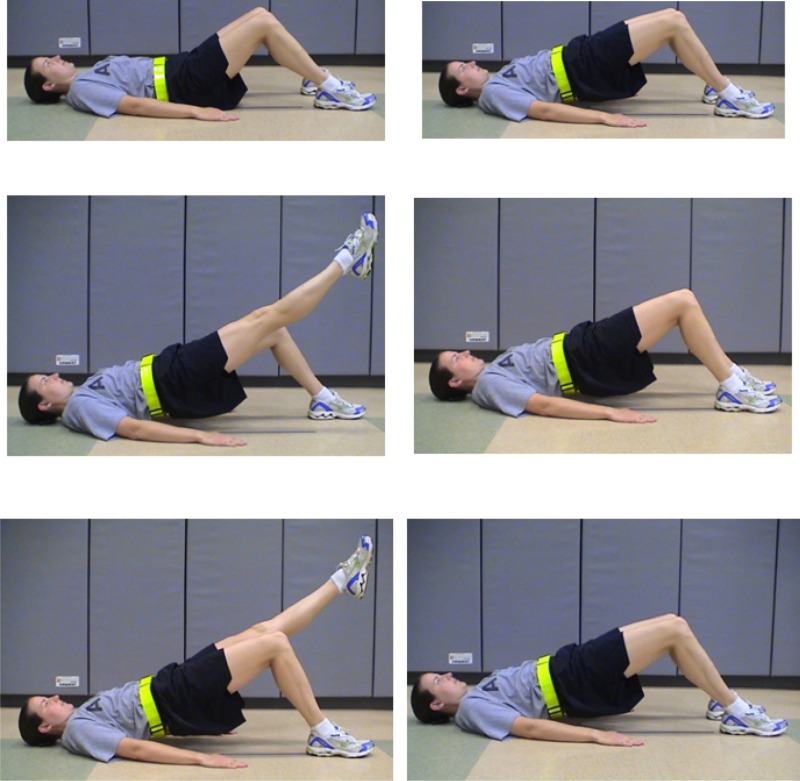 |
Supine Shoulder Bridge Start Position: Lie on back with knees bent 90 degrees, feet flat on the ground. Movement: Pull lower abdominal muscles up and into spine. Lift buttocks off the ground in a straight line (knees, hips, shoulders) supporting weight with shoulders and feet. Straighten right leg and hold for 5 seconds; then slowly bend right knee (5 seconds) and place right foot flat on the ground. Repeat with left leg. Slowly lower buttocks back to start position to complete one repetition. Perform 4 repetitions in 1 minute. |
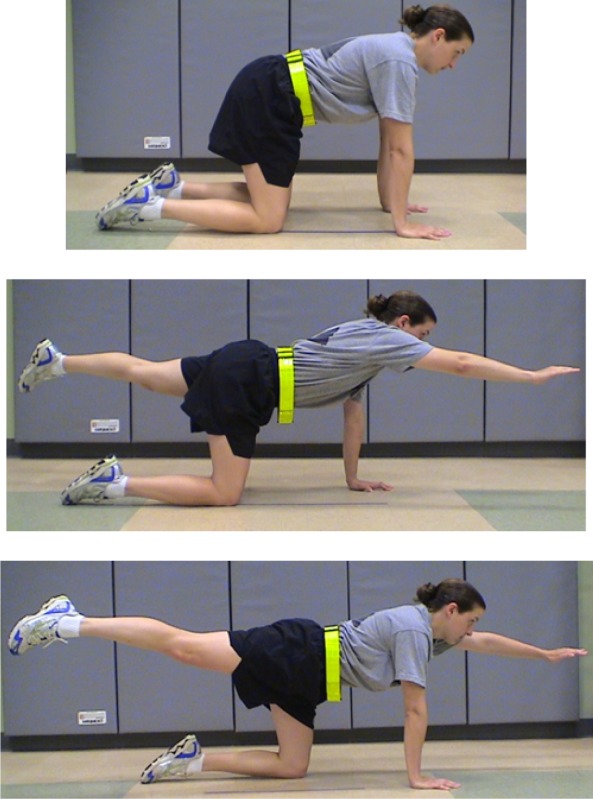 |
Quadruped Alternate Arm and Leg Start Position: On all fours, knees under hips and wrists under shoulders. Movement: Pull lower abdominal muscles up and into spine. Simultaneously stretch out right arm and left leg for a 3 second count, hold for 5 seconds (do not arch back), then slowly return to start position. With each repetition, alternate opposite arm and leg. Perform 4 repetitions in 1 minute. |
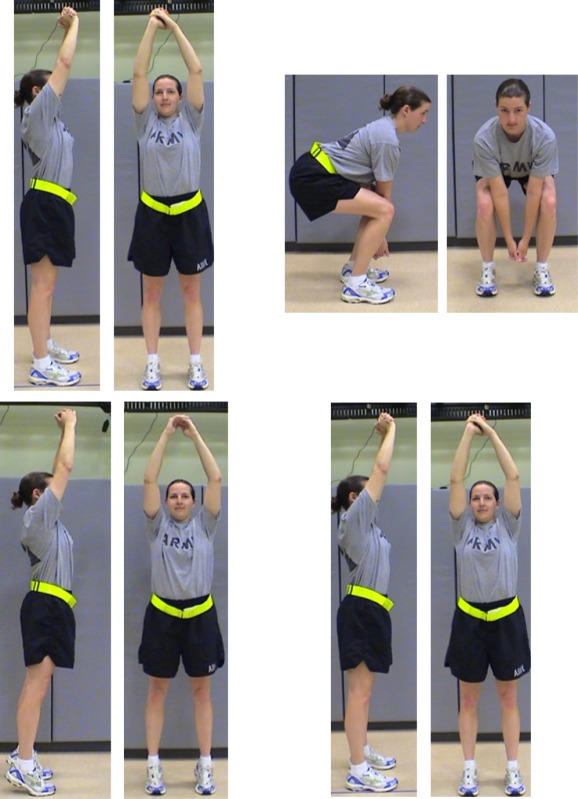 |
Hip Flexor Squat (“Wood-Chopper”) Start Position: Stand with feet shoulder width apart, arms overhead (hands clasped). Movement (2-count): Pull lower abdominal muscles up and into spine. ONE: Squat down, move arms down between knees, keep heels on the floor, stick out buttocks. Do not allow knees to go in front of toes. TWO: Stand up, moving arms overhead, coming up onto toes. Do not arch back. End at start position on the last rep. Perform repetitions of 2-count exercise for 1 minute. |
REFERENCES
- 1.Cohen SP Griffith S Larkin TM Villena F Larkin R. Presentation, diagnoses, mechanisms of injury, and treatment of soldiers injured in Operation Iraqi Freedom: an epidemiological study conducted at two military pain management centers. Anesth Analg. 2005;101(4):1098-1103. [DOI] [PubMed] [Google Scholar]
- 2.Cohen SP Brown C Kurihara C Plunkett A Nguyen C Strassels SA. Diagnoses and factors associated with medical evacuation and return to duty for service members participating in Operation Iraqi Freedom or Operation Enduring Freedom: a prospective cohort study. Lancet. 2010;375(9711):301-309. [DOI] [PubMed] [Google Scholar]
- 3.AFHSC. Absolute and relative morbidity burdens attributable to various illnesses and injuries, US Armed Forces, 2011. MSMR. 2012;19(4):4-8. [PubMed] [Google Scholar]
- 4.Cohen SP Nguyen C Kapoor SG, et al. Back pain during war: an analysis of factors affecting outcome. Arc Intern Med. 2009;169(20):1916-1923. [DOI] [PubMed] [Google Scholar]
- 5.Ulaska J Visuri T Pulkkinen P Pekkarinen H. Impact of chronic low back pain on military service. Mil Med. 2001;166(7):607-611. [PubMed] [Google Scholar]
- 6.Berton H. Weight of War: Military struggles to lighten soldiers’ load. The Seattle Times. 2011. [Google Scholar]
- 7.Erwin SI. Army Has Few Options to Lessen Weight of Body Armor-The Army is considering buying a lighter and comfier vest used by US Special Operations Command. National Defense. 2009(671):36. [Google Scholar]
- 8.Konitzer LN Fargo MV Brininger TL Reed ML. Association between back, neck, and upper extremity musculoskeletal pain and the individual body armor. Hand Ther. 2008;21(2):143-149. [DOI] [PubMed] [Google Scholar]
- 9.Jaworski RL Jensen A Niederberger B Congalton R Kelly KR. Changes in combat task performance under increasing loads in active duty marines. Mil Med. 2015;180(3S):179-186. [DOI] [PubMed] [Google Scholar]
- 10.Attwells RL Birrell SA Hooper RH Mansfield NJ. Influence of carrying heavy loads on soldiers’ posture, movements and gait. Ergonomics. 2006;49(14):1527-1537. [DOI] [PubMed] [Google Scholar]
- 11.Hides JA Jull GA Richardson CA. Long-term effects of specific stabilizing exercises for first-episode low back pain. Spine. 2001;26(11):E243-E248. [DOI] [PubMed] [Google Scholar]
- 12.Koumantakis GA Watson PJ Oldham JA. Trunk muscle stabilization training plus general exercise versus general exercise only: randomized controlled trial of patients with recurrent low back pain. Phys Ther. 2005;85(3):209-225. [PubMed] [Google Scholar]
- 13.O’Sullivan PB Twomey LT Allison GT. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis. Spine. 1997;22(24):2959-2967. [DOI] [PubMed] [Google Scholar]
- 14.Saner J Kool J Sieben JM Luomajoki H Bastiaenen CH de Bie RA. A tailored exercise program versus general exercise for a subgroup of patients with low back pain and movement control impairment: A randomised controlled trial with one-year follow-up. Manual Ther. 2015;20(5):672-679. [DOI] [PubMed] [Google Scholar]
- 15.Vibe Fersum K O’Sullivan P Skouen J Smith A Kvåle A. Efficacy of classification-based cognitive functional therapy in patients with non-specific chronic low back pain: A randomized controlled trial. Eur J Pain. 2013;17(6):916-928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Peate W Bates G Lunda K Francis S Bellamy K. Core strength: a new model for injury prediction and prevention. J Occup Med Toxicol. 2007;2(3):1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Noguchi T Demura S. Relationship between Abdominal Strength Measured by a Newly Developed Device and Abdominal Muscle Thickness. Advances in Physical Education. 2014;4(2):70-76. [Google Scholar]
- 18.Larivière C Gagnon D De Oliveira E Henry SM Mecheri H Dumas J-P. Reliability of ultrasound measures of the transversus abdominis: Effect of task and transducer position. PM&R. 2013;5(2):104-113. [DOI] [PubMed] [Google Scholar]
- 19.Watson T McPherson S Fleeman S. Ultrasound measurement of transversus abdominis during loaded, functional tasks in asymptomatic individuals: Rater reliability. PM&R. 2011;3(8):697-705. [DOI] [PubMed] [Google Scholar]
- 20.McGill SM Childs A Liebenson C. Endurance times for low back stabilization exercises: clinical targets for testing and training from a normal database. Arch Phys Med Rehab. 1999;80(8):941-944. [DOI] [PubMed] [Google Scholar]
- 21.Magee DJ. Orthopaedic Assessment. Canada: Saunders; 2008. [Google Scholar]
- 22.Moritani T. Neural factors versus hypertrophy in the time course of muscle strength gain. Am J Phy Med Rehabil. 1979;58(3):115-130. [PubMed] [Google Scholar]
- 23.Hoppes CW Sperier AD Hopkins CF, et al. Ultrasound Imaging Measurement of the Transversus Abdominis in Supine, Standing, and Under Loading: A Reliability Study of Novice Examiners. Int J Sports Phys Ther. 2015;10(6):910-917. [PMC free article] [PubMed] [Google Scholar]
- 24.Teyhen DS Miltenberger CE Deiters HM, et al. The use of ultrasound imaging of the abdominal drawing-in maneuver in subjects with low back pain. J Orthop Sports Phys Ther. 2005;35(6):346-355. [DOI] [PubMed] [Google Scholar]
- 25.Latimer J Maher CG Refshauge K Colaco I. The reliability and validity of the Biering–Sorensen test in asymptomatic subjects and subjects reporting current or previous nonspecific low back pain. Spine. 1999;24(20):2085-2089. [DOI] [PubMed] [Google Scholar]
- 26.Teyhen DS Rieger JL Westrick RB Miller AC Molloy JM Childs JD. Changes in deep abdominal muscle thickness during common trunk-strengthening exercises using ultrasound imaging. J Orthop Sports Phys Ther. 2008;38(10):596-605. [DOI] [PubMed] [Google Scholar]
- 27.Evans K Refshauge KM Adams R. Trunk muscle endurance tests: reliability, and gender differences in athletes. J Sci Med Sport. 2007;10(6):447-455. [DOI] [PubMed] [Google Scholar]
- 28.FM 7-22 Army Physical Readiness Training. Washington, DC: Headquarters, Department of the Army; 2012.
- 29.George SZ Childs JD Teyhen DS, et al. Rationale, design, and protocol for the prevention of low back pain in the military (POLM) trial (NCT00373009). BMC Musculoskelet Disord. 2007;8(1):92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Soliday KM. Effects of Prolonged Standing on Ground Reaction Force Control and Core Muscle Activation, Colorado State University; 2015. [Google Scholar]