ABSTRACT
Background
Despite the multidirectional quality of human movement, common measurement procedures used in physical therapy examination are often uni-planar and lack the ability to assess functional complexities involved in daily activities. Currently, there is no widely accepted, validated standard to assess movement quality. The Selective Functional Movement Assessment (SFMA) is one possible system to objectively assess complex functional movements. The purpose of this case report is to illustrate the application of the SFMA as a guide to the examination, evaluation, and management of a patient with non-specific low back pain (LBP).
Case Description
An adolescent male athlete with LBP was evaluated using the SFMA. It was determined that the patient had mobility limitations remote to the site of pain (thoracic spine and hips) which therapists hypothesized were leading to compensatory hypermobility at the lumbar spine. Guided by the SFMA, initial interventions focused on local (lumbar) symptom management, progressing to remote mobility deficits, and then addressing the local stability deficit.
Outcomes
All movement patterns became functional/non-painful except the right upper extremity medial rotation-extension pattern. At discharge, the patient demonstrated increased soft tissue extensibility of hip musculature and joint mobility of the thoracic spine along with normalization of lumbopelvic motor control. Improvements in pain exceeded minimal clinically important differences, from 2-7/10 on a verbal analog scale at initial exam to 0-2/10 at discharge.
Discussion
Developing and progressing a plan of care for an otherwise healthy and active adolescent with non-specific LBP can be challenging. Human movement is a collaborative effort of muscle groups that are interdependent; the use of a movement-based assessment model can help identify weak links affecting overall function. The SFMA helped guide therapists to dysfunctional movements not seen with more conventional examination procedures.
Level of Evidence
Level 4
Keywords: Functional movement, low back pain, Selective Functional Movement Assessment
BACKGROUND and PURPOSE
Non-specific low back pain (LBP) is a diagnosis frequently encountered in outpatient orthopedic settings that presents a challenge for both patients and healthcare professionals. LBP is the most commonly reported musculoskeletal complaint among American adults with greater than one in four reporting symptoms in the previous three months.1 Studies have shown that by age fifteen, the incidence of LBP is as high as 36% among adolescents and even more prevalent in those who participate in sports.2 The majority of these cases lack an underlying pathoanatomic diagnosis and are classified as non-specific LBP.3
Despite emphasis on movement and function in physical therapy (PT), traditional examination and evaluation procedures tend to be heavily geared toward measurements of motion in a single plane or isolated assessment of strength of one muscle in order to attempt to identify a patho-anatomic source of pain, lacking the qualitative evaluation of movement patterns as a whole. When considering the composition of musculoskeletal examination, the American Physical Therapy Association's Guide to Physical Therapy practice includes only gross range of motion and strength and lacks specific outcome measures of movement quality.4 Only one study has looked at the psychometric properties of the Selective Functional Movement Assessment (SFMA) and it has been shown to have almost perfect intra-rater reliability and good inter-rater reliability among experienced clinicians when used as a movement-based diagnostic tool that provides clinicians with a standard to identify movement dysfunction in patients with known musculoskeletal injury.5 This objective system assists the healthcare professional in applying a qualitative approach, in parallel with quantitative measurements, in order to guide treatment of musculoskeletal pain and associated movement dysfunction using targeted interventions.6 The SFMA is rooted in the theory of Regional Interdependence which views all regions of the body as being “musculoskeletally linked”.7 Accordingly, seemingly unrelated impairments in remote regions may be the cause of a patient's reports of pain but may go unidentified if the examination is focused on isolated localized movements alone. The SFMA consists of a series of ten functional movements designed to assess fundamental movement patterns of individuals with known musculoskeletal pain. These ten whole body functional movements are then further assessed via algorithms of impairment-based assessments called “breakouts” that dissect each pattern to identify the source of the dysfunction.6,7 The system is intended to help identify meaningful impairments, some of which may initially appear unrelated to the primary complaint, in order to facilitate the development and implementation of an individualized plan of care (POC).
Although this tool is useful with any patient, those with non-specific LBP are particularly good candidates for being evaluated using the SFMA because they lack a clear diagnosis or clearly identified anatomic source for their pain. Van Tulder et al have shown that treatment plans for patients with chronic LBP that focus on a single pathological structure often result in poor outcomes.8 The SFMA can guide the PT to underlying movement dysfunction in remote regions of the system that may be the cause of, or contributory to, abnormal stress in the lumbar spine. Studies have successfully linked limitations in remote regions to symptoms elsewhere in the system, including limitations of hip mobility to LBP and foot dysfunction causing patellofemoral pain.9-10 These correlations suggest the need for a valid evaluative system capable of identifying these dysfunctions to improve outcomes and potentially decrease recurrence. The purpose of this case report is to illustrate the application of the SFMA as a guide to the examination, evaluation, and management of a patient with non-specific low back pain (LBP).
CASE DESCRIPTION
History
The subject signed an informed consent to allow use of his personal medical information for this case report. The subject was an 18 year-old male who had just finished his first year of college and was referred to outpatient PT by his primary care provider with a chief complaint was intermittent low back pain. He reported that the pain had been present for the prior two years, and had become worse in the last three months, including new onset of symptoms in the posterolateral left hip. The subject was an avid weight lifter and participated on his college soccer team. At the time of evaluation he had decreased his lifting frequency from five days a week to two and had significantly adjusted his exercise routine due to his pain; however, he was still playing soccer two to three times a week. The subject reported increased pain and stiffness following weight lifting and sports which were reduced with Ibuprofen and activity modifications. He was otherwise independent in all activities of daily living despite some discomfort. The subject reported his primary goal was to be pain-free with activity so he could return to his full pre-season lifting schedule and full participation in collegiate-level soccer.
Systems Review
The systems review revealed that all systems were unimpaired except the musculoskeletal system. The subject demonstrated limited gross spine and hip range of motion (ROM) and slightly decreased hip strength bilaterally. (Table 1)
Table 1.
Results of systems review at initial examination
| Cardiovascular/Pulmonary | |
| Not Impaired | Heart Rate: 76 beats/min |
| Respiratory Rate: 12 breaths/min | |
| Integumentary | |
| Not Impaired | No presence of scar |
| Skin color and texture within normal limits | |
| Affect, Cognition, Learning Style, Communication | |
| Not Impaired | Alert and oriented times 3 |
| Requests pictures for home exercise program | |
| English speaking, college educated | |
| Neuromuscular | |
| Not Impaired | Lower extremity myotomes, transfers, locomotion, balance, coordination all within normal limits. Did not test dermatomes or deep tendon reflexes |
| Musculoskeletal | |
| Impaired | Hip Strength: 4/5 on L and 4+/5 on R in all planes |
| Spinal AROM: 25% limited/painful in all planes | |
| All other uni-planar AROM within functional limits all planes | |
L = left; R = right; AROM = active range of motion
Clinical Impression 1
The subject's general complaints of LBP for two years and recent left hip pain could be the result of many possible diagnoses; however, he did not present with any red flag signs and therefore had not undergone any diagnostic imaging at the time of evaluation. Based on his complaints, the working differential diagnoses included facet joint dysfunction, intervertebral disc pathology, lumbar strain, sacroiliac joint dysfunction, hip muscular strain, impingement, and/or hip bursitis. The subject was referred to PT to identify and treat the source of his LBP. Based on history, it was suspected that the subject may have had muscle imbalances in the lumbopelvic region leading to LBP with activity.
EXAMINATION
Tests & Measures
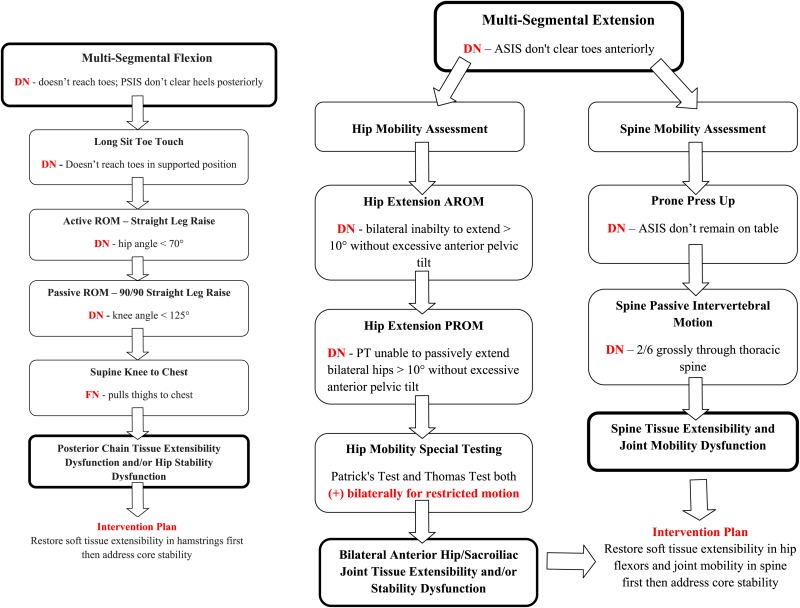
Significant results from initial exam and discharge can be seen in Table 2. The subject was assessed via the SFMA top-tier patterns in order to identify functional movement deficits. A detailed explanation of the administration and interpretation of the SFMA top-tier movements can be found in Appendix A. Results of the SFMA top-tier screening revealed dysfunctional/non-painful movement (DN) in six of the ten motions. He was limited in multi-segmental patterns (including flexion, extension, and rotation), cervical and upper extremity (UE) patterns as well as ability to perform a deep squat. Dysfunctional movement in these patterns can suggest mobility limitations, stability dysfunction or both. Mobility limitations can be categorized as tissue extensibility or joint mobility dysfunction. Stability dysfunctions are more complex and also referred to as a “motor control dysfunction” within the SFMA system. Stability is affected by multiple factors or systems including, but not limited to, the central and peripheral nervous systems, the proprioceptive system, postural alignment, structural integrity, and muscular inhibition, rather than focusing solely on the absolute strength of the stabilizer muscles. Mobility and stability limitations frequently coincide, as the body may sacrifice mobility in one region in an attempt to achieve a compensatory “pseudo-stabilization” in another.6 Based on top-tier results, therapists performed abbreviated versions of the SFMA breakouts over the course of the first two visits in order to narrow down the source of the movement dysfunction. Full details of each breakout is beyond the scope of this manuscript, however, specific follow-up testing using parts of each break out was performed in order to assess mobility and stability impairments (Appendix B).
Table 2.
Results of SFMA and other special tests at initial examination and discharge
| Initial Evaluation Results | Discharge Results | |||||
|---|---|---|---|---|---|---|
| Selective Functional Movement Assessment (SFMA) | Left | Right | Left | Right | ||
| Cervical Flexion | FN | Cervical Flexion | FN | |||
| Cervical Extension | FN | Cervical Extension | FN | |||
| Cervical Rotation | DN | DN | Cervical Rotation | FN | FN | |
| Upper Extremity (LRA) | FN | FN | Upper Extremity (LRA) | FN | FN | |
| Upper Extremity (MRE) | DN | DN | Upper Extremity (MRE) | FN | DN | |
| MSF | DN | MSF | FN | |||
| MSE | DN | MSE | FN | |||
| MSR | DN | DN | MSR | FN | FN | |
| Single Leg Stance | FN | FN | Single Leg Stance | FN | FN | |
| Deep Squat | DN | Deep Squat | FN | |||
| Joint Mobility | Thoracic Spine (all levels): 2/6 | Thoracic Spine (all levels): 3/6 | ||||
| Numeric Pain Rating Scale |
|
|
||||
| Modified Thomas Test | (+) | (-) | ||||
| Patrick Test (FABER) | (-) for hip pathology (+) for limited ROM | (-) for pathology and ROM | ||||
| 90/90 Straight Leg Raise Test (ROM) | (+) | (-) | ||||
| Straight Leg Raise Test (disc pathology) | (-) | (-) | ||||
| Gaenslen's Test | (-) | (-) | ||||
| Hip Scouring Test | (-) | (-) | ||||
| Slump Test | (-) | (-) | ||||
| Quadrant Test | (-) | (-) | ||||
FN = Functional/Non-painful, DN = Dysfunctional/Non-Painful, LRA = Lateral Rotation/Abduction, MRE = Medial Rotation/Extension, MSF = Multi-segmental Flexion, MSE = Multi-segmental Extension, MSR = Multi-segmental Rotation, ROM = range of motion
All special tests and measures were performed according to O'Sullivan and Magee.11-12. Using a verbal numeric pain rating scale, the subject reported his pain was a 7/10 at worst, 2/10 at best and a 3/10 at the time of examination.13 To identify regional sources of dysfunctional patterns, and whether they were due to mobility or stability issues, special tests for soft tissue extensibility of the hip were performed along with a joint mobility assessment of the spine. Special tests were positive for decreased soft tissue extensibility around the hip including the Modified Thomas Test and 90/90 Straight Leg Raise Test. The Modified Thomas Test was graded as a pass/fail, based on whether the test-leg angle at the knee was greater or less than 90 ° and was an indication that the quadriceps and hip flexors were contributing to limited hip mobility, in particular multi-segmental extension.14 FABER's Test was negative for pain provocation and was used to rule out pathology of the hip joint but was positive for ROM restriction.12 The 90/90 Straight Leg Raise Test was performed to asses posterior chain flexibility and was found to be positive for decreased hamstring extensibility determined by a knee angle less than 125 ° and was a likely contributor to limited multi-segmental flexion.12 Decreased joint mobility throughout the thoracic spine was noted to be 2/6 during accessory motion assessment using anterior-posterior glides at the spinous processes.15 Thoracic spine motion was evaluated due to its generally accepted influence on motion of the lumbar spine and lack of thoracic curvature noted with multi-segmental flexion. Isometric break manual muscle tests of the hips were performed bilaterally to assess stability and revealed asymmetrical strength with the right being one-half grade stronger than the left throughout all planes. This method of strength testing has been shown to be both reliable and valid.16 Postural analysis via visual assessment revealed increased thoracic kyphosis and forward shoulders as well as a moderately increased anterior pelvic tilt and lumbar lordosis in standing. Excessive anterior pelvic tilt remained during gait analysis but gait was otherwise unremarkable. Functional gait analysis has been found to be moderately reliable.17 Hip and sacroiliac (SI) joint pathologies were ruled out using the Hip Scouring Test and Gaenslen's Test, respectively. The Hip Scouring Test is a valid and reliable test to detect hip pathology such as impingement. Gaenslen's test has been shown to be reliable (test-retest k = 0.46) based on multiple studies as part of a battery of tests to identify SI joint lesions.12,18 Additionally, SI joint misalignment and leg-length discrepancy were ruled out by palpation and visual observation using the Weber-Barstow Method.12 The Slump Test, which is valid and reliable for adverse neural tension, was negative.12 Facet pathology was ruled out using the Quadrant Test despite literature indicating its poor diagnostic accuracy of this method.19 A Straight Leg Raise Test was also performed during hamstring length assessment and found to be negative, ruling out disc pathology. Palpation revealed tenderness and myofascial density throughout the bilateral erector spinae, quadratus lumborum, gluteus maximus and medius. Therapists assessed core stability using an alternating quadruped (bird dog) exercise; the subject had difficulty maintaining a neutral spine with dynamic motion suggesting underlying core stability deficits. After ruling out hip, SI, facet and disc pathology, the therapists hypothesized that the subject's pain was due to improper movement patterns as a result of the muscular and ROM imbalances identified during examination.
Clinical Impression 2
Examination findings confirmed the hypothesis that the subject had functional movement pattern dysfunctions contributing to his LBP. Based on SFMA and special test findings of decreased mobility in the hips, thoracic spine and shoulder girdle, therapists hypothesized that the lumbar spine was moving excessively as compensation for this lack of motion. His stability and mobility limitations were consistent with the joint-by-joint theory which argues that joints alternate in their primary role from stability to mobility and when a joint isn't able to carry out it's typical mobility or stability role, the next joint in the chain eventually will.6,20. The subject displayed limited functional mobility at the hips, thoracic spine and shoulder which, according to this theory, function primarily as mobile joints while the lumbar spine serves primarily as a stable junction between the thoracic spine and pelvis. Therapists hypothesized that dysfunctional movements identified in basic SFMA patterns indicated a poor fundamental foundation for proper movement, causing excessive compensation at the lumbar spine.
Dysfunctional patterns could be the result of a true mobility deficit stemming from either limited soft tissue extensibility or joint mobility, or due to increased muscular tone as a result of an unstable segment.9 As seen in Appendix B, based on active and passive flexibility testing in supported postures with associated muscular end-feel and the results of special tests, it was believed the primary reason for decreased mobility at the hip was soft tissue extensibility and the thoracic spine limitations were due to impaired gross vertebral joint mobility. Based on the subject's inability to maintain and control pelvic tilt and lumbopelvic positioning during exercise activities (for example an inability to maintain a neutral spine while performing quadruped stability exercises) the therapists believed based on clinical experience there were also underlying core stability deficits contributing to excessive stress at the lumbopelvic junction. This may have resulted in his gross increase in tone as a means to restore or impose stability using the global musculature. However, it was decided this was a secondary dysfunction that would be addressed at a later point once proximal and distal mobility had been restored.
The therapists also believed that a major contributor to limited UE ROM was restricted thoracic spine extension as the subject was only limited in the functional (combined) pattern and had full motion for both shoulder extension and internal rotation assessed in isolation. The working hypothesis was that these limitations had caused this subject to load his lumbar spine in a hyperextended and unstable position when weight training, resulting in excessive pressure.
Physical Therapy Diagnosis
Based on findings from the examination, therapists determined the subject's primary PT diagnosis was impaired muscle performance (pattern 4C) due to chronic musculoskeletal dysfunction as well as a secondary diagnosis of impaired posture (pattern 4B). The ICD – 9 code was Lumbago (724.2).
Prognosis
The subject was a good candidate for PT due to his age, active lifestyle and motivation. In considering prognostic factors for recovery, chronicity was a negative factor, but the subject's young age was a positive factor.21 With improved mobility, stabilization exercises, postural modification and corrected movement patterns, it was anticipated that the subject's symptoms would subside, allowing him to meet his long-term goal of return to full activity with proper form and mechanics. Discharge criteria included being pain-free at rest and with exercise and attainment of a score of 14 or better on the Functional Movement Screen (FMS™) that indicated the subject was no longer at increased risk of injury with return to activity.6,22
INTERVENTIONS
Patient/client related instruction
Therapists communicated to the subject that the plan of care (POC) was to alleviate symptoms first before progressing to mobility, then stability exercises. The subject was educated on what therapists hypothesized was contributing to his LBP. Therapists suggested to the subject that he avoid activities that caused pain and highly recommended he reduce the number of soccer games he was playing while continuing to adjust his weight training program. Finally, the subject was given an initial home exercise program (HEP) which included foam rolling for the hamstrings and quadriceps, a standing hamstring stretch, and half kneeling rear foot elevated hip flexor stretch to address soft tissue extensibility limitations present at the hip. Thoracic spine extension over a foam roller was incorporated to address general thoracic vertebral joint hypomobility. Finally, spine flexion/extension in quadruped was used to incorporate proprioceptive feedback during performance of controlled lumbopelvic motions while also integrating diaphragmatic breathing for its role in stabilization of the spine.25 The subject confirmed he understood the POC, HEP and discharge criteria.
Procedural interventions
The subject was seen for 13 visits over nine weeks. Visits ranged from 45 minutes to one hour in duration and began with one to two visits per week initially, then one visit per week during the last three weeks. Interventions, based on categories put forth by the Guide to Physical Therapist Practice, included manual therapy, motor function training, and therapeutic exercises.4 Manual therapy techniques included soft tissue massage, spinal mobilization, high velocity manipulation of the spine, and passive ROM. Motor function training was incorporated into most exercises in the form of neuromuscular re-education for improved postural stabilization. Therapeutic exercises incorporated into the POC included flexibility, strength and power exercises, and breathing strategies.
Therapists initially prioritized pain relief in the lumbar region for the initial one to three weeks, theorizing that pain would disrupt normal movement patterns and cause continued dysfunction.26 Pain was treated using soft tissue massage to lumbar paraspinals and breathing techniques which were effective in minimizing pain. This same rationale was applied to the decision to attain full ROM of all limited patterns, which was the focus of weeks three to six, before performing stability exercises. Based on clinical experience the therapists believed attempting exercises with limited range would also result in altered movement patterns. Interventions carried out were from one of three categories including “resets” such as modalities or stretching to decrease pain or restore mobility, followed by a “reinforcement” exercise which incorporated newly gained ROM into a motion to protect the reset gains, and finally “reloading” movements which would integrate new gains into a functional pattern using therapeutic exercise.6 An example of this progression for the subject would be hamstring stretching as a mobility “reset”, followed by performance of toe touches with heels elevated to reinforce hamstring length and pattern a posterior weight shift, and finally “reloading” via completion of a proper deadlift with adequate posterior weight shift of the pelvis in order to strengthen within the corrected movement pattern.
To begin every treatment session, the subject was assessed using each of the SFMA top tier movements that were dysfunctional during the previous visit in order to guide treatment. Reports of pain were addressed with soft tissue massage, positioning and breathing techniques or spinal manipulation.27-29 Limited motion or soft tissue extensibility was addressed using sustained stretching including rear foot elevated hip flexor stretches and contract relax stretching for the hamstrings. Joint mobility restrictions were treated with high velocity spinal manipulation of the upper thoracic spine in supine or grade IV P-A glides of the vertebrae throughout the thoracic spine in prone. 12,15,28,29
Once mobility was normalized, as determined by a re-evaluation of special testing, limitations in lumbopelvic control during movement became more apparent; likely due to a loss of secondary stability that was being provided by tightness in hip musculature. This was addressed with static stability exercises such as planks which were progressed to dynamic core stability exercises that incorporated extremity movements while maintaining pelvic control such as ½ kneeling diagonal chops and lifts with resistance bands.28. Stability exercises were progressed based on neurodevelopmental sequencing beginning with a posture that provided more support, such as quadruped or ½ kneeling, to positions demanding more motor control and balance such as asymmetrical split-stance or single-leg stance. The therapists believed that if the subject could not display effective motor control in foundational (lower level developmental) positions, he likely would compensate in more complex (higher level developmental) patterns leading to continued stress on his back. Therefore a stability progression, with a goal of return to power lifting activities, began with cat-camel pelvic tilting to increase proprioceptive sense of a neutral spine. This neutral position was then progressed and strengthened dynamically with alternating upper and lower extremity motion in quadruped. The subject was then challenged to load his spine in this position by shifting his weight into a stability ball and maintaining a neutral pelvis and spine. Once he demonstrated good control of his pelvis with loading to the spine, he was progressed to double leg squatting and deadlifting with kettlebells, followed by asymmetrical lunging and single leg exercises in order to continue to strengthen his hips and promote core stability in more challenging positions. Once the subject could consistently perform these activities with a stabile pelvis, and without excessive lumbar extension, he was progressed to powerlifting with a barbell and finally to sport-specific training for soccer.
Initially the therapists focused on restoring multi-segmental patterns for flexion and extension as these were most limited. These patterns were cleared for mobility issues and pain in the first five sessions using manual therapy techniques and as a result of the subject's commitment to his HEP. These gains were maintained for all subsequent visits and stability exercises were progressed as previously described. Despite patterns being functional, the subject continued to demonstrate excessive lumbar lordosis with advanced exercises. As seen in Appendix C, focus was then shifted to UE movement patterns which were limited in the medial rotation and extension pattern, primarily on the right side. Based on clinical experience and the joint-by-joint theory it was hypothesized that limited motion was promoting compensation with excessive lumbar extension when under a barbell.6,20 Shoulder ROM improved in subsequent treatment sessions, and when combined with previously mentioned core stabilizing neuromuscular-reeducation exercises, the excessive lumbar compensation during power lifts was resolved. Appendix C shows all procedural interventions and progressions performed during each visit.
The subject was sent home to progress his activity over two weeks, then return for a reevaluation. At that time, the subject reported being pain-free with activity and was screened using the FMS™ (Table 3). The subject met his long-term goal of pain-free weight lifting as well as the therapist's criteria for discharge based on FMS™ scoring and was discharged with an updated HEP after ensuring proper technique with deadlift and squat.
Table 3.
Results of the Functional Movement Screen performed at discharge. The patient reached the long term goal of a 14 or higher with no 1's, 0's or asymmetries.
| Functional Movement Screen | |||
|---|---|---|---|
| Screen | Raw Score (R) | Raw Score (L) | Final Score |
| Deep Squat | 2 | 2 | 2 |
| Hurdle Step | 2 | 2 | 2 |
| In-line Lunge | 2 | 2 | 2 |
| Shoulder Mobility | 2 | 2 | 2 |
| Shoulder Clearing Test | Negative | Negative | - |
| Active Straight Leg Raise | 2 | 2 | 2 |
| Trunk Stability Push-up | 3 | 3 | 3 |
| Push-Up Clearing Test | Negative | Negative | - |
| Rotary Stability | 2 | 2 | 2 |
| Posterior Rocking Test | Negative | Negative | - |
| Total | 15 | ||
OUTCOMES
The subject of this case report showed significant improvements in pain (exceeding MCID), ROM (based on special tests and movement patterns), strength, and subjective motor control, achieving his long-term goal of a full pain-free return to weight lifting and soccer (Table 2). Additionally, he met both long-term goals set forth by therapists which included 5/5 symmetrical strength in bilateral hips and an FMS™ score ≥ 14 with no asymmetries or 0's. Thoracic spine joint mobility (T1 – T12) went from a 2/6 to a 3/6 based on a P-A glide assessment and hip mobility improved bilaterally based on special tests. The subject received a designation of DN on nine of the ten SFMA movement patterns at initial evaluation and only one (right UE pattern) at discharge. Most notably, at discharge the subject reported 0-2/10 pain, improved from 2-7/10 at initial examination. The subject demonstrated improved form with deadlifting, with control of his pelvis and decreased lumbar lordosis. Outcomes at initial examination and discharge are detailed in Tables 2 and 3
DISCUSSION
This case report outlines the application of the SFMA and theory of Regional Interdependence to guide initial examination, POC development, exercise selection and discharge criteria for a subject with LBP. Utilizing treatment principles suggested by the creators of the SFMA, this subject made significant improvements over the course of his nine week episode of care which allowed him to return to sports and weight lifting without pain. Emphasis placed on regaining mobility in his hips, mostly through his commitment to the HEP, appeared to be a major contributing factor to his decrease in symptoms. The effects seen after gains in mobility further supports the previously noted relationship between hip ROM restrictions and LBP.11 Once hip mobility was restored, emphasis was placed upon motor control to maintain stability at the lumbopelvic junction, which therapists believed may have been artificially created by the increased tissue tightness in his hips and thoracic spine as opposed to a true active stability. According to a supposition by Cook, limited hip motion has been assumed to cause back pain, however, instability in the back may in fact have facilitated “apparent hip tightness” that serves as a “secondary brace” to allow for continued function, even if it reduces mobility.5 This works in agreement with the joint-by-joint theory, wherein a possible instability at the lumbar spine may have created compensatory stability through increased tone at the joints above and below. It is difficult to determine which came first; therefore it was necessary to focus on maintaining a stabile spine once mobility was restored.
The primary hypothesis was that improved motor control and core stability in addition to the subject's newly acquired functional mobility, would allow him to return to athletics without risk of re-injury. To accomplish this, therapists sought to establish basic functional movement patterns which serve as the foundation for higher movement skills such as weight lifting and soccer.6 The goal of targeting movement pattern interventions was to attempt to resolve total body impairments, such as those identified by the SFMA. The SFMA helped to guide therapists away from the tendency to treat one pathological structure in a region such as the back, and instead identify non-painful impairments in regions adjacent to the site of pain that required intervention. We believe that this approach may help avoid falling into a continued cycle of recurring dysfunction and chronic pain by identifying the cause of pain rather than dealing with local symptoms.
The SFMA and FMS™ provide a means to both assess painful movement and screen pain-free movement. The two systems as a whole identify subtle impairments in movement patterns of the active individual, the correction of which theoretically results in decreased recurrence of injury. Currently only one study has looked at psychometric properties of the SFMA and it demonstrated poor to good reliability among novice evaluators and very good reliability in experienced users.29 However, responsiveness to change and validity of the SFMA has yet to be explored. Further investigation of the application of the SFMA and associated outcomes in various musculoskeletal injuries is needed. Validation of the SFMA as a clinical outcome tool has the potential to function as an adjunct to the current medical/pathoanatomic examination model, with the potential to serve as a standard for the assessment of functional movement patterns.
LIMITATIONS
Typical of case reports, the single subject design limits the relevance of these results when considering similar patients. Interventions based upon the SFMA proposed intervention system can vary greatly between therapists, as there is no definitive treatment prescription related to specific findings, and therefore intervention choices are dependent upon practitioner judgement, experience, and personal equipoise. As a result, each PT may have different approaches for interventions. Therefore it is not known if other treatments for this patient would have resulted in similar outcomes.
CONCLUSIONS
This case report demonstrates the effective use of the SFMA as a method or system used to qualitatively analyze movement at initial examination, and throughout the treatment process, and to direct subsequent intervention choices. In this case, the SFMA helped therapists to recognize dysfunctional movements that were present in subsequent regions that were not seen with more conventional examination procedures. While the ability to establish a cause-and-effect relationship is limited in this single subject, in this instance the SFMA presented an effective framework for the evaluation and treatment of an athlete with non-specific low back pain.
Figure 1.
Medial rotation–extension stretch (left figure). Deadlift with neutral spine (right figure).
Figure 2.
Multi-segmental flexion (left figure) and multi-segmental extension (right figure) were both functional/non-painful at discharge.
Figure 3.
Medial Rotation–Extension pattern was functional/non-painful on the left (left figure) but remained dysfunctional/non-painful on the right at discharge (right figure).
Appendix A: SFMA Instructions, Patterns & Criteria
The SFMA is meant to be used for a patient with pain, unlike the FMS™ which is a pain-free screen. It uses movement to provoke symptoms and demonstrate dysfunction.
The assessment consists of ten basic movements that are standardized for classification. Patterns are broken down into respective “breakouts” for clarity and perspective.
Breakouts include active and passive movements, weight-bearing and non-weight-bearing positions, multiple and single-joint functional movement assessments and unilateral and bilateral challenges.
When performing the assessment the examiner should avoid excessive instructions for form in order to evaluate how the patient moves naturally.
Any additional movements deemed to be compensation outside the specified movement pattern is graded as dysfunctional.
Any movement pattern that results in labored breathing is graded as dysfunctional.
Any movements that provoke pain should be further assessed with caution as pain is known to alter motor control. Pain modulating therapies/modalities should be used and movements reassessed.
- Top-tier movements and breakout tests are graded with 4 possible notations based on subjective assessment:
- Functional/Non-painful (FN)–meets specified criteria and patient reports no pain
- Further investigation of that pattern not recommended
- Consider using FMS™ to asses pain-free functional movement patterns
- Functional/Painful (FP)–meets specified criteria but patient reports pain
- Confirmation of patterns which can provoke pain can be used as a marker
- Pattern can be broken down to sub-movements; proceed to treat symptoms
- Dysfunctional/Non-painful (DN) – does not meet criteria but patient reports no pain
- Breakdown movement uncomplicated by pain
- Further examine using breakout algorithm for that pattern to identify if the dysfunction is due to mobility or stability and whether the limitations stem from soft tissue extensibility or joint mobility
- Dysfunctional/Painful (DP) – does not meet criteria and patient also reports pain
- Need to determine if poor movement is causing pain or pain is causing poor movement
- Treat symptoms first before addressing movement with exercises
Cervical Patterns
Cervical Flexion

Instructions: Stand erect with feet together, toes pointing forward. Touch chin to chest with mouth closed.
Criteria:
Chin touches sternum with mouth closed
Evaluating: available cervical flexion including occipital-axis mobility
Breakout: Active supine cervical flexion → passive supine cervical flexion → active atlanto-occipital supine cervical flexion
Cervical Extension

Instructions: Stand erect with feet together, toes pointing forward. Patient instructed to extend neck back as far as they can.
Criteria:
Head reaches > 10 ° of parallel
Evaluating: available cervical spine extension
Breakout: supine cervical extension
Cervical Rotation (R + L)

Instructions: Stand erect with feet together, toes pointing forward. Patient rotates the head as far as possible, then flexes the neck moving chin to collarbone.
Criteria:
Chin touches mid-clavicle
Evaluating: amount of available cervical spine rotation and lateral flexion in a pattern which combines both movements.
Breakout: active supine cervical rotation → passive cervical rotation → supine C1-C2 passive cervical rotation
Upper Extremity Patterns
Medial Rotation-Extension (MRE) Pattern (R + L)

Instructions: Stand erect with feet together, toes pointing forward. Reach back and up spine with arm to try and touch opposite shoulder blade.
Criteria:
Touches inferior angle of contralateral scapula
Evaluating: internal rotation, extension and adduction of shoulder complex
Lateral Rotation–Abduction (LRA) Pattern (R + L)

Instructions: Stand erect with feet together, toes pointing forward. Reach behind head and down spine to touch opposite shoulder blade.
Criteria:
Touches spine of contralateral scapula
Evaluating: external rotation, flexion and abduction of the shoulder
UE Breakouts: Active pattern in prone → passive pattern in prone → supine reciprocal pattern
Multi-Segmental Patterns

Instructions: Stand erect with feet together and shoes off, toes pointing forward. Bend forward to touch toes and come back to standing.
Criteria:
Touches toes and returns to standing position
Sacral angle is > 70°
Presence of posterior weight shift (T-L junction over foot)
Uniform spinal curves
Evaluating: flexion of the hip and spine
Breakout: Single leg forward bend → toe touch in long sitting →
→ Mobility Breakout: Prone rocking OR Active straight leg raise → Passive straight leg raise → supine knee to chest
→ Stability Breakout: rolling patterns
Multi-segmental Flexion (MSF)

Instructions: Stand erect with feet together and shoes off, toes pointing forward. Bend forward to touch toes and come back to standing.
Instructions: Stand erect with feet together and shoes off, toes pointing forward. Bend forward to touch toes and come back to standing.
Criteria:
Touches toes and returns to standing position
Sacral angle is ≥ 70°
Presence of posterior weight shift (T-L junction over foot)
Uniform spinal curves
Evaluating: flexion of the hip and spine
Breakout:
Spine Extension: backward bend without UE → single leg backbend → prone press up → lumbar locked active extension → lumbar locked passive extension
Lower Body Extension: standing hip extension → prone active hip extension → prone passive hip extension → FABER → Modified Thomas Test
Stability Breakout: rolling pattern
Multi-segmental Rotation (MSR)–(R + L)

Instructions: Stand erect with feet together, shoes off, toes pointing forward. Rotate entire body as far as possible (hips, shoulders and head)
Criteria:
Pelvis rotation ≥ 50°
Trunk/Shoulder rotation ≥ 50°
No deviation of spine and pelvis
Limited knee flexion needed to achieve motion
Evaluating: rotational mobility of neck, trunk, pelvis, hips, knees and feet
Breakout:
Spine Mobility: seated rotation → lumbar locked active rotation → lumbar locked passive rotation → prone on elbow rotation
Hip Mobility: seated active hip rotation → seated passive hip rotation
Stability Breakout: rolling pattern
Single Leg Stance (R + L)

Instructions: Stand erect with feet together and shoes off then lift knee to hip and hold for 10 seconds.
Criteria:
Maintains for 10 seconds
No loss of height (bending of knee)
Evaluating: ability to stabilize independently on each leg
Breakout: vestibular and core testing → ankle ROM assessment
Overhead Squat

Instructions: Stand feet shoulder width apart with shoes off and feet pointed forward. Raise arms over head and squat as deep as possible keeping heels on floor and hands over head.
Criteria:
Maintains shoulder flexion
Maintains neutral thoracic spine (no flexion)
Femur > than parallel to floor
No sagittal plane deviation of lower extremities
Evaluating: bilateral symmetrical mobility of the hips, knees, ankles and shoulders as well as thoracic spine extension.
Breakouts: hands behind head squat → assisted squat → half-kneeling dorsiflexion → supine knees to chest
* Note: all patterns are meant to be performed with shoes off*
Appendix B
Appendix C: Interventions
| Interventions | |||||||
|---|---|---|---|---|---|---|---|
| Rx Day 1(exam) | Foam Rolling: quadriceps, hamstrings, hip flexors, glutes (1 minute each) | Standing rear foot elevated hip flexor stretch (2 × 1 min hold B/L) | Standing hamstring stretch in doorway (10 × 15 second hold B/L) | ||||
| Rx Day 2 DN: MSF, MSE, MSR, B/L cervical rotation, B/L MRE, deep squat | STM erector spinae, multifidi, thoracic-lumbar (T-L) junction 15 minutes | Manual Concentric contract-relax hamstring stretching in supine ( 2 × 5 B/L) | Standing rear foot elevated hip flexor stretch (2 × 1 min hold B/L) | High velocity manipulation of T-spine in supine (T2–T8) | Rear foot elevated MSF (2x10) | Thoracic + lumbar grade III–IV P-A glides in prone (T1–L3) 5 minutes | |
| Forefoot elevated MSE (2x10) | |||||||
| Rx Day 3 DN: MSF, MSE, MSR, B/L cervical rotation, B/L MRE, deep squat | STM erector spinae, T-L junction, posterior rotator cuff 15minutes | Supine rib rolling/thoracic rotation stretch (2x10 with 10 second hold B/L) | ✔ | ✔ | Thoracic/lumbar grade III–IV P-A glides in prine (T1–L3) 5 minutes | Banded MRE stretch in standing (10 × 15 second hold R) | |
| Rx Day 4 DN: MSF, MSE, MSR, B/L cervical rotation, B/L MRE, deep squat | STM erector spinae, posterior rotator cuff 10 minutes | Thoracic/lumbar grade III–IV P-A glides in prine (T1–L3) 5 minutes | Banded MRE stretch in standing (10 × 15 second hold R) | ½ kneeling hip flexor stretch with anterior band pull (2 × 1 min hold B/L) | Manual Concentric contract-relax hamstring stretching in supine ( 2 × 5 B/L ) | Rear foot elevated MSF (2x10) (MSF cleared) | TRX walkout shoulder extension (10 × 10 second hold) |
| Forefoot elevated MSE (2x10) (MSE cleared) | |||||||
| Rx Day 5 DN: MSF, MSE, B/L cervical rotation, R MRE, deep squat | ½ kneeling hip flexor stretch with anterior band pull (2 × 1 min hold B/L) | Self contract-relax hamstring stretch with band in prone ( 2 × 5 B/L) | Rear foot elevated MSF (2x10) (MSF cleared) | Squats to 18” bench (3 × 10) | Planks (3 × 30 seconds) | Cat-camel pelvic rotation in quadruped (1x10) | Posterior weight-shift/spine loading into stability ball in quadruped (2x10) |
| Forefoot elevated MSE (2x10) (MSE cleared) | Bird-dogs (2x10 B/L) | ||||||
| Rx Day 6 DN: B/L cervical rotation, R MRE, deep squat | ✔ | ✔ | ✔ | Planks (3 × 30 seconds) | ½ kneeling diagonal lifts with core activationwith Cook band (2 × 10 B/L) | Squats to 18” bench (3x10) | RNT banded squats with anterior pull at knee (2 × 10) |
| Rx Day 7 DN: B/L cervical rotation, R MRE | STM posterior rotator cuff and pec minor 10 minutes | Banded MRE stretch in standing (10 × 15 second hold R) | TRX walkout shoulder extension (10 × 10 second hold) | Medial shoulder rotation mobility in extension with dowel (10 × 3 second hold) | Goblet Squats to 18” bench with 12kg kettlebell(3 × 10) | Posterior weight shift patterning with dowel(2 × 10) | Deadlift latissimus activation with barbell (1x5) |
| Kettlebell deadlifts from 6” box 16kg (3 × 8) | |||||||
| Rx Day 8 DN: R MRE | Self soft tissue massage to posterior rotator cuff and pec minor with lacrosse ball 5 minutes | Horizontal shoulder adduction self stretch prone on table (5 × 15 second hold) | Banded MRE stretch in standing (10 × 15 second hold R) | ✔ | ✔ | ½ kneeling rhythmic stabilization for core control (2 × 10 B/L) | ½ kneeling diagonal lifts and chops with Cook band (2x10 B/L) |
| Rx Day 9 DN: R MRE | STM posterior rotator cuff and pec minor 10 minutes | High velocity manipulation of T-spine in supine (T2–T8) | ✔ | Barbell squats with 75 lbs (3 × 8) | Sled push with core activation with 90 lbs (4 × 100 ft) | Split squats (3 × 8 B/L) | Barbell deadlifts with 115 lbs (3x6) |
| Rx Day 10 DN: R MRE | Banded MRE stretch in standing (10 × 15 second hold R) | TRX walkout shoulder extension (10 × 10 second hold) | Medial shoulder rotation mobility in extension with dowel (10 × 3 second hold) | Single leg squats to 18” bench (3x8) | Barbell deadlifts with 115 lbs (3x6) | Single leg dead lift patterning with dowel (1x10) | Single leg dead lift to 6” box with 12kg kettlebell (3x6) |
| Rx Day 11 DN: R MRE | ✔ | ✔ | STM pec minor and posterior rotator cuff | Horizontal shoulder adduction self-stretch in prone (5 × 15 second hold) | Sled push with core activation with 90 lbs (4 × 100 ft) | Single leg dead lift to 6” box with 12kg kettlebell (3x8) | Single leg squats to 18” bench (3x10) |
| Rx Day 12 DN: R MRE, B/L cervical rotation | STM scalene and upper trapezius 10 minutes | High velocity manipulation of T-spine in prone (T2–T8) | Barbell shoulder extension stretch (2 × 6 for 5 second hold) | Core engage plank walkouts (2 × 10) | Squat Review | ||
| Rx Day 13 DN: R MRE | FMS Screen | HEP review | |||||
STM = soft tissue massage; P-A = posterior-anterior; R = right, L = left, B/L = bilateral
SFMA = Selective Functional Movement Assessment; DN = dysfunctional/non-painful; MSF = multi-segmental flexion, MSE = multi-segmental extension, MSR = multi-segmental rotation, MRE = medial rotation extension; ✔ = repeat of exercise above, FMS = Functional Movement Screen.
REFERENCES
- 1.Deyo RA Mirza SK Martin BI. Back pain prevalence and visit rates: estimates from U.S. national surveys, 2002. Spine. 2006; 31(23): 2724–2727. [DOI] [PubMed] [Google Scholar]
- 2.De Luigi AJ. Low back pain in the adolescent athlete. Phys Med and Rehabil Clin N Am. 2014; 25(4):763-88. [DOI] [PubMed] [Google Scholar]
- 3.Bhatia NN, Chow G Timon SJ, et al. Diagnostic modalities for the evaluation of pediatric back pain: a prospective study. J Pediatr Orthop. 2008; (2): 230–233. [DOI] [PubMed] [Google Scholar]
- 4.Guide to Physical Therapist Practice 3.0. American Physical Therapy Associationhttp://guidetoptpractice.apta.org/
- 5.Glaws KR Juneau CM Becker LC, et al. Intra- and inter-rater reliability of the Selective Functional Movement Assessment (SFMA). Int J Sports Phys Ther. 2014; 9(2): 195–207. [PMC free article] [PubMed] [Google Scholar]
- 6.Cook G. Movement. California: On Target Publications; 2010. [Google Scholar]
- 7.Sueki DG Cleland JA Wainner RS. A regional interdependence model of musculoskeletal dysfunction: research, mechanisms, and clinical implications. J Man Manip Ther. 2013; 21(2):90-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van Tulder MW Koes BW Bouter LM. Conservative treatment of acute and chronic nonspecific low back pain: A systematic review of randomized controlled trials of the most common interventions. Spine. 1997; 22(18): 2128–2156. [DOI] [PubMed] [Google Scholar]
- 9.Mellin G. Correlations of hip mobility with degree of back pain and lumbar spinal mobility in chronic low-back pain patients. Spine. 1988; 13(6): 668–670. [PubMed] [Google Scholar]
- 10.Molgaard C Rathleff MS Simonsen O. Patellofemoral pain syndrome and its association with hip, ankle and foot function in 16 to 18 year-old high school students: a single-blind case-control study. J Am Podiatr Med Assoc. 2011; 101(3): 215–222. [DOI] [PubMed] [Google Scholar]
- 11.Magee David J. Orthopedic Physical Assessment, 5th Edition. Missouri: Saunders Elsevier; 2008. [Google Scholar]
- 12.O'Sullivan, Susan B. & Schmitz, Thomas J. Physical Rehabilitation, 5th Edition. Philadelphia: F.A. Davis Company; 2007. [Google Scholar]
- 13.Williamson A Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005; 14(7): 798-804. [DOI] [PubMed] [Google Scholar]
- 14.Peeler JD Anderson JE. Reliability limits of the Modified Thomas Test for assessing rectus femoris muscle flexibility about the knee joint. J Athl Train. 2008; 43(5): 470–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kaltenborn FM. Manual Mobilization of the Joints: Joint Examination and Basic Treatment. Volume II, The Spine. Oslo, Norway: Norli; Minneapolis, Minnesota; 2012 [Google Scholar]
- 16.Cuthbert SC Goodheart GJ. On the reliability and validity of manual muscle testing: a literature review. Chiropr Osteopat. 2007; 15: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krebs DE Edelstein JE Fishman S. Reliability of observational kinematic gait analysis. Phys Ther. 1985; 65(7): 1027–1033. [DOI] [PubMed] [Google Scholar]
- 18.Cattley P Winyard J Trevaskis J, et al. Validity and reliability of clinical tests of the sacroiliac joint. A review of the literature. Australas Chiropr Osteopathy. 2002; 10 (2): 73–80. [PMC free article] [PubMed] [Google Scholar]
- 19.Stuber K Lerede C Kristmanson K, et al. The diagnostic accuracy of the Kemp's test: a systematic review. J Can Chiropr Assoc. 2014; 58(3): 258–267. [PMC free article] [PubMed] [Google Scholar]
- 20.Boyle M. Advances in Functional Training. California: On Target Publications; 2011. [Google Scholar]
- 21.Jeffries L.J, et al. Epidemiology of Adolescent Spinal Pain: a systematic overview of the research literature. Spine. 2007; 32(23): 2630–2637. [DOI] [PubMed] [Google Scholar]
- 22.Kiesel K Plisky PJ Voight ML. Can serious injury in professional football be predicted by a preseason Functional Movement Screen? N Am J Sports Phys Ther. 2007; 2(3): 147–158. [PMC free article] [PubMed] [Google Scholar]
- 23.Mallen CD Peat G Thomas E, et al. Prognostic Factors for Musculoskeletal Pain in Primary Care: a systematic review. Br J Gen Pract. 2007; 57(541): 655–661. [PMC free article] [PubMed] [Google Scholar]
- 24.Bronfort G Haas M Evans RL, et al. Efficacy of spinal manipulation and mobilization for low back pain and neck pain: a systematic review and best evidence synthesis. Spine J. 2004; 4(3):335-56. [DOI] [PubMed] [Google Scholar]
- 25.Janssens L McConnel AK Pijnenburg M, et al. Inspiratory muscle training affects proprioceptive use and low back pain. Med Sci Sports Exerc. 2015; 47(1):12-9. [DOI] [PubMed] [Google Scholar]
- 26.Mallen CD Peat G Thomas E, et al. Prognostic Factors for Musculoskeletal Pain in Primary Care: a systematic review. Br J Gen Pract. 2007; 57(541): 655–661. [PMC free article] [PubMed] [Google Scholar]
- 27.Kolar P Sulc J Kyncl M, et al. Postural function of the diaphragm in persons with and without chronic low back pain. J Orthop Sports Phys Ther. 2012; 42(4):352-62 [DOI] [PubMed] [Google Scholar]
- 28.Javadian Y, et al. The effects of stabilizing exercises on pain and disability of patients with lumbar segmental instability. J Back Musculoskelet Rehabil. 2012; 25(3):149-55. [DOI] [PubMed] [Google Scholar]
- 29.Bervoets DC Luijsterburg PA Alessie JJ, et al. Massage therapy has short-term benefits for people with common musculoskeletal disorders compared to no treatment: a systematic review. J Physiother. 2015; 61(3): 106–16. [DOI] [PubMed] [Google Scholar]





