Abstract
Objective
Adult alcohol abstainers have a heightened risk of premature mortality compared to light-to-moderate drinkers. We examine three plausible explanations, other than lack of alcohol, for this observed difference: Abstainers 1) have early life disadvantages that undermine long-term health; 2) lack social support; 3) are less healthy.
Method
In the National Child Development Study, an ongoing national British cohort study of individuals born in 1958, we investigated whether early life disadvantages, lack of social support, and poor physical health reduce or eliminate the elevated risk of mortality through age 51 among those abstaining from alcohol at age 33. Using Cox proportional hazard models in a stepwise approach we examined whether the alcohol-mortality relationship changed when potential confounders were included.
Results
The risk of mortality by age 51 was greater among age-33 abstainers compared to light drinkers (Hazard Ratio [HR]=2.18; 95% CI=1.40, 3.40). Including early life disadvantages and social support in the hazard models did not alter these associations (HR=2.12; 95% CI=1.27, 3.54). Including physical health in the model resulted in a 25% reduction in risk of death among abstainers, though the difference in risk remained statistically significant (HR=1.75; 95% CI=1.04, 2.94).
Conclusions
Abstaining from alcohol in early adulthood, in comparison to light drinking, predicts increased risk for premature mortality, even after accounting for numerous early and young adult confounders. Future research should examine potential moderators of this association.
Keywords: alcohol, mortality, abstention
Introduction
An inverted J-shaped curve linking adult alcohol use with concurrent and prospective health has been found in numerous studies (e.g., Klatsky, 1999; Rehm et al., 2001; Gunzerath et al., 2004; Ronksley et al., 2011). That is, light-to-moderate drinkers experience lower morbidity and mortality across numerous health indicators (e.g., chronic illness, cardiovascular disease, accidents/injuries) compared to heavy drinkers and, to a lesser extent, abstainers. A number of plausible mechanisms underlying the increased risk for poor health and mortality among adult chronic heavy alcohol users have been articulated (Bouchery et al., 2006; Rehm et al., 2009; World Health Organization, 2010). Alcohol is nutritionally unnecessary, a toxin, and addictive; and heavy episodic and chronic heavy use are associated with increased risks of fatal injury, cancer, hypertension, and stroke (e.g., Brien et al., 2014; Jayasekara et al., 2016). Thus, it is clear that chronic heavy consumption may increase risk for morbidity and mortality.
Despite substantial evidence of the dangers of heavy alcohol consumption, at least in comparison to light drinking, the increased risk of poor health and mortality among adult alcohol abstainers remains an issue of contention in the literature. Extrapolating from abstainer health “costs,” Pearson and Terry (1994) estimated that there would be approximately 80,000 additional deaths per year in the US from coronary heart disease if all alcohol use were discontinued. Such findings receive considerable media attention about the benefits of light-to-moderate alcohol use (e.g., Rabin, 2009), and health guidelines in some countries have conceded that moderate alcohol use (defined in the U.S., for example, as one drink per day for women and two for men, e.g., one 12-ounce 5% ABV beer) may be beneficial for some people or some aspects of health (USDA & USDHHS, 2015). Still, guidelines typically caution against initiating or increasing alcohol use due to the increased risk for injuries and multiple cancers (Department of Health, 2016; USDA & USDHHS, 2015) and because the degree to which confounding of this relationship has been addressed remains controversial in the literature (Chikritzhs et al., 2015; Fekjaer, 2013; Stockwell et al., 2016). Thus, the increased risk of mortality among abstainers raises important challenges for public health policy and education strategies. Below we outline three important gaps in the current literature and then state our aims and describe our analytic approach.
Abstainers have Early Life Disadvantages that Undermine Long-Term Health
The first overarching limitation in the current research is a lack of accounting for differences between adult drinkers that emerge much earlier in childhood or adolescence, which may represent the underlying causes of both alcohol use and later mortality (Corrao et al., 2000; Jackson et al., 2005; Ng Fat et al., 2014). For instance, higher cognitive performance, social adaptation, and socioeconomic status in childhood are positively linked to better long-term health and lower risk of mortality (Batty et al., 2007; Bengtsson & Mineau, 2009; Galobardes et al., 2004; Hayward & Krause, 2013; Juon et al., 2014; Power et al., 2005), as well as to light-to-moderate alcohol use in adulthood (Crum et al., 2006; Maggs et al., 2008). Therefore, the observed protective relationship between adult light-to-moderate alcohol use and mortality may reflect differences in child and early adult cognitive, social, behavioral, and economic advantages between these groups. Studies using cross-sectional or short-term follow-up designs in adulthood only are unable to account for these differences in drinking groups that may have their origins earlier in life. If such differences explain the observed higher mortality among abstainers, the apparent risk of abstention may be spurious (Batty et al., 2007; Greenfield et al., 2002; Klatsky, 2002; Smothers & Bertolucci, 2001).
Abstainers Lack Social Support
Abstaining may be associated with higher rates of mortality if abstainers have less social support than light-to-moderate drinkers (Batty et al., 2007). A lack of social support is associated with higher risk of mortality generally (Holt-Lunstad et al., 2010; House et al., 1988), with multidimensional measures of social support having a stronger relationship with health and mortality than unidimensional measures (Holt-Lunstad et al., 2010). A lack of social support is also associated with abstaining from alcohol (Klatsky, 2002; Fillmore et al., 1998) and light-to-moderate drinkers enjoy social benefits associated with their drinking (Hayward & Krause, 2013). However, social support is often not assessed in large national surveys focusing on physical health. Not considering social support as a potential confounding factor may cause selection bias in the alcohol-mortality relationship if it is a common antecedent of both abstaining and mortality risk. An important exception is the Greenfield et al. (2002) analysis of the National Alcohol Survey, which found that socially isolated individuals (i.e., those with little or no social contact) were more likely to be abstainers, but observed no effect of social isolation on the alcohol-mortality relationship. Additional research is needed to examine if social support received rather than simply social contact may serve a confounding role in the alcohol-mortality relationship. Further, scholars have not yet examined distinct dimensions of social support (e.g., instrumental vs. emotional support), which may provide additional insight into the role of social support in the alcohol-mortality relationship.
Abstainers are Less Healthy
Third, the largest body of evidence for cross-sectional, J-shaped associations with alcohol use demonstrates that abstainers report poorer physical health compared to light-to-moderate drinkers (Chikritzhs et al., 2009; Gunzerath et al., 2004; Ng Fat et al., 2014; Rehm et al., 2001). However, the direction of effects is difficult to determine because many studies have measured alcohol use and physical health concurrently or only a couple of years apart. On the one hand, abstaining could increase the risk of death. On the other, physical health in early life or adulthood may be an important driver of becoming an abstainer, such that individuals who have serious or chronic illness may be less likely to drink due to medication restrictions and other factors (i.e., “sick quitter” hypothesis [Fillmore et al., 2007; Shaper et al., 1988]). Indeed, a previous study using the National Child Development Study (NCDS) found that respondents with poorer health at age 16 and 23 were more likely to abstain from alcohol at age 33 and age 42 (Ng Fat et al., 2014). Following this important research, we also use the NCDS to assess whether prior health problems (measured before abstaining or alcohol use is initiated) account for the J-shaped mortality curve in adulthood.
The present analyses use prospective child, adolescent, and adult data from the ongoing NCDS, first to show how drinking status at age 33 predicts all-cause mortality through age 51. We focus on age-33 alcohol use because the J-shaped curve linking alcohol use and mortality does not emerge until mid-adulthood (Gunzerath et al., 2004; Romelsjo et al., 2012). We then assess whether (a) early life factors, (b) adult social support, and (c) physical illness in early life and at age 33 account for the increased risk of mortality in the subsequent two decades among abstainers.
Method
National Child Development Study (NCDS)
Data for the present study come from the NCDS, a prospective, longitudinal cohort study of all children born in Britain during one week in 1958 (Power & Elliott, 2006). The study began in infancy with a focus on perinatal mortality and has expanded to include a broader focus on development and health from early childhood to midlife. Multiple sources of data have been collected, including parent and teacher interviews, cognitive testing and school records, repeated interviews of the cohort members, and death certificates. Following the initial assessment of 17,415 infants in 1958 (99% of births), the cohort has been interviewed at ages 7, 11, 16, 23, 33, 42, 50, and 55 years. Data on mortality are available through age 51. Retention rates have remained high, with 66% taking part in the age 33 interview and over 62% taking part at age 50 (Power & Elliott, 2006; Plewis et al., 2004). Those who were not interviewed at age 33 (not included in our analyses) were more likely to be male, be an abstainer or heavy drinker at age 23 compared to a light drinker, have lower parent education, not have basic housing accommodations in childhood (e.g., indoor plumbing), report an illness at age 16, and be a smoker at age 16 and age 23. In order to reduce further potential bias from missing data (Graham, 2009), multiple imputation using Stata’s mi module (StataCorp, 2011) was used to create 10 imputed datasets for individuals who were interviewed at age 33 (n=11,469). All variables in the analysis, which had missing data ranging from 1% to 34%, were included in the imputation model. All analyses were performed using these multiply imputed data.
Measures
All-cause mortality
Mortality data were obtained from official death certificates providing vital status and the month and year of death. For five individuals, information about their death was obtained from families or neighbors during fieldwork; the exact month and year of death was not known, rather a range of years was provided. For those individuals for which the date was not known we imputed values for age of death at last date in the range, to be conservative. All deaths after 1991 (when participants were age 33) and through 2009 (age 51) were included in the analyses (n=268 deaths). Table 1 shows descriptive statistics for all variables used in the analyses.
Table 1.
Descriptive Characteristics, National Child Development Study, N=11,469
| Variable | %/Mean (SD) |
|---|---|
| Died | 2.34 |
| Age 33 drinking | |
| Abstainers | 4.50 |
| Light drinkers | 78.13 |
| Moderate drinkers | 10.22 |
| Heavy drinkers | 7.15 |
| Early Life Factors | |
| Male | 49.12 |
| Mother’s prenatal smoking | 36.80 |
| Family social class | |
| Unskilled/Semi-skilled | 37.88 |
| Skilled | 49.92 |
| Managerial/Professional | 13.20 |
| Parent education | 55.48 |
| Age 7 housing accommodations | 82.68 |
| Age 7 parent home ownership | 44.76 |
| Age 11 academic ability, unstandardized | 42.94 (16.14) |
| Age 7 social maladjustment | 7.98 (8.35) |
| Age 16 internalizing behavior | 0.38 (0.35) |
| Age 16 externalizing behavior | 0.15 (0.22) |
| Age 16 smoking | |
| Never smoker | 65.04 |
| <1pack/wk | 13.54 |
| 1 pack+/wk | 21.42 |
| Age 23 smoking | |
| Never smoker | 50.22 |
| Former smoker | 10.17 |
| Current smoker | 39.60 |
| Age 16 drinking | |
| Abstainers | 6.49 |
| Light | 40.92 |
| Mod | 31.29 |
| Heavy | 21.29 |
| Age 23 drinking | |
| Abstainers | 4.32 |
| Light drinkers | 71.15 |
| Moderate drinkers | 12.54 |
| Heavy drinkers | 11.98 |
| Education | |
| NVQ 0 | 13.36 |
| NVQ 1 | 13.81 |
| NVQ 2 | 36.35 |
| NVQ 3 | 17.31 |
| NVQ 4 | 9.99 |
| NVQ 5 or 6 | 9.19 |
| Age 23 social class | |
| Unemployed | 8.36 |
| Unskilled/Semi-skilled | 4.05 |
| Skilled | 67.28 |
| Managerial/Professional | 20.31 |
| Social Support | |
| Age 33 instrumental support | 6.70 (3.43) |
| Age 33 emotional support | 5.13 (2.53) |
| Physical Health | |
| Age 16 illness | 6.80 |
| Age 23 longstanding illness | 4.46 |
| Age 23 self-rated health (good/excellent) | 90.88 |
| Age 33 health | |
| Poor | 1.76 |
| Fair | 11.88 |
| Good | 51.99 |
| Excellent | 34.38 |
Note. NVQ= National Vocational Qualifications. SD=standard deviation.
Age 33 drinking
At age 33, respondents self-reported the total number of alcoholic drinks they had consumed in the previous seven days. This information was then summed into the total number of units of alcohol consumed, with a unit defined as approximately equal to half a pint of beer (284 ml), a small glass of wine (125 ml), or a standard pub measure of distilled spirits (25 ml). Individuals were categorized into four groups: abstaining (0 units reported), light drinking (1–14 units/week for females; 1–21 units/week for males), moderate drinking (15–28 units/week for females; 22–35 units/week for males), and heavy drinking (>28 units/week for females; >35 units/week for males). In order to be certain that abstainers at age 33 were “true” abstainers (and not just abstaining from alcohol for that particular week), we compared responses to the past week drinking question to a separate survey question that asked how often they drank (ranging on a 4-point scale from “never” to “most days”). Only abstainers who answered “never” regarding the frequency of their drinking were included in the abstainer group, which led to a large number of respondents who drank at least occasionally but reported 0 drinks in the past week to be coded as light drinkers rather than abstainers (n=4,417). Similar thresholds for light, moderate, and heavy drinking have been used in other studies examining mortality (San José et al., 1999; Klatsky et al., 2003; Rostron, 2012). Furthermore, this definition of light drinking fits with the U.S. Department of Agriculture (USDA) and Department of Health and Human Services (USDA & USDHHS, 2015) recommended guidelines for healthy drinking and is slightly less than the recommended limit from the Royal College of Physicians (2011). As shown in Table 1, 4.50% of respondents were abstaining at age 33 and 7.15% were drinking heavily. The vast majority were light (78.13%) or moderate (10.22%) drinkers.
Early life confounders
Measures assessed at child’s birth included mother’s prenatal smoking (1=mother reported smoking after the fourth month of pregnancy; 0=no smoking); family social class (categorized into three groups based upon father’s [or mother’s if father’s not known] employment: unskilled or semi-skilled, skilled, or managerial/professional position]; and parent’s education (1=either parent reported staying in school past age 15; 0=neither parent stayed past age 15). When the child was age 7, parents reported their housing accommodations (1=access to running hot water, heat, and any lavatory; 0=access to two or fewer of the accommodations) and home ownership (1=yes; 0=no) and teachers rated the child’s social maladjustment (e.g., withdrawal, hostility, restlessness) using the Bristol Social Adjustment Guide. When the child was 11, he or she was given a general academic ability test; standardized scores were used. When children were age 16, parents indicated how frequently they displayed externalizing problem behaviors (e.g., irritable; quick to fly off the handle) or internalizing problems (e.g., worries about many things; upset by new situations). In addition, adolescents self-reported their substance use. Smoking at age 16 was categorized into none, light smoker (< 1 pack [20 cigarettes] per week), or regular smoker (≥ 1 pack per week). Alcohol use at age 16 was based upon self-reported units of alcohol consumed in the previous week. Drinking levels varied by gender and reflected normative age differences and greater potential harm at younger ages (i.e., heavy drinking, >4 units in past week for females; >5 units for males).
Finally, at age 23 individual self-reported measures of educational attainment, social class, and substance use were included. Based on National Vocational Qualifications (Makepeace et al, 2003), educational attainment ranged on a six-point scale from no educational diploma (i.e., NVQ 0) to postsecondary credentials (NVQ 5 or 6). Social class was categorized into four categories based on the respondent’s profession at age 23: unskilled/semi-skilled; skilled; managerial/professional class; or unemployed. Smoking at age 23 was categorized into three groups: nonsmokers, former smokers, and current smokers. Alcohol use at age 23 was categorized in the same way as at age 33.
Adult social support as a confounder
Social support in adulthood was measured using items adapted from the British Social Attitudes Survey (Finch, 1989). At age 33, individuals were asked to nominate up to four people they could turn to in five different situations. Instrumental support was assessed with questions about (1) needing to borrow a large sum of money, (2) needing help with a household job you couldn’t do alone, and (3) being sick in bed and needing help around the house. These were summed with scores ranging from 0 to 12 (α=.82). Emotional support was assessed with questions about (1) feeling down or depressed and needing someone to talk to and (2) needing advice about an important life change, also summed with scores ranging from 0 to 8 (α=.79).
Physical health as a confounder
At age 16, parents reported whether their child had ever experienced 18 types of serious illnesses, including heart problems, epilepsy, diabetes, asthma, congenital malformations, and psychiatric disorders. This measure was dichotomized into any age 16 illness (vs. no illness). At age 23, respondents self-reported whether they had any longstanding illness. At age 23 and 33, respondents self-reported their overall health using four categories ranging from poor to excellent. At age 23, self-reported overall health was dichotomized into poor/fair vs. good/excellent because of the low number of participants reporting poor health at age 23, similar to other national studies of self-reported health and mortality (McGee et al., 1999).
Analysis
Preliminary analyses estimated a series of multinomial logistic regressions to assess the extent to which each hypothesized confounder (i.e., earlier life factors, adult social support, physical health) predicted the four drinking types at age 33 (reference category=light drinking). To test the primary questions, we then used Cox proportional hazard models to assess the unadjusted likelihood of all-cause mortality from age 33 to 51 as a function of age-33 alcohol use. Person-time was counted from age 33 until year and month of death or until age 51, and individuals who were alive in 2009 were censored at 18 years of follow up (n=204,763 person-years). These analyses proceeded in two steps. First, bivariate models evaluated the strength of association between each predictor and mortality between ages 33 and 51, independent of the other predictors. The Kaplan-Meier method and a log-rank test were used to generate survival curves and test for differences across the four age 33 drinking groups. Second, three stepwise models were estimated to examine the change in the estimated association between age 33 drinking and mortality with the sequential inclusion of three types of confounders: earlier life factors, adult social support, and physical health.
Results
Table 2 presents odds ratios and 95% confidence intervals from a series of multinomial logistic regressions estimating age-33 alcohol use as a function of each predictor. As shown in the first column, age-33 abstainers differed from light drinkers on many factors, highlighting the importance of controlling for these potential confounders in analyses predicting premature mortality. For example, abstainers had greater social maladjustment and lower academic ability at age 11; had more internalizing and externalizing problems at age 16; were more likely to have had a serious childhood illness by age 16; were more likely to be unemployed and to have lower educational attainment at age 23; and were more likely to report poor health and less instrumental and emotional social support as adults. Age-33 abstainers, compared to light drinkers, were also significantly more likely to have been abstainers at ages 16 and 23. Additionally, several factors were associated with heavy versus light drinking: being male, having lower academic ability and more social maladjustment at age 7, having greater externalizing problems at age 16, being unemployed at age 23, and having lower social support and poor health at age 33. These substantial differences between age 33 drinking groups suggest that it is important to control for early life factors, social support, and physical health in subsequent analyses.
Table 2.
Multinomial Logistic Regression Estimating the Unadjusted Odds Ratio of Young Adult Drinking Status by Early Life Predictors, Physical Health, and Social Support (Ref = Light Drinkers), N=11,469
| Abstainer | Moderate drinker | Heavy drinker | ||||
|---|---|---|---|---|---|---|
| Predictor | ORa | 95% CI | OR | 95% CI | OR | 95% CI |
| Early Life Factors | ||||||
| Male | 0.63 | 0.52, 0.76* | 2.73 | 2.40, 3.11* | 10.68 | 8.52, 13.40* |
| Mother’s prenatal smoking | 1.21 | 1.01, 1.46* | 1.12 | 0.99, 1.27 | 1.26 | 1.09, 1.46* |
| Family social class | ||||||
| Unskilled/Semi-skilled | 1.21 | 1.00, 1.46 | 0.87 | 0.76, 1.00* | 1.01 | 0.87, 1.18 |
| Skilled | Ref. | Ref. | Ref. | |||
| Managerial/Professional | 1.00 | 0.75, 1.33 | 1.17 | 0.98, 1.40 | 0.78 | 0.62, 1.00* |
| Parent education | 0.83 | 0.69, 0.99* | 1.16 | 1.03, 1.32* | 0.90 | 0.78, 1.03 |
| Age 7 housing accommodations | 0.92 | 0.72, 1.17 | 1.36 | 1.13, 1.63* | 0.89 | 0.73, 1.09 |
| Age 7 parent home ownership | 0.79 | 0.66, 0.96* | 1.10 | 0.97, 1.24 | 0.86 | 0.74, 0.99* |
| Age 11 academic ability | 0.75 | 0.68, 0.82* | 1.16 | 1.09, 1.25* | 0.90 | 0.84, 0.97 |
| Age 7 social maladjustment | 1.32 | 1.14, 1.54* | 1.05 | 0.93, 1.18 | 1.19 | 1.04, 1.36* |
| Age 16 internalizing behavior | 1.47 | 1.12, 1.94* | 0.60 | 0.49, 0.7* | 0.57 | 0.45, 0.73* |
| Age 16 externalizing behavior | 2.48 | 1.70, 3.61* | 0.88 | 0.64, 1.21 | 1.61 | 1.17, 2.21* |
| Age 16 smoking | ||||||
| Never smoker | Ref. | Ref. | Ref. | |||
| <1pack/wk | 0.73 | 0.53, 1.01 | 1.17 | 0.95, 1.45 | 1.45 | 1.14, 1.83* |
| 1 pack+/wk | 0.90 | 0.69, 1.16 | 1.66 | 1.43, 1.93** | 2.66 | 2.27, 3.13* |
| Age 23 smoking | ||||||
| Nonsmoker | Ref. | Ref. | Ref. | |||
| Former smoker | 0.83 | 0.60, 1.16 | 1.41 | 1.12, 1.78* | 2.11 | 1.62, 2.75* |
| Current smoker | 0.86 | 0.71, 1.05 | 1.57 | 1.37, 1.80* | 2.60 | 2.20, 3.08* |
| Age 16 drinking | ||||||
| Abstainers | 5.27 | 4.02, 6.91* | 0.28 | 0.16, 0.48* | 0.48 | 0.27, 0.84* |
| Light drinkers | Ref. | Ref. | Ref. | |||
| Moderate Drinkers | 1.03 | 0.77, 1.36 | 1.34 | 1.11, 1.62* | 1.25 | 0.96, 1.63 |
| Heavy drinkers | 0.64 | 0.43, 0.97* | 2.20 | 1.85, 2.62* | 2.91 | 2.29, 3.69* |
| Age 23 drinking | ||||||
| Abstainers | 21.75 | 17.06, 27.72* | 0.39 | 0.19, 0.82* | 1.13 | 0.56, 2.25 |
| Light drinkers | Ref. | Ref. | Ref. | |||
| Moderate drinkers | 0.47 | 0.26, 0.84* | 3.64 | 3.05, 4.33* | 5.44 | 4.30, 6.89* |
| Heavy drinkers | 0.65 | 0.38, 1.12 | 5.71 | 4.80, 6.79* | 16.31 | 13.41, 19.84* |
| Education | ||||||
| NVQ 0 | 1.84 | 1.45, 2.35* | 0.92 | 0.74, 1.13 | 1.21 | 0.97, 1.50 |
| NVQ 1 | 1.15 | 0.87, 1.51 | 0.97 | 0.79, 1.19 | 1.02 | 0.81, 1.28 |
| NVQ 2 | Ref. | Ref. | Ref. | |||
| NVQ 3 | 0.83 | 0.62, 1.10 | 1.30 | 1.10, 1.55* | 1.05 | 0.85, 1.29 |
| NVQ 4 | 0.87 | 0.62, 1.23 | 0.89 | 0.71, 1.13 | 0.8 | 0.61, 1.05 |
| NVQ 5 or 6 | 0.63 | 0.42, 0.95* | 1.60 | 1.31, 1.95* | 0.62 | 0.45, 0.85* |
| Age 23 social class | ||||||
| Unemployed | 1.48 | 1.06, 2.05* | 1.35 | 1.08, 1.70* | 1.72 | 1.34, 2.19* |
| Unskilled/Semi-skilled | 0.93 | 0.53, 1.63 | 0.61 | 0.33, 1.11 | 1.47 | 1.02, 2.14* |
| Skilled | Ref. | Ref. | Ref. | |||
| Managerial/Professional | 0.94 | 0.73, 1.21 | 1.21 | 1.03, 1.41* | 0.77 | 0.61, 0.98* |
| Social Support | ||||||
| Age 33 instrumental support | 0.97 | 0.95, 1.00* | 1.00 | 0.98, 1.02 | 0.96 | 0.94, 0.98* |
| Age 33 emotional support | 0.96 | 0.92, 0.99* | 0.98 | 0.95, 1.00 | 0.91 | 0.89, 0.94* |
| Physical Health | ||||||
| Age 16 illness | 1.73 | 1.17, 2.56* | 0.98 | 0.73, 1.32 | 1.04 | 0.74, 1.46 |
| Age 23 illness | 3.12 | 2.25, 4.33* | 0.81 | 0.55, 1.18 | 1.02 | 0.70, 1.47 |
| Age 23 good/excellent health | 0.39 | 0.31, 0.51* | 1.17 | 0.90, 1.51 | 0.82 | 0.64, 1.06 |
| Age 33 health | ||||||
| Poor | 3.97 | 2.62, 6.02* | 0.64 | 0.34, 1.19 | 2.16 | 1.40, 3.32* |
| Fair | 1.42 | 1.10, 1.83* | 0.89 | 0.72, 1.09 | 1.22 | 0.98, 1.52 |
| Good | Ref. | Ref. | Ref. | |||
| Excellent | 0.79 | 0.64, 0.98* | 1.06 | 0.93, 1.21 | 0.91 | 0.77, 1.07 |
Odds ratio.
p<.05.
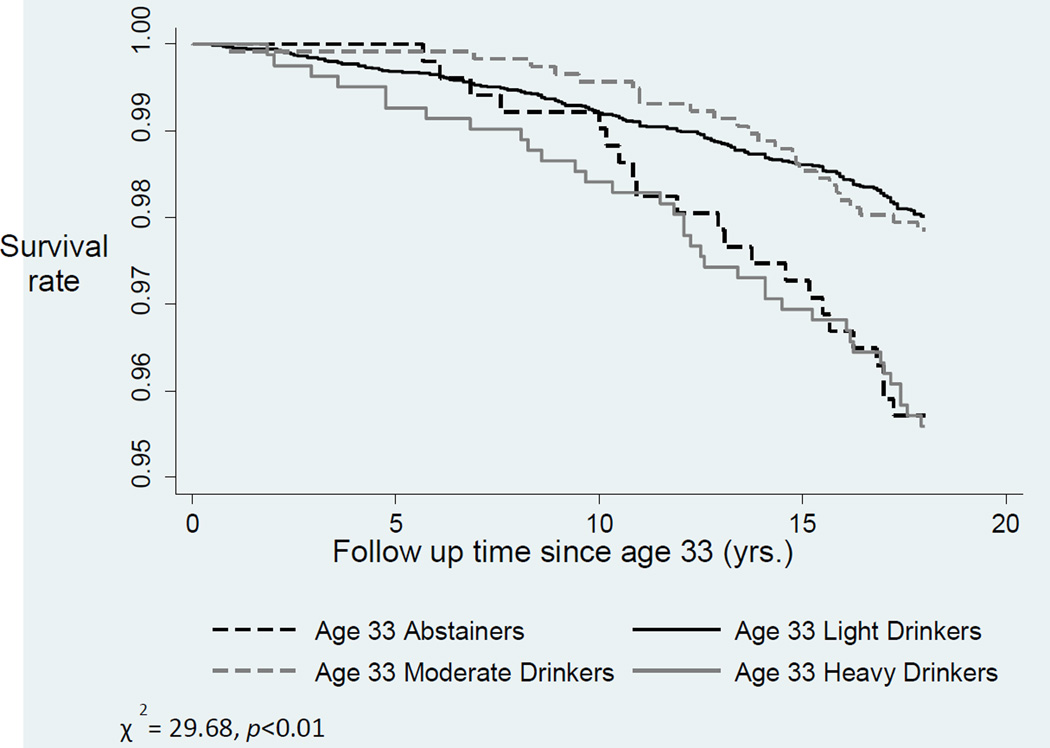
Table 3 presents unadjusted and adjusted hazard ratios of mortality. In the first (unadjusted) bivariate models (Column 1), risk of mortality was significantly higher for individuals who were classified as abstainers at age 33 compared to light drinkers (HR=2.18; 95% CI=1.40, 3.40). The risk of mortality was also significantly higher among heavy drinkers compared to light drinkers (HR=2.25; 95% CI=1.57, 3.22). The risk of mortality did not vary significantly between age 33 light drinkers and moderate drinkers. Figure 1 illustrates these differences in drinking groups with survival curves for the four drinking groups at age 33 (χ2=29.68, p<.01). Drinking at age 23 and at age 16 were not predictive of mortality between age 33 and 51. Many early life factors predicted statistically significantly greater risk of premature mortality in these bivariate analyses, including mother’s prenatal smoking; less advantaged family background as indicated by family social class, parent education, and home ownership; child lower academic ability and behavioral adjustment; adolescent and young adult smoking; and lower achieved education and employment status. Serious childhood illness, poor and fair health, and lack of instrumental and emotional social support at age 33 also predicted mortality in these bivariate models.
Table 3.
Unadjusted and Adjusted Hazard Ratios of Mortality by 4 Age 33 Drinking Types, N=11,469
| Bivariate | Model 1 | Model 2 | Model 3 | |||||
|---|---|---|---|---|---|---|---|---|
| Hazard | Hazard | Hazard | Hazard | |||||
| Predictor | Ratio | 95% CI | Ratio | 95% CI | Ratio | 95% CI | Ratio | 95% CI |
| Age 33 Drinking | ||||||||
| Abstainers | 2.1 8 | 1.40, 3.40* | 2.1 2 | 1.27, 3 .55* | 2.1 2 | 1.27, 3 .54* | 1.7 5 | 1.04, 2 .94* |
| Light drinkers | Ref. | Ref. | Ref. | Ref. | ||||
| Moderate drinkers | 1.08 | 0.71, 1.65 | 1.06 | 0.69, 1.64 | 1.07 | 0.69, 1.64 | 1.09 | 0.71, 1.68 |
| Heavy drinkers | 2.25 | 1.57, 3.22* | 1.95 | 1.30, 2.94* | 1.95 | 1.29, 2.94* | 1.90 | 1.25, 2.88* |
| Early Life Factors | ||||||||
| Male | 1.24 | 0.97, 1.58 | 1.09 | 0.83, 1.45 | 1.06 | 0.80, 1.41 | 1.06 | 0.80, 1.41 |
| Mother’s prenatal smoking | 1.35 | 1.06, 1.72* | 1.17 | 0.91, 1.50 | 1.17 | 0.91, 1.50 | 1.12 | 0.87, 1.45 |
| Family social class | ||||||||
| Unskilled/Semi-skilled | 1.4 0 | 1.09, 1.81* | 1.1 4 | 0.87, 1.49 | 1.1 4 | 0.87, 1.49 | 1.1 3 | 0.86, 1.48 |
| Skilled | Ref. | Ref. | Ref. | Ref. | ||||
| Managerial/Professional | 0.92 | 0.61, 1.40 | 1.06 | 0.68, 1.64 | 1.06 | 0.68, 1.64 | 1.09 | 0.70, 1.68 |
| Parent education | 0.77 | 0.61, 0.99* | 0.92 | 0.71, 1.19 | 0.92 | 0.71, 1.20 | 0.91 | 0.70, 1.18 |
| Housing accommodations- age 7 |
0.75 | 0.55, 1.01 | 0.87 | 0.64, 1.19 | 0.87 | 0.64, 1.20 | 0.87 | 0.63, 1.20 |
| Parent home ownership - age 7 |
0.76 | 0.58, 0.98* | 1.00 | 0.75, 1.33 | 1.00 | 0.75, 1.33 | 0.99 | 0.74, 1.32 |
| Age 11 academic ability | 0.73 | 0.64, 0.83* | 0.82 | 0.68, 0.98* | 0.82 | 0.69, 0.98* | 0.88 | 0.73, 1.05 |
| Age 7 social maladjustment | 1.32 | 1.08, 1.62* | 1.00 | 0.79, 1.27 | 0.99 | 0.78, 1.26 | 0.93 | 0.73, 1.19 |
| Age 16 internalizing behavior |
0.99 | 0.69, 1.42 | 0.98 | 0.67, 1.42 | 0.98 | 0.68, 1.43 | 0.86 | 0.59, 1.26 |
| Age 16 externalizing behavior |
2.21 | 1.33, 3.67* | 1.26 | 0.73, 2.19 | 1.24 | 0.70, 2.15 | 0.99 | 0.56, 1.75 |
| Age 16 Smoking | ||||||||
| Never smoker | Ref. | Ref. | Ref. | Ref. | ||||
| <1pack/wk | 1.24 | 0.80, 1.93 | 1.01 | 0.60, 1.70 | 1.00 | 0.60, 1.69 | 1.05 | 0.63, 1.77 |
| 1 pack+/wk | 2.03 | 1.49, 2.75* | 1.44 | 0.88, 2.36 | 1.43 | 0.88, 2.34 | 1.42 | 0.88, 2.28 |
| Age 23 smoking | ||||||||
| Nonsmoker | Ref. | Ref. | Ref. | Ref. | ||||
| Former smoker | 0.90 | 0.51, 1.59 | 0.78 | 0.43, 1.41 | 0.78 | 0.43, 1.42 | 0.79 | 0.44, 1.44 |
| Current smoker | 1.95 | 1.50, 2.54* | 1.48 | 0.98, 2.22 | 1.47 | 0.98, 2.21 | 1.37 | 0.91, 2.07 |
| Age 16 Drinking | ||||||||
| Abstainers | 0.60 | 0.29, 1.23 | 0.48 | 0.22, 1.06 | 0.47 | 0.22, 1.04 | 0.45 | 0.21, 0.97* |
| Light drinkers | Ref. | Ref. | Ref. | Ref. | ||||
| Moderate Drinkers | 0.84 | 0.56, 1.26 | 0.89 | 0.61, 1.29 | 0.89 | 0.61, 1.29 | 0.90 | 0.62, 1.32 |
| Heavy drinkers | 0.90 | 0.58, 1.40 | 0.74 | 0.49, 1.12 | 0.74 | 0.49, 1.11 | 0.74 | 0.48, 1.14 |
| Age 23 drinking | ||||||||
| Abstainers | 1.42 | 0.68, 2.30 | 1.03 | 0.51, 2.05 | 1.02 | 0.51, 2.02 | 0.99 | 0.51, 1.93 |
| Light drinkers | Ref. | Ref. | Ref. | Ref. | ||||
| Moderate drinkers | 0.97 | 0.64, 1.46 | 0.83 | 0.53, 1.28 | 0.82 | 0.53, 1.28 | 0.82 | 0.53, 1.27 |
| Heavy drinkers | 1.30 | 0.88, 1.90 | 0.88 | 0.57, 1.37 | 0.88 | 0.57, 1.37 | 0.89 | 0.57, 1.39 |
| Education | ||||||||
| NVQ 0 | 2.12 | 1.52, 2.94* | 1.34 | 0.90, 1.99 | 1.31 | 0.88, 1.94 | 1.14 | 0.76, 1.71 |
| NVQ 1 | 1.07 | 0.72, 1.59 | 0.84 | 0.56, 1.26 | 0.83 | 0.55, 1.25 | 0.81 | 0.54, 1.22 |
| NVQ 2 | Ref. | Ref. | Ref. | Ref. | ||||
| NVQ 3 | 1.07 | 0.74, 1.55 | 1.28 | 0.86, 1.89 | 1.28 | 0.87, 1.90 | 1.26 | 0.85, 1.87 |
| NVQ 4 | 0.76 | 0.45, 1.27 | 0.90 | 0.51, 1.59 | 0.91 | 0.51, 1.60 | 0.86 | 0.49, 1.51 |
| NVQ 5 or 6 | 0.86 | 0.51, 1.42 | 1.24 | 0.68, 2.26 | 1.24 | 0.68, 2.27 | 1.18 | 0.64, 2.15 |
| Age 23 social class | ||||||||
| Unemployed | 1.7 0 | 1.14, 2.53* | 1.3 4 | 0.88, 2.03 | 1.3 2 | 0.87, 2.01 | 1.2 8 | 0.85, 1.94 |
| Unskilled/Semi-skilled | 1.26 | 0.63, 2.52 | 1.04 | 0.53, 2.07 | 1.05 | 0.53, 2.08 | 0.89 | 0.44, 1.81 |
| Skilled | Ref. | Ref. | Ref. | Ref. | ||||
| Managerial/Professional | 0.88 | 0.61, 1.29 | 1.22 | 0.78, 1.90 | 1.22 | 0.78, 1.91 | 1.28 | 0.81, 2.02 |
| Social Support | ||||||||
| Age 33 instrumental support | 0.95 | 0.92, 0.99* | -- | -- | 1.00 | 0.94, 1.06 | 1.00 | 0.94, 1.06 |
| Age 33 emotional support | 0.93 | 0.89, 0.97* | -- | -- | 0.97 | 0.89, 1.05 | 0.97 | 0.89, 1.05 |
| Physical Health | ||||||||
| Age 16 illness | 2.74 | 1.87, 4.01* | -- | -- | -- | -- | 2.08 | 1.33, 3.23* |
| Age 23 illness | 2.70 | 1.76, 4.15* | -- | -- | -- | -- | 1.33 | 0.81, 2.21 |
| Age 23 good/excellent | ||||||||
| health | 0.45 | 0.33, 0.63* | -- | -- | -- | -- | 0.98 | 0.66, 1.45 |
| Age 33 health | ||||||||
| Poor | 8.14 | 5.48, 12.08* | -- | -- | -- | -- | 5.15 | 3.27, 8.10* |
| Fair | 1.67 | 1.18, 2.35* | -- | -- | -- | -- | 1.35 | 0.93, 1.95 |
| Good | Ref. | -- | -- | -- | -- | Ref. | ||
| Excellent | 0.74 | 0.54, 1.00 | -- | -- | -- | -- | 0.84 | 0.61, 1.15 |
p<.05.
Figure 1.
Kaplan-Meier Survival Estimates for Age 33 Abstainers, Light Drinkers, Moderate Drinkers, and Heavy Drinkers
To evaluate whether early life factors accounted for the observed elevated risk for premature mortality in abstainers relative to light drinkers, these variables were added to the model (Model 1). Only a small reduction in magnitude in observed differences in mortality was observed among the types of drinkers: Both abstainers and heavy drinkers evidenced higher risk of mortality (HR=2.12; 95% CI=1.27, 3.55 and HR=1.95; 95% CI=1.30, 2.94, respectively) compared to light drinkers after taking the observed early life factors into account.
Model 2 tested whether social support at age 33 accounted for this association by including this predictor along with all previous confounders from Model 1. Estimates for the risk of mortality among abstainers and heavy drinkers remained markedly similar with the addition of social support to the model. Instrumental and emotional social support were no longer significant unique predictors of premature mortality when early life factors were considered.
Finally, Model 3 tested whether physical health problems explained the associations by adding age 16, age 23, and age 33 physical health as predictors. In this case, the risk of mortality decreased in magnitude by 25.30% for abstainers and decreased by 4.42% for heavy drinkers. Despite these reductions, both abstainers and heavy drinkers remained at greater risk of mortality between ages 33 and 51 compared to light drinkers (HR=1.75; 95% CI=1.04, 2.94 and HR=1.90; 95% CI=1.25, 2.88, respectively).
Supplemental Analyses
Literature has suggested former drinkers and never drinkers may have different mortality risk (Rostron, 2012). Although lifetime abstention by age 33 was not assessed, in supplemental analyses (not shown) we compared those who reported abstaining at both age 23 and age 33 to those who only reported abstention at age 33. Those who abstained at age 33 only (former drinkers) had greater mortality risk while those who abstained at both time points did not have greater risk compared to light drinkers.
To evaluate more formally whether physical health and social support accounted for the observed elevated risk for premature mortality in abstainers relative to light drinkers (i.e., Models 2 and 3 in Table 3), in additional analyses we compared changes in the age-33 drinking effects across logistic regression models with and without age-33 physical health and social support using Karlson, Holm, and Breen’s decomposition method that compares coefficients of nested probability models (2013). The magnitude of the effect on mortality for abstainers was significantly reduced (p<.05) when physical health (see Supplemental Table 1), but not social support (see Supplemental Table 2), was included as a confounder.
Finally, given the high number of covariates included as early risk factors (i.e., Model 1 of Table 3), in additional analyses we estimated a series of alternative Cox proportional hazard models to check for over-specification (see Supplemental Table 3). That is, we estimated models that included: (1) the early life covariates in five separate blocks; (2) only a single salient covariate from each block, and (3) only early life covariates that were statistically significant (i.e., p<.05) in bivariate analyses. None of the alternative model specifications revealed substantive differences in the hazard ratios.
Discussion
The present study makes three important advances to the literature on alcohol and mortality. First, poor physical health, but not adult social support, significantly explained at least part of the increased risk of mortality seen among abstainers. Second, by using long-term prospective national data, we demonstrated that the increased risk of mortality among abstainers was not reduced when we controlled for a host of relevant early life factors that distinguished abstainers from light-to-moderate drinkers. Third, while not a primary aim, we observed that the J-shape emerged relatively early in adulthood, by age 33. The inverted J-shaped curve linking alcohol and premature mortality was not present at age 16 or 23.
Consistent with previous studies, abstainers were more likely to exhibit poorer physical health early in life. In fact, poor physical health accounted for approximately one-fourth of the increased risk for death between age 33 and 51 among abstainers (Fillmore et al., 2007; Shaper et al., 1988; Ng Fat et al., 2014). As early childhood and early adult physical health have not been prospectively accounted for previously in studies of adult alcohol use and mortality, this result further informs our understanding of the relationship between poor health and alcohol abstention.
This study was also the first of its kind to prospectively control for early life factors including family disadvantage, childhood cognitive ability, and externalizing and internalizing problems. Results suggest that while the assessed factors in early life are related both to adult drinking patterns and to mortality by age 51, they did not explain the increased risk of mortality among abstainers. Given that abstainers remain at increased risk of mortality even when accounting for self-reported physical health, social support, and early life factors, this study corroborates previous research (e.g., Fillmore et al., 2007; Jayasekara et al., 2014; Ronksley et al., 2011) and suggests that the explanation for an apparent increased mortality among abstainers does not lie solely in differences in these variables.
We also found a noteworthy difference by age in the association of drinking level with midlife mortality: Abstaining at ages 16 and age 23 was not associated with an increase in mortality risk relative to light drinkers. A Swedish cohort study of 18–20 year olds similarly found an increased risk among heavy drinkers compared to abstainers and no difference between light drinkers and abstainers (Romelsjö et al, 2012). Others have found the J-shaped curve to emerge only in midlife, leading to suggestions that age-specific healthy drinking guidelines may be appropriate (e.g., Knott et al., 2014). Further differentiation of guidelines by age, however, is not supported by others who cite insufficient evidence, residual confounding, and disadvantages of complicating public health messages (e.g., Department of Health, 2015; Lovatt et al., 2015). Currently, the only age specification made in the U.S. drinking guidelines is that they apply only to adults of legal drinking age (over 21 years; USDA & DHHS, 2015). We found that this heightened risk seemed to be specific to those who were drinkers at age 23 but abstainers at age 33, not among those abstaining at both ages, which suggests that long-term abstention from alcohol did not confer increased mortality risk, whereas individuals who drank in young adulthood but quit later had a greater risk of early death.
It appears in this study that heavy drinkers and abstainers at age 33 have roughly the same risk of mortality by age 51, suggesting a U-shaped curve in young adulthood that may shift to a J-shape in later adulthood. We speculate this may be because we are examining alcohol use in young adulthood and mortality only up to age 51. Though the relatively small number of deaths experienced by age 51 (n=268) prevented us from examining specific causes of death, extending this research further into later adulthood may demonstrate a greater risk among heavy drinkers as many alcohol-related causes of death experienced by heavy drinkers, such as liver disease, peak in the later 50s and early 60s (Office of National Statistics, 2014). Moreover, liver disease is a public health concern, particularly in the U.K., where it has been dramatically increasing and is the number one cause of alcohol-related deaths (Public Health England, 2014).
Limitations
Despite the strengths of the long-term prospective design following a national birth cohort across more than 50 years, yielding the unique ability to consider early life factors as potential confounders, there are also important limitations to note. Due to the small number of deaths by age 51 and the small number of abstainers, this study lacks sufficient power to assess differences in cause of death between abstainers and drinkers reliably. In addition, the consistently available measures of alcohol use were limited to units of alcohol consumed in the previous week, thus some individuals may be misclassified as lighter or heavier drinkers than their typical pattern. More detailed drinking histories including rigorous assessment of heavy episodic drinking, variability in patterns over time, lifetime abstention, alcohol use disorders, and reasons for quitting would allow key additional questions to be addressed (Rehm et al., 2016). Second, although our hazard models included a host of theoretically plausible confounders from birth to adulthood, unmeasured confounding variables may be underlying causes of the abstention-mortality relationship. Preliminary analyses considered additional potential confounders such as body mass index, physical activity, additional childhood academic variables, and adolescent delinquency, but none of these factors were significantly associated with either drinking or mortality and so were not included. Still, unmeasured differences between abstainers and light drinkers, including diet and other lifestyle factors, may make them more prone to illness and premature death. However, studies taking lifestyle factors into account still find a J-curve (e.g., Mukamal et al., 2006). Finally, the NCDS has prospectively followed respondents for over 50 years, and similar to many long-term longitudinal studies, some respondents were lost over time. We found that respondents who were interviewed at age 33 were different in a number of background variables versus those who were not retained. Additionally, these data come from individuals in a particular cohort born in 1958; therefore, generalizability to the full UK population and to individuals in different countries or birth cohorts may be limited.
Recommendations for drinking in the U.S. in many other countries, including the UK and Canada, recognize the complexity of making recommendations to the public about light drinking being beneficial for specific cardiovascular benefits (Department of Health, 2016; NHMRC, 2009; Stockwell et al., 2012; USDA & USDHHS, 2015), in part because even small amounts of alcohol are associated with increased risk of many types of cancers (Jayasekara et al., 2016; Klatsky et al., 2003; Nelson et al., 2013; Seitz et al., 2012). Our findings suggest that, if light-to-moderate drinking is deemed beneficial to health, public health messages should be clear regarding the possible ages at which there may be a health benefit (midlife), and equally clear about the ages where none has been documented (earlier). Future research could examine additional potential moderators of this relationship such as race/ethnicity or socioeconomic status, as it remains possible that light-to-moderate drinking is differentially detrimental or beneficial to subgroups of the population. We were not able to do so here, as noted, due to the low proportion of individuals who had died at this relatively young age. While the present results suggest that abstention in the 30s, even when accounting for early life factors and physical health, is associated with greater premature mortality risk, the noted complications along with the differences in risk found by age indicate that it may be premature to promote alcohol use, even in small amounts, for its health benefits.
Conclusion
This study contributes to the literature linking adult alcohol abstention with mortality using longitudinal birth cohort data to prospectively examine factors not previously explored, including early life factors. The alcohol-mortality relationship differed by age of alcohol use, pointing to the need for additional research to determine when in development the J-shaped curve emerges.
Supplementary Material
Highlights.
Midlife mortality risk higher for age 33 abstainers vs. light drinkers
Abstainer mortality risk lower when physical health but not social support included
Abstainer mortality risk observed among former (age 23) drinkers
Relative health costs and benefits of alcohol use may vary by age
Acknowledgments
This research and the authors were supported by grant R01AA019606 from the National Institute on Alcohol Abuse and Alcoholism (NIAAA), grant RES-579-0001 from the Economic and Social Research Council (ESRC), and grants T32DA017629 and P50DA010075 from the National Institute on Drug Abuse (NIDA). NIAAA, ESRC, and NIDA had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Batty GD, Deary IJ, Schoon I, Gale CR. Mental ability across childhood in relation to risk factors for premature mortality in adult life: the 1970 British Cohort Study. J. Epidemiol. Comm. Health. 2007;61:997–1003. doi: 10.1136/jech.2006.054494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bengtsson T, Mineau GP. Early-life effects on socio-economic performance and mortality in later life: a full life-course approach using contemporary and historical sources. Soc. Sci. Med. 2009;68:1561–1564. doi: 10.1016/j.socscimed.2009.02.012. [DOI] [PubMed] [Google Scholar]
- Bouchery EE, Harwood HJ, Sacks JJ, Simon CJ, Brewer RD. Economic costs of excessive alcohol consumption in the US, 2006. Am. J. Prev. Med. 2011;41:516–524. doi: 10.1016/j.amepre.2011.06.045. [DOI] [PubMed] [Google Scholar]
- Breen R, Karlson KB, Holm A. Total, Direct, and Indirect Effects in Logit and Probit Models. Sociol. Methods Res. 2013;42:164–191. [Google Scholar]
- Brien SE, Ronksley PE, Turner BJ, Mukamal KJ, Ghali WA. Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: systematic review and meta-analysis of interventional studies. BMJ. 2014:342. doi: 10.1136/bmj.d636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chikritzhs T, Stockwell T, Naimi T, Andreasson S, Dangardt F, Liang W. Has the leaning tower of presumed health benefits from ‘moderate’ alcohol use finally collapsed? Addiction. 2015;110:726–727. doi: 10.1111/add.12828. [DOI] [PubMed] [Google Scholar]
- Chikritzhs T, Fillmore K, Stockwell T. A healthy dose of skepticism: Four good reasons to think again about protective effects of alcohol on coronary heart disease. Drug Alcohol Rev. 2009;28:441–444. doi: 10.1111/j.1465-3362.2009.00052.x. [DOI] [PubMed] [Google Scholar]
- Corrao G, Rubbiati L, Bagnardi V, Zambon A, Poikolainen K. Alcohol and coronary heart disease: a meta-analysis. Addiction. 2000;95:1505–1523. doi: 10.1046/j.1360-0443.2000.951015056.x. [DOI] [PubMed] [Google Scholar]
- Crum RM, Juon HS, Green KM, Robertson J, Fothergill K, Ensminger M. Educational achievement and early school behavior as predictors of alcohol-use disorders: 35-year follow-up of the Woodlawn Study. J. Stud. Alcohol Drugs. 2006;67:75–85. doi: 10.15288/jsa.2006.67.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Health. UK Chief Medical Officers’ Alcohol Guidelines Review: Summary of the proposed new guidelines. 2016 Retrieved from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/489795/summary.pdf.
- Fekjaer HO. Alcohol—a universal preventive agent? A critical analysis. Addiction. 2013;108:2051–2057. doi: 10.1111/add.12104. [DOI] [PubMed] [Google Scholar]
- Fillmore K, Golding JM, Graves K, Kniep S, Leino EV, Romelsjo A, et al. Alcohol consumption and mortality. I. Characteristics of drinking groups. Addiction. 1998;93:183–203. doi: 10.1046/j.1360-0443.1998.9321834.x. [DOI] [PubMed] [Google Scholar]
- Fillmore KM, Stockwell T, Chikritzhs T, Bostrom A, Kerr W. Moderate alcohol use and reduced mortality risk: systematic error in prospective studies and new hypotheses. Ann. Epidemiol. 2007;17:s16–s23. doi: 10.1016/j.annepidem.2007.01.005. [DOI] [PubMed] [Google Scholar]
- Finch J. Kinship and friendship. In: Jowell R, Witherspoon S, Brook L, editors. British Social Attitudes: Special International Report. Gower Publishing; 1989. pp. 87–103. [Google Scholar]
- Galobardes B, Lynch JW, Smith GD. Childhood socioeconomic circumstances and cause-specific mortality in adulthood: systematic review and interpretation. Epidemiol. Rev. 2004;26:7–21. doi: 10.1093/epirev/mxh008. [DOI] [PubMed] [Google Scholar]
- Graham JW. Missing data analysis: making it work in the real world. Ann. Rev. Psychol. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- Greenfield TK, Rehm J, Rogers JD. Effects of depression and social integration on the relationship between alcohol consumption and all-cause mortality. Addiction. 2002;97:29–38. doi: 10.1046/j.1360-0443.2002.00065.x. [DOI] [PubMed] [Google Scholar]
- Gunzerath L, Faden V, Zakhari S, Warren K. National Institute on Alcohol Abuse and Alcoholism report on moderate drinking. Alcohol Clin. Exp. Res. 2004;28:829–847. doi: 10.1097/01.alc.0000128382.79375.b6. [DOI] [PubMed] [Google Scholar]
- Hayward RD, Krause N. The effect of belonging to an alcohol-proscribing religious group on the relationship between moderate alcohol consumption and mortality. Soc. Sci. Med. 2013;101:1–8. doi: 10.1016/j.socscimed.2013.10.039. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7:e1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241:540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- House of Commons Science and Technology Committee. Alcohol guidelines: eleventh report of session 2010–12. Available at: http://www.publications.parliament.uk/pa/cm201012/cmselect/cmsctech/1536/1536.pdf.
- Jackson R, Broad J, Connor J, Wells S. Alcohol and ischaemic heart disease: probably no free lunch [commentary] Lancet. 2005;366:1911–1912. doi: 10.1016/S0140-6736(05)67770-7. [DOI] [PubMed] [Google Scholar]
- Jayasekara H, English DR, Room R, MacInnis RJ. Alcohol consumption over time and risk of death: a systematic review and meta-analysis. Am. J. Epidemiol. 2014;179:1049–1059. doi: 10.1093/aje/kwu028. [DOI] [PubMed] [Google Scholar]
- Jayasekara H, MacInnis RJ, Room R, English DR. Long-term alcohol consumption and breast, upper aero-digestive tract and colorectal cancer risk: A systematic review and meta-analysis. Alcohol Alcohol. 2016;51:315–330. doi: 10.1093/alcalc/agv110. [DOI] [PubMed] [Google Scholar]
- Juon HS, Evans-Polce RJ, Ensminger ME. Early life conditions of overall and cause-specific mortality among inner-city African Americans. Am. J. Public Health. 2014;104:548–554. doi: 10.2105/AJPH.2013.301228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klatsky AL. Moderate drinking and reduced risk of heart disease. Alcohol Res. Health. 1999;23:15–24. [PMC free article] [PubMed] [Google Scholar]
- Klatsky AL. Alcohol and cardiovascular diseases. Annals New York Acad. Sci. 2002;957:7–15. doi: 10.1111/j.1749-6632.2002.tb02901.x. [DOI] [PubMed] [Google Scholar]
- Klatsky AL, Friedman GD, Armstrong MA, Kipp H. Wine, liquor, beer, and mortality. Am. J. Epidemiol. 2003;158:585–595. doi: 10.1093/aje/kwg184. [DOI] [PubMed] [Google Scholar]
- Knott CS, Coombs N, Stamatakis E, Biddulph J. All-cause mortality and the case for age-specific alcohol consumption guidelines: Pooled analyses of up to 10 population based cohorts. BMJ. 2015;350:h384. doi: 10.1136/bmj.h384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovatt M, Eadie D, Meier PS, Li J, Bauld L, Hastings G, et al. Lay epidemiology and the interpretation of low-risk drinking guidelines by adults in the United Kingdom. Addiction. 2015;110:1912–1919. doi: 10.1111/add.13072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maggs JL, Patrick ME, Feinstein L. Childhood and adolescent predictors of alcohol use and problems in adolescence and adulthood in the National Child Development Study. Addiction. 2008;103:7–22. doi: 10.1111/j.1360-0443.2008.02173.x. [DOI] [PubMed] [Google Scholar]
- Makepeace G, Dolton P, Woods L, Joshi H, Galinda-Rueda F. From school to labour market. In: Ferri E, Bynner J, Wads-Worth M, editors. Changing Britain, Changing Lives: Three Generations at the Turn of the Century. London, England: Institute of Education; 2003. [Google Scholar]
- McGee DL, Liao Y, Cao G, Cooper RS. Self-reported health status and mortality in a multiethnic US cohort. Am. J. Epidemiol. 1999;149:41–46. doi: 10.1093/oxfordjournals.aje.a009725. [DOI] [PubMed] [Google Scholar]
- Mukamal KJ, Chiuve SE, Rimm EB. Alcohol consumption and risk for coronary heart disease in men with healthy lifestyles. Arch. Intern, Med. 2006;166:2145–2150. doi: 10.1001/archinte.166.19.2145. [DOI] [PubMed] [Google Scholar]
- National Health and Medical Research Council. Australian guidelines to reduce health risks from drinking alcohol. 2009 Available at: http://www.nhmrc.gov.au/your-health/alcohol-guidelines.
- Nelson DE, Jarman DW, Rehm J, Greenfield TK, Rey G, Kerr WC, et al. Alcohol-attributable cancer deaths and years of potential life lost in the United States. Am. J. Public Health. 2013;103:641–648. doi: 10.2105/AJPH.2012.301199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng Fat L, Cable N, Marmot M, Shelton N. Persistent long-standing illness and non-drinking over time, implications for the use of lifetime abstainers as a control group. J. Epidemiol. Comm. Health. 2014;68:71–77. doi: 10.1136/jech-2013-202576. [DOI] [PubMed] [Google Scholar]
- Office of National Statistics. Liver disease biggest cause of alcohol-related deaths in England and Wales. Retrieved from: http://www.ons.gov.uk/ons/rel/subnational-health4/alcohol-related-deaths-in-the-united-kingdom/2012/sty-alcohol-releated-deaths.html.
- Pearson TA, Terry P. What to advise patients about drinking alcohol: the clinician’s conundrum. JAMA. 1994;272:967–968. [PubMed] [Google Scholar]
- Plewis I, Calderwood L, Hawkes D, Nathan G. CLS Technical Report. London, England: CLS, Institute of Education; 2004. Changes in the NCDS and BCS70 populations and samples over time. [Google Scholar]
- Power C, Hyppönen E, Smith GD. Socioeconomic position in childhood and early adult life and risk of mortality: a prospective study of the mothers of the 1958 British birth cohort. Am. J. Public Health. 2005;95:1396. doi: 10.2105/AJPH.2004.047340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Power C, Elliott J. Cohort profile: 1958 British birth cohort (National Child Development Study) Int. J. Epidemiol. 2006;35:34–41. doi: 10.1093/ije/dyi183. [DOI] [PubMed] [Google Scholar]
- Public Health England. Liver disease profiles. Available at: http://fingertips.phe.org.uk/profile/liver-disease. Updated October 2014.
- Rabin RC. Alcohol’s good for you? Some scientists doubt it. The New York Times. 2009 Jun 15; [Google Scholar]
- Rehm J, Greenfield TK, Rogers JD. Average volume of alcohol consumption, patterns of drinking, and all-cause mortality: results from the US National Alcohol Survey. Am. J. Epidemiol. 2001;153:64–71. doi: 10.1093/aje/153.1.64. [DOI] [PubMed] [Google Scholar]
- Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373:2223–2233. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- Rehm J, Roehecke M, Room R. All-cause mortality risks for “moderate drinkers”: What are the implications for burden-of-disease studies and low risk-drinking guidelines? J. Stud. Alcohol Drugs. 2016;77:203–204. doi: 10.15288/jsad.2016.77.203. [DOI] [PubMed] [Google Scholar]
- Romelsjö A, Allebeck P, Andréasson S, Leifman A. Alcohol, mortality and cardiovascular events in a 35 year follow-up of a nationwide representative cohort of 50,000 Swedish conscripts up to age 55. Alcohol Alcohol. 2012;47:322–327. doi: 10.1093/alcalc/ags021. [DOI] [PubMed] [Google Scholar]
- Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ. 2011;342:d671. doi: 10.1136/bmj.d671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rostron B. Alcohol consumption and mortality risks in the USA. Alcohol Alcohol. 2012;47:334–339. doi: 10.1093/alcalc/agr171. [DOI] [PubMed] [Google Scholar]
- Seitz HK, Pelucchi C, Bagnardi V, La Vecchia C. Epidemiology and pathophysiology of alcohol and breast cancer: Update 2012. Alcohol Alcohol. 2012;47:204–221. doi: 10.1093/alcalc/ags011. [DOI] [PubMed] [Google Scholar]
- Shaper AG, Wannamethee G, Walker M. Alcohol and mortality in British men: explaining the U-shaped curve. Lancet. 1988;332:1267–1273. doi: 10.1016/s0140-6736(88)92890-5. [DOI] [PubMed] [Google Scholar]
- Smothers B, Bertolucci D. Alcohol consumption and health-promoting behavior in a US household sample: leisure-time physical activity. J. Stud. Alcohol Drugs. 2001;62:467–476. doi: 10.15288/jsa.2001.62.467. [DOI] [PubMed] [Google Scholar]
- Stata Statistical Software: Release 12. College Station, TX: StataCorp LP; 2011. [Google Scholar]
- Stockwell T, Butt P, Beirness D, Gliksman L, Paradis C. The basis for Canada’s new low-risk drinking guidelines: A relative risk approach to estimating hazardous levels and patterns of alcohol use. Drug Alcohol Rev. 2012;31:126–134. doi: 10.1111/j.1465-3362.2011.00342.x. [DOI] [PubMed] [Google Scholar]
- Stockwell T, Zhao J, Panwar S, Roemer A, Naimi T, Chikritzhs T. Do “moderate” drinkers have reduced mortality risk? A systematic review and meta-analysis of alcohol consumption and all-cause mortality. J. Stud. Alcohol Drugs. 2016;77:185–198. doi: 10.15288/jsad.2016.77.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Agriculture & United States Department of Health and Human Services. 2015–2020. Dietary guidelines for Americans. Washington, DC: US Government Printing Office; 2015. [Google Scholar]
- World Health Organization. Global strategy to reduce harmful use of alcohol. 2010 doi: 10.2471/BLT.19.241737. Retrieved from: http://www.who.int/substance_abuse/activities/gsrhua/en/ [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.