Abstract
Purpose
To evaluate the factors affecting the bone union time and the occurrence of nonunion after intramedullary nailing of subtrochanteric femoral fractures in adults.
Materials and Methods
We retrospectively reviewed data from 31 patients (22 men and 9 women) who had undergone femoral intramedullary nailing at least 1 year post-operatively and analyzed the bone union time, nonunion rates, and factors that affected the bone union time according to the fracture classification (AO and Fielding classifications), comminution of the medial cortex, reduction method, and additional cerclage wiring.
Results
The average union time was 26.4 weeks. There were no differences in the bone union time according to the fracture classification, reduction method, or additional cerclage wiring. Significant differences were found in the bone union time between the medial cortex comminution and non-comminution groups. A relatively strong positive correlation was detected between the degree of post-operative displacement and the bone union time. Nonunion occurred in three cases and there was no failure of implants.
Conclusion
The bone union time was not affected by the reduction method nor additional cerclage wiring in intramedullary nailing of subtrochanteric femur fractures. Comminution of the medial cortex and the degree of the postoperative displacement of fractures contributed to the delayed time of union.
Keywords: Subtrochanteric fractures, Intramedullary nailing, Ununited fracture
INTRODUCTION
Femoral subtrochanteric fractures, which account for 10-34% of total hip fractures, are occurring with increasing frequency due to traffic accidents as well as a trend towards an aging population1,2,3). In general, femoral subtrochanteric fractures are caused by high energy injuries including fall and traffic accidents in young and middle-aged people and by low-energy injuries like osteoporosis in elderly populations1). The femoral subtrochanteric area is subjected to concentrated biomechanical stress and is very vulnerable to internal fixation mechanical failures. Furthermore, it is difficult to treat due to the high proportion of cortical bone (≈ 50%), a low blood flow rate, serious crush injuries associated with fractures, and heavy displacement by surrounding muscles which hampers the maintenance and reduction of fractures. Based on these anatomical characteristics, an occurrence rate of up to 20% has been reported for ununited fractures1,2).
The frequent ununited fractures and failures of internal fixation associated screw-plate device used for extramedullary fixation have led to an increased use of intramedullary nailing as an alternative. This technique is becoming a more common treatment option, as it has been associated with fewer complications, a low occurrence of ununited fractures, and better mechanical and biological outcomes1,2,3,4).
In treating fractures, it is critical to analyze factors that may impact bony union in order to evaluate prognoses and make therapeutic decisions for patients. Various risk factors for nonunion, including age, sex, history of smoking, classifications of fractures, anatomical locations of fractures, associated injuries, operation methods and techniques, and post-operative methods for rehabilitation have been identified4,5,6,7). Those factors that are subject to adjustment should be carefully reviewed when assessing aspects of patient fractures in order to select the proper operation methods and postoperative treatments. In the current study, factors influencing the time takes for bone union and the occurrence of non-union after intramedullary nailing of subtrochanteric femoral fractures were evaluated. Specifically, classifications of fractures, reduction methods, additional cerclage wiring, the degree of fracture displacement after the surgery, and comminution of the medial cortex were included and analyzed.
MATERIALS AND METHODS
Patients with femoral subtrochanteric fractures who visited Inje University Sanggye Paik Hospital (Seoul, Korea) from February 2004 to March 2013 were included. From this overall patient population, the medical records and radiographic images from 35 patients who had underwent femoral intramedullary treatment and were able to be followed-up at least one year were reviewed retrospectively. Four cases were excluded based on the study criteria.
A total of 31 patients were included (22 male and 9 female). At the time of injury, the average age of patients was 53.7 years (range, 18-78 years) and the average follow-up period was 17.5 months (range, 13-50 months). Patient injuries were attributable to fall from height (11 cases), traffic accidents (9 cases), and injuries sustained during slip (11 cases). Study exclusion criteria included a history of femoral fractures, pathologic fractures, atypical fractures, and paraplegia.
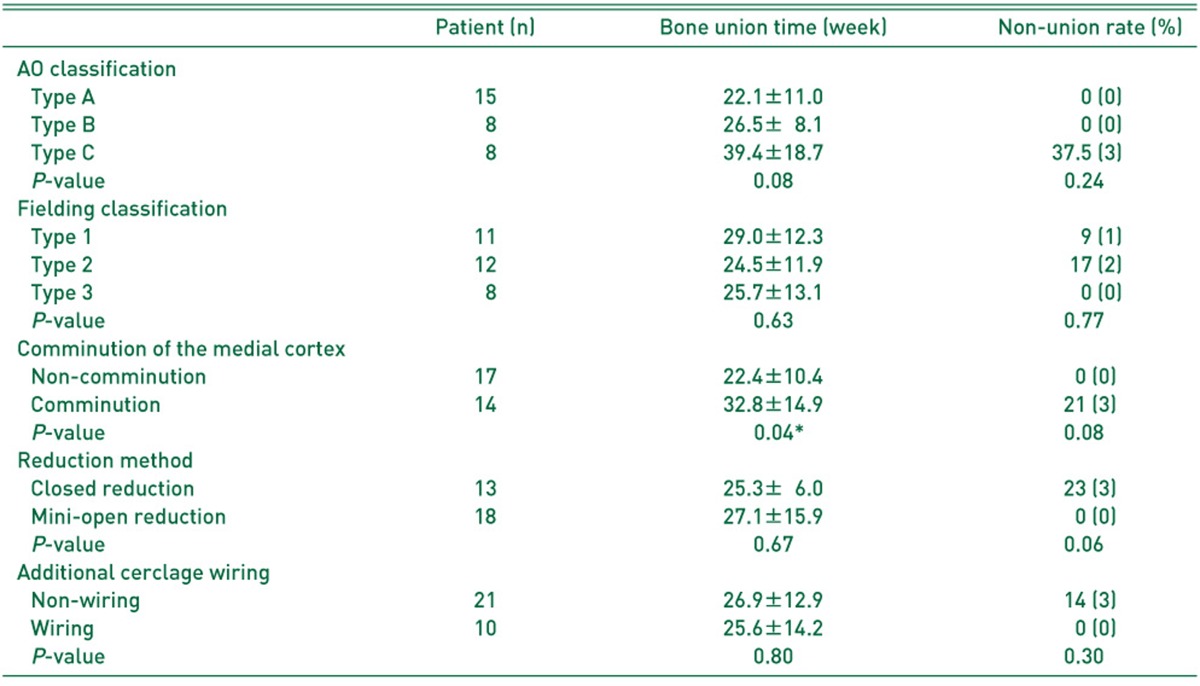
In order to analyze the effects of factors on the amount of time required for bony union and the rate of nonunion, the AO classification and the Fielding classification were utilized for the comminution and locations of fractures, respectively. In order to evaluate their effects on bony union, patients were separated into two groups based on the following conditions: comminution or non-comminution of the medial cortex, closed or mini-reduction methods of fractures, and the presence or absence of a need for additional cerclage wiring. There were 15 type A cases, eight type B cases, and eight type C cases based on AO classification and 11, 12, and eight type 1, type 2, and type 3 cases, respectively, based on the Fielding classification. Of all fracture cases, 14 exhibited comminution of the medial cortex while 17 did not. The closed reduction method was utilized in 13 cases and the remainder used the mini-open reduction method. Lastly, 10 cases required the use of cerclage wiring (Table 1).
Table 1.
Comparison of Bone Union Time and Non-union Rate
Based on AO classification, Fielding classification, comminution of the medial cortex, reduction method, and additional cerclage wiring.
The values are given as the mean±the standard deviation or percentage (number).
*P < 0.05.
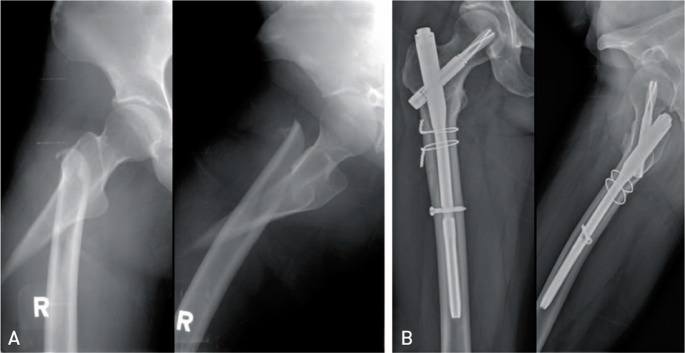
In all cases, patients were asked to lay down in a supine position on a fracture table and then a closed reduction was performed followed by intramedullary nailing via a posterolateral approach. The open reduction method was implemented for cases where the intramedullary insertion of a guide wire was not possible due to serious displacement. In cases where the reduction was either lost or expected to be lost, it was opened up to the fascia with minimizing desquamation of the soft tissue in addition to a skin incision under fluoroscopy to maintain the reduction prior to the passage of a percutaneous cerclage passer through the upper periosteum to provide additional fixation (Fig. 1). Proximal femoral nail (PFN), PFN antirotation (PFNA), and A2FN (Synthes, Paoli, Switzeland) were utilized for the surgery. Specifically, PFN, PFNA, and A2FN were used for 13, 12, and six cases, respectively. Bone grafts were not performed in any cases.
Fig. 1.
(A) A 39-year-old female with right subtrochanteric femoral fracture was treated by proximal femoral nail antirotation and additional cerclage wirings. (B) Radiographic union was achieved at 1 year follow-up.
Considering the stability of fixation as well as the degree of comminution after the surgery, patients were subjected to passive joint motion and closed kinetic chain exercises for the quadriceps femoris and gastrocnemius muscles using passive knee continuous exercise equipment over a seven day period. Partial weight bearing was allowed using crutches two to three weeks postoperatively, and whole body weight bearing was prohibited until the formation of a callus was confirmed on fractures through radiographic images.
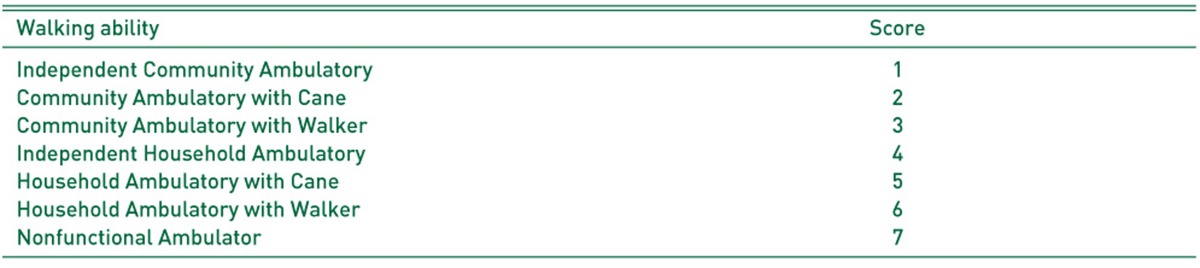
Patient walking ability was evaluated using the category of walking ability score suggested by Koval. Independent walking without any assistive devices received a score of 1 point (i.e., Independent Community Ambulatory) while those that displayed non functional ambulation received a score of 7 points (i.e., Nonfunctional Ambulator). Patients were categorized into seven stages and the differences between the time points when the injury occurred and the end of the follow-up period were analyzed8) (Table 2).
Table 2.
Koval Categories of Walking Ability
A picture archiving communication system (Marosis M-view 5.4; Marotech, Seoul, Korea) was utilized for the radiographic evaluation. Anteroposterior and lateral of hip/femur radiographic images were evaluated to detect modifications of varus/valgus deformities and the continuity of the cortical bone. The bony union was determined radiologically at least three times based on the timing of the physician's opinion regarding the cortical bone union. Clinically, the bony union was determined based on patient reports indicating a lack of oppressive pain on a fracture location and the absence of pain when their body weight was fully loaded. Radiological examinations were performed every four weeks. Fractures were deemed to be ununited if no progress of the bony union could be detected over three months from the time point at which nine months elapsed from the surgery date. The degree of displacement of fractures was measured by analyzing the shortest distance between fracture fragments shown on the anteroposterior and lateral images following the operation.
Statistical analyses were conducted using SPSS software (SPSS for Windows release 16.0; SPSS Inc., Chicago, IL, USA). Effects of comminution of the medial cortex, reduction methods for fractures, and additional cerclage wiring on the time required for bony union were tested via independent sample t-tests. The Koval walking ability score between the time points when the injury occurred and the end of the follow-up period was analyzed using paired t-tests. The amounts of time required for bony union depending on the Fielding and AO classifications were compared using the Kruskal-Wallis test. The occurrence rate of nonunion in response to the respective factor analyzed was assessed via the Fisher's exact test. A P-value <0.05 was considered to be statistically significant. The degree of displacement following the surgery and the association with time required for bony union was assessed via the Pearson correlation coefficient.
RESULTS
The average time to bony union following the operation was 26.4 weeks (range, 11-64 weeks) and the average degree of varus/valgus deformity was varus 0.45°(varus 6°-valgus 8°). No difference was noted in the Koval's walking ability score between the time points when the injury occurred and the end of the follow up-period (1.39±1.17 vs. 1.71±1.24; P=0.00). Nineteen (61%) of 31 patients were able to walk without any assistive devices.
The time to bony union tend to be longer as the AO classification worsened from type A (i.e., simple) to type C (i.e., comminution) fractures, although these differences did not reach the level of statistical significance. Similarly, no statistically significant differences were found in the time to bony union based on the fracture location Fielding classification (Table 1).
A statistically significant difference was found between the time to bony union and presence or absence of comminution of the medial cortex such that it took 22.4±10.4 weeks in the group without comminution and 32.8±14.9 weeks in the group with comminution. No further statistically significant effects of reduction methods of fractures or additional cerclage wiring on the time to bony union were noted (Table 1).
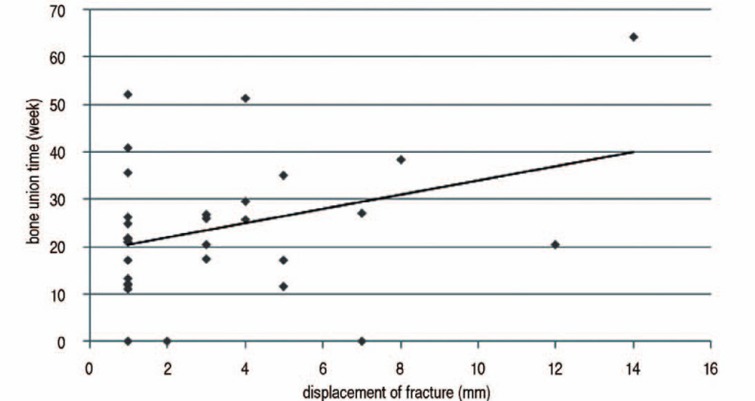
A positive correlation was detected between the postoperative displacement of fractures and the time to bony union as assessed using the Pearson correlation coefficient (Pearson's r=0.411), indicating that more serious degrees of postoperative displacement resulted in greater delays to bony union (P=0.03; Fig. 3).
Fig. 3.
Comparison of Bone Union Time and Non-union Rate
Of 31 cases, only three displayed nonunion (9.6%), and no failure of internal fixations was found. In all cases of nonunion, comminution of the medial cortex and type C comminution fractures were present. Furthermore, additional cerclage wiring treatment was not provided after the closed reduction method in all three cases. To treat the ununited fractures, autogenous bone grafts (2 cases) and intramedullary nailing exchange to plating and bone graft (1 case) were performed and achieved the bony union without additional complications (Fig. 2). None of the factors studied (AO classification, Fielding classification, comminution of the medial cortex, reduction methods for fractures, and additional cerclage wiring) influenced the occurrence of nonunion (Table 1).
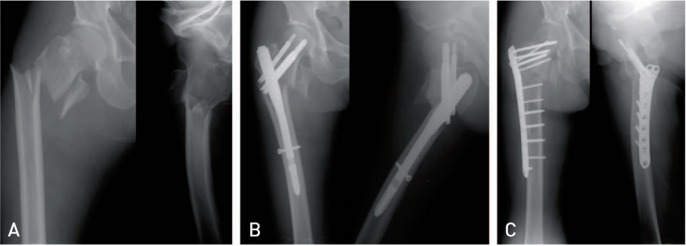
Fig. 2.
(A) A 75 year-old female with right subtrochanteric femoral fracture was injuried by traffic accident. (B) The patient was treated by proximal femoral nail after closed reduction. Postoperative radiograph at 9 months shows nonunion. (C) A follow-up radiograph at 2 years shows bone union after revision surgery with locking compression plate fixation and autogenous iliac bone graft.
DISCUSSION
In the current study, classifications reflecting comminution of fracture and anatomical locations (i.e., AO and Fielding classifications), reduction methods of fractures, and additional cerclage wiring did not influence the time to bony union of femoral subtrochanteric fractures treated with intramedullary devices. Additional study findings, however, indicated that patients with accompanying comminution of the medial cortex or serious displacement of fracture fragments tended to have longer times to bony union. Other factors, such as classification of fractures, comminution of the medial cortex, reduction methods of fractures, and additional cerclage wiring, did not impact the occurrence rate of nonunion.
In femoral subtrochanteric fractures, intramedullary nailing shortens the lever arm towards the internal fixation and thereby lowers the tensile load mechanically while providing efficient load transfer as compared to screw-plate device1,2). Anatomically, the femoral subtrochanteric area tends to be associated with poor bony union attributable to a lesser degree of vascularization as compared to surrounding regions. However, intramedullary nailing has been widely utilized as a standard treatment in this area because it results in a relatively small amount of bleeding due to the lack of desquamation of soft tissues, a low risk in infection and delayed recovery of the femoral quadriceps muscle, low occurrence rates of nonunion, malunion, and failure of internal fixations, and allows for the avoidance of bone grafting1,4).
Multiple analyses regarding whether the classification of fractures impacts the incidence of nonunion have been conducted. The results have been somewhat controversial, as some have indicated that the AO classification was significantly correlated with nonunion6,7), while others reported no difference in the occurrence rate of nonunion but an increased rate of complications5). Although results from the current study did not demonstrate statistically significant differences when cases were compared based on the AO classification (P=0.08), greater degrees of comminution of fractures were associated with longer times to bony union, suggesting that the degree of comminution was positively correlated with time to bony union.
Previous reports have indicated that the occurrence rates of nonunion and varus deformity were elevated as the distance between the location of fractures and the femur lesser trochanter increased, suggesting poor prognoses. Regarding Fielding type 2 and type 3 specifically, performance of either bone grafting or additional fixations in which the location of the fracture is more than one inch apart from the lesser trochanter are strongly recommended9). In the current study, however, conclusions regarding the effects of location of fractures on the time to bony union were difficult to draw, as no significant effect of the Fielding classification was detected.
Biomechanically, the medial cortex of the proximal femur is subjected to heavy pressure, and the continuity of the medial cortex plays an important role in securing internal fixation power. Hence, the comminution of the medial cortex is known to result in varus deformity and delayed union and failure of internal fixations suggestive of poor prognoses10,11,12,13). Therefore, maintenance of the continuity of the medial cortex and the reduction of all possible fracture fragments is recommended14,15). Results from the current study demonstrated that the group with the comminution of the medial cortex tended to have longer times to bony union and an increased occurrence rate of nonunion, indicating that it may be considered as a significant factor for assessing the unstable fractures.
In general, the primary objective of intramedullary nailing is to secure blood circulation around fractures via the closed reduction method to suport bony union16). In their early reports, Charnley17), Newton and Hohn18) suggested avoidance of the cerclage wiring fixation in parallel with the closed reduction method, as it may hinder the formation of bony callus and cause nonunion. In the subsequent reports, however, Partridge and Evans19), Fitzgerald and Southgate20) concluded that there was no association between the cerclage wiring fixation and nonunion. Recently, it was demonstrated that the minimal invasive reduction method along with percutaneous cerclage wiring in the intramedullary nailing operation resulted in satisfactory clinical outcomes for femoral subtrochanteric fractures14,21,22,23,24). Hwang et al.25) suggested that the minimal invasive open reduction method in parallel with additional fixation might be a helpful means to securing sound internal fixation as well as anatomical reduction when compared to the closed reduction method. In addition, the superiority of intramedullary nailing and the cerclage wiring method was reported in another biomechanical study26). As such, we performed the closed reduction method followed by the open reduction via minimal incision in which either internal fixation was not achievable or the reduction was unsatisfactory. In both groups, we were able to obtain favorable clinical outcomes. Furthermore, since the degree of postoperative displacement of fractures was positively correlated with the time to bony union, achieving accurate reduction in the intramedullary nailing might be useful for accomplishing bony union. Collectively, these data suggest that the minimal invasive reduction method followed by cerclage wiring fixation may achieve sound internal fixation in cases associated with a serious comminution of fracture fragments, spiral/oblique fractures, or difficult to perform reduction.
The current study had several limitations. First, it was not possible to perform a multiple regression analysis for risk factors due to the small sample size of retrospective cases available for review. Furthermore, the effects of other patient conditions or associated injuries were not taken into consideration. Therefore, additional cases examined via prospective multi-institutional studies will be necessary in order to further elucidate factors influencing time to bony union.
CONCLUSION
In the current study, factors affecting the bone union time and the occurrence of nonunion after intramedullary nailing of subtrochanteric femoral fractures in adults were evaluated. Study results indicated that classifications of fractures, reduction methods of fractures, and additional cerclage wiring fixation did not influence the time to bony union. Furthermore, cases accompanied by either the comminution of the medial cortex or a serious degree of postoperative displacement of fracture fragments resulted in delayed times to bony union as well as an increased occurrence rate of nonunion.
ACKNOWLEDGEMENTS
This work was supported by the 2013 Inje University Research Grant.
References
- 1.Lee SH. Surgical treatment of femoral subtrochanteric fracture. J Korean Hip Soc. 2006;18:430–436. [Google Scholar]
- 2.Kim JJ, Kim JW. Subtrochanteric fracture: intramedullary nailing. J Korean Fract Soc. 2009;22:114–122. [Google Scholar]
- 3.Yoon TR, Rowe SM, Song EK, Seol JY, Shin SG. Treatment of subtrochanteric fracture - Comparison of treatment efficacy according to internal fixation device. J Korean Soc Fract. 2001;14:189–199. [Google Scholar]
- 4.Shin YW, Sung YB, Choi JY, Kim M. Analysis of risk factors for nonunion after intramedullary nailing of femoral shaft fracture in adult. J Korean Fract Soc. 2011;24:313–320. [Google Scholar]
- 5.Karadimas EJ, Papadimitriou G, Theodoratos G, Papanikolaou A, Maris J. The effectiveness of the antegrade reamed technique: the experience and complications from 415 traumatic femoral shaft fractures. Strategies Trauma Limb Reconstr. 2009;4:113–121. doi: 10.1007/s11751-009-0071-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Noumi T, Yokoyama K, Ohtsuka H, Nakamura K, Itoman M. Intramedullary nailing for open fractures of the femoral shaft: evaluation of contributing factors on deep infection and nonunion using multivariate analysis. Injury. 2005;36:1085–1093. doi: 10.1016/j.injury.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 7.Taitsman LA, Lynch JR, Agel J, Barei DP, Nork SE. Risk factors for femoral nonunion after femoral shaft fracture. J Trauma. 2009;67:1389–1392. doi: 10.1097/TA.0b013e318182afd0. [DOI] [PubMed] [Google Scholar]
- 8.Koval KJ, Skovron ML, Aharonoff GB, Meadows SE, Zuckerman JD. Ambulatory ability after hip fracture. A prospective study in geriatric patients. Clin Orthop Relat Res. 1995;310:150–159. [PubMed] [Google Scholar]
- 9.Fielding JW, Magliato HJ. Subtrochanteric fractures. Surg Gynecol Obstet. 1966;122:555–560. [PubMed] [Google Scholar]
- 10.Lee KH, Kim HM, Kim YS, et al. Treatment of subtrochanteric fractures with compression hip screw. J Korean Fract Soc. 2006;19:1–5. [Google Scholar]
- 11.Kyle RF, Cabanela ME, Russell TA, et al. Fractures of the proximal part of the femur. Instr Course Lect. 1995;44:227–253. [PubMed] [Google Scholar]
- 12.Malkawi H. Bone grafting in subtrochanteric fractures. Clin Orthop Relat Res. 1982;168:69–72. [PubMed] [Google Scholar]
- 13.Fielding JW, Cochran GV, Zickel RE. Biomechanical characteristics and surgical management of subtrochanteric fractures. Orthop Clin North Am. 1974;5:629–650. [PubMed] [Google Scholar]
- 14.Park KC, Kim HS. Efficacy of percutaneous cerclage wiring in intramedullary nailing of subtrochanteric femur fracture: Technical note. J Korean Fract Soc. 2013;26:212–216. [Google Scholar]
- 15.Schatzker J, Waddell JP. Subtrochanteric fractures of the femur. Orthop Clin North Am. 1980;11:539–554. [PubMed] [Google Scholar]
- 16.Kim JW, Chang JS, Lee H, Bae JY, Kim JJ. Clinical results of femoral subtrochanteric fractures. J Korean Hip Soc. 2010;22:222–226. [Google Scholar]
- 17.Charnley J. The closed treatment of common fractures. 3rd ed. London: E & S Livingstone; 1963. [Google Scholar]
- 18.Newton CD, Hohn RB. Fracture nonunion resulting from Cerclage appliances. J Am Vet Med Assoc. 1974;164:503–508. [PubMed] [Google Scholar]
- 19.Partridge AJ, Evans PE. The treatment of fractions of the shaft of the femur using nylon cerclage. J Bone Joint Surg Br. 1982;64:210–214. doi: 10.1302/0301-620X.64B2.7068743. [DOI] [PubMed] [Google Scholar]
- 20.Fitzgerald JA, Southgate GW. Cerclage wiring in the management of comminuted fractures of the femoral shaft. Injury. 1987;18:111–116. doi: 10.1016/0020-1383(87)90185-9. [DOI] [PubMed] [Google Scholar]
- 21.Park CH, Ha CW, Park SJ, Ko MS, Shon OJ. Fixation of the femoral subtrochanteric fracture with minimally invasive reduction techniques. J Korean Fract Soc. 2013;26:112–117. [Google Scholar]
- 22.Afsari A, Liporace F, Lindvall E, Infante A, Jr, Sagi HC, Haidukewych GJ. Clamp-assisted reduction of high subtrochanteric fractures of the femur. J Bone Joint Surg Am. 2009;91:1913–1918. doi: 10.2106/JBJS.H.01563. [DOI] [PubMed] [Google Scholar]
- 23.Kennedy MT, Mitra A, Hierlihy TG, Harty JA, Reidy D, Dolan M. Subtrochanteric hip fractures treated with cerclage cables and long cephalomedullary nails: a review of 17 consecutive cases over 2 years. Injury. 2011;42:1317–1321. doi: 10.1016/j.injury.2011.03.023. [DOI] [PubMed] [Google Scholar]
- 24.Ban I, Birkelund L, Palm H, Brix M, Troelsen A. Circumferential wires as a supplement to intramedullary nailing in unstable trochanteric hip fractures: 4 reoperations in 60 patients followed for 1 year. Acta Orthop. 2012;83:240–243. doi: 10.3109/17453674.2012.665329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hwang CS, Chung PH, Kang S, et al. Treatment of subtrochanteric femur fractures using intramedullary devices. J Korean Fract Soc. 2008;21:13–18. [Google Scholar]
- 26.Müller T, Topp T, Ku¨hne CA, Gebhart G, Ruchholtz S, Zettl R. The benefit of wire cerclage stabilisation of the medial hinge in intramedullary nailing for the treatment of subtrochanteric femoral fractures: a biomechanical study. Int Orthop. 2011;35:1237–1243. doi: 10.1007/s00264-010-1204-4. [DOI] [PMC free article] [PubMed] [Google Scholar]