Abstract
Purpose
The purpose of this study was to evaluate the clinical outcome of arthroscopic treatment for recalcitrant external snapping hip.
Materials and Methods
Between September 2011 and June 2013, we evaluated 7 patients (10 cases) with snapping hip who were refractory to conservative treatments for at least 3 months. Two patients (4 cases) were impossible to adduct both knees in 90°of hip flexion. Surgery was done in lateral decubitus position, under spinal anesthesia. We made 2 arthroscopic portals to operate the patients, and used cross-cutting with flap resection technique to treat the lesion. We performed additional gluteal sling release in those 2 patients (4 cases) with adduction difficulty. Average follow-up length was 19 months (range, 12-33 months). Clinical improvement was evaluated with visual analog scale (VAS), modified Harris hip score (mHHS), and also investigated for presence of limping or other complications as well.
Results
The VAS decreased from 6.8 (range, 6-9) preoperatively to 0.2 (range, 0-2) postoperatively, and the mHHS improved from 68.2 to 94.8 after surgery. None of the patients complained of post-operative wound problem or surgical complications.
Conclusion
The clinical outcome of arthroscopic treatment for recalcitrant external snapping hip was encouraging and all patients were also satisfied with the cosmetic results.
Keywords: External snapping hip, Arthroscopy, Iliotibial band release, Gluteal sling release
INTRODUCTION
Snapping hip, also known as coxa saltans, is characterized by an audible snapping sound or sensation felt when the hip is in motion, and may be associated with pain1). Of different types, external snapping hip is accompanied by popping noise when the posterior border of the iliotibial band slides over the greater trochanter as the hip is flexed or extended, and confirmed a positive Ober's test2). Although snapping hip is usually painless, this syndrome may be painful when greater trochanteric bursitis is associated. For most cases, conservative and medical treatment showed good treatment response.
When symptoms persist despite different conservative treatment, surgical intervention is considered. Surgical treatment options are N-plasty with trochanteric bursectomy, Z-plasty and others. Although these invasive methods are effective in improving pain and snapping sound, skin incision leaves a large scar and the Trendelenburg gait may follow as a complication3,4,5,6,7,8,9,10). Ilizaliturri et al.5) obtained comparable clinical results compared to open surgical techniques by performing arthroscopic iliotibial band release in 10 patients (11 cases). Arthroscopy is increasingly performed in Korea. However, no literature has been reported on evaluating clinical results of arthroscopy for snapping hip. Therefore, this study aimed to indentify benefits of arthroscopic treatment by evaluating clinical results of iliotibial band release and gluteal sling release performed arthroscopically and comparing the results with those of previous studies.
MATERIALS AND METHODS
1. Materials
This study was performed retrospectively by including 7 snapping hip patients who underwent arthroscopic iliotibial band release and gluteal sling release by a single surgeon from September 2011 to June 2013. Subjects were 2 men and 5 women, and 3 patients had snapping hip on both sides. Surgical treatment was performed on a total of 10 cases. The mean age at the time of surgery was 35 years (range, 25-49 years), and the mean follow-up was 19 months (range, 12-33 months). The surgical intervention was done for patients who were refractory to conservative treatment for at least 3 months. All patients were previously diagnosed with snapping hip in other hospitals. The average time period from snapping sound recognition to arthroscopic treatment was 3 years (range, 2-10 years).
Repetitive pain over the greater trochanter with snapping sound was detected in all cases, and snapping sound was externally visible and audible in most cases. Some patients complained of symptoms of pseudosubluxation appearing as a subjective feeling of impending hip dislocation. Two patients (4 cases) were unable to adduct both knees in 90° of hip flexion or cross one leg over the other among patients with external snapping hip on both sides. This study excluded patients with sequelae of childhood hip disease, prior hip fractures, a history of prior hip surgery. This study also excluded patients with other hip diseases confirmed by preoperative radiographic and physical exams, and patients who underwent simultaneous arthroscopic treatment for intra-articular pathologies due to femoroacetabular impingement syndrome or other causes.
2. Surgical Procedures
All patients received surgery in lateral decubitus position, under spinal anesthesia. Two arthroscopic portals were made on the superior and inferior aspects of the greater trochanter. A trocar was inserted through a 6 mm incision made at 1 cm below to the vastus lateralis ridge, and positioned between the greater trochanter and iliotibial band to secure a space between them by gently moving the trocar. The space was maintained by injecting about 40 mL of saline solution, and the second portal was made at 1 cm above the proximal greater trochanter by inserting the arthroscope and viewing inside (Fig. 1). Like the same surgical procedure used by Ilizaliturri et al.5), a parallel incision was made to orientation of the iliotibial band, and then the iliotibial band was incised vertically before and after isolating it. Subsequently, a criss-cross pattern of incised line was made, and a diamond-shaped defect was created by gradually cutting the incised line to four directions using the shaver and high frequency ablator. The release was performed until snapping symptom disappeared through adduction movement and flexion-extension exercise of the hip intra-operatively. The findings of thickening and hyperemia in the greater trochanteric bursa were observed in all cases. Trochanteric bursectomy was done using the shaver and high frequency ablator. Additional gluteal sling release was performed in insertion of the gluteus maximus in 2 patients with hip adduction difficulty (Fig. 2).
Fig. 1.
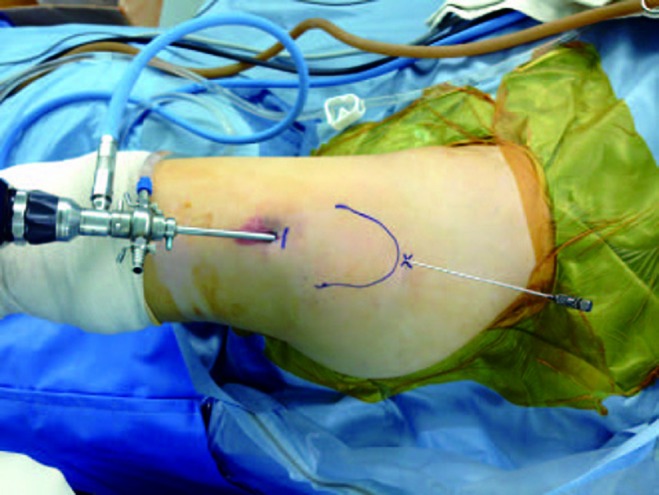
Surgeon's view of the surgical field (left hip). The patient lies in lateral decubitus position and head is to the right. Greater trochanter is delineated on the skin as a curve and two portals were used.
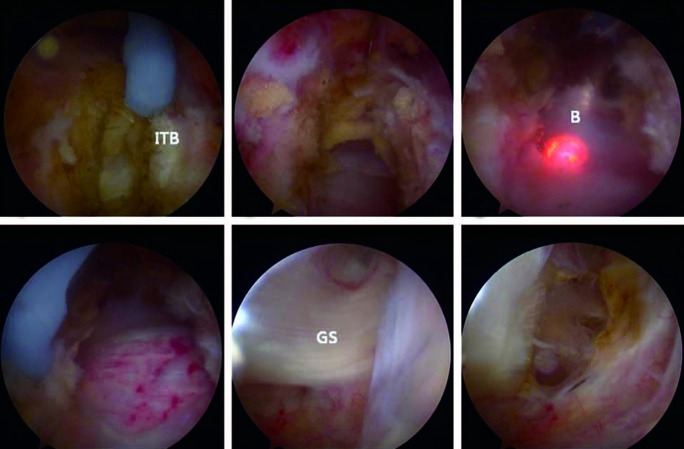
Fig. 2.
Arthroscopic images of left hip of 33-year old female patient. (A) Longitudinal cut is started on the iliotibial band (ITB) distal to the greater trochanter and directed proximally. (B) The final diamondshaped defect of the ITB. (C) Trochanteric bursa is resected through the defect using a shaver and a radiofrequency ablator. (D) Greater trochanter can be observed through the defect after bursectomy. (E) Gluteal sling of the gluteus maximus muscle, inserting to linea aspera. (F) Gluteal sling can be easily and safely released using a flexible radiofrequency ablator.
3. Postoperative Management
To reduce loading imposed to the iliotibial band and alleviate pain during ambulation, patients began ambulating using crutches on the first postoperative day without limitation of weight bearing. The subjects used a continuous passive motion (CPM) device for the first month postoperatively to prevent soft tissue adhesion around the trochanteric area and restore early range of motion in the hip. The patients were instructed to use the CPM device consistently at home after being discharged on the second postoperative day. They were instructed to ambulate using crutches for a month, and restricted from active abduction exercise over the first 6 postoperative weeks. The subjects were allowed to begin active abduction exercise after the 6 weeks, and physical activities and exercise at preoperative levels.
4. Clinical Evaluation
To evaluate the degree of clinical improvement and hip function, the visual analog scale (VAS) and modified Harris hip score (mHHS) were measured preoperatively and at the last follow-up. The presence of hip abduction weakness and ambulation abnormality was examined by performing the Trendelenburg test on the sixth postoperative week and third postoperative month. In addition, the presence of iliotibial band tear and complications such as surgical site infection was checked postoperatively, and the recurrence of limping and snapping sound was evaluated at final follow-up.
RESULTS
The VAS decreased from 6.8 (range, 6-9) preoperatively to 0.2 (range, 0-2) postoperatively, and the mHHS improved from 68.2 (range, 43-73) to 94.8 (range, 89-100) after surgery. Of 7 patients, 6 were pain-free at final follow-up, but a patient complained of mild pain at about VAS score of 2. Hip adduction angles improved from 40° and 30°, respectively, to 0°in two patients with adduction difficulty. Moreover, they were able to cross one leg over the other in a sitting position. All patients had a negative Trendelenburg's test on the sixth postoperative week, and no patient had limping at the last follow-up. All patients were satisfied with scar aesthetically, and there was no recurrence of snapping sound.
DISCUSSION
External snapping hip commonly occurs due to contracture and tension of the iliotibial band, which results in a positive Ober's test. The Ober's test is performed to identify tightness of the illiotibial band, and can be indicative for adduction difficulty when putting legs down suddenly after knee flexion at 90° and hip abduction in a lateral position. However, snapping sound can rarely occur due to contracture and tension of multiple fibrous bands of the gluteus maximus. In this case, Ober's test is negative3,9,11). Although snapping hip is usually painless, this syndrome may be painful when greater trochanteric bursitis is associated. The greater trochanteric bursa is located between the greater trochanter, belonging to insertion of the gluteus medius and origin of the vastus lateralis, and iliotibial band, and pain can be generated from inflammatory response caused by snapping12). Most patients with snapping hip show good results with stretching exercise, antiinflammatory analgesic use, or greater trochanteric bursa injection3,4,5,8,13,14). However, patients may be unable to sit cross-legged or adduct both legs in a sitting position due to pain like those with adduction difficulty in this study. When pain and discomfort persist despite conservative treatment, surgical intervention is unavoidable. Although a wide range of surgical techniques have been reported in previous literature, open surgical approaches have been most commonly introduced3,4,9,15,16). After Ilizaliturri et al.5) have addressed the result of arthroscopic treatment, successive results have been continuously reported in international studies1,8). The surgical results of previous studies varied according to authors. Although surgical management of external snapping hip showed relatively favorable results, snapping or pain persisted postoperatively in some cases requiring reoperation3,4,5,6,7,15)(Table 1). With an average of 19-month follow-up after arthroscopic surgery, snapping symptom was fully recovered with good aesthetic results in this study. Pain was improved in 90% (9 out of 10) patients. Although a patient (1 case) complained of mild pain at about VAS score of 2, the patient had no physical limitations in activities of daily living. Although specific hip arthroscopic instruments should be available to treat intra-articular pathologies, knee or shoulder-length arthroscopic tools can be used to treat snapping hip. Compared to an open Z-plasty release, arthroscopy has a disadvantage of expensive cost. Although not happened in this study, a defect which was created during iliotibial band release and not reconstructed posteoperatively had a risk of abduction weakness or depression on the surface of the thigh1).
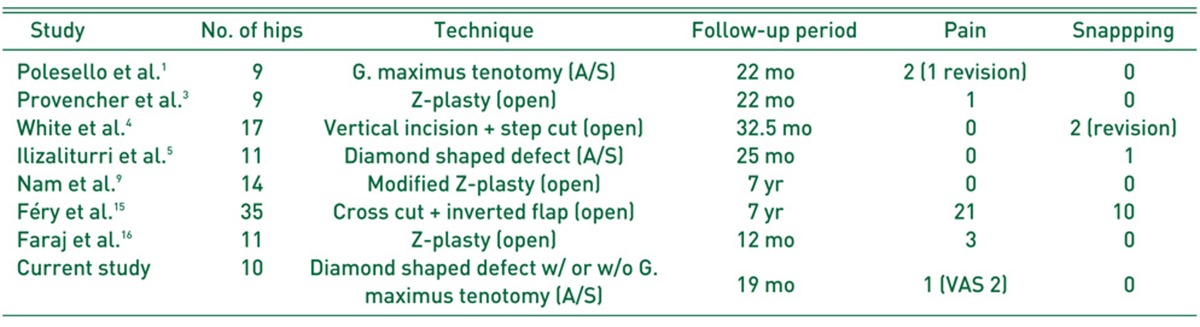
Table 1.
Literature Review
A/S: arthroscopy, VAS: visual analogue scale
Limitations of this study were the relatively small sample size and short follow-up period and a retrospective study design. Since snapping hip improves with conservative management in most patients, only a few patients are eligible to receive surgical treatment and it is difficult to include a large number of subjects7). However, the long-term follow-up is anticipated to be favorable in identifying relapse of symptoms and the risk of complications in order to prove the effectiveness of arthroscopic intervention. Another limitation was that this study did not measure hip abductor muscle strength between the affected and healthy sides before and after the surgery. Since the iliotibial band acts as a static stabilizer of the hip, a diamond-shaped release of the iliotibial band weakens abductor muscle strength of the affected side. As a result, abductor muscle strength of the healthy side can be overloaded1). Therefore, measuring abductor muscle strength of both sides pre- and post-operatively is thought to be helpful in analyzing the effect of iliotibial band release on changes in abductor muscle strength. However, this study was able to measure changes in muscle strength indirectly by regularly examining ambulation impairment caused by weakened abductor muscle strength by performing the Trendelenburg test on the sixth postoperative week and third postoperative month.
CONCLUSION
Patients with external snapping hip recalcitrant to conservative management underwent arthroscopic treatment. Despite a short mean follow-up of 19 months, all patients were highly satisfied with both clinical and cosmetic results. We anticipate the successful treatment of patients with adduction difficulty due to contracture and tension of the gluteus maximus.
References
- 1.Polesello GC, Queiroz MC, Domb BG, Ono NK, Honda EK. Surgical technique: Endoscopic gluteus maximus tendon release for external snapping hip syndrome. Clin Orthop Relat Res. 2013;471:2471–2476. doi: 10.1007/s11999-012-2636-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Teitz CC, Garrett WE, Jr, Miniaci A, Lee MH, Mann RA. Tendon problems in athletic individuals. Instr Course Lect. 1997;46:569–582. [PubMed] [Google Scholar]
- 3.Provencher MT, Hofmeister EP, Muldoon MP. The surgical treatment of external coxa saltans (the snapping hip) by Z-plasty of the iliotibial band. Am J Sports Med. 2004;32:470–476. doi: 10.1177/0363546503261713. [DOI] [PubMed] [Google Scholar]
- 4.White RA, Hughes MS, Burd T, Hamann J, Allen WC. A new operative approach in the correction of external coxa saltans: the snapping hip. Am J Sports Med. 2004;32:1504–1508. doi: 10.1177/0363546503262189. [DOI] [PubMed] [Google Scholar]
- 5.Ilizaliturri VM, Jr, Martinez-Escalante FA, Chaidez PA, Camacho-Galindo J. Endoscopic iliotibial band release for external snapping hip syndrome. Arthroscopy. 2006;22:505–510. doi: 10.1016/j.arthro.2005.12.030. [DOI] [PubMed] [Google Scholar]
- 6.Brignall CG, Stainsby GD. The snapping hip. Treatment by Z-plasty. J Bone Joint Surg Br. 1991;73:253–254. doi: 10.1302/0301-620X.73B2.2005149. [DOI] [PubMed] [Google Scholar]
- 7.Zoltan DJ, Clancy WG, Jr, Keene JS. A new operative approach to snapping hip and refractory trochanteric bursitis in athletes. Am J Sports Med. 1986;14:201–204. doi: 10.1177/036354658601400304. [DOI] [PubMed] [Google Scholar]
- 8.Ilizaliturri VM, Jr, Camacho-Galindo J. Endoscopic treatment of snapping hips, iliotibial band, and iliopsoas tendon. Sports Med Arthrosc. 2010;18:120–127. doi: 10.1097/JSA.0b013e3181dc57a5. [DOI] [PubMed] [Google Scholar]
- 9.Nam KW, Yoo JJ, Koo KH, Yoon KS, Kim HJ. A modified Z-plasty technique for severe tightness of the gluteus maximus. Scand J Med Sci Sports. 2011;21:85–89. doi: 10.1111/j.1600-0838.2009.01011.x. [DOI] [PubMed] [Google Scholar]
- 10.Jacobsen JS, Søballe K, Ulrich-Vinther M. Eccentric hip abductor weakness in patients with symptomatic external snapping hip. Scand J Med Sci Sports. 2012;22:e140–e146. doi: 10.1111/j.1600-0838.2012.01525.x. [DOI] [PubMed] [Google Scholar]
- 11.Brignall CG, Brown RM, Stainsby GD. Fibrosis of the gluteus maximus as a cause of snapping hip. A case report. J Bone Joint Surg Am. 1993;75:909–910. doi: 10.2106/00004623-199306000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Allen WC, Cope R. Coxa saltans: The snapping hip revisited. J Am Acad Orthop Surg. 1995;3:303–308. doi: 10.5435/00124635-199509000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Yoon TR, Park KS, Diwanji SR, Seo CY, Seon JK. Clinical results of multiple fibrous band release for the external snapping hip. J Orthop Sci. 2009;14:405–409. doi: 10.1007/s00776-009-1350-y. [DOI] [PubMed] [Google Scholar]
- 14.Jacobson T, Allen WC. Surgical correction of the snapping iliopsoas tendon. Am J Sports Med. 1990;18:470–474. doi: 10.1177/036354659001800504. [DOI] [PubMed] [Google Scholar]
- 15.Féry A, Sommelet J. The snapping hip. Late results of 24 surgical cases. Int Orthop. 1988;12:277–282. doi: 10.1007/BF00317824. [DOI] [PubMed] [Google Scholar]
- 16.Faraj AA, Moulton A, Sirivastava VM. Snapping iliotibial band. Report of ten cases and review of the literature. Acta Orthop Belg. 2001;67:19–23. [PubMed] [Google Scholar]