Abstract
Background
There are several techniques for harvesting the pedicled transverse rectus abdominis myocutaneous (TRAM) flap after mastectomy in breast cancer patients. We examined the whole muscle with partial sheath sparing technique and determined factors associated with its complications and oncological outcomes.
Methods
We retrospectively reviewed the results of 168 TRAM flaps performed between January 2003 and December 2010, focusing on complications and oncologic outcomes.
Results
Among the 168 pedicled TRAM flap procedures in 158 patients, flap complications occurred in 34%. Most of the flap complications included some degree of fat necrosis. There was no total flap loss. Flap complications were associated with elderly patients and the presence of major donor site complications. Abdominal bulging and hernia occurred in 12% of patients. The bi-pedicled TRAM flap and higher body mass index (BMI) were significant factors associated with increased donor site complications. Seven patients (4%) developed loco-regional recurrence. Within a median follow-up of 27 months, distant metastasis and death occurred in 6% and 4% of patients, respectively.
Conclusions
The pedicled TRAM flap using the whole muscle with partial sheath sparing technique in the present study is consistent with the results from previous studies in flap complication rates and oncological outcomes.
Keywords: Breast reconstruction, transverse rectus abdominis myocutaneous flap (TRAM flap), abdominal wall bulging, abdominal wall hernia, donor site complications
Introduction
The transverse rectus abdominis myocutaneous (TRAM) flap is the most popular technique for breast reconstruction, but its oncological effects and donor-site complications, when the rectus muscle is harvested, remain major concerns. Various modifications of surgical techniques (1), such as whole muscle with sheath pedicled TRAM flap, whole muscle with sheath sparing pedicled TRAM flap, muscle sparing pedicled TRAM flap, and free TRAM flap, have been tested, and the complications of each technique are different (2,3), with incidences ranging from 0 to 35 percent (4-9). These differences are most likely related to the various techniques of harvesting flaps and the closure of the abdominal wall. However, the most important principle of breast cancer surgery is oncological safety, which should be balanced with aesthetic outcome. The purposes of the present study were to determine the complications of whole muscle with partial sheath sparing pedicled TRAM flap, including donor site complications and flap complications, and to identify factors associated with these complications as well as oncological outcomes.
Methods
From January 2003 to December 2010, 158 patients who underwent pedicled TRAM flap procedures by the whole muscle with partial sheath sparing technique in our hospital were included in this study. Patients’ ages, weights, heights, body mass indexes (BMI), smoking histories and associated comorbidities (diabetes mellitus, hypertension, and dyslipidemia) were abstracted from the medical records. Previous abdominal surgeries, modes of reconstruction, duration of operations, and outcomes of reconstruction were also recorded. In our series, patients with previous radiotherapy or neo-adjuvant chemotherapy were also included. Patients with history of previous abdominoplasty, inadequate tissue in the lower abdomen, and substantial weight loss were excluded. Surgical outcomes focused on the incidence of abdominal hernia, bulge, fat necrosis, and flap loss. Abdominal hernia was defined as a protrusion of the abdominal wall with dehiscence of the fascial closure, while an abdominal bulge was defined as any asymmetrical abdominal contour developed after the procedure without an associated fascial defect (10,11). Mild fat necrosis was defined as any palpable firmness of less than one-third of the flap that persisted for more than 3 months after surgery without cancer recurrence, and severe fat necrosis was defined as skin and fat necrosis of more than one-third of the flap that persisted for more than 3 months after surgery without cancer recurrence. Partial flap loss was defined as skin and fat necrosis of one-third to two-thirds of the flap, and complete flap loss was defined as skin and fat necrosis of more than two thirds of the flap (3).
Operative technique
Flap elevation
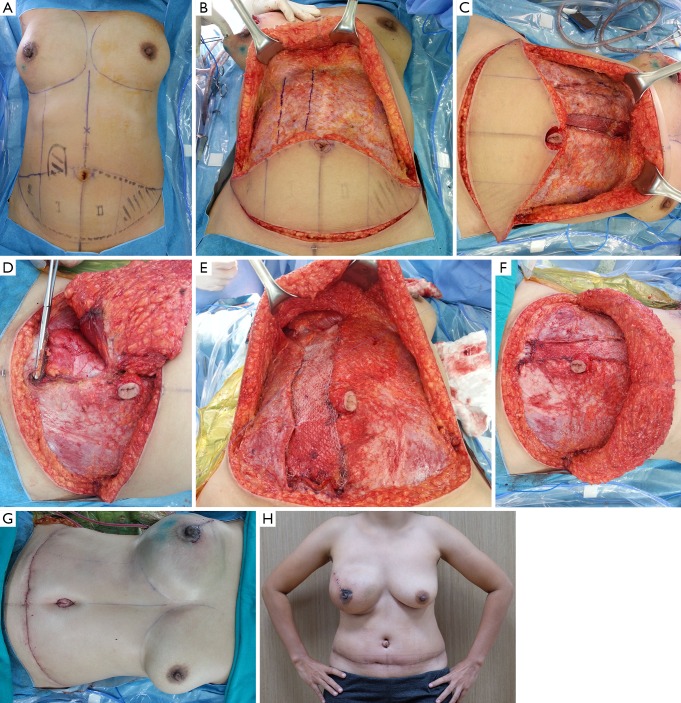
TRAM flap harvesting was performed through a standard elliptical incision of the lower abdomen (Figure 1A). We harvested the TRAM flap from lateral to medial, looking for perforators. The upper abdominal skin flap was elevated above the fascia to the level of the costal margin (Figure 1B). We routinely identified the lateral border of the rectus muscle, leaving 2 cm of the lateral anterior rectus fascia on the pedicle side and leaving 1 cm of the linea alba or the first visible perforator (Figure 1C). This preserved the linea semilunaris and its fibrous part for mesh fixation during abdominal closure. Before harvesting the flap at the cut distal edge of the rectus muscle, it was important to determine the location of the arcuate line. The incision was continued to approximately 1 cm below the arcuate line (Figure 1D). At this level, the inferior epigastric pedicle was visible and doubly clipped, while the anterior fascia and rectus abdominis were transversely divided.
Figure 1.
The operative technique of the pedicled transverse rectus abdominis myocutaneous (TRAM) flap; (A) Preoperative planning photographs showing the area of flap design and the ipsilateral muscle pedicle site; (B) the upper abdominal flap is elevated above the fascia to the level of the costal margin. The lower abdominal skin flap is designed with the suprapubic skin crease, in line with the typical transverse cesarean section incision; (C) we leave 2 cm of the lateral anterior rectus fascia on the pedicle side and leave 1 cm of the linea alba or the first visible perforator; (D) the anterior fascia and rectus abdominis are transversely divided approximately 1 cm below the arcuate line; (E) we fixed the lateral remnant of the rectus sheath with 3 or 4 interrupted sutures at the edge of posterior layer and incorporated a part of an anterior layer of the rectus sheath; (F) the abdominal fascial defects plicated in two layers at the lateral margins of the rectus sheath; (G) immediate post-operative view after the pedicled TRAM flap; (H) the one-month postoperative follow-up.
Closure of the abdominal wall defect
After dissecting the upper flap, we closed the abdominal flap without tension. The anterior sheath fascial defect was closed using polyester mesh. In most cases, we preferred to close the medial remnant of sheath primarily in layers beginning with a continuous running suture. We fixed the lateral remnant of the rectus sheath with 3 or 4 interrupted sutures at the edge of the posterior layer and incorporated a part of the anterior layer of the rectus sheath (Figure 1E). This closure goes down to the distal cut edge of the rectus muscle and up to the costal margin. All closures were reinforced with polyester mesh. The distal mesh was either fixed to the cut distal edge of the rectus muscle and the posterior rectus sheath (“technique 1”) or fixed to Cooper’s ligament (“technique 2”), depending on the surgeon’s preference. Other important points of our technique include the abdominal fascial defects plicated in two layers with a running horizontal mattress suture followed by an over and over stitch at the lateral margins of the rectus sheath over the mesh and the posterior fascia (Figure 1F,G,H).
Statistical analysis
Data analysis was performed using Stata version 12 (Stata Corp, College Station, TX, USA). Continuous variables were summarized as mean and standard deviation or median and range. Categorical variables were summarized as counts and percentage. Tests for differences between continuous variables were done using unpaired t-tests or rank tests. Differences between categorical variables were tested using chi-square tests. Factors related to various types of operative complications were identified using multiple logistic regressions. Survival after cancer treatment was estimated using the Kaplan-Meier method, and factors associated with survival were identified using Cox proportional hazards regressions. A two-side P value of 0.05 or less was considered statistically significant.
Results
The probability of disease-free and overall survival for our patients was comparable to the probabilities seen in other studies (Figures 2,3) (Table 1: mostly early breast cancer). Our patients were relatively young with normal builds (BMI <25 in 76% of patients), had very few underlying diseases, and had almost no histories of smoking. Only 27% had previous abdominal surgeries. Most had early stage breast cancer (77%). 89% of the cancers were invasive ductal carcinoma (IDC), 71% were hormone receptor-positive, 76% were HER2 negative, and only 17% were triple negative. Most patients underwent ipsilateral unilateral TRAM flap reconstruction (82%), and only 6% had bilateral TRAM (Figures 4,5,6). Chemotherapy was given in 71% of patients, of which 4% were given neoadjuvant therapy. Radiotherapy was administered in 27% of patients (Table 2).
Figure 2.
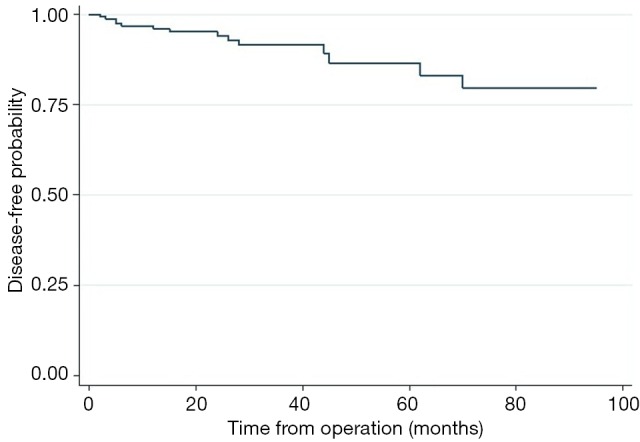
Disease-free survival of all patients in the study.
Figure 3.
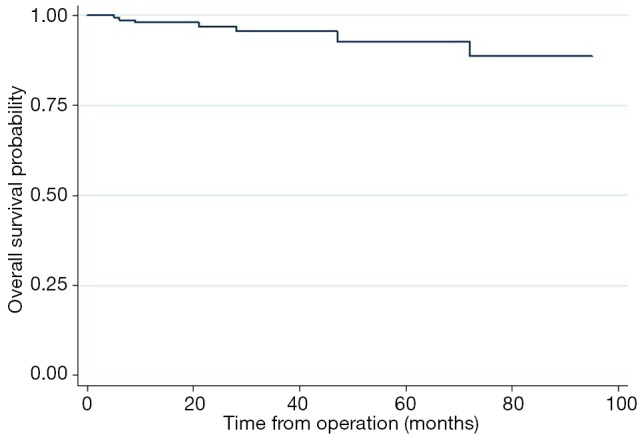
Overall survival of all patients in the study.
Table 1. Five-year survival probabilities based on the Kaplan-Meier estimates.
| Type of survival | Probability, percent (95% CI) |
|---|---|
| Disease-free survival at 5 years | 86.5 (75.4–92.9) |
| Overall survival at 5 years | 92.7 (81.8–97.2) |
Figure 4.
Presentation of right breast cancer. Moderate ptosis can be seen in the left breast. (A) Preoperative view in preparation for skin-sparing mastectomy (SSM) with pedicled transverse rectus abdominis myocutaneous (TRAM) flap at right breast and vertical mastopexy at left breast; (B) anterior view of the results at 6 weeks after performing right SSM with pedicled TRAM flap and vertical mastopexy of the opposite breast; (C) lateral view of the results at 6 weeks.
Figure 5.
Presentation of right breast cancer. Moderate ptosis can be seen in the left breast. (A) Preoperative view in preparation for skin-sparing mastectomy (SSM) with pedicled transverse rectus abdominis myocutaneous (TRAM) flap at right breast and vertical mastopexy at left breast; (B) anterior view of the results at 6 weeks after performing right SSM with pedicled TRAM flap and vertical mastopexy of the opposite breast; (C) anterior view of the results at 3 months.
Figure 6.
Postoperative view after performing right skin-sparing mastectomy (SSM) with pedicled transverse rectus abdominis myocutaneous (TRAM) flap for three patients. (A) Anterior view of the results at 3 months after performing right SSM with pedicled TRAM flap; (B) lateral view of the results at 6 months after performing right SSM with pedicled TRAM flap and nipple reconstruction; (C) anterior view of the results at 2 years after performing right SSM with pedicled TRAM flap and nipple reconstruction with tattooing.
Table 2. Summary of patient characteristics.
| Characteristic | Summary (n=158) |
|---|---|
| Age (years): mean ± SD, [range] | 43.6±7.5, [21–72] |
| BMI (kg/m2): mean ± SD, n [%] | 22.7±3.3 |
| <25 (normal, underweight) | 120 [76] |
| 25–29.9 (overweight) | 33 [21] |
| >30 (obese) | 5 [3] |
| Smoker: n [%] | 1 [1] |
| DM: n [%] | 1 [1] |
| HT: n [%] | 4 [3] |
| Previous abdominal incision: n [%] | 43 [27] |
| Low transverse | 20 [13] |
| Low midline | 12 [8] |
| Periumbilical | 8 [5] |
| Others (2 low paramedian & 1 subcostal) | 3 [2] |
| Bilateral cancer: n [%] | 5 [3] |
| Immediate reconstruction: n [%] | 140 [89] |
| Types of pedicled flaps: n [%] | |
| Ipsilateral unilateral TRAM | 130 [82] |
| Contralateral unilateral TRAM | 13 [8] |
| Bipedicled unilateral TRAM | 5 [3] |
| Bipedicled bilateral TRAM | 10 [6] |
| Operative time (minutes): mean ± SD | 288.8±60.7 |
| Length of hospital stay (days): median [range] | 7 [4–66] |
| Tumor stage (AJCC): n [%]; n=152 | |
| DCIS | 11 [7] |
| I | 49 [32] |
| II | 57 [38] |
| III & IV | 35 [23] |
| Primary tumor | |
| DCIS | 11 [7] |
| IDC (include special types) | 141 [89] |
| Phyllodes tumor | 6 [4] |
| ER positive (yes): n [%]; n=147 | 90 [61] |
| PR positive (yes): n [%]; n=147 | 87 [59] |
| HER-2/neu: n [%]; n=147 | |
| Negative (1+) | 112 [76] |
| Equivocal (2+) | 15 [10] |
| Positive (3+) | 20 [14] |
| Triple negative cancer: n [%]; n=133 | 22 [17] |
| Chemotherapy: n [%] | |
| None | 45 [29] |
| Neoadjuvant | 7 [4] |
| Adjuvant | 106 [67] |
| Radiotherapy: n [%] | 42 [27] |
| Preoperative radiotherapy | 5 [3] |
| Postoperative radiotherapy | 37 [24] |
| Mesh placement technique: n [%] | |
| No Cooper ligament sutures (technique 1) | 86 [54] |
| With Cooper ligament sutures (technique 2) | 72 [46] |
| High volume surgeon (30/year): n [%] | 99 [63] |
TRAM, transverse rectus abdominis myocutaneous; SD, standard deviation; DM, diabetes mellitus; HT, hypertension; DCIS, ductal carcinoma in situ; IDC, invasive ductal carcinoma.
Patients were observed for a median time of 27 months. Flap complications occurred in 32% of patients (Table 3), and most of these complications were some degree of fat necrosis. Extensive fat necrosis and flap necrosis requiring secondary surgery occurred in 11% of patients. Sixteen percent of patients had early donor site complications, of which 7% were seroma formations and not considered serious complications. Nine percent of patients had more serious donor site complications, which included surgical site infection and dehiscence and umbilical necrosis. Longer-term donor site complications, defined here as abdominal bulging and hernia formation, occurred in 13% of patients.
Table 3. Outcomes of interest.
| Outcome | Summary (n=158) |
|---|---|
| Follow up time (months): median [range] | 27 [2–95] |
| Early donor site complications: n [%] | |
| None | 133 [84] |
| Seroma (not serious complication) | 11 [7] |
| Wound dehiscence | 6 [4] |
| Infection | 4 [3] |
| Umbilical necrosis | 4 [3] |
| Donor site bulge or hernia: n [%] | 20 [13] |
| Total donor site complication: n [%] | 45 [28] |
| Flap complications: n [%] | |
| None | 108 [68] |
| Flap or skin necrosis | 8 [5] |
| Fat necrosis, minor | 33 [21] |
| Fat necrosis, extensive | 9 [6] |
| Total flap complication: n [%] | 50 [32] |
| Recurrence: n [%] | |
| None | 145 [92] |
| Locoregional | 5 [3] |
| Distant | 8 [5] |
| Death, any cause: n [%] | 7 [4] |
Factors related to various types of complications as identified in the present study were as follows. Flap complications were significantly associated with older ages and the presence of major donor site complications (odds ratios of 1.06 per year and 3.15, respectively) (Table 4). Higher BMI was of borderline significance. Type of flap was not related to flap complications and neither was the administration of chemotherapy or radiation therapy. High volume surgeons, defined as those performing more than 30 TRAM procedures per year, were slightly and non-significantly associated with fewer flap complications (Table 5).
Table 4. Factors related to flap complications: multiple logistic regression.
| Variable | Odds ratio (95% CI) | P value |
|---|---|---|
| Age (per year increase) | 1.06 (1.01–1.11) | 0.023 |
| Presence of major donor complications | 3.15 (1.01–9.80) | 0.048 |
Table 5. Comparison between patients with and without flap complications (n=158).
| Selected variable | No flap complications (n=108) | With complications (n=50) | P value |
|---|---|---|---|
| Age (years): mean ± SD | 42.6±6.9 | 45.7±8.4 | 0.016 |
| BMI (kg/m2): mean ± SD | 22.4±3.1 | 23.4±3.6 | 0.068 |
| Type of TRAM flaps: n [%] | 0.911 | ||
| Ipsilateral unilateral | 90 [83] | 40 [80] | |
| Contralateral unilateral | 9 [8] | 4 [8] | |
| Bipedicled unilateral | 3 [3] | 2 [4] | |
| Bipedicled bilateral | 6 [6] | 4 [8] | |
| Donor site complications: n [%] | 0.007 | ||
| None | 91 [84] | 42 [84] | |
| Wound infection or dehiscence | 3 [3] | 7 [14] | |
| Umbilicus necrosis | 3 [3] | 1 [2] | |
| Seroma | 11 [10] | 0 [0] | |
| Chemotherapy: n [%] | 0.331 | ||
| None | 31 [29] | 14 [28] | |
| Neoadjuvant | 3 [3] | 4 [8] | |
| Adjuvant | 74 [69] | 32 [64] | |
| Radiotherapy: n [%] | 30 [28] | 13 [26] | 0.815 |
| High volume surgeon: n [%] | 69 [64] | 30 [60] | 0.638 |
TRAM, transverse rectus abdominis myocutaneous; SD, standard deviation; BMI, body mass index.
Early major donor site complications were significantly related only to higher BMI (odds ratio, 1.23 per unit increase) (Tables 6,7).
Table 6. Comparison between patients with and without major donor site complications (excluding seroma) (n=158).
| Selected variable | No donor site complications [n=144] | With donor site complications [n=14] | P value |
|---|---|---|---|
| Age (years): mean ± SD | 43.5±7.6 | 44.8±6.8 | 0.542 |
| BMI (kg/m2): mean ± SD | 22.5±3.1 | 25.1±4.2 | 0.005 |
| Prior abdominal incision (yes) | |||
| N [%] | 37 [26] | 6 [43] | 0.168 |
| Type of TRAM flap: n [%] | |||
| Ipsilateral unilateral | 120 [83] | 10 [71] | 0.100 |
| Contralateral unilateral | 12 [8] | 1 [7] | |
| Bipedicled unilateral | 3 [2] | 2 [14] | |
| Bipedicled bilateral | 9 [6] | 1 [7] | |
| Flap complications: n [%] | 42 [29] | 8 [57] | 0.032 |
| Length of hospital stay (day) | |||
| Median [range] | 7 [4–66] | 7.5 [4–37] | 0.041 |
| Chemotherapy: n [%] | |||
| None | 41 [29] | 4 [29] | 0.872 |
| Neoadjuvant | 6 [4] | 1 [7] | |
| Adjuvant | 97 [67] | 9 [64] | |
| Radiotherapy: n [%] | 39 [27] | 4 [29] | 0.905 |
| Mesh technique 2: n [%] | 49 [45] | 23 [46] | 0.941 |
| High volume surgeon: n [%] | 92 [64] | 7 [50] | 0.305 |
BMI, body mass index; TRAM, transverse rectus abdominis myocutaneous; SD, standard deviation.
Table 7. Factors related to major donor site complications: multiple logistic regression.
| Variable | Odds ratio (95% CI) | P value |
|---|---|---|
| BMI (per unit increase) | 1.23 (1.06–1.43) | 0.007 |
BMI, body mass index.
Abdominal bulging or hernia occurred significantly more frequently with bipedicled unilateral TRAM (Table 8). Other factors, including type of mesh repair, BMI, age, and chemotherapy did not appear to influence bulging and hernia formation. However, the presence of a previous abdominal surgical incision was of borderline significance (Table 9). Early donor site complications appeared not to be related to later abdominal wall complications.
Table 8. Factors related to abdominal bulging or hernia: multiple logistic regression.
| Variable | Odds ratio (95% CI) | P value |
|---|---|---|
| Ipsilateral unilateral TRAM | 1.00 (reference category) | NA |
| Contralateral unilateral TRAM | 1.51 (0.30–7.50) | 0.617 |
| Bipedicled unilateral TRAM | 12.40 (1.19–80.90) | 0.008 |
| Bipedicled bilateral TRAM | 0.92 (0.11–7.82) | 0.940 |
TRAM, transverse rectus abdominis myocutaneous flap; NA, not available.
Table 9. Comparison between patients with and without abdominal wall complications (bulging and hernia) (n=158).
| Selected variable | No abdominal wall complications (n=138) | With abdominal wall complications (n=20) | P value |
|---|---|---|---|
| Age (years): mean ± SD | 43.4±7.6 | 45.2±6.9 | 0.314 |
| BMI (kg/m2): mean ± SD | 22.6±3.2 | 23.6±3.9 | 0.214 |
| Prior abdominal incision (yes): n [%] | 34 [25] | 9 [45] | 0.056 |
| Type of TRAM flap: n [%] | |||
| Ipsilateral unilateral | 116 [84] | 14 [70] | 0.013 |
| Contralateral unilateral | 11 [8] | 2 [10] | |
| Bipedicled unilateral | 2 [1] | 3 [15] | |
| Bipedicled bilateral | 9 [7] | 1 [5] | |
| Operative time (min): mean ± SD | 292.0±61.8 | 266.7±47.9 | 0.082 |
| Chemotherapy: n [%] | |||
| None | 41 [28] | 4 [200] | 0.339 |
| Neoadjuvant | 7 [5] | 0 [0] | |
| Adjuvant | 90 [65] | 16 [80] | |
| Early donor complication: n [%] | 12 [9] | 1 [10] | 0.848 |
| Mesh technique 2: n [%] | 62 [45] | 10 [50] | 0.670 |
| High volume surgeon: n [%] | 83 [69] | 16 [80] | 0.086 |
TRAM, transverse rectus abdominis myocutaneous; SD, standard deviation; BMI, body mass index.
Regarding Cox regression analysis, only tumor staging was significantly related to disease-free survival. No surgical complications were related disease-free survival (Table 10).
Table 10. Factors related to disease-free survival: univariable Cox regression.
| Variable | Hazard ratio (95% CI) | P value |
|---|---|---|
| Staging (per higher stage) | 3.00 (1.39–6.50) | 0.005 |
| Flap complications | 1.87 (0.65–5.43) | 0.249 |
| Major donor site complication | 0.98 (0.13–7.60) | 0.987 |
| Abdominal bulging or hernia | 0.38 (0.05–2.96) | 0.358 |
| Triple negative tumor (n=133) | 1.83 (0.50–6.72) | 0.360 |
Discussion
In our series, few patients had histories of smoking with few comorbidities, when compared with patients in other studies from Western countries (1,3,12). The oncologic outcomes (DFS, OS, and locoregional recurrent rate) of breast cancer patients who underwent pedicled TRAM flap were not different when compared with the oncologic outcomes of breast conserving surgery or mastectomy (13-15). Oncologically, therefore, pedicled TRAM flap is a safe option for breast cancer patients after mastectomy.
The overall incidence of TRAM flap complications was 34% in the present study, a rate similar to the rates seen in previous reports, which ranged from 24.6% to 55.4% for pedicled TRAM flaps (1-3,12,16), and from 23.4% to 49.3% for free TRAM flaps (2,3,17) (Table 11). The overall incidence of fat necrosis in our series was 32%, a rate higher than the 14.2% in a large series reported by Kim et al. (16). This difference might be because we kept zones 1–3 of the TRAM flap in most patients, whereas in the study of Eun Key Kim et al., only zones 1 and 3, which had better blood supply, were used for reconstruction.
Table 11. Comparative total complication of various technique of TRAM flap that published after 2000.
| Study/year | Type of study | Number of flaps | Flap technique | Donor complication (%) | Flap complication (%) | ||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Bulge/Hernia | Total | Fat necrosis/partial flap loss | Flap loss | |||||
| Alderman et al. [2002] (2) | Prospective | 190 | Pedicled TRAM | 19.0 | 7.8 | 32.9 | 16.2 | 1.10 | |
| 77 | Free TRAM | 17.9 | 11.9 | 49.3 | 14.9 | 1.50 | |||
| Ducic et al. [2005] (1) | Retrospective | 224 | Muscle sparing pedicle TRAM | 38.0 | 1.5 | 55.4 | 26.8 | 0.90 | |
| Ascherman et al. [2008] (12) | Retrospective | 117 | Whole muscle with sheath sparing pedicled TRAM | 7.7 | 2.6 | NR | NR | NR | |
| Andrades et al. [2008] (3) | Retrospective | 207 | Pedicled TRAM | 29.9 | 7.5 | 42.9 | 18.4 | 1.00 | |
| 192 | Free TRAM | 24.7 | 3.9 | 23.4 | 7.7 | 0.00 | |||
| Sailon et al. [2009] (17) | Systematic review (six studies) | 812 | Free TRAM | NR | 11.3 | NR | 12.9 | 1.59 | |
| Systematic review (five studies) | 329 | Free DIEP | NR | 8.1 | NR | 29.0 | 4.15 | ||
| Kim et al. [2009] (16) | Retrospective | 500 | Whole muscle with sheath sparing pedicled TRAM | 16.4 | 3.0 | 24.6 | 14.2 | 0.20 | |
| Ramathibodi Hospital, 2012 | Retrospective | 168 | Whole muscle with sheath pedicled TRAM | 34.0 | 12.0 | 34.0 | 32.0 | 0.00 | |
TRAM, transverse rectus abdominis myocutaneous flap; NR, not recorded.
The overall incidence of donor site complications was 34% in the present study, a rate similar to those seen in previous reports, which ranged from 7.7% to 38% of pedicled TRAM flaps and from 17.9% to 24.7% of free TRAM flaps. The overall incidence of bulging or hernia in our series was 12%, higher than those seen in previous reports, which were from 1.5% to 7.8% of pedicled TRAM flaps, and from 3.9% to 11.9% of free TRAM flaps. The incidence of bulging or hernia in our series was higher than that reported by Kim et al. (16), which found an incidence of only 3%. The high incidence in our series could be due to a higher proportion of bilateral pedicled TRAM flaps (9.5% vs. 1%). No patient in the present series developed mesh infections or required mesh removal.
Risk factors related to flap complications identified in the present study included older ages and the presence of major donor site complications (odds ratios of 1.06 per year and 3.15, respectively). Donor site complications were not causally related to flap complications, but rather both complications shared common risk factors. Higher BMI was of borderline significance—a result also found in previous studies (1,18). Preoperative radiation therapy was not related to flap complications in the present study, which may be due to our use of a contralateral TRAM flap for reconstruction. Our findings thus confirmed that postoperative radiotherapy did not increase the risk of flap complications. Prior abdominal incisions, such as lower transverse, lower paramedian, lower midline, or periumbilical incisions, were not related to flap complications, a result also similar those seen in previous reports (19). However, in patients with prior lower midline incision, we preferred to excise zones 2 and 4 of the TRAM flap to decrease the incidence of flap necrosis.
Early major donor site complications were significantly related only to higher BMI (odds ratio, 1.23 per unit increase), corroborating the findings in previous reports (1,18). No other factors, besides the presence of flap complications, which were noted previously, were of significance. One type of flap reconstruction, the bi-pedicled unilateral TRAM flap, had a relatively higher donor complication rate, but the number of such flaps performed was too small to draw generalizations from. Chemotherapy administration was not related to early donor site complications.
Abdominal bulging or hernia occurred significantly more frequently in bipedicled unilateral TRAM flaps, possibly because patients in this group had prior lower midline incisions as well as more extensive surgeries. However, with such a small number of patients, this finding could also be chance. Although the presence of a previous abdominal surgical incision was of borderline significance in relation to bulging or hernia, the surgeon must be more careful when operating on patients with previous abdominal surgeries.
Limitations of the present study include its retrospective design, which inevitably introduced confounding biases due to lack of information on confounding factors not available in the medical records. Also, we did not evaluate patients’ satisfaction and abdominal muscle strength during the preoperative and postoperative period. Further prospective studies comparing complications between different autologous flap techniques would be the best way to identify the ideal flap for breast reconstruction.
Conclusions
The complication rate after pedicled TRAM flap reconstruction by whole muscle with partial sheath sparing technique in breast cancer patients undergoing mastectomy was acceptable and comparable to other techniques. The oncologic outcome was not different when compared with mastectomy or BCT. We continue to offer this technique because of the predictability in survival of transferred tissue.
Acknowledgements
We wish to acknowledge my clinical fellows team as follows: Dr. Saowanee Kitudomrat, Dr. Paweena Luadthai, Dr. Suragit Pornchai, Dr. Watoo Vassanasiri, Dr. Noppadol Trikunagonvong and Dr. Chayanoot Rattadilok to encourage these operations.
Ethical Statement: The study was approved by ethics board of the Committee on Human Rights Related to Research Involving Human Subjects, based on the Declaration of Helsinki, Faculty of Medicine Ramathibodi hospital, Mahidol University (No. 02-51-44) and written informed consent was obtained from all patients.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Ducic I, Spear SL, Cuoco F, et al. Safety and risk factors for breast reconstruction with pedicled transverse rectus abdominis musculocutaneous flaps: a 10-year analysis. Ann Plast Surg 2005;55:559-64. 10.1097/01.sap.0000184463.90172.04 [DOI] [PubMed] [Google Scholar]
- 2.Alderman AK, Wilkins EG, Kim HM, et al. Complications in postmastectomy breast reconstruction: two-year results of the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg 2002;109:2265-74. 10.1097/00006534-200206000-00015 [DOI] [PubMed] [Google Scholar]
- 3.Andrades P, Fix RJ, Danilla S, et al. Ischemic complications in pedicle, free, and muscle sparing transverse rectus abdominis myocutaneous flaps for breast reconstruction. Ann Plast Surg 2008;60:562-7. 10.1097/SAP.0b013e31816fc372 [DOI] [PubMed] [Google Scholar]
- 4.Reece GP, Kroll SS. Abdominal wall complications. Prevention and treatment. Clin Plast Surg 1998;25:235-49. [PubMed] [Google Scholar]
- 5.Kroll SS, Marchi M. Comparison of strategies for preventing abdominal-wall weakness after TRAM flap breast reconstruction. Plast Reconstr Surg 1992;89:1045-51; discussion 1052-3. 10.1097/00006534-199206000-00007 [DOI] [PubMed] [Google Scholar]
- 6.Suominen S, Asko-Seljavaara S, von Smitten K, et al. Sequelae in the abdominal wall after pedicled or free TRAM flap surgery. Ann Plast Surg 1996;36:629-36. 10.1097/00000637-199606000-00012 [DOI] [PubMed] [Google Scholar]
- 7.Feller AM. Free TRAM. Results and abdominal wall function. Clin Plast Surg 1994;21:223-32. [PubMed] [Google Scholar]
- 8.Blondeel N, Vanderstraeten GG, Monstrey SJ, et al. The donor site morbidity of free DIEP flaps and free TRAM flaps for breast reconstruction. Br J Plast Surg 1997;50:322-30. 10.1016/S0007-1226(97)90540-3 [DOI] [PubMed] [Google Scholar]
- 9.Nahabedian MY, Manson PN. Contour abnormalities of the abdomen after transverse rectus abdominis muscle flap breast reconstruction: a multifactorial analysis. Plast Reconstr Surg 2002;109:81-7; discussion 88-90. 10.1097/00006534-200201000-00014 [DOI] [PubMed] [Google Scholar]
- 10.Chang DW, Wang B, Robb GL, et al. Effect of obesity on flap and donor-site complications in free transverse rectus abdominis myocutaneous flap breast reconstruction. Plast Reconstr Surg 2000;105:1640-8. 10.1097/00006534-200004050-00007 [DOI] [PubMed] [Google Scholar]
- 11.Chang DW, Reece GP, Wang B, et al. Effect of smoking on complications in patients undergoing free TRAM flap breast reconstruction. Plast Reconstr Surg 2000;105:2374-80. 10.1097/00006534-200006000-00010 [DOI] [PubMed] [Google Scholar]
- 12.Ascherman JA, Seruya M, Bartsich SA. Abdominal wall morbidity following unilateral and bilateral breast reconstruction with pedicled TRAM flaps: an outcomes analysis of 117 consecutive patients. Plast Reconstr Surg 2008;121:1-8. 10.1097/01.prs.0000295378.43033.c4 [DOI] [PubMed] [Google Scholar]
- 13.DeSantis C, Siegel R, Bandi P, et al. Breast cancer statistics, 2011. CA Cancer J Clin 2011;61:409-18. 10.3322/caac.20134 [DOI] [PubMed] [Google Scholar]
- 14.Early Breast Cancer Trialists' Collaborative Group (EBCTCG) , Darby S, McGale P, et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet 2011;378:1707-16. 10.1016/S0140-6736(11)61629-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jatoi I, Proschan MA. Randomized trials of breast-conserving therapy versus mastectomy for primary breast cancer: a pooled analysis of updated results. Am J Clin Oncol 2005;28:289-94. 10.1097/01.coc.0000156922.58631.d7 [DOI] [PubMed] [Google Scholar]
- 16.Kim EK, Eom JS, Ahn SH, et al. Evolution of the pedicled TRAM flap: a prospective study of 500 consecutive cases by a single surgeon in Asian patients. Ann Plast Surg 2009;63:378-82. 10.1097/SAP.0b013e3181951708 [DOI] [PubMed] [Google Scholar]
- 17.Sailon AM, Schachar JS, Levine JP. Free transverse rectus abdominis myocutaneous and deep inferior epigastric perforator flaps for breast reconstruction: a systematic review of flap complication rates and donor-site morbidity. Ann Plast Surg 2009;62:560-3. 10.1097/SAP.0b013e31819faf0d [DOI] [PubMed] [Google Scholar]
- 18.Spear SL, Ducic I, Cuoco F, et al. Effect of obesity on flap and donor-site complications in pedicled TRAM flap breast reconstruction. Plast Reconstr Surg 2007;119:788-95. 10.1097/01.prs.0000252003.14537.d2 [DOI] [PubMed] [Google Scholar]
- 19.Dayhim F, Wilkins EG. The impact of Pfannenstiel scars on TRAM flap complications. Ann Plast Surg 2004;53:432-5. 10.1097/01.sap.0000130709.23640.60 [DOI] [PubMed] [Google Scholar]