Abstract
Controversy exists regarding whether left atrial enlargement (LAE) is a predictor of stroke/systemic embolism (SE) in atrial fibrillation (AF) patients. The Fushimi AF Registry, a community-based prospective survey, enrolled all AF patients in Fushmi-ku, Japan, from March 2011. Follow-up data and baseline echocardiographic data were available for 2,713 patients by August 2015. We compared backgrounds and incidence of events over a median follow-up of 976.5 days between patients with LAE (left atrial diameter > 45 mm; LAE group) and those without in the Fushimi AF Registry. The LAE group accounted for 39% (n = 1,049) of cohort. The LAE group was older and had longer AF duration, with more prevalent non-paroxysmal AF, higher CHADS2/CHA2DS2-VASc score, and oral anticoagulant (OAC) use. A higher risk of stroke/SE during follow-up in the LAE group was found (entire cohort; hazard ratio (HR): 1.92, 95% confidence interval (CI): 1.40–2.64; p < 0.01; without OAC; HR: 1.97, 95% CI: 1.18–3.25; p < 0.01; with OAC; HR: 1.83, 95% CI: 1.21–2.82; p < 0.01). LAE was independently associated with increased risk of stroke/SE (HR: 1.74, 95% CI: 1.25–2.42; p < 0.01) after adjustment by the components of CHA2DS2-VASc score and OAC use. In conclusion, LAE was an independent predictor of stroke/SE in large community cohort of AF patients.
Atrial fibrillation (AF) increases the risk of thromboembolism, such as stroke or systemic embolism (SE) fivefold1, but this risk is not homogeneous and depends on the various stroke risk factors2. These clinical risk factors are used to formulate clinical risk stratification schemes, such as CHADS23 and CHA2DS2-VASc scores4. Echocardiographic parameters have been proposed as additional risk stratification refinements for predicting thromboembolism in AF patients. Left atrial structure and function may confer a risk for stroke/SE, given that thrombus formation mainly occurs in the left atrium5. In addition, left atrial structure and function represents AF burden or duration6, which might be related to increased risk of stroke/SE7.
Among many indices of left atrial structure and function, left atrial diameter determined by trans-thoracic echocardiography is the simplest method to measure, and used worldwide in daily clinical practice. Left atrial enlargement (LAE), defined as an enlarged left atrial diameter, has been reported to be a predictor of stroke/SE in AF patients in some8,9,10,11,12, but not all studies13,14,15,16, and data from large-scale prospective cohorts are limited. The aim of this study is to investigate the impact of LAE on the incidence of stroke/SE in a large community-based prospective survey of Japanese AF patients, the Fushimi AF Registry.
Methods
The Fushimi AF Registry is a community-based prospective survey of AF patients in Fushimi-ku, Japan17,18. The detailed study design, patient enrollment, the definition of the measurements, and subjects’ baseline clinical characteristics of the Fushimi AF Registry were previously described17. The inclusion criterion for the registry is the documentation of AF on a 12-lead electrocardiogram or Holter monitoring at any time. There are no exclusion criteria. A total of 80 institutions participated in the registry. We started to enroll patients from March 2011. All of the participating institutions attempted to enroll all consecutive patients with AF under regular outpatient care or under admission.
Among the registry participants, we analyzed the patients whose follow-up data were available. The primary endpoint in this analysis was the incidence of stroke/SE during follow-up period. Other clinical endpoints included the incidence of ischemic stroke, hemorrhagic stroke, all-cause death, cardiac death, non-cardiac death, and composite endpoints of ‘stroke, SE, and all-cause death’ during follow-up period. The type of AF was classified into 2 groups; paroxysmal AF and sustained AF which was defined as the combination of persistent AF and permanent AF19. AF duration was calculated from the day of estimated AF documentation to the day of entry into the registry.
Echocardiographic data were collected at the time of entry into the registry. Left atrial diameter was measured using M-mode or two-dimensional echocardiography, from the posterior aortic wall to the posterior left atrial wall, in the parasternal long axis view at the end-ventricular systole20. We simply defined LAE as left atrial diameter more than 45 mm, according to the previous study16. We did not categorize left atrial diameter as gender-specific variable, since mean left atrial diameter was not statistically different between male and female in our registry.
We compared the background and incidence of clinical events during follow-up period between those with left atrial diameter > 45 mm (LAE group) and those without it (non-LAE group). We excluded registry participants for whom data on their left atrial diameter were missing, those with mitral stenosis and/or prior cardiac valve surgery.
Statistical analysis
Continuous variables are expressed as mean ± standard deviation, or median and interquartile range according to the distributions. Categorical variables are presented as numbers and percentages. We compared categorical variables using the chi-square test when appropriate; otherwise, we used Fisher’s exact test. We compared continuous variables using Student’s t-test or Wilcoxon rank-sum test on the basis of the distribution. The Kaplan-Meier method was used to estimate the cumulative incidences of clinical events. Data were analyzed as crude and stratified by oral anticoagulant (OAC) prescription at baseline. Data were also stratified by major subgroups which were considered to be confounders. We carried out multivariate analysis using a Cox proportional hazards model. The covariates chosen to be included were LAE, OAC prescription at baseline, and components of the CHA2DS2-VASc risk score4. We used JMP version 10 (SAS Institute, Cary, NC) to perform all of these analyses. Two-sided P values less than 0.05 were considered statistically significant.
Ethics
The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki, and was approved by the ethical committees of the National Hospital Organization Kyoto Medical Center and Ijinkai Takeda General Hospital. Since the present research involves an observational study not using human biological specimens, written informed consent was not obtained from each patient for their clinical records to be used in this study, according to the ethical guidelines for epidemiological research issued by the Ministry of Education, Culture, Sports, Science and Technology and the Ministry of Health, Labour and Welfare, Japan.
Results
A total of 4,392 patients were enrolled in the Fushimi AF Registry by August 2015. Of 4,124 patients who were enrolled one year before, follow-up data (collected every year) were available for 3,713 patients (follow-up rate: 90.0%). Of these 3,713 patients, we excluded 191 patients with mitral stenosis or prior cardiac valve surgery. Among 3,522 non-valvular AF patients, left atrial echocardiographic data were available for 2,713 patients, and left atrial diameter data were missing for 809 patients. Age and gender were comparable between patients with and without left atrial diameter data (mean age 73.7 vs 73.7 years; p = 0.99, female sex 40% vs. 41%, p = 0.57, respectively). Patients without left atrial diameter data had lower CHADS2 score (1.93 vs. 2.05; p = 0.03), CHA2DS2-VASc score (3.24 vs. 3.39; p = 0.03), and had lower prescription of OAC at baseline (45% vs. 55%; p < 0.01). Cumulative incidence of stroke/SE during follow-up period was comparable between the two groups (5.6% vs. 5.7%; p = 0.90).
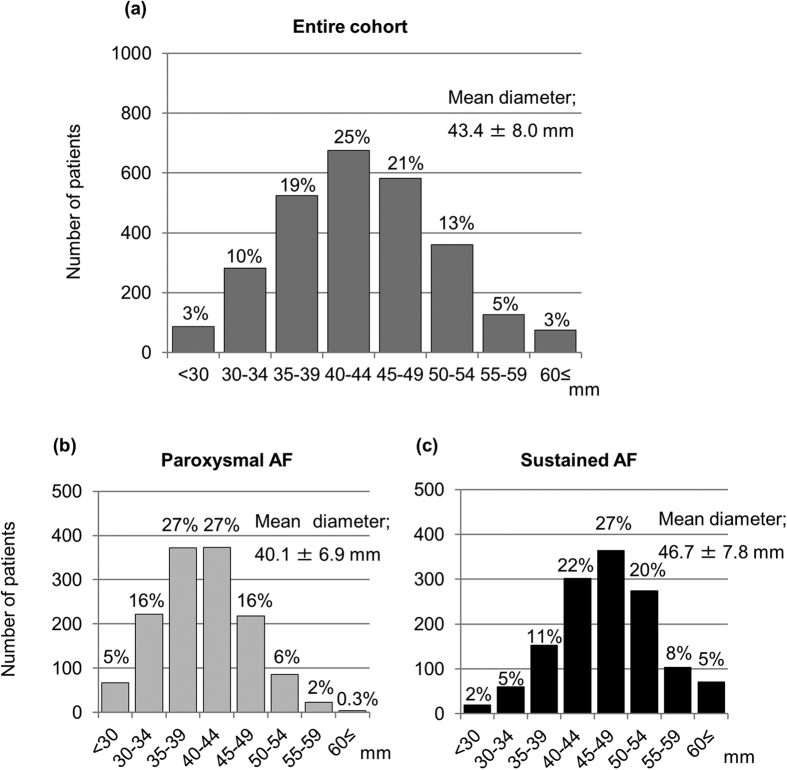
A total of 2,713 patients were included in the analysis. Median follow-up period was 976.5 days (interquartile range: 468 to 1190 days). The distributions of left atrial diameter are shown in Fig. 1. Patients in the LAE group accounted for 39% (n = 1,049) of all patients. Patients with sustained AF had larger left atrial diameter than those with paroxysmal AF (46.7 ± 7.8 vs. 40.1 ± 6.9 mm; p < 0.01).
Figure 1. Distributions of left atrial diameter.
(a) Entire cohort. (b) Patients with paroxysmal atrial fibrillation (AF). (c) Patients with sustained AF. AF = atrial fibrillation.
LAE vs non-LAE patients
Baseline characteristics are shown in Table 1. The LAE group was older, had higher CHADS2 and CHA2DS2-VASc scores (all p < 0.01). Left atrial diameter was correlated with AF duration (p < 0.01). The LAE group had higher use of OAC at baseline (p < 0.01), and OAC prescription data at baseline were missing for 13 patients. Patients without OAC were more often female (p < 0.01), younger (p = 0.03), had lower CHADS2 score and CHA2DS2-VASc score (both p < 0.01), and had smaller left atrial diameter (p < 0.01).
Table 1. Baseline characteristics and Co-morbidities.
| Number | LAE | Non-LAE | p value | Without OAC | With OAC | p value |
|---|---|---|---|---|---|---|
| 1,049 | 1,664 | 1,221 | 1,479 | |||
| Baseline characteristics | ||||||
| Female | 411 (39%) | 669 (40%) | 0.60 | 526 (43%) | 550 (37%) | <0.01 |
| Age (years) | 74.9 ± 10.2 | 72.9 ± 11.2 | <0.01 | 73.2 ± 12.5 | 74.1 ± 9.2 | 0.03 |
| Age ≥ 75 years | 591 (56%) | 795 (48%) | <0.01 | 589 (48%) | 786 (53%) | 0.01 |
| Body mass index (kg/m2) | 24.0 ± 4.2 | 22.4 ± 3.8 | <0.01 | 22.7 ± 4.0 | 23.3 ± 4.0 | <0.01 |
| Body weight (kg) | 61.8 ± 14.4 | 57.7 ± 12.5 | <0.01 | 58.1 ± 13.5 | 60.3 ± 13.3 | <0.01 |
| Systolic blood pressure (mmHg) | 123.9 ± 20.3 | 124.1 ± 18.9 | 0.85 | 125.1 ± 19.4 | 123.0 ± 19.4 | <0.01 |
| Diastolic blood pressure (mmHg) | 69.9 ± 13.6 | 70.1 ± 12.5 | 0.74 | 70.1 ± 13.0 | 69.9 ± 12.9 | 0.57 |
| Heart rate (beats/min) | 77.9 ± 15.6 | 77.9 ± 15.8 | 0.96 | 78.6 ± 16.2 | 77.4 ± 15.3 | 0.04 |
| Paroxysmal AF | 288 (27%) | 1,077 (65%) | <0.01 | 769 (63%) | 591 (40%) | <0.01 |
| AF duration (months) | 43.5 (10.0, 91.3) | 21.0 (4.0, 59.0) | <0.01 | 25.0 (4.0, 62.0) | 31.0 (7.0, 75.0) | <0.01 |
| Smoking history | 354 (34%) | 597 (36%) | 0.26 | 413 (48%) | 535 (51%) | 0.20 |
| Previous catheter ablation | 46 (4%) | 136 (8%) | <0.01 | 86 (7%) | 95 (6%) | 0.52 |
| Calculated CrCl (ml/min) | 56.6 (35.9, 76.5) | 58.6 (39.7, 80.2) | 0.02 | 59.6 (36.0, 82.1) | 56.6 (39.9, 76.2) | 0.11 |
| Hemoglobin (g/dL) | 12.9 ± 2.1 | 12.9 ± 2.0 | 0.65 | 12.7 ± 2.1 | 13.0 ± 2.0 | <0.01 |
| Co-morbidities | ||||||
| CHADS2 score | 2.26 ± 1.30 | 1.92 ± 1.36 | <0.01 | 1.77 ± 1.34 | 2.27 ± 1.31 | <0.01 |
| CHA2DS2-VASc score | 3.64 ± 1.65 | 3.24 ± 1.74 | <0.01 | 3.11 ± 1.77 | 3.63 ± 1.63 | <0.01 |
| History of stroke/SE | 225 (21%) | 348 (21%) | 0.74 | 175 (14%) | 396 (27%) | <0.01 |
| Heart failure | 390 (37%) | 358 (22%) | <0.01 | 259 (21%) | 484 (33%) | <0.01 |
| Hypertension | 691 (66%) | 997 (60%) | <0.01 | 722 (59%) | 957 (65%) | <0.01 |
| Diabetes mellitus | 263 (25%) | 376 (23%) | 0.14 | 261 (21%) | 374 (25%) | 0.02 |
| Dyslipidemia | 444 (42%) | 713 (43%) | 0.79 | 500 (41%) | 653 (44%) | 0.09 |
| Vascular disease | 117 (11%) | 165 (10%) | 0.30 | 130 (11%) | 152 (10%) | 0.75 |
| Chronic kidney disease | 445 (42%) | 564 (34%) | <0.01 | 411 (34%) | 593 (40%) | <0.01 |
| COPD | 56 (5%) | 87 (5%) | 0.90 | 57 (5%) | 84 (6%) | 0.24 |
| History of major bleeding | 43 (4%) | 71 (4%) | 0.83 | 58 (5%) | 55 (4%) | 0.18 |
| OAC prescription at baseline | 693 (66%) | 786 (47%) | <0.01 | 0 (0%) | 1,479 (100%) | <0.01 |
| Warfarin | 611 (59%) | 655 (39%) | <0.01 | 0 (0%) | 1,266 (86%) | <0.01 |
| Non-vitamin K antagonist OAC | 82 (8%) | 131 (8%) | 0.96 | 0 (0%) | 213 (14%) | <0.01 |
| Echocardiography | ||||||
| LV ejection fraction (%) | 61.4 ± 12.2 | 64.2 ± 11.1 | <0.01 | 63.9 ± 11.1 | 62.5 ± 12.0 | <0.01 |
| LV ejection fraction ≤ 40% | 70 (7%) | 82 (5%) | 0.05 | 60 (5%) | 92 (6%) | 0.15 |
| LV end-diastolic dimension (mm) | 48.2 ± 6.9 | 45.5 ± 5.7 | <0.01 | 45.9 ± 6.2 | 47.0 ± 6.4 | <0.01 |
| LV end-systolic dimension (mm) | 32.2 ± 7.5 | 29.4 ± 5.9 | <0.01 | 29.8 ± 6.3 | 31.0 ± 7.0 | <0.01 |
| LV septal wall thickness (mm) | 9.8 ± 1.9 | 9.3 ± 1.6 | <0.01 | 9.4 ± 1.6 | 9.6 ± 1.8 | <0.01 |
| LV posterior wall thickness (mm) | 9.8 ± 1.6 | 9.2 ± 1.4 | <0.01 | 9.3 ± 1.4 | 9.5 ± 1.5 | <0.01 |
| Left atrial diameter (mm) | 51.3 ± 5.4 | 38.4 ± 4.8 | <0.01 | 41.5 ± 7.8 | 44.9 ± 7.9 | <0.01 |
Categorical data are presented as number (%). Continuous data are presented as mean ± standard deviation (SD), or median and interquartile range (25%, 75%) according to the distribution. AF = atrial fibrillation, COPD = chronic obstructive pulmonary disease, CrCl = creatinine clearance, LAE = left atrial enlargement, LV = left ventricular, OAC = oral anticoagulant, SE: systemic embolism.
Outcomes
Major clinical cumulative events in the entire cohort during follow-up period were as follows: stroke/SE in 154, ischemic stroke in 112, hemorrhagic stroke in 43, SE in 4, all-cause death in 418, cardiac death in 64, non-cardiac death in 354, and stroke/SE/all-cause death in 530, respectively. Major clinical events in the entire cohort, patients without OAC, and those with OAC are shown in Table 2.
Table 2. Incidence of clinical events during follow-up (/100 person-years).
| Outcomes | Entire cohort |
Patients without OAC |
Patients with OAC |
|||
|---|---|---|---|---|---|---|
| Incidence rate | p value* | Incidence rate | p value* | Incidence rate | p value* | |
| Stroke/SE | 2.4 | 2.2 | 2.5 | |||
| LAE | 3.4 | <0.01 | 3.4 | <0.01 | 3.3 | <0.01 |
| Non-LAE | 1.7 | 1.7 | 1.8 | |||
| Ischemic stroke | 1.7 | 1.4 | 1.9 | |||
| LAE | 2.4 | <0.01 | 2.2 | 0.02 | 2.6 | 0.01 |
| Non-LAE | 1.2 | 1.1 | 1.3 | |||
| Hemorrhagic stroke | 0.6 | 0.7 | 0.6 | |||
| LAE | 0.9 | 0.046 | 1.0 | 0.26 | 0.8 | 0.11 |
| Non-LAE | 0.5 | 0.6 | 0.4 | |||
| All-cause death | 6.3 | 7.5 | 5.3 | |||
| LAE | 7.0 | 0.05 | 8.3 | 0.31 | 6.3 | <0.01 |
| Non-LAE | 5.8 | 7.2 | 4.4 | |||
| Cardiac death | 1.0 | 0.9 | 1.0 | |||
| LAE | 1.1 | 0.40 | 1.1 | 0.48 | 1.1 | 0.67 |
| Non-LAE | 0.9 | 0.8 | 0.9 | |||
| Non-cardiac death | 5.3 | 6.6 | 4.3 | |||
| LAE | 5.9 | 0.08 | 7.2 | 0.41 | 5.2 | <0.01 |
| Non-LAE | 4.9 | 6.3 | 3.4 | |||
| Stroke/SE/All-cause death | 8.1 | 9.3 | 7.2 | |||
| LAE | 9.5 | <0.01 | 11.0 | 0.07 | 8.6 | <0.01 |
| Non-LAE | 7.3 | 8.7 | 5.3 | |||
*p value for comparison between LAE versus non-LAE from log-rank test. LAE = left atrial enlargement, OAC = oral anticoagulant, SE = systemic embolism.
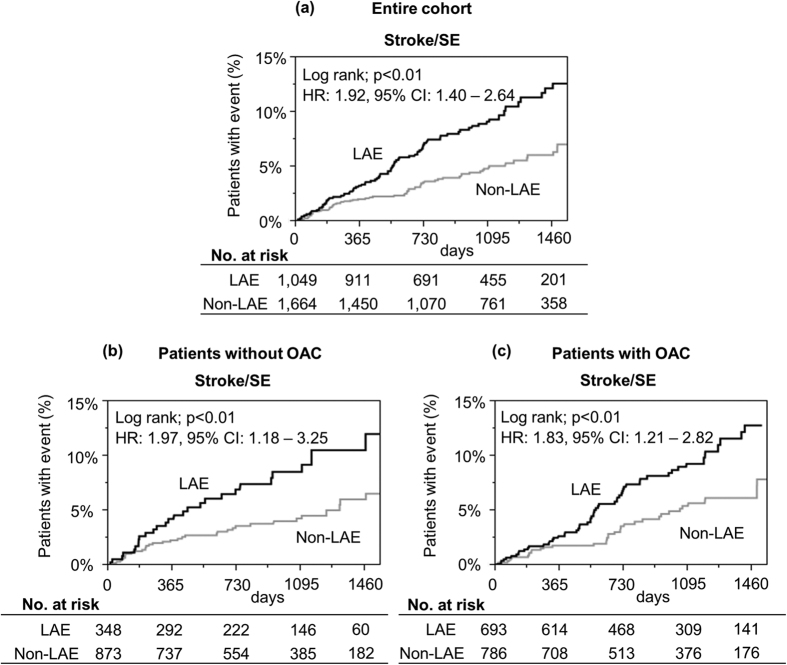
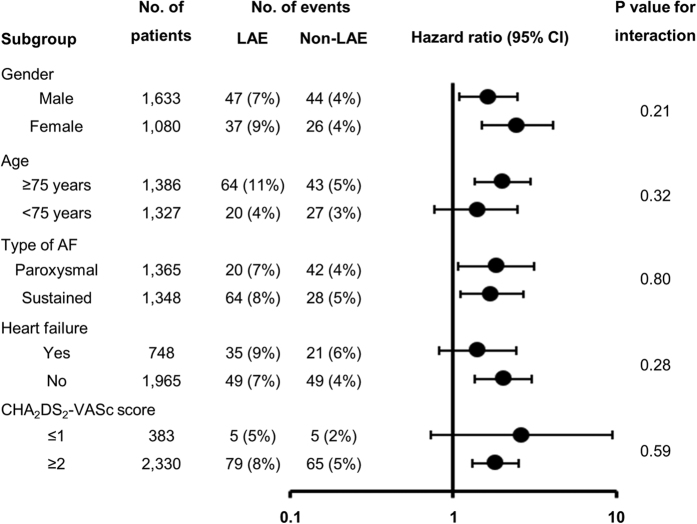
Kaplan-Meier curves for the incidence of stroke/SE are shown in Fig. 2. A higher risk of stroke/SE during follow-up period in the LAE group was consistently observed in the entire cohort, and in patients stratified by OAC prescription at baseline (entire cohort; hazard ratio (HR): 1.92, 95% confidence interval (CI): 1.40–2.64; p < 0.01, patients without OAC; HR: 1.97, 95% CI: 1.18–3.25; p < 0.01, and patients with OAC; HR: 1.83, 95% CI: 1.21–2.82; p < 0.01, respectively). Statistical tests for interaction were not significant for all of the major subgroups (Fig. 3).
Figure 2. Kaplan-Meier curves for the incidence of stroke or systemic embolism (SE) during follow-up period.
(a) Entire cohort, (b) Patients without oral anticoagulant (OAC). (c) Patients with OAC at baseline. CI = confidence interval, HR = hazard ratio, LAE = left atrial enlargement, OAC = oral anticoagulant, SE = systemic embolism.
Figure 3. Impact of left atrial enlargement (left atrial diameter > 45 mm) on the incidence of stroke or systemic embolism, according to major subgroups.
AF = atrial fibrillation, CI = confidence interval, LAE = left atrial enlargement.
Multivariate analysis/Sensitivity analyses
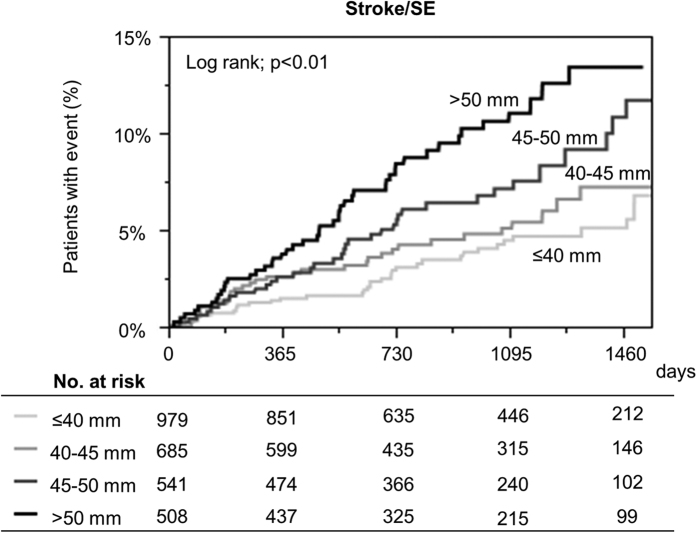
On multivariate analysis, after adjustment by the components of CHA2DS2-VASc score and OAC prescription at baseline, LAE emerged as an independent risk factor of the incidence of stroke/SE (HR: 1.74, 95% CI: 1.25–2.42; p < 0.01) (Table 3). LAE still remained a significant risk factor of stroke/SE, when age was included as continuous variable on multivariate analysis (HR: 1.73, 95% CI: 1.24–2.41; p < 0.01). When we defined the cut-off value of left atrial diameter as more than 50 mm, left atrial diameter > 50 mm was also independently associated with higher risk of stroke/SE on multivariate analysis (HR: 1.69, 95% CI: 1.18–2.41; p < 0.01). Kaplan-Meier curves for the incidence of stroke/SE between ordinal variable of 4 left atrial diameter strata (≤ 40 mm, 40–45 mm, 45–50 mm, > 50 mm) are shown in Fig. 4. Increasing left atrial diameter could stratify the incidence of stroke/SE during follow-up period (log-rank; p < 0.01). When we used left atrial diameter indexed by body surface area, indexed left atrial diameter still remained significantly associated with a higher risk of stroke/SE (HR: 1.08 per 1 mm/m2, 95% CI: 1.05–1.10; p < 0.01).
Table 3. Indicators of the incidence of stroke or systemic embolism during follow-up. Multivariate analysis.
| Variable | HR (95% CI) | p value |
|---|---|---|
| Left atrial enlargement (>45 mm) | 1.74 (1.25–2.42) | <0.01 |
| OAC prescription | 0.88 (0.63–1.24) | 0.46 |
| Heart failure | 1.30 (0.91–1.83) | 0.15 |
| Hypertension | 0.98 (0.70–1.37) | 0.88 |
| Age ≥ 75 years (vs. <65 years) | 2.26 (1.35–4.03) | <0.01 |
| Age 65–74 years (vs. <65 years) | 0.99 (0.55–1.86) | 0.97 |
| Diabetes mellitus | 1.01 (0.70–1.45) | 0.94 |
| History of stroke/SE | 1.55 (1.08–2.20) | 0.02 |
| Vascular disease | 1.10 (0.66–1.73) | 0.71 |
| Female sex | 0.93 (0.66–1.30) | 0.68 |
AF = atrial fibrillation, CI = confidence interval, HR = hazard ratio, OAC = oral anticoagulant, SE = systemic embolism.
Figure 4. Kaplan-Meier curves for the incidence of stroke or systemic embolism (SE) according to 4 left atrial diameter strata (≤40 mm vs. 40–45 mm vs. 45–50 mm vs. >50 mm).
SE = systemic embolism.
We also performed multivariate analysis among patients without OAC at baseline. LAE remained an independent risk factor of stroke/SE (HR: 1.85, 95% CI: 1.10–3.10; p = 0.02). Left atrial diameter > 50 mm was also independently associated with higher risk of stroke/SE (HR: 2.22, 95% CI: 1.19–3.96; p = 0.01), and ordinal variable of 4 left atrial diameter strata (≤40 mm, 40–45 mm, 45–50 mm, >50 mm) could also stratify the incidence of stroke/SE during follow-up (log-rank; p < 0.01).
Discussion
In the contemporary large community-based prospective study, we have shown that LAE was an independent predictor of stroke/SE in non-valvular AF patients. This relationship remained, even after adjustment for differences in baseline characteristics and was consistent whether on OAC or not taking OAC.
A relationship between LAE and increased risk of stroke/SE in AF patients was first proposed in the 1980s8,9. In early 1990s, some reports supported that LAE was significantly associated with increased risk of stroke/SE10,11,12, while other studies found that LAE could not predict stroke events13,14. However, these studies were small-sized and retrospective in design.
In late 1990s and 2000s, sub-analyses of clinical trials reported that left atrial diameter was not independently associated with thromboembolic events15,16. In the sub-analysis of non-anticoagulated AF patients from 3 clinical trials, a total of 1,066 patients were included, and ischemic stroke occurred in 78 patients during a mean period of 1.6 years. In this analysis, left atrial diameter tended to be associated with stroke (relative risk, 1.02 per 1mm; p = 0.10); however, it did not reach a statistical significance15. In a sub-analysis of AFFIRM trial21, a total of 2,334 patients with left atrial diameter data were included, and stroke occurred in 86 patients during a mean period of 1,298 days. This study concluded that left atrial diameter was not a predictor of stroke; however, most of the patients included in the AFFIRM trial were prescribed OAC, and patients with excessively enlarged left atrium might have been excluded (31% of patients had left atrial diameter greater than 45 mm, compared to 39% in our study)16.
More recent studies have reported that LAE was independently associated with increased risk of stroke after adjustment by the CHA2DS2-VASc score, although endpoints in these studies were the transesophageal echocardiographic surrogate markers of stroke22,23. Thus, controversy exists regarding whether LAE is a significant predictor for the incidence of stroke/SE independent from established risk factors, and there have been no data with large-scale, prospective studies with long term follow-up. To the best of our knowledge, our study is one of the largest ‘all-comers” studies, providing longer-term follow-up data about the association between LAE and the incidence of stroke/SE in AF patients, and providing robust evidence that LAE was independently associated with increased risk of stroke/SE.
Several mechanisms could explain how LAE is associated with higher risk of stroke/SE in AF patients. First, LAE promotes blood stasis, which in turn predisposes to thrombus formation and the potential for the embolization. Indeed, transesophageal echocardiography studies have found that LAE was associated with spontaneous echo contrast in left atrium22. Second, left atrial diameter can be related to AF duration24, or arrhythmia burden6. Cardiac implanted electronic device-detected AF burden was reportedly associated with increased risk of stroke/SE7. However, AF burden is difficult to measure in patients without cardiac implanted electronic device. Indeed, left atrial diameter could be a good marker of AF burden/duration, and assessment of left atrial size may add important incremental information in the evaluation of stroke/SE risk in AF patients.
Study Limitations
First, this is an observational study and provides only associative evidence, not causative. We cannot rule out the possibility of unmeasured confounders. Second, we measured only left atrial anterior-posterior diameter. Left atrial volume is a more reliable estimator of left atrial size, and has been recommended when assessing left atrial size, since left atrial dilatation can be eccentric20. However, left atrial diameter is more readily available and more widely employed in daily clinical practice25. Third, among 3,522 patients, left atrial echocardiographic data were missing in 809 patients, leading to selection bias. However, patients without left atrial diameter data were not particularly skewed in our study, considering that the backgrounds and incidence of stroke/SE were comparable between patients with and without echocardiographic data. Fourth, AF duration data were available for only 1,771 patients among the entire cohort, and were mostly based on the physician’s judgement or patient’s self-report. Fifth, antithrombotic therapy were selected at the discretion of the attending physician, and we stratified the entire cohort by OAC prescription only at baseline. Finally, we did not measure 24-hour blood pressure and collected blood pressure data only at the time of entry into the registry, notwithstanding hypertension being associated with the incidence of AF26, and the incidence of thromboembolism among AF patients27.
Conclusions
In this large community cohort of Japanese patients with AF, LAE was an independent predictor of stroke/SE, suggesting this simple echocardiographic parameter could refine thromboembolic risk stratification of AF patients.
Additional Information
How to cite this article: Hamatani, Y. et al. Left atrial enlargement is an independent predictor of stroke and systemic embolism in patients with non-valvular atrial fibrillation. Sci. Rep. 6, 31042; doi: 10.1038/srep31042 (2016).
Acknowledgments
We sincerely appreciate the help of all the institutions and consortium members participating in the Fushimi AF Registry and the clinical research coordinators (Shinagawa T, Mitamura M, Fukahori M, Kimura M, Fukuyama M, Kamata C). The Fushimi AF Registry is supported by research funding from Boehringer Ingelheim, Bayer Healthcare, Pfizer, Bristol-Myers Squibb, Astellas Pharma, AstraZeneca, Daiichi-Sankyo, Novartis Pharma, MSD, Sanofi-Aventis and Takeda Pharmaceutical. This research is partially supported by the Practical Research Project for Life-Style related Diseases including Cardiovascular Diseases and Diabetes Mellitus from Japan Agency for Medical Research and Development, AMED (15656344).
Footnotes
Dr. Akao received lecture fees from Pfizer, Bristol Myers Squibb, Boehringer Ingelheim, Bayer Healthcare and Daiichi-Sankyo. Dr Lip has served as a consultant or advisory board for Bayer/ Janssen, Astellas, Merck, Sanofi, BMS/Pfizer, Biotronik, Medtronic, Portola, Boehringer Ingelheim, Microlife and Daiichi-Sankyo, and has been on the speakers bureau for Bayer, BMS/Pfizer, Medtronic, Boehringer Ingelheim, Microlife, Roche and Daiichi-Sankyo. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Author Contributions All authors have contributed and all agree to the submission of the paper. Y.H. analyzed the data and wrote the paper. Y.Y., H.O., K.T., Y.Y. and D.T. helped data analysis and interpretation. H.W. helped statistical analysis. M.E., Y.C., H.T., H.W., K.H. and M. Abe are executive members of the organizing committee of the Fushimi AF. Registry. M. Akao and G.L. are joint senior authors. M. Akao is a principal investigator of the Fushimi AF Registry, and the corresponding author of this paper.
References
- Wolf P. A., Abbott R. D. & Kannel W. B. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke 22, 983–988 (1991). [DOI] [PubMed] [Google Scholar]
- Pisters R., Lane D. A., Marin F., Camm A. J. & Lip G. Y. Stroke and thromboembolism in atrial fibrillation. Circ J 76, 2289–2304 (2012). [DOI] [PubMed] [Google Scholar]
- Gage B. F. et al. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA 285, 2864–2870 (2001). [DOI] [PubMed] [Google Scholar]
- Lip G. Y., Nieuwlaat R., Pisters R., Lane D. A. & Crijns H. J. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest 137, 263–272, 10.1378/chest.09-1584 (2010). [DOI] [PubMed] [Google Scholar]
- Manning W. J., Silverman D. I., Keighley C. S., Oettgen P. & Douglas P. S. Transesophageal echocardiographically facilitated early cardioversion from atrial fibrillation using short-term anticoagulation: final results of a prospective 4.5-year study. J Am Coll Cardiol 25, 1354–1361, 10.1016/0735-1097(94)00560-d (1995). [DOI] [PubMed] [Google Scholar]
- Gupta D. K. et al. Left atrial structure and function in atrial fibrillation: ENGAGE AF-TIMI 48. Eur Heart J 35, 1457–1465, 10.1093/eurheartj/eht500 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boriani G. et al. Improving stroke risk stratification using the CHADS2 and CHA2DS2-VASc risk scores in patients with paroxysmal atrial fibrillation by continuous arrhythmia burden monitoring. Stroke 42, 1768–1770, 10.1161/strokeaha.110.609297 (2011). [DOI] [PubMed] [Google Scholar]
- Caplan L. R., D’Cruz I., Hier D. B., Reddy H. & Shah S. Atrial size, atrial fibrillation, and stroke. Ann Neurol 19, 158–161, 10.1002/ana.410190208 (1986). [DOI] [PubMed] [Google Scholar]
- Aronow W. S., Gutstein H. & Hsieh F. Y. Risk factors for thromboembolic stroke in elderly patients with chronic atrial fibrillation. Am J Cardiol 63, 366–367 (1989). [DOI] [PubMed] [Google Scholar]
- Seneviratne B. I. & Reimers J. Nonvalvular atrial fibrillation associated with cardioembolic stroke: the role of hypertensive heart disease. Aust N Z J Med 20, 127–134 (1990). [DOI] [PubMed] [Google Scholar]
- Corbalan R. et al. Risk factors for systemic embolism in patients with paroxysmal atrial fibrillation. Am Heart J 124, 149–153 (1992). [DOI] [PubMed] [Google Scholar]
- Cabin H. S., Clubb K. S., Hall C., Perlmutter R. A. & Feinstein A. R. Risk for systemic embolization of atrial fibrillation without mitral stenosis. Am J Cardiol 65, 1112–1116 (1990). [DOI] [PubMed] [Google Scholar]
- Moulton A. W., Singer D. E. & Haas J. S. Risk factors for stroke in patients with nonrheumatic atrial fibrillation: a case-control study. Am J Med 91, 156–161 (1991). [DOI] [PubMed] [Google Scholar]
- Petersen P., Kastrup J., Helweg-Larsen S., Boysen G. & Godtfredsen J. Risk factors for thromboembolic complications in chronic atrial fibrillation. The Copenhagen AFASAK study. Arch Intern Med 150, 819–821 (1990). [PubMed] [Google Scholar]
- Echocardiographic predictors of stroke in patients with atrial fibrillation: a prospective study of 1066 patients from 3 clinical trials. Arch Intern Med 158, 1316–1320 (1998). [DOI] [PubMed] [Google Scholar]
- Olshansky B. et al. Are transthoracic echocardiographic parameters associated with atrial fibrillation recurrence or stroke? Results from the Atrial Fibrillation Follow-Up Investigation of Rhythm Management (AFFIRM) study. J Am Coll Cardiol 45, 2026–2033, 10.1016/j.jacc.2005.03.020 (2005). [DOI] [PubMed] [Google Scholar]
- Akao M. et al. Current status of clinical background of patients with atrial fibrillation in a community-based survey: the Fushimi AF Registry. J Cardiol 61, 260–266, 10.1016/j.jjcc.2012.12.002 (2013). [DOI] [PubMed] [Google Scholar]
- Akao M. et al. Inappropriate Use of Oral Anticoagulants for Patients With Atrial Fibrillation. Circ J 78, 2166–2172 (2014). [DOI] [PubMed] [Google Scholar]
- Takabayashi K. et al. Incidence of Stroke or Systemic Embolism in Paroxysmal Versus Sustained Atrial Fibrillation: The Fushimi Atrial Fibrillation Registry. Stroke 46, 3354–3361, 10.1161/strokeaha.115.010947 (2015). [DOI] [PubMed] [Google Scholar]
- Lang R. M. et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28, 1–39 e14, 10.1016/j.echo.2014.10.003 (2015). [DOI] [PubMed] [Google Scholar]
- Wyse D. G. et al. A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med 347, 1825–1833, 10.1056/NEJMoa021328 (2002). [DOI] [PubMed] [Google Scholar]
- Providencia R. et al. Possible refinement of clinical thromboembolism assessment in patients with atrial fibrillation using echocardiographic parameters. Europace 14, 36–45, 10.1093/europace/eur272 (2012). [DOI] [PubMed] [Google Scholar]
- Faustino A. et al. Which method of left atrium size quantification is the most accurate to recognize thromboembolic risk in patients with non-valvular atrial fibrillation? Cardiovasc Ultrasound 12, 28, 10.1186/1476-7120-12-28 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanfilippo A. J. et al. Atrial enlargement as a consequence of atrial fibrillation. A prospective echocardiographic study. Circulation 82, 792–797 (1990). [DOI] [PubMed] [Google Scholar]
- Gerdts E. et al. Left atrial size and risk of major cardiovascular events during antihypertensive treatment: losartan intervention for endpoint reduction in hypertension trial. Hypertension 49, 311–316, 10.1161/01.hyp.0000254322.96189.85 (2007). [DOI] [PubMed] [Google Scholar]
- Manolis A. J. et al. Hypertension and atrial fibrillation: diagnostic approach, prevention and treatment. Position paper of the Working Group ‘Hypertension Arrhythmias and Thrombosis’ of the European Society of Hypertension. J Hypertens 30, 239–252, 10.1097/HJH.0b013e32834f03bf (2012). [DOI] [PubMed] [Google Scholar]
- Howard G. et al. Is blood pressure control for stroke prevention the correct goal? The lost opportunity of preventing hypertension. Stroke 46, 1595–1600, 10.1161/strokeaha.115.009128 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]