Abstract
For 200 years, the ‘closed box’ analogy of intracranial pressure (ICP) has underpinned neurosurgery and neuro-critical care. Cushing conceptualised the Monro-Kellie doctrine stating that a change in blood, brain or CSF volume resulted in reciprocal changes in one or both of the other two. When not possible, attempts to increase a volume further increase ICP. On this doctrine’s “truth or relative untruth” depends many of the critical procedures in the surgery of the central nervous system. However, each volume component may not deserve the equal weighting this static concept implies. The slow production of CSF (0.35 ml/min) is dwarfed by the dynamic blood in and outflow (∼700 ml/min). Neuro-critical care practice focusing on arterial and ICP regulation has been questioned. Failure of venous efferent flow to precisely match arterial afferent flow will yield immediate and dramatic changes in intracranial blood volume and pressure. Interpreting ICP without interrogating its core drivers may be misleading. Multiple clinical conditions and the cerebral effects of altitude and microgravity relate to imbalances in this dynamic rather than ICP per se. This article reviews the Monro-Kellie doctrine, categorises venous outflow limitation conditions, relates physiological mechanisms to clinical conditions and suggests specific management options.
Keywords: Intracranial pressure, neurotrauma, intracranial hypertension, Monro-Kellie, cerebral venous outflow
Search strategy and selection criteria
Relevant articles were identified by searches of PubMed (1969 to May 2015), and also from the references they quoted. The search terms ‘intracranial pressure’, ‘intracranial hypertension’, ‘neurotrauma’ and ‘traumatic brain injury’ were used with others relevant to each section (e.g. ‘cervical collar’, ‘venous drainage’).
Introduction
History
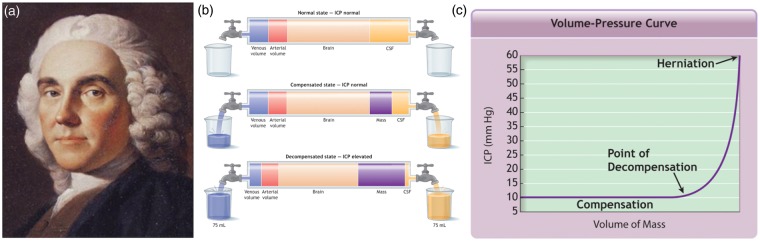
Skulls from as far back as 6000 BC show evidence of trephination (thought to be performed to relieve perceived ‘pressure’ headaches).1 However, it was in 1783 that a ‘science’ of intracranial pressure (ICP) was first proposed. Edinburgh physician Alexander Monro2 (Figure 1(a)), described the skull as a rigid structure containing incompressible brain and stated that the volume of blood must remain constant unless: ‘water or other matter is effused or secreted from the blood-vessels’ in which case ‘a quantity of blood, equal in bulk to the effused matter will be pressed out of the cranium’.
Figure 1.
(a) Alexander Monro secundus (1733–1817). Eminent Scottish physician. (b) Adaptation of current explanation of Monro-Kellie doctrine within advanced trauma life support (ATLS) and most critical care teaching demonstrating that additional mass results in a large volume of CSF then venous blood displacement. (c) Demonstrates that once the period of compliance that this displacement affords runs out, there is an exponential rise in pressure. This description fails to explain the importance of volume flow. From ATLS Course Manual 9th edition.
In 1824, Monro’s former student George Kellie3 confirmed that in human and animal autopsies, cerebral (in particular, venous) blood volume was similar no matter what the cause of death (hanging or exsanguination for example). Local pathologist John Abercrombie4 studied exsanguinated animals and showed that unless the skull and dura were breached, the brain did not exsanguinate in the same way as other organs – the protection the skull offers the brain when ICP is negative to atmospheric pressure often being forgotten. In none of their accounts, however, did any of this Edinburgh group mention cerebral spinal fluid (CSF).
In the 16th century, the peers of Vesalius, a Flemish anatomist, rejected his observation that fluid (rather than gas or spirit) filled the cerebral ventricles. It was the French physiologist François Magendie5 who firmly established the concept of CSF, demonstrating that fluid communicated between the subarachnoid space and fourth ventricle through the foramen that now bears his name.5
Four years later, the English physician George Burrows6 incorporated the role of CSF into Monro’s doctrine, although some were critical, stating that Burrows overplayed CSFs importance and ‘magnified it’s influence’ and role within ICP.7,8 However, the view that CSF shared blood’s importance in ICP regulation was accepted when Harvey Cushing9 vividly presented the summarised doctrine we know today – that with an intact skull, the sum of the volume of brain, blood and CSF is constant: an increase in one causing a decrease in one or both of the remaining two. Even today, this classic explanation forms the basis of neurosurgery and neurotrauma teaching worldwide (Figure 1(b) and (c)). But a precise understanding of what alters ICP is vital as Weed10 stated – on this doctrine’s ‘truth or relative untruth, depend many of the critical procedures in the surgery of the central nervous system’. Interestingly, neuro-critical care practices focusing on arterial and ICP regulation have recently been questioned.11,12 Normal ICP is ∼5–15 mmHg, but is greatly influenced by orthostatic position (for example, it can be negative when standing up) and is generally very similar to cerebral venous pressures (if no distal obstruction).
The dynamic components of ICP
The equal weighting to blood and CSF that the static Monro-Kellie doctrine implies, however, misses the dynamic reality. The slow and (relatively) steady production of CSF (≈0·35 ml/min) is dwarfed by substantial, continuous blood inflow and outflow: at rest, the brain receives approximately 14% of the cardiac output (≈700 ml/min).13 This is a sizeable volume considering that the average male intracranial volume (including brain and CSF) is only twice this (1473 ml).14 At any moment in time, the intracranial blood volume is ∼100–130 ml (∼15% arterial, ∼40% venous and ∼45% in the microcirculation). CSF volume is ∼75 ml (the volume of blood entering in approximately 5 s). Hence, while CSF removal or displacement can reduce ICP, its accumulation is rarely the cause of raised ICP in an acute pathology such as trauma. This is in contrast to CSF obstructive/non-absorption pathology which can result in hydrocephalus and a more gradual rise in ICP.
Arterial influence on ICP
Many have focused on the role of cerebral arterial flow in neuro-critical care. In the early 1970s, Miller and Langfit15,16 drew attention to the concept of estimated cerebral perfusion pressure (CPP) and its calculation from mean arterial pressure (MAP) and ICP (CPP = MAP – ICP). If this equation was entirely true, ICP would equal MAP-CPP implying no venous involvement. By demonstrating a correlation coefficient of 0.98 between ICP and cortical vein pressure in baboons, Johnston and Rowan17 suggested that the equation was true. However, their studies failed to investigate raised ICP secondary to outflow obstruction. It is well recognised that gentle pressure to the neck over the jugular veins causes an ICP rise. The CPP equation has resulted in diverse guidelines that advocate MAP and CPP targets in the management of brain injury. The European Brain Injury Consortium recommend a MAP of >90 mmHg.18 The Association of Anaesthetists of Great Britain and Ireland recommend >80 mmHg19 and The Brain Trauma Foundation advise avoidance of systolic pressures below 90 mmHg.20 A number of pre-hospital organisations have interpreted this as keeping systolic at ‘normal’ levels (100 or 120 mmHg21). Such targets lack a strong evidence base,11,22 perhaps in part because a single ideal CPP is unlikely to exist for all the different forms of brain injury and because increasing CPP also tends to increase ICP. Meanwhile, cerebral blood flow resulting from any given MAP will differ between individuals (amongst whom the range of ‘autoregulation’ of flow may vary), and with differences in the vasodilator PaCO2.23 The ‘static’ view of the factors regulating ICP, and the focus on arterial inflow alone, has meant that the important influence of cerebral veins has been almost entirely neglected.
Venous influence on ICP
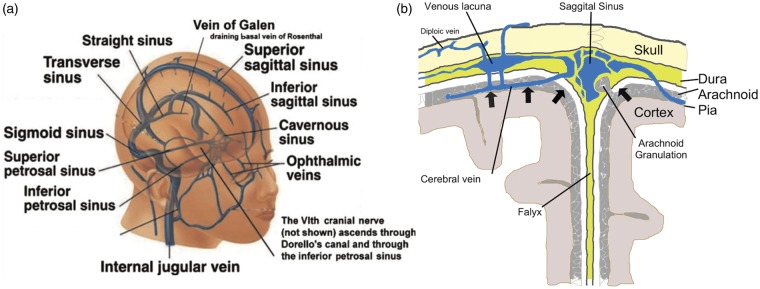
The internal jugular veins are fed from three main intra-cerebral venous drainage systems (Figure 2(a)):24
Cortical veins drain (via bridging veins) into the sagittal sinus which leads posteriorly to the torcula (confluence of sinuses) and then (in most people) to the right transverse sinus.
Deeper (anterior) venous drainage occurs into the cavernous sinuses which in turn drain via superior and inferior petrosal sinuses into the jugular bulbs.
Central (thalamic) areas drain via a series of small veins into the internal cerebral veins superiorly and the basal veins of Rosenthal inferiorly. These unite (behind the splenium of the corpus callosum) to form the Great Vein of Galen which then drains via the straight sinus into the torcula and then (in most people) to the left transverse sinus.
Figure 2.
(a) Schematic representation of the commonest pattern of cerebral venous drainage. Adapted from Wilson et al.24 (b) Cross-sectional representation of the sagittal sinus. The dural reflections create a triangular lumen with no muscular wall in marked contrast to the arterial circulation. This makes venous structures more vulnerable to compression.
Cerebral venous drainage is significantly asymmetric in circa 50% of subjects.25 Transverse sinus drainage is predominantly right sided in approximately 40% of subjects and left sided in about 18%.26,27 This can usually be demonstrated by a predominately larger sinus on CT or MR venography. Obstruction to a dominant sinus has considerably more effect than obstruction to a non-dominant one. Only a small minority of people have significant drainage through the cervical venous plexi28 which are of much greater significance in supine mammals such as swine that have not evolved to the gravitational effects of becoming bipeds.29
Unlike the strong muscular arterial walls, those of the venous sinuses (being triangular dural reflections (Figure 2(b)) are susceptible to dilatation and compression. In the sitting position, the sagittal sinus has a negative pressure that can result in (potentially fatal) air embolism if opened. When supine, bleeding from the sinuses can be torrential. Likewise, when upright, human internal jugular veins tend to collapse under negative pressure, but engorge on lying.30
A role for veins influencing ICP
Concentration on arterial inflow, and failure to consider the role of venous drainage in ICP regulation, means that much important subtlety is missed: reflection suggests that failure for venous efferent flow to precisely match arterial afferent flow (even when the failure results from intracranial venous compromise) will yield immediate and dramatic changes in intracranial volume and pressure. Interpreting the value of regulating ICP, without interrogating its core drivers, may be misleading.
In this regard, much historical work has been forgotten. Leonard Hill8 demonstrated that venous and CSF pressures were aligned and suggested that, given the lack of valves in the cranio-vertebral venous system, vena caval pressure reflected CSF pressure, and retinal venous distension could reflect intracranial venous pressure. With great insight, he suggested that ICP would be more affected by changes in vascular pressure ‘from the venous side to a far greater degree than from the arterial side, because it is on the arterial side that the resistance lies’. Similarly Bedford et al.31 and Ferris32 demonstrated the greater importance of the venous system within the Monro-Kellie doctrine. Specifically, increasing central venous pressure (CVP) results in increasing ICP when compliance is lost,33 and this in turn results in the formation of brain oedema and swelling.34 Queckenstedt’s35 manoeuvre obstructing venous outflow (which he described in 1916) clearly demonstrates the relationship between increased distal venous pressure and ICP. The velocity of blood in the straight sinus and other venous structures, as measured using transcranial Doppler, has been shown to correlate linearly with ICP.36
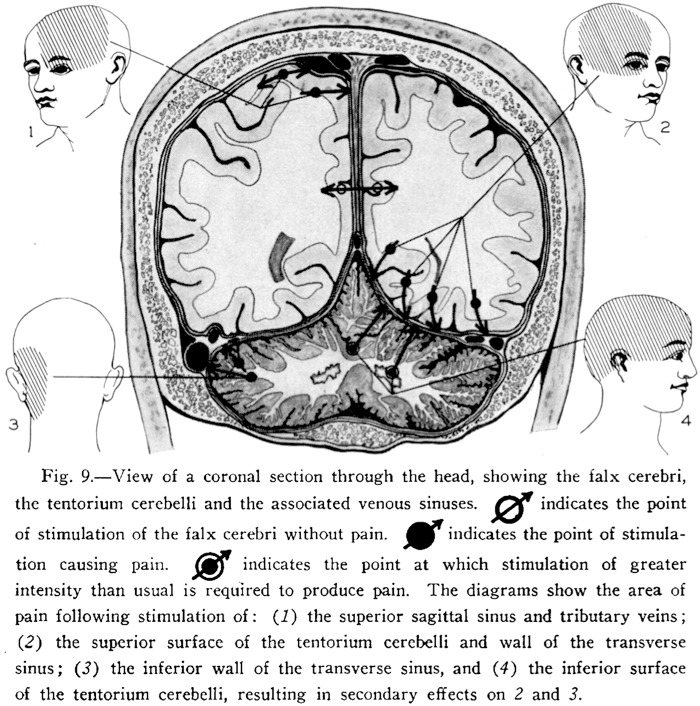
Since most neurosurgery today is performed under general anaesthesia, we are less aware of which intracranial structures are painful. Ray and Wolff37 reported multiple observations on up to 30 patient subjects.37 They demonstrated that pressure on the sinuses (particularly tension at the margins) caused significant headache pain as indicated in Figure 3. Again, the pain of venous structures has largely been forgotten.
Figure 3.
View of a coronal section through the head, showing the falx cerebri, the tentorium cerebelli, and the associated venous sinuses. The full legend is within the figure.37
Causes of raised cerebral venous pressure
Individual susceptibility to intracranial hypertension may thus be influenced by the anatomical balance of cerebral venous drainage and its compliance. As cerebral blood flow rises, so too must venous drainage. Venous distension will occur up to a limit, after which intravenous pressure (and that upstream, and thus ICP) will rise steeply (in a similar manner to when the limits of compliance are reached in the classic Monro-Kellie doctrine of Figure 1). Anatomical imbalance in venous drainage (i.e. an inability to drain venous blood adequately for a given cerebral blood inflow without raising venous pressures) will predispose to such venous and intracranial hypertension despite what may appear to be an ‘atrophic’, anatomically compliant system on plain CT. Clinically, this may present with the headache of venous distension when alert or refractory intracranial hypertension if undergoing ICP monitoring. Intracranial venous hypertension can be caused by increased venous resistance/pressures within the cranium or outside it. Within the cranium this can be focal (from outside the sinus, within the sinus wall or within the sinus lumen) or it can be diffuse compression. Further, venous hypertension can originate in the neck, thorax or abdomen. See Table 1 for a suggested classification with clinical examples.
Table 1.
Suggested classification of venous causes of intracranial hypertension.
| Classification | Location of resistance/pressure | Clinical examples | ||
|---|---|---|---|---|
| I | a | Focal extramural venous sinus compression | External compression of a significant venous sinus at a focal point | Depressed skull fracture, periosteal hematoma, tumor. |
| b | Focal intermural venous sinus stenosis | A focal narrowing within the sinus wall | Idiopathic intracranial hypertension | |
| c | Focal intramural venous sinus obstruction | Obstruction within a significant venous sinus | Sagittal or transverse sinus thrombosis. | |
| d | Diffuse venous compression | Throughout the venous tree | Any cause of cerebral swelling e.g. hypoxia, cerebral edema, contusions | |
| II | Extracranial venous hypertension – cervical | Within the neck | Cervical collars, hanging | |
| III | Extracranial venous hypertension – thoracic | Within the thorax | Any cause of increased intra-thoracic pressure – Chest infection, adult respiratory distress syndrome, mechanical ventilation | |
| IV | Extracranial venous hypertension – abdominal | Within the abdomen | Any cause of increased abdominal pressure - obesity, obstruction | |
| V | Orthostatic/gravity | Visual impairment and raised ICP/space obstruction syndrome | ||
Ia: Focal external venous compression
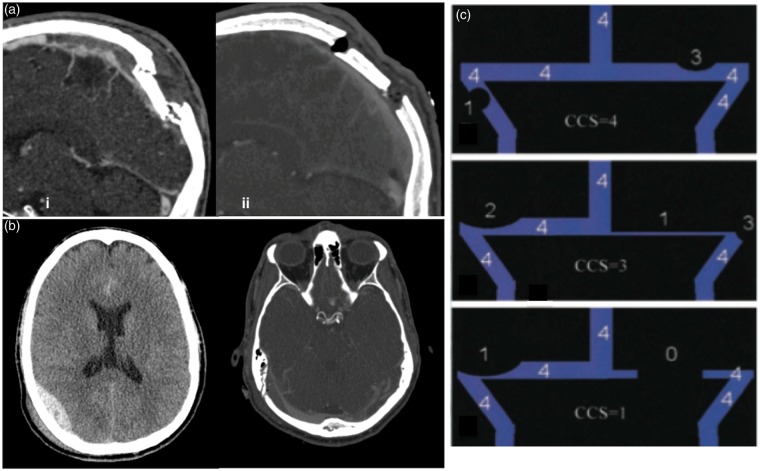
The thin dural venous sinus walls make them prone to both focal and diffuse compression. Acute compression may result from a depressed skull fracture (Figure 4(a)) or, more commonly, from an expanding mass (e.g. extradural/periosteal haematoma) that may actually be the result of a damaged sinus (Figure 4(b)). Compression may in turn lead to thrombosis and both may cause intracranial hypertension.38 The location of the fracture and sinus dominance is important in determining the consequence of this. It is our experience that occipital skull fractures over the right transverse sinus are more significant since this is the dominant sinus in most people. Fractures over a hypoplastic sinus rarely have significant effect on ICP.
Figure 4.
(a) Depressed skull fracture and subsequent (superior sagittal sinus) SSS thrombosis caused by a hammer blow – (i) midsagittal reconstruction on day 2 with increasing headaches demonstrating SSS thrombosis, (ii) – midsagittal reconstruction of CTV day 2 post op demonstrating resolution of SSS thrombosis. (b) Occipital extradural from fracture overlying the right transverse sinus. (i) plain axial CT scan, (ii) CT Venogram. The extradural can be seen compressing and narrowing the dominant right transverse sinus. Note the relatively hypoplastic left transverse sinus. (c) The combined conduit score (CCS) adapted from Farb et al.41 Each transverse sinus is assessed separately and the area with the greatest stenosis graded (0–4) in relation to the superior sagittal sinus (SSS). 0 = discontinuity/aplastic segment; 1 = hypoplasia/severe stenosis with cross-sectional diameter less than 25% of the SSS; 2 = moderate stenosis (25–50% of SSS cross-sectional area); 3 = mild stenosis (50–75% of SSS cross-sectional area), and 4 = no significant stenosis (75–100% of SSS cross-sectional area). Both left and right scores are summed to give a total CCS.
Glomus tumours can have similar effects, although slow growth allows collateral circulation development and the opening of the opposite transverse sinus and cervical plexus.39 Epidural abscesses can also restrict venous outflow.40 Of note, while lesion volume can appear small (see Figure 4(b)), the impact on ICP may be wholly unrelated and excessive (compared to the apparent reserve space/compliance of a CT image).
Treatment depends on how significant the resulting venous compromise is. A conservative management with permissive intracranial hypertension may suffice, although elevating a fracture (Figure 4(a)) or a single burr hole can reduce the mass compressing the sinus and subsequent intracranial hypertension.
Ib: Focal venous sinus stenosis
Focal transverse sinus stenosis (graded as shown in Figure 4(c))41 is associated with idiopathic intracranial hypertension (IIH characterised by headache, loss of peripheral vision and nausea).42,43 Bilateral stenosis is found in up to 90% of sufferers.44–46 Moreover, endoluminal stenting of stenotic regions can dramatically improve symptoms.45,47–49 IIH tends to be a disease of young overweight women. The additional weight may be contributory to intra-cerebral venous hypertension (through mechanisms III, IV, and V outlined below), tipping a patient that would otherwise be asymptomatic into the decompensated category.
Ic: Focal internal obstruction
Ecker50 described dural sinus thrombosis associated with skull fracture and many more cases have been reported.51–66 Nonetheless, it is considered rare – perhaps due to lack of systematic approaches to identify its presence. Indeed, in a series of 21 ventilated head injury patients with a skull fracture over the sinus, Kolias et al.67 found that sinus thrombosis was common (affecting 8 (=38%) patients) and associated with a high mortality (3 of the 8 died compared to none of the 13 without thrombosis). This group also have impaired pressure reactivity. A recent study by our group has demonstrated that 48% of patients with occipital skull fractures over the transverse sinus had thrombosis and a further 13% had external obstruction (see above) sometimes with thrombosis (n = 29).69
Treatments have included conservative management,59 acetazolamide, anticoagulation,52 ventricularperitoneal (VP) shunt insertion,53 endovascular treatment58 and decompressive craniectomy (DC).56 Conservative management is reasonable in the absence of progressive symptoms. In symptomatic cases where there is a depressed skull fracture over the sinus, elevation (raising of the depressed bone piece) should be considered if there is flow disruption or symptomatic thrombosis. This can safely be achieved by drilling off just the bone that is holding the fragment depressed and allowing it to rise (Figure 4(a)). Ozer et al.62 reported elevating 17 depressed skull fractures over sinuses.62 While they make no mention of sinus thrombosis, they reported ‘massive blood loss’ in 11 of the cases although control was regained. Two of the patients died from associated intra-cerebral lesions. If the thrombosis is progressing and results from an undisplaced fracture then endovascular treatment where available may be considered. Failure to elevate depressed skull fractures over the sagittal sinus can result in IIH.63–65,70
Id: Diffuse compression of the venous system
Diffuse brain swelling can also cause generalised venous compression creating an internal starling type resistor. Recent evidence implies that in many cases of IIH, the entire dural sinus tree appears to be compressed.71 A cycle of venous hypertension, cerebral swelling, further venous compression and therefore hypertension occurs. This cycle can be broken with CSF drainage although it is likely to recur again, not as CSF accumulates but as venous hypertension recurs. Pickard et al.46 studied CSF and sagittal sinus pressures in nine patients with IIH. During CSF, drainage CSF pressure decreased below central venous pressure (CVP), while the sagittal sinus pressure fell only to CVP and not lower. This suggests that functional obstruction of venous outflow through the dural sinuses is present in many IIH cases. Raised CSF pressure partly obstructs venous sinus outflow, thereby increasing sinus pressure and then CSF pressure, et sequor.
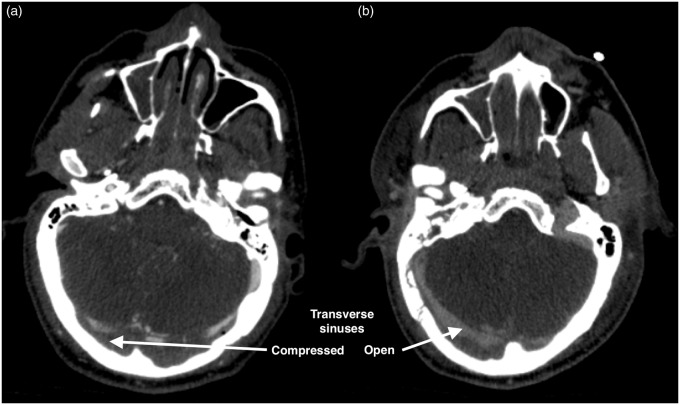
It is our experience that a similar phenomenon can occur with other causes of cerebral swelling, such as that resulting from trauma. Figure 5 is a CT venogram of a patient with diffuse cerebral swelling following trauma which also demonstrates diffuse compression of both transverse sinuses. A DC was performed for refractory high ICP. A post-operative CT venogram demonstrated marked increase in sinus calibre.
Figure 5.
CT venograms of a male patient aged 48-year-old male with refractory intracranial hypertension. (a) Transverse sinuses severely effaced with raised intracranial pressure. (b) Following bifrontal decompressive craniectomy the transverse sinus calibre increases dramatically.
The diffuse parenchymal volume increase that occurs with prolonged hypoxia (such as occurs at altitude) has recently also been demonstrated to cause venous compression which may in turn raise ICP (Sagoo et al, 2016).
Venous pressures can be inferred from brain CT scans. The superior ophthalmic vein is normally between 1.4 and 3.6 mm (mean 2.2 mm).72 Bilateral superior ophthalmic vein enlargement (considered > 2–3 mm) is associated with diffuse cerebral swelling as reported in 11 cases.73
Extracranial causes of cerebral venous hypertension
II Cervical
Neck pressure is well recognised to have a significant effect on ICP. Queckenstedt’s35 test is now an outdated technique for investigating spinal stenosis. The test comprised jugular venous compression with concurrent lumbar puncture. Those with spinal stenosis have a slower lumbar pressure CSF rise than those without. The author has modified this technique. By applying pressure over each jugular (separately) while watching invasively monitored ICP, a crude assessment can be made as to the dominance of venous drainage and the degree of venous compliance.
Poor head position is often overlooked but is an incredibly important cause of raised ICP. Mavrocordatos et al.74 in a study of elective neurosurgery patients without raised ICP (n = 15) demonstrated that ICP was lowest with the head in a neutral position. Flexion and worse still flexion with rotation caused significant increases in ICP (e.g. from mean 8.8 mmHg when neutral to 16.2 mmHg when rotated to the right and flexed). This is an even greater problem in children with larger occiputs (resulting in flexion) and floppier necks.75
Cervical collars can increase ICP from about 4.5 mmHg76–78 to as much as 14.5 mmHg,77 the rise being greater in those with baseline ICP > 15 mmHg.78 This probably reflects the degree of intracranial compliance: a patient who can accommodate less cerebral venous engorgement will have a more immediate rise in ICP. These mean pressure increases may be small, but they can have profound effects if sustained79 or if the patient is at the limit of their compliance. Stone et al.80 have recently demonstrated that collar application causes an increase in internal jugular vein cross-sectional area of 37% (95% confidence interval [CI] = 20% to 53%) strongly supporting the hypothesis that it is venous compression and resulting congestion that underlies the collar induced ICP increase. As a result, the benefits of cervical collars in the acute management of traumatic brain injury are questionable to say the least.81
Other cervical causes of acute venous hypertension include near hanging and strangulation which can induce venous/haemorrhagic infarction.82 More chronic causes include jugular syndromes blocking outflow83 and superior vena cava obstruction.84 A degree of internal jugular stenosis may also occur in patients with IIH.85
III: Intra-thoracic
Positive pressure ventilation in the treatment of chest infection and Adult Respiratory Distress syndrome (ARDS) can severely raise intra-thoracic pressure as can the application of positive end expiratory pressure (PEEP) with inter-individual variation in ICP possibly reflecting differences in venous compliance – i.e. whether venous drainage is still adequate.86,87 Intra-thoracic pressure regulator use (which apply negative pressure during the expiratory phase of ventilation with the aim of reducing intra-thoracic pressure, enhancing venous return, and increasing cardiac output) may reduce ICP.88
IV: Intra-abdominal
Abdominal compartment syndrome (raised intra-abdominal pressure causing organ dysfunction) raises ICP in brain-injured patients89 which can be reduced by decompressive laparotomy (DL).90 Of 24 patients who underwent both DC and DL for refractory ICP,90 15 underwent DC before DL and 9 underwent DL before DC. While both DL and DC significantly reduced ICP, DL, not surprisingly, also reduced intra-thoracic pressure.90 Results of DL are comparable to DC with 17 out of 17 patients (without abdominal compartment syndrome) benefiting from a reduction (mean 27.5 mmHg to 17.5 mmHg) in otherwise refractory ICP, although in six (all of whom subsequently died) this fall was transient.91
Scalea et al.’s92 team point out that fluid therapy to raise CPP may also cause retroperitoneal and visceral oedema increasing intra-abdominal pressure and interstitial pulmonary oedema (also increasing intra-thoracic pressures). It has also been suggested that the raised intra-abdominal pressures in preeclampsia cause raised cerebral venous and ICPs and contribute to the intracerebral haemorrhage that is sometimes seen.92
Figure 6 demonstrates brain herniation occurring as an abdominal wound is closed. This patient who had an acute subdural removed concurrently with a splenectomy for trauma developed acute bleeding from his right transverse sinus and brain herniation as the abdomen was closed, reflecting the rise in venous pressure.93
Figure 6.
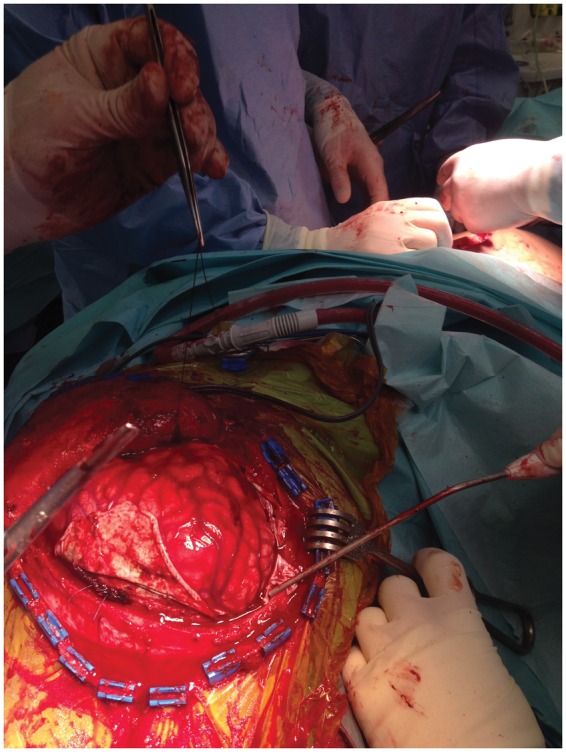
Brain herniation occurring at the time of abdominal closure (see text)93.
V: Hydrostatic/gravity–related cerebral venous hypertension
Microgravity: In recent years a very significant number of astronauts have complained of loss of peripheral vision (so-called visual impairment-ICP),94 a symptom also occurring in IIH. The lack of gravity results in upper thoracic venous hypertension and hence a similar pathological process may underlie this condition.24 This phenomenon has become a considerable problem, jeopardising human exploration to Mars until resolved.
Vasomotor tone: The administration of non-depolarising paralytic agents in intensive care can reduce ICP, while depolarising relaxants cause a transitory ICP rise.95 Both effects likely result from transmission of muscle tension through the venous system.
Hypoxia and conditions increasing CBF: Conditions that result in increased arterial inflow may ‘bring out’/decompensate venous hypertension in those with little reserve. Hypobaric hypoxia increases cerebral blood flow to maintain brain oxygenation96,97 and limitations in cerebral venous drainage may underlie the pathogenesis of high-altitude headache through cerebral venous engorgement.98 Recent work by Sagoo et al.99 have demonstrated that venous outflow restriction appears to have a contributory role in the pathogenesis of cerebral oedema.
There is increasing interest regarding the possible (and controversial) involvement of the venous system in other neurological conditions such as multiple sclerosis,100 normal pressure hydrocephalus,101 dementia102 and leukoaraiosis.103 Chronic cerebrospinal venous insufficiency and decreased venous vasculature appear to be a feature of MS, but the relationship between causation and association is not clear.104 The recent discovery of the co-location of lymphatic vessels with dural sinuses may be of relevance but further investigation is needed.105
Summary
While the traditional Monroe-Kellie doctrine holds, imbalances in arterial inflow and venous outflow also affect ICP. The venous outflow can be altered intracranially and extracranially (Figure 7). Table 2 demonstrates venous causes of intracranial hypertension and outlines treatment options.
Figure 7.
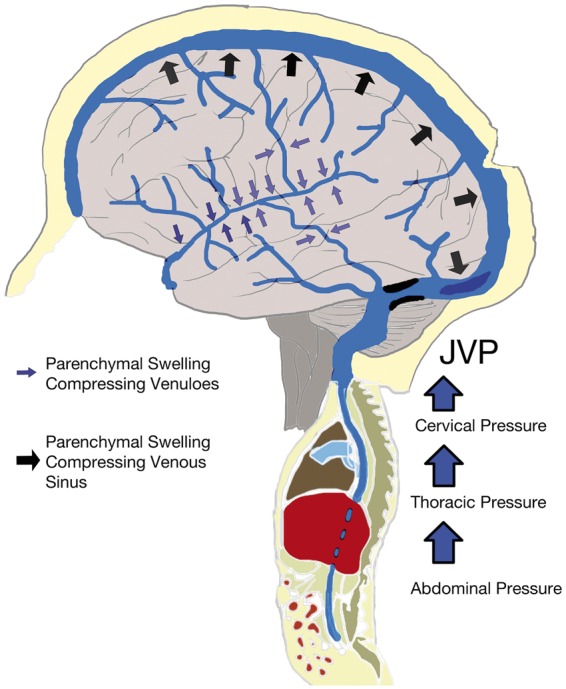
Diagram demonstrating that relative venous outflow restriction can occur intracranially (with compression/obstruction (e.g. with thrombus or fractures) of isolated or diffuse venous structures) and extracranially (from cervical, thoracic and abdominal pressures).
Table 2.
Treatment options to minimise the venous contribution of intracranial hypertension.
| Venous cause of intracranial hypertension | Treatment |
|---|---|
| Orthostatic/ hydrostatic | Avoid hypoxia. Elevate head. Avoid abdominal compression. If intubated, non-depolarising paralysis. |
| Cervical | Avoid neck vein compression (e.g. with collars) and maintain in neutral position or position where dominant jugular is optimised. Avoid “double chin” which compresses jugular. |
| Intracranial causes | Looks for dominance in transverse sinus drainage. Relieve direct sinus compression, e.g. by depressed skull fracture elevation, release of clot compressing sinus. For sinus thrombosis consider anticoagulation or interventional radiological management. Consider decompressive craniectomy. |
| Thoracic causes | Relieve causes of increased intra-thoracic pressure. Minimise risk of infection/ARDS. Ventilate with no excessive positive pressure. |
| Abdominal causes | Relieve causes of intra-abdominal hypertension. Treat constipation. Place urinary catheter. In extreme circumstances, consider decompressive laparotomy. |
Note: The order reflects the clinical order in which they are usually managed.
Conclusion
The balance between cerebral blood in and outflow is vital in maintaining normal ICP. Restrictions in outflow can be as, if not more, significant than mass accumulation within the cranium. There has been a concentration of interest in CPP and ICP; however, the considerable importance of the venous side has often been overlooked. ICP is a function of venous outflow, a combination of intra-cerebral resistance and cervical, thoracic and abdominal pressures. If there was no resistance to venous outflow ICP would be zero, hence using intravenous fluids to ‘maintain CPP’ may increase CVP and worsen ICP (and ironically CPP). The dynamic influence of blood flow on ICP is an essential component of the Monro-Kellie doctrine.
There is increasing evidence that venous pathology is central to multiple conditions that cause a rise in ICP. A greater understanding and appreciation of the role of the venous system in neuro-critical care is vital.
Acknowledgments
Professors Hugh Montgomery and John Pickard very kindly reviewed the original manuscript and advised on a number of aspects. I am extremely grateful to them for their life long support. A number of people have been involved with shaping the venous theory. They include: Chris Imray, Alan Hargens, Laurence Watkins, Martin Smith, John Pickard, Stefan Brew and Fergus Robertson. I am very grateful to all the above.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author contributions
MW authored this manuscript. The concepts were developed based on his work as a neurosurgeon, pre-hospital care physician and high-altitude research with many years working with the people listed in the Acknowledgements section.
References
- 1.Restak R. Fixing the brain. Mysteries of the mind, Washington, DC: National Geographic Society, 2000. [Google Scholar]
- 2.Monro A. Observations on the structure and function of the nervous system, Edinburgh: Creech and Johnson, 1783. [Google Scholar]
- 3.Kellie G. An account of the appearances observed in the dissection of two of the three individuals presumed to have perished in the storm of the 3rd, and whose bodies were discovered in the vicinity of Leith on the morning of the 4th November 1821 with some reflections on the pathology of the brain. Transac Medico Chirurg Soc Edinburgh 1824; 1: 84–169. [PMC free article] [PubMed] [Google Scholar]
- 4.Clarke C, Abercrombie J. Pathological and practical researches in disease of the brain and spinal cord, Edinburgh: Carey, Lea and Blanchard, 1928. [Google Scholar]
- 5.Magendie F. Recherches anatomique et physiologique sur le liquide céphalo-rachidien ou cérebro-spinal, Paris: Méquignon-Marvis fils, 1842. [Google Scholar]
- 6.Burrows G. On disorders of the cerebral circulation and on the connection between affections of the brain and diseases of the heart, Philadelphia: Lea and Blanchard, 1848. [Google Scholar]
- 7.Reid J. Burrows on cerebral circulation. Edinburgh Mon J Med Sci 1846, pp. 111–123. [Google Scholar]
- 8.Hill L. The physiology and pathology of the cerebral circulation, London: J&A Churchill, 1896. [Google Scholar]
- 9.Cushing H. The third circulation in studies in intracranial physiology and surgery, London: Oxford University Press, 1926. [Google Scholar]
- 10.Weed LH. Some limitations on the Monro-Kellie hypothesis. Arch Surg 1929; 18: 1049. [Google Scholar]
- 11.Kirkman MA, Smith M. Intracranial pressure monitoring, cerebral perfusion pressure estimation, and ICP/CPP-guided therapy: a standard of care or optional extra after brain injury? Br J Anaesth 2014; 112: 35–46. [DOI] [PubMed] [Google Scholar]
- 12.Chesnut RM, Temkin N, Carney N, et al. A trial of intracranial-pressure monitoring in traumatic brain injury. N Engl J Med 2012; 367: 2471–2481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McArdle WD, Katch FI, Katch VL. Exercise physiology, 7th ed Baltimore: Lippincott, Williams & Wilkins, 2006. [Google Scholar]
- 14.Abbott AH, Netherway DJ, Niemann DB, et al. CT-determined intracranial volume for a normal population. J Craniofac Surg 2000; 11: 211–223. [DOI] [PubMed] [Google Scholar]
- 15.Miller JD, Stanek AE, Langfitt TW. A comparison of autoregulation to changes in intracranial and arterial pressure in the same preparation. Eur Neurol 1970; 6: 34–38. [DOI] [PubMed] [Google Scholar]
- 16.Miller JD, Stanek A, Langfitt TW. Concepts of cerebral perfusion pressure and vascular compression during intracranial hypertension. Prog Brain Res 1971; 35: 411–432. [DOI] [PubMed] [Google Scholar]
- 17.Johnston IH, Rowan JO. Raised intracranial pressure and cerebral blood flow. 3. Venous outflow tract pressures and vascular resistances in experimental intracranial hypertension. J Neurol Neurosurg Psychiatry 1974; 37: 392–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maas AIA, Dearden MM, Teasdale GMG, et al. EBIC-guidelines for management of severe head injury in adults. Acta Neurochir (Wien) 1997; 139: 286–294. [DOI] [PubMed] [Google Scholar]
- 19.Recommendations for the safe transfer of patients with brain injury. London, 2006, www.aagbi.org/sites/default/files/braininjury.pdf. (accessed 23 April 2016).
- 20.Brain Trauma Foundation, American Association of Neurological Surgeons, Congress of Neurological Surgeons, et al. Guidelines for the management of severe traumatic brain injury. I. Blood pressure and oxygenation. J Neurotrauma 2008; 25: 276–278. [Google Scholar]
- 21.South Western Ambulance Service. swast.nhs.uk. 2013, www.swast.nhs.uk/Downloads/Clinical%20Guidelines%20SWASFT%20staff/CG12_Head_Injury.pdf (8 accessed June 2014).
- 22.Harris TT, Thomas GORG, Brohi KK. Early fluid resuscitation in severe trauma. BMJ 2012; 345: e5752–e5752. [DOI] [PubMed] [Google Scholar]
- 23.Coles JPJ, Minhas PS, Fryer TD, et al. Effect of hyperventilation on cerebral blood flow in traumatic head injury: clinical relevance and monitoring correlates. Crit Care Med 2002; 30: 1950–1959. [DOI] [PubMed] [Google Scholar]
- 24.Wilson MH, Imray CHE, Hargens AR. The headache of high altitude and microgravity–similarities with clinical syndromes of cerebral venous hypertension. High Alt Med Biol 2011; 12: 379–386. [DOI] [PubMed] [Google Scholar]
- 25.Beards SCS, Yule SS, Kassner AA, et al. Anatomical variation of cerebral venous drainage: the theoretical effect on jugular bulb blood samples. Anaesthesia 1998; 53: 627–633. [DOI] [PubMed] [Google Scholar]
- 26.Boushel R, Durgun BB, Ilglt ETE, et al. Evaluation by angiography of the lateral dominance of the drainage of the dural venous sinuses. Surg Radiol Anat 1993; 15: 125–130. [DOI] [PubMed] [Google Scholar]
- 27.Singh M, Nagashima M, Inoue Y. Anatomical variations of occipital bone impressions for dural venous sinuses around the torcular Herophili, with special reference to the consideration of clinical significance. Surg Radiol Anat 2004; 26: 480–487. [DOI] [PubMed] [Google Scholar]
- 28.Doepp F, Schreiber SJ, Munster TV, et al. How does the blood leave the brain? A systematic ultrasound analysis of cerebral venous drainage patterns. Neuroradiology 2004; 46: 565–570. [DOI] [PubMed] [Google Scholar]
- 29.Lavoie P, Metellus P, Velly L, et al. Functional cerebral venous outflow in swine and baboon: feasibility of an intracranial venous hypertension model. J Invest Surg 2008; 21: 323–329. [DOI] [PubMed] [Google Scholar]
- 30.Gisolf J, Van Lieshout JJ, van Heusden K, et al. Human cerebral venous outflow pathway depends on posture and central venous pressure. J Physiol 2004; 560: 317–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bedford THB, Burgess KR, Johnson P, et al. The effect of increased intracranial venous pressure on the pressure of the cerberospinal fluid. Brain 1935; 58: 429–447. [Google Scholar]
- 32.Ferris EB. The effect of high intracranial venous pressure upon the cerebral circulation and its relation to cerebral symptoms. J Clin Invest 1939; 18: 19–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Raisis JE, Kindt GW, McGillicuddy JE, et al. The effects of primary elevation of cerebral venous pressure on cerebral hemodynamics and intracranial pressure. J Surg Res 1979; 26: 101–107. [DOI] [PubMed] [Google Scholar]
- 34.Cuypers J, Cuypers J, Matakas F, et al. Effect of central venous pressure on brain tissue pressure and brain volume. J Neurosurg 1976; 45: 89–94. [DOI] [PubMed] [Google Scholar]
- 35.Queckenstedt H. Diagnose der Ruckenmark-kompression. Deut Nervenheilkd 1916; 55: 325. [Google Scholar]
- 36.Schoser BG, Riemenschneider N, Hansen HC. The impact of raised intracranial pressure on cerebral venous hemodynamics: a prospective venous transcranial Doppler ultrasonography study. J Neurosurg 1999; 91: 744–749. [DOI] [PubMed] [Google Scholar]
- 37.Ray BS, Wolff HG. Experimental studies on headache: pain-sensitive structures of the head and their significance in headache. Arch Surg 1940; 4: 813–856. [Google Scholar]
- 38.Maurice-Williams RSR, DeLong WB, Burney RE. Lateral sinus compression from an epidural hematoma: report of a patient with delayed neurological deterioration. Mil Med 1969; 134: 521–524. [PubMed] [Google Scholar]
- 39.Goldsmith P, Burn DJ, Coulthard AA, et al. Extrinsic cerebral venous sinus obstruction resulting in intracranial hypertension. Postgrad Med J 1999; 75: 550–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ludemann JP, Poskitt K, Singhal A. Intracranial hypertension secondary to sigmoid sinus compression by group a streptococcal epidural abscess. J Laryngol Otol 2010; 124: 93–95. [DOI] [PubMed] [Google Scholar]
- 41.Farb RI, Vanek I, Scott JN, et al. Idiopathic intracranial hypertension: the prevalence and morphology of sinovenous stenosis. Neurology 2003; 60: 1418–1424. [DOI] [PubMed] [Google Scholar]
- 42.Binder DK, Horton JC, Lawton MT, et al. Idiopathic intracranial hypertension. Neurosurgery 2004; 54: 538–51. discussion 551–552. [DOI] [PubMed] [Google Scholar]
- 43.Ball AK, Clarke CE. Idiopathic intracranial hypertension. Lancet Neurol 2006; 5: 433–442. [DOI] [PubMed] [Google Scholar]
- 44.Bono F, Giliberto C, Mastrandrea C, et al. Transverse sinus stenoses persist after normalization of the CSF pressure in IIH. Neurology 2005; 65: 1090–1093. [DOI] [PubMed] [Google Scholar]
- 45.Higgins JNP, Cousins C, Owler BK, et al. Idiopathic intracranial hypertension: 12 cases treated by venous sinus stenting. J Neurol Neurosurg Psychiatry 2003; 74: 1662–1666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pickard JD, Czosnyka Z, Czosnyka M, et al. Coupling of sagittal sinus pressure and cerebrospinal fluid pressure in idiopathic intracranial hypertension – a preliminary report. Acta Neurochir Suppl 2008; 102: 283–285. [DOI] [PubMed] [Google Scholar]
- 47.Donnet A, Metellus P, Levrier O, et al. Endovascular treatment of idiopathic intracranial hypertension: clinical and radiologic outcome of 10 consecutive patients. Neurology 2008; 70: 641–647. [DOI] [PubMed] [Google Scholar]
- 48.Higgins J, Owler BK, Cousins C, et al. Venous sinus stenting for refractory benign intracranial hypertension. Lancet 2002; 359: 228–230. [DOI] [PubMed] [Google Scholar]
- 49.Owler BK, Parker G, Halmagyi GM, et al. Cranial venous outflow obstruction and pseudotumor cerebri syndrome. Adv Tech Stand Neurosurg 2005; 30: 107–174. [DOI] [PubMed] [Google Scholar]
- 50.Ecker AD. Linear fracture of the skull across the venous sinuses. N Y State J Med 1946; 46: 1120. [PubMed] [Google Scholar]
- 51.Kumar GSSG, Chacko AGA, Chacko MM. Superior sagittal sinus and torcula thrombosis in minor head injury. Neurol India 2004; 52: 123–124. [PubMed] [Google Scholar]
- 52.Dalgiç AA, Seçer MM, Ergüngör FF, et al. Dural sinus thrombosis following head injury: report of two cases and review of the literature. Turk Neurosurg 2008; 18: 70–77. [PubMed] [Google Scholar]
- 53.Forbes JA, Reig AS, Tomycz LD, et al. Intracranial hypertension caused by a depressed skull fracture resulting in superior sagittal sinus thrombosis in a pediatric patient: treatment with ventriculoperitoneal shunt insertion. J Neurosurg Pediatr 2010; 6: 23–28. [DOI] [PubMed] [Google Scholar]
- 54.Kabataş SS, Civelek EE, Sencer AA, et al. [A case of superior sagittal sinus thrombosis after closed head injury]. Ulus Travma Acil Cerrahi Derg 2004; 10: 208–211. [PubMed] [Google Scholar]
- 55.Kobayashi S, Hongo K, Koyama T, et al. Re-occlusion of the superior sagittal sinus after surgical recanalisation. J Clin Neurosci 2004; 11: 322–324. [DOI] [PubMed] [Google Scholar]
- 56.Barbati G, Montà G, Coletta R, et al. Post-traumatic superior sagittal sinus thrombosis. Case report and analysis of the international literature. Minerva Anestesiol 2003; 69: 919–925. [PubMed] [Google Scholar]
- 57.Ferrera PC. Sagittal sinus thrombosis after closed head injury. Am J Emerg Med 1998; 16: 4–4. [DOI] [PubMed] [Google Scholar]
- 58.Kuether TA, O'Neill O, Nesbit GM, et al. Endovascular treatment of traumatic dural sinus thrombosis: case report. Neurosurgery 1998; 42: 1163–1166. discussion 1166–1167. [DOI] [PubMed] [Google Scholar]
- 59.Satoh HH, Uozumi TT, Kiya KK, et al. [Venous thrombosis after closed head injury: a report of two cases presenting as intracranial hypertension]. No Shinkei Geka 1993; 21: 953–957. [PubMed] [Google Scholar]
- 60.Hesselbrock RR, Theis MK, Sawaya RR, et al. Superior sagittal sinus thrombosis after closed head injury. Neurosurgery 1985; 16: 825–828. [DOI] [PubMed] [Google Scholar]
- 61.Plessis du JJ. Depressed skull fracture involving the superior sagittal sinus as a cause of persistent raised intracranial pressure: a case report. J Trauma 1993; 34: 290–292. [DOI] [PubMed] [Google Scholar]
- 62.Ozer FD, Yurt A, Sucu HK, et al. Depressed fractures over cranial venous sinus. J Emerg Med 2005; 29: 137–139. [DOI] [PubMed] [Google Scholar]
- 63.Yokota H, Eguchi T, Nobayashi M, et al. Persistent intracranial hypertension caused by superior sagittal sinus stenosis following depressed skull fracture. Case report and review of the literature. J Neurosurg 2006; 104: 849–852. [DOI] [PubMed] [Google Scholar]
- 64.Vender JR, Bierbrauer K. Delayed intracranial hypertension and cerebellar tonsillar necrosis associated with a depressed occipital skull fracture compressing the superior sagittal sinus. Case report. J Neurosurg 2005; 103: 458–461. [DOI] [PubMed] [Google Scholar]
- 65.Fuentes SS, Bärtsch P, Metellus PP, et al. Depressed skull fracture overlying the superior sagittal sinus causing benign intracranial hypertension. Description of two cases and review of the literature. Br J Neurosurg 2005; 19: 438–442. [DOI] [PubMed] [Google Scholar]
- 66.Donovan DJD. Simple depressed skull fracture causing sagittal sinus stenosis and increased intracranial pressure: case report and review of the literature. Surg Neurol 2005; 63: 4–4. [DOI] [PubMed] [Google Scholar]
- 67.Kolias AG, Higgins JN, Scoffings DJ, et al. Skull fractures in patients with traumatic brain injury: when to consider CT venography? Brit J Neurosurg 2012; 26: 132–174. [Google Scholar]
- 68.Kolias AG, Czosnyka M, Smielewski P, et al. Post-traumatic venous outflow obstruction: the effects on intracranial pressure, cerebrovascular pressure reactivity and outcome. w3.cns.org. 2012, http://w3.cns.org/dp/2012CNS/1394.pdf (accessed 4 October 2012).
- 69.Hendrickson S, Murahari S, Scotter J, et al. Venous sinus injuries are common with occipital skull fractures. Scand J Trauma Resusc Emerg Med 2014; 22: O8. [Google Scholar]
- 70.Uzan M, Ciplak N, Dashti SG, et al. Depressed skull fracture overlying the superior sagittal sinus as a cause of benign intracranial hypertension. Case report. J Neurosurg 1998; 88: 598–600. [DOI] [PubMed] [Google Scholar]
- 71.Rohr A, Bindeballe J, Riedel C, et al. The entire dural sinus tree is compressed in patients with idiopathic intracranial hypertension: a longitudinal, volumetric magnetic resonance imaging study. Neuroradiology 2012; 54: 25–33. [DOI] [PubMed] [Google Scholar]
- 72.Brightbill TC, Martin SB, Bracer R. The diagnostic significance of large superior ophthalmic veins in patients with normal and increased intracranial pressure: CT and MR evaluation. Neuro Ophthal 2001; 26: 93–101. [Google Scholar]
- 73.Khanna RK, Pham CJ, Malik GM, et al. Bilateral superior ophthalmic vein enlargement associated with diffuse cerebral swelling. Report of 11 cases. J Neurosurg 1997; 86: 893–897. [DOI] [PubMed] [Google Scholar]
- 74.Mavrocordatos P, Bissonnette B, Ravussin P. Effects of neck position and head elevation on intracranial pressure in anaesthetized neurosurgical patients: preliminary results. J Neurosurg Anesthesiol 2000; 12: 10–14. [DOI] [PubMed] [Google Scholar]
- 75.Goldberg RN, Joshi A, Moscoso P, et al. The effect of head position on intracranial pressure in the neonate. Crit Care Med 1983; 11: 428–430. [DOI] [PubMed] [Google Scholar]
- 76.Mobbs RJ, Vuyk J, Van Den Bos J, et al. Effect of cervical hard collar on intracranial pressure after head injury. ANZ J Surg 2002; 72: 389–391. [DOI] [PubMed] [Google Scholar]
- 77.Davies G, Deakin C, Wilson A. The effect of a rigid collar on intracranial pressure. Injury 1996; 27: 647–649. [DOI] [PubMed] [Google Scholar]
- 78.Hunt K, Hallworth S, Smith M. The effects of rigid collar placement on intracranial and cerebral perfusion pressures. Anaesthesia 2001; 56: 511–513. [DOI] [PubMed] [Google Scholar]
- 79.Craig GR, Nielsen MS. Rigid cervical collars and intracranial pressure. Intensive Care Med 1991; 17: 504–505. [DOI] [PubMed] [Google Scholar]
- 80.Stone MB, Tubridy CM, Curran R. The effect of rigid cervical collars on internal jugular vein dimensions. Acad Emerg Med 2010; 17: 100–102. [DOI] [PubMed] [Google Scholar]
- 81.Sundstrøm T, Asbjørnsen H, Habiba S, et al. Prehospital use of cervical collars in trauma patients: a critical review. J Neurotrauma 2014; 31: 531–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Nakajo M, Onohara S, Shinmura K, et al. Computed tomography and magnetic resonance imaging findings of brain damage by hanging. J Comput Assist Tomogr 2003; 27: 896–900. [DOI] [PubMed] [Google Scholar]
- 83.Graus FF, Slatkin NEN. Papilledema in the metastatic jugular foramen syndrome. Arch Neurol 1983; 40: 816–818. [DOI] [PubMed] [Google Scholar]
- 84.Al-Hilali N, Nampoory MR, Ninan VT, et al. The superior vena cava syndrome: late presentation after hemodialysis catheter removal. Saudi J Kidney Dis Transpl 2003; 14: 186–189. [PubMed] [Google Scholar]
- 85.Alperin N, Roach RC, Lee SH, et al. Evidence for the importance of extracranial venous flow in patients with idiopathic intracranial hypertension (IIH). Acta Neurochir Suppl 2004; 95: 129–132. [DOI] [PubMed] [Google Scholar]
- 86.Yang Z-J, Zhang X-Y, Shen J-F, et al. [The impact of positive end-expiratory pressure on cerebral perfusion pressure and hemodynamics in patients receiving lung recruitment maneuver]. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue 2008; 20: 588–591. [PubMed] [Google Scholar]
- 87.Pulitanò S, Mancino A, Pietrini D, et al. Effects of positive end expiratory pressure (PEEP) on intracranial and cerebral perfusion pressure in pediatric neurosurgical patients. J Neurosurg Anesthesiol 2013; 25: 330–334. [DOI] [PubMed] [Google Scholar]
- 88.Kiehna EN, Huffmyer JL, Thiele RH, et al. Use of the intrathoracic pressure regulator to lower intracranial pressure in patients with altered intracranial elastance: a pilot study. J Neurosurg 2013; 119: 756–759. [DOI] [PubMed] [Google Scholar]
- 89.Citerio G, Vascotto E, Villa F, et al. Induced abdominal compartment syndrome increases intracranial pressure in neurotrauma patients: a prospective study. Crit Care Med 2001; 29: 1466–1471. [DOI] [PubMed] [Google Scholar]
- 90.Scalea TM, Bochicchio GV, Habashi N, et al. Increased intra-abdominal, intrathoracic, and intracranial pressure after severe brain injury: multiple compartment syndrome. J Trauma 2007; 62: 647–656. [DOI] [PubMed] [Google Scholar]
- 91.Guinet P, Joseph DK, Schneider SM, et al. Decompressive laparotomy to treat intractable intracranial hypertension after traumatic brain injury. J Trauma 2004; 57: 687–693. discussion: 693–695. [DOI] [PubMed] [Google Scholar]
- 92.Sugerman HJ. Hypothesis: preeclampsia is a venous disease secondary to an increased intra-abdominal pressure. Med Hypotheses 2011; 77: 841–849. [DOI] [PubMed] [Google Scholar]
- 93.Hendrickson S, Chacko L, Wilson MH. Raised intracranial pressure following abdominal closure in a polytrauma patient. JRSM Open 2015; 6: 2054270414565958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Fogarty JA, Otto C, Kerstman E, et al. Visual Impairement Intracranial Pressure Summit Report. ston.jsc.nasa.gov. 2011, http://ston.jsc.nasa.gov/collections/trs/_techrep/TP-2011-216160.pdf (accessed 8 June 2014).
- 95.Bozeman WP, Idris AH. Intracranial pressure changes during rapid sequence intubation: a swine model. J Trauma 2005; 58: 278–283. [DOI] [PubMed] [Google Scholar]
- 96.Willie CK, Macleod DB, Shaw AD, et al. Regional brain blood flow in man during acute changes in arterial blood gases. J Physiol 2012; 590: 3261–3275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Wilson MH, Edsell MEG, Davagnanam I, et al. Cerebral artery dilatation maintains cerebral oxygenation at extreme altitude and in acute hypoxia – an ultrasound and MRI study. J Cereb Blood Flow Metab 2011; 31: 2019–2029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wilson MH, Davagnanam I, Holland G, et al. Cerebral venous system and anatomical predisposition to high-altitude headache. Ann Neurol 2013; 73: 381–389. [DOI] [PubMed] [Google Scholar]
- 99.Sagoo RS, Hutchinson CE, Wright A, et al. Magnetic resonance investigation into the mechanisms involved in the development of high-altitude cerebral edema. J Cereb Blood Flow Metab. . Epub ahead of print 8 January 2016. DOI: 10.1177/0271678X15625350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Zamboni P, Menegatti E, Weinstock-Guttman B, et al. The severity of chronic cerebrospinal venous insufficiency in patients with multiple sclerosis is related to altered cerebrospinal fluid dynamics. Funct Neurol 2009; 24: 133–138. [PubMed] [Google Scholar]
- 101.Bateman GA. The pathophysiology of idiopathic normal pressure hydrocephalus: cerebral ischemia or altered venous hemodynamics? AJNR Am J Neuroradiol 2008; 29: 198–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Chung C-P, Wang P-N, Wu Y-H, et al. More severe white matter changes in the elderly with jugular venous reflux. Ann Neurol 2011; 69: 553–559. [DOI] [PubMed] [Google Scholar]
- 103.Rohr A, Mórocz IA, Chung C-PC, et al. Pathogenesis of leukoaraiosis: Role of jugular venous reflux. MedHypotheses 2010; 75: 6–6. [DOI] [PubMed] [Google Scholar]
- 104.Zivadinov RR, Poloni GUG, Marr KK, et al. Decreased brain venous vasculature visibility on susceptibility-weighted imaging venography in patients with multiple sclerosis is related to chronic cerebrospinal venous insufficiency. BMC Neurol 2011; 11: 128–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Louveau A, Smirnov I, Keyes TJ, et al. Structural and functional features of central nervous system lymphatic vessels. Nature 2015; 523: 337–341. [DOI] [PMC free article] [PubMed] [Google Scholar]