Abstract
Objective
We try to analyse the effect of renal functions on death in CAD patients with different body compositions.
Methods
A retrospective analysis was conducted in 2989 consecutive patients with CAD confirmed by coronary angiography were enrolled and were grouped into two categories: basically preserved renal function (PRF) (eGFR ≥60 ml/min) and obviously reduced renal function (RRF) (eGFR <60 ml/min). The influence of renal insufficiency on mortality of CAD was detected in every tertile of body composition, including body mass index (BMI), body fat (BF) and lean mass index (LMI). The end points were all-cause mortality.
Results
The mean follow-up time was 29.1 ± 12.5 months and death events occurred in 271 cases. The percentage of patients with RRF was positively correlated with BF and inversely correlated with the LMI, but no relationship to BMI. The survival curves showed that the risk of death was significantly higher in the RRF patients in all subgroups stratified using BMI, BF, or LMI (log rank test, all p < 0.001). The COX multivariate regression analysis showed that the risk of death was significantly higher in the RRF patients with high BF (HR 1.95, CI 1.25–3.05) and low LMI (HR 1.82, CI 1.19–2.79). Meanwhile, risk of death was significantly higher in RRF patients with a high BMI (HR 2.08, CI 1.22–3.55) or low BMI (HR 1.98, CI 1.28–3.08) but this risk was not significant in patients with a medium BMI (HR 1.12, 0.65–1.94). The subgroup analysis of patients with acute coronary syndrome (ACS) showed similar results.
Conclusions
For patients with CAD, renal insufficiency was positively correlated with BF, inversely correlated with LMI, and unrelated to BMI. The effect of renal insufficiency on the risk of death of CAD was related to body composition.
Keywords: Coronary artery disease, Renal function, Body composition, Prognosis
Background
Obesity is becoming one of the most important global health problems. According to the World Health Organization (WHO) survey in 2008, approximately 35 % of adults over the age of 20 were overweight worldwide, accounting for 34 % of men and 35 % of women in this age group, and 10 % of men and 14 % of women were obese [1]. In China, the overweight population grew by nearly 50 % from 1992 to 2008 [2]. Studies have shown that obesity is associated with a range of chronic diseases, such as hypertension, high cholesterol, diabetes, coronary artery disease (CAD), and chronic renal insufficiency [3–5]. Because obesity is a risk factor for both CAD and chronic renal insufficiency, patients with CAD are prone to obesity and renal insufficiency. A range of studies suggested that renal dysfunction was an independent risk factor for death in patients with CAD [6, 7]. Researchers have conducted numerous studies on the relationship between obesity and the outcome of CAD but have reached different conclusions. Recently, researchers have proposed the theory of the “obesity paradox” [8, 9], and studies have shown that the obesity paradox applies to chronic kidney disease in addition to CAD [10, 11]. At present, few studies have been conducted to investigate the effect of renal insufficiency on the outcome of coronary artery disease in patients with different body compositions.
In this study, we evaluated body fat with body composition-related parameters, such as the body mass index (BMI), body fat (BF), and lean mass index (LMI), and analysed the effect of renal functions on death in CAD patients with different body compositions.
Methods
Study population
The data source for this investigation was the West China Hospital CAD database. This single center database prospectively includes all the CAD or high risk patients undergoing angiography in West China Hospital affiliated to Sichuan University. For this analysis, we enrolled consecutive patients with CAD from July 2008 to January 2012 of the database. Patients with CAD were eligible for inclusion if they were restricted to participants with angiographic evidence of ≥50 % stenosis in ≥1 coronary vessels. In addition to the above angiographic criteria, patients with acute coronary symdrome (ACS) were eligible for inclusion if they had the following criteria: (1) ischemic chest discomfort that increased or occurred at rest; and (2) elevated cardiac troponin I levels (≥0.03 μg/L) or elevated cardiac troponin T levels (≥42 ng/L); and/or (3) new or presumably new electrocardiographic deviation in at least two contiguous leads [either pathologic Q waves (≥0.04 s in duration), ST segment dynamic horizontal/down-sloping depression ≥0.05 mV, or persistent ST segment elevation ≥0.1 mV in ≥2 contiguous precordial leads or ≥2 adjacent limb leads or new left bundle branch block (LBBB)]. The exclusion criteria included malignancies, pregnancy, end stage renal disease (ESRD) with hemodialysis or renal transplant and severe liver or hematological diseases. These inclusion and exclusion criteria were met by 3365 continuously enrolled CAD patients. After excluding patients with loss of follow-up (n = 287) or incomplete follow-up data (n = 89), 2989 patients were included in the data analysis. The study protocol was approved by the local institutional review boards in accordance with the Declaration of Helsinki. All subjects provided written informed consent before enrolment.
Baseline characteristics
Demographic data, medical history, cardiovascular risk factor, vital signs at admission, medication at discharge, and final diagnosis were obtained from the patients’ electronic medical records and reviewed by a trained study coordinator. Blood sample were collected before angiography, and plasma biomarkers including liver and kidney function (including the admission SCr levels), blood glucose, serum lipid, etc. were analyzed in the department of Laboratory Medicine, West China hospital, accredited by the College of American Pathologists. Hypertension was defined as those with systolic blood pressure (SBP) ≥140 mm Hg and/or diastolic blood pressure (DBP) ≥90 mm Hg and/or those receiving antihypertensive medications. Diabetes mellitus (DM) was diagnosed in patients who had previously undergone dietary treatment for diabetes, had received additional oral antidiabetic or insulin medication or had a current fasting blood glucose level of ≥7.0 mmol/L or random blood glucose level ≥11.1 mmol/L. Patients received care according to the usual practice; treatment was not affected by participation in this study.
Body composition assessment
During hospitalization, body height and weight of the patients were measured by nurses using standard methods. BMI was calculated as weight (kg) divided by the square of height (m2). BF was estimated using the Clínica Universidad de Navarra—Body Adiposity Estimator (CUN-BAE) equation: BF = −44.988 + (0.503 × age) + (10.689 × sex) + (3.172 × BMI) − (0.026 × BMI2) + (0.181 × BMI × sex) − (0.02 × BMI × age) − (0.005 × BMI2 × sex) + (0.00021 × BMI2 × age), where sex is replaced by 0 for male and 1 for female individuals [12]. This formula has been validated in a large population [13]. The LMI was calculated as follows: (1 − %BF) × BMI kg/m2 [14]. As no reference value has been recommended for Chinese population, we divided the study patients into three groups according to the tertiles of sex-specific BMI, LMI, or BF.
Renal function assessment
SCr was finished before the angiography within first 24 h after admission and assessed by a nonkinetic alkaline picrate (Jaffe) method. The Modification of Diet in Renal Disease (MDRD) equation was used to estimate glomerular filtration rate (eGFR) in milliliters per minute per 1.73 m2 [15]. Patients were divided into two eGFR groups: the basically preserved renal function (PRF) group [normal or mildly impaired renal function corresponding to strata used to define chronic kidney disease (CKD) stages [16], eGFR ≥60 ml/min] and the obviously reduced renal function (RRF) group (moderately or severely impaired renal function, eGFR <60 ml/min).
Follow-up and end points
The follow-up period ended on January 2013. Follow-up information was collected through contact with patients’ physicians, patients or their family. All data were corroborated with the hospital records. The primary end points in this study were all-cause mortality and the secondary end points were cardiovascular death, as documented in the database. Death was considered cardiac when it was caused by acute MI, significant arrhythmias, or refractory heart failure. Sudden unexpected death occurring without another explanation was included as cardiovascular death.
Statistical analyses
We conducted the post hoc analysis on a retrospective basis. Baseline demographics and clinical characteristics were compared among patients categorized by the admission eGFR levels in two groups. Continuous variables are expressed as the mean ± standard deviation (SD), and categorical variables are reported as counts and percentages. Analysis of t test and Chi squared tests were used to test for differences between groups for continuous and categorical variables, respectively. The comparisons of the distribution of eGFR <60 min/ml across the body composition tertiles were performed in Chi squared tests. To determine the association between renal function and all-cause mortality, Kaplan–Meier curves by eGFR levels were constructed in different body composition strata and examined using the log-rank test for comparison, respectively. Hazard ratios (HRs) and 95 % confidence intervals (CIs) were calculated based on Cox proportional hazards regression models, which was used to investigate the independent effect of renal function on the outcome events. Adjustments were made for the possible confounding effects of age, sex, medical history (pre-hypertension and pre-diabetes mellitus), heart function (Killip level), severity of CAD (left main artery and three vessel diseases), discharge medications [statin, angiotensin-converting enzyme (ACE) inhibitors or angiotensin-receptor blockers (ARBs) and beta-receptor blockers]. Two-sided p values of less than 0.05 indicated statistical significance. All analyses were performed with SPSS software (version 19.0).
Results
A total of 2989 patients with coronary artery disease were included in this study. The patients were aged 64.5 ± 10.6 years on average, and 20.5 % were women. SCr was determined within 24 h after admission. The mean estimated glomerular filtration rate (eGFR) was 79.5 ± 22.9 ml/min, with an eGFR <60 ml/min in 506 patients (16.9 %). The baseline data are shown in Table 1. Significant differences were observed in the clinical characteristics between groups, with more severe renal insufficiency associated with an older age, female gender, and comorbidities such as hypertension, diabetes, cardiac dysfunction, and complex CAD.
Table 1.
Baseline characteristics of the study population
| Characteristics | eGFR | p value | ||
|---|---|---|---|---|
| Total | <60 mL/min | ≥60 mL/min | ||
| No. of patients | n = 2989 | n = 506 | n = 2483 | |
| Age, years | 64.5 ± 10.6 | 70.4 ± 8.0 | 63.3 ± 10.7 | <0.001 |
| Gender, female, n (%) | 614 (20.5) | 162 (32.0) | 452 (18.2) | <0.001 |
| Body composition parameters | ||||
| BMI, kg/m2 | 24.2 ± 2.9 | 24.1 ± 2.8 | 24.2 ± 2.9 | 0.477 |
| BF, % | 28.1 ± 6.2 | 30.2 ± 6.6 | 27.7 ± 6.0 | <0.001 |
| LMI, kg/m2 | 17.3 ± 1.8 | 16.7 ± 1.9 | 17.4 ± 1.8 | <0.001 |
| Medical history | ||||
| Current smoking, n (%) | 902 (30.2) | 151 (29.8) | 751 (30.2) | 0.857 |
| Pre-hypertension, n (%) | 1628 (54.5) | 352 (69.6) | 1276 (51.4) | <0.001 |
| Pre-diabetes mellitus, n (%) | 653 (21.8) | 154 (30.4) | 499 (20.1) | <0.001 |
| At admission | ||||
| Systolic blood pressure, mm Hg | 130.3 ± 21.2 | 132.0 ± 24.1 | 129.9 ± 20.6 | 0.059 |
| Diastolic blood pressure, mm Hg | 76.3 ± 12.5 | 74.2 ± 13.4 | 76.7 ± 12.3 | <0.001 |
| Heart rate, beats/min | 74.1 ± 13.9 | 76.3 ± 16.1 | 73.6 ± 13.4 | 0.001 |
| Killip classification ≥ II, n (%) | 344 (11.5) | 93 (18.4) | 251 (10.1) | <0.001 |
| Laboratory values | ||||
| eGFR, ml/min/1.73 m2 | 79.5 ± 22.9 | 45.9 ± 12.4 | 86.3 ± 18.0 | <0.001 |
| Blood glucose, mmol/L | 6.9 ± 3.1 | 7.7 ± 4.1 | 6.8 ± 2.8 | <0.001 |
| Total cholesterol, mmol/L | 4.1 ± 1.1 | 4.0 ± 1.1 | 4.1 ± 1.1 | 0.222 |
| Diagnosis | ||||
| ACS, n (%) | 2163 (72.4) | 382 (75.5) | 1781 (71.7) | 0.084 |
| UA, n (%) | 1533 (51.3) | 257 (50.8) | 1276 (51.4) | 0.806 |
| Severity of CAD | ||||
| Left main artery, n (%) | 282 (9.4) | 54 (10.7) | 228 (9.2) | 0.296 |
| Three vessel diseases, n (%) | 758 (25.4) | 176 (34.8) | 582 (23.4) | <0.001 |
| Discharge medication | ||||
| Aspirin, n (%) | 2760 (92.3) | 432 (85.4) | 2328 (93.8) | <0.001 |
| Clopidogrel, n (%) | 2670 (89.3) | 428 (84.6) | 2242 (90.3) | <0.001 |
| Statin, n (%) | 2678 (89.6) | 432 (85.4) | 2246 (90.5) | 0.001 |
| ACE inhibitors or ARBs, n (%) | 1702 (56.9) | 290 (57.3) | 1412 (56.9) | 0.854 |
| Beta-receptor blockers, n (%) | 1981 (66.3) | 301 (59.5) | 1680 (67.7) | <0.001 |
Data are expressed as mean ± SD or counts and percentages, as appropriate
BMI body mass index; BF body fat; LMI lean mass index; eGFR estimated glomerular filtration rate; ACS acute coronary syndrome; UA unstable angina; CAD coronary artery disease; ACE angiotensin-converting enzyme; ARBs angiotensin-receptor blockers
Figure 1 shows the relationship between renal insufficiency and body composition. For patients with CAD, the percentage of patients with RRF was positively correlated with BF and inversely correlated with the LMI; no significant relationship was observed between the BMI and the percentage of patients with renal insufficiency.
Fig. 1.
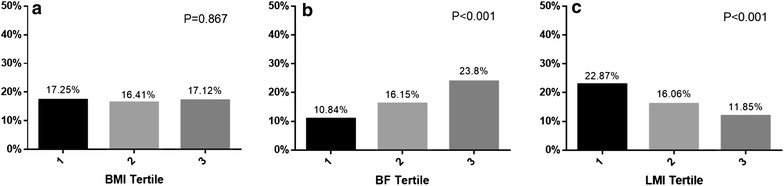
The proportion of patients with eGFR <60 min/ml across the BMI (a), BF (b) and LMI (c) tertiles. eGFR estimated glomerular filtration rate; BMI body mass index; BF body fat; LMI lean mass index
All the patients were followed up for an average of 29.1 ± 12.5 months, during which 271 patients died (mortality rate: 9.1 %), including 150 who died of cardiovascular events (cardiac mortality rate: 5.0 %). The survival curves showed that the risk of death was significantly higher in the RRF patients in all subgroups stratified using BMI, BF, or LMI (log rank test, all p < 0.001; Fig. 2).
Fig. 2.
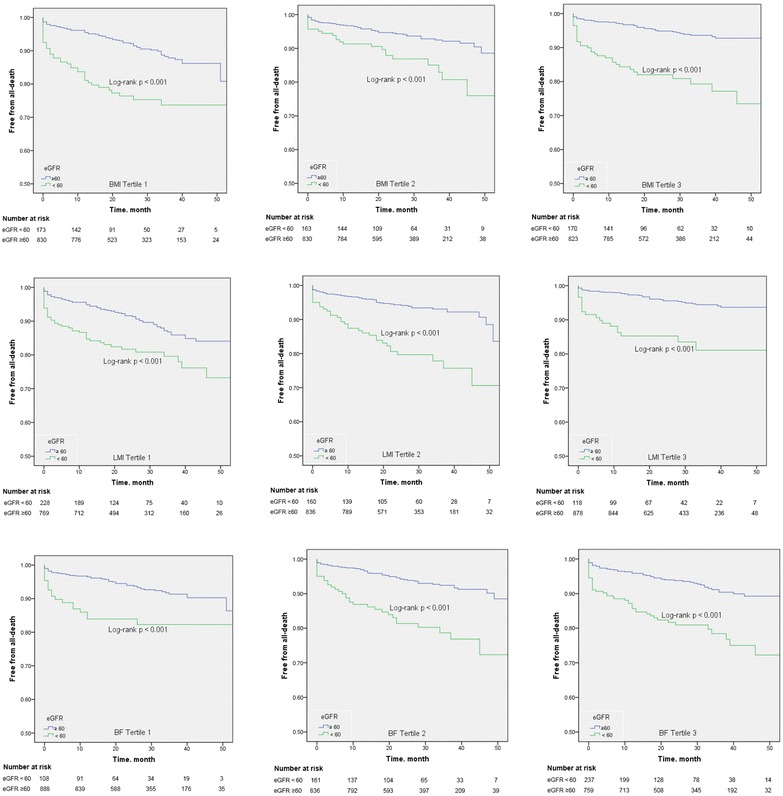
Kaplan-Meier plots according to the eGFR levels (min/ml) across the BMI, BF and LMI tertiles. eGFR estimated glomerular filtration rate; BMI body mass index; BF body fat; LMI lean mass index
The COX multivariate regression analysis showed that the risk of death was significantly higher in the RRF patients with high BF (BF tertile 3) (HR 1.95, CI 1.25–3.05) and low LMI (LMI tertile 1) (HR 1.82, CI 1.19–2.79), whereas the risk of RRF for death was not significant in patients with low BF (BF tertile 1) (HR 1.64 0.92–2.93) and high LMI (LMI tertile 3) (HR 1.71, CI 0.91–3.20) after multivariable correction (Table 2). In contrast, RRF was a risk factor for death in patients with a high BMI (BMI tertile 3) (HR 2.08, CI 1.22–3.55) or low BMI (BMI tertile 1) (HR 1.98, CI 1.28–3.08) but this risk was not significant in patients with a medium BMI (BMI tertile 2) (HR 1.12, 0.65–1.94). The subgroup analysis of patients with ACS showed similar results (Table 2). Analysis of cardiac death (Table 3) showed that RRF was a more significant risk factor for death in patients with high BF (HR 1.90, CI 1.00–3.62) and low LMI (HR 2.46, CI 1.39–4.37), which was consistent with the findings of the analysis of all-cause death; however, the risk of RRF for cardiac death was only significant in patients with a low BMI but not those with a high or medium BMI. For ACS patients, the risk of RRF for cardiac death was only in patients with low LMI and was unrelated to cardiac death in all of the BMI and BF subgroups. This result might be related to the low number of cardiac death cases, which could have resulted in insufficient statistical power in the ACS subgroup.
Table 2.
Hazard ratio for the incidence of all-cause mortality associated with renal function in the tertile subgroups of body composition
| Outcomes | All-cause mortality | All-cause mortality | All-cause mortality | ||||||
|---|---|---|---|---|---|---|---|---|---|
| BMI | BF | LMI | |||||||
| Tertile 1 | Tertile 2 | Tertile 3 | Tertile 1 | Tertile 2 | Tertile 3 | Tertile 1 | Tertile 2 | Tertile 3 | |
| No. of patients | n = 1003 | n = 993 | n = 993 | n = 996 | n = 997 | n = 996 | n = 997 | n = 996 | n = 996 |
| Total CAD patients (n = 2989), HR (95 % CI) | |||||||||
| No. of deaths | 116 | 78 | 77 | 80 | 89 | 102 | 124 | 87 | 60 |
| Unadjusted | 2.91 (1.99–4.26) | 2.30 (1.42–3.75) | 4.03 (2.57–6.34) | 2.75 (1.64–4.61) | 3.15 (2.05–4.86) | 2.97 (2.01–4.40) | 2.10 (1.46–3.03) | 3.32 (2.15–5.12) | 3.93 (2.28–6.78) |
| Adjusteda | 1.98 (1.28–3.08) | 1.12 (0.65–1.94) | 2.08 (1.22–3.55) | 1.64(0.92–2.93) | 1.57(0.95–2.60) | 1.95(1.25–3.05) | 1.82 (1.19–2.79) | 1.69 (1.01–2.82) | 1.71 (0.91–3.20) |
| ACS patients (n = 2163), HR (95 % CI) | |||||||||
| No. of deaths | 89 | 63 | 63 | 57 | 69 | 89 | 100 | 67 | 48 |
| Unadjusted | 3.11 (2.03–4.80) | 2.54 (1.50–4.29) | 4.24 (2.58–6.98) | 2.42 (1.30–4.49) | 3.64 (2.24–5.90) | 3.16 (2.08–4.79) | 2.35 (1.57–3.50) | 3.22 (1.96–5.29) | 4.37 (2.42–7.90) |
| Adjusteda | 1.67 (1.01–2.76) | 1.02 (0.56–1.87) | 1.97 (1.07–3.64) | 1.11 (0.55–2.26) | 1.39 (0.76–2.54) | 1.93 (1.20–3.11) | 1.74 (1.10–2.77) | 1.14 (0.62–2.12) | 1.84 (0.91–3.69) |
Renal function was estimated by levels of the creatinine clearance and binary classified by ≥60 and <60 min/ml
BMI body mass index; BF body fat; LMI lean mass index; HR hazard ratio; CI confidence interval; CAD coronary artery disease; ACS acute coronary syndrome; ACE angiotensin-converting enzyme; ARBs angiotensin-receptor blockers
aRisk factors adjustment included age, sex, medical history (pre-hypertension and pre-diabetes mellitus), heart function (Killip level), severity of CAD (left main artery and three vessel diseases), discharge medication (statin, ACE inhibitors or ARBs and beta-receptor blockers)
Table 3.
Hazard ratio for the incidence of cardiac mortality associated with renal function in the tertile subgroups of body composition
| Outcomes | Cardiac mortality | Cardiac mortality | Cardiac mortality | ||||||
|---|---|---|---|---|---|---|---|---|---|
| BMI | BF | LMI | |||||||
| Tertile 1 | Tertile 2 | Tertile 3 | Tertile 1 | Tertile 2 | Tertile 3 | Tertile 1 | Tertile 2 | Tertile 3 | |
| No. of patients | n = 1003 | n = 993 | n = 993 | n = 996 | n = 997 | n = 996 | n = 996 | n = 997 | n = 996 |
| Total CAD patients (n = 2989), HR (95 % CI) | |||||||||
| No. of cardiac deaths | 65 | 45 | 40 | 50 | 47 | 53 | 68 | 50 | 32 |
| Unadjusted | 3.21 (1.95–5.30) | 1.96 (1.01–3.79) | 3.19 (1.68–6.06) | 3.06 (1.63–5.77) | 2.12 (1.12–4.01) | 3.40 (1.98–5.83) | 2.69 (1.66–4.34) | 2.30 (1.25–4.21) | 2.81 (1.26–6.27) |
| Adjusteda | 2.26 (1.27–4.02) | 0.85 (0.39–1.84) | 0.90 (0.39–2.07) | 1.66 (0.81–3.40) | 0.72 (0.32–1.58) | 1.90 (1.00–3.62) | 2.46 (1.39–4.37) | 0.89 (0.42–1.87) | 0.77 (0.28–2.12) |
| ACS patients (n = 2163), HR (95 % CI) | |||||||||
| No. of cardiac deaths | 50 | 38 | 35 | 36 | 38 | 49 | 56 | 42 | 25 |
| Unadjusted | 3.39 (1.92–5.97) | 2.01 (1.00–4.05) | 3.87 (1.98–7.56) | 2.69 (1.26–5.73) | 2.55 (1.29–5.05) | 3.53 (2.01–6.18) | 2.74 (1.62–4.65) | 2.37 (1.23–4.57) | 3.62 (1.56–8.41) |
| Adjusteda | 1.85 (0.94–3.66) | 0.69 (0.29–1.61) | 1.00 (0.40–2.50) | 1.23 (0.51–2.97) | 0.56 (0.22–1.40) | 1.80 (0.92–3.52) | 1.99 (1.06–3.72) | 0.63 (0.27–1.48) | 0.99 (0.34–2.93) |
Renal function was estimated by levels of the creatinine clearance and binary classified by ≥60 and < 60 min/ml
BMI body mass index; BF body fat; LMI lean mass index; HR hazard ratio; CI confidence interval; CAD coronary artery disease; ACS acute coronary syndrome; ACE angiotensin-converting enzyme; ARBs angiotensin-receptor blockers
aRisk factors adjustment included age, sex, medical history (pre-hypertension and pre-diabetes mellitus), heart function (Killip level), severity of CAD (left main artery and three vessel diseases), discharge medication (statin, ACE inhibitors or ARBs and beta-receptor blockers)
Discussion
The study showed that renal insufficiency was positively correlated with BF, inversely correlated with LMI, and unrelated to BMI for patients with CAD. Moreover, the effect of renal insufficiency on the risk of death of CAD was related to body composition. The relationship between renal insufficiency and risk of mortality was more significant in CAD patients with higher BF and lower LMI, and with lower or higher BMI.
Some previous observational studies showed that obesity was a risk factor for chronic renal insufficiency [17–19], but other studies reached different conclusions [20–22]. Some researchers believed that the discrepancy arose because most of the previous studies used BMI as an indicator of obesity; however, BMI is not an accurate measure of obesity because it does not distinguish between body lean mass and body fat mass and body fat mass may play a major role in renal damage. Thus, recently researchers have proposed using BF and LMI to measure obesity [14, 23]. This study showed that renal insufficiency in patients with CAD was unrelated to BMI but was positively related to BF and inversely related to LMI, suggesting that BF and LMI were more effective measures than BMI when analysing the relationship between obesity and renal insufficiency. However, few studies have been conducted on this topic, and further exploration is warranted. The mechanism by which obesity causes renal damage is unknown. Possible mechanisms may be related to obesity-induced haemodynamic changes, a higher glomerular filtration burden, hormonal effects, and the activation of the renin-angiotensin-aldosterone-system (RAAS). Moreover, obese patients are prone to diabetes and hypertension, which indirectly cause renal damage [24, 25].
Renal insufficiency is an important risk factor for death and cardiovascular events in patients with CAD [6, 7, 26]. Furthermore, obese patients are susceptible to a range of cardiovascular risk factors, including hypertension, blood sugar disorders, dyslipidemia, and active inflammation [4]. Thus, cardiovascular risk factors may superimpose on one another in CAD patients complicated with obesity and renal insufficiency simultaneously. Obesity, especially the visceral adiposity would increase the risk of cardiovascular events and death in patients with renal insufficiency. The previous study found that visceral adiposity index is an optimal method to measure visceral adiposity to assess long-term CV outcomes and all-cause mortality in prevalent hemodialysis patients [27]. Epicardial adipose tissue accumulation in patients with CKD stage 3–5 increases the risk of CV events independent of general adiposity [28]. Visceral adiposity is associated with adverse cardiovascular outcomes for patients with CKD, while sarcopenia is common among patients with ESRD and is associated with higher mortality [29]. Considering the close relationship between obesity and renal insufficiency, accordingly, we have reason to speculate that renal function may perform different influence on the outcome of patients with different body compositions. Our study showed that renal insufficiency was a more significant risk factor for all-cause death and cardiac death in CAD patients with a higher body fat content (i.e., high BF and low LMI), suggesting that the fat mass may have a synergistic effect with renal insufficiency, thereby increasing the risk of death in CAD patients with renal insufficiency and obesity. How obesity causes cardiovascular disease is not entirely clear, but researchers believe that fat cells play an important role in this process as an endocrine organ [30]. Obese patients have a higher inflammation level and leptin resistance, which increase the risk of cardiovascular events [31, 32]. Moreover, obesity induces haemodynamic changes, increases the cardiac burden, induces cardiac remodelling, and affects cardiac functions [33].
Previous study found a U-shaped association of body mass index with inflammation and atherosclerosis in hemodialysis patients [34]. Interestingly, our study showed that renal insufficiency increased the risk of death of CAD in patients with a low BMI or high BMI but not in patients with a medium BMI (after multivariate correction), indirectly demonstrating that the BMI reflects the patient’s physical and nutritional status but not necessarily the body fat content. Patients with a high BMI are more likely to be obese, and thus, renal insufficiency may increase the risk of death in these patients, whereas patients with a low BMI are likely to have both a low fat body mass and low lean body mass (poor nutritional status); thus, renal insufficiency may more likely increase the risk of death in these patients. A previous cross-sectional study investigated the BMI and BF% (measured with air displacement plethysmography) in coronary artery disease (CAD) patients and showed that BMI failed to distinguish the fat mass from lean mass [35]. Our results indirectly support this opinion. For studies of the outcome of CAD, BF% and LMI may be more effective indicators than BMI for the risk of death.
This study has certain limitations. First, this study was a single-centre observational study. Despite multivariate correction, it was difficult to avoid all the confounding effect of (residual) selection bias absolutely. Moreover, in this single-centre study, all of the enrolled subjects were Chinese; thus, the potential for racial variation is unknown. Second, because the sample size of ACS subgroup was small relatively, the statistical power might have been inadequate in the analysis of cardiac death; thus, caution is needed when considering these results. In addition, the sample size of hemodialysis is small and we could hardly perform the analysis for this special subgroup. Considering the heterogeneity of patients with hemodialysis compared with patients without hemodialysis, we excluded the patients with hemodialysis in this study. Third, serum creatinine was collected only once after admission, and thus, measurement error could not be rule out definitely. Meanwhile, the serum creatinine levels might substantially change in some patients during hospitalization and the follow-up treatment after discharge. However, it is not always possible to repeat the serum creatinine test in an observational study, which is an inherent limitation of real world studies. Finally, this study was conducted in patients with CAD, and thus, it is unknown whether the results can be applied to renal insufficient patients without CAD.
Conclusions
For patients with CAD, renal insufficiency was positively correlated with BF, inversely correlated with LMI, and unrelated to BMI. The effect of renal insufficiency on the risk of death of CAD was related to body composition. Renal insufficiency was a more significant risk factor in CAD patients with higher BF and lower LMI, and with lower or higher BMI.
Authors’ contributions
YP and HW designed the study, collected the data, and drafted the article. FC and FYH analyzed the data and revised the article. TLX, YBL, HC, PJW, ZLZ, WL, CZ, YJL and YYG collected the data and revised the article. MC and DJH designed the study, drafted the article and revised it. All the co-authors finally contributed to the final approval of the version to be published. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Funding
This work was supported by the National High-tech Research and Development Program of China (2012AA02A510, Beijing, China), the Chinese National Nature Science Foundation (Grant numbers 81370219 and 81400267, Beijing, China) and the Supporting Project of Sichuan Provincial Department of Science and Technology (Grant numbers 2012FZ0065 and 2014SZ0004, Sichuan, China).
Abbreviations
- ACE
angiotensin-converting enzyme
- ACS
acute coronary syndrome
- ARBs
angiotensin-receptor blockers
- BF
body fat
- BMI
body mass index
- CAD
coronary artery disease
- CI
confidence interval
- eGFR
estimated glomerular filtration rate
- ESRD
end stage renal disease
- HR
hazard ratio
- LMI
lean mass index
- PRF
preserved renal function
- RRF
reduced renal function
- SCr
serum creatinine
- SD
standard deviation
- UA
unstable angina
Footnotes
Yong Peng and Hua Wang contributed equally to this work
Contributor Information
Yong Peng, Email: pengyongcd@126.com.
Hua Wang, Email: 13679024891@163.com.
Fei Chen, Email: 821662561@qq.com.
Fang-yang Huang, Email: stevenyd@qq.com.
Tian-li Xia, Email: xiatianli888@qq.com.
Yan-biao Liao, Email: 931862892@qq.com.
Hua Chai, Email: chhua014@263.net.
Peng-ju Wang, Email: 185920403@qq.com.
Zhi-liang Zuo, Email: 18284509496@qq.com.
Wei Liu, Email: liuw98@126.com.
Chen Zhang, Email: 511603520@qq.com.
Yi-jian Li, Email: 1033223512@qq.com.
Yi-yue Gui, Email: 549605621@qq.com.
Mao Chen, Email: hmaochen@vip.sina.com.
De-jia Huang, Email: huangdjmd@163.com.
References
- 1.Global health observatory (GHO): Obesity 2008. Geneva: World Health Organization 2014. http://www.who.int/gho/ncd/risk_factors/obesity_text/en/index.html. Accessed 2 June 2016.
- 2.Hou X, Lu J, Weng J, Ji L, Shan Z, Liu J, Tian H, Ji Q, Zhu D, Ge J, Lin L, Chen L, Guo X, Zhao Z, Li Q, Zhou Z, Shan G, Yang Z, Yang W, Jia W, China National Diabetes and Metabolic Disorders Study Group Impact of waist circumference and body mass index on risk of cardiometabolic disorder and cardiovascular disease in Chinese adults: a national diabetes and metabolic disorders survey. PLoS One. 2013;8:e57319. doi: 10.1371/journal.pone.0057319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Poirier P, Giles TD, Bray GA, Hong Y, Stern JS, Pi-Sunyer FX, Eckel RH, American Heart Association. Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2006;113:898–918. doi: 10.1161/CIRCULATIONAHA.106.171016. [DOI] [PubMed] [Google Scholar]
- 4.Emerging Risk Factors Collaboration. Wormser D, Kaptoge S, Di Angelantonio E, Wood AM, Pennells L, Thompson A, Sarwar N, Kizer JR, Lawlor DA, Nordestgaard BG, Ridker P, Salomaa V, Stevens J, Woodward M, Sattar N, Collins R, Thompson SG, Whitlock G, Danesh J. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. Lancet. 2011;377:1085–1095. doi: 10.1016/S0140-6736(11)60105-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cignarelli M, Lamacchia O. Obesity and kidney disease. Nutr Metab Cardiovasc Dis. 2007;17:757–762. doi: 10.1016/j.numecd.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 6.Sarnak MJ, Levey AS, Schoolwerth AC, Coresh J, Culleton B, Hamm LL, McCullough PA, Kasiske BL, Kelepouris E, Klag MJ, Parfrey P, Pfeffer M, Raij L, Spinosa DJ, Wilson PW, American Heart Association Councils on Kidney in Cardiovascular Disease HBPRCC, Epidemiology, Prevention Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation. 2003;108:2154–2169. doi: 10.1161/01.CIR.0000095676.90936.80. [DOI] [PubMed] [Google Scholar]
- 7.Schiffrin EL, Lipman ML, Mann JF. Chronic kidney disease: effects on the cardiovascular system. Circulation. 2007;116:85–97. doi: 10.1161/CIRCULATIONAHA.106.678342. [DOI] [PubMed] [Google Scholar]
- 8.Gruberg L, Weissman NJ, Waksman R, Fuchs S, Deible R, Pinnow EE, Ahmed LM, Kent KM, Pichard AD, Suddath WO, Satler LF, Lindsay J., Jr The impact of obesity on the short-term and long-term outcomes after percutaneous coronary intervention: the obesity paradox? J Am Coll Cardiol. 2002;39:578–584. doi: 10.1016/S0735-1097(01)01802-2. [DOI] [PubMed] [Google Scholar]
- 9.Dagenais GR, Yi Q, Mann JF, Bosch J, Pogue J, Yusuf S. Prognostic impact of body weight and abdominal obesity in women and men with cardiovascular disease. Am Heart J. 2005;149:54–60. doi: 10.1016/j.ahj.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 10.Kovesdy CP, Anderson JE, Kalantar-Zadeh K. Paradoxical association between body mass index and mortality in men with CKD not yet on dialysis. Am J Kidney Dis. 2007;49:581–591. doi: 10.1053/j.ajkd.2007.02.277. [DOI] [PubMed] [Google Scholar]
- 11.Kalantar-Zadeh K, Abbott KC, Salahudeen AK, Kilpatrick RD, Horwich TB. Survival advantages of obesity in dialysis patients. Am J Clin Nutr. 2005;81:543–554. doi: 10.1093/ajcn/81.3.543. [DOI] [PubMed] [Google Scholar]
- 12.Gomez-Ambrosi J, Silva C, Galofre JC, Escalada J, Santos S, Millan D, Vila N, Ibanez P, Gil MJ, Valenti V, Rotellar F, Ramirez B, Salvador J, Fruhbeck G. Body mass index classification misses subjects with increased cardiometabolic risk factors related to elevated adiposity. Int J Obes. 2012;36:286–294. doi: 10.1038/ijo.2011.100. [DOI] [PubMed] [Google Scholar]
- 13.Gomez-Ambrosi J, Silva C, Catalan V, Rodriguez A, Galofre JC, Escalada J, Valenti V, Rotellar F, Romero S, Ramirez B, Salvador J, Fruhbeck G. Clinical usefulness of a new equation for estimating body fat. Diabetes Care. 2012;35:383–388. doi: 10.2337/dc11-1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lavie CJ, De Schutter A, Patel DA, Romero-Corral A, Artham SM, Milani RV. Body composition and survival in stable coronary heart disease: impact of lean mass index and body fat in the “obesity paradox”. J Am Coll Cardiol. 2012;60:1374–1380. doi: 10.1016/j.jacc.2012.05.037. [DOI] [PubMed] [Google Scholar]
- 15.Levey AS, Coresh J, Greene T, Stevens LA, Zhang YL, Hendriksen S, Kusek JW, Van Lente F, Chronic Kidney Disease Epidemiology Collaboration Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006;145:247–254. doi: 10.7326/0003-4819-145-4-200608150-00004. [DOI] [PubMed] [Google Scholar]
- 16.KDIGO Board K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39:S1–S266. [PubMed] [Google Scholar]
- 17.Burton JO, Gray LJ, Webb DR, Davies MJ, Khunti K, Crasto W, Carr SJ, Brunskill NJ. Association of anthropometric obesity measures with chronic kidney disease risk in a non-diabetic patient population. Nephrol Dial Transplant. 2012;27:1860–1866. doi: 10.1093/ndt/gfr574. [DOI] [PubMed] [Google Scholar]
- 18.Hsu CY, McCulloch CE, Iribarren C, Darbinian J, Go AS. Body mass index and risk for end-stage renal disease. Ann Intern Med. 2006;144:21–28. doi: 10.7326/0003-4819-144-1-200601030-00006. [DOI] [PubMed] [Google Scholar]
- 19.Wang Y, Chen X, Song Y, Caballero B, Cheskin LJ. Association between obesity and kidney disease: a systematic review and meta-analysis. Kidney Int. 2008;73:19–33. doi: 10.1038/sj.ki.5002586. [DOI] [PubMed] [Google Scholar]
- 20.Hobbs H, Farmer C, Irving J, Klebe B, Stevens P. Is high body mass index independently associated with diminished glomerular filtration rate? An epidemiological study. J Ren Care. 2011;37:148–154. doi: 10.1111/j.1755-6686.2011.00231.x. [DOI] [PubMed] [Google Scholar]
- 21.Mohsen A, Brown R, Hoefield R, Kalra PA, O’Donoghue D, Middleton R, New D. Body mass index has no effect on rate of progression of chronic kidney disease in subjects with type 2 diabetes mellitus. J Nephrol. 2012;25:384–393. doi: 10.5301/jn.5000062. [DOI] [PubMed] [Google Scholar]
- 22.Brown RN, Mohsen A, Green D, Hoefield RA, Summers LK, Middleton RJ, O’Donoghue DJ, Kalra PA, New DI. Body mass index has no effect on rate of progression of chronic kidney disease in non-diabetic subjects. Nephrol Dial Transplant. 2012;27:2776–2780. doi: 10.1093/ndt/gfr757. [DOI] [PubMed] [Google Scholar]
- 23.Lavie CJ, De Schutter A, Patel D, Artham SM, Milani RV. Body composition and coronary heart disease mortality–an obesity or a lean paradox? Mayo Clin Proc. 2011;86:857–864. doi: 10.4065/mcp.2011.0092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Henegar JR, Bigler SA, Henegar LK, Tyagi SC, Hall JE. Functional and structural changes in the kidney in the early stages of obesity. J Am Soc Nephrol. 2001;12:1211–1217. doi: 10.1681/ASN.V1261211. [DOI] [PubMed] [Google Scholar]
- 25.Wahba IM, Mak RH. Obesity and obesity-initiated metabolic syndrome: mechanistic links to chronic kidney disease. Clin J Am Soc Nephrol. 2007;2:550–562. doi: 10.2215/CJN.04071206. [DOI] [PubMed] [Google Scholar]
- 26.Garimella PS, Katz R, Patel KV, Kritchevsky SB, Parikh CR, Ix JH, Fried LF, Newman AB, Shlipak MG, Harris TB, Sarnak MJ, Health ABCS. Association of serum erythropoietin with cardiovascular events, kidney function decline, and mortality: the health aging and body composition study. Circ Heart Fail. 2016;9:e002124. doi: 10.1161/CIRCHEARTFAILURE.115.002124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen HY, Chiu YL, Chuang YF, Hsu SP, Pai MF, Yang JY, Peng YS. Visceral adiposity index and risks of cardiovascular events and mortality in prevalent hemodialysis patients. Cardiovasc Diabetol. 2014;13:136. doi: 10.1186/s12933-014-0136-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cordeiro AC, Amparo FC, Oliveira MA, Amodeo C, Smanio P, Pinto IM, Lindholm B, Stenvinkel P, Carrero JJ. Epicardial fat accumulation, cardiometabolic profile and cardiovascular events in patients with stages 3–5 chronic kidney disease. J Intern Med. 2015;278:77–87. doi: 10.1111/joim.12344. [DOI] [PubMed] [Google Scholar]
- 29.Johansen KL, Lee C. Body composition in chronic kidney disease. Curr Opin Nephrol Hypertens. 2015;24:268–275. doi: 10.1097/MNH.0000000000000120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lavie CJ, Milani RV, Ventura HO. Untangling the heavy cardiovascular burden of obesity. Nat Clin Pract Cardiovasc Med. 2008;5:428–429. doi: 10.1038/ncpcardio1257. [DOI] [PubMed] [Google Scholar]
- 31.Enriori PJ, Evans AE, Sinnayah P, Cowley MA. Leptin resistance and obesity. Obesity. 2006;14(Suppl 5):254S–258S. doi: 10.1038/oby.2006.319. [DOI] [PubMed] [Google Scholar]
- 32.Gomez-Marcos MA, Recio-Rodriguez JI, Gomez-Sanchez L, Agudo-Conde C, Rodriguez-Sanchez E, Maderuelo-Fernandez J, Gomez-Sanchez M, Garcia-Ortiz L, LOD-DIABETES Group Gender differences in the progression of target organ damage in patients with increased insulin resistance: the LOD-DIABETES study. Cardiovasc Diabetol. 2015;14:132. doi: 10.1186/s12933-015-0293-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lavie CJ, Milani RV, Ventura HO, Cardenas GA, Mehra MR, Messerli FH. Disparate effects of left ventricular geometry and obesity on mortality in patients with preserved left ventricular ejection fraction. Am J Cardiol. 2007;100:1460–1464. doi: 10.1016/j.amjcard.2007.06.040. [DOI] [PubMed] [Google Scholar]
- 34.Kahraman S, Yilmaz R, Akinci D, Arici M, Altun B, Erdem Y, Yasavul U, Turgan C. U-shaped association of body mass index with inflammation and atherosclerosis in hemodialysis patients. J Ren Nutr. 2005;15:377–386. doi: 10.1053/j.jrn.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 35.Romero-Corral A, Somers VK, Sierra-Johnson J, Jensen MD, Thomas RJ, Squires RW, Allison TG, Korinek J, Lopez-Jimenez F. Diagnostic performance of body mass index to detect obesity in patients with coronary artery disease. Eur Heart J. 2007;28:2087–2093. doi: 10.1093/eurheartj/ehm243. [DOI] [PubMed] [Google Scholar]


