Abstract
Background
Limited English proficient (LEP) patients receive fewer recommended preventive screenings than English-speaking patients. Studies have explored patients’ perceptions of the factors that contribute to this disparity, but little research has focused on physicians’ perceptions.
Objective
To describe physicians’ perceptions of the barriers and facilitators to preventive cancer screening in LEP patients.
Design
Qualitative interview study using a semi-structured interview guide.
Participants
Eight primary care physicians from Wisconsin.
Approach
Each interview was systematically coded to illuminate important themes.
Key Results
A variety of barriers specifically hinder LEP patients’ receipt of cancer screening, including poor language proficiency, lack of transportation, unfamiliarity with the concept of prevention, complex scheduling systems, poor interpretation, and limited physician time to discuss preventive care. While physicians identified many factors that facilitate preventive screening in general, they mentioned few that are perceived as specific to LEP patients.
Conclusion
We found that primary care physicians attribute the low rates of preventive cancer screening among LEP populations to a variety of patient, provider, interpreter, and system factors, most of which go beyond simple language barriers. Interventions designed to reduce these barriers and enhance the impact of identified facilitators should be multifactorial and designed to engage primary care physicians.
Keywords: Limited English proficiency, cancer screening, disparities, qualitative research
1. INTRODUCTION
Language barriers in the health care setting are prevalent in the United States. In 2007, an estimated 55 million people spoke a language other than English at home (United States Census Bureau). According to the 2010 U.S. Census, 9% of the population over the age of five was limited English proficient (LEP), meaning that they spoke English not well or not at all (Pandya 2011). LEP populations are growing across the United States, including in the state in which this study was conducted, Wisconsin; specifically, between 1990 and 2000 the number of LEP citizens grew by 60% in Wisconsin (Youdelman 2004).
It is well documented that LEP patients are marginalized in the U.S. health care system; importantly, LEP patients receive recommended preventive care less often than patients of a similar ethnicity who speak English (Harlan, Bernstein, & Kessler 1991; Jacobs et al. 2005; De Alba & Sweningson 2006; Cheng, Chen, & Cunningham 2007; Liang et al. 2009; Lim 2010). Decreased rates of screening among LEP populations are not entirely explained by factors such as sociodemographics or contact with a physician, suggesting that language may play a significant role in explaining the discrepancy (Jacobs et al. 2005). Qualitative studies on the barriers to preventive cancer screening in LEP populations support the crucial role of language in this disparity (Natale-Pereira et al. 2008; Fang & Baker 2013). These studies also suggest that there are other significant factors that affect LEP populations’ preventive care-seeking behavior, including low knowledge and awareness of cancer, lack of insurance, undocumented legal status, seeking care only when sick, low prioritization of health care, stigmatization, fear, embarrassment, lack of time, and use of traditional medicine and rituals (Natale-Pereira et al. 2008; Fang & Baker 2013; Lor et al. 2013).
Access to preventive cancer screenings is highly variable around the world. For example, countries such as China, Columbia, and the United Kingdom report that they provide access to preventive cancer screening at the primary health care level while other countries such as Egypt and India provide access to some screenings, and countries such as Afghanistan and Ghana don’t generally provide access to preventive cancer screening at the primary health care level (World Health Organization). Furthermore, there have been growing numbers of patients with language barriers in countries around the world (Diez Guardia & Pichelmann 2006; Somerville 2009; Australian Government). Therefore, a better understanding of how to effectively provide preventive cancer screenings to patients with language barriers is increasing in importance worldwide.
While many studies have described the barriers to preventive cancer screening from the patient perspective, few have characterized the provider perspective (Gadon et al. 2007). It is important to understand the provider perspective, in addition to the patient perspective, because previous works have documented that provider recommendation is one of the biggest predictors of patients’ participation in cancer screening and that it is important to consider providers’ perspectives when considering ways to enhance cross cultural communication (Cioffi 2003; Roberts et al. 2007). Our study fills this gap in the literature by seeking to better understand the factors that contribute to the disparities in LEP patients’ receipt of preventive cancer screening through the lens of the primary care provider.
2. METHODS
Sample
We conducted eight in-depth, semi-structured interviews with primary care physicians in a large health system in Wisconsin as part of a larger qualitative study to understand preventive cancer screening rates in LEP patients. The current study, which reports primary care providers’ understanding of cancer screening disparities, is part of a larger study in which Spanish- and Hmong-speaking patients were interviewed regarding their experiences with preventive screening. We chose to study Spanish and Hmong-speaking patients because these are two of the most common languages spoken in Wisconsin (CTC & Associates LLC 2010). The results of the physician interviews are presented in the current manuscript, while the results of the patient interviews will be presented in future work.
We recruited primary care physicians involved in caring for LEP patients at a variety of clinic locations. The participants were either general internists or family medicine practitioners who contacted the Principle Investigator (PI) in response to presentations she gave on the study or in response to an email solicitation. All physicians that responded were invited to participate in the study and interviews were scheduled at the convenience of the physician. All participants received $50 in appreciation of his/her time. This study was deemed exempt from review by the human subjects institutional review board of the University of Wisconsin because we did not collect any personal identifying information or protected health information.
The final sample size was determined by when the investigative team determined that we had reached theme saturation, using the constant comparison method; the Principle Investigator and research team proceeded with sampling, data collection, and preliminary data analysis concurrently and stopped data collection when the physician responses became redundant and attempts to uncover new themes failed to reveal novel data (Bowen 2008).
Procedure
The PI, a female General Internist, conducted interviews in a private room in the physician’s clinic or in a research office building and at least one observer from the research team was present at each interview. The interview guide consisted of eleven open-ended questions designed to promote discussion, and follow-up, probing questions were used to clarify answers or elicit a more thorough response (Appendix). Major topics for discussion included: (1) Physicians’ experiences providing preventive cancer screening and behavioral health screening, in general; (2) Physicians’ perspectives of barriers/facilitators of screening, in general; (3) Physicians’ experiences providing preventive cancer screening and behavioral health screening to LEP populations; (4) Physicians’ perspectives of barriers/facilitators of screening in LEP populations; (5) Physician-patient language concordance; (6) Interpreter services and access; and (7) Physicians’ recommendations for system improvement. Physicians were encouraged to consider mammograms, colonoscopies, fecal occult blood test (FOBT), prostate screenings, and behavioral health screenings for alcohol and tobacco use when responding to interview questions.
Each interview lasted 20–35 minutes, after which we asked each participant to complete a demographic survey. We audio recorded the interviews and observers took notes in real-time. We transcribed the recordings verbatim and reviewed them for accuracy.
Coding and analysis
In this study, conventional content analysis was used to analyze the data. (Graneheim et al; 2004; Hsieh et all 2005; Caelli et al. 2008). Conventional content analysis avoids the use of preconceived categories in order to allow themes to emerge from the data (Hsieh et al. 2005). Transcriptions were imported into NVivo software and an initial codebook was created based on the interview guide. Three investigators independently coded two transcripts and met to discuss the addition of new codes. Collaboratively, the investigators developed a revised, working codebook, to which no new codes were added during the coding process but to which code definitions were modified based on the group’s collective use of the codes. This final codebook was used to code all transcripts. The three investigators met regularly and resolved disagreements and discrepancies in coding through consensus. When all interviews were coded, we identified themes and subthemes in interviews and presented the analysis to study team members for discussion.
3. RESULTS
Demographic characteristics
Four female and four male physicians between the ages of 36 and 55 participated in this study; each holds a faculty position in a university health system. The physicians saw patients for an average of 5.75 clinic half days per week in one of six different clinics. All but one participant listed English as their first language, but four listed that they can speak another language well or very well, including two who spoke Spanish. The proportion of the physicians’ patients that were LEP, as reported by the interviewees, varied from <1% to 25%. Three physicians lived outside of the United States while growing up and six had previously received cross-cultural training.
Overview of barriers and facilitators
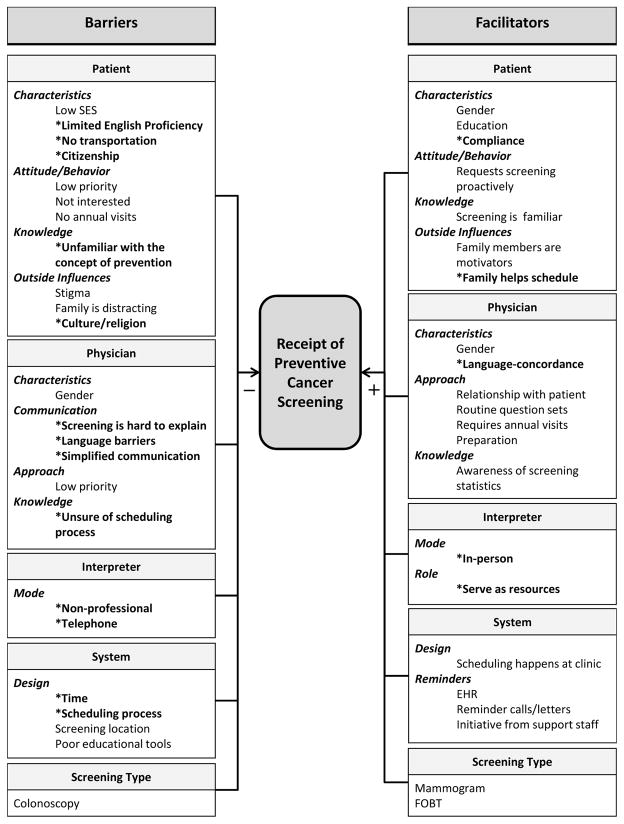
Providers described many barriers and facilitators to the receipt of preventive cancer screening among English proficient and LEP patients. We informed providers that they were being interviewed as part of a larger study that included interviews with Spanish- and Hmong-speaking patients; as a result, they occasionally made comments specific to Hmong- or Spanish-speaking populations. Figure 1 displays the factors identified by primary care physicians in the current study, organizes them into patient-, provider-, interpreter-, and system-level barriers and facilitators, and highlights how different types of screening were viewed by the physicians. Due to space limitations, Figure 1 is a more complete list of barriers and facilitators identified by physician interviewees than we can elaborate on in the text that follows; we represent in writing the most important themes across physician interviews.
Figure 1. Barriers and facilitators to preventive cancer screening.
Starred, bolded items represent factors that physicians discussed specifically in regard to LEP patients. Normal text represents factors that physicians discussed as factors for all patients, regardless of their LEP status.
Patient barriers
Characteristics
Physicians identified a number of barriers to screening that related to the patient. According to our participants, patients with low socioeconomic status (SES) have trouble obtaining screening due to the out-of-pocket cost of the tests. One physician noted:
I put [LEP patients] in a category with my patients that are either under insured or don’t [have insurance] …there’s a growing population where they’re very reluctant to get colonoscopies because of the cost. Cost is becoming a big concern…we can’t even tell people how much it costs…if they are going to pay out of pocket.
In addition, patients without transportation had difficulty getting screened. One physician stated:
A lot of my [LEP] patients are also indigent. So that’s hard. So, uhh, transport, we have a hard time arranging that.
Attitudes and behaviors
Providers described how many patients place prevention low on their list of priorities. This could be due to competing priorities in life, such as employment and caregiving, or due to more imminent health care concerns, such as chronic disease management. Physicians themselves also viewed prevention as a lower priority than other concerns. Prioritization is expressed in the following quotation.
I mean their struggle is with day to day life and where they’re gonna stay that night and where their food is gonna come from. So for them to realize you have a one in eight chance of developing breast cancer during your lifetime and we should screen for it cause you’re at high risk, uhh that’s not on their radar screen I don’t think...so that’s just the prioritizing of their life concerns.
Physicians reported that other patients are simply not interested in screening, regardless of their continued encouragement of their patients to get screened.
Some people…tend to fall into the category of like “no I don’t want it I don’t think I need it, I don’t, you know, I poop every day my colon is fine” … and like no matter what you tell them, and however you try…to explain it you know nothing is going to change their mind.
Physicians reflected on how Hmong-speaking patients, particularly, are more likely to say no to screenings, especially colonoscopies. One physician explained:
I must say the Hmong patients I always still feel like are on another planet when talking about stuff like that. It’s just I feel like it’s a much more difficult conversation to have um to get them to the point where they kind of get why we’re wanting to do screening tests.
Knowledge
Our participants cited that a lack of familiarity with prevention precludes some LEP patients from accepting screening. They felt that despite their attempts to explain it thoroughly, some of the concept of prevention is lost due to language or cultural barriers.
In particular colonoscopy always comes to mind because to try to um get across the importance that you know…it’s easier to remove…this tiny polyp that’s precancerous rather than wait for it to become invasive? Ah there is some of that- I’m assuming is being lost in translation.
Outside influences
Physicians spoke of various factors external to the patient that affected their decision to obtain preventive screening, the most important of which was culture. Physicians felt that cultural barriers can be discouraging and hard to overcome. This feeling was more pronounced when physicians spoke about Hmong-speaking patients in contrast to Spanish-speaking patients. Physicians’ discomfort with cultural issues is showcased below.
I have this most in my mind about my Hmong patients…in general, their beliefs about health or their beliefs about health being tied to spiritual issues and therefore like, I’m not sick why are you doing something to me right now, or I don’t feel like I have a great way of addressing their spiritual issues…so therefore I feel like boy I don’t think I’ve done a very good job of dealing with- though I do the best I can, I still am dealing with them with a very Western point of view.
Physician barriers
Communication
Our participants felt that language barriers impeded their ability to recommend screening to LEP patients. They felt that they were often unable to provide sufficient information and explanation for the patients to participate in shared decision-making.
I get concerned that I haven’t been able to communicate, you know, the certain risks and benefits that the patient might be just too agreeable to certain things, so informed consent might be a little bit more of an issue [with LEP patients].
Also, our participants noted that screenings, especially colonoscopies, were often harder to explain to LEP patients.
The invasive ones are kind of umm very hard to explain because we can’t demonstrate; we just tell them verbally like preps and stuff like that.
Knowledge
Many physicians expressed uncertainty about what happens to patients when they leave the exam room and need to schedule a preventive screening appointment. Physicians acknowledged that the process for obtaining a screening procedure frequently includes many steps; they viewed this as a barrier specific to LEP patients, who may or may not be able to communicate through each step of the process. Physicians’ discomfort with their apparent gap in knowledge is expressed in the following quotation.
Or when I schedule [the colonoscopy], I just say “do it”. And then I don’t know how they’re going to do it. I don’t know who’s going to call them and how they call.
Interpreter barriers
Mode
According to our participants, interpreters themselves can also be a barrier. Physicians felt that in-person interpreters were of a variable quality. Mainly though, they spoke of technical difficulties with telephone interpreters and the difficulties that arise when using a non-professional interpreter. When non-professional family members interpreted, physicians feared inaccurate communication.
If you’ve got an older patient and the family member, the son or the daughter, are kind of half interpreting for the patient…it can definitely be an issue. It makes your time go faster, but…you definitely see the, the filtering of information and the response back is usually highly filtered and highly, uhh maybe biased.
System barriers
Time
Physicians noted that using interpreters for patients with language barriers slows down clinic visits, which creates time constraints, forces physicians to break up topics across visits, and obliges them to push prevention to a later date. One physician explains:
I also think that there’s probably a little bit more of a delay sometimes in me getting to the screening topic. Like if there is someone who has a language barrier, for instance, sometimes I’ll break the topics up over a period of visits because it just is too much to fit into a normal visit length if you’re also working with an interpreter.
Patient facilitators
Outside influence
Physicians believed that family members motivate patients to get necessary screenings. A few physicians spoke specifically of female family members encouraging male members get screened. Referencing his English-speaking patients, one physician said:
I think [the] female attitude about preventive healthcare … is more accepted. Like they’re the ones that make their husbands and boyfriends and brothers come to the doctor because hey you need these colonoscopies, you need this, you need that.
While physicians spoke about a positive familial influence for all patients, they also mentioned how it specifically affected those with LEP, saying that family member interpreters could play the role of motivators and encourage their LEP family member to get screened.
You know, sometimes its motivating [using family members as interpreters]…sometimes that can be, because as opposed to them just telling, you just being an interpreter, they will haha be an enforcer.
Physician facilitators
Approach
Physicians spoke about how their own approach to providing preventive screening encourages patients to get screened. The most important facilitator was physicians having a routine or a previously prepared plan.
I run through my schedule, I probably take twenty minutes or more to go through my schedule and get up to speed on just what the patient needs I think are going to be but then also to go through health maintenance stuff with every patient that I have coming in.
Interpreter facilitators
Role
Providers mentioned interpreter facilitators in two instances: when interpreters are in-person and when they fill a dual role as a care coordinator or scheduler for the patient they are working with. This idea is summarized in the quotation below, in which the physician was responding to a question regarding interpreters doubling as care coordinators.
I mean it is a big help… like say I see a patient who is completely English proficient…but say I order a mammogram, a colonoscopy, some fasting labs, an X-ray and an electrocardiogram…I say now you need to go to the scheduling desk and you need to do these five things in this order…it is just a lot to keep track of …so then if you add language barrier on top of that…there’s no way they can probably navigate that situation at the desk…So usually I make sure the interpreter really clearly knows that I am expecting that they’re going to help them do that part. So I’m putting them in that role.
System facilitators
Reminders
Physicians spoke of system reminders as facilitators for patients in general. For example, physicians said that they are reminded via the electronic health record or via their support staff when a patient is due for a certain screen. Initiative from support staff is explained in this quotation:
Our [medical assistants] and everyone is pretty clued into [delivering cancer screening], so now as we’ve been able to shift some of the work, I have a very good [medical assistant] and she’ll come and take the lead putting somebody’s in there so making it even easier for me.
Screening type
When looking across screening types, physicians spoke more often of barriers to colorectal cancer screening. They mentioned that colonoscopies are hard to explain to LEP patients and that, in general, their LEP patients did not want to get them. To facilitate colorectal cancer screening, physicians used FOBT, which is less invasive, more cost effective, and more appealing for patients.
You’re more likely to do the fecal occult blood test [than] a colonoscopy and whether that’s because of the cost or because it’s less invasive or because it’s deflecting in terms of well you know…it’s more independent- you go to the lab, you pick up the kit…they are more agreeable to be like “I’ll pick up the kit”.
In addition to FOBT, mammograms were spoken about in a positive light. Some providers mentioned that scheduling for mammograms was easier and involved better accountability, while others mentioned that patients were just more willing to accept mammograms.
I think that the breast center and the schedulized mammogram screening happens with some better accountability. It seems like, I very seldom order a mammogram and then it doesn’t get scheduled.
Physician suggestions for improvement
Patient-level
Physicians were asked to provide ideas on how to improve the delivery of preventive cancer screenings to LEP populations in their area. To address the patient barriers, physicians suggested increasing patient education through a trusted community member.
In my mind again it really comes back to the fact of education…you know…contacting a community center where there [are] Hmong people or Spanish people and…trying to educate people about what those crazy western medicine doctors are trying to do and why umm, and having perhaps someone in their community who’s-- who can be a potential advocate or liaison between would I think, really help get the word across.
Physician-level
To address the identified physician barriers, physicians entertained the idea of increased cultural competency training. Some physicians questioned the effectiveness of these types of trainings or found them discouraging in the past, but in general, they supported the idea of evidence-based trainings.
You know, just like anything else there is always the need for ongoing cultural competence training…If there is a strong barrier that we are seeing in uhh the Hmong community, then it’s got to be addressed.
System-level
Providers suggested increasing appointment length with LEP patients, having more in-person interpreters available, making sure the system alerts physicians when screenings are not completed, and having educational material in multiple languages as ways to improve the system. Because physicians found some screenings hard to explain to LEP patients, they were enthusiastic about pictures or other forms of explanation that could be given to patients in the proper language.
You know having language appropriate information about all the screening seems logical, that is describing it in ah the particular language that’s very readily available…like easily accessed by the clinician or their staff in real time.
1. DISCUSSION
The physicians we interviewed indicated that there are many barriers beyond language that influence an LEP patient’s likelihood of obtaining preventive cancer screening. Additional barriers included socioeconomic status, transportation, prioritization of healthcare and other life concerns, having less familiarity with preventive care, culture, complex scheduling systems that are poorly understood by physicians, poor interpretation by ad hoc and phone interpreters, and limited physician time to discuss preventive care. Physicians identified many factors that facilitate preventive screening in general, but fewer that are specific to LEP patients. Two possible explanations for this finding are that physicians are not sensitized to the specific needs of LEP patients or that most facilitators are common across patients and few are unique to LEP populations in our setting.
We were struck by the fact that language barriers were only one of many barriers that physicians mentioned and that they were often not discussed as a significant barrier. This may be because we conducted our interviews in a health system with ample access to high quality interpreters and so this barrier was most often effectively overcome. We also found heterogeneity in some of what physicians shared with us regarding the two LEP groups that we focused on in this study—Spanish-speaking and Hmong populations. For example, physicians expressed greater unfamiliarity with the Hmong culture that that of their Spanish-speaking patients and discussed their struggles with how to cross this perceived greater cultural divide. Clearly, there need to be different approaches for different LEP groups to facilitate screening.
It is also important to note that while we distinguish between patient, provider, interpreter, and system factors, all categories are constantly interacting and barriers/facilitators often represent the intersection of more than one category. Because the listed factors do not act in isolation, an effective intervention to increase screening rates in LEP populations would need to be multifactorial.
Previous literature supports many of our findings. For instance, previous work suggests that time constraints in primary care encounters are a major barrier to the provision of recommended preventive services; this constraint disproportionately affects LEP patients, whose encounters often take extra time (Yarnall et al. 2003; Ginsburg 2007). The literature also suggests that culture is an important influence to patients’ beliefs about cancer screening. In a study of Hmong women’s beliefs about breast and cervical cancer screenings, Lor et al. found that Hmong women encountered cultural barriers such as embarrassment undressing for an exam and listening to authority figures (2013). In addition, cancer itself is an unfamiliar concept to Hmong people, making it more difficult for physicians to explain the rationale behind each screening (Lor & Bowers 2014). This study adds to the current literature because we provide information about physicians’ perspectives regarding barriers and facilitators to screening and demonstrate how the factors they identified are very similar to those previously identified by LEP patients (Akers et al. 2007; Watts et al. 2009; Fang & Baker 2013; Lor et al. 2013). Additionally, we propose a multifactorial model that includes patient, physician, interpreter and system level facilitators or barriers as a way of organizing and conceptualizing these barriers (Figure 1).
Our study suggests that there are a number of areas for focusing interventions to improve screening rates. For example, transportation barriers may be mitigated by developing programs to transport hard-to-reach patients to screening sites or by employing mobile screening techniques like FOBT and HPV self-collection sampling kits and mobile mammography buses (Ogilvie et al. 2007; Natale-Pereira et al. 2008; Maar et al. 2013). Using FOBT techniques may also address other barriers to colorectal cancer screening we identified, including the fact that colonoscopies are more invasive, taboo, and harder to explain than other preventive measures. For these reasons, substituting FOBT screening for colonoscopies when appropriate may increase screening rates in LEP populations.
Our physician participants also identified a need to raise awareness and familiarity of cancer prevention among LEP populations through a trusted community member. Culturally-appropriate interventions conducted by lay community workers have been shown to increase mammography and Pap test screening rates among Latinas (Navarro et al. 1998; Fernandez et al. 2009). This concept holds for the Hmong community as well; the Hmong Health Awareness Project suggested that the use of visual aids, videos, and hand-on activities developed by Hmong community members with the specific origins and traditions of the Hmong culture in mind enhanced knowledge of breast and cervical cancer screening among Hmong women (Lor & Bowers 2014).
Finally, it was clear that physicians need a better understanding of the barriers LEP patients face in navigating the scheduling system so that they may better help them overcome these barriers. Physicians’ confidence in communicating across cultures also needs to be enhanced; this could be done through targeted educational programs and by providing them with access to educational materials and illustrative diagrams about screenings in multiple languages. Studies support the efficacy of linguistically- and culturally-appropriate educational materials for increasing cancer screening knowledge and rates (Tu et al. 2008; Lor & Bowers 2014). Alternatively, some responsibility could be taken off the providers’ shoulders by employing language-concordant prevention care managers to help LEP patients navigate the scheduling system; Beach et al. suggest that prevention care managers increased screening rates in Spanish-speaking women facing barriers such as lack of information and trouble scheduling appointments (Beach et al. 2007).
This study has several limitations. While our results raise important questions for further investigation, they are limited by our focus on one health care system in the US and two language groups. Factors that impact screening in these particular groups or that are unique to the US, such as our lack of universal healthcare, may impact screening differently than in other groups and national contexts. Additionally, as our recruitment strategy was an opt-in system, it is possible that only physicians informed and interested in language disparities sought to participate in the study. Finally, the interviews were conducted by the PI, who holds a leadership position in our health system; participant responses may have been influenced by this relationship.
5. CONCLUSION
The current study was a qualitative interview study of primary care physicians that sought to illuminate and organize the factors affecting receipt of preventive care in Limited English proficient (LEP) populations. We found that primary care physicians attribute the low rates of preventive cancer screening among LEP patients to a variety of patient, physician, interpreter, and system barriers, most of which go beyond simple language barriers. We organized these factors into a novel conceptual model. Our results suggest that multifactorial interventions that address screening at the patient, physician, and system level can and should be developed to reduce these barriers and enhance the impact of facilitators. Ideas for interventions include providing mobile screening options, increasing use of low-cost, non-invasive screening techniques, implementing culturally competent patient education, and addressing physician discomfort with complex scheduling systems and different cultures. We plan to use the information presented to develop an intervention specific to our system and to investigate its impact on increasing screening rates among LEP patients so that the rates are comparable to their English-speaking peers.
Acknowledgments
Funders: The authors would like to thank the University of Wisconsin Carbone Comprehensive Cancer Center (UWCCC) for the funds to complete this project. This work is also supported in part by NIH/NCI P30 CA014520- UW Comprehensive Cancer Center Support. Additional support was provided by the Health Innovation Program. The project described was supported by the Clinical and Translational Science Award (CTSA) program, previously through the National Center for Research Resources (NCRR) grant 1UL1RR025011, and now by the National Center for Advancing Translational Sciences (NCATS), grant 9U54TR000021. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Additional funding for this project was provided by the UW School of Medicine and Public Health from the Wisconsin Partnership Program and the Shapiro Summer Research Program.
Contributors: We are grateful for the support of our study participants and the other members of our research team.
Biographies
Kelly H Bruce received her BA in Biological Chemistry from Grinnell College in Grinnell, Iowa. She is currently a medical student at the University of Wisconsin School of Medicine and Public Health. Her research interests include health disparities and global health. Address for correspondence: 800 University Bay Drive, Suite 210, MC 9445, Madison, WI, USA, 53705. khbruce@wisc.edu
Rebecca J Schwei received her MPH in Global Health from Emory University and is currently a Research Specialist at the University of Wisconsin. Her research interests include health disparities, provision of linguistically appropriate health care, and the social determinants of health. Address for correspondence: 800 University Bay Drive, Suite 210, Madison, WI, USA 53705. rschwei@medicine.wisc.edu
Linda S Park received her Ph.D. in Human Development and Family Studies from the University of Wisconsin-Madison. Her research interests include cultural gerontology, health disparities, health literacy, and policy. She is currently an associate lecturer in the School of Social Work and involved in research with the Department of Medicine in the School of Medicine and Public Health at the University of Wisconsin-Madison. Address for correspondence: School of Social Work, University of Wisconsin-Madison, 1350 University Ave, Madison, WI 53706. lsujinpark@gmail.com
Elizabeth A Jacobs attended medical school at the University of California at San Francisco. She is currently Associate Professor at the University of Wisconsin School of Medicine and Public Health. Her research interests include access to, and cultural specificity of, medical care delivered to minority patients, the impact of interpreter service interventions on the cost and quality of healthcare, and health literacy and numeracy. Address for correspondence: 800 University Bay Drive, Suite 210, Madison, WI, USA, 53705. eajacobs@medicine.wisc.edu
APPENDIX
Semi-Structured Interview Guide for Physician Interviews
Warm Up: Thank you for agreeing to take time out of your busy schedule to speak with me today. I am going to ask you a few questions about what facilitates and hinders your ability to deliver preventive cancer services in your primary care practice. By preventive cancer services I mean those on this card [Hand physician card with services on it so they can keep them in mind]: mammography, pap smears, FOBT or other colorectal screening and behavioral risks such as alcohol and tobacco use.
Before we begin the discussion we need to go over the information form. This is a form that provides you with information about the discussion today. You will take a copy of it with you at the end of the day. I will give you a couple of minutes for you to read it.
[Complete the consent process]
Ok, if you don’t have any more questions, let’s get started.
Q1: What has been your experience providing cancer screenings in general?
Q2: What in the clinic facilitates your ability to provide these services? What hinders it?
Q3: What in your own practice facilitates your ability to provide these services? What hinders it?
-
Q4: What has been your experience providing behavioral screenings in general?
[Probe on facilitators and barriers for each behavioral screening.] Q5: What is your experience providing these services to patients who do not speak English well enough to communicate or understand English? (Probe on each)
Q6: What facilitates your ability to provide these services to LEP patients? What hinders it?
-
Q7: Do you ever communicate with patients in a language other than English?
IF YES.…Is it all different than when communicating in English? If yes, how?How about compared to using an interpreter for languages you do not know?DO YOU EVER communicate through interpreters? If NO, SKIP to Q10? -
Q8: What has been your experience working with interpreters services in your clinic
[Probes: What kind of influence does it have on care? How hard/easy is it?] -
Q9: What do you do if you cannot access interpreter services?
[Probes: How do you communicate? What do you think of the quality of your communication:?] -
Q10: What could be done from a system and/or primary care redesign level to reduce these barriers for LEP patients?
[Probe on if these are special to LEP or not. AND if they think it is culture, language or both if they say yes to it is special for LEP] -
Q11: Are there recommendations you have for the clinic or health care system to make it easier to provide preventive cancer screenings to LEP patients?
Thank you for your time, anything else you want us to know on this topic?
References
- Akers AY, Newmann SJ, et al. Factors underlying disparities in cervical cancer incidence, screening, and treatment in the United States. Curr Probl Cancer. 2007;31(3):157–81. doi: 10.1016/j.currproblcancer.2007.01.001. [DOI] [PubMed] [Google Scholar]
- Australian Government, Department of Immigration and Citizenship. Australia’s Migration Trends 2011–12 at a glance. [Google Scholar]
- Beach ML, Flood AB, Robinson CM, Cassells AN, Tobin JN, Greene MA, et al. Can language-concordant prevention care managers improve cancer screening rates? Cancer Epidemiology Biomarkers & Prevention. 2007;16(10):2058–2064. doi: 10.1158/1055-9965.EPI-07-0373. [DOI] [PubMed] [Google Scholar]
- Bowen GA. Naturalistic inquiry and the saturation concept: a research note. Qualitative Research. 2008;8(1):137–152. [Google Scholar]
- Caelli K, Ray L, Mill J. “Clear as mud”: Toward greater clarity in generic qualitative research. International Journal of Qualitative Methods. 2008;2(2):1–13. [Google Scholar]
- Cheng EM, Chen A, Cunningham W. Primary language and receipt of recommended health care among Hispanics in the United States. Journal of General Internal Medicine. 2007;22(Suppl 2):283–288. doi: 10.1007/s11606-007-0346-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cioffi RN. Communicating with culturally and linguistically diverse patients in an acute care setting: nurses’ experiences. International Journal of Nursing Studies. 2003;40(3):299–306. doi: 10.1016/s0020-7489(02)00089-5. [DOI] [PubMed] [Google Scholar]
- CTC & Associates LLC. Limited English Proficiency in Wisconsin. Wisconsin Department of Transportation, Transportation Synthesis Report; 2010. [Google Scholar]
- De Alba I, Sweningson JM. English proficiency and physicians’ recommendation of Pap smears among Hispanics. Cancer Detection & Prevention. 2006;30(3):292–296. doi: 10.1016/j.cdp.2006.05.003. [DOI] [PubMed] [Google Scholar]
- Diez Guardia N, Pichelmann K. Labour Migration Patterns in Europe: Recent Trends, Future Challenges; European Economy, Economic Papers. 2006. [Google Scholar]
- Fang DM, Baker DL. Barriers and facilitators of cervical cancer screening among women of Hmong origin. Journal of Health Care for the Poor & Underserved. 2013;24(2):540–555. doi: 10.1353/hpu.2013.0067. [DOI] [PubMed] [Google Scholar]
- Fernandez ME, Gonzales A, Tortolero-Luna G, Williams J, Saavedra-Embesi M, Chan W, et al. Effectiveness of Cultivando la Salud: a breast and cervical cancer screening promotion program for low-income Hispanic women. American Journal of Public Health. 2009;99(5):936–943. doi: 10.2105/AJPH.2008.136713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gadon M, Balch GI, Jacobs EA. Caring for patients with limited English proficiency: the perspectives of small group practitioners. Journal of General Internal Medicine. 2007;22(Suppl 2):341–6. doi: 10.1007/s11606-007-0311-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Education Today. 2004;24(2):105–112. doi: 10.1016/j.nedt.2003.10.001. [DOI] [PubMed] [Google Scholar]
- Ginsburg JA. Language Services for Patients with Limited English Proficiency: Results of a National Survey of Internal Medicine Physicians (Position Paper) American College of Physicians; 2007. [Google Scholar]
- Harlan LC, Bernstein AB, Kessler LG. Cervical cancer screening: who is not screened and why? American Journal of Public Health. 1991;81(7):885–890. doi: 10.2105/ajph.81.7.885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qualitative Health Research. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- Jacobs EA, Karavolos K, Rathouz PJ, Ferris TG, Powell LH. Limited English proficiency and breast and cervical cancer screening in a multiethnic population. American Journal of Public Health. 2005;95(8):1410–1416. doi: 10.2105/AJPH.2004.041418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang W, Wang JH, Chen MY, Mandelblatt JS. Language use and the receipt of cancer screening recommendations by immigrant Chinese American women. Journal of Womens Health (Larchmt) 2009;18(2):201–207. doi: 10.1089/jwh.2007.0709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim JW. Linguistic and ethnic disparities in breast and cervical cancer screening and health risk behaviors among Latina and Asian American women. Journal of Womens Health (Larchmt) 2010;19(6):1097–1107. doi: 10.1089/jwh.2009.1614. [DOI] [PubMed] [Google Scholar]
- Lor M, Bowers B. Evaluating teaching techniques in the Hmong breast and cervical cancer health awareness project. Journal of Cancer Education. 2014;29(2):358–365. doi: 10.1007/s13187-014-0615-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lor M, Khang PY, Xiong P, Moua KF, Lauver D. Understanding Hmong women’s beliefs, feelings, norms, and external conditions about breast and cervical cancer screening. Public Health Nursing. 2013;30(5):420–428. doi: 10.1111/phn.12043. [DOI] [PubMed] [Google Scholar]
- Maar M, Burchell A, Little J, Ogilvie G, Severini A, Yang JM, et al. A qualitative study of provider perspectives of structural barriers to cervical cancer screening among first nations women. Womens Health Issues. 2013;23(5):e319–325. doi: 10.1016/j.whi.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Natale-Pereira A, Marks J, Vega M, Mouzon D, Hudson SV, Salas-Lopez D. Barriers and facilitators for colorectal cancer screening practices in the Latino community: perspectives from community leaders. Cancer Control. 2008;15(2):157–165. doi: 10.1177/107327480801500208. [DOI] [PubMed] [Google Scholar]
- Navarro AM, Senn KL, McNicholas LJ, Kaplan RM, Roppe B, Campo MC. Por La Vida model intervention enhances use of cancer screening tests among Latinas. American Journal of Preventive Medicine. 1998;15(1):32–41. doi: 10.1016/s0749-3797(98)00023-3. [DOI] [PubMed] [Google Scholar]
- Ogilvie G, Krajden M, Maginley J, Isaac-Renton J, Hislop G, Elwood-Martin R, et al. Feasibility of self-collection of specimens for human papillomavirus testing in hard-to-reach women. Canadian Medical Association Journal. 2007;177(5):480–483. doi: 10.1503/cmaj.070013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandya C, Batalova Jeanne, McHugh Margie. Limited English Proficient Individuals in the United States: Number, Share, Growth, and Linguistic Diversity. Washington, DC: Migration Policy Institute; 2011. [Google Scholar]
- Roberts GW, Irvine FE, Jones PR, Spencer LH, Baker CR, Williams C. Language awareness in the bilingual healthcare setting: a national survey. International Journal of Nursing Studies. 2007;44(7):1177–1186. doi: 10.1016/j.ijnurstu.2006.03.019. [DOI] [PubMed] [Google Scholar]
- Somerville W. Future Immigration Patterns and Policies in the United Kingdom. Washington, DC: Migration Policy Institute; 2009. [Google Scholar]
- Tu SP, Yip MP, Chun A, Choe J, Bastani R, Taylor V. Development of intervention materials for individuals with limited English proficiency: lessons learned from “Colorectal Cancer Screening in Chinese Americans”. Medical Care. 2008;46(9 Suppl 1):S51–61. doi: 10.1097/MLR.0b013e31817f0cde. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census Bureau. Language Use. 2014 Feb 11; Retrieved February 26, 2014, from http://www.census.gov/hhes/socdemo/language/
- Watts L, Joseph N, et al. Understanding barriers to cervical cancer screening among Hispanic women. Am J Obstet Gynecol. 2009;201(2):199.e1–199.e8. doi: 10.1016/j.ajog.2009.05.014. [DOI] [PubMed] [Google Scholar]
- World Health Organization. [Accessed January 23, 2015];Cancer country profiles. 2014 Available at: http://www.who.int/cancer/country-profiles/en/
- Yarnall KS, Pollak KI, Ostbye T, Krause KM, Michener JL. Primary care: is there enough time for prevention? American Journal of Public Health. 2003;93(4):635–641. doi: 10.2105/ajph.93.4.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youdelman M, Kohn Nancy, Pryor Carol, Rukavina Mark, Seifert Robert. Language Services Action Kit: The Growing Need for Language Services. Washington, DC and Boston, MA: National Health Law Program (NHeLP) and The Access Project; 2004. [Google Scholar]