Abstract
Do your kidneys know what time it is? Mounting evidence from human studies and animal models strongly suggests that the answer to this question is yes. The time has come to start reporting the time of day at which renal physiology studies are performed.
Keywords: circadian rhythm, physiology, reproducibility, rigor
do your kidneys know what time it is? Mounting evidence from human studies and animal models strongly suggests that the answer to this question is yes. Human studies dating back several decades have consistently demonstrated time-of-day-dependent changes in glomerular filtration rate, renal electrolyte excretion, renal blood flow, and circulating levels of several hormones that act directly on the kidney, including aldosterone (Fig. 1) (for review see Refs. 14 and 19). A new report suggests that these rhythms are evident in children and teenagers, in addition to adults (6). Animal data from several laboratories have established a role for the molecular clock in the regulation of blood pressure, renal electrolyte handling, fetal kidney development, glomerular filtration rate, and renal metabolism (reviewed in Refs. 2 and 13). Importantly, unbiased global transcriptomic studies also support a role for circadian rhythms in renal function; the kidney is second only to the liver in terms of the absolute number of mRNAs that oscillate with a significant circadian rhythm (20). Collectively, these studies support the concept that time is an important aspect of renal function. A logical consequence of this finding is that researchers should consider the time of day in experimental design and, subsequently, should report the time of day at which experiments are conducted.
Fig. 1.
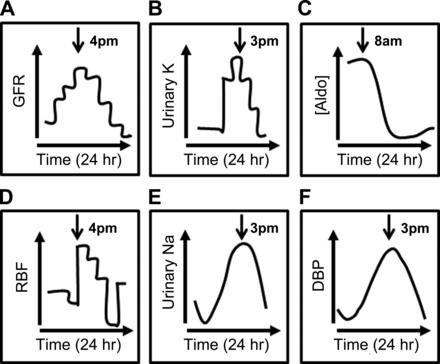
Circadian rhythms related to renal physiology. Representative human data are illustrated to convey the inherent circadian rhythm present in many physiological functions related to the kidney. Data have been redrawn from the original publications: A and D from Vagnucci et al. (15), B from Moore-Ede (8), C from Williams et al. (17), E from Voogel et al. (16), and F from Agarwal and Light (1). Arrows indicate the approximate time of the peak signal for each parameter. GFR, glomerular filtration rate; [Aldo], plasma aldosterone concentration; RBF, renal blood flow; DBP, diastolic blood pressure.
The timing of physiological function is controlled by the circadian clock. On a basic level, the core molecular clock comprises several transcription factors, including BMAL1, CLOCK, PER, and CRY, that regulate gene expression [for details on this mechanism, see an excellent review (10)]. These clock proteins are expressed in nearly every cell type and tissue that has been tested, and this mechanism underlying circadian rhythms is conserved from bread mold to humans (4). The term “circadian” comes from the Latin circa dia, meaning “about a day.” Franz Halberg first coined this term in the 1950s to describe rhythmic physiological functions exhibiting a period of ∼24 h (5). Together with Frederic Bartter and their colleagues, Halberg established that adrenocortical hormones, including cortisol and aldosterone, were produced with a circadian pattern (3, 7). Importantly, they demonstrated that these rhythms persisted, even under constant conditions, the defining characteristic for a process to be considered truly “circadian.”
The time of day at which physiological parameters are measured can affect the results of an experiment. One of the best examples of this concept comes from the laboratory of Dr. Ueli Schibler, arguably one of the giants in the field of circadian biology. Dr. Schibler's group published an important article in 1990 describing their discovery of a new transcription factor, D-site albumin-binding protein (DBP) (9). DBP is a master regulator of metabolic pathways in a number of tissues, including the kidney, where it exhibits dramatic circadian oscillations (11). This early work was led by Dr. Mueller, a “night owl,” who performed his animal experiments late in the day (9). Follow-up work in the laboratory failed to reproduce the initial findings! The later studies were performed by Dr. Wuarin, who had grown up on a farm and was an early riser, or a “morning lark.” Collecting animal liver samples every 4 h over a 24-h period led to the finding that DBP was only expressed at distinct times of day, as the animal was approaching its active period (18). As Dr. Schibler later described, “the ‘success’ and ‘failure’ in working with DBP depended on one's chronotype” (12).
At least one example of the importance of time in studying renal physiology comes from the laboratory of Dr. Dmitri Firsov. Zuber et al. uncovered differences in urine and plasma osmolality between wild-type and Clock-knockout mice in samples collected in the morning (2 h after lights on) compared with urine samples collected 10 h later (21). The morning samples were not significantly different, but the evening samples did exhibit significant differences. Together with hematocrit data, these data led the investigators to identify a mild diabetes insipidus in the Clock-knockout animals. This phenotype might have been missed had the separate time points not been investigated. Findings such as these lead one to wonder how often phenotypes may have been missed in animal studies, since negative findings are rarely reported in the literature. Given the recent calls by the National Institutes of Health for improved rigor and reproducibility in scientific research (http://grants.nih.gov/reproducibility/index.htm), reporting the time of day at which experiments are performed in animal models represents a critical variable affecting not only interpretation of the resulting data but also another investigator's ability to accurately reproduce those data. Moreover, consistent collection of animal tissue from control and treated groups at the same time of day would only improve data quality and experimental rigor while reducing experimental artifacts due to time-of-day-dependent differences in sampling.
An important concept related to consideration of the importance of circadian rhythms in physiology is that the vast majority of animal research is conducted during daylight hours. This time frame corresponds to the diurnal nature of humans, but it means that physiological parameters are being studied during the rodent rest phase, because mice and rats are nocturnal. The implications of this disconnect between animal and human physiology are serious, especially given the hurdle of translating animal model findings to human disease. How can this issue be addressed? A logical, and easy, first step in addressing this critical issue is to simply begin reporting the time of day at which we conduct experiments. Considering the time of day in experimental design and reporting of outcomes need not constitute a significant burden to investigators. It requires just one additional note to be made in a lab notebook and one additional sentence to be added to the methods section of scientific manuscripts. Such an important addition to our investigative and reporting mechanisms may explain data that otherwise appear to be disparate or inconsistent and is likely to have major benefits for reproducibility of our findings.
GRANTS
This work was supported by National Institute of Diabetes and Digestive and Kidney Diseases Grant R03 DK-098460 and the American Society of Nephrology Foundation for Kidney Research.
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author.
AUTHOR CONTRIBUTIONS
M.L.G. drafted the manuscript; M.L.G. edited and revised the manuscript; M.L.G. approved the final version of the manuscript.
ACKNOWLEDGMENTS
The author thanks Dr. Charles S. Wingo for critical reading of the manuscript.
REFERENCES
- 1.Agarwal R, Light RP. Physical activity is a determinant of circadian blood pressure variation in chronic kidney disease. Am J Nephrol 31: 15–23, 2010. [DOI] [PubMed] [Google Scholar]
- 2.Bonny O, Firsov D. Circadian regulation of renal function and potential role in hypertension. Curr Opin Nephrol Hypertens 22: 439–444, 2013. [DOI] [PubMed] [Google Scholar]
- 3.Gordon RD, Spinks J, Dulmanis A, Hudson B, Halberg F, Bartter FC. Amplitude and phase relations of several circadian rhythms in human plasma and urine: demonstration of rhythm for tetrahydrocortisol and tetrahydrocorticosterone. Clin Sci 35: 307–324, 1968. [PubMed] [Google Scholar]
- 4.Gumz ML, Rabinowitz L, Wingo CS. An integrated view of potassium homeostasis. N Engl J Med 373: 60–72, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Halberg F. [Physiologic 24-hour periodicity; general and procedural considerations with reference to the adrenal cycle]. Int Z Vitaminforsch Beih 10: 225–296, 1959. [PubMed] [Google Scholar]
- 6.Mahler B, Kamperis K, Ankarberg-Lindgren C, Djurhuus JC, Rittig S. The effect of puberty on diurnal sodium regulation. Am J Physiol Renal Physiol 309: F873–F879, 2015. [DOI] [PubMed] [Google Scholar]
- 7.Meyer WJ 3rd, Diller EC, Bartter FC, Halberg F. The circadian periodicity of urinary 17-ketosteroids, corticosteroids, and electrolytes in congenital adrenal hyperplasia. J Clin Endocrinol Metab 43: 1122–1127, 1976. [DOI] [PubMed] [Google Scholar]
- 8.Moore-Ede MC. Physiology of the circadian timing system: predictive versus reactive homeostasis. Am J Physiol Regul Integr Comp Physiol 250: R737–R752, 1986. [DOI] [PubMed] [Google Scholar]
- 9.Mueller CR, Maire P, Schibler U. DBP, a liver-enriched transcriptional activator, is expressed late in ontogeny and its tissue specificity is determined posttranscriptionally. Cell 61: 279–291, 1990. [DOI] [PubMed] [Google Scholar]
- 10.Partch CL, Green CB, Takahashi JS. Molecular architecture of the mammalian circadian clock. Trends Cell Biol 24: 90–99, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pizarro A, Hayer K, Lahens NF, Hogenesch JB. CircaDB: a database of mammalian circadian gene expression profiles. Nucleic Acids Res 41: D1009–D1013, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schibler U. Peripheral phase coordination in the mammalian circadian timing system. J Biol Rhythms 24: 3–15, 2009. [DOI] [PubMed] [Google Scholar]
- 13.Solocinski K, Gumz ML. The circadian clock in the regulation of renal rhythms. J Biol Rhythms 30: 470–486, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stow LR, Gumz ML. The circadian clock in the kidney. J Am Soc Nephrol 22: 598–604, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vagnucci AH, Shapiro AP, McDonald RH Jr. Effects of upright posture on renal electrolyte cycles. J Appl Physiol 26: 720–731, 1969. [DOI] [PubMed] [Google Scholar]
- 16.Voogel AJ, Koopman MG, Hart AA, van Montfrans GA, Arisz L. Circadian rhythms in systemic hemodynamics and renal function in healthy subjects and patients with nephrotic syndrome. Kidney Int 59: 1873–1880, 2001. [DOI] [PubMed] [Google Scholar]
- 17.Williams GH, Cain JP, Dluhy RG, Underwood RH. Studies of the control of plasma aldosterone concentration in normal man. I. Response to posture, acute and chronic volume depletion, and sodium loading. J Clin Invest 51: 1731–1742, 1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wuarin J, Schibler U. Expression of the liver-enriched transcriptional activator protein DBP follows a stringent circadian rhythm. Cell 63: 1257–1266, 1990. [DOI] [PubMed] [Google Scholar]
- 19.Wuerzner G, Firsov D, Bonny O. Circadian glomerular function: from physiology to molecular and therapeutical aspects. Nephrol Dial Transplant 29: 1475–1480, 2014. [DOI] [PubMed] [Google Scholar]
- 20.Zhang R, Lahens NF, Ballance HI, Hughes ME, Hogenesch JB. A circadian gene expression atlas in mammals: implications for biology and medicine. Proc Natl Acad Sci USA 111: 16219–16224, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zuber AM, Centeno G, Pradervand S, Nikolaeva S, Maquelin L, Cardinaux L, Bonny O, Firsov D. Molecular clock is involved in predictive circadian adjustment of renal function. Proc Natl Acad Sci USA 106: 16523–16528, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]


