Abstract
Infective endocarditis is a rare occurrence in the main pulmonary artery trunk and even rarer in tetralogy of Fallot.
Keywords: Echocardiography, Infective endocarditis, Main pulmonary artery, Tetralogy of Fallot
INTRODUCTION
Tetralogy of Fallot (TOF) is the most common congenital heart disease with survival to adulthood. Infective endocarditis accounts for 1.7–6.2 cases per 100,000 in the Western world but such estimates are not available from India for patients with a congenital heart lesion.[1] This report is unique in that an embolic lesion of the main pulmonary artery (MPA), probably of infective etiology, was noted in a child with TOF.
CASE REPORT
An unusual association of TOF and bacterial endocarditis of the MPA is presented.
CONCLUSION
In this case report, the diagnostic implications and therapeutic consequences of TOF with infective endocarditis are discussed. In addition, this case report emphasizes the use of transesophageal echocardiography (TEE) in patients with congenital heart disease for shunt surgery. The risk of a coincident infective endocarditis in patients with congenital heart disease is highlighted, and the need for careful attention to this possibility during intraoperative evaluation of such patients emphasized, especially if it has been overlooked in the preoperative data!
A 7-year-old male known case of TOF presented to emergency room with a history of cyanotic spells. On the basis of clinical examination, he was cyanosed and was not able to maintain saturation, thus intubated and was planned to shift to operation room for emergency central shunt. Primary examination of transthoracic echo or angiography was not done; however, old echo confirmed the diagnosis of TOF. Detailed intraoperative examination of TEE revealed a large perimembranous ventricular septal defect (VSD) of 1.52 mm, overriding of aorta more than 50% [Figure 1] and to our surprise a vegetation in MPA, measuring 1.67 mm × 0.735 mm [Figures 2 and 3], which is a rarity. Continuous-wave Doppler showed a gradient of 40 mmHg across VSD [Figure 4]. The child was extubated after 5 days following recovery from pneumonia and discharged from the hospital on the 20th postoperative day, after full recovery. On the first follow-up visit, he had no complaints. His histopathology and culture report confirmed the diagnosis of bacterial endocarditis.
Figure 1.
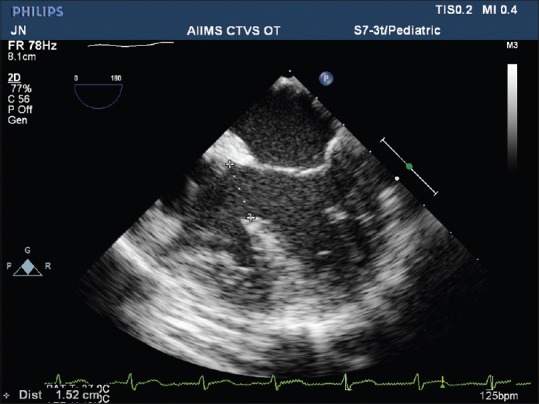
Mid-esophageal four chamber view showing subaortic ventricular septal defect of size 1.52 cm
Figure 2.
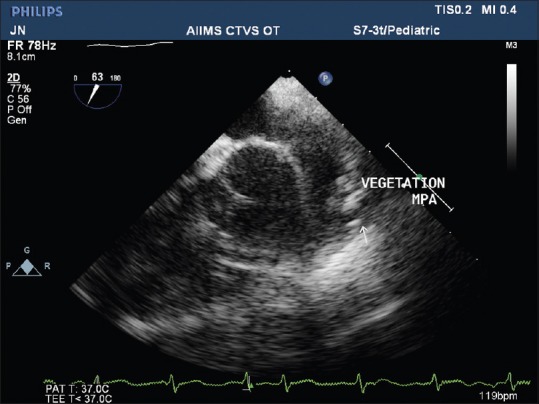
Mid-esophageal ascending aorta short axis showing vegetation in main pulmonary artery with attachment at the base
Figure 3.
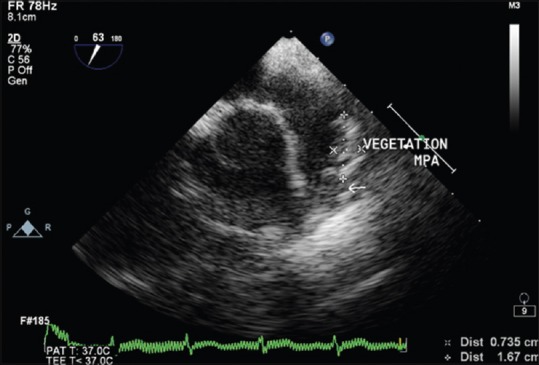
Mid-esophageal ascending aorta short axis showing vegetation 1.67 cm × 0.735 cm in main pulmonary artery
Figure 4.
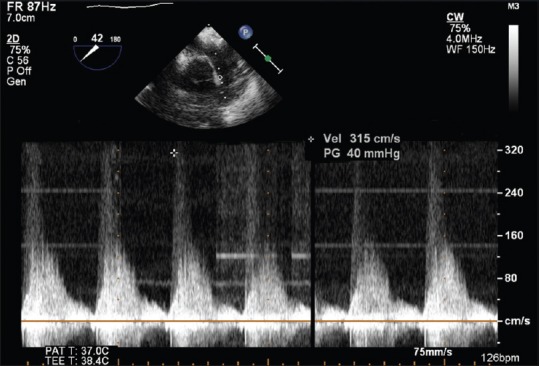
Continuous-wave Doppler showing a gradient of 40 mmHg across the ventricular septal defect
Echocardiography plays a key role in the diagnosis of infective endocarditis, its complications, follow-up evaluation after therapy, and prognostic assessment.[2,3] This report describes patient with TOF with vegetations in MPA who presented with cyanotic spells. This case illustrates and reiterates the important role of TEE in diagnosis of intraoperative infective endocarditis lesion in providing hemodynamic data and helped to review the surgical discussion of the central shunt and converted the case into total correction and gave a new lease of life to the patient. It was being overlooked as an artifact otherwise. TEE intraoperatively in TOF is a must.[4]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kothari SS, Ramakrishnan S, Bahl VK. Infective Endocarditis – An Indian Perspective. Indian Heart J. 2005;57:289–94. [PubMed] [Google Scholar]
- 2.Habib G, Badano L, Tribouilloy C, Vilacosta I, Zamorano JL, Galderisi M, et al. Recommendations for the practice of echocardiography in infective endocarditis. Eur J Echocardiogr. 2010;11:202–19. doi: 10.1093/ejechocard/jeq004. [DOI] [PubMed] [Google Scholar]
- 3.Shapira Y, Weisenberg DE, Vaturi M, Sharoni E, Raanani E, Sahar G, et al. Contemporary results of mitral valve repair for infective endocarditis. IMAJ. 2007;9:299–302. [PubMed] [Google Scholar]
- 4.Gupta SD, Das S, Ghose T, Sarkar A, Goswami A, Kundu S. Controlled transient respiratory arrest along with rapid right ventricular pacing for improving balloon stability during balloon valvuloplasty in pediatric patients with congenital aortic stenosis - A retrospective case series analysis. Annals of Cardiac Anaesthesia. 2010;13:236–40. doi: 10.4103/0971-9784.69076. [DOI] [PubMed] [Google Scholar]


