Abstract
Purpose
There is little to guide clinicians in terms of evidence-based interventions for children with cochlear implants who demonstrate morpheme errors. This feasibility study tested the utility of a treatment targeting grammatical morpheme errors.
Method
Three children (ages 4–5 years) received Enhanced Conversational Recast treatment, a version of conversational recast treatment that focuses on a single morpheme error at a time, emphasizes attention to clinician input, and uses high linguistic variability with clinician input. A period of recasting was followed by 24 auditory presentations of the target morpheme in short sentences. After an initial baseline period, children were treated in individual sessions over 21–26 days.
Results
All children showed improved use of targeted grammatical morpheme use, both in elicited contexts and in terms of spontaneous use. Spontaneous use was best for the 2 children who were implanted earliest and whose audiograms showed the best hearing postimplant. Performance by a 3rd child diagnosed with auditory neuropathy spectrum disorder was more variable but still showed positive change.
Conclusions
The results indicate that the treatment can be effective for children with cochlear implants. The pattern of results across children also suggests potential variables that may moderate treatment effects.
Cochlear implants are an effective means to facilitate spoken language development in prelingually deaf children. Prior to the availability of cochlear implants, children with significant hearing loss showed highly variable language delays compared with their hearing peers. With the advent of cochlear implantation, this gap has been reduced significantly. Svirsky, Robbins, Kirk, Pisoni, and Miyamoto (2000) indicated that the average child who received cochlear implants learned 1 year's worth of language in the same time period, although others have suggested considerably slower language learning rates compared with hearing peers (Blamey et al., 2001). Despite variable findings, the current research agrees that early implantation facilitates positive language outcomes (Kirk et al., 2002; Kirk, Miyamoto, Ying, Perdew, & Zuganelis, 2002; Tobey et al., 2013). Research indicates that children implanted before 2 years of age develop language faster than children implanted later, and early-implanted children may achieve expressive language skills that approach typical language development (Holt & Svirsky, 2008; Nicholas & Geers, 2007).
Despite these positive reports, many children present with significant delays at the time of implantation that do not resolve postimplantation (Blamey et al., 2001; Geers, 2004; Niparko et al., 2010). Geers (2004) evaluated a nationwide sample of 8- and 9-year-olds who were implanted between 24 and 35 months. Of these children, only 43% demonstrated average language skills for their chronological age, leaving 57% with language delays. Others have reported that children with cochlear implants frequently present with delays in grammatical morphology, regardless of age of implantation (Nikolopoulos, Dyar, Archbold, & O'Donoghue, 2004; Rudmin, 1983; Tomblin, Spencer, Flock, Tyler, & Gantz, 1999). Such delays often persist longer than deficits in other language domains. Hammer, Coene, Rooryck, and Govaerts (2014) suggested that fewer than 50% of cochlear implant users achieve age-appropriate use of grammatical morphology. Grammatical morphology may be difficult to acquire because these morphemes tend to add little to utterance meaning, are in the word-final position, and often consist of high-frequency consonants (e.g., /s/, /t/, /d/) that tend to be less audible than other consonants.
To date, there is a paucity of research on language treatment for children with cochlear implants. For example, a 2014 review of auditory–verbal therapies for children with hearing loss concluded that there were no studies that met the research quality criteria for inclusion in a Cochrane Database review (Brennnan-Jones, White, Rush, & Law, 2014). This is not a new problem, with similar concerns raised concerning the paucity of quality studies 10 years previously (Eriks-Brophy, 2004). The reasons for the absence of a coherent treatment literature include the diversity of the population of those with hearing impairment (e.g., Ertmer, Leonard, & Pachuilo, 2002; White & Brennan-Jones, 2014) as well as the diversity of the goals addressed by different treatment methods (White & Brennan-Jones, 2014). For example, some of the more recent studies have targeted diverse areas such as narratives (Justice, Swanson, & Buehler, 2008), literacy (Lederberg, Miller, Easterbrooks, & Connor, 2014), and language development broadly defined (Ertmer et al., 2002; Hogan, Stokes, White, Tyzkiewicz, & Woolgar, 2008). To our knowledge, there has not been a treatment procedure that specifically targets morphology in the oral domain for children with cochlear implants.
In contrast, there are multiple studies addressing treatment of grammatical deficits for another population that also routinely displays these deficits (i.e., children with specific language impairment [SLI]). Given that both groups of children share grammatical deficits, approaches that have been successful for children with SLI might also be useful for children with cochlear implants. Conversational recast is one treatment technique that has been used successfully to treat morpheme deficits in children with SLI (see Cleave, Becker, Curran, Owen Van Horne, & Fey, 2015, or McCauley & Fey, 2006 for reviews). Conversational recast treatment does not involve explicit instruction of targeted grammatical forms, but rather provides verbal models of at least one grammatical form (e.g., auxiliary is, plural s) that is the target of treatment. Intervention occurs in the context of a conversation between a child and a clinician who are both engaged in a child-friendly activity (e.g., book reading, craft activity, games). The clinician specifically arranges the environment to create situations in which the child will attempt to use the targeted grammatical form(s). Children may make spontaneous utterances, or clinicians may elicit utterances from the child (Hassink & Leonard, 2010). A child utterance, either spontaneous or elicited, is referred to as a platform utterance because it serves as the base for a clinician response to that utterance. The clinician then provides the recast by immediately repeating the child's utterance, correcting any ungrammatical aspects that may have occurred. The recasts maintain the semantic content and the approximate length of the child's utterance. Because recasts follow child utterances, candidates for this intervention must have enough language to provide opportunities for the clinician to recast. For treatment of grammatical morphemes, this would imply that children are minimally combining words into two-word sentences.
Enhanced conversational recast is a new application of the conversational recast technique that has yielded successful outcomes in grammatical acquisition in children with SLI (Plante et al., 2014). This approach to recast intervention includes three key features that are not always present in traditional conversational recast treatment. First, enhanced conversational recast treatment recasts a single grammatical form (i.e., focused recasting). Other versions of conversational recast have included recasts of any grammatical errors that a child produces in a treatment session (i.e., broad recasting). Broad recasts have not been as successful as targeting a single grammatical error at a time (Yoder, Molfese, & Gardner, 2011). By focusing recasts on a single linguistic form, the child may be more likely to recognize the correct form of the targeted morpheme in the clinician's input than when many grammatical forms are recast. Second, the enhanced conversational recast approach recasts 24 unique exemplars of a single grammatical form in each treatment session and presents a high diversity of verbs across sessions (Plante et al., 2014). Several experimental studies of language learning (Gómez, 2002; Grunow, Spaulding, Gómez, & Plante, 2006; Von Koss Torkildsen, Dailey, Aguilar, Gómez, & Plante, 2013) have documented that listeners who heard 24 unique exemplars within a single session learned the intended grammatical form and could generalize it to untrained exemplars, but those who heard fewer exemplars could not, even when the few exemplars were repeated multiple times. Therefore, presentation of a large variety of unique exemplars was more effective than repeated presentation of a limited number of exemplars.
Attentional focus is the final component of enhanced conversational recast treatment. Toro, Sinnett, and Soto-Faraco (2005) investigated the role of attention to auditory input in statistical learning of a novel language and found that performance was significantly affected by attention. This suggests that attentional resources must be actively directed to the speech stream in order for learning to occur. The present study acknowledged the central role of attention to the clinician's input for successful extraction of the target grammatical morpheme. Therefore, treatment used attentional cues, tailored to each child, just prior to clinician recasts to facilitate the child's attention to those recasts.
The Current Study
The present study sought to evaluate the feasibility of a language treatment method that combined enhanced conversational recast treatment with auditory bombardment for young cochlear implant users who present with morphosyntax delays. We supplemented the recast technique with a brief (2–3 min) of auditory bombardment to provide a period of condensed input for the children with cochlear implants. The rationale for this addition was that the additional auditory models may particularly benefit children above and beyond recasting alone, particularly for children who have reduced auditory experience or residual hearing loss. This is consistent with the known benefits of increased auditory input for language learning in children with cochlear implants (Svirsky et al., 2000). We provided auditory bombardment after the conversational recast component because preliminary data (Meyers et al., 2014) suggested that ending a recast session with bombardment may be more effective than beginning with bombardment.
This study can be characterized as a feasibility study under Fey and Finestack's (2009) five-phase system for the development of language interventions for children. According to their system, feasibility studies constitute the first step in the treatment research process. Feasibility studies evaluate the clinical viability of an intervention approach with a specific population. Such studies are exploratory, preliminary to larger studies, and often include a small number of participants. However, feasibility studies do establish that an intervention technique can work. Positive outcomes in a feasibility study encourage larger studies with larger numbers of participants. This particular feasibility study uses a multiple probe design, as described by Murphy and Bryan (1980), with replication across children.
Given that the morphosyntax errors exhibited by children with SLI are similar to those made by cochlear implant users (Hammer et al., 2014), we hypothesized that treatment using enhanced conversational recast and auditory bombardment methods would result in increasing both elicited and spontaneous use of a treated morpheme over the intervention period. Likewise, children would show evidence that they can use the treated morpheme with untrained words. We tested this hypothesis in a single-subject study of three children who used cochlear implants for hearing amplification and who all showed omissions of grammatical morphemes.
Methods
Participants
Three children (two boys, one girl) between 4 and 5 years of age participated in this study. All children had bilateral cochlear implants. Their audiological history, languages used, and mother's education level (as a proxy for socioeconomic status) are summarized in Table 1. All participants were given a battery of assessments to determine participant qualification prior to treatment. The Goldman-Fristoe Test of Articulation–Second Edition (Goldman & Fristoe, 2000) ensured that the participants could produce or were stimulable for speech sounds that were necessary for producing targeted grammatical morphemes. The Peabody Picture Vocabulary Test–Fourth Edition (PPVT-4; Dunn & Dunn, 2007) was administered to determine lexical knowledge at the time of treatment. The Structured Photographic Expressive Language Test–Preschool II (SPELT-P2; Dawson et al., 2003) and spontaneous language sample assisted in establishing grammatical deficits and helped to identify potential targets for remediation. Refer to Table 1 for test scores for each participant.
Table 1.
Participant characteristics.
| Participant characteristics | S1: Male | S2: Female | S3: Male |
|---|---|---|---|
| Age at study (years;months) | 5;1 | 4;8 | 5;4 |
| Age at implantation (years;months) | 1;4 | Right ear: 1;1 | Right ear: 3;3 |
| Left ear: 1;6 | Left ear: 3;11 | ||
| Device | Bilateral: Cochlear Nucleus 5 | Right ear: Cochlear Nucleus 5 | Bilateral: Cochlear Nucleus 5 |
| Left ear: Cochlear Nucleus 6 | |||
| Speech recognition thresholds | Not provided | WIPI at 60 dB HL: 100% with 0 dB SNR; 80% with 5dB SNR | Right ear: Nu-CHIPS score 88% at 25 dB HL |
| Left ear: Nu-CHIPS score 92% at 20 dB HL | |||
| MLU a | 2.54 | 4.70 | 1.89 |
| SPELT-P2 b | 39 | 77 | 31 |
| PPVT-4 c | 73 | 106 | 63 |
| GFTA-2 d | 102 | 103 | 69 |
Note. SNR = signal-to-noise ratio; WIPI = Word Intelligibility by Picture Identification Test; NU-CHIPS = Northwestern University-Children's Perception of Speech.
Mean length of utterance in morphemes.
Structured Photographic Elicited Language Test, Preschool–Second Edition. Standard scores have M = 100 and SD = 15.
Peabody Picture Vocabulary Test–Fourth Edition. Standard scores have M = 100 and SD = 15.
Goldman-Fristoe Test of Articulation–Second Edition. Standard scores have M = 100 and SD = 15.
Subject 1
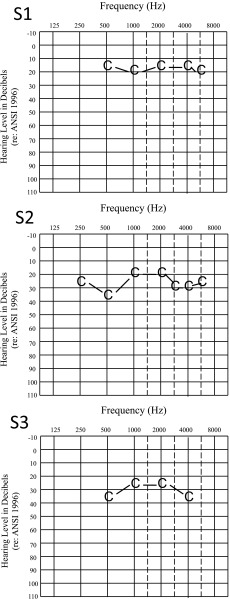
Subject 1 (S1; age 5 years, 1 month) presented with a diagnosis of congenital bilateral profound sensorineural hearing loss, mixed-receptive expressive language disorder, and developmental articulation disorder secondary to hearing loss. He communicated primarily through spoken English but occasionally utilized single-word American Sign Language (ASL). In addition, his mother was a native speaker of Russian but spoke English fluently. His father was a native monolingual English speaker. As a result, S1 was occasionally exposed to Russian, but English was spoken exclusively in his home and to him, according to his mother. During pregnancy, his mother was diagnosed with cytomegalovirus and intrauterine growth restriction. S1 was born 6 weeks premature. He passed his newborn hearing screening at birth and at 3 months of age. At 13 months, an auditory brainstem response indicated a bilateral profound hearing loss with normal middle ear function. He began receiving speech-language services at this time. This child was implanted bilaterally at 16 months with Cochlear Nucleus 5 cochlear implants. The implants were activated 1 month later. His last audiogram was obtained 3 months prior to the onset of treatment (see Figure 1).
Figure 1.
Audiograms for the three participants. Each reflects hearing levels obtained at the date closest in time to the child's participation in the treatment study.
In preschool, he received 30 min of speech-language services at school and an additional 60 min at the University of Arizona clinic each week. This child participated in the current study during the summer between preschool and kindergarten, when other treatments were on hiatus. Therefore, this child did not receive language treatment outside of the experiment during the period of his participation.
Subject 2
Subject 2 (S2; age 4 years, 8 months) was identified at 5 months of age with a bilateral profound sensorineural hearing loss of unknown origin. She did not present with any other co-occurring disorders. She began a trial period with bilateral hearing aids at 8 months of age and began receiving speech-language services with the hearing aids 2 months later. At 13 months of age, she underwent surgery to implant a Cochlear Nucleus 5 in the right ear. The same surgery followed for the left ear 5 months later. Her most recent audiogram, shown in Figure 1, occurred during the period of this study. This child began receiving speech-language services at the time of identification through an early intervention program. In preschool, she received weekly speech-language services for 60 min at school and 60 min at a private clinic, along with 60 min of school-based hearing-impaired services each week. She continued to receive speech-language services outside of the context of the experiment; however, treatment focused on vocabulary and literacy rather than grammatical forms.
S2's parents were fluent in both Arabic and English. S2 heard primarily Arabic at home and English only at school. She predominantly spoke English but understood and occasionally spoke Arabic. As her language testing indicated (see Table 1), she had relatively strong English vocabulary on the PPVT-4 (the language of the treatment) despite weak morphosyntax on the SPELT-P2.
Subject 3
Subject 3 (S3; 5 years, 4 months) was born full-term following complications throughout pregnancy. At 2 years, 11 months, he was diagnosed with a bilateral profound sensorineural hearing loss. At the time of identification, he reportedly was using 25 different words, indicating limited language for his age. He used hearing aids soon after initial identification of hearing loss, with little benefit. He was later diagnosed with auditory neuropathy spectrum disorder. This diagnosis indicates a hearing loss due to dysfunction of the inner hair cells or auditory nerve. The participant's specific characteristics consistent with this disorder were not specified in his medical records. At 3 years, 3 months he was aided with a Cochlear Nucleus 5 cochlear implant on the right ear. Eight months later he underwent the same surgery for implantation of a Cochlear Nucleus 6 implant on the left ear. This participant began receiving speech-language services at the time of identification and continued to receive school-based and private speech-language therapy throughout the course of the experiment. More specifically, each week he received 45 min of speech-language therapy at a private clinic and 60 min at school (e.g., 30 min one-on-one; 30 min push-in to the classroom). Treatment outside of the context of the experiment focused on improving vocabulary, language comprehension, utterance length, speech intelligibility, and listening skills.
This child's most recent audiogram was 3 months prior to his participation in this study and indicated a relatively flat, mild pure-tone hearing loss (see Figure 1). Despite this, he was able to identify the Ling-6 sounds (i.e., /i/, /ɑ/, /u/, /m/, /s/, /ʃ/). These assess a range of high- and low-frequency speech sounds necessary for adequate speech perception. He was able to identify all six sounds without visual cues and also to detect the allophones /t/ and /d/. Per parent report, it typically took a minimum of three sessions to complete an audiogram and speech sound identification testing due to the child's difficulty remaining in a seated position and sustaining his attention.
S3 primarily heard Spanish at home and used English and ASL at school. He spoke both English and Spanish, and used single-word ASL. To better quantify input and output in English and Spanish during a typical day, his mother and father completed the Input-Output scale as part of the Bilingual English-Spanish Assessment (Peña, Gutiérrez-Clellen, Iglesias, Goldstein, & Bedore, 2014). The Home Language Profile indicated greater percentages of English input and output. This measure indicated that 69% of S3's language input was in English, as was 72% of his language output.
The Semantics subtest of the Bilingual English-Spanish Assessment was also administered to further compare his vocabulary in English and Spanish. He had significant difficulty maintaining attention throughout the assessment and provided nearly all responses in English, despite the fact that the Spanish version was administered by a Spanish speaker who spoke to him only in Spanish and who was not the English-speaking treatment clinician. On this assessment, he received a standard score of 65 on the English subtest and a standard score of 62 on the Spanish subtest. This indicated low vocabulary scores in each language.
Materials and Procedures
General Treatment Context
Treatment was administered by the first author at a university clinic at the University of Arizona and, for S2, off-site at a preschool in a conference room. This treatment consisted of pretreatment probes, conversational recast treatment, auditory bombardment, and generalization probes.
Pretreatment Baseline
Pretreatment probe targets were identified on the basis of analysis of the SPELT-P2 and a language sample. Six to seven morphosyntactic forms were selected per child and probed for baseline use. These forms consisted of grammatical elements that the child used at low rates, incorrectly, or inconsistently. Children were seen for three consecutive sessions individually for 45 min to probe these forms. During these sessions, the clinician used toys and reading activities to engage the child in conversation. Each form was elicited 10 times in obligatory contexts (i.e., a clinician's question to the child obligated his or her use of the target morpheme). The clinician recorded whether the child correctly used the grammatical form, attempted to use the form but used it incorrectly, or did not respond despite attending to the clinician's prompt. The two morphosyntactic forms with the lowest percent accuracy across the three pretreatment probe sessions were used during the treatment phase of the study for that child. One of the forms was the treated target, and the other was the nontreated control form. The use of both target and control morphemes was intended to determine whether gains during treatment were specific to the morpheme that was the focus of treatment.
Treatment Sessions
Children participated in one-on-one treatment sessions for 30 min a day, 5 days a week. Treatment sessions were individualized according to the child's interests. Each treatment session consisted of two parts: a period of conversational recast lasting approximately 20–25 min followed by a period of auditory bombardment lasting approximately 2 min.
For the recast portion of the session, the clinician created activities that allowed for spontaneous or elicited use of the target morpheme. Sessions typically consisted of three separate activities that varied every session. Activities included games, book reading, crafts, flash cards, and free play with toys, among others. Activities were varied each day, which naturally promoted the use of different verbs from one day to the next. During each session, the clinician recast a total of 24 utterances, each of which contained a unique verb. In addition, the remaining words within the recasts were varied to the extent that the context of the conversational interaction allowed. These included verbs that the child introduced or verbs the clinician elicited. Hassink and Leonard (2010) suggested that recasts following utterances initiated by the child and those prompted by the clinician are equally effective in producing child gains. To achieve high variability of verbs recast, it was the case that the clinician elicited most verb forms during a treatment session. Recasts followed either the child's correct or incorrect attempts of the target morpheme. The recast retained the content of the child's utterance and corrected the child's use of the target morpheme when it was incorrectly used.
Auditory bombardment included sequential presentation of 24 unique exemplars of the child's target morpheme in short sentences (e.g., noun + verb, article + noun + verb). Sentences used during bombardment were short but grammatically complete (e.g., “He cried” or “The boy jumped”). Some of the words used during bombardment overlapped with words used in the recast portion of treatment, but the clinician's input was never identical for the two parts of the treatment. Children were required to attend to each auditory presentation. A simple activity (e.g., looking at picture cards, pulling paper strips from a basket that contained sentences, and handing them to the clinician to be read) was used to maintain attention during bombardment.
Most studies that have used the recast technique have not addressed the issue of attention to the recast itself. Obtaining the child's attention immediately before the recast eliminated distractions and drew the child's attention to the target grammatical form. This was intended to aid the child in making a more effective comparison between their own utterance and the clinician's recast. Prior to providing the recast, the clinician ensured that the child was attending by using auditory verbal cue (e.g., calling the child's name), a visual cue (pointing to the clinician's own chin), or tactile cues (e.g., briefly touching the child's arm). Throughout the course of treatment, a cueing system was developed for each child on the basis of what led to attention during the recast and subsequent correct usage of the target morpheme.
Warren, Fey, and Yoder (2007) noted the importance of reporting treatment intensity and duration to highlight the differences in treatment effects across studies. Table 2 reports treatment dose (number of teaching episodes in a single session), dose frequency (number of times the treatment was administered per day and per week), total number of treatment days (total number of completed sessions), and total intervention duration for each child.
Table 2.
Treatment parameters for the three participants.
| Participant | Treatment target | Treatment doses per day | Dose frequency | Total number of treatment days | Total intervention duration |
|---|---|---|---|---|---|
| S1 | Past tense –ed | 24 | Once per day; 5 times a week | 26 | 7 weeks |
| S2 | 3rd person –s | 24 | Once per day; 5 times a week | 21 | 5 weeks |
| S3 | Past tense –ed | 24 | Once per day; 5 times a week | 24 | 5 weeks |
Probe Sessions
Progress was monitored during the treatment period through probing for use of the target and control morphological forms. Probes occurred during structured play activities in which the clinician created communicative contexts that obligated the child to use the target grammatical morpheme. Probes used verbs and sets of materials that were not used during treatment sessions. This meant that probes measured generalization of the target and control morphemes to untreated verbs used in new play contexts.
Probe kits provided materials for use during probe sessions. Kits consisted of a set of materials that reflected a central theme: farm, ocean, zoo, race car, and soccer. There was also a Play-Doh kit that contained Play-Doh and items to mold and cut the Play-Doh. The clinician rotated use of the probe kits each probe day. The clinician was free to use all or some of the materials from each set to elicit the target and control morphemes.
Probe words consisted of 20 verb stems that were not used during treatment sessions. The words were common verbs for preschoolers (e.g., jump, wash, roll) that were easily implemented with the probe materials. In addition, all 20 verb stems allowed for regular past tense inflection. The clinician selected a subset of 10 words each probe session. The 10 words selected varied; however, all 20 probe words were used over the course of the study. Note that if the child used a probe word during a treatment session, the clinician did not recast the utterance.
The target and control morphemes were probed for generalization on Mondays, Wednesdays, and Fridays for 15 min prior to treatment sessions. Therefore, probe data reflected the child's use of these forms prior to that day's treatment. The clinician was able to elicit the probes in blocks (e.g., target followed by control) or randomly intermix the target and control words in a single activity as the context allowed. The clinician created conversational contexts that obligated the child to reply using the target verb and morpheme. Clinicians could use the uninflected form of the verb prior to eliciting the child's use, in order to increase the likelihood of the child using a particular probe word in their utterance. The clinician elicited the target and control morphemes 10 times each in obligatory contexts. However, if the child spontaneously used a probe verb with the target morphemes during probe sessions, this was counted towards the 10 probes for that morpheme. The clinician recorded the child's responses (i.e., correct, incorrect, no response) on paper forms.
Outcome Measures
The primary outcome measure was responses to generalization probes. These included 10 elicitation of target and 10 elicitations of control grammatical forms. Although these were elicited, they had the advantage of providing a consistent number of opportunities for use for each child. A secondary outcome measure was children's spontaneous use of their target morphemes during treatment and probe sessions. Spontaneous use was defined as a child's use of a morpheme with a verb that was not used by the clinician immediately preceding the child's use.
At the completion of treatment, parents were asked about any notable changes in their child throughout the course of the study. An open-ended question format was used to avoid guiding the parents toward a particular response. In each case, the participant's mother was interviewed.
Procedural Fidelity and Scoring Reliability
A certified speech-language pathologist supervised the first author throughout the course of this study and ensured adherence to treatment protocol. A second individual (the speech-language pathologist or a speech-language pathology assistant in training) attended treatment sessions and coded child utterances and clinician recasts during the entire session. The number of treatment sessions coded varied across children but ranged from 29% to 52% of all sessions provided to the child. The observer recorded the verbs used in the child's utterances that were then subsequently recast. This served to verify that 24 unique verbs were recast per session. Deviations from the protocol (e.g., too few or too many recasts, using the same verb in two recasts, or elicitations that did not obligate the target morpheme) were noted as procedural errors, and treatment fidelity was expressed as the percent deviations from 24 correctly administered recasts and 24 correctly administered bombardment items. Procedural reliability ranged from 89% to 99% accuracy during treatment sessions.
Point-to-point scoring reliability was also calculated for probe sessions. Reliability measures assessed the agreement for the coding of each individual child utterance as correct or incorrect. Deviations between the clinician and observer were deducted from the base of 20, corresponding to 10 target and control morpheme elicitations. Reliability ranged from 91.5% to 100% across children.
Experimental Blinding
Parents were encouraged to wait in the lobby during sessions to ensure that they were unaware of treatment targets. The parents of S2 and S3 never attended treatment sessions. S1, however, had difficulty separating from his mother. His mother preferred to stay in the room during treatment but used headphones and engaged in other activities to avoid hearing treatment targets. By the third week of treatment, she waited in the lobby. S2's mother has a background in speech-language pathology. As a result, the mother was familiar with and utilized language facilitation techniques; however, she reported that during the course of treatment, she did not change the use of language facilitation or use recasts in particular. Neither the mother nor father attended treatment sessions, and both were blind to the treatment target throughout the treatment period.
Results
Data collected during treatment are displayed graphically in Figure 2. Performance on elicited generalization probes constituted the primary measure of treatment effects. In Figure 2, production of target and control morphemes during probe sessions is compared with elicited use during the pretreatment baseline period (i.e., see B1, B2, and B3 in Figure 2). Effect sizes (d) were calculated for both target and control morphemes during generalization probes. Effect sizes have been recommended as a method for evaluating the strength of single-subject treatment data (Beeson & Robey, 2006). The d value here is one used previously for child language treatment data (Plante et al., 2014). It is calculated as follows: d = (average of three end-treatment data points – average of three pretreatment data points) / standard deviation of final three data points. Therefore, d reflects the degree of change in units of standard deviation that reflect the level of change at the end of treatment. Effect sizes are reported in Table 3.
Figure 2.
Treatment data from three participants. Bar graphs on the left indicate use of the target morpheme that occurred during treatment sessions. Target morpheme use is divided into elicited (out of 24 opportunities) and spontaneous use during each treatment session. Line graphs on the right show elicited use during generalization probes compared with elicited use during the pretreatment baseline. The total number of opportunities for use for target and control morphemes was 10 each per session.
Table 3.
Enhanced Conversational Recast treatment results.
| Child | Probe data
a
|
Spontaneous use
b
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Treated morpheme |
Control morpheme |
Treated morpheme |
|||||||
| Mean pretreatment accuracy (%) | Mean end-treatment accuracy (%) | Effect size (d) c | Mean pretreatment accuracy (%) | Mean end-treatment accuracy (%) | Control effect size (d) c | Total spontaneous use | Mean end-treatment use | Effect size (d) c | |
| S1 | 13 | 73 | 2.7 | 0 | 0 | 0.0 | 148 | 25.0 | 24.2 |
| S2 | 7 | 30 | 1.9 | 20 | 53 | 1.1 | 96 | 11.3 | 19.6 |
| S3 | 0 | 37 | 1.8 | 7 | 0 | 0.6 | 14 | 0.7 | 1.2 |
Probe data consists of child productions elicited by the clinician that used verbs that were never used during treatment.
Number of correctly inflected verbs used spontaneously during the treatment period. Note that children did not use their target morpheme spontaneously in the pretreatment phase.
Effect size d = (average end-treatment correct use – average pretreatment correct use) / standard deviation of the end-treatment correct use.
All three children showed increases in target morpheme use relative to the pretreatment baseline. S1 and S2 both showed marked gains in target morpheme use shortly after the 10th treatment day. S3 showed earlier gains, but his performance was much more variable over time compared with the other two participants. S1 and S3 showed no change in use of the control morpheme. S2, in contrast, showed gains in both the treated and control morphemes.
Spontaneous use of the child's target morpheme was a secondary measure of treatment effects. The bar graphs in Figure 2 display spontaneous use as well as children's use that was elicited as part of the recast procedures during the treatment sessions. This comparison conceptually represents the distinction between training (elicited use during treatment) and a secondary measure of learning (spontaneous use) proposed by Kamhi (2014). Note that no child used the target morpheme spontaneously during the pretreatment period. Therefore, change in the spontaneous use during treatment is relative to a pretreatment baseline of zero. The effect size d was calculated to reflect change in spontaneous use over the treatment period from a baseline of zero use. These effect sizes are reported in Table 3.
For S1 and S2, spontaneous use during the treatment session paralleled correct target use in the children's platform utterances that were then recast by the clinician. This indicates that children were increasing both their spontaneous and elicited use of the morphemes in parallel during the treatment sessions. S3 showed a different profile. Although he could correctly produce the target morpheme in platform utterances (elicited use), his spontaneous use of the target was much more limited than seen for the first two children. However, he did show one to two spontaneous productions for approximately half the treatment sessions, compared with no pretreatment spontaneous use.
During a posttreatment interview, all three mothers expressed positive views concerning their child's treatment. S1's mother noted an increase in overall output as well as use of grammatical morphology. His mother indicated that she was highly satisfied with his progress throughout the course of treatment. S2's mother and father separately made unsolicited comments regarding her increased use of the target grammatical morpheme, despite being blinded to the treatment target. This suggests that the child had significantly increased her use of the target morpheme at home. They also described the child's occasional use of short pauses between the verb root and target morpheme as treatment progressed (e.g., “She listen_s”). This indicated that she was consciously applying the rule for the target morpheme and generalizing its use outside of the therapy room. In addition, 5 months after completion of the study, this participant's mother reported that she continued to use the target form and was beginning to correctly use additional grammatical morphemes correctly (i.e., possessive –s). Likewise, S3's mother noted an increased sentence length and complexity and noted similar reports from those who frequently interacted with the child (i.e., teachers, family, etc.). Additional subject-specific treatment information is provided below.
Results for S1
S1 had difficulty adjusting initially to the structure of sessions. For this reason, the clinician implemented behavioral management techniques and created highly structured sessions with a reward system for positive behavior. After approximately 10 sessions, he adapted to the structure of treatment sessions and modified his behavior according to what was deemed good behavior (e.g., playing nicely with the clinician, complying with clinician requests, absence of disruptive behavior).
This child increased his use of the target grammatical morpheme in both spontaneous use and elicited contexts over the treatment period (see Figure 2). During treatment, he showed an increase in the primary measure, spontaneous use of the target morpheme. The clinician began to use a verbal cue (i.e., “tell me the whole thing”) on Session 11 without success, and this was subsequently discontinued. During Session 13, the clinician introduced the tactile cue of touching her chin to mark her own use the grammatical morpheme during recasts. The number of correct productions produced during the 13th session was the highest up to that point in time and continued to improve after that time. The use of the visual cue was faded, first to a briefer duration of the visual cue and then eventually to an expectant wait (pause after an elicitation request). However, S1's mother indicated during the posttreatment interview that he frequently looked at her expectantly before adding the morpheme to verb roots within conversation, as if he was waiting for her to use the visual cue utilized in treatment sessions.
As illustrated by the change in the slope of the line graph in Figure 2, this participant's progress accelerated with the introduction of the visual cue in treatment Session 13. From the onset of treatment to completion, both the spontaneous use and average percent correct use of the target morpheme during generalization probes increased. The treatment effect size (d) was 2.7 for use of the target morpheme on generalization probes and 24.2 for spontaneous use. This is consistent with end levels that are visually greater than pretreatment levels in Figure 2. In contrast, throughout the treatment, this child did not show improvement on the control (i.e., copula “was”).
Results for S2
The treatment was easily implemented for this child. It is likely that her experience in a structured preschool program facilitated a smooth transition to the structure of this treatment. In addition, her prior experience in preschool likely helped her understand the pragmatic aspects of the therapist–child interaction because it was similar to the teacher–child interactions of her school. Overall, she was an enthusiastic child who required some structure primarily due to her high levels of energy. Despite this, she quickly adapted to the implemented structure and adjusted to the routine of treatment sessions. Her treatment lasted only 20 sessions, due to extended family travel plans that limited the treatment duration to this time period.
On the primary measure of treatment progress, the effect size for S2's target morpheme use in response to generalization probes was 1.9. Recall that for probe sessions, the child was provided with a clinician model of the root for each probe word she was meant to use. The graphs of both her spontaneous productions and generalization probes showed a noteworthy increase in slope after Day 9 of treatment. Also of note, her accuracy in using her control grammatical form (wh– questions) measure also improved with the target morpheme (d = 1.1). Although somewhat variable initially, performance on the control morpheme tracked performance on the target morpheme fairly closely after Day 9.
This participant's spontaneous use of the target grammatical morpheme was initially variable but improved steadily after the ninth treatment session. On multiple treatment days, her correct spontaneous productions exceeded the number of correct elicited productions. This suggests that this child preferred to use vocabulary she generated rather than respond using the specific vocabulary provided by the clinician. When she did generate the root verb on her own, she was more successful at using the target grammatical morpheme compared with elicited use of a specific verb modeled by the clinician. On Session 16, the clinician began using the verbal cue, “tell me the whole thing,” in treatment sessions only. This was not used during generalization probes. Her elicited use of the target grammatical morpheme increased in the following session. However, spontaneous use did not show a similar jump after this cue was introduced. The change in this child's spontaneous production of her target morpheme showed a robust effect size (d) of 11.3, which is consistent with higher end-treatment levels than baseline levels in Figure 2.
Results for S3
S3 was an enthusiastic child who was most successful in highly structured sessions with a reward system for positive behavior. He required frequent redirections within sessions as he was often distracted by environmental stimuli. Despite this, he quickly adapted to the implemented structure and routine of treatment sessions. This participant typically produced one- and two-word utterances in conversation. He also frequently produced strings of jargon and sound effects, likely due to his limited expressive vocabulary. During treatment he consistently produced the phrase “She's gonna” before the elicited verb regardless of the conversational context. Because of this, the clinician's recasts included an alternate, more appropriate subject relative to the context of the activity (e.g., child: “She's gonna moved”; clinician: “It moved”). Note that the child used “she” for all pronouns, rather than to indicate female gender specifically.
S3's limited vocabulary and utterance length significantly reduced production of platform utterances, especially within free-play activities. For this reason, the clinician elicited nearly all productions within highly structured activities. Prior to elicitations, the clinician first asked the child to produce the verb root (e.g., “Say ‘yell’”), then carried out the activity (e.g., “Look at him yell at the dog”), and finally asked the participant what happened in a number of ways to maintain high linguistic variability (e.g., “What happened?; What did the boy do?”; etc.).
This child also had 4 days in which his cochlear implants were not working optimally. These occurred during Sessions 2 and 13 when the hook of one of the cochlear implants broke and in Session 14 when one implant was turning on and off throughout. On these days, this child was quick to alert the clinician that his cochlear implants were broken or not working correctly. Particularly problematic was Day 20 when the left cochlear implant was not usable due to a dead battery. As seen in Figure 2, on Session 20 the production of correct elicited verbs decreased from the previous session and substantially increased the following session. During this session, the clinician sat on the side of the functioning implant. Nonetheless, it appears that this disruption affected the child's performance on that day.
Unlike the previous two participants, this child showed an explicit, rule-based application of a phonological form, which did not necessarily represent full understanding of past tense morphology. During the first treatment session, he attended to the past tense markers /t/ and /d/ in the recasts and correctly applied these forms to word endings. Although he correctly differentiated production of /t/ and /d/ at the start of treatment, he began marking all elicited verb roots with /t/ beginning on Session 4. To counteract this trend, the clinician primarily produced verbs ending in /d/ during the bombardment phase at the end of each session. The clinician also used visual cues to differentiate /t/ and /d/. To mark /t/, the clinician pointed to her chin upon production of the grammatical morpheme. In contrast, for past tense verbs requiring the ending /d/, the clinician used the ASL sign for d on her cheek. On Session 16, the clinician began fading visual cues with variable success. This included attempts to use the verbal cue “tell me the whole thing” when he did not mark the verb in the elicited platform utterance. This was not successful in producing gains in the child's performance.
On Session 8, the child began marking the end of most utterances with /t/ (e.g., “he running/t/”). This indicated that he was overgeneralizing the placement of the target grammatical morpheme to the end of all utterances. In an attempt to reduce this behavior and implicitly illustrate that the morphological marker is attached only to the verb root, the clinician intentionally did not end the recast with the marked verb (e.g., child: “She cooked”; clinician: “She cooked the food”). The clinician utilized this same technique during the bombardment portion at the end of each session. As treatment progressed, this participant began to use /d/ and /t/ with increased accuracy on the verb rather than on the last word of the utterance, indicating recognition of which word needed to be marked. However, although the verb was almost always marked, it was not necessarily marked with the correct phoneme for that word (e.g., drool/t/, stop/d/). Therefore, by the end of treatment, errors remained in terms of marking past tense with the correct phonological form.
On the primary measure, this participant's use of the target morpheme in probe sessions increased from the onset of treatment to completion. His effect size (d) for generalization probes was 1.8. Again, this reflects a moderately higher ending level compared to pretreatment levels. However, progress was highly variable from session to session, reducing the stability of this effect size estimate. As indicated by the graphs in Figure 2, there was no appreciable slope in performance levels after the increase seen in the initial days of treatment.
S3's highly variable performance appeared to be directly related to the phoneme obligated to correctly mark the past tense form (i.e., /t/ vs. /d/). More specifically, he correctly marked most all verb roots obligating a /t/ ending, and either did not mark those ending in /d/ or marked them with /t/ (e.g., peel/t/). On probe Session 15, the majority of words elicited required the ending /d/, resulting in an overall decrease in accuracy. In contrast, on probe Session 17 eight of the 10 probe words obligated the phoneme /t/. Of these eight, he correctly marked seven, and correctly marked one requiring an ending of /d/. Although it appears as though he performed at near 100% accuracy on this session, it is important to note that this was the case due to the random selection of probe words primarily requiring the ending /t/ instead of /d/. Subsequent sessions were more balanced in regards to root verbs ending in /t/ and /d/. In contrast to his performance on target morphemes, his control form showed negligible change (d = 0.6).
S3's spontaneous use of the target grammatical morpheme did not exceed two productions within a single session. In addition, he did not produce the target grammatical morpheme spontaneously during 11 of the 23 sessions. The effect size (d) for his end-treatment spontaneous use was 1.2. Although this reflects a higher ending level for this child, this was considerably lower than the other two children. Six of the 14 spontaneous productions involved correctly inflected probe words that he used during the treatment sessions (these were not recast). His use of probe words may have occurred because these words were primed due to their repeated use during probe sessions. This also suggests that he had difficulty using his target morpheme with words he had to generate on his own.
Despite this child's limited performance, we suspect that his language had improved in other ways. At the completion of treatment, the clinician collected a language sample and administered the PPVT-4 to assess broad measures of language improvement informally observed throughout the experiment. Overall, this participant's standard score on the PPVT-4 increased by 2 points (63 to 65). Informal observations of vocabulary improvement were better than suggested by this minor increase in standard score, which was within the standard error of measurement for this test. On the other hand, this participant's mean length of utterance (MLU) increased from 1.89 (late Brown's stage I; Miller, 1981) to 2.20 (Brown's stage III) over the 5 weeks of treatment. Of note, his overall use of morphemes increased—that is, there were significantly more productions of present progressive –ing, plural –s, and evidence of emerging third person –s.
Discussion
Multiple studies using versions of conversational recast therapy have resulted in significant improvements in children's grammatical skills (see Cleave et al., 2015, for a review). Enhanced conversational recast treatment, as used by Plante et al. (2014), yielded positive gains in use of morphology by preschool children with SLI. The current study extends the Plante et al. (2014) method, combined with auditory bombardment, to address morphosyntactic deficits in children with cochlear implants.
Each child who participated in this experiment received speech-language services from the time at which their hearing loss was identified. Prior to their participation in the present study, each child was reportedly responsive to treatment in other language domains; however, they continued to show noteworthy delays in the use of morphosyntax. Following enhanced conversational recast treatment, all participants made gains. Two participants (S1 and S2) made significant gains in spontaneous use of their trained morpheme. However, one of these (S2) also made gains on a grammatical form intended to serve as a control. The third child (S3) made modest gains in spontaneous use and with better performance in elicited productions. These improvements were observed in a relatively short time period (i.e., 21–26 sessions).
Clinical validity is an important factor to consider in treatment research because functional outcomes are typically of most significance to families. The present study resulted in outcomes that extended beyond the treatment context. S1 and S3's parents noted increased language output and increased sentence length and complexity. S2's parents specifically noted gains on the treated morpheme, even though they were blinded to the target of treatment. Regardless of the degree of progress on the target grammatical morpheme, all parents expressed satisfaction with this treatment.
S1 appeared to benefit from visual cues from the clinician marking the grammatical morpheme during the recast. S1's performance improved markedly on the day that the visual cue was introduced (note the change in slope on the line graph in Figure 2). It is important to note that these cues were used in only treatment and never used within probe sessions. As treatment progressed, the clinician faded cues as the child showed increased accuracy of the target. S1 showed increased use of the target morpheme after the introduction of visual cues compared with S3, who was also given visual cues to differentiate /t/ versus /d/ past tense marking in attempt to stabilize his differential use of these past tense forms. However, the use of the visual cue for S3 did not have the same obvious impact as it had for S1. Therefore, the clinician faded cues earlier with S1 than with S3. The clinician began fading cues with S3 later in the course of treatment due to his variable use of /t/ and /d/ for the past tense form. If treatment had progressed past 23 sessions, the clinician would have likely been more successful in fading cues due to more stable use of the target form.
In addition to her gains on the target morpheme, S2 also showed gains in use of the control syntactic form (i.e., wh– questions). The gain for her control (d = 1.1) was slightly less than that seen for her treated morpheme (d = 1.9). It is important to point out that wh– questions are inherent to the format of this intervention method. That is, the clinician used wh– questions consistently when eliciting an utterance from the child that the clinician could recast, (e.g., “What does the girl do?”; “What happened?”; etc.). This resulted in high rates of exposure to wh– question forms throughout the course of treatment. Given that both the form heard within the context of the treatment methods (recasts and bombardment) and the form heard during procedural elicitations both improved, it is difficult to attribute this child's gains specifically to the treatment doses per se. Therefore, it may be that a concentrated period of exposure to previously unacquired forms was sufficient to promote development of these forms. This is consistent with the effects of targeted input on the development of linguistic forms in typically developing children (Huttenlocher, Vasilyeva, Cymerman, & Levine, 2002; Naigles & Hoff-Ginsberg, 1998).
Although not all formally tested, we present three potential factors that may have contributed to the participants' overall success with this treatment approach: MLU, vocabulary, and attention. This pretreatment metric of language production varied across children. Both S1 and S2 had MLU values of above 2.5, corresponding to Brown's Stage III (Miller, 1981). In contrast, S3's MLU was 1.89, placing him at a late Brown's Stage I. Yoder et al. (2011) reported that children who present with an MLU of less than 1.84 make more progress with milieu language training than they do with a conversational recast treatment that includes broad recasts. Although focused recasts were used in the present study, the findings of Yoder et al. (2011) raise the possibility that an alternate treatment may have been more effective for this child, given his limited language. A restricted MLU ultimately reduces the use and variety of platform utterances produced by the child. This, in turn, reduces the clinician's opportunity to recast the target morpheme despite creating obligatory linguistic contexts.
A second factor that appeared to affect outcomes may be vocabulary level. This is consistent with findings of Meyers (2015), indicating that vocabulary development at the onset of enhanced conversational recast treatment was predictive of treatment outcomes. At the start of treatment, S1 received a standard score of 39 on the PPVT-4, S3 received a 31, and S2 scored the highest with a standard score of 77. S1 and S3 attained the lowest score, but it is plausible that S1's increased MLU (2.54) counterbalanced the effects of his low vocabulary, thus improving his response to treatment. On the other hand, it is also possible that the combination of S3's reduced MLU and low vocabulary interacted to interfere with his ability to respond to this treatment in a way that low vocabulary alone for S1 did not. It is also possible that the results of the PPVT-4, administered pretreatment, underestimated S1's true skill level, due to his poor behavior during the early stages of the study.
On the contrary, S2 presented with the greatest MLU (4.70) and highest PPVT-4 score of the three participants. This is likely why she was more successful when she generated the root verb independently and less successful when prompted by the clinician to use a specific root. More specifically, she was able to generate a root verb to include in the platform utterance because she could spontaneously produce verbs already in her lexicon. This was not the case for S1 and S2 because they had lower overall language levels as evidenced by their MLU and PPVT-4 scores. For this reason, the clinician elicited most of the verb roots for these participants. According to Hassink and Leonard (2010), however, high rates of elicited utterances do not affect a child's response to recast treatment.
The final factor that has not been formally highlighted in previous conversational recast studies is attention. Recall that each treatment session consisted of three unique activities that were designed to keep the child engaged for the full treatment period. Researchers have suggested that the interactive context inherent to conversational recast therapy increases the child's attention and motivation to communicate (Camarata & Nelson, 2006; Nelson, 1989). However, this fails to fully acknowledge the highly variable attention spans across children. A child's inability to maintain attention significantly reduces their ability to attend to and benefit from the recast. If the child is not fully attending to the recast, they are much less likely to be able to successfully compare their own utterance with the adult's model provided during the recast. As a result, inattention during the recast will reduce the effectiveness of the treatment dose (the recast) and in turn, should affect the child's ability to learn the targeted morphology. In the present study, the clinician facilitated attention at the time of the recast, first by maintaining eye contact and then by using an auditory cue just prior to the recast or a tactile or visual cue during the recast. Depending on the child, these included touching the child's arm or lightly touching the underside of their chin (tactile cues), touching the clinician's own chin (visual cue), or calling the child's name (auditory cue). To the greatest extent possible, this ensured the child was attending to the clinician at the time the recast was administered. As treatment progressed, S1 and S2 adapted to the format of the treatment and learned to anticipate recasts, and eventually directly attended to the clinician without these cues. Of note, due to S3's reduced attention, the clinician consistently made multiple efforts to obtain his attention prior to each recast throughout the course of treatment. This could have been an additional factor affecting his performance.
As previously described, S3 was the poorest responder to treatment. Although each child with cochlear implants presents differently, this child presented with a hearing and communication profile that varied in potentially significant ways from the other two participants. This child was implanted later than the other two children, presented with lower thresholds (mild hearing loss), and had a diagnosis of auditory neuropathy spectrum disorder. The etiology, type, and degree of his hearing loss were likely the primary factors that affected his performance in this study. However, he had the capacity to hear the difference between the allophones in the recast of the past tense form, but he had difficulty differentially applying them. During the last 13 sessions, his progress was relatively steady in the treatment sessions. However, his performance on generalization probes was highly variable. Highly variable performance was consistent with parent and clinician reports of his functioning in other contexts. His mother reported days when he had difficulty comprehending single words and other days when he was listening and correctly responding at high rates.
Fey and colleagues (Fey, Cleave, & Long, 1997; Fey, Cleave, Long, & Hughes, 1993) assessed outcomes of recast treatment following 5 and 10 months of intervention with children with language impairment and without hearing loss. The children in their studies made greater gains in use of the grammatical target after 10 months of treatment than the children who received treatment for 5 months. In addition, Leonard, Camarata, Brown, and Camarata (2004) and Leonard et al. (2006) used conversational recast treatment for a total of 48 sessions over 3 months, and then continued to a total of 96 intervention sessions over 6 months. Children showed modest gains after 3 months but continued to improve with additional time. Consistent with these patterns, a meta-analysis of morphosyntax treatment, including but not limited to conversational recast, suggested that interventions lasting longer than 8 weeks resulted in better outcomes than those lasting less than 8 weeks (Law, Garrett, & Nye, 2004). These studies suggest that greater treatment durations are more effective. However, the present study indicated that generalization of morpheme use can be seen in less than 8 weeks. In addition, accuracy for elicited generalization probes obtained in the present study was comparable to those seen after 6 months of treatment in Leonard et al. (2006). If this finding generalizes to larger studies of children with cochlear implants, this method could prove to be a relatively efficient means of producing change in morpheme use for these children.
There is a paucity of treatment research that targets morphosyntax with cochlear implant users. This is particularly problematic considering the persistent morphosyntactic errors observed in children with cochlear implants as compared to their hearing peers. This study represents a first attempt to apply a well-documented treatment approach to children with cochlear implants. Fey and Finestack (2009) note that feasibility studies should primarily address the clinical viability of a treatment approach. The results of the present research indicate that enhanced conversational recast treatment along with auditory bombardment is a viable option for some children with cochlear implants to address morphosyntax delays. Differences in treatment response for the three participants suggest potential factors that may influence treatment response in larger groups of children. Future studies are needed to verify the influence of the child-related factors discussed here. Furthermore, the results of this study justify advancing to the early efficacy stage of treatment research for this particular form of conversational recast treatment. Early efficacy studies include more children, use greater experimental control, and further investigate the characteristics of good and poor responders to intervention. Enhanced conversational recast treatment is an easily implemented approach that shows promise for addressing the persistent morphosyntax delays in children with cochlear implants.
Acknowledgments
This work was completed as a master's thesis by the first author. It was supported in part by National Institute on Deafness and Other Communication Disorders Grant R21DC014203, awarded to the second author. We thank Mary Alt, PhD, CCC-SLP and Cassandra Faux, MS, CCC-SLP for input during the project.
Funding Statement
This work was completed as a master's thesis by the first author. It was supported in part by National Institute on Deafness and Other Communication Disorders Grant R21DC014203, awarded to the second author.
References
- Beeson P. M., & Robey R. R. (2006). Evaluating single-subject treatment research: Lessons learned from the aphasia literature. Neuropsychological Review, 16, 161–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blamey P., Sarant J., Paatsch L., Barry J., Bow C., Wales R., … Tooher R. (2001). Relationships among speech perception, production, language, hearing loss, and age in children with impaired hearing. Journal of Speech, Language, and Hearing Research, 44, 264–285. [DOI] [PubMed] [Google Scholar]
- Brennan-Jones C. G., White J., Rush R. W., & Law J. (2014). Auditory-verbal therapy for promoting spoken language development in children with permanent hearing impairments. Cochrane Database of Systematic Reviews, 3, CD010100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camarata S. M., & Nelson K. (2006). Conversational recast intervention with preschool and older children. In McCauley R. J. & Fey M. E. (Eds.), Treatment of language disorders in children (pp. 237–264). Baltimore, MD: Brookes. [Google Scholar]
- Cleave P. L., Becker S. D., Curran M. K., Owen Van Horne A. J., & Fey M. E. (2015). The efficacy of recasts in language intervention: A systematic review and meta-analysis. American Journal of Speech-Language Pathology, 24, 237–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson J. I., Stout C. E., & Eyer J. A., Tattersall P., Fonkalsrud J., & Croley K. (2003). Structured Photographic Expressive Language Test: Preschool–Second Edition. DeKalb, IL: Janelle Publications. [Google Scholar]
- Dunn L. M., & Dunn D. M. (2007). Peabody Picture Vocabulary Test–Fourth Edition. Minneapolis, MN: Pearson Educational. [Google Scholar]
- Eriks-Brophy A. (2004). Outcomes of auditory-verbal therapy: A review of the evidence and a call for action. The Volta Review, 104, 21–35. [Google Scholar]
- Ertmer D. J., Leonard J. S., & Pachuilo M. L. (2002). Communication intervention for children with cochlear implants: Two case studies. Language, Speech, and Hearing Services in Schools, 33, 205–217. [DOI] [PubMed] [Google Scholar]
- Fey M. E., Cleave P. L., & Long S. H. (1997). Two models of grammar facilitation in children with language impairments: Phase 2. Journal of Speech, Language, and Hearing Research, 40, 5–19. [DOI] [PubMed] [Google Scholar]
- Fey M. E., Cleave P. L., Long S. H., & Hughes D. L. (1993). Two approaches to the facilitation of grammar in children with language impairments: An experimental evaluation. Journal of Speech and Hearing Research, 36, 141–157. [DOI] [PubMed] [Google Scholar]
- Fey M. E., & Finestack L. (2009). Research and development in child language intervention: A five-phase model. In Schwartz R. G. (Ed.), Handbook of child language disorders (pp. 513–531.) New York, NY: Psychology Press. [Google Scholar]
- Geers A. (2004). Speech, language, and reading skills after early cochlear implantation. Archives of Otolaryngology—Head & Neck Surgery, 130, 634–638. [DOI] [PubMed] [Google Scholar]
- Goldman R., & Fristoe M. (2000). Goldman-Fristoe Test of Articulation–Second Edition. Circle Pines, MN: American Guidance Services. [Google Scholar]
- Gómez R. (2002). Variability and detection of invariant structure. Psychological Science, 13, 431–436. [DOI] [PubMed] [Google Scholar]
- Grunow H., Spaulding T., Gómez R., & Plante E. (2006). The effects of variation on learning word order rules by adults with and without language-based learning disabilities. Journal of Communication Disorders, 39, 158–170. [DOI] [PubMed] [Google Scholar]
- Hammer A., Coene M., Rooryck J., & Govaerts P. (2014). The production of Dutch finite verb morphology: A comparison between hearing-impaired CI children and specific language impaired children. Lingua, 139, 68–79. [Google Scholar]
- Hassink J., & Leonard L. (2010). Within-treatment factors as predictors of outcomes following conversational recasting. American Journal of Speech-Language Pathology, 19, 213–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogan S., Stokes J., White C., Tyszkiewicz E., & Woolgar A. (2008). An evaluation of auditory verbal therapy using the rate of early language development as an outcome measure. Deafness & Education International, 10, 143–167. [Google Scholar]
- Holt R. F., & Svirsky M. A. (2008). An exploratory look at pediatric cochlear implantation: Is earliest always best? Ear and Hearing, 29, 492–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huttenlocher J., Vasilyeva M., Cymerman E., & Levine S. (2002). Language input and child syntax. Cognitive Psychology, 45, 337–374. [DOI] [PubMed] [Google Scholar]
- Justice E. C., Swanson L. A., & Buehler V. (2008). Use of narrative-based language intervention with children who have cochlear implants. Topics in Language Disorders, 28, 149–161. [Google Scholar]
- Kamhi A. G. (2014). Improving clinical practices for children with language and learning disorders. Language, Speech, and Hearing Services in Schools, 45, 92–103. [DOI] [PubMed] [Google Scholar]
- Kirk K., Miyamoto R., Lento C., Ying E., O'Neill T., & Fears B. (2002). Effects of age at implantation in young children. Annals of Otology, Rhinology & Laryngology, 111, 69–73. [DOI] [PubMed] [Google Scholar]
- Kirk K., Miyamoto R., Ying E., Perdew A., & Zuganelis H. (2002). Cochlear implantation in young children: Effects of age at implantation and communication mode. The Volta Review, 102, 127–144. [Google Scholar]
- Law J., Garrett Z., & Nye C. (2004). The efficacy of treatment for children with developmental speech and language delay/disorder: A meta-analysis. Journal of Speech, Language, and Hearing Research, 47, 924–943. [DOI] [PubMed] [Google Scholar]
- Lederberg A. R., Miller E. M., Easterbrooks S. R., & Connor C. M. (2014). Foundations for Literacy: An early literacy intervention for deaf and hard-of-hearing children. Journal of Deaf Studies and Deaf Education, 19, 438–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard L. B., Camarata S. M., Brown B., & Camarata M. N. (2004). Tense and agreement in the speech of children with specific language impairment: Patterns of generalization through intervention. Journal of Speech, Language, and Hearing Research, 47, 1363–1379. [DOI] [PubMed] [Google Scholar]
- Leonard L. B., Camarata S. M., Pawlowska M., Brown B., & Camarata M. N. (2006). Tense and agreement morphemes in the speech of children with specific language impairment during intervention: Phase 2. Journal of Speech, Language, and Hearing Research, 49, 749–770. [DOI] [PubMed] [Google Scholar]
- McCauley R. J., & Fey M. E.. (Eds.). (2006). Treatment of language disorders in children. Baltimore, MD: Brookes. [Google Scholar]
- Meyers C. M. (2015). Investigation of treatment dose schedule for children with specific language impairment (Doctoral dissertation). Retrieved from University of Arizona Campus Repository (http://hdl.handle.net/10150/560819) [Google Scholar]
- Meyers C., Plante E., Nicholas K., Dailey N., Aguilar J., Ogilivie T., & Vance R. (June, 2014). Attention orienting or consolidation? Optimizing the use of an auditory stimulation phase for treatment of morpheme errors. Poster presented at the Symposium on Research in Child Language Disorders, Madison, WI. [Google Scholar]
- Miller J. F. (1981). Procedures for analyzing free-speech samples. In Assessing language production in children. Baltimore, MD: University Park Press. [Google Scholar]
- Murphy R. J., & Bryan A. J. (1980). Multiple-baseline and multiple-probe designs: Practical alternatives for special education assessment and evaluation. Journal of Special Education, 14, 325–335. [Google Scholar]
- Naigles L., & Hoff-Ginsberg E. (1998). Why are some verbs learned before other verbs? Effects of input frequency and structure on children's early verb use. Journal of Child Language, 25, 95–120. [DOI] [PubMed] [Google Scholar]
- Nelson K. E. (1989). Strategies for first language teaching. In Rice M. L. & Schiefelbusch R. L. (Eds.), The teachability of language (pp. 263–310). Baltimore, MD: Brookes. [Google Scholar]
- Nicholas J. G., & Geers A. E. (2007). Will they catch up? The role of age at cochlear implantation in the spoken language development of children with severe to profound hearing loss. Journal of Speech, Language, and Hearing Research, 50, 1048–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikolopoulos T., Dyar D., Archbold S., & O'Donoghue G. (2004). Development of spoken language grammar following cochlear implantation in prelingually deaf children. Archives of Otolaryngology—Head & Neck Surgery, 130, 629–633. [DOI] [PubMed] [Google Scholar]
- Niparko J., Tobey E., Thal D., Eisenberg L., Wang N., Quittner A., … CDaCI Investigative Team. (2010). Spoken language development in children following cochlear implantation. JAMA, 303, 1498–1506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peña E. D., Gutiérrez-Clellen V. F., Iglesias A., Goldstein B. A., & Bedore L. M. (2014). Bilingual English-Spanish Assessment. San Rafael, CA: AR-Clinical Publications. [Google Scholar]
- Plante E., Ogilvie T., Vance R., Aguilar J. M., Dailey N. S., Meyers C., … Burton R. (2014). Variability in the language input to children enhances learning in a treatment context. American Journal of Speech-Language Pathology, 23, 530–545. [DOI] [PubMed] [Google Scholar]
- Rudmin F. (1983). The why and how of hearing/s/. The Volta Review, 85, 263–269. [Google Scholar]
- Svirsky M., Robbins A., Kirk K., Pisoni D., & Miyamoto R. (2000). Language development in profoundly deaf children with cochlear implants. Psychological Science, 11, 153–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobey E., Thal D., Niparko J., Eisenberg L., Quittner A., Wang N., & CDaCI Investigative Team. (2013). Influence of implantation age on school-age language performance in pediatric cochlear implant users. International Journal of Audiology, 52, 219–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomblin J., Spencer L., Flock S., Tyler R., & Gantz B. (1999). A comparison of language achievement in children with cochlear implants and children using hearing aids. Journal of Speech, Language, and Hearing Research, 42, 497–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toro J. M., Sinnett S., & Soto-Faraco S. (2005). Speech segmentation by statistical learning depends on attention. Cognition, 97, B25–B34. [DOI] [PubMed] [Google Scholar]
- Von Koss Torkildsen J., Dailey N., Aguilar J., Gómez R., & Plante E. (2013). Exemplar variability facilitates rapid learning of an otherwise unlearnable grammar by individuals with language-based learning disability. Journal of Speech, Language, and Hearing Research, 56, 618–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren S. F., Fey M. E., & Yoder P. J. (2007). Differential treatment intensity research: A missing link to creating optimally effective communication interventions. Mental Retardation and Developmental Disabilities Research Reviews, 13, 70–77. [DOI] [PubMed] [Google Scholar]
- White J., & Brennan-Jones C. G. (2014). Auditory verbal therapy: Improving the evidence-base. Deafness & Education International, 16, 125–128. [Google Scholar]
- Yoder P., Molfese D., & Gardner E. (2011). Initial mean length of utterance predicts the relative efficacy of two grammatical treatments in preschoolers with specific language impairment. Journal of Speech, Language, and Hearing Research, 54, 1170–1181. [DOI] [PMC free article] [PubMed] [Google Scholar]