Abstract
Drawing from evidence from epidemiology and exposure assessment studies and recommendations from expert practice, we describe a process to guide healthcare providers helping their patients who present with symptoms that might be associated with living in damp housing. We present the procedure in the form of a guided two-part interview. The first part has five questions that triage the patient towards a more detailed questionnaire that reflects features of housing conditions known to be reliably associated with exposures to mold and dampness contaminants. We chose the questions based upon conditions associated with moisture problems in homes across the United States and Canada. The goal is to facilitate the clinician’s effort to help patients reduce exposure to environmental triggers that elicit symptoms in order to better manage their disease.
Keywords: Home Assessment, mold, fungi, allergens, questionnaire, allergy, asthma
Introduction
In 2004 the Institute of Medicine’s Committee on Damp Indoor Spaces and Health conducted a comprehensive literature review and concluded that there was sufficient evidence of an association between damp indoor environments and persistent upper respiratory tract symptoms, namely cough, wheeze, and asthma in persons with allergic sensitization to fungi1. Subsequent epidemiologic and mechanistic studies have refined and extended these findings 2–4. For the epidemiology research discussed here, dampness has been most commonly associated with the simultaneous occurrence of three factors: visible water damage or stains, visible mold, and odors from microbial growth 2. The American Society of Heating, Refrigeration, and Air Conditioning (ASHRAE) concluded “that the presence of all three factors is therefore useful as an interim definition for a damp building”5.
The air in a clean and dry building contains spores and spore- and mycelial fragments of the fungi present in outdoor air 6, 7 as well other outdoor air contaminants 8. Fungal spores and fragments can enter the living space of a building from the outside air through intentional openings in the building envelope such as open windows and doors, as well as fresh air intakes of forced air ventilation systems on commercial buildings. Importantly, exposures to fungi in outdoor air are associated with significant impacts on asthma 9. Fungal growth inside of a building envelope tends to occur in micro-environments containing nutrients and moisture sufficient for spore germination leading to subsequent growth into colonies and eventual generation of additional spores and hyphae. This is known as colonization, and applies to actively growing colonies (i.e., fungal growth) and dormant or dead colonies (also fungal growth). The more fungal growth in a building the greater the proportion of spore-and mycelial fragments compared to intact spores in the air 10, 11.
Using a weight of evidence approach, three recent reviews considering the implementation of interventions combining elimination of moisture intrusion and removal of moldy items concluded that comprehensive remediation measures reduce fungal exposure and consequently respiratory symptoms and asthma morbidity 2, 3, 12. However, as with reviews of other environmental allergens (such as dust mites, rodents and cockroaches), none have shown that asthma development can be prevented by reducing these exposures 13–15. Nonetheless, the position that prevention or remediation of fungal growth indoors can reduce respiratory disease symptoms has been adopted by several prominent panels and health agencies 1, 4, 16, 17. This is an important public health issue in that the maximum attributable risk for asthma associated with fungi and dampness has been estimated at 20% 18, 19.
The intent of this review is to discuss fungi and dampness inside buildings and provide evidence-based questions useful to determine when home visits are warranted to assess potential fungal exposure. Ultimately the goal is to reduce exposure to fungi and fungal products from growth inside the building.
Provider-Facilitated Home Assessment
While many issues related to fungi and dampness can be managed by the patient with the guidance of a healthcare professional, there are situations where consultation with a trained indoor environment professional (IEP) is necessary. However, it is not practical or necessary for all patients to have such an assessment. Recognizing that assessments are inconvenient for the occupant, currently expensive, and may be unnecessary or inconclusive, what is needed are criteria for determining which patients and which homes would most likely benefit from a home assessment.
Since the evidence above indicates that patients who have respiratory illnesses (e.g., asthma, rhinitis) are at increased risk of developing symptoms from exposure to fungal growth and dampness, such individuals might benefit from a home assessment if increased exposure to fungal growth is suspected. Other considerations for a home assessment include the following:
Has the patient lived in the home long enough for respiratory symptoms to occur in response to indoor fungal exposure? The biologically-relevant time period for exposure to occur and lead to many types of symptoms or disease onset is not known. A history of increased symptoms following occupancy of a home would be evidence of a relevant exposure.
Is the patient likely to occupy the home for long enough to justify the assessment? If the patient plans to move to another home in the near future, an assessment might not be justified.
Does the patient have enough control of the environment to implement interventions (i.e., remediate or otherwise change the occupied space) if necessary? While it may help to understand what indoor exposures are present, such knowledge is less useful if interventions cannot be performed easily as may be the case for a rental unit or subsidized housing. However, evidence of significant exposure might encourage the landlord to perform necessary interventions or the patient to move to a different home.
Tools to determine if a home assessment is warranted for fungi and dampness
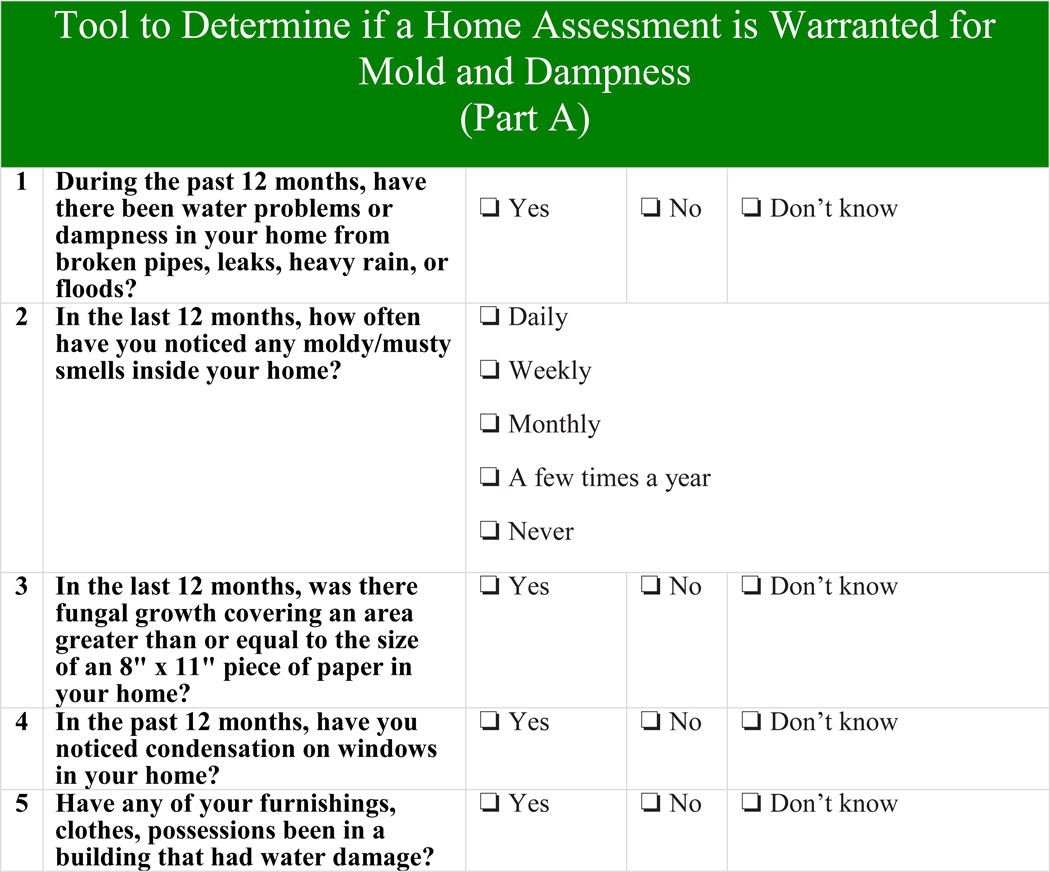
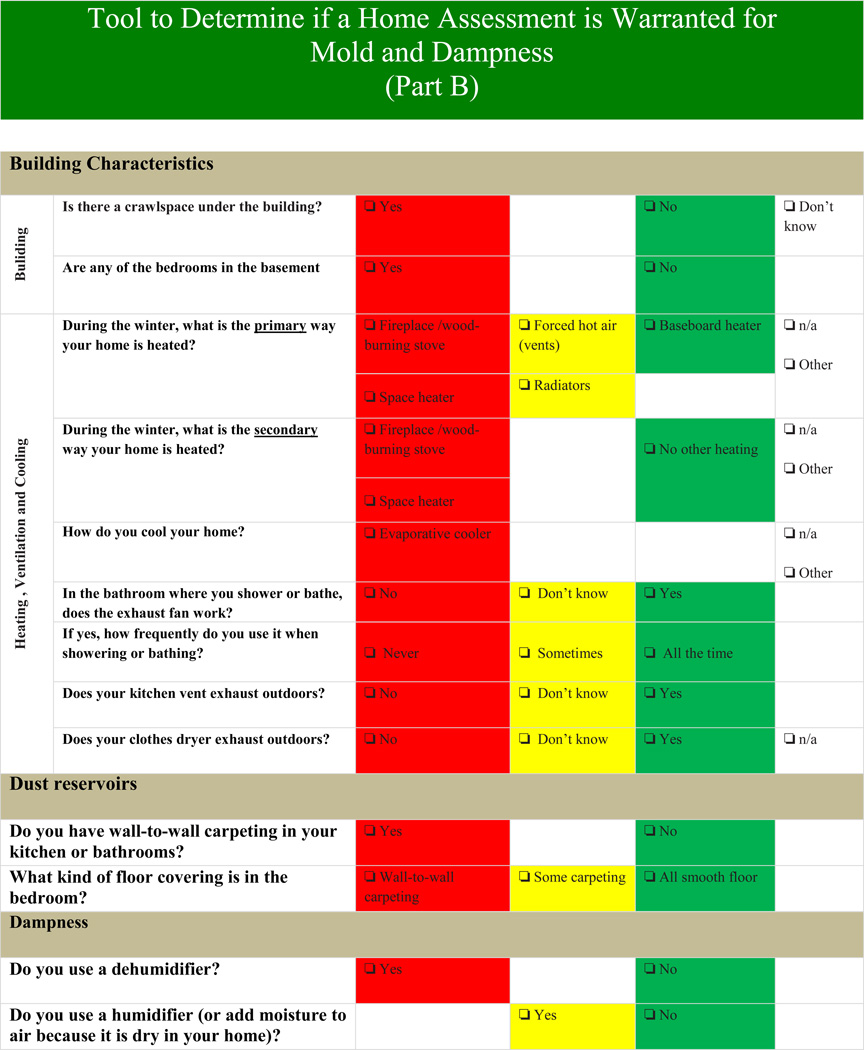
In cases where possible fungal related illness is reported, a two-step process (Part A and B described below) is recommended to decide whether or not there is justification for a building assessment focused on moisture / fungal growth issues. The first step is for clinicians to consider asking key questions to determine whether the common facilitative factors associated with environmental exposure to moisture and fungal growth may be present 20 Part A (shown in Figure 1) includes five (5) questions for the clinician (or designate) to administer to a patient with confirmed symptoms that are consistent with an increased likelihood of exposure to fungal growth. They are not specific to fungal exposure, so dust mites and other relevant allergens should also be considered 13–15. A positive reply to all five questions in Part A is sufficient indication for the need of a home assessment. However, ANY one of these indicators may justify the application of Part B (shown in Figure 2) by an allied health professional (or designate) in order to aid in the decision whether or not to recommend a home assessment for the patient. A majority of answers in the red section of Part B (i.e., first column) indicates that a home assessment might be helpful to understand potential sources of dampness and pathways of exposure to fungal growth.
Figure 1.
Key introductory questions to determine whether the mold or dampness may be present
Figure 2.
Comprehensive questions to determine whether the mold or dampness may be present
Rationale for including the five questions in Part A
The first four questions have been used in several epidemiologic studies of allergy and asthma over the years1, 3, 4, 21. However, many of the questions were often considered for proxies of other allergen exposures that can occur in damp buildings, namely those from dust mite allergens 22, 23. Therefore, in order to assess associations between dampness characteristics with fungal levels in the indoor environment, studies have incorporated one or more types of fungal measurement including culture (to identify and quantify propagules), spore counts (include viable and nonviable spores), fungal cell components (e.g., glucan, ergosterol), and molecular methods such as next generation sequencing). The fifth question is more recent and reflects increased interest in major flooding events. Furnishings (visibly moldy or otherwise) that are transported into a new home could serve as a source of biologically-relevant exposure (via spores, fungal fragments), even when a new home is relatively dry.
Each of the epidemiology and exposure assessment studies used different variations of these first four fungi/dampness questions, so we sought to find questions that were standardized and had been cognitively tested for comprehension. Therefore, we chose questions that have been used in the American Housing Survey (AHS). The U.S. Census Bureau conducts the AHS every two years in order to assess the quality of housing in the United States. AHS is a national representative survey that collects data on an average of 55,000 U.S. housing units, including apartments, single-family homes, and mobile homes. The methodology of this survey has been described in more detail elsewhere24.
When an AHS question was not available, we focused on the most commonly-used and plainly-written versions of questions that were used in peer-reviewed epidemiology and exposure assessment studies.
Here is a detailed explanation for each of those five questions
1. During the past 12 months, have there been water problems or dampness in your home from broken pipes, leaks, heavy rain, or floods?
Water damage has been associated with both high fungal concentrations in homes and with asthma symptoms. In the IOM report 1, the tables on pages 60–65 contain a comprehensive list of exposure studies that have seen associations between water damage and higher levels of fungi. In the WHO report 4, water damage was associated with asthma symptoms.
2. In the last 12 months, how often have you noticed any moldy/musty smells inside your home?
Mold odor has been associated with both fungal concentrations in homes as well as with asthma symptoms. In a prospective birth cohort study, one of the strongest associations was between mold odor and development of childhood asthma (OR = 2.44, 95% CI= 1.07-5.88) 25. In the WHO report 4 and a recent meta-analysis 3,, mold odor also was associated with development of asthma. These authors further state that water damage per se was not associated with increased risk of developing asthma because water damage itself is not the etiologic agent. Rather, water-damaged materials or furnishings (if not remediated promptly) can lead to microbial products or dust mite exposure. Mold odor is associated with increased concentrations of viable fungi 26 and of fungal glucan loadings in settled dust 27. In a more recent study, mold odor was also found to be strongly associated with total culturable fungi in air samples (OR = 3.48, 95% CI= 1.13-11.6) 28.Therefore, mold odor is a reliable sign of water damage and fungal growth that suggests a continuous source of exposure to fungal particulates.
3. In the last 12 months, was there fungal growth covering an area greater than or equal to the size of an 8" × 11" piece of paper in your home?
Visible fungal growth has been associated with both elevated fungal concentrations in homes as well as with asthma symptoms. In the WHO report 4, water damage was considered an asthma trigger and a recent meta-analysis 3 considered visible fungal growth as an agent in the causal pathway (of fungal-related agents) to asthma development.
4. In the past 12 months, have you noticed condensation on windows in your home?
Not as many studies have used resident-reported condensation on windows as a proxy for fungal exposure or fungi-related asthma symptoms. An early Danish study found that fungal levels in house dust samples were strongly associated with “window vapor” 29. Because of the small sample size (n=57 homes), the association did not reach statistical significance (OR=3.1, 95%CI = 0.9-10.8). In a meta-analysis of birth cohort studies 21, the exact wording of a condensation question was provided in an online supplemental table, “In your child’s bedroom, during the winter months, does condensation ever form on the walls?” The Leicester study was one of the birth cohorts in the meta-analysis which found an increased risk of visible mold/dampness and childhood allergic respiratory symptoms30. Therefore, we used a combination of the questions from both the Danish study and the Leicester study to formulate our window condensation question. We speculate that residents might not be able to see water vapor condensing on hidden surfaces (e.g., behind furniture, behind paintings hanging on the indoor side of exterior walls), but they might be able to at least see the water vapor on windows. The question in the Health Canada questionnaires for housing and health studies is similar to that in the UK study noted above11, 27.
5. Have any of your furnishings, clothes, possessions been in a building that had water damage?
This last question was developed by the current authors. We have not seen it used previously; however, given studies from major flood events (e.g., Mississippi floods 1993, Hurricane Katrina 2005, and Iowa floods 2008), this question will prompt the clinician to the potential for belongings which might pose a risk to continued and/or new fungal growth 31–33. Also, removal of colonized building materials (a common part of remediation activities) can generate fungal-contaminated dust. This dust can accumulate on unprotected contents remaining in the building. Given sufficient moisture, such belongings could have visible or hidden fungal growth.
Rationale for including the questions in Part B
Part B includes additional questions for the clinician (or designate) to administer to a patient to aid in the decision of whether or not to recommend a home assessment for the patient. The selection of these questions was based upon epidemiologic studies as well as purely exposure assessment studies 21, 27, 29, 34–36. Several studies often had housing stock that was unique to their locality, so questions such as “How do you heat your home?” might be relevant for that one location but not for others.
Crawlspaces and basements
Poorly designed or maintained crawl spaces and basements can result in dampness and hidden fungal damage that affects the occupied space.
Heating, Ventilation and Cooling
The use of wood stoves or fireplaces is a risk factor for increased fungal growth for a number of reasons including excess storage of wood indoors. Like wood stoves and fireplaces, the use of a space heater overheats one room which can result in other rooms being too cool and thus increasing the risk of condensation. For homes in warmer climates, condensation can also be a problem. Without a home assessment, it is difficult to determine if air conditioning is helping to decrease humidity or adding to fungi and dampness problems. Common in some parts of the country, evaporative coolers are especially difficult to maintain properly without increasing relative humidity (RH) which can foster fungal growth.
Some occupant activities such as showering, cooking, and washing clothes can release large amounts of water into the air. Exhaust fans that are properly maintained and vent to the outdoors have the ability to quickly reduce humidity levels. If the exhaust fans are absent, do not work or do not vent outside, conditions of localized high humidity can develop and produce greater risk for condensation and fungal damage.
Dust reservoirs
Dust and lint that gathers in carpets is hygroscopic. This means that like salt or sugar they are prone to absorbing moisture in damp environments. If the relative humidity rises above 85% at floor surface level (within a few millimeters), dust can gain enough moisture to support the growth of some fungi 37. A simple and effective action to mitigate this problem is to reduce the dust burdens in carpets and soft furniture by thorough cleaning with a vacuum cleaner equipped with a HEPA filter. A study conducted in Canadian homes has shown that it might take 4-6 methodical cleanings to reduce the fine dust burden in carpeting. However, this has many benefits other than just reducing potential exposure to dust mite allergens (another indoor allergy/asthma trigger related to dampness)36.
Humidification and Dehumidification
When most residents use a dehumidifier, this is clearly an indication that the home has a dampness problem. The use of a dehumidifier shows positive corrective steps by the resident. Even so, a home assessment may still be warranted to identify the source of the moisture and determine whether or not the dehumidifier is sufficient (i.e., proper size and maintenance) for controlling moisture in the structure or if other steps may be needed to mitigate any potential fungal growth problem (e.g., hidden fungal damage in wall cavities) that occurred before use of the dehumidifier. Conversely, using a humidifier to add moisture to the air indicates that the home is perceived as dry. Nonetheless, humidifiers add moisture that can condense at cold surfaces and they result in the aerosolization of bacteria and fungi if not properly cleaned and maintained.
The Home Assessment Process
Once it is determined that a home assessment is required, a good working relationship between the healthcare provider and the IEP is important. The IEP should be careful not to comment on health effects from potential mold exposures, yet should be able to convey the “health” of the home to the healthcare provider in a clear manner. Likewise, the clinician might not be able to grade the “health” of the home unless the clinician understands construction, moisture behavior in building materials and the complexities of sampling and analysis for surface or airborne fungal materials. Similar to the activity of administering the home assessment tool (Part A and B), an actual home assessment might need repetition. A good assessment report will drive any remediation activities (if necessary) and can also provide insight for the healthcare provider to improve the management of their patients’ respiratory disease symptoms. Details of IEP selection, home assessments, and assessment reports are described in the Appendix.
Conclusions
The main objective of this manuscript was to help healthcare professionals determine when a home visit might be helpful to assess fungal exposure. The two-part tool for mold/dampness-associated home assessment determination contains many evidence-based questions which are supported by peer-reviewed literature. Given that homes are a dynamic environment, the process might need to be repeated depending upon circumstances in the home (e.g., flooding events, seasonal variation, and renovations to the home). Changing characteristics of the occupants (e.g., new pets, number of residents, changes in showering, cooking, or cleaning habits) can also affect fungi and dampness, so these should be considered by the healthcare provider too.
As homes become more complex environments, the home assessment determination tool (Part A and B) should evolve too. For now, this tool is based upon peer-reviewed literature and professional opinion of building scientists, environmental mycologists, exposure assessment scientists, environmental epidemiologists, immunologists who specialize in fungi, and physicians who specialize in asthma. However, advances in each of these fields occur every year and these advances will certainly improve our ability to recognize, evaluate, and control dampness and fungal exposure in the home in meaningful ways that will hopefully decrease the burden of respiratory disease for the occupants.
Supplementary Material
List of Abbreviations
- AHS
American Housing Survey
- ASHRAE
American Society of Heating, Refrigeration, and Air Conditioning
- CI
Confidence Interval
- HEPA
High-efficiency Particulate Arresting
- IEP
Indoor Environment Professional
- IOM
Institute of Medicine
- WHO
World Health Organization
- OR
Odds Ratio
Footnotes
Disclaimer: The findings and conclusions in this manuscript are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention (CDC).
References
- 1.IOM (Institute of Medicine) Damp Indoor Spaces and Health. Washington, D.C.: The National Academies Press; 2004. [PubMed] [Google Scholar]
- 2.Mendell MJ, Mirer AG, Cheung K, Tong M, Douwes J. Respiratory and allergic health effects of dampness, mold, and dampness-related agents: a review of the epidemiologic evidence. Environ Health Perspect. 2011;119:748–756. doi: 10.1289/ehp.1002410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Quansah R, Jaakkola MS, Hugg TT, Heikkinen SA, Jaakkola JJ. Residential dampness and molds and the risk of developing asthma: a systematic review and meta-analysis. PLoS One. 2012;7:e47526. doi: 10.1371/journal.pone.0047526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO (World Health Organization) WHO guidelines for indoor air quality: Dampness and mould. Copenhagen: World Health Organization; 2009. [PubMed] [Google Scholar]
- 5.ASHRAE (American Society of Heating Refrigeration, and Air Conditioning) Limiting Indoor Mold and Dampness in Buildings Position Document. Atlanta: 2012. [Google Scholar]
- 6.Burge HA, Pierson DL, Groves TO, Strawn KF, Mishra SK. Dynamics of airborne fungal populations in a large office building. Curr Microbiol. 2000;40:10–16. doi: 10.1007/s002849910003. [DOI] [PubMed] [Google Scholar]
- 7.Li D-W, Kendrick B. Indoor aeromycota in relation to residential characteristics and allergic symptoms. Mycopathologia. 1995;131:149–157. doi: 10.1007/BF01102894. [DOI] [PubMed] [Google Scholar]
- 8.Miller JD, Dugandzic R, Frescura AM, Salares V. Indoor- and outdoor-derived contaminants in urban and rural homes in Ottawa, Ontario, Canada. J Air Waste Manag Assoc. 2007;57:297–302. doi: 10.1080/10473289.2007.10465337. [DOI] [PubMed] [Google Scholar]
- 9.Horner WE, Helbling A, Salvaggio JE, Lehrer SB. Fungal allergens. Clin. Microbiol. Rev. 1995;8:161–179. doi: 10.1128/cmr.8.2.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adhikari A, Reponen T, Rylander R. Airborne fungal cell fragments in homes in relation to total fungal biomass. Indoor Air. 2013;23:142–147. doi: 10.1111/j.1600-0668.2012.00799.x. [DOI] [PubMed] [Google Scholar]
- 11.Foto M, Vrijmoed LL, Miller JD, Ruest K, Lawton M, Dales RE. A comparison of airborne ergosterol, glucan and Air-O-Cell data in relation to physical assessments of mold damage and some other parameters. Indoor Air. 2005;15:257–266. doi: 10.1111/j.1600-0668.2005.00370.x. [DOI] [PubMed] [Google Scholar]
- 12.Sauni R, Uitti J, Jauhiainen M, Kreiss K, Sigsgaard T, Verbeek JH. Remediating buildings damaged by dampness and mould for preventing or reducing respiratory tract symptoms, infections and asthma. Cochrane Database Syst Rev. 2011:CD007897. doi: 10.1002/14651858.CD007897.pub2. [DOI] [PubMed] [Google Scholar]
- 13.Phipatanakul W, Matsui E, Portnoy J, Williams PB, Barnes C, Kennedy K, et al. Environmental assessment and exposure reduction of rodents: a practice parameter. Ann Allergy Asthma Immunol. 2012;109:375–387. doi: 10.1016/j.anai.2012.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Portnoy J, Chew GL, Phipatanakul W, Williams PB, Grimes C, Kennedy K, et al. Environmental assessment and exposure reduction of cockroaches: a practice parameter. J Allergy Clin Immunol. 2013;132:802–808. e1–e25. doi: 10.1016/j.jaci.2013.04.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Portnoy J, Miller JD, Williams PB, Chew GL, Miller JD, Zaitoun F, et al. Environmental assessment and exposure control of dust mites: a practice parameter. Ann Allergy Asthma Immunol. 2013;111:465–507. doi: 10.1016/j.anai.2013.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Health Canada. Fungal Contamination in Public Buildings: Health Effects and Investigation Methods. Ottawa: Health Canada; 2004. [Google Scholar]
- 17.Health Canada. Residential indoor air quality guidelines: moulds. Ottawa: Health Canada; 2007. [Google Scholar]
- 18.Dekker C, Dales R, Bartlett S, Brunekreef B, Zwanenburg H. Childhood asthma and the indoor environment. Chest. 1991;100:922–926. doi: 10.1378/chest.100.4.922. [DOI] [PubMed] [Google Scholar]
- 19.Mudarri D, Fisk WJ. Public health and economic impact of dampness and mold. Indoor Air. 2007;17:226–235. doi: 10.1111/j.1600-0668.2007.00474.x. [DOI] [PubMed] [Google Scholar]
- 20.Ciaccio CE, Kennedy K, Portnoy JM. A new model for environmental assessment and exposure reduction. Curr Allergy Asthma Rep. 2012;12:650–655. doi: 10.1007/s11882-012-0297-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tischer CG, Hohmann C, Thiering E, Herbarth O, Muller A, Henderson J, et al. Meta-analysis of mould and dampness exposure on asthma and allergy in eight European birth cohorts: an ENRIECO initiative. Allergy. 2011;66:1570–1579. doi: 10.1111/j.1398-9995.2011.02712.x. [DOI] [PubMed] [Google Scholar]
- 22.Peat JK, Dickerson J, Li J. Effects of damp and mould in the home on respiratory health: a review of the literature. Allergy. 1998;53:120–128. doi: 10.1111/j.1398-9995.1998.tb03859.x. [DOI] [PubMed] [Google Scholar]
- 23.Wilson J, Dixon SL, Breysse P, Jacobs D, Adamkiewicz G, Chew GL, et al. Housing and allergens: a pooled analysis of nine US studies. Environ Res. 2010;110:189–198. doi: 10.1016/j.envres.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 24.American Housing Survey. [Accessed June 23, 2015];United States Census Bureau. 2013 http://www.census.gov/programs-surveys/ahs/
- 25.Jaakkola JJ, Hwang BF, Jaakkola N. Home dampness and molds, parental atopy, and asthma in childhood: a six-year population-based cohort study. Environ. Health Perspect. 2005;113:357–361. doi: 10.1289/ehp.7242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dales RE, Miller D, McMullen E. Indoor air quality and health: validity and determinants of reported home dampness and moulds. Int J Epidemiol. 1997;26:120–125. doi: 10.1093/ije/26.1.120. [DOI] [PubMed] [Google Scholar]
- 27.Loo CK, Foty RG, Wheeler AJ, Miller JD, Evans G, Stieb DM, et al. Do questions reflecting indoor air pollutant exposure from a questionnaire predict direct measure of exposure in owner-occupied houses? Int J Environ Res Public Health. 2010;7:3270–3297. doi: 10.3390/ijerph7083270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Crawford JA, Rosenbaum PF, Anagnost SE, Hunt A, Abraham JL. Indicators of airborne fungal concentrations in urban homes: understanding the conditions that affect indoor fungal exposures. Sci Total Environ. 2015;517:113–124. doi: 10.1016/j.scitotenv.2015.02.060. [DOI] [PubMed] [Google Scholar]
- 29.Wickman M, Gravesen S, Nordvall SL, Pershagen G, Sundell J. Indoor viable dust-bound microfungi in relation to residential characteristics, living habits, and symptoms in atopic and control children. J Allergy Clin Immunol. 1992;89:752–759. doi: 10.1016/0091-6749(92)90384-e. [DOI] [PubMed] [Google Scholar]
- 30.Kuehni CE, Brooke AM, Strippoli MP, Spycher BD, Davis A, Silverman M. Cohort profile: the Leicester respiratory cohorts. Int J Epidemiol. 2007;36:977–985. doi: 10.1093/ije/dym090. [DOI] [PubMed] [Google Scholar]
- 31.Ross MA, Curtis L, Scheff PA, Hryhorczuk DO, Ramakrishnan V, Wadden RA, et al. Association of asthma symptoms and severity with indoor bioaerosols. Allergy. 2000;55:705–711. doi: 10.1034/j.1398-9995.2000.00551.x. [DOI] [PubMed] [Google Scholar]
- 32.Chew GL, Wilson J, Rabito FA, Grimsley F, Iqbal S, Reponen T, et al. Mold and endotoxin levels in the aftermath of Hurricane Katrina: a pilot project of homes in New Orleans undergoing renovation. Environ Health Perspect. 2006;114:1883–1889. doi: 10.1289/ehp.9258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hoppe KA, Metwali N, Perry SS, Hart T, Kostle PA, Thorne PS. Assessment of airborne exposures and health in flooded homes undergoing renovation. Indoor Air. 2012;22:446–456. doi: 10.1111/j.1600-0668.2012.00785.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Airaksinen M, Pasanen P, Kurnitski J, Seppanen O. Microbial contamination of indoor air due to leakages from crawl space: a field study. Indoor Air. 2004;14:55–64. doi: 10.1046/j.1600-0668.2003.00210.x. [DOI] [PubMed] [Google Scholar]
- 35.Chew GL, Rogers C, Burge HA, Muilenberg ML, Gold DR. Dustborne and airborne fungal propagules represent a different spectrum of fungi with differing relations to home characteristics. Allergy. 2003;58:13–20. doi: 10.1034/j.1398-9995.2003.00013.x. [DOI] [PubMed] [Google Scholar]
- 36.Salares V, Hinde CA, Miller JD. Analysis of Settled Dust in Homes and Fungal Glucan in Air Particulate Collected during HEPA Vacuuming. Indoor and Built Environment. 2009;18:485–491. [Google Scholar]
- 37.Hung LL, Miller JD, Dillon HK, editors. Field Guide for the Determination of Biological Contaminants in Environmental Samples. 2nd. Fairfax, VA: American Industrial Hygiene Association; 2005. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.