Abstract
Background: Considering the role of laboratory tests as a central part of controlling health expenditure, this study intends to investigate laboratory tests overutilization in Iran to pave the way for future interventions.
Methods: Inappropriate laboratory utilization was reviewed in a cross-sectional survey through the retrospective analysis of 384 medical records at a tertiary center. To pave the way for future intervention, overutilization tests were classified into two categories, inappropriate and inefficient, and then they were analyzed. Frequency analysis was used to analysis patient’s age, gender, hospital wards, length of stay, and diagnosis as well as inappropriate test and inefficient tests.
Results: A total of 143 (1.50 %) of the tests were inefficient and was ordered due to laboratory errors including hemolysis, inefficient sampling, or absurd results. 2522 (26.40%) of the tests were inappropriate and stem from failure to meet medical/clinical appropriateness criteria.
Conclusion: Whereas, inappropriate test ordering was more frequent than inefficient tests, the initial improvement strategy should focus on physicians’ test ordering behavior through conducting proper teaching strategies, ongoing audit and educational feedback, implementing health information technology tools and employing laboratory practice guidelines (LPGs) and testing algorithms. Conducting continuous quality improvement cycle for laboratory services and training of personnel involved in blood sampling is recommended for inefficient tests.
Keywords: Health Expenditures, Laboratories, Utilization review, Hemolysis, Quality Improvement, Algorithms
Introduction
Healthcare budgets worldwide are facing increasing pressure to reduce costs while maintaining quality (1). The laboratories are often targeted as a central part of controlling health expenditure (2,3). Regardless of raising demands to lower the costs, studies indicated a 17-fold difference in the number of tests ordered by health care providers as early as 1973 (3). The inappropriate laboratory tests vary widely, ranging from 11% to 70% for general biochemistry and hematology tests, 5% to 95% for urine screens and microbiology, and 17.4% to 55% for cardiac enzymes and thyroid tests (4). In the field of immunology, number of tests performed annually represents a raising trend by 63% between 1995 and 2003. Studies indicated that pathology investigations are involved in 70%–80% of all healthcare decisions and cost the UK National Health Service (NHS), £2.5 billion (US$4 billion) per year (1,5). Under pressure of optimizing the use of scarce resources, numerous of the laboratory test perceived to be unnecessary or inappropriate; 2.9% to 56% of all laboratory tests is estimated over utilized globally (6). Approximately 30% of the outpatient laboratory tests were found to be inappropriate and ordered just for patient checkup (7). With the growing pressure of the efficient use of available resources, integral role of laboratory data in medical decision making impose additional burden to many health systems. Because 60% to 70% of the objective information on the patient’s chart is laboratory information, any hinder in reporting laboratory results would effect on patient treatment and hospital length of stay (LOS) (8). Apart from their financial cost, diagnostic tests have negative impact effectiveness of care and patient outcomes (9). Inappropriate testing contributes in increasing patient anxiety, iatrogenic anemia and patient dissatisfaction (3,8). In this climate, understanding the utilization of laboratory tests is important to address health care challenges both clinically and economically (10). Thus, to find pathology of laboratory overutilization and developing effective strategies to optimize healthcare practitioners’ diagnostic test ordering behavior has become a major concern (9). Planned interventions to reduce the demand for utilization of the tests through the Utilization Management (UM) programs and physicians change behavior seems imperative (6,10-11). This study intends to estimate proportion of laboratory tests overutilizationin Kashan – Iran to pave the way for future tailored intervention to change physicians’ test ordering behavior.
Methods
Setting
This study conducted at a tertiary center in Kashan at the central part of Iran. In 2013 this General Hospital admitted 2802 patients and its bed occupancy rate was 82%.
Test Selection
To identify the most over-utilized tests, a frequency report of laboratory tests utilization was extracted through the Laboratory-information system during a 6-month period. Related data was reviewed by the panel of six experts in small meetings and 22 tests including Fasting blood sugar (FBS), Blood urea nitrogen (BUN), Urine Analysis (Urinalysis (UA), Creatinine, Prothrombin Time (PT), Partial thromboplastin time (PTT), Sodium (Na), Potassium (K), Calcium, Blood sugar (BS), Complete blood count (CBC), alkaline phosphatase, Bilirubin, Erythrocyte Sedimentation Rate (ESR), Magnesium (Mg), Serum glutamic oxalacetic transaminase (SGOT), Serum glutamic pyruvic transaminase (SGPT), total cholesterol, low density lipoprotein-cholesterol, high density lipoprotein-cholesterol , Triglycerides, Phosphorus (P) was selected by consensus to assess the utility of laboratory tests ordered at four internal medicine inpatient wards.
Laboratory Test Utilization Review
Utilization review is defined as “Evaluation of the necessity, appropriateness, and efficiency of the use of health care services, procedures, and facilities. Utilization review can be done by a peer review group or a public agency” (12).
Whereas, utilization review (UR) activities focus on appropriateness and efficient use of health care resources, we categorized laboratory tests utilization into two domains; 1) evaluating appropriateness and necessity of laboratory tests and 2) efficient utilization of hospital resources to perform laboratory tests. A pilot study of data from 50 randomly selected medical records confirmed that Hospital physician test ordering behavior could be classified into two categories according to the UR definition:
Inappropriate testing: referred to tests which failed to meet above mentioned appropriateness criteria e.g. relevancy to the patient’s sign, and symptoms and primary diagnosis, etc.
Inefficient testing: These tests were unrelated to clinical indication and occurred when 1) the blood sample was hemolyzed, 2) the result was assumed to be under question or erroneous by physicians called “absurd results”, or 3) the sample was inefficient.
These categories assumed as overutilization of services. In inappropriateness domain we investigated if laboratory tests have met appropriateness/ medical necessity criteria. In the domain of inefficient utilization of tests, we examined the right utilization of hospital resources to perform laboratory testing free from any waste/errors. Our strategy for deciding on the mentioned two main domains will be discussed below.
Assessment of Inappropriate Laboratory Tests
Evidence revealed that definitions of appropriateness so- called "medical necessity" vary greatly. Some policies define appropriateness simply, such as "such services as are reasonably intended, in the exercise of good medical practice, for the treatment of illness or injury." Other literature indicated that the services provided considered appropriate if services rendered to a patient meet clinical indication and criteria (13). One policy provides an explicit criteria for appropriate services (medically necessary services) including: 1) Appropriate for the symptoms and diagnosis or treatment of a condition, illness or injury; 2) Provided for the diagnosis, or the direct care and treatment of the condition, illness or injury; 3) In accordance with the standards of good medical practice; 4) Not primarily for the convenience of the physician and surgeon, or the provider; 5) The most appropriate supply or level of service which can safely be provided to the member of the health plan.
According to similar studies on laboratory utilization review (14,15), a laboratory test was accepted as appropriate in current study when: 1) the test was relevant to the patient's sign, and symptoms; 2) the test was related to primary diagnosis and medical impression; 3) a repeated test was employed for monitoring treatment; 4) a test was conducted to track changes in the patient clinical status and for following interventions; 5) and the test was applied to confirm a suspected condition. Through the retrospective study, two well-trained internal medicine specialists who were blind about the research goal assessed 384 medical records to determined test utilization pattern, independently. Participating physicians never assumed as an attending physician for the treated patient and employed their own clinical reasoning based on patient demographic, history and diagnosis to justify appropriateness of each test.
Assessment of Inefficient Laboratory Tests
Efficiency is the ability to cutting down the cost of care without declining obtainable improvements in health (16). So efficiency commits to contain costs by reducing the costs of services rendered. However, no one wants to contain costs by reducing health outcomes, so seeking efficiency gains should also be seen as a means of extending coverage for the same cost. To work more efficient, hospitals need to reduce waste and duplication (17). Producing repeated services (repeated tests) serves as an operational waste and implies to the inefficient and unnecessary use of resources in delivery of health care services (18). In current study our preliminary analysis of data from 50 randomly selected medical records indicated that there are some other sorts of tests ordering behavior among physicians. This ordering behavior leads to reordering and repetition of tests. Reordered and repeated tests was unrelated to test medical necessity and occurred when 1) the blood sample was hemolyzed 2) the result was assumed to be under question or erroneous by physicians called “absurd results” and 3) the blood sample was inefficient. Repeated tests as an operational waste refer to the inefficient and unnecessary use of laboratory resources to render services called that inefficient testing in current study (close to the meaning of utilization review activities).
Overall, this tests ordering behavior stem from laboratory errors and need which necessitate quality improvement cycle. According to laboratory testing cycle there are three types of laboratory errors pre-analytic (insufficient sample, incorrect sample, hemolysis sample), analytic (absurd results, sample mix- up/ interference), and post-analytic (improper data entry, high turnaround times, reporting and analysis) (19).
Figure 1 illustrated the flowchart of decision making process about over-utilized unnecessary tests in the current study.
Fig. 1 .
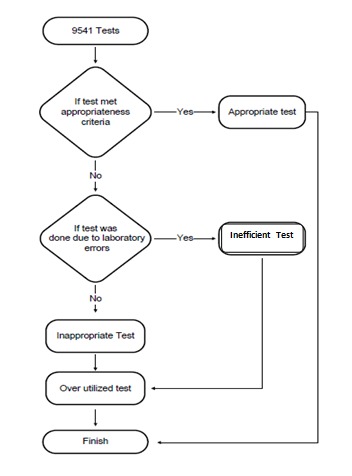
Flowchart for decision making about over utilized /unnecessary tests
Study Sampling and Data Collection
This study conducted retrospectively on 384 medical records using three checklists. Within preliminary step, medical record forms including medical history and physical examination, progress notes, consultations, operative procedures, pertinent electrocardiographic and radiographic reports, medical summary, discharge notes, physician order sheets, and all laboratories and other pathology data were reviewed to collect related information about patient condition. Test appropriateness criteria including relevance of test to sign and symptoms, medical condition, intervention and monitoring, and confirmation of suspected disease was assessed using a checklist. Test was considered appropriate if any of the appropriateness criteria was met. Further clinical and demographic information including patient age, gender, length of stay, principal diagnosis and secondary diagnosis, main medical and surgical procedures and total tests (appropriate and in appropriate) for each medical record were collected. A trained medical record practitioner reviewed each patient record and marked predefined data elements about tests’ characteristics including time of the tests, results of tests, etc and patient data including demographic data, medical history and diagnosis into the checklists.
Two trained physicians who were blind about the research goal assessed 384 medical records and filled checklist to determine test utilization pattern, independently. In this study and related literature, clinical reasoning served as a gold standard to assess test appropriateness. It means that we asked from the participating physicians, to know if they asked for the laboratory test in cases they were instead of the attending physicians of the patient considering the patient’s signs, symptoms, medical history and diagnosis documented in patient medical records. When there was inconsistency between reviewers’ opinions on overutilization of a test, the case was assessed by third senior physicians to decide about appropriateness and inappropriateness of the tests. Patients were excluded from the study if (a) they leave hospital before 48 h of admission; (b) they were admitted for follow-up care (c) their medical records suffer from inaccurate and incomplete information for evaluating the test medical necessity; and (d) if they leave hospital without physicians’ advice before completion of care episode.
Statistical Analysis of Overutilized Tests
Frequency analysis was used to analysis patient’s age, gender, hospital wards, length of stay, and diagnosis as well as inappropriate test and inefficient tests. Cross tabulation was employed to analysis cost of tests and frequency of appropriate tests based on appropriateness criteria (relevancy to sign and symptoms, diagnosis, etc) and inefficient tests. The relationship between patients’ variable and over-utilized tests was estimated using chi-square measure. Cohen's kappa coefficient calculated inter-rater agreement of two reviewers ‘opinion.
Results
Findings of the study indicated that a total of 9541 laboratory tests were ordered; 4994 (52.3%) of the tests were done for male and 4547 (47.7%) were ordered for female. Total hospital stay was 1461 days and the average patient length of stay was 3.8 days. Findings represented that 6876 (72.1%) of the tests were appropriate; 2522 (26.4 %) were inappropriate and 143 (1.5%) were inefficient (Fig. 2).
Fig. 2 .
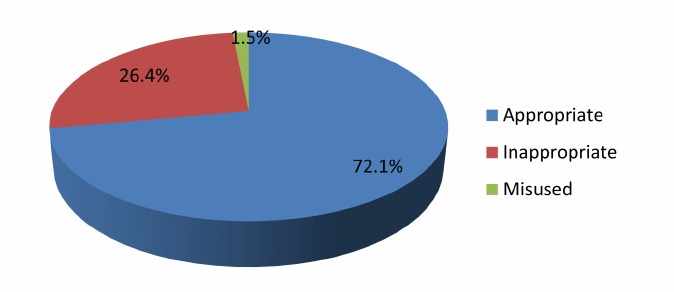
Proportion of overutilization of laboratory tests at Hospital
Table 1 indicated that absurd results accounted for the most contributing factor for inefficient tests (n=24, 0.25%) in Hospital.
Table 1. Frequency of inefficient tests in Hospital .
| Inefficient testing | N | % |
| Absurd results | 24 | 0.25 |
| Inefficient sample | 18 | 0.19 |
| Hemolysis | 101 | 1.06 |
| Total | 143 | 1.50 |
Out of 22 investigated tests, Mg (n=281, 80.7%) and Billirubin (n=109, 74.7%) presented the most inappropriate tests; BS (n=529, 97.2 %) and FBS (n=521, 95.6%) tests were reported as the most appropriate tests (Fig. 3).
Fig. 3 .
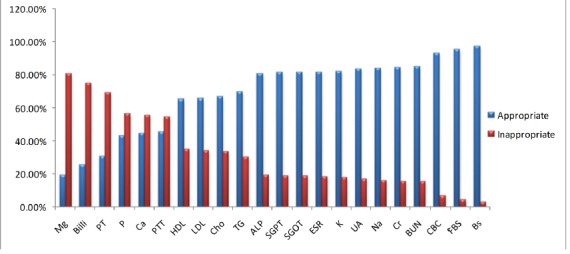
Comparisons of inappropriate and appropriate laboratory tests in Hospital
Table 2 indicated that relevancy to medical intervention was considered as the most accepted appropriateness criteria (n=5012, 52.53%) for laboratory tests according to reviewers’ judgment.
Table 2. Appropriateness criteria for laboratory tests based on reviewers’ judgment .
| Appropriateness Criteria | N | % |
| Criteria I | 23 | 0.24 |
| Criteria I & II | 11 | 0.12 |
| Criteria I & III | 6 | 0.06 |
| Criteria I & IV | 3 | 0.03 |
| Criteria II | 378 | 3.96 |
| Criteria II & III | 28 | 0.30 |
| Criteria II & IV | 197 | 2.07 |
| Criteria II & V | 2 | 0.02 |
| Criteria III | 957 | 10.05 |
| Criteria III & IV | 251 | 2.63 |
| Criteria IV | 5012 | 52.53 |
| Criteria V | 8 | 0.09 |
| Total | 6876 | 72.1 |
Criteria I: Relevance to signs and symptoms
Criteria II: Relevance to diagnosis
Criteria III: Relevance to monitoring of treatment
Criteria IV: Relevance to medical intervention
Criteria V: To confirm suspected condition
Table 3 indicated that 38210400 Rials out of 123397000 Rials laboratory test costs was inappropriate and 1881000 Rials was inefficient.
Table 3. Cost and percentage for laboratory tests utilization Review .
| Laboratory Test Utilization | Cost (Rials) | % | |
| Appropriate | 83305600 | 67.5 | |
| Inappropriate | 38210400 | 31 | |
| Inefficient testing | Absurd results | 312100 | 0.2 |
| Inefficient sample | 216600 | 0.2 | |
| Hemolysis | 1352300 | 1.1 | |
| Total | 1881000 | 1.5 | |
| Total | 123397000 | 100 |
Discussion
This study aimed to identify most contributing factors in laboratory tests’ over-utilization in Kashan. Inappropriate tests’ ordering behavior was classified into two categories, inappropriate and inefficient. The study finding indicated that 2522 (26.40 %) of the tests were inappropriate. Inappropriate testing not only would cause patient dissatisfaction, but also waste hospital resources (10). In the current study inappropriate testing accounted for nearly one third (38210400 Rials out of 123397000 Rials) of hospital laboratory costs during a 6-month period. 6876 (72.1%) of the tests were appropriate and most used criteria (n=378, 3.96%) was related to confirm a clinical diagnosis. Our findings support previous research on highlighted role of the test results in clinical decision making. Knoop believed that laboratory tests serve as supplementary information for clinical history to establish a diagnosis (20). Sandler revealed that 101 (25%) of the test results were used to establish a clinical diagnosis (14). However, laboratory services critical role is not narrowed to establish medical diagnosis. Forsman suggested that 60–70% of the most important medical decisions including admission, discharge, and medical intervention are made based on laboratory test results (21). Numerous evidence focus on the integral role of laboratory tests in disease intervention and monitoring in terms of drug dispensing, preventing adverse drug events and monitoring treatment (22-24). McDowell (2010) debated that many biochemical adverse drug reactions are found only by laboratory monitoring (25). Peter (2010) reported clinical chemistry and hematology of patient with HIV infection should be monitored by laboratory tests (22). In this area of practice, our study concluded that 5012 (52.53%) of the test results were applied for handling disease intervention. Our findings are not consistent with Sandlers’ findings (34%) (14). It seems that there is considerable variability between physician to physician practices regarding to using the tests result for medical decision making. To narrow the variation of test ordering behavior between physicians and hospitals, developing more objective and explicit criteria for appropriate use of laboratory tests is critical. In the field of laboratory, objective criteria have been emerged in the form of test algorithm and laboratory practice guideline (LPGs). The evidence has highlighted wide spreads use of laboratory guideline and its intrinsic role on laboratory inappropriate use (1,24,26-28). Moreover, implementation of LPGs can facilitate training and education of laboratory test utilization among health care professionals (29). A group of studies introduce lack of knowledge about the appropriate use of tests as a major complexity for physicians (2,5,30). Khromova claim that more than 70% of the medical students require proper education to improve their use of laboratory tests (31). Mishra debated that 98% of doctors and medical students agreed to improve their skills in interpreting laboratory investigations (32).
To improve physicians’ knowledge about use and interpretation of laboratory tests, following steps appear to be essential: 1) investigation of physicians’ learning needs and employing proper teaching strategies e.g. case based learning to inspire medical decision making based on laboratory test results (33);2) providing ongoing audit and educational feedback about tests utilization to physicians; 3) formulating more explicit and objective criteria in the forms of practice guideline and algorithm for test utilization.
In the area of the inefficient tests, finding of the study indicated that 143 (1.50%) out of 9541 of tests were inefficient due to laboratory errors. However, the amount of laboratory errors in this study was not significant; it can bring substantial financial losses to hospital and massive negative consequences for patient. Previous research indicated that cost of an “absurd” result of 0.1mg/dL serum calcium test could range from $8 to $31 per patient and $60 million per year. Furthermore, absurd results (analytical errors) can cause duplication of laboratory tests, more invasive testing (CAT scan, biopsies, etc) and increase patient length of stay. Related literature indicates that one laboratory error can reflect into 15 clinical consultations with other specialists, 77 laboratory tests, a computed tomography scan and inappropriate treatment (4,34).
Furthermore, laboratory errors can lead to a new test request and prolongs laboratory turnaround time (TAT). Long laboratory test TATs can mean a longer patient LOS and superimpose extra costs to hospital due to patient inappropriate stay and bed utilization (8,35). Therefore, investigations of potential causes of laboratory errors are critical to develop proper intervention for controlling costs of laboratory errors.
In the case of blood sample hemolysis, an increasing body of evidence demonstrates that training and continuous education of healthcare personnel with blood collection and increased use of straight needle venipuncture over catheter is effective strategy to reduce the hemolysis rates (36-39).
Limitations
Our study was limited in several ways. First, the study was conducted in retrospective approach and based on medical record. To increase the reliability of findings, two trained physicians assessed medical records, independently. The absence of real patient to investigate signs, symptoms and medical condition blurred the research findings. Second medical records suffer from poor documentation and justifying medical necessity of laboratory test is in jeopardized. To solve that, medical records with inaccurate and incomplete information were excluded from the study. Thirdly, assessment of the laboratory test utilization review was limited to 6 month. To provide more comprehensive prospective around laboratory test utilization, future study should be conducted based on ongoing audit of laboratory tests through the established utilization review committee.
Implications for Practice, Education, and Research
Controlling health expenditure due to scarce resources is a major concern for all health care systems. No previous research has highlighted the laboratory test utilization review or even rate of laboratory tests utilization in Iran. Therefore, laboratory utilization review should be conducted to determine the proportion and possible causes including improving physicians’ knowledge about use and interpretation of tests and test prices; investigation of physicians’ learning needs and employing proper teaching strategies; training healthcare personnel about blood collection and using appropriate equipment (e.g. Venipuncture); need for formulating practice guideline and algorithm for test utilization; and employing ongoing audit and educational feedback about tests utilization. Baseline data about potential causes of inappropriate testing allow establishing the necessary actions based on identified organizational problems. Therefore, it is recommended future studies focus more on targeted intervention based on an analysis of causes of inappropriateness to pave the way for improvement in health care effectiveness and efficiency.
Conclusion
We conclude that laboratory tests utilization in Kashan is poor; nearly one third of hospital laboratory tests were ordered without medical induction (inappropriate); slight numbers of laboratory tests were inefficient and produced repeated services (repeated tests) due to laboratory errors. Both inappropriate and inefficient testing imply to the waste and unnecessary use of resources in delivery of health care services. To cut costs and improve quality of services planned interventions through the Utilization Management (UM) programs and based on potential causes seems imperative. The diversity of potential causes of inappropriate testing requires a multidisciplinary team including physicians, nursing, laboratory staff, medical education, health care management and health information technology to develop more targeted strategy based on pinpoint problematic areas.
Acknowledgments
This work was supported by the Kashan University Medical Research Council (grant number: 9249).
Cite this article as: Meidani Z, Farzandipour M, Farrokhian AR, Haghighat M. A review on laboratory tests’ utilization: a trigger for cutting costs and quality improvement in health care settings. Med J Islam Repub Iran 2016 (8 May). Vol. 30:365.
References
- 1.Driskell OJ, Holland D, Hanna FW, Jones PW, Pemberton R J, Tran M. et al. Inappropriate requesting of glycatedhemoglobin (Hb A1c) is widespread: assessment of prevalence, impact of national guidance, and practice-to-practice variability. Clin Chem. 2012;58:906–15. doi: 10.1373/clinchem.2011.176487. [DOI] [PubMed] [Google Scholar]
- 2.Fryer AA, Smellie WS. Managing demand for laboratory tests: a laboratory toolkit. J ClinPathol. 2013;66:62–72. doi: 10.1136/jclinpath-2011-200524. [DOI] [PubMed] [Google Scholar]
- 3.Pageler NM, Franzon D, LonghurstCA LonghurstCA, Wood M, Shin AY, Adams ES. et al. Embedding time-limited laboratory orders within computerized provider order entry reduces laboratory utilization. PediatrCrit Care Med. 2013;14:413–19. doi: 10.1097/PCC.0b013e318272010c. [DOI] [PubMed] [Google Scholar]
- 4.Plebani M. Errors in clinical laboratories or errors in laboratory medicine? Clinical Chemical Laboratory Medicine. 2006;44:750–9. doi: 10.1515/CCLM.2006.123. [DOI] [PubMed] [Google Scholar]
- 5.Kwok J, Jones B. Unnecessary repeat requesting of tests: an audit in agovernment hospital immunology laboratory. J ClinPathol. 2005;58:457–62. doi: 10.1136/jcp.2004.021691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kiechle FL, Arcenas RC, Rogers LC. Establishing benchmarks and metrics fordisruptive technologies, inappropriate and obsolete tests in the clinical laboratory. ClinChimActa. 2014;427:131–6. doi: 10.1016/j.cca.2013.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baricchi R, Zini M, Nibali M G, Vezzosi W, Insegnante V, Manfuso C. et al. Using pathology-specific laboratory profiles in clinical pathology to reduce inappropriate test requesting: two completed audit cycles. BMC Health Serv Res. 2012;12:187. doi: 10.1186/1472-6963-12-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Holland LL, Smith LL, Blick KE. Reducing laboratory turnaround time outlierscan reduce emergency department patient length of stay: an 11-hospital study. Am J ClinPathol. 2005;124:672–4. doi: 10.1309/E9QP-VQ6G-2FBV-MJ3B. [DOI] [PubMed] [Google Scholar]
- 9.Roshanov PS, You JJ, Dhaliwal J, Koff D, Mackay JA, Weise-Kelly L. et al. Can computerized clinical decision support systems improve practitioners' diagnostic test ordering behavior? A decision-maker-researcher partnership systematic review. Implement Sci. 2011;6:88. doi: 10.1186/1748-5908-6-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Iwashyna TJ, Fuld A, Asch DA, Bellini LM. The impact of residents, interns,and attendings on inpatient laboratory ordering patterns: a report from oneuniversity's hospitalist service. Acad Med. 2011;86:139–45. doi: 10.1097/ACM.0b013e3181fd85c3. [DOI] [PubMed] [Google Scholar]
- 11.Plebani M, Zaninotto M, Faggian D. Utilization management: a Europeanperspective. ClinChimActa. 2014;427:137–41. doi: 10.1016/j.cca.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 12. Academy Health. Glossary of terms commonly used in health care. Washington; 2004. Available from:http://www.academyhealth.org/files/publications/glossary.pdf Academy Health. Glossary of terms commonly used in health care. Washington; 2004. Available from:http://www.academyhealth.org/files/publications/glossary.pdf.
- 13. Abdelhak M, Hanken MA, Grostick S, Jacobs E. Health information management: management of a strategic resources Fourth edition. London, England: Saunders WB Co; 2012.
- 14.Sandler G. Do emergency tests help in the management of acute medicaladmissions? Br Med J (Clin Res Ed) 1984;289:973–7. doi: 10.1136/bmj.289.6450.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miyakis S, Karamanof G, Liontos M, Mountokalakis TD. Factors contributing to inappropriate ordering of tests in an academic medical department and the effect of an educational feedback strategy. Postgrad Med J. 2006;82:823–9. doi: 10.1136/pgmj.2006.049551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Donabedian A. An introduction to quality assurance in health care. New York: Oxford University Press; 2002.
- 17. World Health Organization. Financing for Universal Health Coverage. World Health Report, 2010.
- 18.Bentley TG, Effros RM, Palar K, Keeler EB. Waste in the US health care system: a conceptual framework. Milbank Quarterly. 2008;86:629–59. doi: 10.1111/j.1468-0009.2008.00537.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bonini P, Plebani M, Ceriotti F, Rubboli F. Errors in laboratory medicine. Clin Chem. 2002;48:691–8. [PubMed] [Google Scholar]
- 20.Knoop FC, Owens M, Crocker IC. Clostridium difficile: clinical disease anddiagnosis. ClinMicrobiol Rev. 1993;6:251–65. doi: 10.1128/cmr.6.3.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Forsman RW. Why is the laboratory an afterthought for managed careorganizations? Clin Chem. 1996;42:813–6. [PubMed] [Google Scholar]
- 22.Peter TF, Rotz PD, Blair DH, Khine AA, Freeman RR, Murtagh MM. Impact of laboratory accreditation on patient care and the health system. Am J ClinPathol. 2010;134:550–5. doi: 10.1309/AJCPH1SKQ1HNWGHF. [DOI] [PubMed] [Google Scholar]
- 23.Fischer SH, Tjia J, Field TS. Impact of health information technology interventions to improve medication laboratory monitoring for ambulatorypatients: a systematic review. J Am Med Inform Assoc. 2010;17:631–6. doi: 10.1136/jamia.2009.000794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dufour DR, Lott JA, Nolte FS, Gretch DR, Koff RS, Seeff LB. Diagnosis andmonitoring of hepatic injury II Recommendations for use of laboratory tests in screening, diagnosis, and monitoring. Clin Chem. 2000;46:2050–68. doi: 10.1093/clinchem/46.12.2050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McDowell SE, Coleman JJ, Evans SJ, Gill PS, Ferner RE. Laboratory monitoring and adverse patient outcomes with antihypertensive therapy in primary care. Pharmacoepidemiol Drug Saf. 2010;19:482–9. doi: 10.1002/pds.1935. [DOI] [PubMed] [Google Scholar]
- 26.Sacks DB, Bruns DE, Goldstein DE, Maclaren NK, McDonald JM, Parrott M. Guidelines and Recommendations for Laboratory Analysis in the Diagnosis and Management of Diabetes Mellitus. Clinical Chemistry. 2002;48:436–72. [PubMed] [Google Scholar]
- 27.Ozbek OA, Oktem MA, Dogan G, Abacioglu YH. Application of hepatitis serology testing algorithms to assess inappropriate laboratory utilization. J EvalClinPract. 2004;10:519–23. doi: 10.1111/j.1365-2753.2003.00447.x. [DOI] [PubMed] [Google Scholar]
- 28.Pilon CS, Leathley M, London R, McLean S, Phang PT, Priestley R. et al. Practice guideline for arterial blood gas measurement in the intensive care unit decreases numbers and increases appropriateness of tests. Crit Care Med. 1997;25:1308–13. doi: 10.1097/00003246-199708000-00016. [DOI] [PubMed] [Google Scholar]
- 29.Oosterhuis WP, Bruns DE, Watine J, Sandberg S, Horvath AR. Evidence-basedguidelines in laboratory medicine: principles and methods. Clin Chem. 2004;50:806–18. doi: 10.1373/clinchem.2003.025528. [DOI] [PubMed] [Google Scholar]
- 30.Hickner J, Thompson PJ, Wilkinson T, Epner P, Sheehan M, Pollock AM. et al. Primary care physicians' challenges in ordering clinical laboratory tests and interpreting results. J Am Board Fam Med. 2014;27:268–74. doi: 10.3122/jabfm.2014.02.130104. [DOI] [PubMed] [Google Scholar]
- 31.Khromova V, Gray TA. Learning needs in clinical biochemistry for doctors infoundation years. Ann ClinBiochem. 2008;45:33–8. doi: 10.1258/acb.2007.007122. [DOI] [PubMed] [Google Scholar]
- 32.Mishra V, Kumar S, Siwach V. et al. Need for bringing in a change in biochemistry curriculum to make it clinically oriented? J Assoc Physicians India. 2000;48:635–8. [PubMed] [Google Scholar]
- 33.Sathishkumar S, Thomas N, Tharion E, Neelakantan N, Vyas R. Attitude of medical students towards Early Clinical Exposure in learning endocrine physiology. BMC Med Educ. 2007;5:30. doi: 10.1186/1472-6920-7-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Favaloro EJ, Funk DM, Lippi G. Pre-analytical Variables in Coagulation Testing Associated With Diagnostic Errors in Hemostasis. Lab Medicine. 2012;43:1–10. [Google Scholar]
- 35.Westbrook JI, Georgiou A, Lam M. Does computerized provider order entry reduce test turnaround times? A before-and-after study at four hospitals. Stud HealthTechnol Inform. 2009;150:527–31. [PubMed] [Google Scholar]
- 36.Lippi G, Bonelli P, Cervellin G. Prevalence and cost of hemolyzed samples in a large urban emergency department. Int J Lab Hematol. 2014;36:24–6. doi: 10.1111/ijlh.12135. [DOI] [PubMed] [Google Scholar]
- 37.Lippi G, Avanzini P, Cervellin G. Prevention of hemolysis in blood samplescollected from intravenous catheters. ClinBiochem. 2013;46:561–4. doi: 10.1016/j.clinbiochem.2013.01.021. [DOI] [PubMed] [Google Scholar]
- 38.Tanabe P. The effect of blood-drawing techniques and equipment on thehemolysis of ED laboratory blood samples. J EmergNurs. 2004;30:106–8. doi: 10.1016/j.jen.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 39.Lowe G, Stike R, Pollack M, Bosley J, O'Brien P, Hake A. et al. Nursing blood specimen collection techniques and hemolysis rates in an emergency department: analysis of venipuncture versus intravenous catheter collection techniques. J EmergNurs. 2008;34:26–32. doi: 10.1016/j.jen.2007.02.006. [DOI] [PubMed] [Google Scholar]


