Abstract
Background: Diagnosis of anemia is challenging in resource-poor settings due to inadequate laboratory resources. This study assessed the validity of the Tallquist haemoglobinometer in assessing anemia among pregnant women in Osogbo, Southwestern Nigeria.
Methods: This was a cross - sectional study, in which 200 pregnant women of reproductive age were selected using multistage sapling method. A checklist was used to collect socio-demographic data and the results of the screening test. Blood collection and analysis were carried out using standardized referenced methods.
Results: Mean±SD age of the respondents was 28.9+3.9 yrs.; and 62 (62.6%) had up to primary level education. When Tallquist and Haematocrit methods were compared, there was 68.4%, 83.5% and 100% likelihood of Tallquist method (TM) diagnosing severe, moderate and mild anemia, respectively. The validity indices of the TM versus Haematocrit method as the gold standard revealed the sensitivity of 97.9%, specificity of 92.1%, positive predictive value of 92.4%, and negative predictive value of 97.9% and diagnostic accuracy of 95.0%. When compared to the Haemoglobin Cyanide method, the Tallquist method showed a calculated sensitivity of 96.6%, specificity of 87.4%, positive predictive value of 86.0%, and negative predictive value of 97.0% and diagnostic accuracy of 91.5%.
Conclusion: The TM is a valid tool in screening anemia among pregnant women in resource- poor settings and rural primary health care centers in Southwestern Nigeria; therefore, its use should be encouraged, particularly to assess mild to moderate anemia.
Keywords: Anemia, Tallquist method, Validity, Pregnant women, Southwestern Nigeria
Introduction
Anemia is a common public health problem affecting over half of the pre-school children and pregnant women mostly in developing countries, with major consequences for human health, and social and economic development (1). WHO showed that anemia affected 1.62 billion people globally from 1993 to 2005, which corresponded to 24.8% of the world’s population (1).
Anemia remains one of the most intractable public health problems in malaria-endemic countries of Africa, affecting more than half of all pregnant women and children less than five years old in this region (2). A study carried out among pregnant women of rural areas of Eastern Nigeria revealed a prevalence of 59.9 % (3), similar to WHO estimates of half of pregnant women suffering from anemia (4). The requirements for a number of red blood cells sufficient to meet the body physiologic needs vary with a person’s age and gender among other factors.
A recent literature has also shown that about 20% of maternal and perinatal mortality in developing countries can be attributed to iron deficiency anemia (5). The dangerous nature of its presentation is that mild-to-moderate degrees of anemia frequently remain undetected and untreated in the community, blurring the diagnosis and causing a delay in its effective management (6). In some cases, inaccurate haemoglobin measurement has led to erroneous prescription of blood transfusion for severe anemia, unnecessarily exposing the patient to the risk of infection with Human Immunodeficiency Virus (HIV), Hepatitis and other blood-borne pathogens.
Diagnosis of anemia is challenging in resource-poor settings. Clinical diagnosis is the most common method of detecting anemia, but it is inaccurate and is even less useful in detecting non-severe anemia (1,7). Haemoglobin Colour Scales (HCS), such as the Tallquist Method, are inexpensive, simple and effective alternatives to the gold standards for assessing anemia by virtue of its validity indices being close to that of the gold standards (4,6). It is mostly used in rural and poor healthcare delivery centres where other expensive, complex methods of assessing haemoglobin are impractical due to inadequate resources (8). The majority of Nigerians live in rural areas where there is poor access and availability of efficient and affordable healthcare. Most of these rural areas are hyper-endemic to diseases like malaria, tuberculosis, and typhoid fever which are common causes of anemia in pregnancy (9). Rural primary health care centers in Nigeria lack constant electricity, clinicians and laboratory scientists and basic infrastructure for the highly technical methods of assessing anemia. This necessitates the need to implement and utilize a less technical method such as Tallquist method that may be desirable in all these areas and circumstances.
Therefore, the validity and repeatability of Tallquist method need to be determined. The aim of this study was to assess the validity of the Tallquist haemoglobinometer method in assessing anemia among pregnant women in Osogbo, Southwestern Nigeria.
Methods
Study Location
The study location was Osogbo, the capital city of Osun State, with a population of about 750,000 (10). State specific prevalence of anemia has not been yet documented. Based on the average demographic statistics in Nigeria, women of reproductive age constitute about 22% (168,000) of the population. There are three local government areas: Osogbo, Olorunda and Egbedore; and there is a teaching hospital and numerous primary health care (PHC) centers in the city
Study Design
This was a cross- sectional study among pregnant women of reproductive age (15-49 years).
Study Population
The study population included seemingly healthy pregnant women attending ante- natal clinics (ANC) in selected rural primary health care centers. Pregnant women with history of fever or malaria or those who were sick or on treatment for malaria or any febrile illnesses were excluded from the study.
Ethical Approval
The UNIOSUN Health Research Ethics Committee and the medical officers in respective LGAs approved this study. After providing ample explanations about the aim of the study, we obtained written informed consent from each participant.
Sampling Size Calculation
Using the Leslie Fischer’s formula to calculate sample size for populations greater than 10,000, (11) and considering the prevalence of anemia of 59.9% among Nigerian women, a sample size of 181 was calculated, which was increased to 200 to take care of attrition and non-response.
Sampling Procedure
A multistage sampling method was adopted. There are three LGAs in Osogbo; of which, two were selected using simple random sampling method employing simple balloting. These evolved Osogbo and Olorunda LGA. In stage 2, a list of wards per LGA designated as rural and urban by the LGA was obtained from the Community Development office of the LGA. Two rural PHCs were selected at random employing simple balloting. Questionnaires were shared among PHCs using equal allocation techniques. In Stage 3, and on every weekly ANC visit day, a list of eligible pregnant women was obtained from the head nurse. Every third woman on the list was selected using systematic sampling method. This continued until desired sample size was obtained.
Data Collection Tool
A checklist was used to collect socio-demographic data from each respondent as well as the results of both Tallquist and Haematocrit methods. Data were collected from July to December 2014.
Blood Sample Collection
About 5mls of blood sample was collected from the cubital vein of each participant, using a sterile needle and syringe employing aseptic procedure into EDTA bottle, and was stored at 4±2°c before analysis.
Basis for Sample Analysis and Estimation
Anemia was assessed using haematocrit and hemoglobin color scale methods. Mild anemia was classified as hemoglobin concentrations of 9.0 to 10.9g/dL, moderate anemia as hemoglobin concentrations of 7.0 to 8.9g/dL, and severe anemia as hemoglobin concentrations <7.0g/d (12). A mature erythrocyte is mainly a package of the molecule haemoglobin. This molecule gives the erythrocyte its oxygen carrying power. A departure from these norms, such as a deficiency, indicates that the oxygen-carrying capability is not normal. The amount of haemoglobin present in red blood cells is a good indicator of oxygen-carrying capacity of the blood. The Tallquist method of measuring haemoglobin is used to compare a small piece of Tallquist paper that has been saturated with a sample of blood with a Tallquist colour chart.
Data Analysis
Data were analyzed using the SPSS software version 17.0 after sorting out the checklists. The validity of data was ascertained through double entry and random checks. Frequency table described simple tables. Calculation of validity indices were done by a cross tab of the relevant variables to bring out ‘True Positive (TP), True Negative (TN), False Positive (FP) and False Negative (FN) results.
Results
Table 1 demonstrates that the mean±SD age of the respondents was 28.9+3.9 years, and the age group of 15-24 constituted the highest frequency. Sixty-two (62.6%) had up to primary level education, while 75 (75.8%) were in the lower socio-economic class (I and II).
Table 1. Comparison of Anemia using Tallquist, Haematocrit and Hemoglobin Cyanide Methods in Relation to Some Socio-demographic Characteristics .
| Variables | Anemia present n (%) | p | ||
|
Haematocrit method (n=99) |
Hb Cyanide method (n=86) |
Tallquist method (n=78) |
||
|
Age in years 15-24 25-34 35-44 |
41(41.4) 26(26.3) 32(32.3) |
34(39.5) 23(26.7) 29(33.8) |
38(48.7) 12(15.4) 28(35.9) |
0.090 |
|
Education level Up to primary Above primary |
62(62.6) 37(37.4) |
60(69.8) 26(30.2) |
52(66.7) 26(33.3) |
0.040 |
|
Socio-economic class by occupation Lower(I &2) Higher(3&4) |
75(75..8) 24(24.2) |
65(75..6) 21(24.4) |
60(76.9) 18(23.1) |
0.001 |
When Tallquist and Haematocrit methods were compared, there was 68.4%, 83.5% and 100% likelihood of TM diagnosing severe, moderate and mild anemia, respectively (Table 2).
Table 2. Contingency Table of Validity of the Tallquist Method (T) vs. Haematocrit (H) as the Gold Standard .
| Actual Disease state (H) | |||
| Test for disease (T) | Positive | Negative | Total |
| Anaemic | 97 (TP) | 8 (FP) | 105 |
| Non anaemic | 2 (FN) | 93(TN) | 95 |
| Total | 99 | 101 | 200 |
TP- True Positive; FP- False Positive; FN- False Negative; and TN- True Negative
Table 3 displays the contingency table of validity of the Tallquist method versus Haematocrit method as the gold standard. Validity indices for TM include sensitivity of 97.9%, specificity of 92.1%, positive predictive value of 92.4% and negative predictive value of 97.9% and diagnostic accuracy of 95.0%.
Table 3. Contingency Table of Validity of the Tallquist Method (T) vs. Hemoglobin Cyanide Method as the Gold Standard .
| Actual Disease state | |||
| Test for disease | Positive | Negative | Total |
| Anaemic | 86 (TP) | 14 (FP) | 100 |
| Non anaemic | 3(FN) | 97 (TN) | 100 |
| Total | 89 | 111 | 200 |
Comparing the Tallquist method to the Hemoglobin Cyanide method as the gold standard, it showed a calculated sensitivity of 96.6%, specificity of 87.4%, positive predictive value of 86.0% and negative predictive value of 97.0% and diagnostic accuracy of 91.5% (Table 4).
Table 4. Diagnostic Accuracy Parameters of Hematocrit, and Hemoglobin Cyanide (n = 200) .
| Group | Sensitivity | Specificity | PPV | NPV | Accuracy | LR+ | LR- | CI 95% | ||
| L | U | |||||||||
| Haematocrit (H) | 0.979 | 0.920 | 0.923 | 0.978 | 0.95 | 12.36 | 0.021 | 0.88 | 0.98 | |
| Hemoglobin Cyanide | 0.966 | 0.873 | 0.860 | 0.970 | 0.915 | 7.66 | 0.038 | 0.82 | 0.95 | |
Fig. 1 .
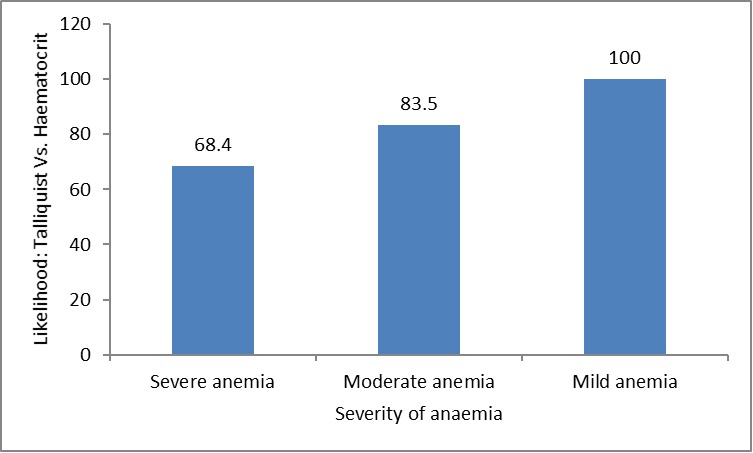
Grading of Anemia (Tallquist Method vs. Haematocrit Method as the Gold Standard)
Discussion
The lower socio-economic class, responsible for about three quarters of anemia in this study, was correlated with poverty and poor infrastructural facilities in the rural areas of Nigeria (13). In a country like Nigeria where a significant proportion of the population live on less than one US dollar per day, huge spending on health care is not unlikely, particularly among the lower socioeconomic people of Agrarian communities. Using Tallquist method in rural areas is cost effective; therefore, cost minimization, effectiveness and eventual benefits are feasible.
The appropriate technology in Tallquist method srelies on comparing the colour of a drop of blood absorbed onto a filter paper with standard colours on a laminated card, varying from pink to dark red. These colours correspond to haemoglobin levels of 4, 6, 8, 10, 12, and 14g/dl. Intermediate shades can be identified, allowing haemoglobin levels to be judged to 1g/dl.
Using the Tallquist method, anemia was diagnosed in about half and in about two-fifth of the participants. These figures were significant but lower when compared to several other studies including 76.5% in Abeokuta and 62.86% in Enugu (14). Others include prevalence rates of 61.29% and 74.46% within and around Owerri metropolis in Southeastern Nigeria (13). However, similar prevalence of anemia was diagnosed using the other two methods (Haematocrit and Haemoglobin Cyanide methods). This observation has not portrayed the TM as a less effective tool in diagnosing anemia among pregnant women when compared to other methods. These studies found that anemia is common in pregnant women and it needs to be diagnosed early to avoid complications in pregnant women or their children. It also gives an indication into seeking for the possible causes of anemia and ways of early management and prevention. Iron deficiency and nutritional anemia are examples of causes that are amenable to early treatment and primary and secondary prevention.
TM was able to diagnose all mild anemia cases and most of the moderately anaemic cases. This supports other studies that reported TM is able to detect mild and moderate anemia, which is likely to be missed by clinical diagnosis alone (7,8). However, because Tallquist method is divided into increments, it may be less accurate in measuring severe anemia than other methods of measuring haemoglobin such as the Haemoglobin Cyanide (HCN) and HemoCue methods, which measure haemoglobin levels to the nearest 0.1g/dl (15).
Another study has also shown that Tallquist method performs better than clinical diagnosis alone in detecting mild and moderate anemia, but this advantage is reduced, as anemia becomes more severe and more clinically obvious (15). In this study, the majority of the anemia cases were either mild or moderate; thus, TM is a useful tool to uncover the majority of the anemia cases.
Tallquist method was found to be scored very high on various validity indices used in this study. This finding was in accordance with another study that described usefulness of the Tallquist method in diagnosing anemia in resource-poor settings (15). In another study assessing the Tallquist method, sensitivity for detecting anemia was high (75–97%), and specificity was generally lower (41–98%) (16). In some other studies (17-19), estimates of sensitivity and specificity from the five laboratory-based studies were all high, varying from 0.85 to 0.99 for sensitivity and from 0.91 to 1.0 for specificity.
Like other screening tests, TM method has addressed a disease of public health importance with a high magnitude of affecting a significant proportion of the population and causing mortality and morbidity. In addition, there are ways of confirming the diagnosis and effective treatments for anemia, most especially if discovered early using TM.
The higher number of false positive in TM vs. Haemoglobin Cyanide method when compared to TM vs. Haematocrit method could be supported by a meta-analytical study with a wide-ranged positive predictive index of 63.0 to 98.5% when using the Tallquist method. This also suggested the superiority of Haemoglobin cyanide method in diagnosing anemia compared to Haematocrit method. Moreover, the validity indices found in this study were lower when Tallquist was compared to Haemoglobin cyanide method than when using Haematocrit as the gold standard. The observations supported by another study (18) may require further validation by some other applied research findings to make categorical statements, though it has not been the focus of this study. These indices support the use of TM in assessment of anemia in settings where full scale laboratory resources are inadequate such as in rural areas of Southwestern Nigeria.
One limitation of this study was that diagnosis of anemia, using TM, was not based on morphology or aetiology, but on reticulocyte count. Although this may call for further studies in the future, in most settings anemia should be quantitatively assessed to determine taking the most appropriate action. However, this did not affect the outcome of this study in any significant way. Another limitation was the computation of anemia using different methods in different socio-economic classes of clients. Further studies could compare the three common ways of estimating anemia (Tallquist among, Hydrogen Cyanic method and the Haematocrit methods) among different social strata of the human population.
Conclusion
The use of the Tallquist method in assessing anemia is of high validity and diagnostic accuracy in rural PHCs where resources are poor despite the high client load. Since the majority of pregnant women in ANC were seemingly healthy, TM should be an effective method to detect mild to moderate anemia in a reliable manner comparable to other standard methods such as the Haematocrit and haemoglobin cyanide methods.
Acknowledgments
The authors wish to thank the medical officers at the primary health care facilities, as well as all pregnant women who consented into taking part in this study.
Cite this article as: Wasiu Olalekan A, Olufemi Emmanuel A. How valid is the tallquist method in screening pregnant women with anemia in poor rural settings of southwestern Nigeria?. Med J Islam Repub Iran 2016 (15 June). Vol. 30:389.
References
- 1. De Benoist B, McLean E, Egli I, Cogswell ME. Worldwide Prevalence of Anemia 1993–2005: WHO Global Database on Anemia. Geneva, Switzerland: WHO 2008.
- 2.Jane C. Reducing the burden of anemia in infants and young children in malaria-endemic countries of Africa: from evidence to action. Am J Trop Med Hyg. 2004;71(2):25–34. [PubMed] [Google Scholar]
- 3.Irwin JJ, Kirchner JT. Anemia in children. Am FamPhysician. 2001;64:1379–1386. [PubMed] [Google Scholar]
- 4.Phillips PA, Wannemuehler KA, TerKuile FO, Hawley WA, Kolczak MS, Odhacha A. Diagnostic and prescribing practices in peripheral health facilities in rural western Kenya. Am J Trop Med Hy. 2005;68(4):44–49. [PubMed] [Google Scholar]
- 5. World Health Organization. Prevention and Management of Severe Anemia in Pregnancy; Report of a technical working group. Geneva: 1994. WHL/FHE/MSM/93.3.
- 6.Idowu O, Mafiana ACF, Dapo S. Anemia in pregnancy: a survey of pregnant women in Abeokuta, Nigeria; African Health Science. 2005;5(4):295–9. doi: 10.5555/afhs.2005.5.4.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Raj KP, Maharjan MR, Pragya M, Philip WJ. Success in Delivering Interventions to Reduce Maternal Anemia in Nepal: A Case Study of the Intensification of Maternal and Neonatal Micronutrient Program 2011.
- 8.Kahn KS. Analysis of causes of maternal death: a systematic review. Lancet. 2006;367:1066–74. doi: 10.1016/S0140-6736(06)68397-9. [DOI] [PubMed] [Google Scholar]
- 9.Janz TG, Johnson RL, Rubenstein SD. "Anemia in the emergency department; evaluation and treatment”. Emergency medicine practice. 2007;11:1–15. [PubMed] [Google Scholar]
- 10.National Population Commission NPC Nigeria demographic and health survey. Calverton Maryland. NPC and ORC Macro. 2006:45–47. [Google Scholar]
- 11.Araoye MO. Research Methodology with Statistics for Health and Social Sciences Ilorin, Nigeria: Nathadex Publishers. 2004:117–120. [Google Scholar]
- 12.Northrop-Clewes CA, Thurnham DI. Biomarkers for the differentiation of anemia and their clinical usefulness. Journal of Blood Medicine. 2013:411–22. doi: 10.2147/JBM.S29212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Okwu GN, Ukoha AI. Studies on the Predisposing Factors of Iron Deficiency Anemia among Pregnant women in a Nigerian community Pakistan J. Nutri. 2008;7(1):151–158. [Google Scholar]
- 14.Ekejindu IM, Udigwe GO, Chijioke IRC. Malaria and anemia in pregnancy in Enugu, Southeast, Nigeria Afri. J Med Sci. 2006;35(1):1–3. [PubMed] [Google Scholar]
- 15.Julia C, Imelda B. Haemoglobincolour scale for anemia diagnosis where there is no laboratory: a systematic review. International Journal of Epidemiology. 2005;34:1425–1434. doi: 10.1093/ije/dyi195. [DOI] [PubMed] [Google Scholar]
- 16.Critchley J, Bates I. Haemoglobincolour scale for anemia diagnosis where there is no laboratory: a systematic review. Int J Epidemiol. 2005;34(6):1425–1434. doi: 10.1093/ije/dyi195. [DOI] [PubMed] [Google Scholar]
- 17.Ingram CF, Lewis SM. Clinical use of WHO haemoglobincolour scale: Validation and Critique. J ClinPathol. 2000;53:933–37. doi: 10.1136/jcp.53.12.933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Timan IS, Tatsumi N, Aulia D, Wangsasaputra E. Comparison of haemoglobinometry by WHO haemoglobincolour scale and copper sulphate against haemiglobincyanide reference method. Clin Lab Haematol. 2004;26:253–58. doi: 10.1111/j.1365-2257.2004.00622.x. [DOI] [PubMed] [Google Scholar]
- 19.Lewis SM, Emmanuel J. Validity of the haemoglobincolour scale in blood donor screening. Vox Sang. 2001;80:28–33. doi: 10.1046/j.1423-0410.2001.00013.x. [DOI] [PubMed] [Google Scholar]


