Abstract
Mobile devices, digital technologies, and web-based applications—known collectively as eHealth (electronic health)—could improve health care delivery for costly, chronic diseases such as schizophrenia. Pharmacologic and psychosocial therapies represent the primary treatment for individuals with schizophrenia; however, extensive resources are required to support adherence, facilitate continuity of care, and prevent relapse and its sequelae. This paper addresses the use of eHealth in the management of schizophrenia based on a roundtable discussion with a panel of experts, which included psychiatrists, a medical technology innovator, a mental health advocate, a family caregiver, a health policy maker, and a third-party payor. The expert panel discussed the uses, benefits, and limitations of emerging eHealth with the capability to integrate care and extend service accessibility, monitor patient status in real time, enhance medication adherence, and empower patients to take a more active role in managing their disease. In summary, to support this technological future, eHealth requires significant research regarding implementation, patient barriers, policy, and funding.
Key Words: Schizophrenia, eHealth, web-based applications, health information technology, mobile
There is a growing appreciation among a range of stakeholders that mobile devices, digital technologies, and web-based applications, collectively described in this paper as eHealth, offer considerable potential for improving health care. Globally, personal digital devices such as smartphones and tablets are almost ubiquitous and offer not only extensive social connectivity but also enable people to capture, monitor, and share biometric and other forms of health-related data through extensive wireless communications networks and cloud-based storage (Proudfoot, 2013). In the United States, 85% of the adult population owns a mobile phone, and nearly 46 million smartphone owners used health or fitness applications (apps) in January 2014 (Fox and Duggan, 2012; Nielsen, 2014). At the same time, the use of electronic health records (EHRs) and health information technology (HIT) has been expanding in response to federal incentives offered by the Affordable Care Act (ACA) and the 2009 Health Information Technology (HITECH) Act (Buntin et al., 2010; Centers for Medicare & Medicaid Services, 2015; Paget et al., 2014; United States Department of Health and Human Services, 2013). Similarly, industry reports note a 40% increase among health care professionals who use electronic and digital tools for patient communications, and more than 20% of physicians now use mobile technologies for remote patient monitoring (Terry, 2014).
A number of these eHealth innovations are being used to augment point-of-care medical practice and represent a significant area of opportunity in mental health management for diseases such as schizophrenia. Schizophrenia is a complex, costly, chronic disease that affects approximately 1.1% of the adult population in the US and continues to be associated with profound stigma for patients and their families (Wilson et al., 2011; Wu et al., 2005; National Institutes of Mental Health. Schizophrenia. Cited April, 2015). Pharmacologic medications and psychosocial therapies are the primary treatment modalities used to support individuals with schizophrenia and encourage recovery (Kasckow et al., 2014); however, nonadherence to treatment is high, and substantial mental health and specialist psychiatric resources are required to prevent potential relapse, rehospitalization, incarceration, suicide, homelessness, and substance abuse (Feldman et al., 2014; Millier et al., 2014; Velligan and Kamil, 2014; Velligan et al., 2013). Many patients with this condition also have extensive comorbidities that require ongoing primary-care management, yet access to such care is often fragmented (Cahoon et al., 2013) and compounded by considerable variability across states in insurance coverage (Feldman et al., 2014). Finally, the human cost of this disease is extensive. People with schizophrenia often experience deteriorating cognitive functioning before their first psychotic episode, which can impair social relationships, self-care, and independent living skills, as well as the ability to gain and hold employment or remain in school (McGurk et al., 2013). Given the extensive economic and human burden of schizophrenia, the implementation of innovative health technologies may improve patient access to care, provide remote patient monitoring, and augment behavioral therapy.
METHODS
A group of patient care team members consisting of psychiatrists, a medical technology innovator, a mental health advocate, a family caregiver, a health policy maker, and a third-party payor met in Baltimore, Maryland, on February 27th, 2015 to discuss the opportunities and challenges associated with eHealth technologies in mental health with a specific focus on schizophrenia. The panel was selected based on their expertise in management of schizophrenia, health policies, medical technologies, and/or mental health advocacy. There was no patient in attendance at the roundtable. With the exception of Alexandra Howson, all the authors attended the roundtable discussion. Johns Hopkins School of Medicine (JHU) and Med-IQ, a medical education company (the Collaborators), proposed this activity and selected these multidisciplinary expert faculty to develop this paper to discuss the use of eHealth in managing schizophrenia and address how these technologists can support quality improvement efforts and optimal health outcomes for patients with schizophrenia. A thorough search of literature was performed and, whenever possible, references were added to support the ideas from the roundtable discussion.
The initiative was supported by an educational grant from Janssen Therapeutics, Division of Janssen Products, LP. The funding source had no role in the planning and execution of the roundtable or the development of the resulting manuscript. None of the authors have any financial relationships with any commercial interests.
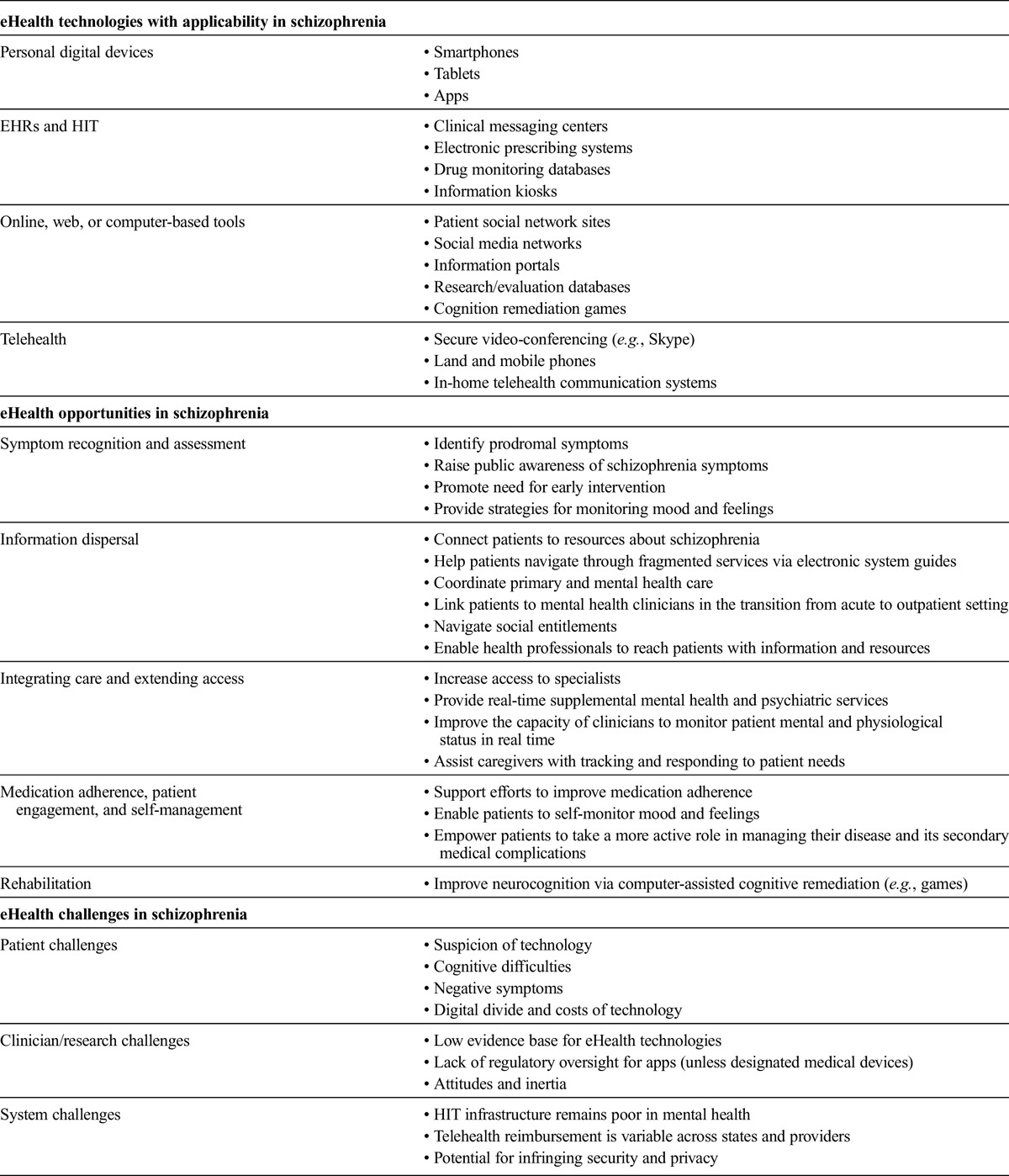
The insights presented here are drawn from the available research supporting opportunities and challenges in eHealth (Table 1), and were guided by a roundtable discussion among key stakeholders, including family members/caregivers, clinicians, and clinical researchers who manage patients with schizophrenia and/or develop innovative health care technologies.
TABLE 1.
Opportunities and Challenges With eHealth Technologies in Schizophrenia
USES, BENEFITS, AND LIMITATIONS ASSOCIATED WITH eHEALTH IN SCHIZOPHRENIA
eHealth could potentially transform health care delivery for patients with schizophrenia by enabling early symptom recognition and intervention; disseminating information at diagnosis and beyond; integrating care and extending service accessibility; and supporting medication adherence, patient engagement, self-management, and rehabilitation.
Early Symptom Recognition and Intervention
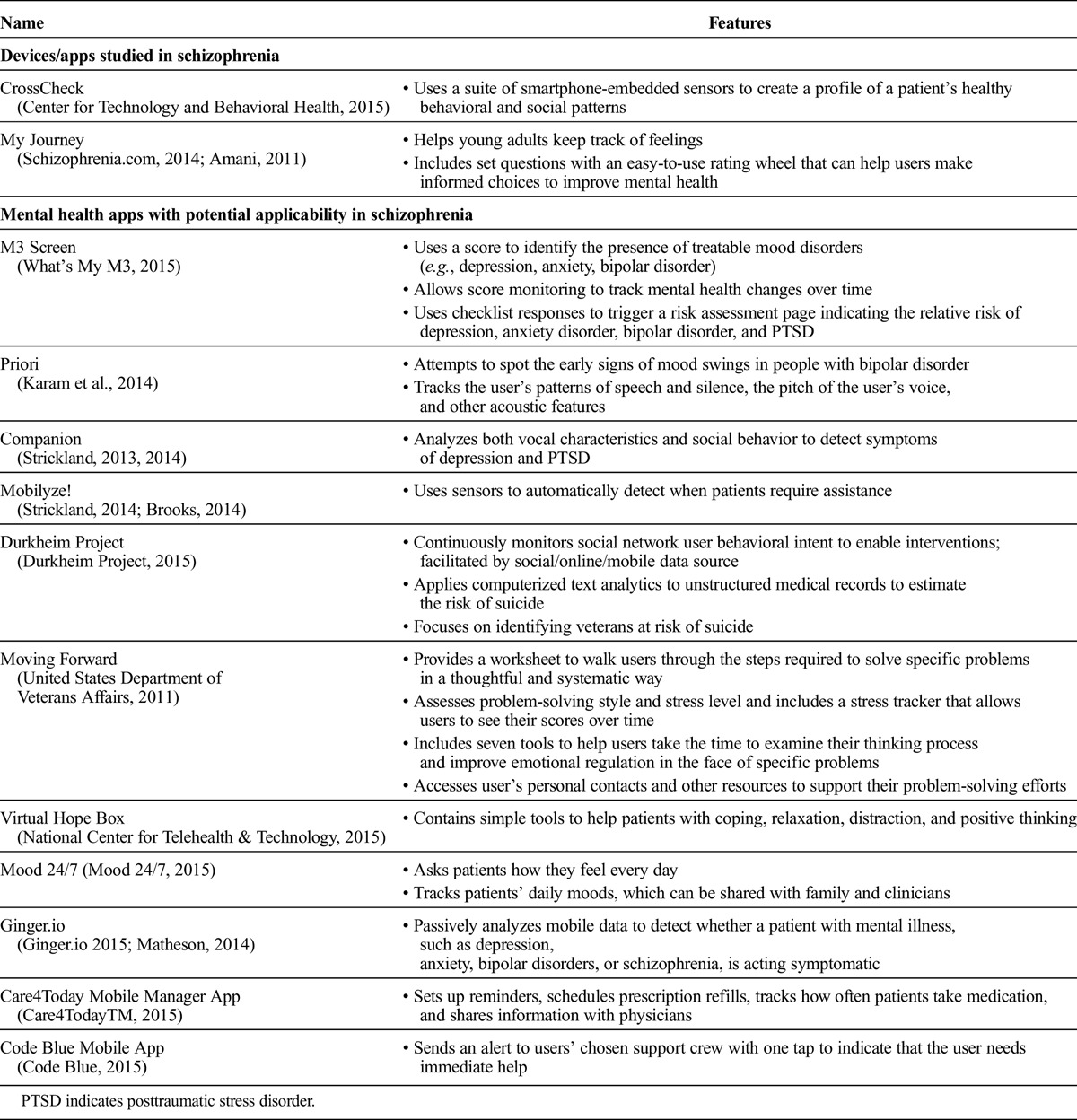
Identifying individuals at risk of schizophrenia is a crucial step toward early intervention that can prevent escalation and improve connection to care (Larson et al., 2010). Despite identifiable risk factors including family history of the disorder, age of onset (16–24 years), and prodromal changes such as social isolation and odd thinking, young adults who show early signs of schizophrenia often do not receive assessment or treatment, due in part to unfamiliarity with symptoms, concerns about stigma, and limited access to services (Gulliver et al., 2010; Robert Wood Johnson Foundation, 2013). Online social networking support (Alvarez-Jimenez et al., 2013) as well as mobile technologies and associated apps, such as My Journey (Table 2), present an untapped opportunity to raise public awareness about prodromal symptoms and promote the need for prevention and early intervention (Giota and Kleftaras, 2014; Killackey et al., 2011). Although few smartphone apps have been evaluated for schizophrenia management, Psyberguide, a non-profit mental health resource established by the One Mind Institute, reviews research and provides expert ratings for apps and online tools (http://psyberguide.org/).
TABLE 2.
Mobile Technologies in Schizophrenia and Mental Health
Online and web-based tools can engage young adults in mental health and wellness activities (especially after experiencing their first psychotic episode) by offering strategies for monitoring mood and feelings and seeking support (Giota and Kleftaras, 2014; Killackey et al., 2011). Targeted efforts in other countries to increase public awareness of mental illness via community outreach programs have been associate with a reduction in hospitalization and psychotic episode rates among young people with early symptoms (Robert Wood Johnson Foundation, 2013). For instance, Headspace is an Australian program that provides country-wide accessible, user-friendly mental health services to youth (http://headspace.org.au/). Although no comparable programs exist in the US, the Adolescent Depression Awareness Program represents an effort to educate high-school staff and students about depression, and provides an important precedent for targeted efforts to increase public awareness of mental illness (Ruble et al., 2013).
Finally, telemental health—defined here as the use of technology in the mental health field to develop and apply preventive and patient-centered measures that empower patients in the treatment of psychiatric disorders—could have a role to play in the early identification and assessment of people at risk of psychosis and in expanding access to specialists for patients who reside in underserved areas (Hilty et al., 2013).
Information Dispersal at Diagnosis and Beyond
After diagnosis, mental health services can be daunting to navigate, especially for patients living in underserved areas in which care is not always geographically accessible. The current mental health delivery system in the US is a complex web of disparate public and private clinicians and services in which the public sector predominates (Horvitz-Lennon et al., 2009). Because patients with schizophrenia are often detached from family support systems, live in suboptimal housing, have low incomes, or lead transient lives that further compound access to care (Feldman et al., 2014), many patients do not receive adequate ambulatory treatment for their disorder. This can lead to relapse, emergency department (ED) visits, and hospitalization (Feldman et al., 2014; Kasckow et al., 2014). eHealth-driven access to current, evidence-based information about mental health and primary care services could be a valuable navigation resource.
For instance, many patients with schizophrenia already use the Internet as an informal means of gathering information about treatment and peer-to-peer support (Daker-White and Rogers, 2013). Curated web-based or onsite electronic system guides (e.g., tablets or information kiosks) could provide information to patients and their families about the benefits and risks of various treatment options for schizophrenia and, thereby, prepare them to discuss and make treatment decisions with their clinicians (Ben-Zeev et al., 2013a). In addition, such technology could offer contact information to easily link patients to mental health clinicians and connect patients who are transitioning from acute care to structured outpatient programs with wrap-around services (Andrews et al., 2010; Ben-Zeev et al., 2012, 2013a, 2013b). eHealth can also help patients navigate social entitlement materials such as geographically and culturally targeted information about relevant programs and treatment facilities. Moreover, mobile phone technology, social media networks, online blogs, and patient social network sites (e.g., PatientsLikeMe, Smart Patients, Patient Fusion) can enable health care professionals to reach patients with relevant information and services (Jones et al., 2014; Paget et al., 2014).
Integrating Care and Extending Service Accessibility
Continuity of care with psychiatrists, primary care clinicians, and mental health professionals is essential in preventing potential relapse and other sequelae (Feldman et al., 2014). However, patients with schizophrenia may delay in seeking primary care services or may receive care that is inadequate, leading to avoidable hospitalizations (Li et al., 2008). Access may be impeded by patients’ inability to recognize or communicate symptoms that warrant primary care attention or by poor coordination between mental health services and primary care (Cahoon et al., 2013). In addition, although psychosocial interventions in schizophrenia can be effective, they are often underused due to barriers such as out-of-pocket costs and inaccessibility (Depp et al., 2010), which can increase patients’ risk of rehospitalization (Mental Health Quality Forum, 2014).
Health Information Technology (HIT)
HIT, including electronic health records (EHRs) and telemental health, offer the potential to improve the quality, accountability, and cost-effectiveness of health care services (Clarke and Yarborough, 2014; Hilty et al., 2013). Thus, HIT is increasingly being implemented to integrate mental health and primary care into the health home model. For instance, some collaborative care programs are using HIT to link primary and mental health services under the Medicaid health home authority (Unützer et al., 2013). Similarly, New York State recently funded the Brooklyn Health Information Exchange to improve data exchange and care coordination among patients with schizophrenia and bipolar disorder in eight hospitals by using clinical event notifications. Admission to a participating ED triggers an automated alert to the patient’s psychiatrist, who can access information through a secure “Clinical Messaging Center” and proactively check in with his or her patient while the patient is still in the ED (Galvez, 2013; Lape and Miller, 2013). In 2013, this project was serving more than 5,000 patients with schizophrenia and bipolar disorder and had generated more than 10,000 alerts.
Telehealth
Telemental health is increasingly being used to extend therapy beyond the conventional office setting and is considered an effective means of increasing access to care (Hilty et al., 2013). Real-time, secure video-conferencing; land and mobile phones; computer-based Internet tools; and in-home telehealth communication systems that link phones to additional services support virtual interactions across remote locations (Kasckow et al., 2014). Clinicians can use telehealth technology to assess, treat, and educate patients, as well as ensure faster access to psychiatric consultations. Telehealth can also support “booster” psychosocial sessions, which a recent systemic review found to have similar outcomes as standard care (Välimäki et al., 2013). A recent meta-analysis concluded that telepsychiatry can help patients feel less stigmatized and more engaged and that 90% of patients would use these services if they were available (Kasckow et al., 2014).
Telepsychiatry (i.e., telecommunications access to psychiatric specialists) seems to be effective in improving quality of care and providing discrete access to patients who fear stigmatization or have limited access to services. For instance, in rural Florida, an independent behavioral health and wellness company, ValueOptions, partnered with community mental health organization David Lawrence Center and Verizon to implement a pilot project to improve access to specialist care. The project was able to provide telepsychiatry services to Medicaid beneficiaries through easy-to-use, real-time videoconferencing. In a 14-week period in 2010, they experienced a 62% increase in care delivery to clients compared with the previous year, with a 90% patient and clinician satisfaction rate. Based on its success, the project is expanding to include telebehavioral health services as well as mobile services using 4G wireless technology (Medicaid Health Plans of America Center for Best Practices, 2012). Other programs using telecommunications technology to provide patients with schizophrenia with stable phone access and preprogrammed mental health support phone numbers have reported improvement in key Healthcare Effectiveness Data and Information Set indicators, including higher diabetes screening rates for people with schizophrenia (Miller et al., 2014). Similarly, a telepsychiatry program in rural South Carolina linked psychiatrists to patients at 21 hospital EDs in underserved areas and has increased the daily number of patients receiving psychiatric consultations, reduced the average length of stay in the ED, and reduced average mental health care costs (South Carolina Department of Mental Health, 2014). State Medicaid plans are increasingly taking advantage of coverage within the home health model for remote, telemedicine patient assessment and monitoring from an appropriate specialist for patients with a single serious and persistent mental health condition (American Telemedicine Association, 2013).
Medication Adherence
Approximately 50% of patients with schizophrenia do not take their medications as prescribed, which can lead to symptom exacerbation, relapse, and repeated hospitalization (Velligan and Kamil, 2014). Electronic prescribing systems and drug monitoring databases—such as the Maryland Chesapeake Regional Information System for our Patients database—can help clinicians monitor patient medication adherence by allowing them to view patient and clinical data alongside dispensing information (Morris et al., 2012). Other technology-supported adherence strategies include automated voice or short message service (SMS) text messages generated within and linked to EHRs (Granholm et al., 2012; Ben-Zeev et al., 2013a), electronic diaries with ringtone reminders (Velligan and Kamil, 2014; Mutschler et al., 2012), or microelectromechanical systems. For instance, the Medication Event Monitoring System uses integrated microcircuits to not only remind patients to take their prescribed medications at the correct time but also record and store the date and time a patient opens a vial. It also tracks the intake of medication by asking the patient when the drawer was opened, whether the patient took the medication, and, if not, the reason for failing to do so (Brain et al., 2014; Remington et al., 2007). Because this technology may fail in patients who are reluctant to take medications and are not forthcoming about missing doses, “smart pills” can indicate whether the pills have actually been taken.
Patient Engagement and Self-Management
Patients with schizophrenia often struggle to remain involved in managing their illness due to cognitive impairment and other problems. Mobile technology guided by ecological momentary assessment or the experience sampling method could support treatment engagement and disease self-management by enabling patients to self-monitor their clinical status and provide real-time text- or audio-based data on their thoughts, feelings, and changes in symptom severity (Swendsen et al., 2011; Palmier-Claus et al., 2012). Clinicians can use these data to suggest coping strategies for avoiding stressors, adjust antipsychotic medication, or recommend acute care when patients report symptom exacerbations or symptoms that predict relapse (Ben-Zeev et al., 2013a; Depp et al., 2010; Giota and Kleftaras, 2014; Oorschot et al., 2012). SMS texts could also direct patients to relevant services and resources for recovery, such as skills training or housing support (Fuber et al., 2014; Jones et al., 2014). Because mobile monitoring technologies lack the geographical, temporal, or spatial constraints of face-to-face clinical encounters, they may offer patients a sense of immediacy and constancy that can establish rapport with clinicians and improve engagement (Daker-White and Rogers, 2013; Kasckow et al., 2014). Mobile technologies can also strengthen the therapeutic relationship because they allow patients more control over how and when they discuss their concerns with clinicians (Ben-Zeev et al., 2013a).
Rehabilitation
Computer-assisted cognitive remediation (CACR) is increasingly being used to improve neurocognition across a variety of conditions including schizophrenia and is a growing area of research (Reddy et al., 2014). For instance, cognitive rehabilitation programs using problem-solving games can help patients with schizophrenia improve cognitive functioning and negative symptoms, such as social withdrawal, affective flattening, and motor retardation (Genevsky et al., 2010; Eack et al., 2010; Eack et al., 2013). However, these programs vary widely in their methods, intensity, duration, and relationship to other psychiatric rehabilitation programs, and little evidence is available to guide payers in determining which programs are likely to have most benefit (McGurk et al., 2013).
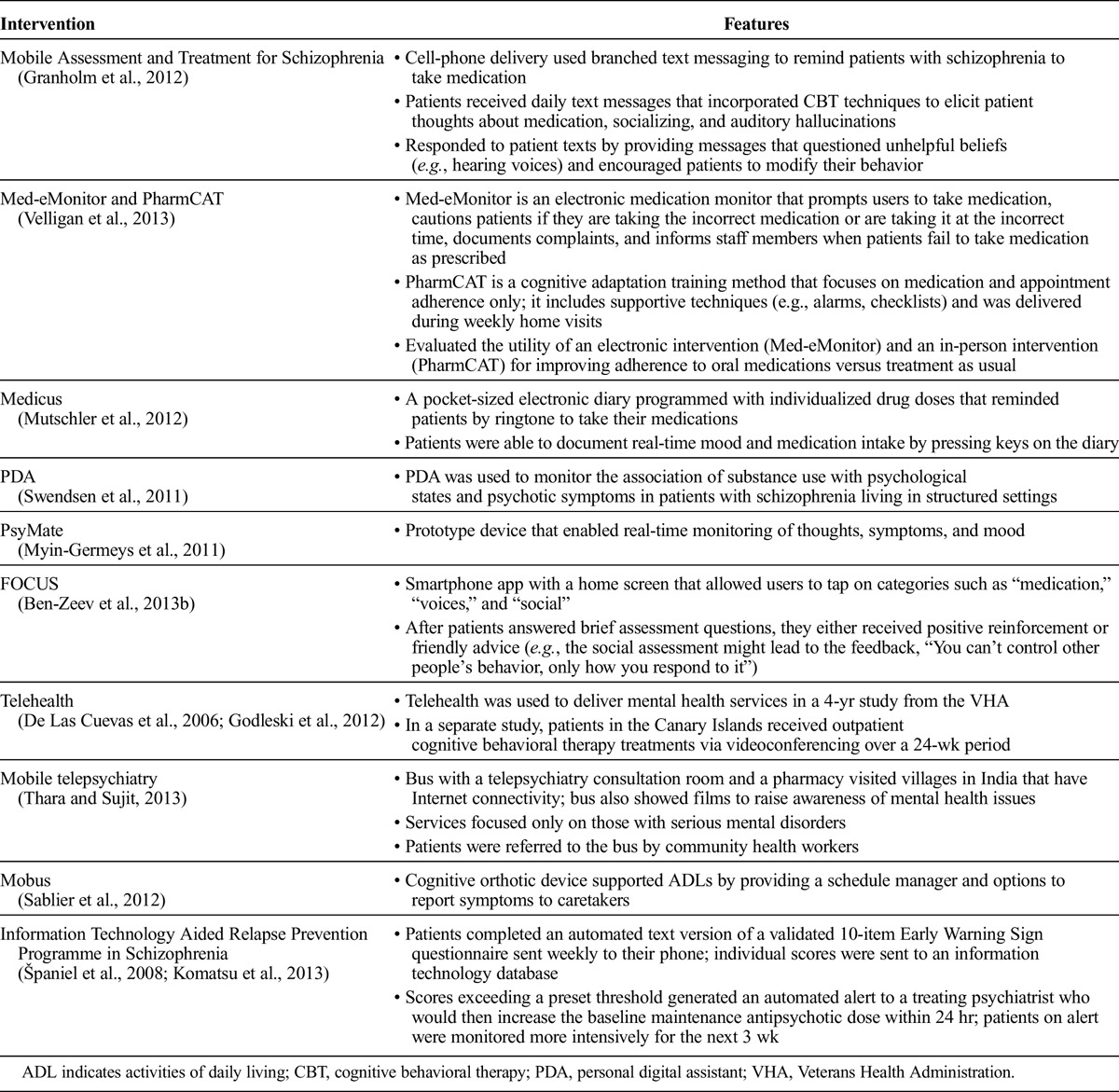
The feasibility of several eHealth interventions for supporting medication adherence and self-monitoring in schizophrenia has been evaluated or is currently under investigation (Table 3).
TABLE 3.
eHealth Interventions Under Investigation to Support Medication Adherence and Self-Monitoring in Schizophrenia
CHALLENGES IN IMPLEMENTING eHEALTH
Despite the potential uses and benefits of eHealth, many implementation challenges lie ahead, as outlined below and in Table 1.
Patient Challenges
Suspiciousness is a primary symptom of schizophrenia, and suspicion of technology (or paranoid delusions concerning it) can induce fear of computer-based devices at certain stages of psychosis (Freeman, 2008; Sendt et al., 2015). Cognitive difficulties—ranging from subtle to disabling—may require a focused intervention to familiarize the patient with new assistive technologies or simplifications/adaptations of existing ones (Young and Geyer, 2015). Research is ongoing to design self-management software for smartphone devices that incorporates user considerations, including compensatory considerations for patients with cognitive deficits (Table 2) (Ben-Zeev et al., 2013b).
Patients with schizophrenia also frequently manifest negative symptoms, including lack of energy and motivation, which can greatly derail mobile interactions if patients ignore messages, respond inconsistently, or become tired of mobile engagement (Depp et al., 2010; Foussias et al., 2015). Nonetheless, uptake of mobile technology among those with schizophrenia is growing closer to that of the general population, and interest in using such technology to monitor symptoms and connect patients to services is high (Ben-Zeev et al., 2013a).
Legitimate concerns have been expressed regarding the “digital divide” and the costs of accessing technological interventions; however, this divide may be narrowing. For instance, a 13% uptick was seen between May 2011 and February 2012 in smartphone use in rural populations (Smith, 2012). In addition, as cell phones and data plans become less expensive, the rate at which disadvantaged populations use them may continue to rise (Kurti and Dallery, 2014).
Clinician/Research Challenges
Although clinician attitudes about implementing mobile mental health technologies are not well characterized (Jones et al., 2014), some research suggests high receptivity among psychiatrists and other clinicians toward the potential benefits of telehealth in engaging patients, supporting self-monitoring, increasing access to services, and reducing costs (Daker-White and Rogers, 2013). However, with the exception of a small group of cross-sectional, noncontrolled, nonrandomized studies, most apps with potential use in schizophrenia lack an evidence base (Donker et al., 2013; Giota and Kleftaras, 2014). Currently, the US Food and Drug Administration (FDA) does not provide regulatory oversight for apps unless they are deemed to be “medical devices” (Center for Devices and Radiological Health, 2015).
The convergence of sensor, global positioning, vocal pattern, and other data associated with mobile technologies can be overwhelming to many clinicians, though the effect of such data on the therapeutic relationship is also under-researched (Clarke and Yarborough, 2014). Stakeholders must not only continue to track real-time patient-reported data but also consider designing formative research on optimal methods for distilling such data (Ben-Zeev et al., 2013b). Innovative research designs (e.g., single-case design) should be implemented to evaluate the applicability of technology-based tools at the point of care (Lillie et al., 2011).
System Challenges
HIT Infrastructure
A lack of HIT infrastructure is a key barrier to high-quality care in schizophrenia (Horvitz-Lennon et al., 2009). Indeed, many mental health professionals were ineligible to receive the EHR incentives allocated by the HITECH Act (Miller et al., 2014). It is anticipated that enacting the Behavioral Health Information Technology Act would provide financial incentives for behavioral health professionals to adopt EHR/HIT (National Council for Community Behavioral Health, 2012) and help them meet the 2014 federal requirements for Meaningful Use incentives, such as secure e-mail and a system for allowing patients to view and download electronic clinical information (Paget et al., 2014).
Telehealth Reimbursement
Although studies suggest that telehealth technologies can be cost-effective when capital expenditure costs are weighed against long-term savings (Kasckow et al., 2014), no clear reimbursement models are available for electronically delivered schizophrenia-related services (American Telemedicine Association, 2013). Although 39 states have some form of Medicaid coverage and reimbursement for mental health services provided via telemedicine, state policies for reimbursement vary in specificity and scope (American Telemedicine Association, 2013). Consequently, several organizations (e.g., Healthcare Information and Management Systems Society) are exploring innovative payment structures and policies to streamline licensure, practice standards, and e-prescribing across states. The American Medical Association has recently produced a new set of standards and safeguards intended to ensure appropriate telemedicine reimbursement, codify standards of care, and improve access to remote medical care (American Medical Association, 2014). Moreover, in January 1, 2015, the Centers for Medicare & Medicaid Services (CMS) began reimbursing previously uncovered telehealth services (United States Department of Health and Human Services, 2015). For instance, the new Chronic Care Management code reimburses clinicians for remotely managing patients with at least two chronic conditions, including conditions like schizophrenia that place patients at risk of functional decline (Centers for Medicare & Medicaid Services, 2015). The CMS reimbursement process is important because most private payers are likely to implement similar policies. Indeed, some private payers (e.g., Aetna, Cigna, United Health, and Anthem BlueCross and BlueShield) are beginning to reimburse delivery of remote behavioral health services via interactive audio, video, or data communication (Anthem BlueCross and BlueShield, 2012).
Security and Privacy Concerns
The precise real-time location and biometric data collected by mobile technology software potentially infringes on freedom of movement and may be viewed by some patients as a form of unwelcome surveillance (Daker-White and Rogers, 2013). Privacy concerns also pertain to the upload/download of personally identifiable or clinical data to mobile devices, which can be destabilized by battery or Internet connection failures (Kumar and Lee, 2012). Additionally, “eavesdropping” on communication channels raises privacy concerns as well as questions about who should use the data and to whom the data can be revealed without patient consent (Kumar and Lee, 2012). To ensure privacy and protect the confidentiality of users, the expansion and clarification of HIT—currently broadly defined—will require oversight of wireless security measures, such as cryptography and user authentication (Giota and Kleftaras, 2014; Kumar and Lee, 2012).
FUTURE APPLICATIONS AND INNOVATIONS
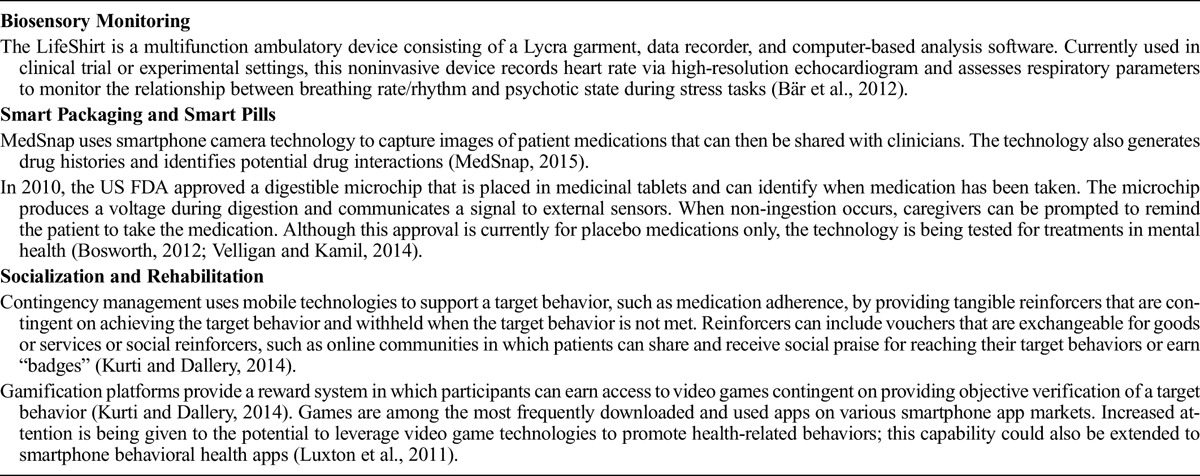
Despite these real obstacles, eHealth technologies could become support systems in schizophrenia management in a few years. For example, machine learning techniques could be implemented in smartphones to facilitate speech recognition that could accurately predict the initial stages of relapse in schizophrenia. Other instrumental ideas include providing each patient with a free cell phone, with the cost borne by payers. Such a strategy could empower patients, improve communication and access, and reduce hospitalizations. Other innovations with utility in schizophrenia are emerging, such as ambulatory biosensors to monitor mood and predict relapse, smart pills, and gamification platforms that improve cognitive function and support socialization (Table 4).
TABLE 4.
Select Examples of Emerging eHealth Innovations in Schizophrenia Management
Many of the eHealth technologies described here as potentially transformative in schizophrenia (and in mental health more generally) have been—or are currently being—evaluated in other diseases and show that the transformation of care management toward a more individualized, patient-empowered, data-driven, resource-mindful approach is on the horizon (Topol, 2012). For instance, in cardiovascular disease, recent research shows that eHealth supervision of exercise-based cardiac rehabilitation, in which heart rate data are transmitted to a programmed smartphone to support remote monitoring, is a feasible alternative for patients unable to participate in hospital-based programs and is associated with comparable rehabilitation improvements (Worringham et al., 2011). Similarly, cost-effective “snap on” or embedded mobile technology is now available to screen for and detect atrial fibrillation in community settings (Lowres et al., 2014). These technologies, as well as the technologies described in this paper, will create momentum for further research as the foundation for an evidence base in eHealth.
CONCLUSION: THE VALUE OF eHEALTH
In the US, a lack of public awareness for mental health problems, persistent stigma, and inadequate political action regarding the need for resources have led to a chronic underinvestment in mental health care (DeSilva et al., 2014). The adoption of eHealth in the context of a service delivery system that is moving toward value- and performance-based payment models represents opportunities for investment and a critical building block in the path to quality improvement, although clinical trials measuring outcomes continue to be needed (Free et al., 2013). Moreover, although data are generally lacking on the costs of implementing eHealth, the evidence presented here suggests that technology-driven schizophrenia management has the potential to achieve the goals of the ACA’s triple aim: improving population health, enhancing patient satisfaction, and reducing costs. The capacity to share patient-generated health information across clinician types and settings via remote access could help coordinate care, support self-management, and improve patient satisfaction with care, as well as reduce the cost of interventions such as ED visits or acute psychiatric hospitalization (Ben-Zeev et al., 2012, 2013a).
Despite this potential and the acceleration of eHealth use in schizophrenia by both patients and clinicians, no central agency currently exists to connect stakeholders who engage in eHealth, nor do mechanisms exist to align their interests in technology implementation. Therefore, stakeholders with the ability to bridge different worlds—academic and industry research, technology innovation, clinical practice, policy, and insurance/funding—must drive research, policy, and implementation agendas that harness technology to improve the lives of people with schizophrenia and their caregivers.
ACKNOWLEDGMENTS
The authors thank the following individuals for their assistance in the development of this manuscript: Lisa Barnhill, Manager at the Office of Continuing Medical Education, John Hopkins University School of Medicine; Laura Rafferty, Associate Managing Editor at Med-IQ; Amy Sison, Director of Continuing Medical Education at Med-IQ; and Whitney Stevens, Director, Project and Event Management at Med-IQ. Med-IQ is a full-service, accredited medical education company providing exceptional learning experiences for physicians, nurses, pharmacists, and other health care professionals.
DISCLOSURE
The initiative was supported by an unrestricted educational grant from Janssen Therapeutics, Division of Janssen Products, LP. The funding source had no role in the planning and execution of the roundtable or the development of the resulting manuscript.
The authors declare no conflict of interest.
Footnotes
The accompanying manuscript has been reviewed and approved by all of the authors listed.
REFERENCES
- Alvarez-Jimenez M, Bendall S, Lederman R, Wadley G, Chinnery G, Vargas S, Larkin M, Killackey E, McGorry PD, Gleeson JF. (2013) On the HORYZON: moderated online social therapy for long-term recovery in first episode psychosis. Schizophr Res. 143:143–149. [DOI] [PubMed] [Google Scholar]
- Amani S. (2011) “My Journey” mobile app. Department of Health Maps & Apps Competition. Cited April 2015. Available from: www.ehi.co.uk/img/Document_Library0365/My_Journey_Youth_Mental_Health_App_-_Sarah_Armani.pdf.
- American Medical Association (2014) Report 7 of the Council on Medical Service: coverage of and payment for telemedicine. Cited March 2015. Available from: http://mb.cision.com/Public/373/9600400/99c2f1db96d7fec3.pdf.
- American Telemedicine Association (2013) State Medicaid best practice telemental and behavioral health. Cited March 2015. Available from: www.americantelemed.org/docs/default-source/policy/ata-best-practice---telemental-and-behavioral-health.pdf?sfvrsn=10.
- Andrews G, Cuijpers P, Craske MG, McEvoy P, Titov N. (2010) Computer therapy for the anxiety and depressive disorders is effective, acceptable and practical health care: a meta-analysis. PLoS One. 5:e13196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anthem BlueCross and BlueShield (2012) Anthem now offering telehealth services for behavioral health. Cited March 2015. Available from: www.anthem.com/provider/in/f3/s4/t1/pw_e189873.pdf?refer=ahpprovider.
- Bär K, Rachow T, Schultz S, Bassarab K, Haufe S, Berger S, Koch K, Voss A. (2012) The phrenic component of acute schizophrenia—a name and its psychological reality. PLoS One. 7:E33459–E33459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Zeev D, Davis KE, Kaiser S, Krzsos I, Drake RE. (2013a) Mobile technologies among people with serious mental illness: opportunities for future services. Adm Policy Ment Health. 40:340–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Zeev D, Drake R, Corrigan P, Rotondi A, Nilsen W, Depp C. (2012) Using contemporary technologies in the assessment and treatment of serious mental illness. Am J Psychiatr Rehabil. 15:357–376. [Google Scholar]
- Ben-Zeev D, Kaiser SM, Brenner CJ, Begale M, Duffecy J, Mohr DC. (2013b) Development and usability testing of FOCUS: a smartphone system for self-management of schizophrenia. Psychiatr Rehabil J. 36:289–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosworth HB. (2012) How can innovative uses of technology be harnessed to improve medication adherence? Expert Rev Pharmacoecon Outcomes Res. 12:133–135. [DOI] [PubMed] [Google Scholar]
- Brain C, Sameby B, Allerby K, Lindström E, Eberhand J, Burns T, Waern M. (2014) Twelve months of electronic monitoring (MEMS®) in the Swedish COAST-study: a comparison of methods for the measurement of adherence in schizophrenia. Eur Neuropsychopharmacol. 24:215–222. [DOI] [PubMed] [Google Scholar]
- Brooks L. (2014) Mobile apps for mental health. Psychiatric Times. Cited April 2015. Available from: www.psychiatrictimes.com/telepsychiatry/mobile-apps-mental-health.
- Buntin MB, Jain SH, Blumenthal D. (2010) Health information technology: laying the infrastructure for national health reform. Health Aff (Millwood). 29:1214–1219. [DOI] [PubMed] [Google Scholar]
- Cahoon EK, McGinty EE, Ford DE, Daumit GL. (2013) Schizophrenia and potentially preventable hospitalizations in the United States: a retrospective cross-sectional study. BMC Psychiatry. 13:37 Available from: www.biomedcentral.com/1471-244X/13/37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Care4TodayTM (2015) Cited April 2015. Available from: https://mhm.care4today.com/mhm-web/select-country.do;jsessionid=delpTO7ls2+yBQ6mwx4d6TID.
- Center for Devices and Radiological Health (2015) Mobile medical applications: guidance for Industry and Food and Drug Administration staff. Cited March 2015. Available from: http://www.fda.gov/downloads/MedicalDevices/DeviceRegulationandGuidance/GuidanceDocuments/UCM263366.pdf.
- Centers for Medicare & Medicaid Services (2015) EHR incentive programs. Cited April 2015. Available from: www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/index.html?redirect=/EHRIncentivePrograms.
- Center for Technology and Behavioral Health (2015) A new paradigm for illness monitoring and relapse prevention in schizophrenia. Cited April 2015. Available from: www.c4tbh.org/the-center/what-we-re-up-to/active-projects/a-new-paradigm-for-illness-monitoring-and-relapse-prevention-in-schizophrenia.
- Clarke G, Yarborough BJ. (2014) Evaluating the promise of health IT to enhance/expand the reach of mental health services. Gen Hosp Psychiatry. 35:339–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Code Blue (2015) Cited April 2015. Available from: www.indiegogo.com/projects/code-blue.
- Daker-White G, Rogers A. (2013) What is the potential for social networks and support to enhance future telehealth interventions for people with a diagnosis of schizophrenia: a critical interpretive synthesis. BMC Psychiatry. 13:279 Available from: www.biomedcentral.com/1471-244X/13/279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Las Cuevas C, Arredondo MT, Cabrera MF, Sulzenbacher H, Meise U. (2006) Randomized clinical trial of telepsychiatry through videoconference versus face-to-face conventional psychiatric treatment. Telemed J E Health. 12:341–350. [DOI] [PubMed] [Google Scholar]
- Depp CA, Mausbach B, Granholm E, Cardenas V, Ben-Zeev D, Patterson TL, Lebowitz BD, Jeste DV. (2010) Mobile interventions for severe mental illness: design and preliminary data from three approaches. J Nerv Ment Dis. 198:715–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeSilva M, Samele C, Patel V, Darzi A. (2014) Policy actions to achieve integrated community-based mental health services. Health Aff (Millwood). 33:1595–1602. [DOI] [PubMed] [Google Scholar]
- Donker T, Petrie K, Proudfoot J, Clarke J, Birch MR, Christensen H. (2013) Smartphones for smarter delivery of mental health programs: a systematic review. J Med Internet Res. 15:e247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durkheim Project (2015) Cited April 2015. Available from: www.durkheimproject.org/our-project.
- Eack SM, Hogarty GE, Cho RY, Prasad KM, Greenwald DP, Hogarty SS, Keshavan MS. (2010) Neuroprotective effects of cognitive enhancement therapy against gray matter loss in early schizophrenia. Arch Gen Psychiatry. 67:674–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eack SM, Mesholam-Gately RI, Greenwald DP, Hogarty SS, Keshavan MS. (2013) Negative symptom improvement during cognitive rehabilitation: results from a two-year trial of cognitive enhancement therapy. Psychiatry Res. 209:21–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman R, Bailey RA, Muller J, Le J, Dirani R. (2014) Cost of schizophrenia in the Medicare program. Popul Health Manag. 17:190–196. [DOI] [PubMed] [Google Scholar]
- Foussias G, Siddiqui I, Fervaha G, Agid O, Remington G. (2015) Dissecting negative symptoms in schizophrenia: translation into new treatments. J Psychopharmacol. 29:116–126. [DOI] [PubMed] [Google Scholar]
- Fox S, Duggan M. (2012) Mobile health 2012. Pew Research Center. Cited March 2015. Available from: http://pewinternet.org/Reports/2012/Mobile-Health.aspx.
- Free C, Phillips G, Watson L, Galli L, Felix L, Edwards P, Patel V, Haines A. (2013) The effectiveness of mobile-health technologies to improve health care service delivery processes: a systematic review and meta-analysis. PLoS One. 10:e1001363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman D. (2008) Studying and treating schizophrenia using virtual reality: a new paradigm. Schizophr Bull. 34:605–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuber G, Jones GM, Healey D, Bidargaddi N. (2014) A comparison between phone-based psychotherapy with and without text messaging support in between sessions for crisis patients. J Med Internet Res. 16:e219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galvez E. (2013) HIE bright spots: supporting mental health coordination, part 3. Cited March 2015. Available from: www.healthit.gov/buzz-blog/state-hie/hie-bright-spots-supporting-mental-health-care-coordination-part-3/.
- Genevsky A, Garrett CT, Alexander PP, Vinogradov S. (2010) Cognitive training in schizophrenia: a neuroscience-based approach. Dialogues Clin Neurosci. 12:416–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginger.io (2015) Cited April 2015. Available from: https://ginger.io/.
- Giota K, Kleftaras G. (2014) Mental health apps: innovations, risks and ethical considerations. E-Health Telecommunication Systems and Networks. 3:19–23. [Google Scholar]
- Godleski L, Darkins A, Peters J. (2012) Outcomes of 98,609 U.S. Department of Veterans Affairs patients enrolled in telemental health services, 2006–2010. Psychiatr Serv. 63:383–385. [DOI] [PubMed] [Google Scholar]
- Granholm E, Ben-Zeev D, Link P, Bradshaw KR, Holden JL. (2012) Mobile Assessment and Treatment for Schizophrenia (MATS): a pilot trial of an interactive text-messaging intervention for medication adherence, socialization, and auditory hallucinations. Schizophr Bull. 38:414–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gulliver A, Griffiths KM, Christensen H. (2010) Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry. 10:113 Available from: www.biomedcentral.com/1471-244X/10/113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilty DM, Ferrer DC, Parish MB, Johnston B, Callahan EJ, Yellowlees PM. (2013) The effectiveness of telemental health. Telemed J E Health. 19:444–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horvitz-Lennon M, Donohue JM, Domino ME, Normand SL. (2009) Improving quality and diffusing best practices: the case of schizophrenia. Health Aff (Milwood). 28:701–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones SP, Patel V, Saxena S, Radcliffe N, Ali Al-Marri S, Darzi A. (2014) How Google’s ‘ten things we know to be true’ could guide the development of mental health mobile apps. Health Aff (Milwood). 33:1603–1611. [DOI] [PubMed] [Google Scholar]
- Karam ZN, Provost EM, Singh S, Montgomery J, Archer C, Harrington G, Mcinnis MG. (2014) Ecologically valid long-term mood monitoring of individuals with bipolar disorder. Available from: http://web.eecs.umich.edu/~baveja/Papers/Priori_ICASSP_final.pdf. [DOI] [PMC free article] [PubMed]
- Kasckow J, Felmet K, Appelt C, Thompson R, Rotondi A, Haas G. (2014) Telepsychiatry in the assessment and treatment of schizophrenia. Clin Schizophr Relat Psychoses. 8:21–27A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killackey E, Anda AL, Gibbs M, Alvarez-Jimenez M, Thompson A, Sun P, Baksheev GN. (2011) Using internet enabled mobile devices and social networking technologies to promote exercise as an intervention for young first episode psychosis patients. BMC Psychiatry. 11:80 Available from: www.biomedcentral.com/1471-244X/11/80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Komatsu H, Sekine Y, Okamura N, Kanahara N, Okita K, Marsubara S, Hirata T, Komiyama T, Watanabe H, Minabe Y, Iyo M. (2013) Effectiveness of information technology aided relapse prevention programme in schizophrenia excluding the effect of user adherence: a randomized controlled trial. Schizophr Res. 150:240–244. [DOI] [PubMed] [Google Scholar]
- Kumar P, Lee HJ. (2012) Security issues in healthcare applications using wireless medical sensor networks: a survey. Sensors (Basel). 12:55–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurti AN, Dallery J. (2014) Integrating technological advancements in behavioral interventions to promote health: unprecedented opportunities for behavior analysts. Rev Mex Anal Conducta. 40:106–126. [PMC free article] [PubMed] [Google Scholar]
- Lape M, Miller JE. (2013) Information technology: opportunities for care coordination. Substance Abuse and Mental Health Services Administration. Cited March 2015. Available from: www.nasmhpd.org/docs/Webinars%20ppts/SAMHSA_NASMHPD_it.pdf.
- Larson MK, Walker EF, Compton MT. (2010) Early signs, diagnosis and therapeutics of the prodromal phase of schizophrenia and related psychotic disorders. Expert Rev Neurother. 10:1347–1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Glance LG, Cai X, Mukamel DB. (2008) Mental illness and hospitalization for ambulatory care sensitive medical conditions. Med Care. 46:1249–1256. [DOI] [PubMed] [Google Scholar]
- Lillie EO, Patay B, Diamant J, Issell B, Topol EJ, Schork NJ. (2011) The n-of-1 clinical trial: the ultimate strategy for individualizing medicine? Per Med. 8:161–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowres N, Neubeck L, Salkeld G, Krass I, McLachlan AJ, Redfern J, Bennett AA, Briffa T, Bauman A, Martinez C, Wallenhorst C, Lau JK, Brieger DB, Sy RW, Freedman SB. (2014) Feasibility and cost-effectiveness of stroke prevention through community screening for atrial fibrillation using iPhone ECG in pharmacies. The SEARCH AF study. Thromb Haemost. 111:1167–1176. [DOI] [PubMed] [Google Scholar]
- Luxton DD, McCann RA, Bush NE, Mishkind MC, Reger GM. (2011) mHealth for mental health: integrating smartphone technology in behavioral healthcare. Prof Psychol Res Pract. 42:505–512. [Google Scholar]
- Matheson R. (2014) Mental-health monitoring goes mobile. MIT News. Cited April 2015. Available from: http://newsoffice.mit.edu/2014/mental-health-monitoring-goes-mobile-0716.
- McGurk SR, Mueser KT, Covell NH, Cicerone KD, Drake RE, Silverstein SM, Medialia A, Myers R, Bellack AS, Bell MD, Essock SM. (2013) Mental health system funding of cognitive enhancement interventions for schizophrenia: summary and update of the New York Office of Mental Health expert panel and stakeholder meeting. Psychiatr Rehabil J. 36:133–145. [DOI] [PubMed] [Google Scholar]
- Medicaid Health Plans of America Center for Best Practices (2012) Best practices compendium for serious mental illness. Cited March 2015. Available from: http://www.mhpa.org/_upload/SMICompendiumFINALweb_744522.pdf.
- MedSnap. Cited April 2015. Available from: https://medsnap.com/medsnap-id/.
- Mental Health Quality Forum (2014) An ecosystem approach to quality. J Clin Psych. 20:1–19. [Google Scholar]
- Miller JE, Glover RJ, Gordon SY. (2014) Crossing the behavioral health digital divide: the role of health information technology in improving care for people with behavioral health conditions in state behavioral health systems. National Association of State Mental Health Program Directors. Cited March 2015. Available from: www.nasmhpd.org/publications/HIT%20and%20BH%20Issue%20Paper%20-%20Final%20%20-%209-29-14.pdf.
- Millier A, Schmidt U, Angermeyer MC, Chauhan D, Murthy V, Toumi M, Cadi-Soussi N. (2014) Humanistic burden in schizophrenia: a literature review. J Psychiatr Res. 54:85–93. [DOI] [PubMed] [Google Scholar]
- Mood 24/7 (2015) Cited April 2015. Available from: www.mood247.com.
- Morris G, Afzal S, Finney D. (2012) Supporting prescription drug monitoring programs. Cited March 2015. Available from: www.healthit.gov/sites/default/files/pdmp_support_final.pdf.
- Mutschler J, von Zitzewitz F, Rössler W, Grosshans M. (2012) Application of electronic diaries in patients with schizophrenia and bipolar disorders. Psychiatr Danub. 24:206–210. [PubMed] [Google Scholar]
- Myin-Germeys I, Birchwood M, Kwapil T. (2011) From environment to therapy in psychosis: a real-world momentary assessment approach. Schizophr Bull. 37:244–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Telehealth & Technology. Virtual hope box. Cited April 2015. Available from: http://t2health.dcoe.mil/apps/virtual-hope-box.
- National Council for Community Behavioral Health (2012) HIT adoption and readiness for meaningful use in community behavioral health. Cited March 2015. Available from: www.thenationalcouncil.org/wp-content/uploads/2012/10/HIT-Survey-Full-Report.pdf.
- National Institutes of Mental Health. Schizophrenia. Cited April 2015. Available from: www.nimh.nih.gov/health/statistics/prevalence/schizophrenia.shtml.
- Nielsen (2014) Hacking health: how consumers use smartphones and wearable tech to track their health. Cited March 2015. Available from: www.nielsen.com/us/en/insights/news/2014/hacking-health-how-consumers-use-smartphones-and-wearable-tech-to-track-their-health.html.
- Oorschot M, Lataster T, Thewissen V, Wichers M, Myin-Germeys I. (2012) Mobile assessment in schizophrenia: a data-driven momentary approach. Schizophr Bull. 38:405–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paget L, Salzberg C, Scholle SH. (2014) Building a strategy to leverage health information technology to support patient and family engagement. National Committee for Quality Assurance. Cited March 2015. Available from: www.ncqa.org/HEDISQualityMeasurement/Research/BuildingaStrategytoLeverageHealthInformationTechnology.aspx.
- Palmier-Claus JE, Ainsworth J, Machin M, Barrowclough C, Dunn G, Barkus E, Rogers A, Wykes T, Kapur S, Buchan I, Salter E, Lewis SW. (2012) The feasibility and validity of ambulatory self-report of psychotic symptoms using a smartphone software application. BMC Psychiatry. 12:172 Available from: www.biomedcentral.com/1471-244X/12/172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proudfoot J. (2013) The future is in our hands: the role of mobile phones in the prevention and management of mental disorders. Aust N Z J Psychiatry. 47:111–113. [DOI] [PubMed] [Google Scholar]
- Reddy LF, Horan WP, Jahsan C, Green MJ. (2014) Cognitive remediation for schizophrenia: a review of recent findings. Curr Treat Options Psych. 121–133. [Google Scholar]
- Remington G, Kwon J, Collins A, Laporte D, Mann S, Christensen B. (2007) The use of electronic monitoring (MEMS) to evaluate antipsychotic compliance in outpatients with schizophrenia. Schizophr Res. 90:229–237. [DOI] [PubMed] [Google Scholar]
- Robert Wood Johnson Foundation (2013) How can early treatment of serious mental illness improve lives and save money? Cited March 2015. Available from: www.rwjf.org/healthpolicy.
- Ruble AE, Leon PJ, Gilley-Hensley L, Hess SG, Swartz KL. (2013) Depression knowledge in high school students: effectiveness of the adolescent depression awareness program. J Affect Disord. 150:1025–1030. [DOI] [PubMed] [Google Scholar]
- Sablier J, Stip E, Jacquet P, Giroux S, Pigot H, Franck N; Mobus Group (2012) Ecological assessments of activities of daily living and personal experiences with Mobus, an assistive technology for cognition: a pilot study in schizophrenia. Assist Technol. 24:67–77. [DOI] [PubMed] [Google Scholar]
- Schizophrenia.com (2014) New smartphone app may help in schizophrenia outcomes. Cited April 2015. Available from: http://schizophrenia.com/?p=151.
- Sendt KV, Tracy DK, Bhattacharyya S. (2015) A systematic review of factors influencing adherence to antipsychotic medication in schizophrenia-spectrum disorders. Psychiatry Res. 225:14–30. [DOI] [PubMed] [Google Scholar]
- Smith A. (2012) Nearly half of American adults are smartphone owners. Cited March 2012. Available from: http://www.pewinternet.org/2012/03/01/nearly-half-of-american-adults-are-smartphone-owners/.
- South Carolina Department of Mental Health (2014) The Duke telepsychiatry program. Cited March 2015. Available from: www.state.sc.us/dmh/telepsychiatry/index.htm.
- Španiel F, Vohlídka P, Hrdlička J, Kožený J, Novák T, Motlová L, Čermák J, Bednařík J, Novák D, Höschl C. (2008) ITAREPS: information technology aided relapse prevention programme in schizophrenia. Schizophr Res. 98:312–317. [DOI] [PubMed] [Google Scholar]
- Strickland E. (2013) App captures the Boston bombing’s psychological effects. IEE Spectrum. Cited April 2014. Available from: http://spectrum.ieee.org/biomedical/diagnostics/app-captures-the-boston-bombings-psychological-effects.
- Strickland E. (2014) Smartphone app keeps watch over schizophrenic patients. IEE Spectrum. Cited April 2014. Available from: http://spectrum.ieee.org/biomedical/diagnostics/smartphone-app-keeps-watch-over-schizophrenic-patients.
- Swendsen J, Ben-Zeev D, Granholm E. (2011) Real-time electronic ambulatory monitoring of substance use and symptom expression in schizophrenia. Am J Psychiatry. 168:202–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terry K. (2014) Physicians warm to digital communications with patients. Cited March 2015. Available from: www.medscape.com/viewarticle/826596.
- Thara R, Sujit J. (2013) Mobile telepsychiatry in India. World Psychiatry. 12:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topol E. (2012) The Creative Destruction of Medicine: How the Digital Revolution Will Create Better Health Care. New York: Basic Books, A Member of the Perseus Books Group. [Google Scholar]
- United States Department of Health and Human Services (2013) Doctors and hospitals’ use of health IT more than doubles since 2012. Cited April 2015. Available from: www.hhs.gov/news/press/2013pres/05/20130522a.html.
- United States Department of Health and Human Services (2015) Chronic care management services. Cited March 2015. Available from: www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/ChronicCareManagement.pdf. [DOI] [PubMed]
- United States Department of Veterans Affairs (2011) Moving forward. Cited April 2015. Available from: https://mobile.va.gov/app/moving-forward.
- Unützer J, Harbin H, Schoenbaum M, Druss B. (2013) The collaborative care model: an approach for integrating physicians and mental health care in medical health homes. Health Home, Brief. Cited April 2015. Available from: www.medicaid.gov/State-Resource-Center/Medicaid-State-Technical-Assistance/Health-Homes-Technical-Assistance/Downloads/HH-IRC-Collaborative-5-13.pdf.
- Välimäki M, Hätönen H, Lahti M, Kuosmanen L, Adams CE. (2013) Information and communication technology in patient education and support for people with schizophrenia (review). Schizophr Bull. 39:496–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velligan D, Mintz J, Maples N, Xueying L, Gajewski S, Carr H, Sierra C. (2013) A randomized trial comparing in person and electronic interventions for improving adherence to oral medications in schizophrenia. Schizophr Bull. 39:999–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velligan DI, Kamil SH. (2014) Enhancing patient adherence: introducing smart pill devices. Ther Deliv. 5:611–613. [DOI] [PubMed] [Google Scholar]
- What’s My M3. Cited April 2015. Available from: http://whatsmym3.com/AboutAssessment.aspx.
- Wilson L, Gitlin M, Lightwood J. (2011) Schizophrenia costs for newly diagnosed versus previously diagnosed patients. Am J Pharm Benefits. 3:107–115. [Google Scholar]
- Worringham C, Rojek A, Stewart I. (2011) Development and feasibility of a smartphone, ECG and GPS based system for remotely monitoring exercise in cardiac rehabilitation. PLoS One. 6:e14669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu EQ, Birnbaum HG, Shi L, Ball DE, Kessler RC, Moulis M, Aggarwal J. (2005) The economic burden of schizophrenia in the United States in 2002. J Clin Psychiatry. 66:1122–1129. [DOI] [PubMed] [Google Scholar]
- Young JW, Geyer MA. (2015) Developing treatments for cognitive deficits in schizophrenia: the challenge of translation. J Psychopharmacol. 29:178–196. [DOI] [PMC free article] [PubMed] [Google Scholar]


