Abstract
The neonatal intensive care unit (NICU) is a setting with high nurse-to-patient ratios. Little is known about the factors that determine nurse workload and assignment. The goals of this study were to (1) develop a measure of NICU infant acuity; (2) describe the acuity distribution of NICU infants; (3) describe the nurse/infant ratio at each acuity level, and examine the factors other than acuity, including nurse qualifications and the availability of physicians and other providers, that determined staffing ratios; and (4) explore whether nurse qualifications were related to the acuity of assigned infants. In a two-stage cohort study, data were collected in 104 NICUs in 2008 by nurse survey (6,038 nurses and 15,191 infants assigned to them) and administrators reported on unit-level staffing of non-nurse providers; in a subset of 70 NICUs in 2009–2010, census data were collected on four selected shifts (3,871 nurses and 9,276 infants assigned to them). Most NICU infants (62%) were low-acuity (Levels 1 and 2); 12% of infants were high-acuity (Levels 4 and 5). The nurse-to-infant ratio ranged from 0.33 for the lowest-acuity infants to 0.95 for the highest-acuity infants. The staffing ratio was significantly related to the acuity of assigned infants but not to nurse education, experience, certification, or availability of other providers. There was a significant but small difference in the percentage of high-acuity (Levels 4 and 5) infants assigned to nurses with specialty certification (15% vs. 12% for nurses without certification). These staffing patterns may not optimize patient outcomes in this highly intensive pediatric care setting.
Keywords: neonatal intensive care, NICU, staffing and scheduling, hospitals, nursing care, nurse-patient ratio, patient acuity
Neonatal intensive care units (NICUs) care for the most vulnerable pediatric patient population. NICU stays are among the most expensive hospitalizations (Institute of Medicine, 2006). Patients in the NICU have complex care needs that require high levels of nursing resources overall. Individual infants, however, may differ in their nursing care requirements. The five categories of acuity for neonatal intensive care as depicted in the AAP/ACOG inpatient perinatal guidelines (American Academy of Pediatrics & American College of Obstetricians and Gynecologists, 1992, 2007) did not include detailed definitions, making implementation in practice settings potentially difficult.
Little is known about how NICUs determine nursing staffing, particularly in relation to the acuity of the infants. Acuity measures are, in fact, not in wide use for any population. The IOM, in Keeping Patients Safe (Institute of Medicine, 2003), called for more reliable and valid measures of patient acuity, as well as approaches to determine nurse staffing levels that take into account patient acuity. There have been no data available to assess how infant, nurse, or unit-level factors affect nurse workloads in US NICUs. In this paper, using data from a large national sample of NICUs, we report on the development of acuity definitions for the AAP/ACOG guidelines; the acuity distribution of NICU infants; the determinants of NICU nurse staffing ratios, including infant acuity levels, nurse characteristics, and physician and other provider staffing; and the association of acuity levels with assignment to nurses of differing qualifications.
Nurse Staffing in Relation to NICU Outcomes
The levels at which NICUs are staffed with nurses may affect patient outcomes, particularly for the most vulnerable infants—those with very low birth weights (VLBW) and those born preterm. In 67 NICUs in the US, nurse under-staffing relative to guidelines was associated with higher rates of nosocomial infection for VLBW infants (Rogowski et al., 2013), but this relationship has not been consistent. Cimiotti and colleagues, in a study of two NICUs in New York, found that more RN hours per patient day were associated with lower risk of infection in one NICU but not in the second NICU (Cimiotti, Haas, Saiman, & Larson, 2006). In a single NICU in Australia, higher staffing within the first three days after admission was associated with higher mortality rates (Callaghan, Cartwright, O'Rourke, & Davies, 2003).
Matching NICU Staff Characteristics to Infants’ Needs
In the Synergy Model, patient outcomes are optimized by matching nurse competencies to patients’ characteristics and needs (Baggs et al., 1999; Curley, 1998). The AAP/ACOG guidelines for NICU nurse-to-patient ratios call for assessment of infant, nursing staff, and nursing unit factors (American Academy of Pediatrics & American College of Obstetricians and Gynecologists, 2012). Acuity is a principal infant factor, and staff and unit factors also must be taken into account.
Registered nurses in the NICU have varying levels of training and experience that may complement infants with more and less complex statuses (Lake et al., 2015). The AAP/ACOG has called for NICU registered nurses to have “specialty certification or advanced training and experience in the nursing management of high risk neonates and their families” (American Academy of Pediatrics & American College of Obstetricians and Gynecologists, 2012, pp. 32–33). In 54 randomly selected NICUs in the UK, the proportion of nurses with neonatal qualifications was positively related to the survival of very-low-birth-weight and preterm infants (Hamilton, Redshaw, & Tarnow-Mordi, 2007).
NICU nurses work in care teams that differ across hospitals (Lake, Rochman, de Cordova, Kumar, & Rogowski, 2014). The configuration of the team may result in differing nursing care responsibilities. The AAP/ACOG acknowledged that “the number of staff and level of skill required are influenced by the scope of nursing practice and the degree of nursing responsibilities within an institution” (American Academy of Pediatrics & American College of Obstetricians and Gynecologists, 2012, p. 30).
Using a unique dataset, the goals of this study were to develop a measure of NICU infant acuity, to describe the acuity distribution of NICU infants across the hospital sample and by NICU care level, to estimate nurse-to-infant ratios for five infant acuity levels in the NICU, and to determine the factors other than infant acuity that determined the number and acuity of assigned infants. The factors we considered were nurse education, experience, specialty certification, and the availability of physicians and other providers on the unit.
Methods
After acuity definitions were developed to classify infants into five acuity levels for nursing care according to the AAP/ACOG guidelines, data were collected in two sequential studies in the same cohort of hospitals through different approaches.
NICU Samples
Data were collected from a cohort of hospitals in the US Vermont Oxford Network (VON), a voluntary, international quality and safety consortium dedicated to improving the quality and safety of neonatal care (Vermont Oxford Network, 2014). When the first data collection began in 2008, the VON included 576 US hospitals, approximately 65% of NICUs, based on the American Hospital Association Annual Survey data on general hospitals with nonzero neonatal intensive care beds (American Hospital Association, 2010) and 80% of VLBW infants in the US (Horbar et al., 2012). The VON is broadly representative of US NICUs (Lake et al., 2012).
The VON classifies NICUs into Levels A (restriction on ventilation, no surgery), B (major surgery), and C (open heart surgery permitted), which correspond roughly to levels II (special care nursery), III (NICU), and IV (regional NICU) in the AAP classification (American Academy of Pediatrics Committee on Fetus and Newborn, 2012). In the VON NICUs nationally (N = 615 with complete data for 633 in 2010), level A was about one-quarter AAP level II and about three-quarters AAP level III. Almost all (96%) of level B NICUs fell into AAP level III, and 91% of level C NICUs fell into AAP level IV.
Recruitment of hospitals was designed to achieve a sample representative of VON NICU levels of care and geographic regions. The NICU directors at all US VON hospitals initially were invited to participate. Midway through recruitment, a second invitation was sent only to NICUs in levels and regions with fewer recruits, in order to yield a representative sample. One hundred and four US VON hospitals participated in the first study in 2008. These NICUs represented one in five VON NICUs and one in nine US NICUs at that time. In the second data collection, 70 of the 104 hospitals participated.
Measures
Infant acuity
To operationalize infant acuity, an expert panel defined five mutually exclusive categories of infant need for nursing resources (Table 1) congruent with the AAP/ACOG inpatient perinatal care guidelines (American Academy of Pediatrics & American College of Obstetricians and Gynecologists, 2007). In the AAP guidelines, the five categories range from the lowest acuity, “Newborns requiring continuing care,” to the highest acuity, “Unstable newborns requiring complex critical care.” The expert panel included a neonatologist, a perinatal nurse specialist, and a representative from the National Association of Neonatal Nurses (NANN).
Table 1.
Operational Definitions of Infant Acuity Levels Originally Described by AAP/ACOG
| Infant Acuity Level | Original Description | Operational Definition |
|---|---|---|
| 1 | Continuing care | Infant only requiring PO or NG feedings, occasional enteral medications, basic monitoring. May or may not have a heparin lock for meds. |
| 2 | Requiring intermediate care | Stable infant on established management plan, not requiring significant support. Examples would include: Room air, supplemental oxygen or low flow nasal cannula, several meds. |
| 3 | Requiring intensive care | Infant is stabilized, though requires frequent treatment and monitoring to assure maintenance of stability. Examples would include: Ventilator, CPAP, high-flow nasal cannula, multiple IV meds via central or peripheral line. |
| 4 | Requiring multi-system support | Infant requires continuous monitoring and interventions. Examples would include: Conventional ventilation, stable on HFV, continuous drug infusions, several IV fluid changes via central line. |
| 5 | Unstable, requiring complex critical care | Infant is medically unstable and vulnerable, requiring many simultaneous interventions. Examples would include: ECMO, HFV, nitric oxide, frequent administration of fluids, medication. |
Note. AAP/ACOG, American Academy of Pediatrics & American College of Obstetricians and Gynecologists (1992; 2007). PO, by mouth; NG, nasogastric; CPAP, continuous positive airway pressure; IV, intravenous; HFV, high-frequency ventilation; ECMO, extracorporeal membrane oxygenation.
The definitions were subsequently refined through sessions with neonatal nurses at national conferences of the NANN and the VON. At these sessions, participants were provided with 15 vignettes (3 for each acuity level) developed from actual NICU infants to illustrate the five acuity levels. Participants were asked to provide feedback.
Before the first data collection, inter-rater reliability of the classification of infants into acuity levels was assessed on 258 infants by two independent raters in each of nine hospitals. The nine hospitals were a stratified random sample according to NICU level and geographic region of the 104 hospitals participating in the first data collection. The number of infants in each hospital ranged from 3 to 56, with an average of 29 infants per hospital. Fewer than 10% of infants were classified as Level 4 or 5, consistent with the overall distribution of infants. All levels of infant acuity were assessed in 3 of the nine hospitals. The classification had high inter-rater reliability (κ = 0.79; Landis & Koch, 1977).
Nurse-to-patient ratio
The fraction of a nurse that was assigned to each infant was computed as 1.0 divided by the number of assigned patients. This calculation was adjusted when an infant was assigned to more than one nurse, which happened rarely (3.3% of infants in 2008 and 1.5% in 2009).
Nurse assignment
The percentage of the nurse's assignment composed of infants of each acuity level was calculated based on the number and acuity of all infants assigned to the nurse on the shift.
Nurse qualifications
Nurses’ qualifications included education (BSN degree or not), experience (less than 1 year, 1 to 5 years, more than 5 years of NICU experience), and national specialty certification.
Non-nurse staffing
The FTE number of non-nursing providers per shift included the following categories of providers: social worker, nutritionist, respiratory therapist, pharmacist, patient care technician, lactation consultant, nurse practitioner, and other. Non-nurse FTEs per shift were computed by summing the number of providers present for the full shift and one half the number present for part of the shift. FTE number of neonatologists and FTE number of residents and neonatal fellows per shift were calculated separately from other providers, as were FTE for weekday, weeknight, and weekend/holiday shifts.
NICU characteristics
The NICU level of care (A, B, or C) was derived from the VON's annual institutional survey. Hospital ownership (non-profit, for-profit, public), teaching status (as indicated by membership in the Council of Teaching Hospitals), and NICU bed size (as measured by the number of neonatal intermediate care beds plus intensive care beds) were derived from the American Hospital Association Annual Survey of Hospitals.
Data Collection
This project was approved by the Institutional Review Boards of the University of Medicine and Dentistry of New Jersey, Rutgers, the University of Pennsylvania, the University of Vermont, The Ohio State University, Dartmouth College, and the study hospitals.
In February 2008, a site coordinator in each hospital trained the NICU staff nurses to classify infants using the acuity definitions. Then, nurses were surveyed through a web-based survey about the last shift worked and their personal characteristics. Within the study NICUs, the survey sampling frame included all staff nurses who worked at least 16 hours per week and had been employed at least three months on the nursing unit. The website opened in March 2008, and nurses chose a shift during the month to respond to the survey. The overall nurse response rate was 77%; the response rate exceeded 50% in 101 hospitals.
Nurses reported on the number and acuity of all infants assigned to them on the last shift worked. The respondent was presented with his or her responses about all assigned infants to correct any errors before submission of the survey. They also reported on their education, NICU experience, and specialty certifications. Nurse managers provided data on the number of neonatologists, residents and fellows, and other non-nursing providers present (for all of the shift or part of the shift) for the typical weekday, week-night, and weekend/holiday shifts. The data from the first data collection are referred to as survey data in this report.
In the second data collection, 70 of the 104 hospitals participated in a follow-on study. Data pertaining to all nurses working in the NICU on a selected shift, the infants assigned to each nurse, and the infant acuity level were collected by a site coordinator appointed by the hospital. The data were collected mid-shift on specified types of shifts, in four rounds between summer 2009 and summer 2010. The first shift at all hospitals was a day shift. The remaining three data collections were randomized to day, night and weekend shifts, and hospitals collected data on that type of shift in the remaining three rounds. Sixty-five hospitals collected data in the first round, 70 in the second round, and 69 in each of the third and fourth rounds. The data from the second data collection are referred to as census data in this report.
In both data collections, using the definitions in Table 1, the acuity level of all infants assigned to each nurse was collected, as well as whether one or more other nurses was also assigned to any of the infants.
Descriptive and Statistical Analyses
The goals of the analyses were to describe the acuity distribution of NICU infants, estimate the average nurse-to-patient ratio for each infant acuity level and to determine whether the nurse-to-patient ratio was related to the nurse qualifications or the presence of physicians and non-nursing providers on the unit. To compare the sample hospitals to the universe of US hospitals with NICUs, the authors computed the distribution of hospital characteristics and NICU bed size using the American Hospital Association Annual Survey data on general hospitals with nonzero neonatal intensive care beds (American Hospital Association, 2010). We calculated the nurse-to-patient ratio of RNs and LPNs. We also explored whether the infant acuity distribution differed by nurse qualifications and nurse skill level (RN vs. LPN).
A nurse-level regression was estimated for both hospital samples with the nurse-to-patient ratio (i.e., 1 over the number of patients assigned, adjusted for co-assigned infants, which were rare) as the dependent variable. The independent variables were the fraction of infants in each of the five acuity levels in the nurse's adjusted assignment. The models did not have an overall intercept term, so that all five acuity coefficients could be interpreted as the fraction of a nurse's time assigned to an infant of each acuity level, rather than as an incremental difference in staffing relative to a reference acuity category. Post-estimation commands tested whether the coefficients were equal and different from zero.
A second model, estimated on the survey data, included as independent variables the nurse's level of education, experience, and specialty certification; and the FTE of neonatologists, residents and fellows, and other providers present on the unit. To test for sensitivity of the FTE definition, we estimated a model with variables defined as 0.25 FTE for part-shift providers to compare to the 0.5 FTE definition.
All models were estimated using random effects linear regression, including hospital random effects. These models adjusted for clustering of nurses within NICUs. Among models that adjust for clustering of nurses within NICUs, random effects yield the most precise standard errors, account for the correlation within shift and hospital, and thereby increase model efficiency. The models for the census data additionally contained random effects for the round of data collection. Variance accounted for by the regression model was computed as a linear mixed model R-squared statistic.
We calculated the mean number of infants per nurse across qualification subgroups in the survey data. An additional nurse-level regression was run with the fraction of the nurse's assignment accounted for by high-acuity (Levels 4 and 5) infants as the dependent variable, with the independent variables being a BSN degree, NICU experience, and specialty certification. All analyses were performed in STATA 11.
Results
Hospital and Nurse Characteristics
Compared to the universe of US hospitals with NICUs, our samples contained more teaching hospitals (27% in the US vs. about 50% in the study samples) and somewhat more not-for-profit hospitals (71% in the US vs. 81–86% in the study samples), as well as larger units (a mean of 22 beds in the US vs. 32 in the study samples). Our samples were disproportionately Magnet® hospitals (35–43%), compared with all US hospitals with NICUs, in which one in five hospitals was a Magnet hospital. Sample characteristics and univariate statistics for key variables are presented in Table 2.
Table 2.
Hospital Neonatal Intensive Care Unit (NICU) and Infant Characteristics
| Survey |
Census |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | Subcategory | N | n | % | Mean | SD | N | n | % | Mean | SD | |
| Hospitals | Total Number | 104 | 70 | |||||||||
| Hospital Ownership | Non-Profit | 81 | 86 | |||||||||
| For Profit | 6 | 4 | ||||||||||
| Public | 13 | 10 | ||||||||||
| Member, Council of Teaching Hospitalsa | 48 | 51 | ||||||||||
| Geographic Region | Northeast | 21 | 26 | |||||||||
| Midwest | 28 | 24 | ||||||||||
| South | 31 | 30 | ||||||||||
| West | 19 | 19 | ||||||||||
| Magnet® Accreditation | 35 | 43 | ||||||||||
| NICUs | NICU Level | A | 13 | 10 | ||||||||
| B | 60 | 59 | ||||||||||
| C | 27 | 31 | ||||||||||
| Number of Beds | 32 | 20 | 32 | 19 | ||||||||
| Nurses | Total Number | 6,038 | 3,871 | |||||||||
| 5 or More Years of Experience | 74 | 44 | ||||||||||
| BSN | 58 | 49 | ||||||||||
| Neonatal Specialty Certification | 26 | 44 | ||||||||||
| Non-Nurse Providers | FTE Physicians | Neonatologists | 1.5 | 1.40 | ||||||||
| Residents and Fellows | 1.7 | 2.00 | ||||||||||
| FTE Other Professional Staff | 6.4 | 4.60 | ||||||||||
| Infants | Number of Infants | 15,191 | 9,276 | |||||||||
| Nurse-to-Infant Ratio | 0.46 | 0.08 | 0.47 | 0.07 | ||||||||
| Acuity Level Distribution | Level 1 | 33 | 32 | |||||||||
| Level 2 | 29 | 33 | ||||||||||
| Level 3 | 26 | 26 | ||||||||||
| Level 4 | 8 | 7 | ||||||||||
| Level 5 | 4 | 2 | ||||||||||
Note. Survey=nurse survey (2008); Census= all nurse assignments on shift, collected in 4 rounds (2009-2010). SD, standard deviation; BSN, bachelor of science degree in nursing; FTE, full-time equivalent.
Hospital characteristics were not available for 3 hospitals.
The level of care in the sample NICUs was about 10% in level A (restriction on ventilation, no surgery), 60% in level B (major surgery), and 30% in level C (open heart surgery permitted). The study samples had disproportionately fewer level A units and more level C units compared to the VON as a whole, which had 30% level A and 18% level C in 2008. The geographic distribution of the study cohorts was balanced, with 20 to 30% of hospitals in each of the four regions.
The survey data sample consisted of 6,038 nurses who reported on the care of 15,191 infants. The census data included 3871 nurses who were assigned 9276 infants. The survey sample was nearly entirely (99%) registered nurses. Most NICUs (71%) employed only registered nurses. The NICUs with licensed practical nurses (LPNs) employed three, on average. Among nurses surveyed, 41% reported about a weekday shift, 28% about a weeknight, and 31% about a weekend. The average nurse-to-patient ratio in the survey data was .46, and was .47 in the census data. RNs had a lower ratio (.47) than LPNs (.39); LPNs cared for 2.6 infants on average, and RNs cared for 2.1. The mean availability of physicians and other staff were as follows: 1.5 FTE neonatologists, 1.7 residents, and 6.4 other professional providers. (The .25 FTE definition for part-shift providers yielded slightly lower average FTEs: 1.37 neonatologists, 1.63 residents, and 6.0 other professional providers.)
Based on survey data, there were few infants in the highest acuity levels (4% in Level 5, 8% in Level 4), with the majority in levels 3, 2, and 1 (26%, 29%, and 33%, respectively) as shown in Table 2. The proportions of highest-acuity infants were slightly lower in the census data. Level C NICUs had more high-acuity infants (47% in acuity Levels 3, 4, and 5) compared to Level A NICUs (30%). The proportion of infants at each acuity level except acuity Level 2 differed significantly across NICU levels of care (p < .05; see Table 3). LPNs cared for lower-acuity infants (90% of their assigned infants were Level 1 or 2) than RNs (53% were Level 1 or 2).
Table 3.
Infant Acuity Levels across Hospital NICU Levels of Care.
| Hospitals by NICU Level of Care (%) |
|||
|---|---|---|---|
| Infant Acuity Level | A (n= 15) | B (n= 59) | C (n= 30) |
| Level 1 (continuing care) | 39 | 35 | 25 |
| Level 2 (intermediate care) | 31 | 29 | 29 |
| Level 3 (intensive care) | 23 | 25 | 30 |
| Level 4 (multi-system support) | 4 | 8 | 11 |
| Level 5 (unstable/complex critical care) | 3 | 3 | 6 |
Note. Data source: 2008 nurse survey. NICU levels of care per the Vermont Oxford Network: A (restriction on ventilation, no surgery), B (major surgery), and C (open heart surgery permitted). Differences in acuity distribution were significant (p< .05) across NICU levels of care for all acuity levels except acuity Level 2.
Multivariable Regression Results
Estimated nurse-to-patient ratios differed significantly based on infant acuity level (p < .001) and from zero (p < .001), as shown in Table 4. The coefficients serve as estimated nurse-to-patient ratios for each acuity level and demonstrate that nurse-to-patient ratios increased with infant acuity. Based on the survey data, infants in the highest acuity level (5) had an average nurse-to-patient ratio of 0.95. The ratio was lower in acuity Level 4 (.66). The ratio dropped to .49 for acuity 3, to .38 for acuity 2, and .34 for acuity 1. The results of the estimation were robust across the two data collections, with only slight differences in the estimated coefficients (.03 difference on average). Figure 1 depicts the reciprocal of the nurse-to-patient ratio, that is, infants per nurse for each acuity level, in the survey data.
Table 4.
Estimated NICU Nurse-to-Patient Ratios (Coefficients From Random Effects Linear Regression) as a Function of Infant Acuity
| Survey (N=6038) |
Census (N=3871) |
|||
|---|---|---|---|---|
| Infant Acuity | Ratio | 95% CI | Ratio | 95% CI |
| Level 1 (continuing care) | .34 | .32–.35 | .36 | .34–.38 |
| Level 2 (intermediate care) | .38 | .36–.39 | .41 | .39–.43 |
| Level 3 (intensive care) | .49 | .48–.51 | .52 | .50–.53 |
| Level 4 (multi-system support) | .66 | .64–.68 | .72 | .69–.74 |
| Level 5 (unstable/complex critical care) | .95 | .93–.98 | .96 | .93–.99 |
| R 2 | .36 | – | .35 | – |
Note. NICU= neonatal intensive care unit. Survey= nurse survey (2008); Census= all nurse assignments on shift, collected in 4 rounds (2009–2010). CI= confidence interval. Estimated nurse-to-patient ratios differed significantly across acuity levels (p< .001) and from zero (p< .001). Both R2 values were significant (p< 0.01).
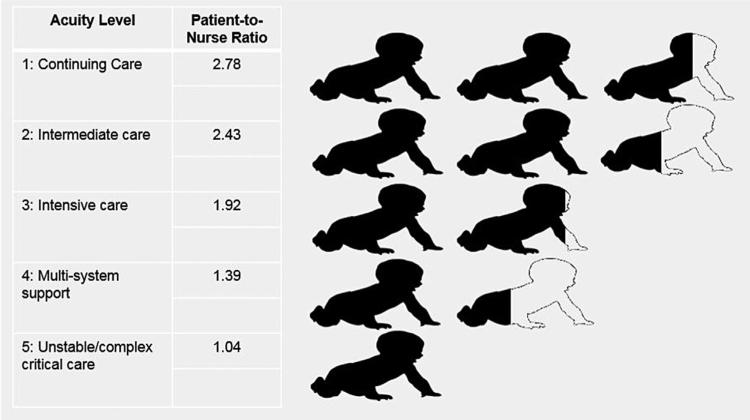
Figure 1.
Infants per nurse for each acuity level, calculated as the reciprocal of estimated nurse-to-patient ratios, from 2008 nurse survey data in which 6,038 nurses reported on the care of 15,191 infants.
The number of neonatologists, residents and fellows, and other professional providers on the unit were not significant predictors of nurse-to-patient ratio, under either FTE definition (.50 versus .25 of a shift) of part-shift providers. Similarly, nurse education, experience, and specialty certification were not significant predictors of nurse-to-patient ratio when each type of qualification was viewed separately. In nurse-level multivariable regression with all nurse qualifications, only specialty certification was significantly related to the percentage of high-acuity infants assigned (β = .03, p < .01), that is, having specialty certification increased the average nurse's percentage of high-acuity infants by 3%. The proportions of high-acuity infants in the assignments were 15% for certified nurses and 12% for non-certified nurses.
Discussion
Very little is known about nurse staffing of NICUs in the United States, particularly in relation to infant acuity. In this study, we defined the five infant acuity categories that were first specified in the AAP/ACOG nurse staffing guidelines in 1992 (American Academy of Pediatrics & American College of Obstetricians and Gynecologists, 1992) and then examined nurse staffing patterns by infant acuity level. This is the first known report of national data on nurse-to-patient ratios in the NICU by infant acuity and of the factors associated with nurse staffing levels. The average nurse cared for two infants, but the nurse-to-infant ratio varied from .33 for the lowest-acuity infants to .95 for the highest-acuity infants. This finding was robust across two data collections in two different years using two different data collection methods. We note that these data reveal the prevailing staffing patterns across acuity levels. These levels may not necessarily be sufficient to meet patient needs or the nurse-to-patient ratios called for by specialty groups. Other evidence from these data indicates that relative to the 2007 AAP/ACOG guidelines, understaffing in NICUs is pervasive (Rogowski et al., 2013).
Infant acuity was found to be the sole determinant of nurse workloads; the presence of other members of the care team was not associated with nurse-to-patient ratios. Because NICUs vary in the number and composition of non-nurse providers (Lake et al., 2014), infant outcomes may not be optimized if infant acuity is the only determinant of nurse staffing. Similarly, in this highly intensive care setting with the most vulnerable pediatric population, nurse education, experience, and specialty certification were not reflected in nurse-to-infant ratios. Although it has been theorized that consideration of patient needs and nurse qualifications should yield an optimal match of higher-acuity infants to more qualified nurses (Curley, 1998), this pattern was only minimally apparent in these data. In light of the IOM Future of Nursing recommendations (Institute of Medicine, 2010), further study of the outcomes of patient assignment by nurse qualifications is warranted.
Studies linking staffing to outcomes can be difficult to interpret, as higher acuity can be associated with both higher staffing and worse outcomes. Without control for acuity, higher staffing can appear to lead to worse outcomes. The current study advances this field by providing an acuity classification system, which is a first step toward staffing-outcomes research that adequately accounts for acuity. A bill introduced in the US Congress would require a national patient acuity tool be used in staffing plans (Registered Nurse Safe Staffing Act of 2014, S. 2353, 2014), but there are few patient populations in which such acuity classifications exist. The evidence reported here on current staffing levels in the NICU using a uniform acuity definition across a large number of hospitals might be useful in informing such efforts.
While the hospitals in this study are broadly representative of the VON, the VON hospitals do not fully represent all US hospitals with NICUs. In particular, very small units are underrepresented in the VON. In addition, our samples were disproportionately Magnet-accredited and included more NICUs that had open heart surgery capacity. Nevertheless, the evidence presented here reflects the care settings of the large majority of critically ill infants in the US.
Conclusions
Our findings suggest that the most vulnerable hospitalized patients, unstable newborns requiring complex critical care, receive levels of nursing resources that reflect patient acuity but do not take into account the nurse's qualifications or the availability of other NICU providers. Acuity classification and staffing adjustment for acuity and other factors remain notable gaps in current evidence and limit the capacity for optimal staffing practices. This study fills that gap for one vulnerable population. Further research is needed to better understand whether these assignment patterns optimize outcomes for critically ill infants.
Acknowledgments
This research was funded by NINR grant number R01NR010357 and by the Robert Wood Johnson Foundation INQRI program. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health. We thank Dr. Robyn Cheung, the project manager, and the nurses, nurse managers, and project site coordinators at the 104 Vermont Oxford Network institutions that participated in the study. We thank Rizie Kumar for excellent programming assistance.
Footnotes
Disclosure of Conflicts of Interest
Dr. Horbar is chief executive and scientific officer for the Vermont Oxford Network. Dr. Staiger holds an equity interest in ArborMetrix, Inc., a company that sells efficiency measurement systems and consulting services to insurers and hospitals.
Contributor Information
Jeannette A. Rogowski, Rutgers The State University of New Jersey, New Brunswick, NJ
Douglas O. Staiger, Dartmouth College, Hanover, NH
Thelma E. Patrick, The Ohio State University, Columbus, OH
Jeffrey D. Horbar, University of Vermont, Burlington, VT
Michael J. Kenny, University of Vermont Burlington, VT
Eileen T. Lake, Center for Health Outcomes and Policy, Research, School of Nursing, University of Pennsylvania, 418 Curie Blvd., Philadelphia, PA 19104.
References
- American Academy of Pediatrics & American College of Obstetricians and Gynecologists . Guidelines for perinatal care. 3rd ed. American Academy of Pediatrics; The American College of Obstetricians and Gynecologists; Elk Grove Village, IL: Washington, DC: 1992. [Google Scholar]
- American Academy of Pediatrics & American College of Obstetricians and Gynecologists . Guidelines for perinatal care. 6th ed. American Academy of Pediatrics; The American College of Obstetricians and Gynecologists; Elk Grove Village, IL: Washington, DC: 2007. [Google Scholar]
- American Academy of Pediatrics & American College of Obstetricians and Gynecologists . Guidelines for perinatal care. 7th ed. American Academy of Pediatrics; The American College of Obstetricians and Gynecologists; Elk Grove Village, IL: Washington, DC: 2012. [Google Scholar]
- American Academy of Pediatrics Committee on Fetus and Newborn Levels of neonatal care. Pediatrics. 2012;130:587–597. doi: 10.1542/peds.2012-1999. doi: 10.1542/peds.2012-1999. [DOI] [PubMed] [Google Scholar]
- American Hospital Association . AHA annual survey database 2008 edition. American Hospital Association; Chicago, IL: 2010. [Google Scholar]
- Baggs JG, Schmitt MH, Mushlin AI, Mitchell PH, Eldredge DH, Oakes D, Hutson AD. Association between nurse-physician collaboration and patient outcomes in three intensive care units. Critical Care Medicine. 1999;27:1991–1998. doi: 10.1097/00003246-199909000-00045. [DOI] [PubMed] [Google Scholar]
- Callaghan LA, Cartwright DW, O'Rourke P, Davies MW. Infant to staff ratios and risk of mortality in very low birth weight infants. Archives of Disease in Childhood Fetal & Neonatal Edition. 2003;88:F94–F97. doi: 10.1136/fn.88.2.F94. doi: 10.1136/fn.88.2.F94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cimiotti JP, Haas J, Saiman L, Larson EL. Impact of staffing on bloodstream infections in the neonatal intensive care unit. Archives of Pediatrics & Adolescent Medicine. 2006;160:832–836. doi: 10.1001/archpedi.160.8.832. doi: 10.1001/archpedi.160.8.832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curley MAQ. Patient-nurse synergy: Optimizing patients’ outcomes. American Journal of Critical Care. 1998;7:64–72. [PubMed] [Google Scholar]
- Hamilton KES, Redshaw ME, Tarnow-Mordi W. Nurse staffing in relation to risk-adjusted mortality in neonatal care. Archives of Disease in Childhood. 2007;92:F99–F103. doi: 10.1136/adc.2006.102988. doi: 10.1136/adc.2006.102988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horbar JD, Carpenter JH, Badger GJ, Kenny MJ, Soll RF, Morrow KA, Buzas JS. Mortality and neonatal morbidity among infants 501 to 1500 grams from 2000 to 2009. Pediatrics. 2012;129:1019–1026. doi: 10.1542/peds.2011-3028. doi: 10.1542/peds.2011-3028. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine . Keeping patients safe: Transforming the work environment of nurses. The National Academies Press; Washington, DC: 2003. [Google Scholar]
- Institute of Medicine . Preterm birth: Causes, consequences, and prevention. The National Academies Press; Washington, DC: 2006. [Google Scholar]
- Institute of Medicine The future of nursing - Leading change, advancing health. Report brief. 2010 Retrieved from http://www.iom.edu/Reports/2010/The-Future-of-Nursing-Leading-Change-Advancing-Health.aspx/
- Lake ET, Staiger D, Horbar J, Cheung R, Kenny M, Patrick T, Rogowski J. Association between hospital recognition for nursing excellence and outcomes of very low birth weight infants. Journal of the American Medical Association. 2012;307:1709–1716. doi: 10.1001/jama.2012.504. doi: 10.1001/jama.2012.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake ET, Rochman M, de Cordova P, Kumar A, Rogowski JA. Composition and wage costs of the healthcare team in the neonatal intensive care unit.. Paper presented at the AcademyHealth 2014 Annual Research Meeting; San Diego, CA.. 2014. [Google Scholar]
- Lake ET, Staiger D, Patrick T, Horbar J, Kenny MJ, Rogowski J. Disparities in perinatal quality outcomes for very low birth weight infants in neonatal intensive care. Health Services Research. 2015;50:374–397. doi: 10.1111/1475-6773.12225. doi: 10.1111/1475-6773.12225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- Registered Nurse Safe Staffing Act of 2014, S. 2353, 113th Cong. 2014 Retrieved from https://www.congress.gov/bill/113th-congress/senate-bill/2353.
- Rogowski J, Staiger D, Patrick T, Horbar J, Kenny MJ, Lake E. Nurse staffing and NICU infection rates. JAMA Pediatrics. 2013;167:444–450. doi: 10.1001/jamapediatrics.2013.18. doi: 10.1001/jamapediatrics.2013.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vermont Oxford Network What is the Vermont Oxford Network? 2014 Retrieved from http://www.vtoxford.org/about/about.aspx.