Abstract
IMPORTANCE
Research has shown that higher activation and engagement with health care is associated with better self-management. To our knowledge, the linkage intervention (LINKAGE) is the first to engage patients receiving addiction treatment with health care using the electronic health record and a patient activation approach.
OBJECTIVE
To examine the effects of an intervention aiming to link patients receiving addiction treatment with health care.
DESIGN, SETTING, AND PARTICIPANTS
A nonrandomized clinical trial evaluating the LINKAGE intervention vs usual care by applying an alternating 3-month off-and-on design over 30 months. Participants were recruited from an outpatient addiction treatment clinic in a large health system between April 7, 2011, and October 2, 2013.
INTERVENTIONS
Six group-based, manual-guided sessions on patient engagement in health care and the use of health information technology resources in the electronic health record, as well as facilitated communication with physicians, vs usual care.
MAIN OUTCOMES AND MEASURES
Primary outcomes, measured at 6 months after enrollment, were patient activation (by interview using the Patient Activation Measure), patient engagement in health care (by interview and electronic health record), and alcohol, drug, and depression outcomes (by interview using the Addiction Severity Index for alcohol and drug outcomes and Patient Health Questionnaire (PHQ) for depression).
RESULTS
A total of 503 patients were recruited and assigned to the LINKAGE (n = 252) or usual care (n = 251) conditions, with no differences in baseline characteristics between conditions. The mean (SD) age of the patients was 42.5 (11.8) years, 31.0% (n = 156) were female, and 455 (90.5%) completed the 6-month interview. Compared with usual care participants, LINKAGE participants showed an increase in the mean number of log-in days (incidence rate ratio, 1.53; 95% CI, 1.19–1.97; P = .001). Similar results were found across types of patient portal use (communicating by email, viewing laboratory test results and information, and obtaining medical advice). LINKAGE participants were more likely to talk with their physicians about addiction problems (odds ratio, 2.30; 95% CI, 1.52–3.49; P < .001). Although 6-month abstinence rates were high for both conditions (≥70.0% for both) and depression symptoms improved (the proportion with scores≥15 on the 9-item PHQ dropped from 15.1% [38 of 252] to 8.0% [18 of 225] among LINKAGE participants), there were no differences between conditions. Those who received all intervention components had significantly better alcohol and other drug outcomes than those who received fewer intervention components.
CONCLUSIONS AND RELEVANCE
Findings support the feasibility and effectiveness of the LINKAGE intervention in helping patients receiving addiction treatment engage in health care and increase communication with their physicians. The intervention did not affect short-term abstinence or depression outcomes. Understanding if the LINKAGE intervention helps prevent relapse and manage long-term recovery will be important.
TRIAL REGISTRATION
clinicaltrials.gov Identifier: NCT01621711
Patients with alcohol and other drug (AOD) use disorders have high rates of medical and psychiatric comorbidities and complex treatment needs.1–4 They often rely on emergency services, seldom using preventive services even when they have health insurance,5–7 with that trend increasing in recent years.8 At the same time, health care has a key role in positive AOD use outcomes and lower cost trajectories.7,9–13 Although a robust linkage between mainstream health care and addiction treatment would benefit these patients,14 this goal has not been accomplished.2,3
Health care reform and related policy changes have brought unprecedented opportunities to improve integration of care for patients with AOD problems.15 Building on the Mental Health Parity and Addiction Equity Act,16,17 the Patient Protection and Affordable Care Act18 made addiction services an “essential benefit” rather than being subject to more limitations than for other health conditions.18 In addition, the fast-paced evolution and implementation of health information technology (eg, electronic health records [EHRs], including patient portals)19–23 stemming from “meaningful use” regulations offer innovative mechanisms for patients with AOD disorders to engage in their health care.15–17
However, patients with AOD disorders lag behind individuals with other health conditions in participating in their health care through patient portals,24 and few interventions to facilitate their use have been tested. At the same time, studies25–27 demonstrate the use of health technology by patients with AOD and psychiatric disorders. Patient portals provide opportunities to engage in health care, such as interacting with clinicians, using online programs for health problems (eg, sleep disorders or coping with pain), and obtaining medical information and appointments. To our knowledge, the linkage intervention (LINKAGE) is the first trial of an intervention focused on increasing engagement of patients having AOD disorders with health care using the EHR and patient portals as a platform, as well as a patient activation approach used for other health conditions for engaging patients.22
Building on research in other health conditions demonstrating that higher activation levels are associated with better self-management,28–30 we hypothesized that the LINKAGE intervention would increase patient activation and engagement in health care, decrease AOD use, and reduce depression symptoms. We also examined intervention results for the subset of patients with psychiatric comorbidity.
Methods
Study Design
The study site was the San Francisco outpatient addiction treatment clinic of Kaiser Permanente Northern California, a large health care system. The study was a nonrandomized clinical trial31 comparing the LINKAGE intervention and usual care (UC). Intervention allocation was determined by a nonrandomized, alternating off-and-on design over 30 months (ie, 5 alternating 3-month periods for each condition). After a random start, the LINKAGE intervention groups alternated with the UC medical education groups, changing every 3 months. Eligible patients were recruited in each period, were assigned to the current arm, and received LINKAGE or UC medical education sessions accordingly. The study used an off-and-on design rather than randomization due to high risk of contamination because patients in both conditions attended the larger treatment program together. Although it was nonrandom, patient allocation was independent of patient characteristics, thus enhancing comparability in potential confounders between conditions.
Key Points.
Question
What is the effect of an intervention aiming to engage patients receiving addiction treatment with health care using the electronic health record and a patient activation approach?
Findings
This nonrandomized clinical trial found a significant effect of the LINKAGE intervention on patient engagement in health care, including patient portal use and communication with physicians about alcohol and other drug problems. Six-month abstinence rates were high and comparable between conditions.
Meaning
Teaching and activating patients receiving addiction treatment on how to use health care may empower them to better engage in their health management, and electronic health record patient portals may be useful in accomplishing this goal.
Study Participants
Patients 18 years or older deemed eligible by their physician were recruited between April 7, 2011, and October 2, 2013, after completing a 10-day stabilization program. Nine potential participants were not eligible because of severe cognitive disability, and 40 were ineligible due to severe psychiatric comorbidity (ie, exhibiting severe mania, active psychosis, or severe aggressive behavior) (26 LINKAGE participants and 23 UC participants). All participants provided written informed consent, receiving $50 compensation for the baseline interview and $60 compensation for the 6-month interview. The institutional review boards of the University of California, San Francisco, and Kaiser Permanente Northern California approved the study, and it received a National Institutes of Health Certificate of Confidentiality.
Baseline Assessment
After informed consent, the baseline interview was self-administered by computer with a research technician (S.B.W.) present. Data were collected on demographics, socioeconomic status (education and income), computer and smart-phone access and use, AOD dependence by type (using the Diagnostic Interview Schedule for Psychoactive Substance Dependence in the DSM-IV),32,33 and baseline measures of 6-month outcome measures. Nineteen substance abuse–related medical condition categories and 4 psychiatric disorders (major depression, anxiety, bipolar, and other psychotic disorders)1,10,13 were collected from the EHR.
Usual Care
Participants in both arms received standard treatment, including medical examinations and detoxification. Standard treatment first included a 2-week stabilization program. The next phase (when study recruitment occurred) lasted 6 weeks and consisted of 2 groups per day, 5 days a week, during which participants received either the LINKAGE or UC medical education sessions depending on whether it was an on or off period. Usual care medical education sessions were 45 minutes and were conducted by a licensed therapist. They focused on AOD-associated medical and psychological problems. Standard treatment also included therapy groups, individual counseling, 12-step meetings, and weekly breathalyzer and urine screens. Appointments with physicians and medications were available.
LINKAGE Intervention
LINKAGE participants received standard treatment. However, instead of the UC medical education sessions, they received six 45-minute group-based, manual-guided sessions (2 per week) conducted by a clinical psychologist (T.B.R.), which focused on demonstrating how health care is related to overall health, accessing and engaging with health care, and improving communication with physicians. The theoretical approach was patient activation, namely, “understanding one’s role in the care process and having the knowledge, skill, and confidence to manage one’s health and health care.”34(p207) Participants were taught key patient portal skills (eg, using secure email, viewing laboratory test results and medical information, and accessing prevention services) and were motivated to use them. They also practiced skills necessary for collaborative communication with health care professionals and were offered contact with their primary care physician facilitated by a therapist (T.B.R.) (ie, a 15-minute telephone appointment, a secure email, or help in preparation for an in-person medical visit to discuss their addiction and treatment, health concerns, and ongoing care).
Follow-up Assessment
Telephone interviews were conducted at 6 months after study enrollment. Electronic health record data were obtained for both the intervention period (study enrollment through 6 weeks, conservatively allowing for missed and makeup sessions) and the postintervention period (week 7 through 6 months).
Outcome Measures
The Patient Activation Measure score assessed patient beliefs, knowledge, and confidence regarding engaging in health behaviors on a 13-item scale (score range, 1–100 points).35 Again of 3 to 5 points is associated with improved health behaviors and positive health outcomes.36
Patient engagement primary outcomes were days of patient portal log-in measured by the EHR and communication about AOD problems with the primary care physician measured by the following interview question: “Have you talked to your primary care provider about AOD problems?” (yes or no). Electronic health record data were also collected on the use of the patient portal to email physicians, check laboratory test results, access information about laboratory tests and medical conditions, and obtain medical advice.
Addiction treatment retention during the 6 months after study recruitment was calculated from the EHR as the number of days attending treatment without a gap of 7 or more continuous days, consistent with the program’s definition of dropout.9 Alcohol and other drug abstinence and heavy drinking were measured by the Addiction Severity Index37 and by the National Institute on Alcohol Abuse and Alcoholism evidence-based questions on the numbers of days drinking and days of heavy drinking (≥5 drinks per day for men and ≥4 drinks per day for women)38,39 and the use of each of 9 substances in the past 30 days.
Depression symptoms were measured by the 9-item Patient Health Questionnaire.40 Scores range from 0 to 27. A score of at least 15 indicates moderate to severe depression and need for active depression treatment.41 We found no differences between conditions using cut points of 10 or 15.
Statistical Analysis
Power calculations are 2 sided, with a significance level of .05. Assuming an overall proportion of 60.0% improvement in patient activation (eg, ≥3-point improvement in the Patient Activation Measure score), we had greater than 0.80 power to test at least a 13.0% difference between conditions with a sample size of 225 per group. With a total abstinence rate of 60.0%13,42 in the UC condition, power to detect a 15.0% between-condition difference was 0.92 with a sample size of 219. Although longitudinal Poisson regression models were used in analyzing patient portal use, we present a more conservative estimation for analysis of a single time point. We had power of 0.99 with a sample size of 142 in each condition to detect a risk ratio of 1.5 for patient portal use between conditions.
We examined comparability between conditions on baseline characteristics using general linear regression for continuous variables and Pearson χ2 test for categorical variables. The LINKAGE intervention effect on patient portal use was analyzed using generalized estimating equation Poisson regression, with allowance for overdispersion using a quasi-likelihood approach43 adjusting for dependence and time. We report main effects from models without inclusion of the interaction of the intervention with time because the time-averaged effect of the LINKAGE intervention (compared with UC) was the main interest. The intervention effect on nonportal outcomes at 6 months was examined using logistic regression for binary-measures and general linear regression for continuous measures. To account for multiple comparisons, we conducted both unadjusted analyses and analyses with Bonferroni correction for 5 outcomes (patient activation, days of patient portal log-in, communication about AOD problems with the primary care physician, AOD use outcomes, and depression outcomes).
Exploratory analysis within the LINKAGE condition examined the effects of the number of LINKAGE sessions attended and facilitated physician communication on each outcome using Pearson χ2 test for categorical variables and general linear regression for continuous variables. We also examined the differences between conditions among the subsample with psychiatric comorbidity.1,13 Analyses were conducted using the intent-to-treat principle with statistical software (SAS, version 9.3; SAS Institute Inc).
Results
Enrollment and Follow-up
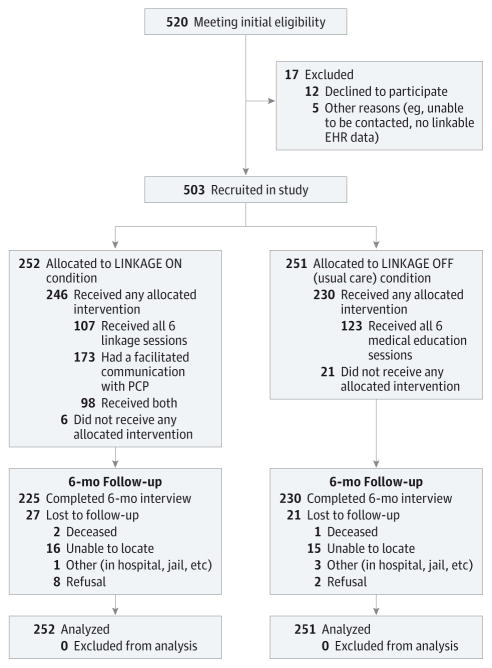
Of 520 eligible patients, 503 were recruited and completed a baseline interview (Figure). Of these patients, 455 (90.5%) completed the 6-month interview, with no significant differences between conditions. Three hundred ninety-five of 503 (78.5%) had a psychiatric comorbidity.
Figure. CONSORT Study Flow Diagram for the LINKAGE Study.
CONSORT indicates Consolidated Standards of Reporting Trials; EHR, electronic health record; and PCP, primary care physician.
Receipt of the LINKAGE Intervention
Of the 252 LINKAGE participants, 246 (97.6%) attended at least 1 session, with 139 (55.2%) attending 1 to 5 and 107 (42.5%) attending all 6. Among the UC participants, 230 (91.6%) attended at least 1 session, with 107 (42.6%) attending 1 to 5 and 123 (49.0%) attending all 6. Facilitated telephone, email, or in-person visits by LINKAGE participants with primary care physicians were received by 173 of 252 (68.7%) (Figure).
Baseline Patient Characteristics
We found no significant differences in age, sex, race/ethnicity, education, annual household income, AOD dependence, level of patient activation, or access to computer or smartphone or use between LINKAGE and UC conditions (Table 1). The mean length of Kaiser Permanente Northern California membership was 6.5 years, with no difference between conditions. We found no differences in the prevalence of medical and psychiatric comorbidities10,13,44 except for liver cirrhosis (11 [4.4%] for LINKAGE and 25 [10.0%] for UC) and diabetes (10 [4.0%] for LINKAGE and 22 [8.8%] for UC) (P < .05 for both). The only difference among either the full sample or the subsample with psychiatric comorbidity was that more UC participants reported talking with their physician about AOD problems (P = .02 for the full sample and P = .001 for the subsample with psychiatric comorbidity).
Table 1.
Characteristics of Study Participants at Baseline, by Intervention and Psychiatric Comorbidity
| Variable | Among the Full Sample | P Value | Among the Subsample With Psychiatric Comorbidity | P Value | ||
|---|---|---|---|---|---|---|
|
|
|
|||||
| LINKAGE (n = 252) | Usual Care (n = 251) | LINKAGE (n = 197) | Usual Care (n = 198) | |||
| Demographics and socioeconomic status, No. (%) | ||||||
|
| ||||||
| Age group, y | ||||||
|
| ||||||
| 18–30 | 56 (22.2) | 40 (15.9) | .06 | 47 (23.9) | 32 (16.2) | .14 |
|
|
|
|||||
| 31–45 | 98 (38.9) | 101 (4.2) | 78 (39.6) | 76 (38.4) | ||
|
|
|
|||||
| 46–60 | 87 (34.5) | 86 (34.3) | 63 (32.0) | 75 (37.9) | ||
|
|
|
|||||
| ≥61 | 11 (4.4) | 24 (9.6) | 9 (4.6) | 15 (7.6) | ||
|
| ||||||
| Female sex | 76 (30.2) | 80 (31.9) | .70 | 67 (34.0) | 75 (37.9) | .44 |
|
| ||||||
| Race/ethnicity | ||||||
|
| ||||||
| African American | 17 (6.7) | 20 (8.0) | .96 | 10 (5.1) | 14 (7.1) | .63 |
|
|
|
|||||
| Asian | 16 (6.3) | 18 (7.2) | 14 (7.1) | 9 (4.5) | ||
|
|
|
|||||
| Hispanic | 49 (19.4) | 52 (20.7) | 32 (16.2) | 42 (21.2) | ||
|
|
|
|||||
| Native American | 6 (2.4) | 4 (1.6) | 4 (2.0) | 3 (1.5) | ||
|
|
|
|||||
| White | 156 (61.9) | 150 (59.8) | 130 (66.0) | 123 (62.1) | ||
|
|
|
|||||
| Other | 8 (3.2) | 7 (2.8) | 7 (3.6) | 7 (3.5) | ||
|
| ||||||
| Education | ||||||
|
| ||||||
| ≤High school graduate or GED | 96 (38.1) | 107 (42.6) | .40 | 69 (35.0) | 83 (41.9) | .29 |
|
|
|
|||||
| Associate in arts, associate in science, or technical school | 49 (19.4) | 52 (20.7) | 40 (20.3) | 41 (20.7) | ||
|
|
|
|||||
| College or higher | 107 (42.5) | 92 (36.7) | 88 (44.7) | 74 (37.4) | ||
|
| ||||||
| Annual household income ≥$50 000 | 140 (55.6) | 138 (55.0) | .90 | 112 (56.9) | 96 (48.5) | .10 |
|
| ||||||
| Substance use, No. (%) | ||||||
|
| ||||||
| Any dependence | ||||||
|
| ||||||
| Alcohol | 170 (67.5) | 159 (63.3) | .33 | 134 (68.0) | 133 (67.2) | .86 |
|
| ||||||
| Marijuana | 31 (12.3) | 30 (12.0) | .90 | 26 (13.2) | 23 (11.6) | .63 |
|
| ||||||
| Sedatives | 18 (7.1) | 13 (5.2) | .36 | 17 (8.6) | 12 (6.1) | .33 |
|
| ||||||
| Heroin | 12 (4.8) | 8 (3.1) | .37 | 8 (4.1) | 5 (2.5) | .39 |
|
| ||||||
| Painkillers | 37 (14.7) | 33 (13.1) | .62 | 29 (14.7) | 27 (13.6) | .76 |
|
| ||||||
| Cocaine | 46 (18.3) | 33 (13.2) | .12 | 35 (17.8) | 27 (13.6) | .26 |
|
| ||||||
| Amphetamines | 27 (10.7) | 32 (12.7) | .48 | 24 (12.2) | 23 (11.6) | .86 |
|
| ||||||
| Dependence type | ||||||
|
| ||||||
| Alcohol only | 107 (42.5) | 118 (47.0) | .12 | 81 (41.1) | 96 (48.5) | .24 |
|
|
|
|||||
| Drug only | 61 (24.2) | 67 (26.7) | 49 (24.9) | 49 (24.7) | ||
|
|
|
|||||
| Alcohol and drug | 63 (25.0) | 41 (16.3) | 53 (26.9) | 37 (18.7) | ||
|
|
|
|||||
| Abuse | 21 (8.3) | 25 (10.0) | 14 (7.1) | 16 (8.1) | ||
|
| ||||||
| Mental health, No. (%) | ||||||
|
| ||||||
| Moderate to severe depressiona | 38 (15.1) | 34 (13.5) | .62 | 36 (18.3) | 31 (15.7) | .49 |
|
| ||||||
| Patient activation, mean (SD) | ||||||
|
| ||||||
| Patient Activation Measure score, mean (SD) | 65.2 (16.2) | 64.3 (17.4) | .56 | 63.9 (16.1) | 64.0 (17.4) | .94 |
|
| ||||||
| Access to computer or smartphone, No. (%) | ||||||
|
| ||||||
| Have access | 235 (93.3) | 225 (89.6) | .15 | 186 (94.4) | 177 (89.4) | .07 |
|
| ||||||
| Can access the internet | 237 (94.1) | 232 (62.4) | .47 | 188 (95.4) | 188 (92.9) | .29 |
|
| ||||||
| Can receive email | 233 (92.5) | 228 (90.8) | .51 | 185 (93.9) | 183 (92.4) | .56 |
|
| ||||||
| Patient engagement in health care | ||||||
|
| ||||||
| Ever accessed kp.org, No. (%) | 190 (75.4) | 178 (70.9) | .26 | 152 (77.2) | 142 (71.7) | .22 |
|
| ||||||
| Ever talked with PCP about AOD problems at baseline, No./total No. (%)b | 130/220 (59.1) | 153/218 (70.2) | .02 | 103/172 (59.9) | 132/173 (76.3) | .001 |
Abbreviations: AOD, alcohol and other drug; GED, General Education Development; PCP, primary care physician.
Nine-item Patient Health Questionnaire score of at least 15.
The question was asked only among those who had a Kaiser Permanente health care professional whom the patient considered to be his or her regular or personal physician or nurse practitioner.
Six-Month Outcomes
Patient Activation and Engagement in Health Care
At 6 months, participants in both conditions had higher mean Patient Activation Measure scores than at baseline. More participants in the LINKAGE condition had an increase of at least 3 points, although the difference was not statistically significant (129 of 225 [57.3%] vs 116 of 230 [50.4%], P = .14 among the full sample and 104 of 172 [60.5%] vs 92 of 182 [50.6%], P = .06 among the subsample with psychiatric comorbidity) (Table 2). LINKAGE participants had significantly more patient portal use during the intervention period, and the differences remained significant after the intervention through the 6-month followup. The results from generalized estimating equation overdispersed Poisson models demonstrated that, compared with UC participants, LINKAGE participants showed a 1.53-fold increase in the mean number of log-in days (incidence rate ratio [IRR], 1.53; 95% CI, 1.19–1.97; P = .001). Similar results were found across the following types of patient portal use: the mean number of log-in days for medical advice (IRR, 1.55; 95% CI, 1.13–2.11; P = .006), the mean number of messages sent by a health care professional (IRR, 1.45; 95% CI, 1.08–1.94; P = .02), the mean number of log-in days for laboratory test results review (IRR, 1.92; 95% CI, 1.43–2.56; P < .001), and the mean number of log-in days for laboratory test information (IRR, 1.89; 95% CI, 1.43–2.51; P < .001). Among the subsample with psychiatric comorbidity, those in the LINKAGE condition also had significantly higher use of each activity.
Table 2.
Effects of the LINKAGE Intervention on Patient Activation and Patient Engagement in Health Care
| Variable | 1–6 wk | wk 7 to 6-mo Follow-up | Measure (95% CI) | P Value | ||
|---|---|---|---|---|---|---|
|
|
|
|||||
| LINKAGE | Usual Care | LINKAGE | Usual Care | |||
|
| ||||||
| Among the full sample | (n = 252) | (n = 251) | (n = 225) | (n = 230) | ||
| Patient activation, No. (%) | ||||||
|
| ||||||
| Having a PAM score increase of ≥3 points | NA | NA | 129 (57.3) | 116 (50.4) | 1.32(0.91 to 1.91)a | .14 |
|
| ||||||
| Patient engagement in health care | ||||||
|
| ||||||
| Patient portal use per month, mean (SD) | ||||||
|
| ||||||
| No. of log-in days to kp.org | 2.4 (2.7) | 1.1 (2.0)b | 1.7 (2.4) | 1.1 (1.7)b | 1.53 (1.19 to 1.97)c | .001d |
|
| ||||||
| No. of log-in days for medical advice | 0.8 (1.1) | 0.4 (0.9)b | 0.6 (1.0) | 0.4 (0.8)e | 1.55 (1.13 to 2.11)c | .006 |
|
| ||||||
| No. of messages sent by health care professional | 1.2 (1.9) | 0.7 (1.7)e | 1.1 (1.9) | 0.8 (1.2)e | 1.45 (1.08 to 1.94)c | .02 |
|
| ||||||
| No. of log-in days for laboratory test results review | 0.8 (1.2) | 0.2 (0.5)b | 0.3 (0.5) | 0.2 (0.4)e | 1.92 (1.43 to 2.56)c | <.001 |
|
| ||||||
| No. of log-in days for laboratory test information review | 1.0 (1.4) | 0.3 (0.7)b | 0.4 (0.7) | 0.3 (0.6)e | 1.89 (1.43 to 2.51)c | <.001 |
|
| ||||||
| Talked with PCP about AOD problems at 6-mo follow-up, No./total No. (%)f | NA | NA | 134/190 (70.5) | 103/202 (51.0)b | 2.30 (1.52 to 3.49)a | <.001d |
|
| ||||||
| Addiction treatment length of stay, mean (SD), d | NA | NA | 79.3 (65.7) | 70.9 (64.6) | 8.42 (−3.57 to 20.42)f | .17 |
|
| ||||||
| Among the subsample with psychiatric comorbidity | (n = 197) | (n = 198) | (n = 172) | (n = 182) | ||
|
| ||||||
| Patient activation, No. (%) | ||||||
|
| ||||||
| Having a PAM score increase of ≥3 points | NA | NA | 104 (60.5) | 92 (50.6)h | 1.50 (0.98 to 2.28)a | .06 |
|
| ||||||
| Patient engagement in health care | ||||||
|
| ||||||
| Patient portal use per month, mean (SD) | ||||||
|
| ||||||
| No. of log-in days to kp.org | 2.6 (2.9) | 1.1 (1.9)b | 1.8 (2.5) | 1.2 (1.8)e | 1.55 (1.18 to 2.04)c | .003d |
|
| ||||||
| No. of log-in days for medical advice | 0.8 (1.2) | 0.4 (1.0)b | 0.7 (1.1) | 0.4 (0.8)e | 1.59 (1.13 to 2.24)c | .009 |
|
| ||||||
| No. of messages sent by health care professional | 1.3 (2.0) | 0.8 (1.7)e | 1.2 (2.0) | 0.8 (1.3)h | 1.44 (1.04 to 2.00)c | .03 |
|
| ||||||
| No. of log-in days for laboratory test results review | 0.8 (1.3) | 0.3 (0.6)b | 0.3 (0.5) | 0.2 (0.4) | 1.94 (1.40 to 2.69)c | <.001 |
|
| ||||||
| No. of log-in days for laboratory test information review | 1.0 (1.5) | 0.3 (0.8)b | 0.4 (0.7) | 0.3 (0.6)e | 1.95 (1.42 to 2.67)c | <.001 |
|
| ||||||
| Talked with PCP about AOD problems at 6-mo follow-up, No./total No.f | NA | NA | 99/144 (68.8) | 92/159 (57.9)e | 1.60 (1.00 to 2.57)a | .05 |
|
| ||||||
| Addiction treatment length of stay, mean (SD), d | NA | NA | 80.8 (65.7) | 71.8 (66.3) | 9.06 (−4.75 to 22.87)g | .20 |
Abbreviations: AOD, alcohol and other drug; NA, not applicable; PAM, Patient Activation Measure; PCP, primary care physician.
Odds ratio from the logistic regression model.
P < .001.
Relative risk from the generalized estimating equation Poisson regression model.
P values from analyses with Bonferroni corrections are also significant.
P < .05.
The question was asked only among those who had a Kaiser Permanente health care professional whom the patient considered to be his or her regular or personal physician or nurse practitioner.
Mean difference from the general liner regression model.
P < .10.
LINKAGE participants had twice the odds of having talked with their primary care physician about AOD problems (odds ratio, 2.30; 95% CI, 1.52–3.49; P < .001 among the full sample and odds ratio, 1.60; 95% CI, 1.00–2.57; P = .05 among the subsample with psychiatric comorbidity). No differences were found in addiction treatment length of stay for the full sample or the subsample with psychiatric comorbidity.
AOD Use and Depression Symptoms
Among both the full sample and the subsample with psychiatric comorbidity, LINKAGE participants and UC participants had high AOD abstinence rates at 6 months, with no significant differences between conditions (Table 3). No differences were found for heavy drinking or moderate to severe depression, although the proportion with scores of at least 15 on the 9-item Patient Health Questionnaire dropped by almost half from 15.1% (38 of 252) to 8.0% (18 of 225) for LINKAGE participants and from 13.5% (34 of 251) to 7.0% (16 of 230) for UC participants.
Table 3.
Effects of the LINKAGE Intervention on Alcohol and Other Drug (AOD) Use Outcomes and on Mental Health Outcomes
| Variable | 6-mo Follow-up, No. (%) | Odds Ratioa (95% CI) | P Value | |
|---|---|---|---|---|
| LINKAGE | Usual Care | |||
| Among the full sample | (n = 225) | (n = 230) | ||
| AOD use outcome | ||||
| Total abstinence | 159 (70.7) | 154 (67.0) | 1.17 (0.79–1.75) | .43 |
| Alcohol abstinence | 173 (76.9) | 168 (73.0) | 1.21 (0.79–1.90) | .39 |
| Drug abstinence | 186 (82.7) | 188 (81.7) | 1.07 (0.66–1.72) | .80 |
| Any heavy drinking during the past 30 d | 32 (14.2) | 39 (17.0) | 0.80 (0.48–1.34) | .40 |
| Mental health outcome | ||||
| Moderate to severe depressionb | 18 (8.0) | 16 (7.0) | 1.16 (0.58–2.34) | .67 |
| Among the subsample with psychiatric comorbidity | (n = 172) | (n = 182) | ||
| AOD use outcome | ||||
| Total abstinence | 122 (70.9) | 122 (67.0) | 2.05 (0.70–6.06) | .19 |
| Alcohol abstinence | 134 (77.9) | 135 (74.2) | 1.20 (0.74–1.97) | .46 |
| Drug abstinence | 142 (82.6) | 147 (80.8) | 1.13 (0.66–1.93) | .66 |
| Any heavy drinking during the past 30 d | 22 (12.8) | 34 (18.7) | 0.63 (0.35–1.13) | .12 |
| Mental health outcome | ||||
| Moderate to severe depressionb | 15 (8.7) | 16 (8.8) | 0.99 (0.47–2.07) | .98 |
From the logistic regression model.
Nine-item Patient Health Questionnaire score of at least 15.
Effects of the Number of LINKAGE Sessions and Facilitated Physician Communication
Among LINKAGE participants, those receiving all 6 sessions had higher patient portal use than those receiving fewer sessions. They also had higher alcohol abstinence rates (83.7% [82 of 98] vs 71.7% [91 of 127], P = .03) and total abstinence rates (77.6% [76 of 98] vs 65.4% [83 of 127], P = .05) and longer treatment retention (103.8 vs 60.4 days, P < .001) (Table 4). We did not examine a dose-response effect because, while the sessions built on each other, they each had a unique focus. Participants receiving facilitated physician communication (68.7% [173 of 252]) had significantly higher mean patient portal use during the intervention period than those not receiving facilitated physician communication, and the differences remained significant for the postintervention period except for physician email exchange. More of those receiving facilitated physician communication also reported talking to their physician about AOD problems and had longer treatment retention (92.0 vs 49.3 days, P < .001), better alcohol abstinence (82.9% [131 of 158] vs 62.7% [42 of 67], P < .001), and less heavy drinking (8.9% [14 of 158] vs 26.9% [18 of 67], P < .001). Similar results were found for the subsample with psychiatric comorbidity, although some findings were not statistically significant.
Table 4.
Effects of the LINKAGE Intervention on Patient Activation, Patient Engagement in Health Care, Alcohol and Other Drug (AOD) Use Outcomes, and Mental Health Outcomes Among the LINKAGE Groupa
| Variable | No. of LINKAGE Sessions Attended | P Value | Having a Facilitated PCP Communication | P Value | ||
|---|---|---|---|---|---|---|
|
|
|
|||||
| ≥6 | <6 | Yes | No | |||
| Among the full sample | ||||||
|
| ||||||
| Patient activation, No./total No. (%) | ||||||
|
| ||||||
| Having a PAM score increase of ≥3 points | 62/98 (63.3) | 67/127 (52.8) | .11 | 95/158 (60.1) | 34/67 (50.8) | .19 |
|
| ||||||
| Patient engagement in health care | ||||||
|
| ||||||
| Patient portal use per month, mean (SD) | ||||||
|
| ||||||
| No. of log-in days to kp.org | ||||||
|
| ||||||
| 1–6 wk, out of the baseline sample | 3.1 (3.0) | 1.9 (2.5) | <.001 | 2.9 (3.0) | 1.3 (1.7) | <.001 |
|
| ||||||
| wk 7 to 6-mo follow-up, out of the 6-mo sample | 1.8 (2.5) | 1.6 (2.4) | .49 | 1.9 (2.6) | 1.1 (1.8) | .02 |
|
| ||||||
| No. of log-in days for medical advice | ||||||
|
| ||||||
| 1–6 wk, out of the baseline sample | 1.0 (1.3) | 0.6 (0.9) | .006 | 0.9 (1.2) | 0.5 (0.9) | .01 |
|
| ||||||
| wk 7 to 6-mo follow-up, out of the 6-mo sample | 0.6 (0.9) | 0.6 (1.0) | .76 | 0.7 (1.1) | 0.4 (0.7) | .02 |
|
| ||||||
| No. of log-in days for laboratory test results review | ||||||
|
| ||||||
| 1–6 wk, out of the baseline sample | 1.1 (1.4) | 0.6 (1.0) | <.001 | 1.0 (1.3) | 0.2 (0.5) | <.001 |
|
| ||||||
| wk 7 to 6-mo follow-up, out of the 6-mo sample | 0.3 (0.6) | 0.2 (0.5) | .14 | 0.3 (0.6) | 0.2 (0.3) | .06 |
|
| ||||||
| No. of log-in days for laboratory test information review | ||||||
|
| ||||||
| 1–6 wk, out of the baseline sample | 1.4 (1.6) | 0.7 (1.1) | <.001 | 1.3 (1.5) | 0.3 (0.7) | <.001 |
|
| ||||||
| wk 7 to 6-mo follow-up, out of the 6-mo sample | 0.5 (0.7) | 0.3 (0.6) | .11 | 0.5 (0.8) | 0.2 (0.4) | .02 |
|
| ||||||
| No. of messages sent by health care professional | ||||||
|
| ||||||
| 1–6 wk, out of the baseline sample | 1.4 (2.2) | 1.0 (1.7) | .09 | 1.3 (2.1) | 0.8 (1.4) | .03 |
|
| ||||||
| wk 7 to 6-mo follow-up, out of the 6-mo sample | 1.0 (1.7) | 1.2 (2.0) | .40 | 1.2 (2.0) | 0.8 (1.5) | .13 |
|
| ||||||
| No. of messages sent by patient | ||||||
|
| ||||||
| 1–6 wk, out of the baseline sample | 1.3 (2.1) | 0.8 (1.6) | .02 | 1.1 (2.0) | 0.7 (1.3) | .05 |
|
| ||||||
| wk 7 to 6-mo follow-up, out of the 6-mo sample | 0.8 (1.8) | 1.0 (2.1) | .37 | 1.0 (2.1) | 0.7 (1.5) | .24 |
|
| ||||||
| Talked with PCP about AOD problems at 6-mo follow-up, No./total No. (%) | 62/88 (70.5) | 72/102 (70.6) | .98 | 105/138 (76.1) | 29/52 (55.8) | .006 |
|
| ||||||
| Addiction treatment length of stay, mean (SD), d | 103.8 (61.5) | 60.4 (62.6) | <.001 | 92.0 (64.7) | 49.3 (58.1) | <.001 |
|
| ||||||
| AOD use outcome at 6-mo follow-up, No./total No. (%) | ||||||
|
| ||||||
| Total abstinence | 76/98 (77.6) | 83/127 (65.4) | .05 | 117/158 (74.1) | 42/67 (62.7) | .09 |
|
| ||||||
| Alcohol abstinence | 82/98 (83.7) | 91/127 (71.7) | .03 | 131/158 (82.9) | 42/67 (62.7) | <.001 |
|
| ||||||
| Drug abstinence | 84/98 (85.7) | 102/127 (80.3) | .29 | 130/158 (82.3) | 56/67 (83.6) | .81 |
|
| ||||||
| Any heavy drinking during the past 30 d | 7/98 (7.1) | 25/127 (19.7) | .008 | 14/158 (8.9) | 18/67 (26.9) | <.001 |
|
| ||||||
| Mental health outcome at 6-mo follow-up, No./total No. (%) | ||||||
|
| ||||||
| Moderate to severe depressionb | 5/98 (5.1) | 13/127 (10.2) | .16 | 11/158 (7.0) | 7/67 (10.5) | .38 |
|
| ||||||
| Among the subsample with psychiatric comorbidity | ||||||
|
| ||||||
| Patient activation, No./total No. (%) | ||||||
|
| ||||||
| Having a PAM score increase of ≥3 points | 53/81 (65.4) | 51/91 (56.0) | .21 | 79/124 (63.7) | 25/48 (52.1) | .16 |
|
| ||||||
| Patient engagement in health care | ||||||
|
| ||||||
| Patient portal use per month, mean (SD) | ||||||
|
| ||||||
| No. of log-in days to kp.org | ||||||
|
| ||||||
| 1–6 wk, out of the baseline sample | 3.1 (3.0) | 2.2 (2.7) | .04 | 3.1 (3.1) | 1.5 (1.9) | <.001 |
|
| ||||||
| wk 7 to 6-mo follow-up, out of the 6-mo sample | 1.6 (2.4) | 1.9 (2.6) | .51 | 1.9 (2.7) | 1.4 (1.9) | .21 |
|
| ||||||
| No. of log-in days for medical advice | ||||||
|
| ||||||
| 1–6 wk, out of the baseline sample | 1.0 (1.3) | 0.7 (1.0) | .07 | 0.9 (1.2) | 0.6 (1.0) | .08 |
|
| ||||||
| wk 7 to 6-mo follow-up, out of the 6-mo sample | 0.6 (1.0) | 0.7 (1.1) | .28 | 0.7 (1.2) | 0.5 (0.8) | .16 |
|
| ||||||
| No. of log-in days for laboratory test results review | ||||||
|
| ||||||
| 1–6 wk, out of the baseline sample | 1.1 (1.4) | 0.6 (1.0) | .007 | 1.0 (1.4) | 0.2 (0.5) | <.001 |
|
| ||||||
| wk 7 to 6-mo follow-up, out of the 6-mo sample | 0.3 (0.6) | 0.3 (0.5) | .60 | 0.3 (0.6) | 0.2 (0.4) | .22 |
|
| ||||||
| No. of log-in days for laboratory test information review | ||||||
|
| ||||||
| 1–6 wk, out of the baseline sample | 1.1 (1.7) | 0.7 (1.2) | .004 | 1.3 (1.6) | 0.3 (0.7) | <.001 |
|
| ||||||
| wk 7 to 6-mo follow-up, out of the 6-mo sample | 0.5 (0.7) | 0.4 (0.7) | .62 | 0.5 (0.8) | 0.3 (0.4) | .10 |
|
| ||||||
| No. of messages sent by health care professional | ||||||
|
| ||||||
| 1–6 wk, out of the baseline sample | 1.4 (2.2) | 1.2 (1.8) | .60 | 1.4 (2.2) | 0.9 (1.5) | .12 |
|
| ||||||
| wk 7 to 6-mo follow-up, out of the 6-mo sample | 0.9 (1.6) | 1.4 (2.3) | .11 | 1.3 (2.1) | 1.0 (1.6) | .44 |
|
| ||||||
| No. of messages sent by patient | ||||||
|
| ||||||
| 1–6 wk, out of the baseline sample | 1.3 (2.1) | 0.7 (1.7) | .19 | 1.2 (2.1) | 0.8 (1.5) | .24 |
|
| ||||||
| wk 7 to 6-mo follow-up, out of the 6-mo sample | 0.7 (1.7) | 1.3 (2.3) | .10 | 1.1 (2.2) | 0.9 (1.6) | .64 |
|
| ||||||
| Talked with PCP about AOD problems at 6-mo follow-up, No./total No. (%) | 48/70 (68.6) | 51/74 (68.9) | .96 | 78/106 (73.6) | 21/38 (55.3) | .04 |
|
| ||||||
| Addiction treatment length of stay, mean (SD), d | 100.9 (62.0) | 63.3 (64.2) | <.001 | 93.0 (64.6) | 50.2 (58.7) | <.001 |
|
| ||||||
| AOD use outcome at 6-mo follow-up, No./total No. (%) | ||||||
|
| ||||||
| Total abstinence | 59/80 (73.8) | 63/92 (68.5) | .45 | 91/123 (74.0) | 31/49 (63.3) | .16 |
|
| ||||||
| Alcohol abstinence | 65/80 (81.3) | 69/92 (75.0) | .32 | 103/123 (83.7) | 31/49 (63.3) | .003 |
|
| ||||||
| Drug abstinence | 66/80 (82.5) | 76/92 (82.6) | .99 | 101/123 (82.1) | 41/49 (63.3) | .81 |
|
| ||||||
| Any heavy drinking during the past 30 d | 7/80 (8.8) | 15/92 (16.3) | .14 | 9/123 (7.3) | 13/49 (26.5) | <.001 |
|
| ||||||
| Mental health outcome at 6-mo follow-up, No./total No. (%) | ||||||
|
| ||||||
| Moderate to severe depressionb | 5/80 (6.3) | 10/92 (10.9) | .28 | 9/123 (7.3) | 6/49 (12.2) | .30 |
Abbreviations: PAM, Patient Activation Measure; PCP, primary care physician.
Among the full sample, the baseline sample size was 252, and the 6-month follow-up sample size was 225. Among the subsample with psychiatric comorbidity, the baseline sample size was 197, and the 6-month follow-up sample size was 172.
Nine-item Patient Health Questionnaire score of at least 15.
Discussion
The LINKAGE intervention taught skills to help patients communicate effectively with physicians and engage in their health care using the EHR as a platform. LINKAGE participants had more days of patient portal log-in, including seeking medical advice, receiving messages from primary care physicians, checking on laboratory test results, and reviewing medical information. Participants with psychiatric comorbidity had findings similar to those of the full sample, indicating that the intervention was also beneficial in engaging these complex patients.
However, the intervention did not result in better 6-month AOD or depression outcomes. We note that the LINKAGE intervention did not focus on AOD use or depression, which was the emphasis of the standard treatment program. Abstinence rates were high for both conditions (≥70.0% for both), similar to the results of other trials conducted in this health system.13,42 Depression outcomes also significantly improved for both groups but with no differences between conditions. Six months may not have been long enough to observe any differences in these outcomes given the intensive treatment program. However, by taking better care of their health, we expect that LINKAGE participants will have better outcomes than UC participants over time. Because AOD disorders are chronic health conditions requiring ongoing care,3,45 we also expect that, by engaging patients in their health care, potential service needs will be identified earlier and relapse avoided.36
Another approach to providing services in a separate primary care clinic, the Addiction Health Evaluation and Disease Management (AHEAD) trial, also found no differences in AOD use outcomes.46 A trial that provided facilitated referral to primary care after detoxification demonstrated that patients were more likely to access medical services, but no differences were observed in AOD use outcomes.47 The LINKAGE intervention may best be placed in specialty addiction treatment, where patients can address their AOD problems as part of a larger program and may be more open to thinking about their overall health while also practicing patient engagement activities.
Findings on patient portal use were conservative in not counting the first 6 weeks of treatment. Many patients completed the intervention in 3 weeks, but we extended the analysis during the intervention to 6 weeks to allow for potential missed sessions and makeup sessions. For those who received the full intervention, beneficial effects were more robust, including alcohol abstinence and heavy drinking outcomes. This finding suggests a potential significant effect if the intervention was adopted as part of standard treatment. The LINKAGE intervention was innovative in its use of the EHR to engage patients in health prevention and other services. Our findings suggest that patients receiving addiction treatment are interested in having a role in their health care and in using health information technology.45 The intervention is scalable because EHR use and patient portal use are increasing under the Patient Protection and Affordable Care Act and related incentives.20,23,25,48 The intervention is manual based and relies on the common addiction group therapy format.2 Although patients with AOD disorders often use episodic care rather than comprehensive health services, similar to other patients,4,5 the intervention helped them better connect with their overall health care and improve communication with their physician.
We note that the intervention focused on patients rather than physicians. Physicians often are unaware of their patients’ AOD problems,2 and patients may change health plans or physicians. The patient empowerment and skills in managing health care that were the core elements of the intervention can be used by patients wherever they receive medical care.
Our study had some limitations. It used an off-and-on, non-randomized clinical trial design, in which participant allocation was done by alternation, with different cohorts changing every 3 months over 30 months. Patient allocation was independent of patient characteristics. Most important, randomization would have resulted in contamination between study conditions because patients in both conditions were together during other parts of the standard program. It successfully resulted in similar demographic and clinical baseline characteristics between conditions. The study may have been under powered for examining the effect on patient activation level. It did not include validation with biological specimens because follow-up interviews were conducted by telephone; however, self-reported differences should have been similar for both conditions, and other studies13,49–53 have found high concurrence. Although the study was conducted in an integrated health system with a mature EHR, it provides an excellent laboratory for examining the intervention. By 2014, more than 80% of US primary care physicians had adopted an EHR, and more than half were using all basic EHR functions.21
Conclusions
Every year, more than 3 million US adults enter addiction treatment, and this number will increase with its new status as an essential benefit of patient care.18 Among the adult general population, 3.9% in 2013 met diagnostic criteria for drug use disorders54 and 13.9% for alcohol use disorders.55 These individuals often have co-occurring problems, and their care needs to be integrated with mainstream health care.14 Teaching patients receiving addiction treatment how to use health care may empower them to better engage in their health management. Electronic health record patient portals may be useful in accomplishing this goal. Although the LINKAGE intervention did not achieve short-term differences in AOD and depression outcomes, it will be important to understand if it is helpful in avoiding AOD relapse and in improving overall health.
Acknowledgments
Funding/Support: This study was supported by National Institutes of Health Center Grant P50 DA009253 from the National Institute on Drug Abuse. Dr Weisner was the principal investigator of the LINKAGE Study and received those funds from the center grant.
Role of the Funder/Sponsor: The funding organization had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Conflict of Interest Disclosures: None reported.
Author Contributions: Dr Weisner and Ms Chi had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Weisner, Chi, Ross, Wood, Hinman, Pating, Satre, Sterling.
Acquisition, analysis, or interpretation of data: Weisner, Chi, Lu, Wood, Hinman, Pating, Satre, Sterling.
Drafting of the manuscript: Weisner, Chi, Lu, Ross, Wood, Satre, Sterling.
Critical revision of the manuscript for important intellectual content: Weisner, Ross, Hinman, Pating, Sterling.
Statistical analysis: Weisner, Chi, Lu, Satre.
Obtained funding: Weisner.
Administrative, technical, or material support: Weisner, Ross, Wood, Hinman, Pating, Satre.
Study supervision: Weisner, Hinman, Sterling.
Additional Contributions: We acknowledge the administrative and scientific support of the University of California, San Francisco/National Institute on Drug Abuse Treatment Research Center and its director, Joe Guydish, PhD. Andrea Kline-Simon, MS, and Sujaya Parthasarathy, PhD, provided statistical consultation, and Cynthia Campbell, PhD, contributed additional consultation (all 3 are affiliated with the Division of Research, Kaiser Permanente Northern California, Oakland). We also acknowledge the staff at the Chemical Dependency Recovery Program (Kaiser Permanente Medical Center, San Francisco), particularly the program director Wayne Green, CADC, as well as the support of the addiction medicine chiefs and program directors in the Kaiser Permanente Northern California. None received compensation.
References
- 1.Mertens JR, Lu YW, Parthasarathy S, Moore C, Weisner CM. Medical and psychiatric conditions of alcohol and drug treatment patients in an HMO: comparison with matched controls. Arch Intern Med. 2003;163(20):2511–2517. doi: 10.1001/archinte.163.20.2511. [DOI] [PubMed] [Google Scholar]
- 2.Institute of Medicine. Improving the Quality of Health Care for Mental and Substance-Use Conditions. Washington, DC: National Academies Press; 2006. [PubMed] [Google Scholar]
- 3.McLellan AT, Starrels JL, Tai B, et al. Can substance use disorders be managed using the Chronic Care Model? review and recommendations from a NIDA consensus group. Public Health Rev. 2014;35(2) doi: 10.1007/BF03391707. http://www.journalindex.net/visit.php?j=6676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Young JQ, Kline-Simon AH, Mordecai DJ, Weisner C. Prevalence of behavioral health disorders and associated chronic disease burden in a commercially insured health system: findings of a case-control study. Gen Hosp Psychiatry. 2015;37(2):101–108. doi: 10.1016/j.genhosppsych.2014.12.005. [DOI] [PubMed] [Google Scholar]
- 5.Cederbaum JA, Guerrero EG, Mitchell KR, Kim T. Utilization of emergency and hospital services among individuals in substance abuse treatment. Subst Abuse Treat Prev Policy. 2014;9:16. doi: 10.1186/1747-597X-9-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Smith MW, Stocks C, Santora PB. Hospital readmission rates and emergency department visits for mental health and substance abuse conditions. Community Ment Health J. 2015;51(2):190–197. doi: 10.1007/s10597-014-9784-x. [DOI] [PubMed] [Google Scholar]
- 7.Parthasarathy S, Chi FW, Mertens JR, Weisner C. The role of continuing care in 9-year cost trajectories of patients with intakes into an outpatient alcohol and drug treatment program. Med Care. 2012;50(6):540–546. doi: 10.1097/MLR.0b013e318245a66b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cherpitel CJ, Ye Y. Trends in alcohol- and drug-related emergency department and primary care visits: data from four U.S. national surveys (1995–2010) J Stud Alcohol Drugs. 2012;73(3):454–458. doi: 10.15288/jsad.2012.73.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chi FW, Parthasarathy S, Mertens JR, Weisner CM. Continuing care and long-term substance use outcomes in managed care: early evidence for a primary care–based model. Psychiatr Serv. 2011;62(10):1194–1200. doi: 10.1176/appi.ps.62.10.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mertens JR, Flisher AJ, Satre DD, Weisner CM. The role of medical conditions and primary care services in 5-year substance use outcomes among chemical dependency treatment patients. Drug Alcohol Depend. 2008;98(1–2):45–53. doi: 10.1016/j.drugalcdep.2008.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saitz R, Horton NJ, Larson MJ, Winter M, Samet JH. Primary medical care and reductions in addiction severity: a prospective cohort study. Addiction. 2005;100(1):70–78. doi: 10.1111/j.1360-0443.2005.00916.x. [DOI] [PubMed] [Google Scholar]
- 12.Saitz R, Larson MJ, Horton NJ, Winter M, Samet JH. Linkage with primary medical care in a prospective cohort of adults with addictions in inpatient detoxification: room for improvement. Health Serv Res. 2004;39(3):587–606. doi: 10.1111/j.1475-6773.2004.00246.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weisner C, Mertens J, Parthasarathy S, Moore C, Lu Y. Integrating primary medical care with addiction treatment: a randomized controlled trial. JAMA. 2001;286(14):1715–1723. doi: 10.1001/jama.286.14.1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Compton WM, Blanco C, Wargo EM. Integrating addiction services into general medicine. JAMA. 2015;314(22):2401–2402. doi: 10.1001/jama.2015.12741. [DOI] [PubMed] [Google Scholar]
- 15.Ghitza UE, Tai B. Challenges and opportunities for integrating preventive substance-use-care services in primary care through the Affordable Care Act. J Health Care Poor Underserved. 2014;25(1 suppl):36–45. doi: 10.1353/hpu.2014.0067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beronio K, Glied S, Frank R. How the Affordable Care Act and Mental Health Parity and Addiction Equity Act greatly expand coverage of behavioral health care. J Behav Health Serv Res. 2014;41(4):410–428. doi: 10.1007/s11414-014-9412-0. [DOI] [PubMed] [Google Scholar]
- 17.Subtitle B—Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act of 2008 (HR 1424). 117–129.
- 18.Patient Protection and Affordable Care Act, 42 USC §18001 (2010).
- 19.Ancker JS, Osorio SN, Cheriff A, Cole CL, Silver M, Kaushal R. Patient activation and use of an electronic patient portal. Inform Health Soc Care. 2015;40(3):254–266. doi: 10.3109/17538157.2014.908200. [DOI] [PubMed] [Google Scholar]
- 20.EHR Incentive Program, Centers for Medicare & Medicaid Services. [Accessed January 18, 2016];Eligible professional meaningful use: table of contents: core and menu set objectives: stage 1 (2013 definition) https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/downloads/EP-MU-TOC.pdf. Published July 2014.
- 21.Heisey-Grove D, Danehy LN, Consolazio M, Lynch K, Mostashari F. A national study of challenges to electronic health record adoption and meaningful use. Med Care. 2014;52(2):144–148. doi: 10.1097/MLR.0000000000000038. [DOI] [PubMed] [Google Scholar]
- 22.Jones JB, Weiner JP, Shah NR, Stewart WF. The wired patient: patterns of electronic patient portal use among patients with cardiac disease or diabetes. J Med Internet Res. 2015;17(2):e42. doi: 10.2196/jmir.3157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Office of the National Coordinator for Health Information Technology. [Accessed January 18, 2016];Health IT regulations: meaningful use regulations. http://www.healthit.gov/policy-researchers-implementers/meaningful-use. Published 2013.
- 24.Shimada SL, Brandt CA, Feng H, et al. Personal health record reach in the Veterans Health Administration: a cross-sectional analysis. J Med Internet Res. 2014;16(12):e272. doi: 10.2196/jmir.3751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Druss BG, Ji X, Glick G, von Esenwein SA. Randomized trial of an electronic personal health record for patients with serious mental illnesses. Am J Psychiatry. 2014;171(3):360–368. doi: 10.1176/appi.ajp.2013.13070913. [DOI] [PubMed] [Google Scholar]
- 26.Gustafson DH, McTavish FM, Chih MY, et al. A smartphone application to support recovery from alcoholism: a randomized clinical trial. JAMA Psychiatry. 2014;71(5):566–572. doi: 10.1001/jamapsychiatry.2013.4642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Leveille SG, Huang A, Tsai SB, Allen M, Weingart SN, Iezzoni LI. Health coaching via an internet portal for primary care patients with chronic conditions: a randomized controlled trial. Med Care. 2009;47(1):41–47. doi: 10.1097/MLR.0b013e3181844dd0. [DOI] [PubMed] [Google Scholar]
- 28.Hibbard JH, Mahoney ER, Stock R, Tusler M. Do increases in patient activation result in improved self-management behaviors? Health Serv Res. 2007;42(4):1443–1463. doi: 10.1111/j.1475-6773.2006.00669.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mosen DM, Schmittdiel J, Hibbard J, Sobel D, Remmers C, Bellows J. Is patient activation associated with outcomes of care for adults with chronic conditions? J Ambul Care Manage. 2007;30(1):21–29. doi: 10.1097/00004479-200701000-00005. [DOI] [PubMed] [Google Scholar]
- 30.Remmers C, Hibbard J, Mosen DM, Wagenfield M, Hoye RE, Jones C. Is patient activation associated with future health outcomes and healthcare utilization among patients with diabetes? J Ambul Care Manage. 2009;32(4):320–327. doi: 10.1097/JAC.0b013e3181ba6e77. [DOI] [PubMed] [Google Scholar]
- 31.Mathe N, Johnson ST, Wozniak LA, Majumdar SR, Johnson JA. Alternation as a form of allocation for quality improvement studies in primary healthcare settings: the on-off study design. Trials. 2015;16:375. doi: 10.1186/s13063-015-0904-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 2000. text revision. [Google Scholar]
- 33.Caetano R, Raspberry K. Drinking and DSM-IV alcohol and drug dependence among white and Mexican-American DUI offenders. J Stud Alcohol. 2000;61(3):420–426. doi: 10.15288/jsa.2000.61.420. [DOI] [PubMed] [Google Scholar]
- 34.Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Aff (Millwood) 2013;32(2):207–214. doi: 10.1377/hlthaff.2012.1061. [DOI] [PubMed] [Google Scholar]
- 35.Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004;39(4 pt 1):1005–1026. doi: 10.1111/j.1475-6773.2004.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hibbard JH, Greene J, Shi Y, Mittler J, Scanlon D. Taking the long view: how well do patient activation scores predict outcomes four years later? Med Care Res Rev. 2015;72(3):324–337. doi: 10.1177/1077558715573871. [DOI] [PubMed] [Google Scholar]
- 37.McLellan AT, Kushner H, Metzger D, et al. The fifth edition of the Addiction Severity Index. J Subst Abuse Treat. 1992;9(3):199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- 38.National Institute on Alcohol Abuse and Alcoholism. [Accessed January 18, 2016];Helping patients who drink too much: a clinician’s guide. http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/clinicians_guide.htm. Updated 2005.
- 39.Smith PC, Schmidt SM, Allensworth-Davies D, Saitz R. Primary care validation of a single-question alcohol screening test. J Gen Intern Med. 2009;24(7):783–788. doi: 10.1007/s11606-009-0928-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann. 2002;32(9):509–515. [Google Scholar]
- 42.Weisner C, Mertens J, Parthasarathy S, et al. The outcome and cost of alcohol and drug treatment in an HMO: day hospital versus traditional outpatient regimens. Health Serv Res. 2000;35(4):791–812. [PMC free article] [PubMed] [Google Scholar]
- 43.McCullagh P, Nelder JA. Generalized Linear Models. New York, NY: Chapman & Hall; 1989. [Google Scholar]
- 44.Parthasarathy S, Mertens J, Moore C, Weisner C. Utilization and cost impact of integrating substance abuse treatment and primary care. Med Care. 2003;41(3):357–367. doi: 10.1097/01.MLR.0000053018.20700.56. [DOI] [PubMed] [Google Scholar]
- 45.McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284(13):1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- 46.Saitz R, Cheng DM, Winter M, et al. Chronic care management for dependence on alcohol and other drugs: the AHEAD randomized trial. JAMA. 2013;310(11):1156–1167. doi: 10.1001/jama.2013.277609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Samet JH, Larson MJ, Horton NJ, Doyle K, Winter M, Saitz R. Linking alcohol- and drug-dependent adults to primary medical care: a randomized controlled trial of a multi-disciplinary health intervention in a detoxification unit. Addiction. 2003;98(4):509–516. doi: 10.1046/j.1360-0443.2003.00328.x. [DOI] [PubMed] [Google Scholar]
- 48.Terry K. Patient portal explosion has major health care implications. iHealthBeat. 2013 Feb 12; [Google Scholar]
- 49.Brown J, Kranzler HR, Del Boca FK. Self-reports by alcohol and drug abuse inpatients: factors affecting reliability and validity. Br J Addict. 1992;87(7):1013–1024. doi: 10.1111/j.1360-0443.1992.tb03118.x. [DOI] [PubMed] [Google Scholar]
- 50.Calhoun PS, Sampson WS, Bosworth HB, et al. Drug use and validity of substance use self-reports in veterans seeking help for posttraumatic stress disorder. J Consult Clin Psychol. 2000;68(5):923–927. [PubMed] [Google Scholar]
- 51.Decker SE, Frankforter T, Babuscio T, Nich C, Ball SA, Carroll KM. Assessment concordance and predictive validity of self-report and biological assay of cocaine use in treatment trials. Am J Addict. 2014;23(5):466–474. doi: 10.1111/j.1521-0391.2014.12132.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Napper LE, Fisher DG, Johnson ME, Wood MM. The reliability and validity of drug users’ self reports of amphetamine use among primarily heroin and cocaine users. Addict Behav. 2010;35(4):350–354. doi: 10.1016/j.addbeh.2009.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Weisner C, Ray GT, Mertens JR, Satre DD, Moore C. Short-term alcohol and drug treatment outcomes predict long-term outcome. Drug Alcohol Depend. 2003;71(3):281–294. doi: 10.1016/s0376-8716(03)00167-4. [DOI] [PubMed] [Google Scholar]
- 54.Grant BF, Saha TD, Ruan WJ, et al. Epidemiology of DSM-5 drug use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions–III. JAMA Psychiatry. 2016;73(1):39–47. doi: 10.1001/jamapsychiatry.2015.2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Grant BF, Goldstein RB, Saha TD, et al. Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72(8):757–766. doi: 10.1001/jamapsychiatry.2015.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]