Abstract
Introduction
First trimester ultrasound (US) for anatomy assessment may improve anomaly detection but may also increase overall US utilization. We sought to assess the utility of first trimester US for evaluation of fetal anatomy.
Materials and Methods
A decision analytic model was created to compare first plus second trimester anatomy scans to second trimester anatomy scan alone in 4 populations: general, normal weight women, obese women, and diabetics. Probability estimates were obtained from the literature. Outcomes considered were number of: major structural anomalies detected, number of US performed, and false positive US. Multivariable sensitivity analyses were performed to evaluate the consistency of the model with varying assumptions.
Results
A strategy of first trimester US detected the highest number of anomalies but required more US examinations per anomaly detected. The addition of a first trimester anatomy US was associated with a small increase in false positive US (<10/10,000). In populations with higher anomaly prevalence and lower second trimester US sensitivity (i.e. diabetes, obese), the number of additional US performed per anomaly detected with the first trimester US was fewer than 60.
Discussion
In high-risk populations, a first trimester US in addition to a second trimester US may be a beneficial approach to detecting anomalies.
Keywords: Anatomy ultrasound, first trimester, second trimester, decision analysis, sensitivity
Introduction
Ultrasound to evaluate fetal anatomy at 18–22 weeks is now a routine obstetric practice.[1] The timing of this ultrasound is typically chosen in order to balance the ability to visualize structures and complete the scan in one appointment, but this may delay the diagnosis of some anomalies. With advances in technical skill and ultrasound technology, sonography in the first trimester to evaluate fetal anatomy has become a feasible option and even routine in some institutions.[2–5] Anatomical surveys can be completed during this time period with the use of transabdominal and transvaginal probes in up to 82% of subjects.[6] A recent systematic review and meta-analysis demonstrated an overall detection rate of fetal anomalies of 51% at 11–14 weeks gestation,[7] although costs and benefits of this practice have not been evaluated.
While it cannot supplant the second-trimester scan, a first trimester ultrasound for anatomy may supplement the mid-trimester scan by allowing identification of key anatomical features early in pregnancy, leaving the second trimester scan to target features that are not yet present or identifiable in the first trimester. This may be particularly beneficial in populations at high risk for fetal anomalies (e.g. pregestational diabetics) or in populations where second trimester ultrasound is technically difficult, such as in obese women.
On the other hand, initiating anatomy scans in the first trimester will necessitate an additional ultrasound visit, expertise, and expense. Unique features of first trimester anatomy compared to second trimester anatomy may be misdiagnosed as a fetal anomaly,[1,8] increasing the chances of a false positive diagnosis. Additionally, since some normal fetal structures (e.g. the cerebellar vermis) are not fully formed until the second trimester, a reassuring first trimester scan will be unable to exclude abnormalities in these structures.
Studies of first trimester anatomy scans have largely focused on the ability to visualize anatomical structures, optimal timing of the scan, optimal scanning technique (transabdominal versus transvaginal) and the sensitivity for anomaly detection.[6,9–22] With mounting evidence that first trimester anatomy scans are technically feasible and have a clinically useful sensitivity, it is important to understand for which populations a first trimester anatomy scan is an appropriate strategy for prenatal diagnosis. Therefore, we sought to assess the utility of first trimester ultrasound, in terms of additional anomalies detected per additional ultrasound.
Materials and Methods
We created a decision analytic model based on a systematic literature review to compare a strategy of first trimester anatomy scan followed by second trimester anatomy scan to a strategy of second trimester anatomy scan alone (Figure 1). Outcomes assessed included the number of major structural fetal anomalies detected (defined as a lethal anomaly or an anomaly requiring surgery; genetic syndromes without structural anomalies were not considered in this analysis), the number of anatomy scans performed, and the number of false positive results. The decision analytic model was used to analyze the utility of first trimester anatomy scan in 4 populations: a general unselected obstetric, normal weight women, obese women, and women with pregestational diabetes.
Figure 1.
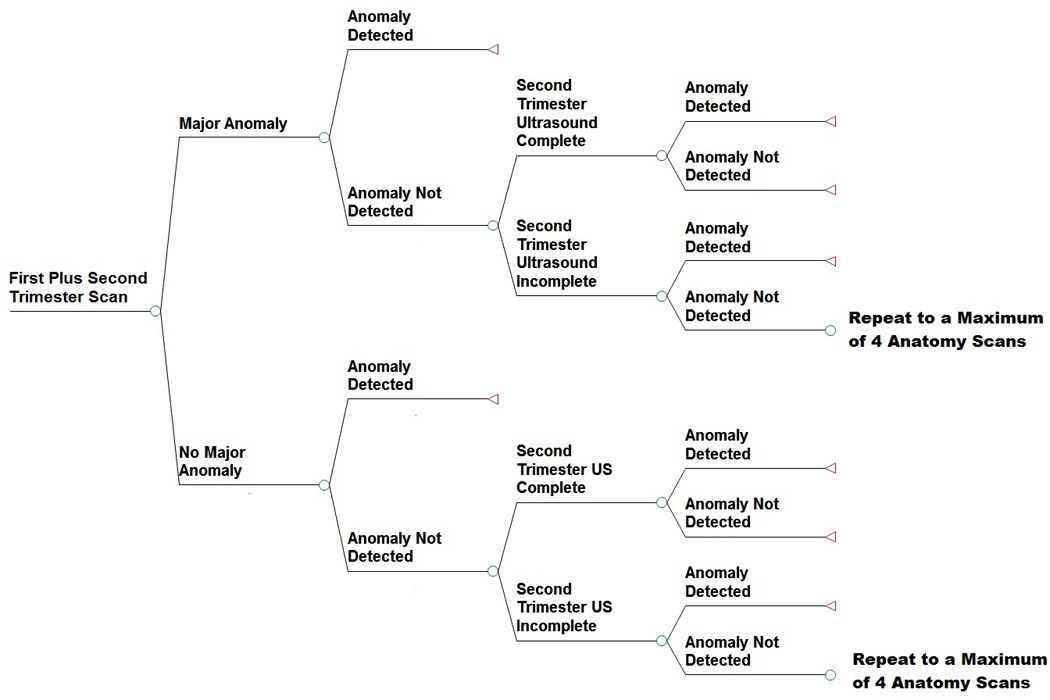
Decision Analytic Model
A structural fetal anomaly was considered detected if it was diagnosed on either the first or second trimester anatomy scan. If no structural fetal anomaly was detected on the first trimester ultrasound, it was assumed the subject would undergo a second trimester anatomy scan. In the model, the second trimester anatomy scan was repeated until a major structural fetal anomaly was detected or all components of an anatomy scan were visualized (i.e. a complete anatomy scan), with a maximum of 4 anatomic surveys permitted after the first trimester scan. Given the short time frame in which to perform a first trimester anatomy scan, we assumed that a first trimester anatomy scan would be performed only once.
We conducted a systematic literature review searching the PubMed database of English articles using the MeSH terms “Ultrasonography, Prenatal,” “Prenatal Diagnosis,” “Echocardiography,” “Congenital Abnormalities,” and “Obesity.” These terms were also searched as keywords in PubMed. Articles considered for review were randomized control trials, prospective cohorts, retrospective cohorts, and systematic reviews and meta-analyses that reported the sensitivity and specificity of first and second trimester anatomy scans for detecting major fetal structural anomalies. Point estimates for the incidence of fetal anomalies, test characteristics (sensitivity, specificity), and completion rates for anatomic surveys are shown in Table 1. Studies reporting the sensitivity and specificity of ultrasounds performed for anatomy at 12–15 weeks were considered first trimester and studies reporting the sensitivity of ultrasounds for anatomy at 16–20 weeks were considered for second trimester. Reports of the sensitivity of first trimester ultrasounds for nuchal thickness for the purposes of genetic screening were not considered in the sensitivity and specificity of first trimester anatomy scans.
Table 1.
| Base Case | Range | Reference | |
|---|---|---|---|
| Incidence of Fetal Anomalies | |||
| General | 0.03 | 0.02–0.08 | Abu-Rustum[9] Baronciani[29] Becker[20] Callen[1] Carvalho[12] Chen[14] Crane[30] Hildebrand[31] Kontopoulos[3] Levi[32] McAuliffe[33] Novotna[34] Oztekin[35] Papp[36] Saltvedt[27] Whitworth[37] |
| Normal Weight | 0.0209 | 0.0076–0.0245 | Biggio[38] Dashe[39] Whitworth[37] |
| Obese | 0.055 | 0.055–0.111 | Anderson[40] Biggio[38] Callaway[41] Dashe[39] Naeye[42] Moore[43] Quiesser-Luft[44] Stothard[45] Watkins[46] Watkins[47] |
| Diabetic | 0.14 | 0.14–0.18 | Anderson[40] Biggio[38] Chung[48] Dashe[39] Moore[43] |
| Sensitivity of First Trimester Anatomy | |||
| For All Populations | 0.51 | 0.2–0.837 | Abu-Rustum[9] Becker[20] Carvalho[12] Cedegren[13] Chen[14] D’Ottavio[24] Ebrashy[6] Hernadi[49] Ileiscu[15] Lim[17,35] Novotna[34] Oztekin[35] Pilalis[26] Rossi[7] Saltvedt[27] Souka[50] Srisupundit[18] Syngelaki[22] Weiner[51] Whitlow[52] |
| Specificity of First Trimester Anatomy | |||
| For All Populations | 0.9993 | 0.99–0.999 | Abu-Rustum[9] Hernadi[49] Iliescu[15] Souka[53] Weiner[51] Whitlow[52] |
| Sensitivity of Second Trimester Anatomy Scan – Complete | |||
| General Population | 0.447 | 0.15–0.853 | Baronciani[29] Best[54] Carvalho[12] Crane[30] Dashe[39] Hildebrand[31] Levi[32] McAuliffe[33] Oztekin[35] Saari-Kamppainen[55] Saltvedt[27] Tabor[56] Whitworth[37] Whitlow[52] |
| Normal Weight | 0.66 | 0.3–0.97 | Best[54] Dashe[39] Hildebrand[31] Tabor[56] |
| Obese | 0.42 | 0.25–0.48 | Best[54] Dashe[39] Hildebrand[31] Tabor[56] |
| Diabetic | 0.38 | 0.35–0.38 | Dashe[39] Miller[57] |
| Sensitivity of Second Trimester Anatomy Scan - Incomplete | |||
| For All Populations | 0.2*Sensitivity of Completed Scan | Local Data | |
| Specificity of Second Trimester Anatomy Scan | |||
| For All Populations | 0.999 | 0.99–0.999 | Abu-Rustum[9] Dashe[39] Levi[32] Saari-Kamppainen[55] |
| Completion of Second Trimester Anatomy Scan – First Attempt | |||
| General Population | 0.728 | 0.672–0.779 | Dashe[58] Fuchs[59] Phatak[60] Thornburg[61] |
| Normal Weight | 0.817 | 0.696–0.905 | Dashe[58] Fuchs[59] Phatak[60] Thornburg[61] Tsai[62] |
| Obese | 0.704 | 0.639–0.763 | Chung[63] Dashe[58] Fuchs[59] Tsai[62] Thornburg[61] |
| Diabetic | 0.728 | 0.672–0.779 | Fuchs[59] |
| Completion of Second Trimester Anatomy Scan – Second Attempt | |||
| General | 0.844 | 0.744–0.917 | Fuchs[59] |
| Normal Weight | 0.999 | 0.715–0.99 | Chung[63] Fuchs[59] Tsai[62] |
| Obese | 0.818 | 0.704–0.902 | Chung[63] Fuchs Tsai[62] |
| Diabetic | 0.844 | 0.744–0.917 | Fuchs[59] |
| Completion of Second Trimester Anatomy Scan – Third & Fourth Attempt | |||
| General | 0.999 | 0.99–0.9999 | Fuchs[59] |
| Normal Weight | 0.999 | 0.99–0.9999 | Fuchs[59] |
| Obese | 0.999 | 0.99–0.9999 | Fuchs[59] |
| Diabetic | 0.999 | 0.99–0.9999 | Fuchs[59] |
To address uncertainty regarding several of the baseline assumptions and probability estimates, sensitivity analyses were performed varying estimates of probabilities across their plausible ranges, alone and in combination (Table 1).
All computations were performed using TreeAge Pro Software, 2014, Williamstown, MA. As no human subjects were involved, institutional review board approval was not obtained.
Results
In each of the 4 populations considered (general/unselected, normal weight, obese, and pregestational diabetics), a strategy of first trimester anatomy followed by second trimester scan detected the highest number of anomalies per 10,000 pregnancies (Table 2). However, this strategy was also associated with an increase in the number of anatomy scans performed per anomaly detected as well as small increase in the number of false positive ultrasounds (i.e. report of a major structural anomaly when none existed).
Table 2.
Results of Decision Analytic Model, per 10,000 Pregnancies
| Anomalies Detected |
Number of Anatomy Scans |
False Positive USs |
Number of Additional Anatomy Scans per Anomaly Detected |
|
|---|---|---|---|---|
| General Population | ||||
| First + Second Trimester | 240 | 22,927 | 20 | 110 |
| Second Trimester | 151 | 13,132 | 13 | |
| Normal Weight Population | ||||
| First + Second Trimester | 194 | 21,693 | 18 | 233 |
| Second Trimester | 151 | 11,825 | 12 | |
| Obese Population | ||||
| First + Second Trimester | 532 | 23,065 | 134 | 58 |
| Second Trimester | 367 | 13,443 | 127 | |
| Diabetic Population | ||||
| First + Second Trimester | 1002 | 22,177 | 17 | 21 |
| Second Trimester | 564 | 13,104 | 11 | |
In one-, two-, and three-way sensitivity analyses, across the specified point estimate ranges, the approach of a first trimester US followed by a second trimester US detected the highest number of fetal anomalies. These results were not sensitive to the prevalence of anomalies, the sensitivity and specificity of first trimester anatomy scan, the sensitivity and specificity of second trimester anatomy scan, or completion rates of second trimester anatomy scans.
The number of additional ultrasounds performed for every additional anomaly detected varied based on the prevalence of anomalies (Figure 2). In the lowest risk population considered, normal weight women, an additional 233 anatomy scans were performed for every major structural anomaly detected. Conversely, in the highest risk population, pregestational diabetes, an additional 21 scans were performed for every major structural anomaly detected.
Figure 2.
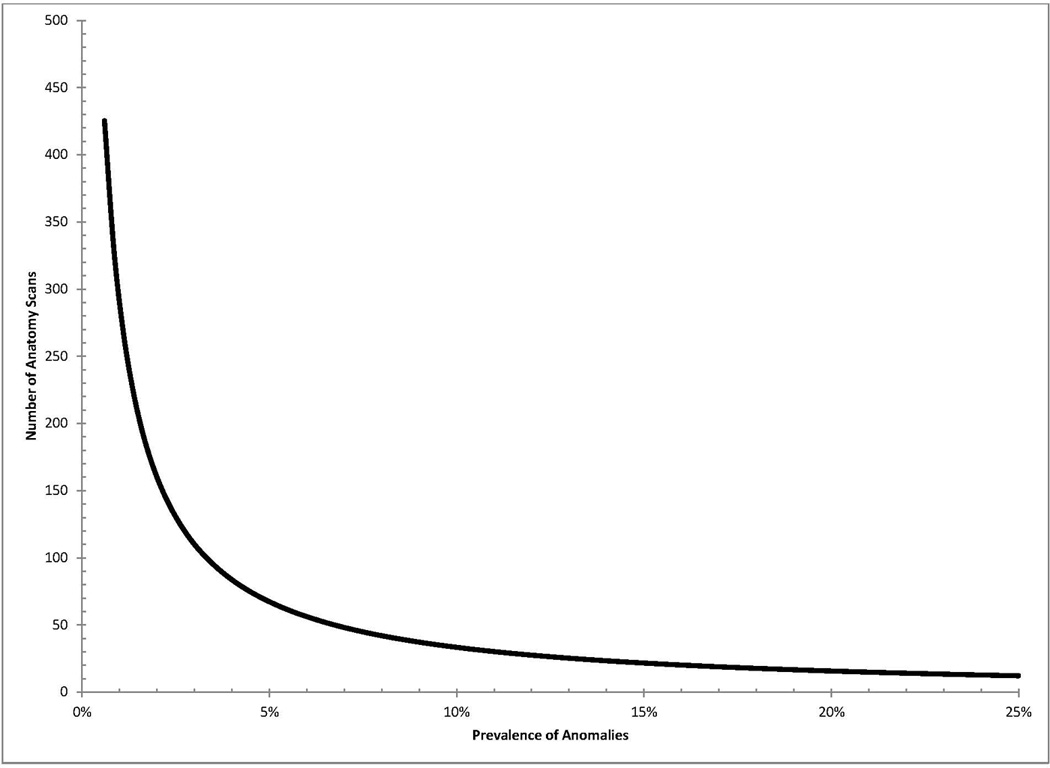
Number of Anatomy Scans Needed to Detect One Anomaly
Discussion
Initiating anatomy scans in the first trimester may increase the detection of fetal anomalies; however, in the overall and normal weight populations (≤5% prevalence of fetal anomalies), excessive numbers of additional scans are needed to detect a single additional anomaly. A strategy of first trimester anatomy scans may therefore be most appropriate only in populations at high risk for fetal anomalies (>5% prevalence of fetal anomalies).
We did not assess costs in this study for several reasons. First, as we were considering any congenital anomaly, the lifetime costs of care and quality of life were impossible to accurately estimate in the model, as these vary significantly with the type of defect. Additionally, the rate of termination and the impact of prenatal diagnosis on outcomes also vary significantly with the type of defect. However, the average Medicare National Fee for a level 2 ultrasound is $138 (range $68–257). Thus in the diabetic population, where only an additional 21 ultrasounds are required to diagnose one anomaly, an additional $2,898 would be required to diagnose one additional anomaly. Given that the average hospital cost per child in the first year of life with a birth defect is estimated approximately $78,000 (or six times the cost of a newborn with no birth defect), first trimester ultrasound could lead to significant cost-savings even if only a small percentage of diagnoses led to pregnancy termination.[23] Additionally, prenatal diagnosis may lead to delivery in tertiary care centers, thus improving immediate neonatal outcomes and improving quality of life for affected infants and their parents.
The majority of studies examining the sensitivity of first trimester anatomy scans that we identified were observational cohorts where an attempted anatomy scan was performed in both the first and second trimester.[6,14,17,24–26] Although these studies provide a reasonable assessment of the sensitivity and specificity of first trimester ultrasound, a direct comparison of first and second trimester anatomy scans cannot be reasonably made due to the bias introduced by presumed provider knowledge of the results of the first trimester scan when performing the second trimester scan.
We identified only one randomized control trial of first versus second trimester anatomy scan; in this study, the detection of major fetal anomalies, including heart defects, was not significantly different at the two time points.[27,28] In this trial, subjects assigned to a first trimester anatomy scan did not routinely undergo a second trimester scan. However, most authors recommend performing the second trimester ultrasound even when the first trimester anatomy scan is completed due to the fact that some components of fetal anatomy do not form until the second trimester and this may partly explain the results.
Some limitations of our model must be noted. First of all, we assessed a very broad category of major structural fetal anomalies. Because of this broad designation, we did not consider outcomes such as stillbirth and termination. This would likely have minimal impact on the number of ultrasounds performed per anomaly since the model ended after the diagnosis of an anomaly (i.e. once an anomaly was diagnosed, no further anatomy scans would be performed in the model); nevertheless, this did prevent us from considering costs in our analysis, as early termination of pregnancy is less costly than a late termination or a term birth. Secondly, we considered the prevalence of anomalies at birth as this is the statistic most commonly reported in the literature. Due to miscarriages and fetal deaths, the incidence of anomalies at birth may be different from the incidence at the time of first and second trimester scan. Consequently, the first trimester scan may actually diagnose anomalies that would have been missed if only a second trimester scan was performed due to an intervening miscarriage. Also, we did not consider the possible increase in invasive testing that may be associated with an increase in prenatal diagnosis of major structural anomalies. This may increase chorionic villous sampling or amniocentesis uptake depending on the timing of ultrasound and the anomaly diagnosed; increased invasive testing may be associated with increased costs of prenatal diagnosis and increased procedure-related pregnancy losses.
Finally, the sensitivity of first trimester ultrasound for anomalies has not been extensively studied in some populations. As such, we assumed that sensitivity was the same in each population, which may not be true. For example, we assumed that the sensitivity of first trimester ultrasound was the same in obese and in normal weight women. In reality, obesity may result in a decreased sensitivity in the first trimester similar to as in the second trimester. On the other hand, first trimester anatomy scan may still be beneficial in the obese population if a transvaginal probe is used before the fetus and uterus have risen out of the pelvis.
In sum, this decision analysis to compare a strategy of first and second trimester anatomy scan to only second trimester anatomy scan suggests that more anomalies will be diagnosed by initiating anatomy scans in the first trimester. However, in low risk populations, a significant number of additional anatomy scans will be required. As the incidence of anomalies increases, the number of additional anatomy scans per anomaly decreases, assuming that the sensitivity of first trimester anatomy scan is not significantly reduced. Randomized control trials of first trimester anatomy scan in high risk populations, such as obese women and pregestational diabetics, are needed to determine the most effective strategy.
Acknowledgments
Dr. Harper is supported by K12HD001258-13, PI WW Andrews, which partially supports this work.
Footnotes
The authors report no conflict of interest.
Abstract presented as a poster at The Pregnancy Meeting, Society for Maternal-Fetal Medicine, February 5, 2015
References
- 1.Callen PW. Ultrasonography in obstetrics and gynecology. 5th. Philadelphia: Saunders Elsevier; 2008. [Google Scholar]
- 2.Dugoff L. Ultrasound diagnosis of structural abnormalities in the first trimester. Prenatal diagnosis. 2002;22:316–320. doi: 10.1002/pd.309. [DOI] [PubMed] [Google Scholar]
- 3.Kontopoulos E, Odibo A, Wilson RD. Current controversies in prenatal diagnosis 2: Are we ready to screen for fetal anomalies with first trimester ultrasound? Prenatal diagnosis. 2013;33:9–12. doi: 10.1002/pd.4030. [DOI] [PubMed] [Google Scholar]
- 4.Rossi AC, Prefumo F. Accuracy of ultrasonography at 11–14 weeks of gestation for detection of fetal structural anomalies: A systematic review. Obstetrics and gynecology. 2013 doi: 10.1097/AOG.0000000000000015. [DOI] [PubMed] [Google Scholar]
- 5.Salomon LJ, Alfirevic Z, Bilardo CM, Chalouhi GE, Ghi T, Kagan KO, Lau TK, Papageorghiou AT, Raine-Fenning NJ, Stirnemann J, Suresh S, Tabor A, Timor-Tritsch IE, Toi A, Yeo G International Society of Ultrasound in O. Isuog practice guidelines: Performance of first-trimester fetal ultrasound scan. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2013;41:102–113. doi: 10.1002/uog.12342. [DOI] [PubMed] [Google Scholar]
- 6.Ebrashy A, El Kateb A, Momtaz M, El Sheikhah A, Aboulghar MM, Ibrahim M, Saad M. 13–14-week fetal anatomy scan: A 5-year prospective study. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2010;35:292–296. doi: 10.1002/uog.7444. [DOI] [PubMed] [Google Scholar]
- 7.Rossi AC, Prefumo F. Accuracy of ultrasonography at 11–14 weeks of gestation for detection of fetal structural anomalies: A systematic review. Obstetrics and gynecology. 2013;122:1160–1167. doi: 10.1097/AOG.0000000000000015. [DOI] [PubMed] [Google Scholar]
- 8.Woodward PJ. Obstetrics. 2nd. Salt Lake City, Utah: Amirsys; 2011. Diagnostic imaging. [Google Scholar]
- 9.Abu-Rustum RS, Daou L, Abu-Rustum SE. Role of first-trimester sonography in the diagnosis of aneuploidy and structural fetal anomalies. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2010;29:1445–1452. doi: 10.7863/jum.2010.29.10.1445. [DOI] [PubMed] [Google Scholar]
- 10.Achiron R, Weissman A, Rotstein Z, Lipitz S, Mashiach S, Hegesh J. Transvaginal echocardiographic examination of the fetal heart between 13 and 15 weeks' gestation in a low-risk population. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 1994;13:783–789. doi: 10.7863/jum.1994.13.10.783. [DOI] [PubMed] [Google Scholar]
- 11.Borrell A, Robinson JN, Santolaya-Forgas J. Clinical value of the 11- to 13+6-week sonogram for detection of congenital malformations: A review. American journal of perinatology. 2011;28:117–124. doi: 10.1055/s-0030-1263302. [DOI] [PubMed] [Google Scholar]
- 12.Carvalho MH, Brizot ML, Lopes LM, Chiba CH, Miyadahira S, Zugaib M. Detection of fetal structural abnormalities at the 11–14 week ultrasound scan. Prenatal diagnosis. 2002;22:1–4. doi: 10.1002/pd.200. [DOI] [PubMed] [Google Scholar]
- 13.Cedergren M, Selbing A. Detection of fetal structural abnormalities by an 11–14-week ultrasound dating scan in an unselected swedish population. Acta obstetricia et gynecologica Scandinavica. 2006;85:912–915. doi: 10.1080/00016340500448438. [DOI] [PubMed] [Google Scholar]
- 14.Chen M, Lam YH, Lee CP, Tang MH. Ultrasound screening of fetal structural abnormalities at 12 to 14 weeks in hong kong. Prenatal diagnosis. 2004;24:92–97. doi: 10.1002/pd.798. [DOI] [PubMed] [Google Scholar]
- 15.Iliescu D, Tudorache S, Comanescu A, Antsaklis P, Cotarcea S, Novac L, Cernea N, Antsaklis A. Improved detection rate of structural abnormalities in the first trimester using an extended examination protocol. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2013;42:300–309. doi: 10.1002/uog.12489. [DOI] [PubMed] [Google Scholar]
- 16.Khalil A, Nicolaides KH. Fetal heart defects: Potential and pitfalls of first-trimester detection. Seminars in fetal & neonatal medicine. 2013;18:251–260. doi: 10.1016/j.siny.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 17.Lim J, Whittle WL, Lee YM, Ryan G, Van Mieghem T. Early anatomy ultrasound in women at increased risk of fetal anomalies. Prenatal diagnosis. 2013;33:863–868. doi: 10.1002/pd.4145. [DOI] [PubMed] [Google Scholar]
- 18.Srisupundit K, Tongsong T, Sirichotiyakul S, Chanprapaph P. Fetal structural anomaly screening at 11–14 weeks of gestation at maharaj nakorn chiang mai hospital. Journal of the Medical Association of Thailand = Chotmaihet thangphaet. 2006;89:588–593. [PubMed] [Google Scholar]
- 19.Volpe P, Ubaldo P, Volpe N, Campobasso G, De Robertis V, Tempesta A, Volpe G, Rembouskos G. Fetal cardiac evaluation at 11–14 weeks by experienced obstetricians in a low-risk population. Prenatal diagnosis. 2011;31:1054–1061. doi: 10.1002/pd.2831. [DOI] [PubMed] [Google Scholar]
- 20.Becker R, Wegner RD. Detailed screening for fetal anomalies and cardiac defects at the 11–13-week scan. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2006;27:613–618. doi: 10.1002/uog.2709. [DOI] [PubMed] [Google Scholar]
- 21.Moon-Grady A, Shahanavaz S, Brook M, Rodriguez H, Hornberger LK. Can a complete fetal echocardiogram be performed at 12 to 16 weeks' gestation? Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography. 2012;25:1342–1352. doi: 10.1016/j.echo.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 22.Syngelaki A, Chelemen T, Dagklis T, Allan L, Nicolaides KH. Challenges in the diagnosis of fetal non-chromosomal abnormalities at 11–13 weeks. Prenatal diagnosis. 2011;31:90–102. doi: 10.1002/pd.2642. [DOI] [PubMed] [Google Scholar]
- 23.Health; RIDoP. Health; RIDoP. Providence, Rhode Island: 2015. Rhode island birth defects data book 2014. [Google Scholar]
- 24.D'Ottavio G, Mandruzzato G, Meir YJ, Rustico MA, Fischer-Tamaro L, Conoscenti G, Natale R. Comparisons of first and second trimester screening for fetal anomalies. Annals of the New York Academy of Sciences. 1998;847:200–209. doi: 10.1111/j.1749-6632.1998.tb08941.x. [DOI] [PubMed] [Google Scholar]
- 25.Persico N, Moratalla J, Lombardi CM, Zidere V, Allan L, Nicolaides KH. Fetal echocardiography at 11–13 weeks by transabdominal high-frequency ultrasound. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2011;37:296–301. doi: 10.1002/uog.8934. [DOI] [PubMed] [Google Scholar]
- 26.Pilalis A, Basagiannis C, Eleftheriades M, Faros E, Troukis E, Armelidou E, Papastefanou I, Souka AP. Evaluation of a two-step ultrasound examination protocol for the detection of major fetal structural defects. The journal of maternal-fetal & neonatal medicine : the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstet. 2012;25:1814–1817. doi: 10.3109/14767058.2012.664199. [DOI] [PubMed] [Google Scholar]
- 27.Saltvedt S, Almstrom H, Kublickas M, Valentin L, Grunewald C. Detection of malformations in chromosomally normal fetuses by routine ultrasound at 12 or 18 weeks of gestation-a randomised controlled trial in 39,572 pregnancies. BJOG : an international journal of obstetrics and gynaecology. 2006;113:664–674. doi: 10.1111/j.1471-0528.2006.00953.x. [DOI] [PubMed] [Google Scholar]
- 28.Westin M, Saltvedt S, Bergman G, Kublickas M, Almstrom H, Grunewald C, Valentin L. Routine ultrasound examination at 12 or 18 gestational weeks for prenatal detection of major congenital heart malformations? A randomised controlled trial comprising 36,299 fetuses. BJOG : an international journal of obstetrics and gynaecology. 2006;113:675–682. doi: 10.1111/j.1471-0528.2006.00951.x. [DOI] [PubMed] [Google Scholar]
- 29.Baronciani D, Scaglia C, Corchia C, Torcetta F, Mastroiacovo P. Ultrasonography in pregnancy and fetal abnormalities: Screening or diagnostic test? Ipimc 1986–1990 register data. Indagine policentrica italiana sulle malformazioni congenite. Prenatal diagnosis. 1995;15:1101–1108. doi: 10.1002/pd.1970151204. [DOI] [PubMed] [Google Scholar]
- 30.Crane JP, LeFevre ML, Winborn RC, Evans JK, Ewigman BG, Bain RP, Frigoletto FD, McNellis D. A randomized trial of prenatal ultrasonographic screening: Impact on the detection, management, and outcome of anomalous fetuses. The radius study group. American journal of obstetrics and gynecology. 1994;171:392–399. doi: 10.1016/s0002-9378(94)70040-0. [DOI] [PubMed] [Google Scholar]
- 31.Hildebrand E, Gottvall T, Blomberg M. Maternal obesity and detection rate of fetal structural anomalies. Fetal Diagn Ther. 2013;33:246–251. doi: 10.1159/000343219. [DOI] [PubMed] [Google Scholar]
- 32.Levi S, Schaaps JP, De Havay P, Coulon R, Defoort P. End-result of routine ultrasound screening for congenital anomalies: The belgian multicentric study 1984–92. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 1995;5:366–371. doi: 10.1046/j.1469-0705.1995.05060366.x. [DOI] [PubMed] [Google Scholar]
- 33.McAuliffe FM, Fong KW, Toi A, Chitayat D, Keating S, Johnson JA. Ultrasound detection of fetal anomalies in conjunction with first-trimester nuchal translucency screening: A feasibility study. American journal of obstetrics and gynecology. 2005;193:1260–1265. doi: 10.1016/j.ajog.2005.06.075. [DOI] [PubMed] [Google Scholar]
- 34.Novotna M, Haslik L, Svabik K, Zizka Z, Belosovicova H, Brestak M, Calda P. Detection of fetal major structural anomalies at the 11–14 ultrasound scan in an unselected population. Ceska gynekologie / Ceska lekarska spolecnost J Ev Purkyne. 2012;77:330–335. [PubMed] [Google Scholar]
- 35.Oztekin O, Oztekin D, Tinar S, Adibelli Z. Ultrasonographic diagnosis of fetal structural abnormalities in prenatal screening at 11–14 weeks. Diagnostic and interventional radiology (Ankara, Turkey) 2009;15:221–225. [PubMed] [Google Scholar]
- 36.Papp Z, Toth-Pal E, Papp C, Toth Z, Szabo M, Veress L, Torok O. Impact of prenatal mid-trimester screening on the prevalence of fetal structural anomalies: A prospective epidemiological study. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 1995;6:320–326. doi: 10.1046/j.1469-0705.1995.06050320.x. [DOI] [PubMed] [Google Scholar]
- 37.Whitworth M, Bricker L, Neilson JP, Dowswell T. Ultrasound for fetal assessment in early pregnancy. The Cochrane database of systematic reviews. 2010:CD007058. doi: 10.1002/14651858.CD007058.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Biggio JR, Jr, Chapman V, Neely C, Cliver SP, Rouse DJ. Fetal anomalies in obese women: The contribution of diabetes. Obstetrics and gynecology. 2010;115:290–296. doi: 10.1097/AOG.0b013e3181c9b8c3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dashe JS, McIntire DD, Twickler DM. Effect of maternal obesity on the ultrasound detection of anomalous fetuses. Obstetrics and gynecology. 2009;113:1001–1007. doi: 10.1097/AOG.0b013e3181a1d2f5. [DOI] [PubMed] [Google Scholar]
- 40.Anderson JL, Waller DK, Canfield MA, Shaw GM, Watkins ML, Werler MM. Maternal obesity, gestational diabetes, and central nervous system birth defects. Epidemiology. 2005;16:87–92. doi: 10.1097/01.ede.0000147122.97061.bb. [DOI] [PubMed] [Google Scholar]
- 41.Callaway LK, Prins JB, Chang AM, McIntyre HD. The prevalence and impact of overweight and obesity in an australian obstetric population. The Medical journal of Australia. 2006;184:56–59. doi: 10.5694/j.1326-5377.2006.tb00115.x. [DOI] [PubMed] [Google Scholar]
- 42.Naeye RL. Maternal body weight and pregnancy outcome. The American journal of clinical nutrition. 1990;52:273–279. doi: 10.1093/ajcn/52.2.273. [DOI] [PubMed] [Google Scholar]
- 43.Moore LL, Singer MR, Bradlee ML, Rothman KJ, Milunsky A. A prospective study of the risk of congenital defects associated with maternal obesity and diabetes mellitus. Epidemiology. 2000;11:689–694. doi: 10.1097/00001648-200011000-00013. [DOI] [PubMed] [Google Scholar]
- 44.Queisser-Luft A, Kieninger-Baum D, Menger H, Stolz G, Schlaefer K, Merz E. Does maternal obesity increase the risk of fetal abnormalities? Analysis of 20,248 newborn infants of the mainz birth register for detecting congenital abnormalities. Ultraschall in der Medizin (Stuttgart, Germany : 1980) 1998;19:40–44. doi: 10.1055/s-2007-1000457. [DOI] [PubMed] [Google Scholar]
- 45.Stothard KJ, Tennant PW, Bell R, Rankin J. Maternal overweight and obesity and the risk of congenital anomalies: A systematic review and meta-analysis. Jama. 2009;301:636–650. doi: 10.1001/jama.2009.113. [DOI] [PubMed] [Google Scholar]
- 46.Watkins ML, Scanlon KS, Mulinare J, Khoury MJ. Is maternal obesity a risk factor for anencephaly and spina bifida? Epidemiology. 1996;7:507–512. [PubMed] [Google Scholar]
- 47.Watkins ML, Botto LD. Maternal prepregnancy weight and congenital heart defects in offspring. Epidemiology. 2001;12:439–446. [PubMed] [Google Scholar]
- 48.Chung CS, Myrianthopoulos NC. Factors affecting risks of congenital malformations. Ii. Effect of maternal diabetes on congenital malformations. Birth defects original article series. 1975;11:23–38. [PubMed] [Google Scholar]
- 49.Hernadi L, Torocsik M. Screening for fetal anomalies in the 12th week of pregnancy by transvaginal sonography in an unselected population. Prenatal diagnosis. 1997;17:753–759. doi: 10.1002/(sici)1097-0223(199708)17:8<753::aid-pd148>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 50.Souka AP, Nicolaides KH. Diagnosis of fetal abnormalities at the 10–14-week scan. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 1997;10:429–442. doi: 10.1046/j.1469-0705.1997.10060429.x. [DOI] [PubMed] [Google Scholar]
- 51.Weiner Z, Goldstein I, Bombard A, Applewhite L, Itzkovits-Eldor J. Screening for structural fetal anomalies during the nuchal translucency ultrasound examination. American journal of obstetrics and gynecology. 2007;197:181–e181. doi: 10.1016/j.ajog.2007.03.057. [DOI] [PubMed] [Google Scholar]
- 52.Whitlow BJ, Chatzipapas IK, Lazanakis ML, Kadir RA, Economides DL. The value of sonography in early pregnancy for the detection of fetal abnormalities in an unselected population. British journal of obstetrics and gynaecology. 1999;106:929–936. doi: 10.1111/j.1471-0528.1999.tb08432.x. [DOI] [PubMed] [Google Scholar]
- 53.Souka AP, Pilalis A, Kavalakis I, Antsaklis P, Papantoniou N, Mesogitis S, Antsaklis A. Screening for major structural abnormalities at the 11- to 14-week ultrasound scan. American journal of obstetrics and gynecology. 2006;194:393–396. doi: 10.1016/j.ajog.2005.08.032. [DOI] [PubMed] [Google Scholar]
- 54.Best KE, Tennant PW, Bell R, Rankin J. Impact of maternal body mass index on the antenatal detection of congenital anomalies. BJOG : an international journal of obstetrics and gynaecology. 2012;119:1503–1511. doi: 10.1111/j.1471-0528.2012.03462.x. [DOI] [PubMed] [Google Scholar]
- 55.Saari-Kemppainen A, Karjalainen O, Ylostalo P, Heinonen OP. Fetal anomalies in a controlled one-stage ultrasound screening trial. A report from the helsinki ultrasound trial. Journal of perinatal medicine. 1994;22:279–289. doi: 10.1515/jpme.1994.22.4.279. [DOI] [PubMed] [Google Scholar]
- 56.Tabor A, Zdravkovic M, Perslev A, Moller LK, Pedersen BL. Screening for congenital malformations by ultrasonography in the general population of pregnant women: Factors affecting the efficacy. Acta obstetricia et gynecologica Scandinavica. 2003;82:1092–1098. doi: 10.1046/j.1600-0412.2003.00238.x. [DOI] [PubMed] [Google Scholar]
- 57.Miller JL, de Veciana M, Turan S, Kush M, Manogura A, Harman CR, Baschat AA. First-trimester detection of fetal anomalies in pregestational diabetes using nuchal translucency, ductus venosus doppler, and maternal glycosylated hemoglobin. American journal of obstetrics and gynecology. 2013;208:385, e381–e388. doi: 10.1016/j.ajog.2013.01.041. [DOI] [PubMed] [Google Scholar]
- 58.Dashe JS, McIntire DD, Twickler DM. Maternal obesity limits the ultrasound evaluation of fetal anatomy. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2009;28:1025–1030. doi: 10.7863/jum.2009.28.8.1025. [DOI] [PubMed] [Google Scholar]
- 59.Fuchs F, Houllier M, Voulgaropoulos A, Levaillant JM, Colmant C, Bouyer J, Senat MV. Factors affecting feasibility and quality of second-trimester ultrasound scans in obese pregnant women. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2013;41:40–46. doi: 10.1002/uog.12311. [DOI] [PubMed] [Google Scholar]
- 60.Phatak M, Ramsay J. Impact of maternal obesity on procedure of mid-trimester anomaly scan. Journal of obstetrics and gynaecology : the journal of the Institute of Obstetrics and Gynaecology. 2010;30:447–450. doi: 10.3109/01443611003797679. [DOI] [PubMed] [Google Scholar]
- 61.Thornburg LL, Miles K, Ho M, Pressman EK. Fetal anatomic evaluation in the overweight and obese gravida. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2009;33:670–675. doi: 10.1002/uog.6401. [DOI] [PubMed] [Google Scholar]
- 62.Tsai LJ, Ho M, Pressman EK, Thornburg LL. Ultrasound screening for fetal aneuploidy using soft markers in the overweight and obese gravida. Prenatal diagnosis. 2010;30:821–826. doi: 10.1002/pd.2554. [DOI] [PubMed] [Google Scholar]
- 63.Chung JH, Pelayo R, Hatfield TJ, Speir VJ, Wu J, Caughey AB. Limitations of the fetal anatomic survey via ultrasound in the obese obstetrical population. The journal of maternal-fetal & neonatal medicine : the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstet. 2012;25:1945–1949. doi: 10.3109/14767058.2012.670332. [DOI] [PubMed] [Google Scholar]


