ABSTRACT
Guided by the extended parallel process model (EPPM) and reactance theory, this study examined the relationship between efficacy beliefs, reactance, and adult smokers’ responses to pictorial health warning labels (HWL) on cigarette packaging, including whether efficacy beliefs or reactance modify the relationship between HWL responses and subsequent smoking cessation behavior. Four waves of data were analyzed from prospective cohorts of smokers in Australia and Canada (n = 7,120 observations) over a period of time after implementation of more prominent, pictorial HWLs. Three types of HWL responses were studied: psychological threat responses (i.e., thinking about risks from smoking), forgoing cigarettes due to HWLs, and avoiding HWLs. The results from Generalized Estimating Equation models indicated that stronger efficacy beliefs and lower trait reactance were significantly associated with greater psychological threat responses to HWLs. Similar results were found for models predicting forgoing behavior, although response efficacy was inversely associated with it. Only response efficacy was significantly associated with avoiding HWLs, showing a positive relationship. Higher self-efficacy and stronger responses to HWLs, no matter the type, were associated with attempting to quit in the follow-up period; reactance was unassociated. No statistically significant interactions were found. These results suggest that stronger efficacy beliefs and lower trait reactance are associated with some stronger responses to fear-arousing HWL responses; however, these HWL responses appear no less likely to lead to cessation attempts among smokers with different levels of self-efficacy to quit, of response efficacy beliefs, or of trait reactance against attempts to control their behavior.
The World Health Organization (WHO) Framework Convention on Tobacco Control (FCTC) promotes prominent pictorial health warnings labels (HWLs) on cigarette packaging (WHO, 2008), and as of 2014, more than 70 countries had adopted this policy (Canadian Cancer Society, 2014). As more prominent pictorial HWLs have been implemented, smokers’ attention toward and cessation-related responses to HWLs increase (Borland et al., 2009; Thrasher, Pérez-Hernández, Arillo-Santillán, & Barrientos-Gutierrez, 2012). These effects appear to translate into lower smoking prevalence (Azagba & Sharaf, 2013; Huang, Chaloupka, & Fong, 2014), although some concerns have been raised about the quality of the evidence (Monarrez-Espino, Liu, Greiner, Bremberg, & Galanti, 2014). Concerns also have been raised that pictorial HWLs with threatening content may result in “boomerang” effects that inadvertently increase smoking (Peters, Ruiter, & Kok, 2013), particularly among smokers with low self-efficacy to quit and smokers who exhibit defensive avoidance and reactance against attempts to control their behavior. However, no studies of which we are aware have addressed whether self-efficacy or reactance moderates the influences of pictorial HWLs on smoking cessation behaviors.
Conceptualizing threatening communications: Extended parallel process model and reactance
According to the extended parallel process model (EPPM), the effects of threatening communications depend both on the intensity of the emotional response to the message and on efficacy beliefs (i.e., response efficacy and self-efficacy) (Witte, 1994; Witte & Allen, 2000). When someone perceives a threatening message as significant and personally relevant, that person experiences strong negative emotional responses, like fear or worry. Beliefs about response efficacy (i.e., perceived effectiveness of the recommended response to avoid the threat, such as the benefits of quitting smoking) and self-efficacy (i.e., perceived ability to perform the recommended response) determine whether the response to the threatening message is adaptive (e.g., changes in attitude, intention or behavior consistent with the message) or maladaptive (e.g., minimization of the threat, message avoidance, suppression of thoughts, reactance). According to EPPM, threatening messages are most likely to produce adaptive, desired responses when both perceived threat is high and efficacy is high.
EPPM posits that reactance is one possible maladaptive response to threatening messages (Witte & Allen, 2000). According to psychological reactance theory (Brehm, 1966), people may reject persuasive messages when they feel their freedom is threatened (Brehm & Brehm, 1981; Rains & Turner, 2007). In particular, persuasive messages that aim to change behavior may conflict with desires for autonomy, individuality, or self-determination (Grandpre, Alvaro, Burgoon, Miller, & Hall, 2003; Miller & Quick, 2010), causing some people to reject the messages. People with particularly intense reactance responses may try to restore their threatened freedom by more strongly embracing attitudes or behaviors that are contrary to the persuasive message (Brehm, 1966; Grandpre et al., 2003). Some studies have found empirical support for this kind of “boomerang” effect (Ringold, 2002; Wright, Wadley, Danner, & Phillips, 1992), although others have found effects only under particular circumstances, such as when messages do not “restore” a sense of individual autonomy (Bessarabova, Fink, & Turner, 2013).
Early research on reactance largely defined it as a transient state (Eagly & Chaiken, 1993; Wiium, Aaro, & Hetland, 2009); however, scholars have increasingly examined reactance as a more stable trait (Grandpre et al., 2003; Miller & Quick, 2010; Quick & Stephenson, 2008) that concerns “people’s general tendency to react negatively toward any kind of threats to their behavioral freedom” (Wiium et al., 2009). Indeed, trait reactance predicts state reactance (Donnell, Thomas, & Buboltz, 2001; Hong & Page, 1989; Quick, Scott, & Ledbetter, 2011) and has been shown to moderate the effects of persuasive messages on attitudes and behaviors (Dillard & Shen, 2005; Quick & Bates, 2010; Quick & Stephenson, 2008). Smokers with stronger trait reactance should engage in counterarguing, message denigration, and other strategies that restore their sense of autonomy and thereby reduce the threat (Dillard & Shen, 2005; Raines, 2013). Hence, threatening messages should be most effective when perceived threat is high and trait reactance is low.
EPPM constructs and smoking cessation communications
Reviews of research on smoking cessation campaigns (Durkin, Brennan, & Wakefield, 2012) and on pictorial HWLs on cigarette packs (Hammond, 2011; Noar et al., 2015) consistently indicate that strong, threatening communications have an independent, main effect on risk perceptions and cessation behaviors. Also, stronger self-efficacy to quit smoking predicts subsequent smoking cessation behaviors (Baer, Holt, & Lichtenstein, 1986; Borrelli et al., 2002; Schnoll et al., 2003; Sperry & Nicki, 1991), although this relationship is attenuated when accounting for smoking addiction (Gwaltney, Metrik, Kahler, & Shiffman, 2009). Some experimental evidence supports hypothesized EPPM interactions (Van ’t Riet, Ruiter, Werrij, & Vries, 2009), including a study finding that pictorial HWLs are most effective for smokers with stronger self-efficacy to quit (Romer, Peters, Strasser, & Langleben, 2013). Moreover, pictorial HWLs appear to promote greater reactance than text-only HWLs (Erceg-Hurn & Steed, 2011). Nevertheless, trait reactance does not appear to moderate pictorial HWLs effects by lowering intention to smoke or by reducing quit intentions among young adult smokers (Blanton, Snyder, Strauts, & Larson, 2014). Overall, studies of smoking cessation communications are similar to conclusions from systematic reviews of threatening communications across an array of topics, which indicate relatively consistent main effects for perceived threat and both self- and response-efficacy beliefs on desired outcomes, with some, less consistent evidence to support an interaction between them (De Hoog, Stroebe, & De Wit, 2007; Werrij, Ruiter, Van ‘t Riet, & De Vries, 2011; Witte, 1994; Witte & Allen, 2000).
Some critiques of pictorial HWLs emphasize that arousing fear without also increasing efficacy will lead to maladaptive responses among smokers (Peters et al., 2013). Indeed, other smoking cessation interventions have successfully promoted quitting by increasing self-efficacy (Brandon, Tiffany, Obremski, & Baker, 1990; Cinciripini et al., 2003; O’Hea et al., 2004). However, we are unaware of any observational studies that have assessed whether efficacy beliefs or reactance influence responses to pictorial HWLs. Evidence from Malaysia suggests that stronger responses to pictorial HWLs are associated with stronger self-efficacy to quit (Fathelrahman et al., 2009); however, this cross-sectional study could not determine the temporal ordering of effects, and it assessed quit intentions, not cessation behaviors. Longitudinal observational research is necessary to understand pictorial HWL effects, because the frequent exposure to HWLs (i.e., many times a day, every day) is different from one-time exposures in standard experimental research on threatening communications. Indeed, contrary to EPPM expectations, some observational longitudinal research has found that smokers who report avoiding HWLs are no less likely to try to quit than smokers who do not avoid HWLs (Borland et al., 2009; Hammond, Fong, McDonald, Brown, & Cameron, 2004). Research is needed to determine the effects of pictorial HWLs across key smoker subpopulations, such as those at differing levels of self-efficacy to quit, so that future development of HWL messages considers strategies to influence all key smoker subgroups.
Study context and aims
In 2012, Canada and Australia both implemented new pictorial HWLs that mostly included graphic imagery of bodily harm and suffering from smoking-related disease. Canada implemented its first round of pictorial HWLs in 2001, and its second round of 16 new HWLs was implemented in July 2012, accompanied by an increase in the size of HWLs from 50% to 75% of the front and back of the package. Australia had implemented its first round of pictorial HWLs in 2006, and in December 2012 it introduced its second round of 14 new HWLs (7 implemented in 2012 and 7 others in 2013). At that time, Australia increased HWL size from 30% to 75% of the front of the pack (maintaining HWLs covering 90% of the back), while also implementing “plain” packaging that standardized the pack shape, color, and size and prohibited brand imagery.
HWLs in Australia and Canada include messages that could enhance smokers’ efficacy beliefs. HWLs in both countries provide information about cessation resources (i.e., quitline numbers, websites, pharmacists) that are freely available for smokers who want to quit. HWLs appear to have increased awareness of these resources (Thrasher et al., 2015), and this greater awareness could translate into greater self-efficacy to quit. Additionally, HWLs in Canada include package inserts (i.e., leaflets and material printed inside of packages) with efficacy messages, such as descriptions of the benefits of quitting (i.e., response efficacy messages) and tips to enhance cessation success (i.e., self-efficacy messages) (Thrasher et al., 2015).
By analyzing four waves of data collected over a year-long period from panels of adult smokers in Australia and Canada, the present study aims to assess (a) the relationship between efficacy beliefs, reactance and pictorial HWL responses, and (b) whether efficacy beliefs or reactance modify the relationship between HWL responses and subsequent cessation behavior. Based on EPPM and reactance theory, we hypothesized that (a) stronger efficacy beliefs and lower trait reactance will be associated with stronger threat responses to HWLs (i.e., frequency of risk processing, forgoing cigarettes, not avoiding HWLs); (b) stronger efficacy beliefs and stronger threat responses to HWLs will be associated with subsequent cessation behavior; and (c) the relationship between threat responses to HWLs and subsequent cessation behaviors will be modified by efficacy beliefs and reactance, such that threat responses will have a stronger relationship with subsequent cessation behavior among those with stronger efficacy beliefs and lower reactance (see Figure 1).
Figure 1.
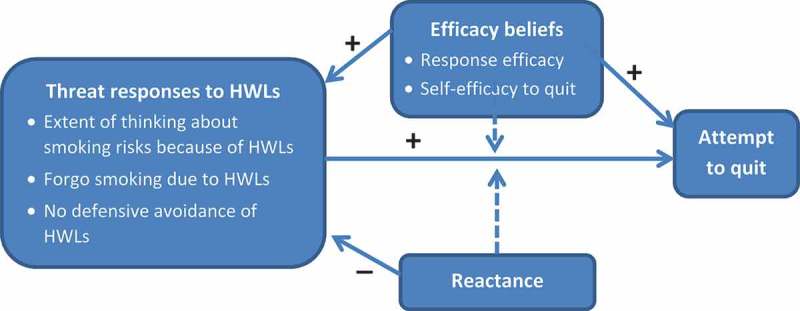
Conceptual model for the influence of efficacy beliefs and reactance on threat responses to health warning labels (HWLs) and attempts to quit smoking.
Method
Sample
Longitudinal data were analyzed from online consumer panels of Canadian and Australian residents, who were part of the Global Market Insight panel (Swayampakala et al., 2015). At study entry, eligible participants were 18 to 64 years old, had smoked at least 100 cigarettes in their lifetime, and had smoked at least once in the month prior to study enrollment. Over 1 year, four waves of data were collected at 4-month intervals (September 2012; January 2013; May 2013; September 2013), following up and surveying both those who continued to smoke and those who quit. To address attrition and maintain sample sizes of approximately 1,000 participants from each country at each wave, samples were replenished with new participants who met study eligibility criteria. Because the current study focused on predictors of downstream cessation attempts, the analytic sample included only participants with at least one wave of follow-up (Australia: n = 923 smokers providing 3,854 observations, and Canada: n = 915 smokers providing 3,266 observations). A pilot study using Mechanical Turk (Paolacci & Chandler, 2014) was conducted with adult smokers from the United States (n = 146) to determine test–retest reliability of measures over 2 weeks.
Measures
Efficacy beliefs
Self-efficacy to quit was measured at each wave by asking, “If you decided to give up smoking completely in the next 6 months, how sure are you that you would succeed?”(IARC, 2008), with responses on a 1- to 9-point scale with verbal anchors provided for every other option (i.e., not at all, a little, moderately, very much, extremely). Because of the multimodal distribution of responses, this variable was recoded as a five-level variable that combined response options with verbal anchors and adjacent response options without a verbal anchor. The pilot study test–retest reliability for this measure was good (r = .70). Response efficacy beliefs were measured at each wave by asking,“How much do you think you would benefit from health and other gains if you were to quit smoking permanently in the next 6 months?” (IARC, 2008), with a 1- to 9-point scale, as for self-efficacy. In our pilot study, the test–retest reliability of this measure was good (r = .72). Because of the skewed distribution of responses, this variable was recoded as a three-level variable: less than very much (i.e., 1–6), very much and the higher category (i.e., 7–8), and extremely (i.e., 9).
Reactance
To measure trait reactance, at initial enrollment into the study, participants reported responses to a subset of five questions adapted from a validated scale (Hong & Faedda, 1996) (i.e., “I don’t like people pointing out things that I already know”; “I resist attempts of others to influence me”; “It makes me angry when another person is held up as a role model for me to follow”; “When something is prohibited, I usually think, ‘That’s exactly what I am going to do’”; and “Regulations trigger a sense of resistance in me”). Five-point Likert scale response options were used, and “don’t know” responses were recoded as “neither agree nor disagree.” Internal consistency was acceptable in both countries (alpha = .67 and .69 for Canada and Australia, respectively). Question responses were averaged and treated as continuous variable in the analysis. Pilot study test–retest reliability for the summary reactance measure was good (r = .78) (Kline, 2000).
Threat responses to pictorial HWLs
Psychological threat responses to HWLs were assessed by asking participants “To what extent do the warning labels make you think about the health risks of smoking?,” with responses ranging from 1 to 9 (see Efficacy Beliefs section). A behavioral threat response to HWLs that predicted cessation behavior in prior research (Borland et al., 2009) was also assessed: “In the last month, have the warning labels stopped you from having a cigarette when you were about to smoke one?” (yes, no). Defensive avoidance behavior was assessed by asking participants, “In the last month, have you made any effort to avoid looking at or thinking about the warning labels—such as covering them up, keeping them out of sight, using a cigarette case, avoiding certain warnings, or any other means?” Responses were dichotomized to indicate any avoidance of HWLs in the last month (no vs. “once,” “a few times,” and “many times”).
Quit attempts
At each survey wave, smokers indicated whether they had made any attempts to stop smoking in the prior 4 months, while the question was anchored by providing the actual date 4 months prior to the interview. Adult smokers’ recall of quit attempts in the prior 3 months appears valid (Berg et al., 2010; Borland, Partos, & Cummings, 2012), so our study extended this by 1 month to encompass the 4-month interval between survey waves. At follow-up, participants could also indicate that they had quit smoking. Participants were classified as having made a quit attempt if they were no longer smoking (and were smoking at the previous wave) or if they reported attempting to quit in the prior 4 months.
Adjustment variables
Nicotine dependence was measured with the Heaviness of Smoking Index (HSI) (Heatherton, Kozlowski, Frecker, Rickert, & Robinson, 1989), which has predictive validity (Borland, Yong, O’Connor, Hyland, & Thompson, 2010). At each wave, participants were asked the number of cigarettes smoked per day and their time to first cigarette, which were combined to provide the HSI score (range = 0 to 6). Participants were asked whether they planned to quit (i.e., in the next month, in the next 6 months, sometime beyond 6 months, or not at all), and responses were dichotomized to indicate intention to quit within the next 6 months versus not (IARC, 2008). Recent quit attempts were assessed (see Quit Attempts, earlier section). Dummy variables were derived for age (i.e., 18–24; 25–34; 35–44; 45–54; 55–64 years), educational attainment (i.e., high school or less; some college or university; completed college or university), annual household income (i.e., $29,000 or less; $30,000 to $59,999; $60,000 or more), country (Australia as reference), survey wave (wave I as reference), and time-in-sample (i.e., number of prior survey waves the participant completed, with the first wave of participation as reference).
Analysis
All analyses were conducted using SAS, version 9.3. Omnibus chi-squared tests were used to assess differences between countries and between the analytic sample (i.e., at least two surveys) and the excluded sample (i.e., surveyed only once). Data from waves 1, 2, and 3 were pooled and analyzed in a series of bivariate and adjusted Generalized Estimating Equation (GEE) models, treating data from each wave as a separate observation while adjusting for within-individual correlations of data due to repeated observations from participants using an exchangeable correlation matrix. Separate GEE models were run for each of the three HWL responses regressed on self-efficacy to quit, response efficacy, reactance, and the adjustment variables. Linear GEE models were used for models assessing threat responses and logistic GEE models were used for the behavioral responses to HWLs. Then, bivariate and adjusted logistic GEE models were estimated regressing having made an attempt to quit by follow-up period (i.e., t + 1) on self-efficacy, perceived response efficacy, reactance, HWL responses, and adjustment variables, all assessed at t (i.e., wave 1 data predicted wave 2 quit attempts, etc.). Because threat responses to HWLs are conceptualized as working along similar pathways toward cessation (see Figure 1), separate adjusted models were estimated for each HWL response variable while excluding the others. Finally, a series of adjusted logistic GEE models predicting downstream quit attempts were estimated that included the aforementioned independent variables as well as multiplicative interaction terms, which were tested one at a time (i.e., self-efficacy by each HWL response; perceived response efficacy by each HWL response; reactance by each HWL response).
Because our sample was from unknown sampling frames that may not be representative of the general population of smokers, we also re-ran analyses after weighing the data to sex, age, and educational profiles of nationally representative smoker populations in each country. Furthermore, to determine whether our results were biased by differential attrition we created country-specific propensity scores that involved estimating predicted probabilities of completing survey waves. These propensity scores were calculated using a range of variables that may be associated with the period of time over which people participated in the study but that were not already included in our analyses (e.g., employment status, marital status, number of online surveys completed in the last 4 months, number of online surveys on smoking in the last month, overall health status, reasons to consider quitting smoking). After additional adjustment for weights and for propensity scores (done separately), all adjusted models reported in this article were estimated again. Finally, all models were rerun using the reactance item that best captures the “emotional response” subscale of reactance (i.e., “I don’t like people pointing out things that I already know”), because pictorial HWLs could work primarily through emotional pathways. The results from each model in these sensitivity analyses were consistent in direction, magnitude, and statistical significance to the results presented in the following, and therefore would not cause any changes in our interpretation of results (results available upon request).
Results
Sample characteristics
The analytic sample (n = 1,838 smokers providing for 3,560 observations) was compared to the excluded sample (n = 2,443 smokers) that participated in only one survey wave (Table 1). In addition to sociodemographic and smoking-related differences found, smokers in the analytic sample were more likely to report lower self-efficacy to quit, lower response efficacy, and higher reactance; however, no differences in HWL responses were found. Some statistically significant sociodemographic and smoking-related differences were found across countries, including higher self-efficacy, higher response efficacy, lower reactance, and stronger psychological (but not behavioral) threat responses to HWLs for Canadians compared to Australians.
Table 1.
Analytic sample characteristics by country and in comparison to excluded sample.
| Sample characteristics | Analytic sample |
Excluded sample* |
||
|---|---|---|---|---|
| Canada |
Australia |
Total |
|
|
| Nsmokers = 915 | Nsmokers = 923 | Nsmokers = 1,838 | Nsmokers = 2,443 | |
| Age (years)c,f | ||||
| 18–24 | 8% | 5% | 6% | 17% |
| 25–34 | 19% | 20% | 20% | 26% |
| 35–44 | 22% | 23% | 22% | 22% |
| 45–54 | 24% | 25% | 25% | 18% |
| 55–64 | 27% | 27% | 27% | 17% |
| Sexf | ||||
| Female | 54% | 54% | 54% | 64% |
| Educationa,f | ||||
| High school or less | 29% | 34% | 32% | 40% |
| Some college or university | 46% | 42% | 43% | 45% |
| University or more | 26% | 24% | 25% | 15% |
| Incomec,f | ||||
| $29,999 or less | 25% | 23% | 24% | 29% |
| $30,000-$59,999 | 31% | 26% | 28% | 32% |
| $60,000 or more | 44% | 51% | 48% | 39% |
| Heaviness of smokingc,f | ||||
| Mean (SD) | 2.45 (1.57) | 2.76 (1.63) | 2.62 (1.61) | 2.4 (1.62) |
| Quit attempt in prior 4 monthsb,d | ||||
| Yes | 40% | 36% | 38% | 41% |
| Quit Intentions in next 6 monthsa,e | ||||
| Yes | 43% | 39% | 41% | 46% |
| Self-efficacyb,f | ||||
| Mean (SD) | 2.88 (1.16) | 2.77 (1.17) | 2.83 (1.16) | 2.98 (1.19) |
| Response efficacyc,f | ||||
| Less than very much | 23% | 29% | 26% | 19% |
| Less than extremely | 32% | 31% | 32% | 29% |
| Extremely | 44% | 40% | 42% | 52% |
| Reactancec,e | ||||
| Mean (SD) | 3.26 (0.68) | 3.36 (0.66) | 3.32 (0.67) | 3.26 (0.67) |
| Thinking about health risksc | ||||
| Mean (SD) | 4.5 (2.5) | 4.2 (2.5) | 4.4 (2.5) | 4.5 (2.5) |
| Avoided HWLs | ||||
| Yes | 31% | 32% | 32% | 34% |
| Forwent cigarette due to HWLs | ||||
| Never | 80% | 78% | 79% | 80% |
| Once or more | 20% | 22% | 21% | 20% |
Note. CA vs. AU: a, p < .05; b, p < .01; c, p < .001. Analytic vs. ineligible sample: d, p < .05; e, p < .01; f, p < .001. In analytic sample, n observations = 7,120 (CA n observations = 3,266 and AU n observations = 3,854).
*Excluded sample consists of participants who were not followed up.
HWL responses, efficacy beliefs, and reactance
In adjusted GEE models that regressed HWL responses on study variables (Table 2), higher self-efficacy, higher response efficacy, and lower reactance were independently associated with stronger psychological threat responses to HWLs, a result that was similar to models predicting forgoing cigarettes, except that the response efficacy association was negative in adjusted models. In both bivariate and adjusted models, self-efficacy and reactance were unassociated with avoidance of HWLs, while the highest category of response efficacy was positively associated with avoidance of HWLs in adjusted models. Prior quit intentions and recent quit attempts were associated positively with all three HWL responses, except that the association between quit intentions and HWL avoidance was no longer statistically significant in adjusted models.
Table 2.
Predictors of adult smokers’ responses to health warning labels (HLWs) on cigarette packages, Canada and Australia, 2012–2013.
| | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Think about health risks due to HWLs |
Forwent cigarette due to HWLs |
Avoidance of HWLs |
||||||||||
| Bivariate |
Adjusted model |
Bivariate |
Adjusted model |
Bivariate |
Adjusted model |
|||||||
| Independent variables | B | (95% CI) | B | (95% CI) | OR | (95% CI) | AOR | (95% CI) | OR | (95% CI) | AOR | (95% CI) |
| Country | ||||||||||||
| Australia | REF | REF | REF | REF | REF | REF | ||||||
| Canada | 0.24a | [0.02–0.45] | 0.07 | [−0.14–0.27] | 0.91 | [0.73–1.13] | 0.81 | [0.64–1.02] | 0.96 | [0.88–1.14] | 0.96 | [0.79–1.16] |
| Heaviness of smoking | −0.15c | [−0.21- −0.09] | −0.02 | [−0.08–0.05] | 0.83c | [0.78–0.89] | 0.97 | [0.89–1.04] | 0.99 | [0.94–1.05] | 1.03 | [0.97–1.1] |
| Recent quit attempt | ||||||||||||
| No | REF | REF | REF | REF | REF | REF | ||||||
| Yes | 0.74c | [0.58–0.9] | 0.43c | [0.25–0.61] | 2.66c | [2.19–3.24] | 2.45c | [1.94–3.09] | 1.49c | [1.28–1.74] | 1.40c | [1.17–1.7] |
| Quit intentions | ||||||||||||
| No | REF | REF | REF | REF | REF | REF | ||||||
| Yes | 0.89c | [0.73–1.06] | 0.40c | [0.22–0.58] | 1.87c | [1.57–2.24] | 1.39b | [1.12–1.73] | 1.44c | [1.23–1.67] | 1.16 | [0.96–1.4] |
| Self-efficacy | 0.38c | [0.3–0.46] | 0.25c | [0.17–0.33] | 1.24c | [1.15–1.34] | 1.19c | [1.09–1.3] | 1.00 | [0.94–1.07] | 0.98 | [0.91–1.06] |
| Response efficacy | ||||||||||||
| Low | REF | REF | REF | REF | REF | REF | ||||||
| Middle | 0.75c | [0.58–0.92] | 0.66c | [0.49–0.84] | 0.87 | [0.7–1.09] | 0.71b | [0.56–0.9] | 1.25c | [1.02–1.52] | 1.15 | [0.93–1.48] |
| High | 1.42c | [1.22–1.61] | 1.26c | [1.06–1.46] | 0.94 | [0.76–1.18] | 0.73a | [0.57–0.94] | 1.56c | [1.29–1.9] | 1.38b | [1.12–1.72] |
| Reactance | −0.41c | [−0.59- −0.24] | −0.38c | [−0.54- −0.22] | 0.86 | [0.73–1.02] | 0.82a | [0.69–0.98] | 1.12 | [0.98–1.28] | 1.06 | [0.92–1.21] |
Note. Adjusted models adjust for all the independent variables listed in the table, as well as for age, gender, education, income, survey wave, and time in sample. Bivariate models: a, p < .05; b, p < .01; c, p < .001. Adjusted models: d, p < .05; e, p < .01; f, p < .001. n smokers = 1,838 providing n observations = 7,120 (in CA n smokers = 917 providing n observations = 3,266 and in AU n smokers = 923 providing n observations = 3,854).
Quit-related behaviors
Thirty-eight percent of the sample attempted to quit during follow-up to the subsequent survey. In bivariate logistic GEE models, all three HWL responses were associated with cessation, as was greater self-efficacy and response efficacy, but not reactance (Table 3). In adjusted models, smokers were more likely to attempt to quit if they reported stronger psychological threat responses to HWLs, any forgoing behavior due to HWLs, or any avoidance behavior. Higher self-efficacy, intention to quit, prior quit behavior, and lower HSI were all associated with greater likelihood of making quit attempts across all three adjusted models. Perceived response efficacy was associated with greater likelihood of quit attempts only in the adjusted model predicting forgoing behavior. Reactance was unassociated with quit attempts in any model (see Table 3 for results). In subsequent adjusted models that included interactions of HWL responses with self-efficacy, response efficacy, and reactance, none of the interaction terms approached statistical significance (i.e., self-efficacy × HWL responses: p-value range = .70–.72; perceived response efficacy × HWL responses: p-value range = .39–.84; reactance by HWL responses: p-value range = .18–.64).
Table 3.
Predictors of attempting to quit by the subsequent wave of observation.
| Bivariate |
Adjusted model 1* |
Adjusted model 2** |
Adjusted model 3*** |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Independent variables | % | OR | (95% CI) | AOR | (95% CI) | AOR | (95% CI) | AOR | (95% CI) |
| Country | |||||||||
| Australia | 35% | REF | REF | REF | REF | ||||
| Canada | 41% | 1.19 a | [1.01–1.41] | 1.06 | [0.89–1.26] | 1.08 | [0.90–1.30] | 1.03 | [0.86–1.24] |
| Heaviness of Smoking | 2.2^ | 0.82 c | [0.78–0.86] | 0.91e | [0.85–0.96] | 0.91 e | [0.85–0.97] | 0.90 e | [0.85–0.96] |
| Recent quit behavior | |||||||||
| No | 19% | REF | REF | REF | REF | ||||
| Yes | 69% | 12.48 c | [10.42–14.93] | 5.33 f | [4.35–6.53] | 4.93 f | [4.00–6.08] | 5.76 f | [4.68–7.08] |
| Quit intentions | |||||||||
| No | 21% | REF | REF | REF | REF | ||||
| Yes | 59% | 3.45 c | [2.96–4.03] | 2.15 f | [1.76–2.61] | 2.15 f | [1.76–2.64] | 2.24 f | [1.84–2.73] |
| Self-efficacy | 3.15^ | 1.37 c | [1.29–1.46] | 1.17 f | [1.08–1.27] | 1.17 f | [1.07–1.27] | 1.19 f | [1.09–1.29] |
| Response efficacy | |||||||||
| Low | 29% | REF | REF | REF | REF | ||||
| Middle | 33% | 1.13 | [0.95–1.35] | 0.85 | [0.66–1.09] | 0.99 | [0.77–1.28] | 0.87 | [0.68–1.11] |
| High | 45% | 1.76 c | [1.47–2.1] | 1.13 | [0.89–1.45] | 1.43 e | [1.11–1.83] | 1.23 | [0.97–1.57] |
| Reactance | 3.3^ | 0.95 | [0.84–1.08] | 1.01 | [0.88–1.16] | 1.04 | [0.90–1.20] | 0.98 | [0.85–1.12] |
| Thinking about health risks | 5.2^ | 1.19 c | [1.15–1.22] | 1.08 f | [1.04–1.12] | N/A** | N/A*** | ||
| Forwent cigarettes due to HWLs | |||||||||
| Never | 30% | REF | REF | REF | REF | ||||
| Once or more | 63% | 2.78 c | [2.31–3.34] | N/A* | 1.97 f | [1.576–2.466] | N/A*** | ||
| Avoiding HWLs | |||||||||
| No | 33% | REF | REF | REF | REF | ||||
| Yes | 46% | 1.34 c | [1.16–1.56] | N/A* | N/A** | 1.41 f | [1.17–1.70] | ||
Note. ^ = Mean. Bivariate models: a, p < .05; b, p < .01; c, p < .001. Adjusted models: d, p < .05; e, p < .01; f, p < .001. n smokers = 1,838 providing n observations = 7,120 (in CA n smokers = 917 providing n observations = 3,266 and in AU n smokers = 923 providing n observations = 3,854).
*Model adjusts for age, gender, education, income, survey wave, and time in sample, as well as all variables listed in the table but not forwent cigarettes due to HWLs and avoid HWLs.
**Model adjusts for age, gender, education, income, survey wave, and time in sample, as well as all variables listed in the table but not thinking about health risks and avoid HWLs.
***Model adjusts for age, gender, education, income, survey wave, and time in sample, as well as all variables listed in the table but not thinking about health risks and forwent cigarettes due to HWLs.
Discussion
Our study results are consistent with prior research suggesting that prominent, pictorial HWLs promote cessation behavior (Hammond, 2011; Huang et al., 2014). We also found that cessation behavior was predicted by stronger threat responses to HWLs, stronger self-efficacy, and, to some extent, by stronger response efficacy; however, neither efficacy beliefs nor reactance moderated the effects of HWL responses on cessation attempts. Hence, results did not support arguments that pictorial HWLs are counterproductive (Peters et al., 2013). To the extent that pictorial HWLs promote cessation-related responses in smokers, our study finds no evidence that these responses are less likely to promote cessation attempts among smokers with different levels of self-efficacy to quit, of response efficacy beliefs, or of trait reactance against attempts to control their behavior. Indeed, our results are consistent with reviews indicating the additive, but not interactive, effects of efficacy beliefs and perceived threat on desired outcomes (Durkin et al., 2012; Witte & Allen, 2000). Future research should consider evaluation of equivalence tests to establish more strongly the null results of the interaction effects. Also, future research should explore whether these relationships occur for successful quitting, as our relatively small sample of successful quitters did not provide sufficient power to examine this issue.
Study results are also suggestive about the relationship between HWL responses and reactance. Prior studies found that trait reactance predicts state reactance to persuasive messages (Dillard & Shen, 2005; Donnell et al., 2001; Quick et al., 2011), which is consistent with our finding that smokers with higher levels of trait reactance reported weaker cessation-related psychological threat responses to HWLs. However, we found that trait reactance was generally unassociated with cessation-related behaviors (i.e., forgoing cigarette due to HWLs, avoiding HWLs, quit attempts). Future research should consider whether reactance matters more for psychosocial than for behavioral outcomes. At least for pictorial HWL messages, where smokers are regularly exposed to threatening messages, reactance may be similar to avoidance behaviors, which do not seem to impede cessation behavior (Borland et al., 2009). Indeed, in our study, avoidance of HWLs was positively associated with quit attempts. Future research should also consider measurement of state reactance that is specific to HWLs. Experimental evidence indicates that pictorial HWLs elicit stronger state reactance than text-only HWLs (Erceg-Hurn & Steed, 2011). This line of research should be extended to studies with ecological validity (e.g., repeated HWL exposure) to determine whether state and trait reactance influence perceptions and behaviors in similar ways, as has been found in prior experimental research (Quick & Bates, 2010; Quick & Stephenson, 2008).
Our results indicate that greater self-efficacy to quit is independently associated with stronger psychological threat responses to HWLs and engaging in forgoing behavior, but not with avoiding HWLs. A similar pattern of results was found for response efficacy, except for the unexpected, inverse relationship with forgoing cigarettes. The explanation for this inverse relationship is unclear; however, it was found only in adjusted models, suggesting that a fuller explanation resides in a more detailed examination of the interrelationships between smoking-related variables, efficacy beliefs, and reactance. Future research should aim to assess the extent to which HWLs can reasonably modify efficacy beliefs and whether this matters for smoking cessation. Indeed, the implementation of pictorial HWLs has increased cessation-related threat responses across a variety of countries (Borland et al., 2009; Thrasher, Perez-Hernandez, et al., 2012), but changes in efficacy beliefs have not been studied. Efficacy beliefs may be influenced by the inclusion of HWL content about quitting resources, which has raised awareness and utilization of these resources (Miller, Hill, Quester, & Hiller, 2009; Thrasher et al., 2015; Thrasher, Perez-Hernandez, et al., 2012; Wilson, Li, Hoek, Edwards, & Peace, 2010). More elaborated efficacy messages in Canada appear to complement threatening HWL content and thereby promote efficacy beliefs and cessation behavior, including sustained cessation attempts (Thrasher et al., 2015; 2016). Although our study found that self-efficacy was higher in the study sample from Canada than in Australia, this comparison is speculative, as cross-country differences in sociodemographics and smoking-related variables, including greater efficacy and stronger reactions to HWLs in Canada, may also indicate systematic differences in sampling across countries. Future experimental research should aim to identify the combinations of pictorial HWL content that most effectively promote cessation and consumer understanding of tobacco-related risks.
This study has a number of limitations. Our reactance measure includes a subset of scale items drawn from three of four factors identified in prior research (Thomas, Donnell, & Buboltz, 2001). Although our sensitivity analysis of the item representing the emotional reaction subscale produced a consistent pattern of results, enhanced measurement of the emotional domain and assessment of state reactance should be explored in future research. To measure self-efficacy to quit we used a single item recommended for use in policy evaluation research (IARC, 2008), as it appears equally, if not more, accurate than multi-item measures that encompass an array of contexts and behaviors (Gwaltney, Shiffman, Balabanis, & Paty, 2005). As in our study, this single-item measure has predicted downstream cessation (Yan, 2007), suggesting its predictive validity. Furthermore, our pilot research for the project indicated reasonably good test–retest reliability for both self-efficacy and reactance. Future research could still consider richer measurement of these constructs, especially where they can capture both HWL content and their hypothesized pathways to smoking cessation. Another potential influence on self-efficacy concerns the length of time that pictorial HWLs have been on cigarette packages, which was more than 10 years in Canada and more than 6 years in Australia. Hence, influences of pictorial HWLs on efficacy beliefs, reactance, or defensive responses may have been set into motion well before data collection began, impeding understanding of HWL effects due to the new rounds of larger pictorial HWLs that circulated during the period of our study. Additional research with different study designs may be necessary to better understand mediation and moderation of HWL responses due to specific types of HWL content.
The generalizability of the results is limited by concerns about selection and attrition bias. Our sample had no known sampling frame and was purposively recruited to represent key consumer segments in each country. Compared to those who participated in only one survey wave, the analytic sample was older, more highly educated, more addicted, and less likely to have recently tried to quit or to intend to quit. These characteristics of the analytic sample have been associated with weaker reactions to pictorial HWLs (Hammond et al., 2012; Thrasher, et al., 2012; Thrasher et al., 2010), suggesting that our study may have underestimated HWL effects. However, there was no difference between the two samples with regard to the strength of HWL responses, so any underestimation may be minimal. Furthermore, when we adjusted our models for propensity of loss to follow-up over time, the results were similar in direction and magnitude. The current study did not aim to be representative of the broader population, but to examine in a large sample the general processes around responses to pictorial HWLs with shorter intervals between survey waves (i.e., 4 months) than has been customary (i.e., every 1 - 2 years). Nevertheless, the pattern of results and interpretations from our study were the same after we adjusted models to weight the sample so that it was similar to the general population profile of smokers in each country.
Conclusions
Our study is consistent with prior research that has found that prominent pictorial HWLs produce psychological and behavioral threat responses that independently promote smoking cessation behaviors. We found no evidence that this relationship would be different for adult smokers at different levels of self-efficacy to quit, response efficacy, or trait reactance. These results suggest that fear-arousing pictorial HWLs do not produce “boomerang” effects.
Funding Statement
This work was supported by a grant from the U.S. National Cancer Institute National Institute of Health (R01 CA167067). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Funding
This work was supported by a grant from the U.S. National Cancer Institute National Institute of Health (R01 CA167067). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Azagba S., Sharaf M. F. The effect of graphic cigarette warning labels on smoking behavior: Evidence from the Canadian experience. Nicotine & Tobacco Research. 2013;15:708–717. doi: 10.1093/ntr/nts194. [DOI] [PubMed] [Google Scholar]
- Baer J. S., Holt C. S., Lichtenstein E. Self-efficacy and smoking reexamined: Construct validity and clinical utility. Journal of Consulting and Clinical Psychology. 1986;54:846–852. doi: 10.1037/0022-006X.54.6.846. [Research Support, U.S. Gov’t, P.H.S.] [DOI] [PubMed] [Google Scholar]
- Berg C. J., An L. C., Kirch M., Guo H., Thomas J. L., Patten C. A., West R. Failure to report attempts to quit smoking. Addictive Behaviors. 2010;35:900–904. doi: 10.1016/j.addbeh.2010.06.009. [Research Support, Non-U.S. Gov’t] [DOI] [PubMed] [Google Scholar]
- Bessarabova E., Fink E. L., Turner M. Reactance, restoration, and cognitive structure: Comparative statics. Human Communication Research. 2013;39:339–364. doi: 10.1111/hcre.12007. [DOI] [Google Scholar]
- Blanton H., Snyder L. B., Strauts E., Larson J. G. Effect of graphic cigarette warnings on smoking intentions in young adults. PLoS ONE. 2014;9(5):e96315. doi: 10.1371/journal.pone.0096315. [Randomized Controlled Trial Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borland R., Partos T. R., Cummings K. M. Systematic biases in cross-sectional community studies may underestimate the effectiveness of stop-smoking medications. Nicotine & Tobacco Research. 2012;14:1483–1487. doi: 10.1093/ntr/nts002. [Comparative Study Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borland R., Wilson N., Fong G. T., Hammond D., Cummings K. M., Yong -H.-H., McNeill A. Impact of graphic and text warnings on cigarette packs: Findings from four countries over five years. Tobacco Control. 2009;18:358–364. doi: 10.1136/tc.2008.028043. [Multicenter Study Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borland R., Yong H. H., O’Connor R. J., Hyland A., Thompson M. E. The reliability and predictive validity of the heaviness of smoking index and its two components: Findings from the international tobacco control four country study. Nicotine & Tobacco Research. 2010;12(Suppl):S45–50. doi: 10.1093/ntr/ntq038. [Comparative Study Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borland R., Yong -H.-H., Wilson N., Fong G. T., Hammond D., Cummings K. M., McNeill A. How reactions to cigarette packet health warnings influence quitting: Findings from the ITC four-country survey. Addiction. 2009;104:669–675. doi: 10.1111/j.1360-0443.2009.02508.x. [Multicenter Study Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrelli B., Hogan J. W., Bock B., Pinto B., Roberts M., Marcus B. Predictors of quitting and dropout among women in a clinic-based smoking cessation program. Psychology of Addictive Behaviors. 2002;16:22–27. doi: 10.1037/0893-164X.16.1.22. [Clinical Trial Randomized Controlled Trial Research Support, U.S. Gov’t, P.H.S.] [DOI] [PubMed] [Google Scholar]
- Brandon T. H., Tiffany S. T., Obremski K. M., Baker T. B. Postcessation cigarette use: The process of relapse. Addictive Behaviors. 1990;15:105–114. doi: 10.1016/0306-4603(90)90013-N. [Research Support, U.S. Gov’t, P.H.S.] [DOI] [PubMed] [Google Scholar]
- Brehm J. W. A theory of psychological reactance. Oxford, England: Academic Press; 1966. [Google Scholar]
- Brehm S. S., Brehm J. W. Psychological reactance: A theory of freedom and control. New York, NY: Academic Press; 1981. [Google Scholar]
- Canadian Cancer Society . Cigarette package health warnings: International status report. 2014. http://www.cancer.ca/~/media/cancer.ca/CW/for%20media/Media%20releases/2014/Tobacco%20Warnings%20Oct%202014/CCS-international-package-warnings-report-2014-ENG.pdf?la=fr-CA Retrieved from. [Google Scholar]
- Cinciripini P. M., Wetter D. W., Fouladi R. T., Blalock J. A., Carter B. L., Cinciripini L. G., Baile W. F. The effects of depressed mood on smoking cessation: Mediation by postcessation self-efficacy. Journal of Consulting and Clinical Psychology. 2003;71:292–301. doi: 10.1037/0022-006X.71.2.292. [Clinical Trial Randomized Controlled Trial Research Support, U.S. Gov’t, P.H.S.] [DOI] [PubMed] [Google Scholar]
- De Hoog N., Stroebe W., De Wit J. B. F. The impact of vulnerability to and severity of a health risk on processing and acceptance of fear-arousing communications: A meta analysis. Review of General Psychology. 2007;11:258–285. doi: 10.1037/1089-2680.11.3.258. [DOI] [Google Scholar]
- Dillard J. P., Shen L. On the nature of reactance and its role in persuasive health communication. Communication Monographs. 2005;72:144–168. doi: 10.1080/03637750500111815. [DOI] [Google Scholar]
- Donnell A. J., Thomas A., Buboltz W. C. Psychological reactance: Factor structure and internal consistency of the questionnaire for the measurement of psychological reactance. Journal of Social Psychology. 2001;141:679–687. doi: 10.1080/00224540109600581. [DOI] [PubMed] [Google Scholar]
- Durkin S., Brennan E., Wakefield M. Mass media campaigns to promote smoking cessation among adults: An integrative review. Tobacco Control. 2012;21:127–138. doi: 10.1136/tobaccocontrol-2011-050345. [Review] [DOI] [PubMed] [Google Scholar]
- Eagly A. H., Chaiken S. The psychology of attitudes. Fort Worth, TX: Harcourt; 1993. [Google Scholar]
- Erceg-Hurn D. M., Steed L. G. Does exposure to cigarette health warnings elicit psychological reactance in smokers? Journal of Applied Social Psychology. 2011;41:219–237. doi: 10.1111/j.1559-1816.2010.00710.x. [DOI] [Google Scholar]
- Fathelrahman A. I., Omar M., Awang R., Borland R., Fong G. T., Hammond D., Zain Z. Smokers’ responses toward cigarette pack warning labels in predicting quit intention, stage of change, and self-efficacy. Nicotine & Tobacco Research. 2009;11:248–253. doi: 10.1093/ntr/ntn029. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandpre J., Alvaro E. M., Burgoon M., Miller C. H., Hall J. R. Adolescent reactance and anti-smoking campaigns: A theoretical approach. Health Communication. 2003;15:349–366. doi: 10.1207/S15327027HC1503_6. [DOI] [PubMed] [Google Scholar]
- Gwaltney C. J., Metrik J., Kahler C. W., Shiffman S. Self-efficacy and smoking cessation: A meta-analysis. Psychology of Addictive Behaviors. 2009;23:56–66. doi: 10.1037/a0013529. [Meta-Analysis Research Support, N.I.H., Extramural] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gwaltney C. J., Shiffman S., Balabanis M. H., Paty J. A. Dynamic self-efficacy and outcome expectancies: Prediction of smoking lapse and relapse. Journal of Abnormal Psychology. 2005;114:661–675. doi: 10.1037/0021-843X.114.4.661. [Randomized Controlled Trial Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t] [DOI] [PubMed] [Google Scholar]
- Hammond D. Health warning messages on tobacco products: A review. Tobacco Control. 2011;20:327–337. doi: 10.1136/tc.2010.037630. [Research Support, Non-U.S. Gov’t Review] [DOI] [PubMed] [Google Scholar]
- Hammond D., Fong G. T., McDonald P. W., Brown K. S., Cameron R. Graphic Canadian cigarette warning labels and adverse outcomes: Evidence from Canadian smokers. American Journal of Public Health. 2004;94:1442–1445. doi: 10.2105/AJPH.94.8.1442. [Evaluation Studies Research Support, Non-U.S. Gov’t Research Support, U.S. Gov’t, P.H.S.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond D., Thrasher J., Reid J. L., Driezen P., Boudreau C., Santillan E. A. Perceived effectiveness of pictorial health warnings among Mexican youth and adults: A population-level intervention with potential to reduce tobacco-related inequities. Cancer Causes Control. 2012;23(Suppl. S1):57–67. doi: 10.1007/s10552-012-9902-4. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heatherton T. F., Kozlowski L. T., Frecker R. C., Rickert W., Robinson J. Measuring the heaviness of smoking: Using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Addiction. 1989;84:791–800. doi: 10.1111/j.13600443.1989.tb03059.x. [DOI] [PubMed] [Google Scholar]
- Hong S.-M., Faedda S. Family life satisfaction, age, length of residency: Predicting alcohol and cigarette use among Korean adolescents in Australia. Psychological Reports. 1996;78:187–193. doi: 10.2466/pr0.1996.78.1.187. [DOI] [PubMed] [Google Scholar]
- Hong S.-M., Page S. A psychological reactance scale: Development, factor structure and reliability. Psychological Reports. 1989;64:1323–1326. doi: 10.2466/pr0.1989.64.3c.1323. [DOI] [Google Scholar]
- Huang J., Chaloupka F. J., Fong G. T. Cigarette graphic warning labels and smoking prevalence in Canada: A critical examination and reformulation of the FDA regulatory impact analysis. Tobacco Control. 2014;23(Suppl. 1):i7–12. doi: 10.1136/tobaccocontrol-2013-051170. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t] [DOI] [PMC free article] [PubMed] [Google Scholar]
- IARC . IARC handbooks of cancer prevention, tobacco control, vol. 12: Methods for evaluating tobacco control policies. Vol. 12. Lyon, France: International Agency for Research on Cancer; 2008. [Google Scholar]
- Kline P. The handbook of psychological testing. 2nd ed. London, UK: Routledge; 2000. [Google Scholar]
- Miller C. H., Quick B. L. Sensation seeking and psychological reactance as health risk predictors for an emerging adult population. Health Communication. 2010;25:266–275. doi: 10.1080/10410231003698945. [DOI] [PubMed] [Google Scholar]
- Miller C. L., Hill D. J., Quester P. G., Hiller J. E. Impact on the Australian Quitline of new graphic cigarette pack warnings including the Quitline number. Tobacco Control. 2009;18:235–237. doi: 10.1136/tc.2008.028290. [Research Support, Non-U.S. Gov’t] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monarrez-Espino J., Liu B., Greiner F., Bremberg S., Galanti R. Systematic review of the effect of pictorial warnings on cigarette packages in smoking behavior. American Journal of Public Health. 2014;104(10):e11–30. doi: 10.2105/AJPH.2014.302129. [Review] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noar S. M., Hall M. G., Francis D. B., Ribisl K. M., Pepper J. K., Brewer N. T. Pictorial cigarette pack warnings: A meta-analysis of experimental studies. Tobacco Control. 2015 doi: 10.1136/tobaccocontrol-2014-051978. [Review] Published Online First: 6 May 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Hea E. L., Boudreaux E. D., Jeffries S. K., Carmack Taylor C. L., Scarinci I. C., Brantley P. J. Stage of change movement across three health behaviors: The role of self-efficacy. American Journal of Health Promotion. 2004;19:94–102. doi: 10.4278/0890-1171-19.2.94. [DOI] [PubMed] [Google Scholar]
- Paolacci G., Chandler J. Inside the Turk: Understanding mechanical turk as a participant pool. Current Directions in Psychological Science. 2014;23:184–188. doi: 10.1177/0963721414531598. [DOI] [Google Scholar]
- Peters G. J., Ruiter R. A., Kok G. Threatening communication: A critical re-analysis and a revised meta-analytic test of fear appeal theory. Health Psychology Review. 2013;7(Suppl. 1):S8–S31. doi: 10.1080/17437199.2012.703527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quick B. L., Bates B. R. The use of gain- or loss-frame messages and efficacy appeals to dissuade excessive alcohol consumption among college students: A test of psychological reactance theory. Journal of Health Communication. 2010;15:603–628. doi: 10.1080/10810730.2010.499593. [DOI] [PubMed] [Google Scholar]
- Quick B. L., Scott A. M., Ledbetter A. M. A close examination of trait reactance and issue involvement as moderators of psychological reactance theory. Journal of Health Communication. 2011;16:660–679. doi: 10.1080/10810730.2011.551989. [DOI] [PubMed] [Google Scholar]
- Quick B. L., Stephenson M. T. Examining the role of trait reactance and sensation seeking on perceived threat, state reactance, and reactance restoration. Human Communication Research. 2008;34:448–476. doi: 10.1111/j.1468-2958.2008.00328.x. [DOI] [Google Scholar]
- Raines S. The nature of psychological reactance revisited: A meta-analytic review. Human Communication Research. 2013;39:47–73. doi: 10.1111/j.1468-2958.2012.01443.x. [DOI] [Google Scholar]
- Rains S. A., Turner M. Psychological reactance and persuasive health communication: A test and extension of the interwined model. Health Communication Research. 2007;33:241–269. doi: 10.1111/j.1468-2958.2007.00298.x. [DOI] [Google Scholar]
- Ringold D. J. Boomerang effects in response to public health interventions: Some unintended consequences in the alcoholic beverage market. Journal of Consumer Policy. 2002;25:27–63. doi: 10.1023/A:1014588126336. [DOI] [Google Scholar]
- Romer D., Peters E., Strasser A. A., Langleben D. Desire versus efficacy in smokers’ paradoxical reactions to pictorial health warnings for cigarettes. PLoS ONE. 2013;8(1):e54937. doi: 10.1371/journal.pone.0054937. [Research Support, Non-U.S. Gov’t] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnoll R. A., James C., Malstrom M., Rothman R. L., Wang H., Babb J., Goldberg M. Longitudinal predictors of continued tobacco use among patients diagnosed with cancer. Annals of Behavioral Medicine. 2003;25:214–221. doi: 10.1207/S15324796ABM2503_07. [Research Support, U.S. Gov’t, P.H.S.] [DOI] [PubMed] [Google Scholar]
- Sperry J. M., Nicki R. M. Cognitive appraisal, self-efficacy, and cigarette smoking behavior. Addictive Behaviors. 1991;16:381–388. doi: 10.1016/0306-4603(91)90046-K. [Clinical Trial Comparative Study Randomized Controlled Trial] [DOI] [PubMed] [Google Scholar]
- Swayampakala K., Thrasher J. F., Hammond D., Yong -H.-H., Bansal-Travers M., Krugman D., Hardin J. Pictorial health warning label content and smokers’ understanding of smoking-related risks-a cross-country comparison. Health Education Research. 2015;30:35–45. doi: 10.1093/her/cyu022. [Research Support, N.I.H., Extramural] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas A., Donnell A., Buboltz W. C. The Hong psychological reactance scale: A confirmatory factor analysis. Measurement and Evaluation in Counseling and Development. 2001;34:2–13. [Google Scholar]
- Thrasher J. F., Carpenter M. J., Andrews J. O., Gray K. M., Alberg A. J., Navarro A., Cummings K. M. Cigarette warning label policy alternatives and smoking-related health disparities. American Journal of Preventive Medicine. 2012;43:590–600. doi: 10.1016/j.amepre.2012.08.025. [Comparative Study Randomized Controlled Trial Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thrasher J. F., Osman A., Abad-Vivero E. N., Hammond D., Bansal-Travers M., Cummings K. M., Moodie C. The use of cigarette package inserts to supplement pictorial health warnings: An evaluation of the Canadian policy. Nicotine & Tobacco Research. 2015;17:870–875. doi: 10.1093/ntr/ntu246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thrasher J. F., Osman A., Moodie C., Hammond D., Bansal-Travers M., Cummings K. M., Hardin J. Promoting cessation resources through cigarette package warning labels: A longitudinal survey with adult smokers in Canada, Australia and Mexico. Tobacco Control. 2015;24(e1):e23–31. doi: 10.1136/tobaccocontrol-2014-051589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thrasher J. F., Pérez-Hernández R., Arillo-Santillán E., Barrientos-Gutierrez I. Towards informed tobacco consumption in Mexico: Effects of pictorial warning labels among smokers. Revista de Salud Pública de México. 2012;54:242–253. [PMC free article] [PubMed] [Google Scholar]
- Thrasher J. F., Swayampakala K., Cummings K. M., Hammond D., Anshari D., Krugman D. M., Hardin J. W. Cigarette package inserts can promote efficacy beliefs and sustained smoking cessation attempts: A Longitudinal assessment of an innovative policy in Canada. Preventive Medicine. 2016;88:59–65. doi: 10.1016/j.ypmed.2016.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thrasher J. F., Villalobos V., Szklo A., Fong G. T., Perez C., Sebrie E., Bianco E. Assessing the impact of cigarette package health warning labels: A cross-country comparison in Brazil, Uruguay and Mexico. Salud Pública De México. 2010;52(Suppl 2):SS206–215. doi: 10.1590/S0036-36342010000800016. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van ’t Riet J., Ruiter R., Werrij M., Vries H. What difference does a frame make? Potential moderators of framing effects and the role of self-efficacy. European Health Psychologist. 2009;11:26–29. [Google Scholar]
- Werrij M. Q., Ruiter R. A., Van ‘t Riet J., De Vries H. Self-efficacy as a potential moderator of the effects of framed health messages. Journal of Health Psychology. 2011;16:199–207. doi: 10.1177/1359105310374779. [Research Support, Non-U.S. Gov’t] [DOI] [PubMed] [Google Scholar]
- Wiium N., Aaro L. E., Hetland J. Psychological reactance and adolescents’ attitudes toward tobacco-control measures. Journal of Applied Social Psychology. 2009;39:1718–1738. doi: 10.1111/j.1559-1816.2009.00501.x. [DOI] [Google Scholar]
- Wilson N., Li J., Hoek J., Edwards R., Peace J. Long-term benefit of increasing the prominence of a quitline number on cigarette packaging: 3 years of Quitline call data. New Zealand Medical Journal. 2010;123:109–111. [PubMed] [Google Scholar]
- Witte K. Fear control and danger control: A test of the extended parallel process model (EPPM) Communication Monographs. 1994;61:113–134. doi: 10.1080/03637759409376328. [DOI] [Google Scholar]
- Witte K., Allen M. A meta-analysis of fear appeals: Implications for effective public health campaigns. Health Education & Behavior. 2000;27:591–615. doi: 10.1177/109019810002700506. [DOI] [PubMed] [Google Scholar]
- World Health Organization . Guidelines for implementation of Article 11 of the WHO Framework Convention on Tobacco Control (packaging and labelling of tobacco products) Geneva, Switzerland: World Health Organization; 2008. [Google Scholar]
- Wright R. A., Wadley V. G., Danner M., Phillips P. N. Persuasion, reactance, and judgments of interpersonal appeal. European Journal of Social Psychology. 1992;22:85–91. doi: 10.1002/ejsp.2420220109. [DOI] [Google Scholar]
- Yan M. ITC Project technical report. Waterloo, ON, Canada: University of Waterloo; 2007. Test–retest reliability and predictive validity for selected questions in the ITC four country survey . [Google Scholar]


