Abstract
Purpose
This study was conducted to evaluate the results of internal fixation for stable femoral neck fractures occurring in patients over 65 years old.
Materials and Methods
Between 2008 and 2014, we evaluated 25 patients over 65 years old with Garden type 1 and 2 femoral neck fractures that were treated with internal fixation after a minimum follow up of 1 year. There were 5 males and 20 females and the average age was 72.3 years (range, 65-84 years) at the time of surgery. Fracture site union, horizontal shortening and complications were evaluated as radiographic parameters and change of walking ability (as measured using Koval walking ability score) was investigated as a clinical parameter.
Results
Union of fracture site was achieved in 24 out of the 25 cases (96.0%). The average length of horizontal shortening was 6.5 mm (range, 0.2-19.7 mm). At final follow up, 3 cases experienced complications: nonunion (n=1), avascular necrosis (n=1), and subtrochanteric fracture after minor trauma (n=1). Walking ability decreased an average of 1 step at the final follow up.
Conclusion
Internal fixation for stable femoral neck fractures occurring in patients over 65 years showed satisfactory union rates. However, care should be taken with this technique given the possibility of decreased walking ability resulting from horizontal shortening.
Keywords: Femur, Stable fracture, Internal fracture fixation
INTRODUCTION
The incidence of femoral neck fractures, one of the leading causes of death in elderly patients is increasing as average life spans and prevalence of osteoporosis continue to rise1,2). Fracture site displacement, patient age, comorbid disorders, pre-fracture activity level are some of the critical factors in determining the clinical practice for treating femoral neck fractures3). Compared to internal fixation, hip arthroplasty is more commonly performed in elderly patients with displaced femoral neck fractures because of more significant improvements in pain and early ambulation, lower rates of re-operation and other advantages4,5,6). Internal fixation is considered a better treatment choice for younger patients7,8). Additionally, internal fixation has traditionally been the preferred method for treating incomplete fractures, stable fractures (Garden type 1) or undisplaced fractures (Garden type 2) regardless of age, and satisfactory outcomes have been achieved including relatively short operation time and joint preservation9,10,11,12). However, some authors have reported a high re-operation rate in older patients with undisplaced fractures, because of fixation failure, avascular necrosis of the femoral head and others13,14,15,16). Others have suggested that a postoperative decrease in abductor moment arm may reduce mobility and quality of life17). For these reasons, the optimal treatment strategy for elderly patients with stable femoral neck fractures remains unclear.
In this study, we used internal fixation for the treatment of stable femoral neck fractures occurring in patients over 65 year old. Follow ups included: i) monitoring for fracture union using radiography, ii) measuring for horizontal shortening at final follow up, iii) tracking complications, and iv) investigating clinical changes in walking ability between preoperative and at final follow-up.
MATERIALS AND METHODS
We obtained the approval from institutional review board of Keimyung University Dongsan Medical Center to search surgical database of our institution to identify cases for the current study. Eighty-five patients underwent internal fixation for femoral neck fracture from January 2008 to December 2014. Thirty-one patients were age 65 years or older and considered for this study. Of these, 6 were excluded because of death within 1 year due to underlying disease regardless of fracture surgery (n=3) or because they were not available for follow ups (n=3). The remaining 25 patients with a minimum follow-up of 1 year were included in this retrospective study. Fractures occurred after a slip or fall accident in all but 1 case. Five of the subjects were men and the remaining 20 were women; their mean age was 72.3 years (range, 65-84 years) at the time of surgery. The average body mass index was 22.1 kg/m2 (range, 16.0-29.6 kg/m2). Bone mineral density test was performed in 20 cases; 16 had osteoporosis and 4 had osteopenia. The average follow-up period was 32 months (range, 12-183 months). Stable femoral neck fractures were defined as Garden types 1 and 2 according to the Garden classification18); 16 were type 1 and 9 were type 2.
In all cases, surgeries were performed under general anesthesia on a fracture table using an image intensifier, and internal fixation was applied without attempting additional fracture reduction. Fixation was conducted using: i) 3 cannulated screws in 10 patients between 2008 and 2009, and ii) blade-type compression hip screws in 15 patients after 2010 (Table 1). Wheelchair ambulation was allowed on the second and third postoperative days, and partial weight bearing ambulation was permitted using assistive devices such as canes from the first postoperative week. Weight bearing was gradually increased according to extent of fracture union as determined using radiography.
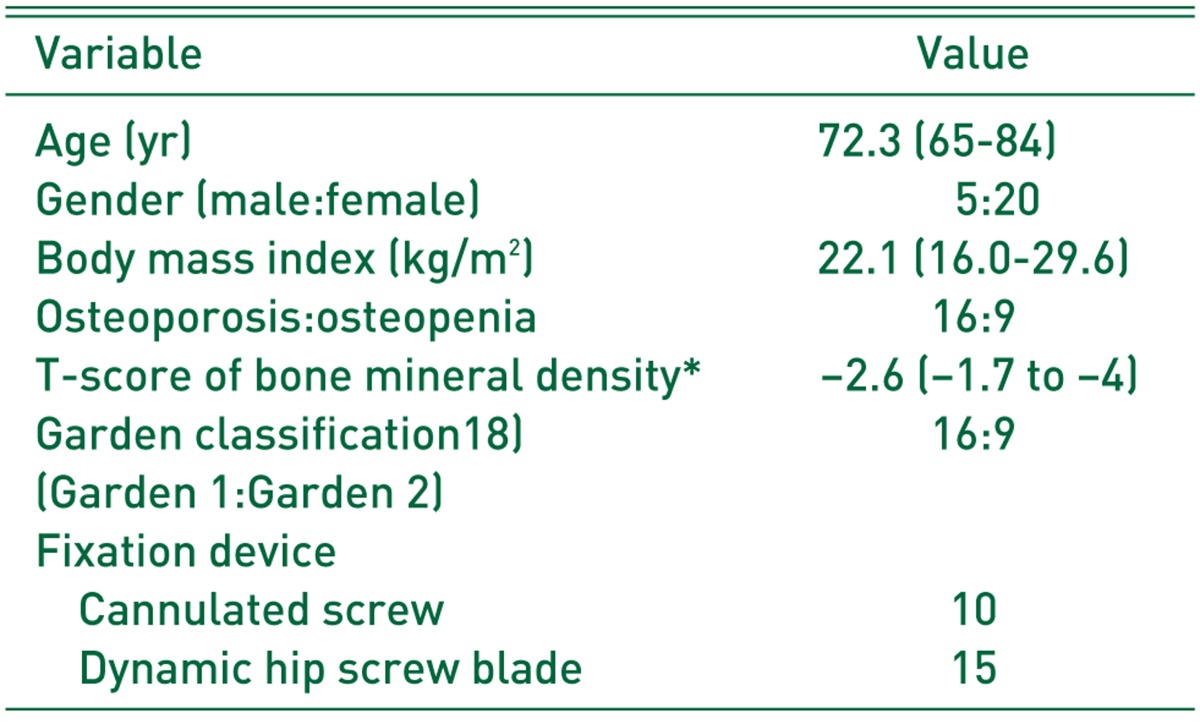
Table 1. Demographic Data of Study Cohort (n=25).
Values are presented as mean (range) or number only.
*Measured in twenty patients.
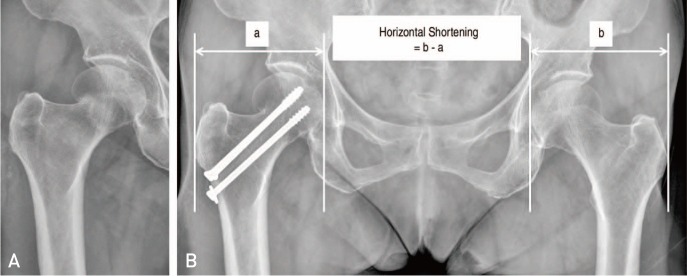
Using radiography, union at the fracture site was checked at follow-up on a regular basis. Nonunion was defined as: i) displacement of the fracture site by more than 1 cm without fracture union, ii) change in the angle of cannulated screws by more than 5%, iii) screw or blade back-out by more than 2 cm, or iv) femoral perforation; these measurements were made at the 3-month follow-up radiography visits19). To assess decreases in abductor moment arm, the difference in length between the healthy and unhealthy sides (horizontal shortening) was quantified by measuring the distance from medial border of the femoral head to lateral border of the greater trochanter at the final follow-up radiography visit following bone union17) (Fig. 1). We also examined patients to determine if other complications were present. Pre-fracture and final follow-up ambulatory levels were evaluated as a clinical parameter according to the Koval classiflcation20) which grades ambulatory ability from independent community ambulatory (grade 1) to nonfunctional ambulatory (grade 7).
Fig. 1. (A) Preoperative radiograph of 77 years old female shows stable femoral neck fracture (Garden type 1). (B) Radiograph taken 29 months after internal fixation with cannulated screws shows well united fracture site but decreased horizontal shortening more than 6.5 mm compared to opposite femur. The horizontal shortening was measured as the difference of length from medial border of femoral head to lateral border of greater trochanter between contralateral femur (b) and ipsilateral femur (a).
All statistical analyses were performed using IBM SPSS Statistics ver. 20 (IBM Co., Armonk, NY, USA). Differences were analyzed with the Mann-Whitney U-test and Wilcoxon signed rank test. P-values of less than 0.05 were considered statistically significant.
RESULTS
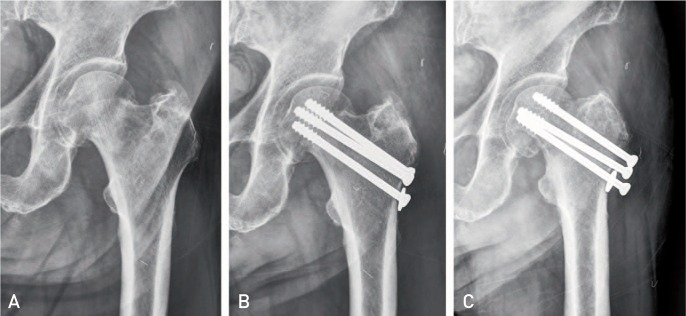
Bone union at the fracture site was obtained in 24 out of 25 cases (96.0%) at final follow-up (Fig. 1, 2), and the average time for bone union was 4.3 months (range, 3-6 months). On the final follow-up radiographs, the average horizontal shortening was 6.5 mm (range, 0.2-19.7 mm). Horizontal shortening was greater than 6.5 mm in 5 cases and less than 6.5 mm in 20 cases. As seen in Fig. 3, 3 patients experienced complications; nonunion (n=1), avascular necrosis (n=1), and subtrochanteric fracture after minor trauma (n=1). In all cases with complications, fracture site was fixed with cannulated screws, but no statistical difference was shown between fixation devices (P=0.22). Total hip arthroplasty was performed in patients with nonunion and avascular necrosis, and re-fixation with compression screws and metal plates was done in those with subtrochanteric fracture.
Fig. 2. (A) Preoperative radiograph of 67 years old male shows stable femoral neck fracture (Garden type 2). (B) Radiograph taken 36 months after internal fixation shows well united fracture site.
Fig. 3. (A) Preoperative radiograph of 84 year old female shows stable femoral neck fracture (Garden type 2). (B) In situ fixation with cannulated screws was done within 24 hours. (C) Radiograph taken 5 months after internal fixation shows nonunion of fracture site.
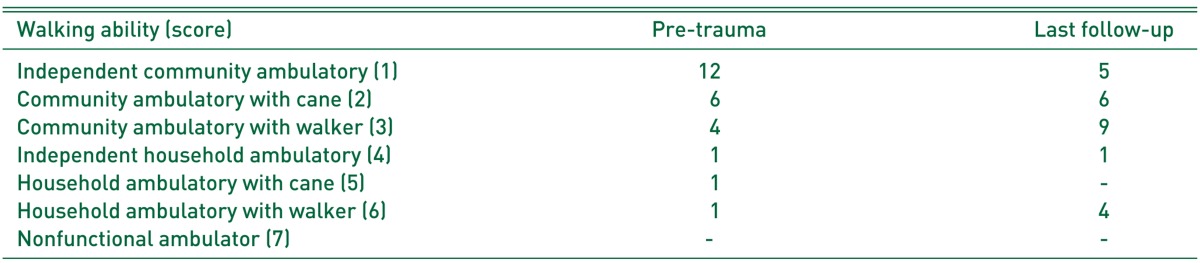
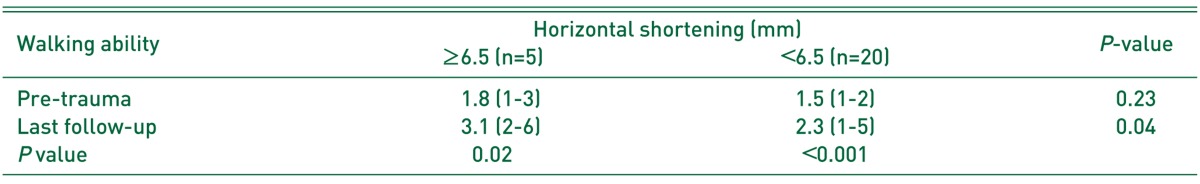
Using the Koval classification20), walking ability of the patients before surgeries were as follows; independent community ambulatory (grade 1; n=12), community ambulatory with cane (grade 2; n=10), household ambulatory independently or with assistive devices (n=3). However, at the final follow up, these changed to 5, 15 and 5 cases, respectively. The average score increased from 2.0 at pre-fracture to 2.9 at the final follow up. On average, walking ability decreased 1 step (Table 2). The average score increased from 1.8 (range, 1-3) at prefracture to 3.1 (range, 1-5) at the final follow up in 5 patients with horizontal shortening by more than 6.5 mm, and from 1.5 (range, 1-4) to 2.3 (range, 1-5) in 20 patients with horizontal shortening less than 6.5 mm. Statistically significant decreases in walking ability because of a decrease in abductor moment arm due to horizontal shortening were observed in both groups (P=0.02, P<0.001). A statistically significant decrease in walking ability was seen in patients with horizontal shortening by more than 6.5 mm at the final follow up (P=0.04) (Table 3).
Table 2. Change of Walking Ability by Koval20) between Pre-trauma and Last Follow-up (n=25).
Table 3. Comparison of Walking Ability by Koval20) according to Horizontal Shortening.
DISCUSSION
Hip fracture is one of the leading causes of death in elderly patients with 5-year mortality rate up to 50%1,21). Femoral neck and intertrochanteric fractures are becoming more prevalent later in life due an increase in average life spans, an increased prevalence of osteoporosis and other reasons. Treatment options for femoral neck fractures include internal fixation, hip arthroplasty (hip hemiarthroplasty, total hip arthroplasty) and others, and may vary depending on the displacement of fracture site, age, comorbid disorders, prefracture activity level and operator's preference3,14).
Hip arthroplasty is more commonly performed in elderly patients with displaced femoral neck fractures than internal fixation because of more significant improvements in pain and early ambulation, less re-operation rate and other advantages4,5,6). Although internal fixation has traditionally been the preferred treatment for stable femoral neck fractures in older patients and has produced satisfactory outcomes, the optimal treatment strategy still remains controversial as some authors have reported a high fixation failure leading to re-operation9,11,13,14,15,22,23,24). Chen et al.9) performed internal fixation using cannulated screws in patients who are over 80 years old and who have stable femoral neck fractures classified as Garden type 1 or 2. This group suggested that this treatment strategy is easy, safe, inexpensive and useful in this patient population and they report achieving a union rate of 94.59% and a success rate of 83.78% at two-year follow-up. After analyzing 14,757 cases of hip fractures registered in the Norwegian Patient Registry and reporting a 1-year survival rate of 89%, Gjertsen et al.11) also propose that internal fixation is the recommended surgical procedure for older patients with undisplaced femoral fractures. In the present study, despite a small sample size, a satisfactory level of bone union (96.0%) was achieved using internal fixation in 25 patients over 65 years old with stable femoral neck fractures. On the contrary, Kain et al.13) reported a relatively high re-operation rate of 11.6% due to complications (avascular necrosis of the femoral head, nonunion, and fixation failure) of internal fixation among 121 patients over 65 years old with stable femoral neck fractures at a mean follow-up of 9 months. Parker et al.15) also reported an increased risk of nonunion following internal fixation in elderly female patients. Moreover, some studies suggest that primary hip arthroplasty could be an alternative choice for some patients because the incidence of complications requiring re-operation following internal fixation ranged between 18.2-34.6% in over 70-year-old patients with stable femoral neck fractures14,23,24,25). In this study, after internal fixation in elderly patients with a mean age of 72 years, the re-operation rate was relatively high at 12.0% due to nonunion, avascular necrosis of the femoral head and subtrochanteric fracture.
Ultimate treatment goals for elderly patients with femoral neck fractures are recovery to pre-fracture levels of physical and social functioning. Choo et al.17) achieved satisfactory radiographic results in 83% of patients with femoral neck fractures (n=47) with a mean age of 72 years and by performing internal fixation for femoral neck fractures. However, they observed that a decrease in abductor moment arm caused by horizontal shortening of the femoral neck may reduce postoperative quality of life and ambulation. Although we observed a high union rate of 96.0% in our study, an average decrease in ambulatory ability by one grade (Koval) was observed at the final follow up. A statistically significant decrease in walking ability was seen in patients with an average horizontal shortening of 6.5 mm, and additional studies are warranted to further investigate this outcome.
There are several limitations to note in the present study. This research was a retrospective study with a small sample size and two distinct surgical devices. This study was also limited by the lack of a comparator arm, no assessment of underlying diseases, and no analysis of factors affecting horizontal shortening. However, strengths of this study are that all surgical procedures were done by a single surgeon and that changes in quality of life after fractures were evaluated by examining the correlation between radiographic measurements and clinical changes in walking ability. However, long-term comparative studies with larger sample sizes are warranted to determine the best treatment strategy for elderly patients with stable femoral neck fractures.
CONCLUSION
A satisfactory level of bone union (96.0%) was achieved by performing internal fixation in patients over 65 years old with stable femoral neck fractures. However, the risk of decreased walking ability because of horizontal shortening and other reasons is possible, and warrants close attention to potential complications.
Footnotes
CONFLICT OF INTEREST: The authors declare that there is no potential conflict of interest relevant to this article.
References
- 1.Holt G, Smith R, Duncan K, Finlayson DF, Gregori A. Early mortality after surgical fixation of hip fractures in the elderly: an analysis of data from the scottish hip fracture audit. J Bone Joint Surg Br. 2008;90:1357–1363. doi: 10.1302/0301-620X.90B10.21328. [DOI] [PubMed] [Google Scholar]
- 2.Sikand M, Wenn R, Moran CG. Mortality following surgery for undisplaced intracapsular hip fractures. Injury. 2004;35:1015–1019. doi: 10.1016/j.injury.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 3.Shah AK, Eissler J, Radomisli T. Algorithms for the treatment of femoral neck fractures. Clin Orthop Relat Res. 2002;(399):28–34. doi: 10.1097/00003086-200206000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Waaler Bjørnelv GM, Frihagen F, Madsen JE, Nordsletten L, Aas E. Hemiarthroplasty compared to internal fixation with percutaneous cannulated screws as treatment of displaced femoral neck fractures in the elderly: cost-utility analysis performed alongside a randomized, controlled trial. Osteoporos Int. 2012;23:1711–1719. doi: 10.1007/s00198-011-1772-1. [DOI] [PubMed] [Google Scholar]
- 5.Gjertsen JE, Vinje T, Engesaeter LB, et al. Internal screw fixation compared with bipolar hemiarthroplasty for treatment of displaced femoral neck fractures in elderly patients. J Bone Joint Surg Am. 2010;92:619–628. doi: 10.2106/JBJS.H.01750. [DOI] [PubMed] [Google Scholar]
- 6.Leighton RK, Schmidt AH, Collier P, Trask K. Advances in the treatment of intracapsular hip fractures in the elderly. Injury. 2007;38(Suppl 3):S24–S34. doi: 10.1016/j.injury.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 7.Bhandari M, Devereaux PJ, Tornetta P, 3rd, et al. Operative management of displaced femoral neck fractures in elderly patients. An international survey. J Bone Joint Surg Am. 2005;87:2122–2130. doi: 10.2106/JBJS.E.00535. [DOI] [PubMed] [Google Scholar]
- 8.Sendtner E, Renkawitz T, Kramny P, Wenzl M, Grifka J. Fractured neck of femur--internal fixation versus arthroplasty. Dtsch Arztebl Int. 2010;107:401–407. doi: 10.3238/arztebl.2010.0401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen WC, Yu SW, Tseng IC, Su JY, Tu YK, Chen WJ. Treatment of undisplaced femoral neck fractures in the elderly. J Trauma. 2005;58:1035–1039. discussion 1039. doi: 10.1097/01.ta.0000169292.83048.17. [DOI] [PubMed] [Google Scholar]
- 10.Bjørgul K, Reikerås O. Outcome of undisplaced and moderately displaced femoral neck fractures. Acta Orthop. 2007;78:498–504. doi: 10.1080/17453670710014149. [DOI] [PubMed] [Google Scholar]
- 11.Gjertsen JE, Fevang JM, Matre K, Vinje T, Engesæter LB. Clinical outcome after undisplaced femoral neck fractures. Acta Orthop. 2011;82:268–274. doi: 10.3109/17453674.2011.588857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Conn KS, Parker MJ. Undisplaced intracapsular hip fractures: results of internal fixation in 375 patients. Clin Orthop Relat Res. 2004;(421):249–254. [PubMed] [Google Scholar]
- 13.Kain MS, Marcantonio AJ, Iorio R. Revision surgery occurs frequently after percutaneous fixation of stable femoral neck fractures in elderly patients. Clin Orthop Relat Res. 2014;472:4010–4014. doi: 10.1007/s11999-014-3957-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Han SK, Song HS, Kim R, Kang SH. Clinical results of treatment of garden type 1 and 2 femoral neck fractures in patients over 70-year old. Eur J Trauma Emerg Surg. doi: 10.1007/s00068-015-0528-6. Published online Apr 18, 2015. [DOI] [PubMed] [Google Scholar]
- 15.Parker MJ, Raghavan R, Gurusamy K. Incidence of fracture-healing complications after femoral neck fractures. Clin Orthop Relat Res. 2007;458:175–179. doi: 10.1097/BLO.0b013e3180325a42. [DOI] [PubMed] [Google Scholar]
- 16.Song HK, Lee JJ, Oh HC, Yang KH. Clinical implication of subgrouping in valgus femoral neck fractures: comparison of 31-B1.1 with 31-B1.2 fractures using the OTA/AO classification. J Orthop Trauma. 2013;27:677–682. doi: 10.1097/BOT.0b013e31828e18c5. [DOI] [PubMed] [Google Scholar]
- 17.Choo SK, Oh HK, Kim JI, Lee HD, Jang GR. The result of osteosynthesis for femur neck fracture in old age patients. J Korean Hip Soc. 2011;23:32–38. [Google Scholar]
- 18.Garden RS. Low-angle fixation in fractures of the femoral neck. J Bone Joint Surg Br. 1961;43:647–663. [Google Scholar]
- 19.Chang JD, Lee WS. Chapter 4, Femoral neck fracture. In: Park MS, Lee KJ, editors. Textbook of the hip. 1st ed. Seoul: Koonja; 2014. pp. 805–817. [Google Scholar]
- 20.Koval KJ, Skovron ML, Aharonoff GB, Meadows SE, Zuckerman JD. Ambulatory ability after hip fracture. A prospective study in geriatric patients. Clin Orthop Relat Res. 1995;(310):150–159. [PubMed] [Google Scholar]
- 21.Iorio R, Healy WL, Appleby D, Milligan J, Dube M. Displaced femoral neck fractures in the elderly: disposition and outcome after 3- to 6-year follow-up evaluation. J Arthroplasty. 2004;19:175–179. doi: 10.1016/j.arth.2003.09.002. [DOI] [PubMed] [Google Scholar]
- 22.Parker MJ, White A, Boyle A. Fixation versus hemiarthroplasty for undisplaced intracapsular hip fractures. Injury. 2008;39:791–795. doi: 10.1016/j.injury.2008.01.011. [DOI] [PubMed] [Google Scholar]
- 23.Seo JS, Shin SK, Jun SH, Cho CH, Lim BH. The early result of cementless arthroplasty for femur neck fracture in elderly patients with severe osteoporosis. Hip Pelvis. 2014;26:256–262. doi: 10.5371/hp.2014.26.4.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim YC, Lee JY, Song JH, Oh S. The result of in sit pinning for valgus impacted femoral neck fractures of patients over 70 years old. Hip Pelvis. 2014;26:263–268. doi: 10.5371/hp.2014.26.4.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Clement ND, Green K, Murray N, Duckworth AD, McQueen MM, Court-Brown CM. Undisplaced intracapsular hip fractures in the elderly: predicting fixation failure and mortality. A prospective study of 162 patients. J Orthop Sci. 2013;18:578–585. doi: 10.1007/s00776-013-0400-7. [DOI] [PubMed] [Google Scholar]