Highlights
-
•
Melanoma skeletal muscle metastasis (MSMM) are exceptional.
-
•
Despite all new advances in melanoma therapy, cure for most MSMM is still elusive.
-
•
This is the third case of an isolated metastasis of melanoma to the rectus abdominis muscle published in the literature.
-
•
Radical compartmental surgery should be considered for selected stage IV melanoma patients, with isolated rectus abdominis MSMM, whose disease could be amenable to complete resection, in order to extend median survival.
-
•
Nowadays, the use of synthetic meshes seems to be one of the best choices for repairing the abdominal wall defect.
Keywords: Melanoma, Metastasis, Rectus abdominis muscle, SPECT/CT, Mesh reconstruction
Abstract
Introduction
Melanoma is a health problem world-wide. Its incidence has tripled in the last decade. The main cause of death in melanoma patients is widespread metastases. It can metastasize to almost every organ. However, melanoma skeletal muscle metastases (MSMM) are exceptional, and only two cases of MSMM to rectus abdominis muscles have been previously published. Regardless of all new advances seen in melanoma therapy, cure for most MSMM is still elusive. Surgical approaches are still not well defined.
Presentation of case
A 35-year-old woman had been previously operated of an ulcerated scapular melanoma (Clark level III, Breslow 2.3 mm) in January 2014. Subsequently she underwent a sentinel lymph node which resulted negative. Twenty months later, a CT scan revealed a well-enhanced nodule of 25 mm in the right rectus abdominis, without any other metastases. The PET-CT uptake was pathologic (SUV maximum of 13.16). An ultrasound-guided biopsy confirmed it was a metastatic melanoma. A radical compartmental resection of the right rectus abdominis muscle was performed. The abdominal wall was reconstructed with two polypropylene meshes buried preperitoneally. The final histologic diagnosis of the specimen proved to be a metastasis of melanoma.
Discussion
Surgery is the only potentially curative therapy for patients with isolated MSMM. The ultimate goal of negative resection margins, in order to avoid local recurrences, is paramount in those difficult cases.
Conclusion
Radical compartmental surgery should be considered for selected stage IV melanoma patients whose disease could be amenable to complete resection, in order to extend median survival.
1. Introduction
The incidence of melanoma has been increasing faster than that of any other cancer. It has nearly tripled over the last ten years. It caused 73,780 new cases in the United States with 9960 deaths in 2015 [1]. Melanoma is known to be more aggressive than most other neoplasms. Widespread metastasis is the main cause of death in melanoma patients. The major sites of distant metastases of melanoma are adjacent skin, subcutaneous fat and lymph nodes. Haematogenous spread is mainly to lung followed then by liver, brain, bone and small bowel. Melanoma metastasis to skeletal muscle (MMSM) remains a relatively unusual event. Moreover, metastatic lesions to rectus abdominis muscles are extremely rare, only two cases have been previously published [2], [3].
The number of detected MMSM has increased since the wide-spread use of computed tomography (CT) and positron emission tomography/computed tomography (PET/CT) as the imaging modalities of choice in diagnostic oncologic follow-up. MMSM may be more prevelant than previously estimated [4]. MMSM do occur, and they can have an important impact on staging, prognosis, and patient management, especially when they are the only site of metastatic disease.
The treatment of metastatic melanoma continues to be a challenging disease that portends a poor prognosis with less than 12 months of median survival, and a 10–15% 5-year survival rate. Systemic therapy is the mainstay of treatment for most patients. Treatment of MMSM remains still elusive.
Patients with limited burden of disease do best with surgical treatment. Surgical metastasectomy has the unique potential to remove the whole tumor in patients with fully resectable oligometastatic disease [5]. Complete surgical resection may extend median survival, but still there are not uniform criteria for surgical treatment of metastatic abdominal wall lesions.
2. Presentation of case
A 35-year-old woman had been previously operated of an ulcerated scapular skin melanoma (Clark III, Breslow 2.3 mm) in January 2014, and she was subsequentially treated with a sentinel lymph node (SLN) biospsy, which was negative with no residual disease. Twenty months later, and during her follow-up, a routine regular dynamic CT scan revealed a well-enhanced solid nodule in her right rectus abdominis muscle, measuring 25 mm of maximum diameter (Fig. 1), without any other distant metastasis. This lesion was suspicious to be pathologic on the PET/CT which showed an increased metabolic activity, maximum standardized uptake values (SUVmax) of 13.16, related to an isolated lesion in the right rectus abdominis muscle (Fig. 2, Fig. 3). An ultrasonography-guided biopsy of the nodular mass, confirmed it was a metastatic melanoma (HMB-45 positve, MelanA positive, Protein S-100 positive).
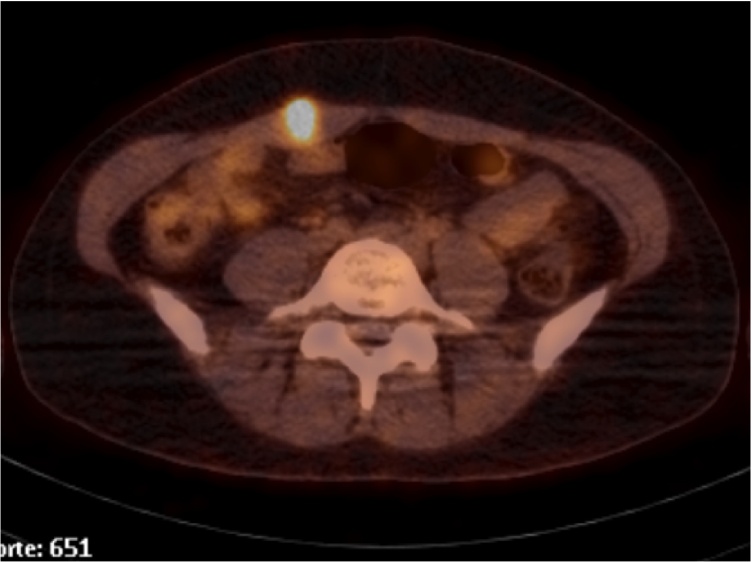
Fig. 1.
Abdominal contrast-enhanced CT scan showing a detailed rim well-enhanced nodule in the right rectus abdominis muscle with central hypoattenuation.
Fig. 2.
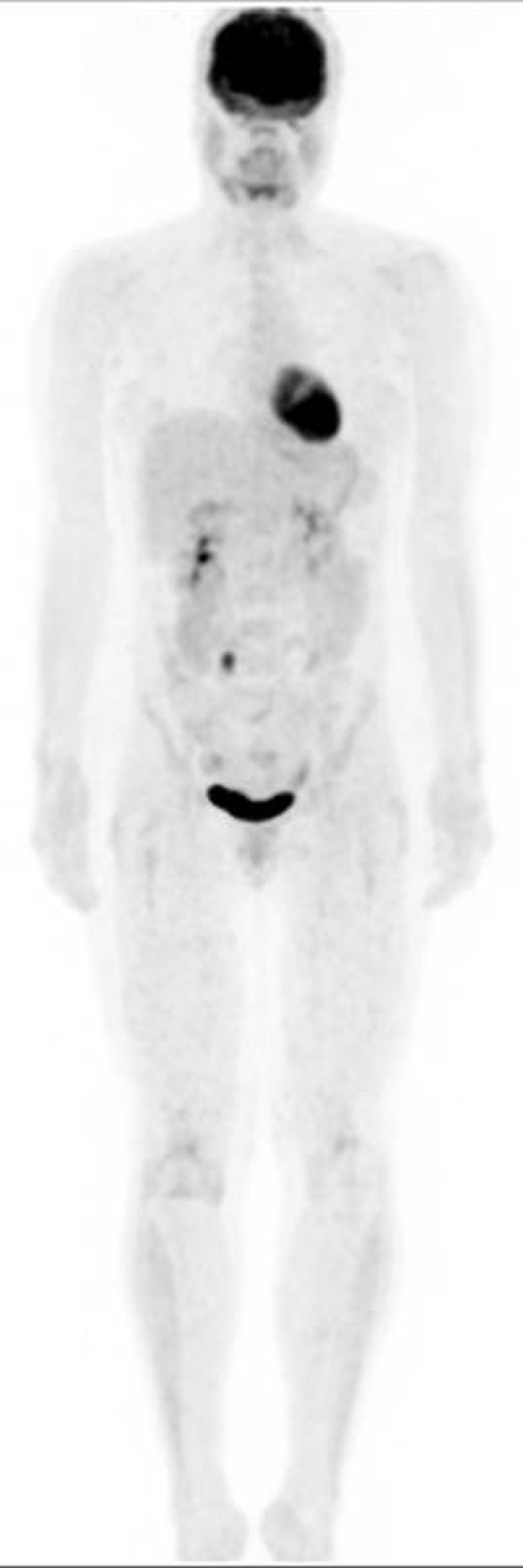
Whole-body bone PET/CT scan.
Fig. 3.
Selected transaxial slice of PET/CT showing a focus of increased metabolic activity in the right rectus abdominis muscle.
She was remitted to our Unit for surgical evaluation. A radical wide en-block compartmental extraperitoneal resection of her right rectus abdominis muscle was undertaken. The abdominal wall defect was reconstructed with two overlapped preperitoneal retromuscular Composite Parietex® meshes.
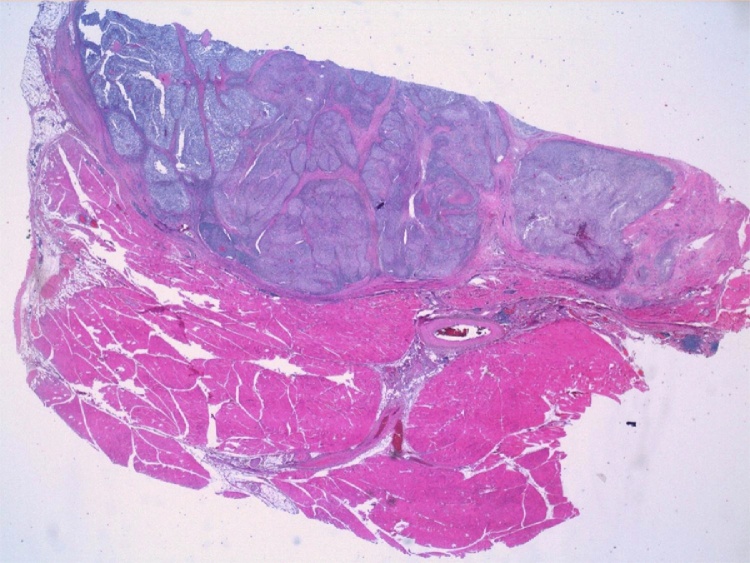
The histologic diagnosis of the specimen showed a tumor nodule measuring 6 cm in its greatest diameter in the right rectus abdominis muscle, which infiltrated the muscle and the addipose tissue (Fig. 4). The tumor had a solid and firm pattern with irregular clusters of poorly differentiated tumor cells, polygonal or ovoid in shape. They had large cytoplasms, irregular hyperchromatic nuclei with noticeably anisocariosis, and occasional atypical mitoses.
Fig. 4.
The pathology of the right rectus abdominis muscle definitive specimen. The skeletal muscle showed metastatic tumor cells from melanoma (HE macro-micro).
Inmunohistochemistry confirmed it was HMB-45 positve, MelanA positive, Protein S-100 positive, and Ki 67 in more than 50% of the tumor.
Braf V600E and V600E/K mutation analyses were negative. The diagnosis of sarcoma of clear cells was rejected, due to a negative EWSR1 re-arrangement of the locus of the gen (22q12) [6]. The ultimate histologic diagnosis of the specimen was consistent with metastasis of melanoma.
3. Discussion
MMSM tend to be found in patients with advanced-stage neoplasms. They occur often in patients with widely disseminated disease and have no influence on the treatment of primary disease. MMSM per se is evidence of systemic spread, and it is a worse prognosis than a metastasis to any other organ. Exceptionally, MMSM may present as an isolated distant metastasis [2], [3].
Most MSMM are usually asymptomatic. On CT, they are manifested usually as a rim contrast-enhanced CT appearance. On PET/CT they translate an intramuscular focus of abnormally increased metabolic activity. Any incidental lesion discovered during the follow-up of melanoma patients, as it happened in our case, should be considered suspicious of metastasis, and confirmation of the diagnosis with ultrasound-guided biopsy should always be sought, as tissue sampling is essential.
Treatment of the patients with isolated MMSM is challenging, and it must be based on the clinical condition of the patient. Despite all new advances in melanoma therapy, cure is usually not a realistic aim.
Surgery is the only potentially curative therapy for patients with isolated MMSM, with the ultimate goal of negative resection margins in order to avoid local recurrences. A radical wide en-block compartmental extraperitoneal resection of the rectus abdominis muscle is proposed to obtain a survival benefit.
Success should be assessed under caution in view of the frequent development of recurrence and metastases after the initial therapy [4].
After harvesting the rectus muscle several options are available for repairing the abdominal defect. The use of synthetic meshes seems to be one of the best choices nowadays. It offers excellent structural support, allowing a strong dynamic reconstruction of the abdominal wall. Our patient was able to return to her previous level of normal, routine abdominal functions after two months postoperatively.
4. Conclusion
MMSM may be more prevelant than previously estimated, although to the best of our knowledge, this is the third case of an isolated metastasis of melanoma to the rectus abdominis muscle published in the literature.
Any benefit of surgery in these patients depends on the complete resection of the disease. The ultimate goal of surgical negative resection margins in patients with single MSMM is paramount.
Radical compartmental surgery should be considered for selected stage IV melanoma patients with sole rectus abdominis MSMM, whose disease could be amenable to complete resection, in order to extend median survival. However, success should be assessed always under caution.
Conflicts of interest
There are no conflicts of interest.
Funding
None.
Ethical approval
Ethical approval not required.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
All the Authors have contributed on the study design, data analysis, and writing the paper. All authors (A. Gómez Portilla, A. Cruz, N. Juan, P. Malo, E. López de Heredia, M. Larrañaga), have approved the submission of this article for publication.
Guarantor
Alberto Gómez Portilla.
Contributor Information
Alberto Gómez Portilla, Email: agomezpor@gmail.com.
Anais Cruz, Email: anais.crznz@gmail.com.
Nuria Juan, Email: nuriajuand@gmail.com.
Palmira Malo, Email: PALMIRA.MALODIEZ@osakidetza.eus.
Eduardo López de Heredia, Email: eduarmentia@gmail.com.
Maitane Larrañaga, Email: maitanelz@hotmail.com.
References
- 1.Siegel R.L., Miller K.D., Jemal A. Cancer statistics CA 2015. Cancer J. Clin. 2015;65:5–29. doi: 10.3322/caac.21254. [DOI] [PubMed] [Google Scholar]
- 2.Namikawa K., Yamazaki N. Metastatic melanoma on the abdominal wall image of the month. Jpn. J. Clin. Oncol. 2009;39(5):336. doi: 10.1093/jjco/hyp042. [DOI] [PubMed] [Google Scholar]
- 3.Hichem A., Saber R., Bassem M., Alifa D., Lamia R.M., Ayoub Z. Mélanome du muscle droit de l’abdomen: à propos d’un cas. La Tunisie Medicale. 2014;92:432–433. [PubMed] [Google Scholar]
- 4.Arpaci T., Ugurluer G., Akbas T., Arpaci R.B., Serin M. Imaging of the skeletal muscle metastases. Eur. Rev. Med. Pharmacol. Sci. 2012;16:2057–2063. [PubMed] [Google Scholar]
- 5.Caudle A.S., Ross M.I. Metastasectomy for stage IV melanoma: for whom and how much? Surg. Oncol. Clin. N. Am. 2011;20:133–144. doi: 10.1016/j.soc.2010.09.010. [DOI] [PubMed] [Google Scholar]
- 6.Yang L., Chen Y., Cui T., Knösel T., Zhang Q., Geier C. Identification of biomarkers to distinguish clear cell sarcoma from malignant melanoma. Hum. Pathol. 2012;43:1463–1470. doi: 10.1016/j.humpath.2011.10.022. [DOI] [PubMed] [Google Scholar]