Highlights
-
•
Laparoscopic surgery for colon and liver is also widely recognized to be safe.
-
•
Simultaneous laparoscopic resection of colon cancer and synchronous liver metastases is safe.
-
•
Simultaneous laparoscopic resection in elderly patients is feasible and safe.
Abbreviations: CA19-9, carbohydrate antigen 19-9; CEA, carcinoembryonic antigen; CRC, colorectal cancer; Hb, hemoglobin; Ht, hematocrit; PS, performance status; RBC, red blood cell count; RFA, radiofrequency ablation; SLM, synchronous liver metastases
Keywords: Colorectal cancer, Liver metastasis, Synchronous colorectal liver metastasis, Simultaneous laparoscopic resection, Case report
Abstract
Introduction
The laparoscopic resection of colorectal cancer and laparoscopic liver surgery are widely considered to be safe. Recently, it has been reported that the simultaneous laparoscopic resection of primary colorectal cancer and liver metastasis is technically feasible and safe when it is performed at experienced centers. However, the feasibility of simultaneous laparoscopic procedures for colorectal cancer and synchronous colorectal liver metastases in elderly patients has not been studied sufficiently. In this study, two cases in which elderly patients with colorectal cancer and synchronous liver metastases were treated with simultaneous laparoscopic resection are reported.
Presentation of cases
An 83-year-old female was diagnosed with ascending colon cancer and synchronous hepatic metastases. Simultaneous laparoscopic resection of the primary colon cancer and the liver metastasis was performed. Another tiny hepatic metastasis was subsequently detected in the right hepatic lobe. It was treated with hand-assisted radiofrequency ablation (RFA). The total operative time was 470 min, and 340 g of intraoperative blood loss occurred. The other case involved a 78-year-old male who was diagnosed with ascending colon cancer and synchronous hepatic metastasis in the right hepatic lobe. Simultaneous laparoscopic resection of the primary colon tumor and liver metastasis was performed. The total operative time was 471 min, and 240 g of intraoperative blood loss occurred. The postoperative courses of both patients were uneventful.
Discussion and conclusion
Our results indicate that simultaneous laparoscopic resection of colorectal cancer and synchronous liver metastases is feasible and safe in elderly patients.
1. Introduction
Colorectal cancer (CRC) is the fourth most common type of cancer worldwide [1], and metastases from CRC most frequently occur in the liver. Fourteen to twenty percent of CRC patients develop synchronous liver metastases (SLM), and approximately 25% of CRC patients have metachronous hepatic metastases [2], [3], [4]. However, it has been reported that curative resection aids long-term survival in CRC patients with liver metastases [5]. Recently, laparoscopic surgery has been performed as a minimally invasive treatment for various cancers including CRC around the world. Several randomized controlled trials comparing laparoscopic colectomy with open surgery have demonstrated that laparoscopic surgery is a safe and more effective treatment for colon cancer than open surgery [6], [7], [8], [9]. In addition, laparoscopic liver surgery is also widely recognized to be safe [10], [11]. In 2015, it was reported that the simultaneous laparoscopic resection of CRC and SLM is technically feasible and safe [12]. However, the feasibility of simultaneous laparoscopic procedures for CRC and SLM in cases involving elderly patients has not been studied sufficiently. In this study, two cases in which elderly patients with CRC and SLM were treated with simultaneous laparoscopic resection are reported.
2. Presentation of case 1
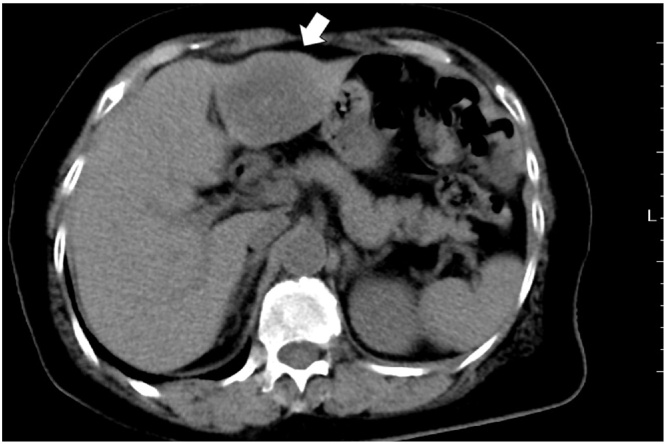
An 83-year-old female had an operation for a trigger finger. She presented with right hypochondrial pain during hospitalization. Hepatic tumors were detected during abdominal ultrasonography and computed tomography. The patient had a history of bronchial asthma. A physical examination demonstrated the following characteristics: height, 129.3 cm; weight, 39.4 kg; blood pressure, 124/56 mmHg; and pulse rate, 66 beats/min. Her performance status (PS) was 0. The liver was palpable in the epigastric region. A laboratory examination detected anemia (RBC: 336 × 104/μl, Hb: 9.4 g/dl, Ht: 26.5%). The patient’s serum levels of carcinoembryonic antigen (CEA) and carbohydrate antigen 19-9 (CA19-9), tumor markers, were elevated (63 ng/ml and 456 U/ml, respectively). Colonoscopy demonstrated a type 2 tumor in the ascending colon. An abdominal computed tomography scan showed a hepatic metastasis measuring 45 mm in segments 2/3 of the liver (Fig. 1), thickening of the ascending colonic wall and swelling of the regional lymph nodes. An ultrasound examination also detected a hepatic metastasis measuring 17 mm in segment 6 of the liver.
Fig. 1.
An abdominal computed tomography scan showed a hepatic metastasis measuring 45 mm in the left hepatic lobe (segments 2/3).
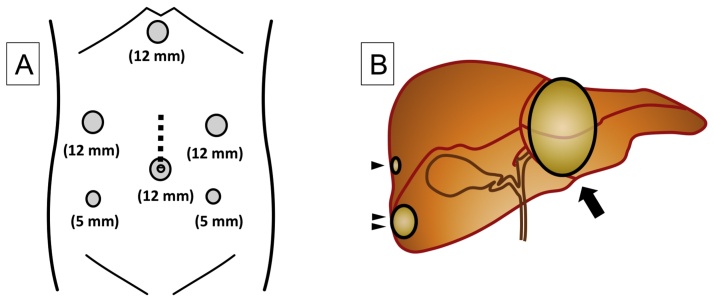
With the patient in the dorsosacral position, pneumoperitoneum was established at 10 mmHg. Trocars were inserted at the locations shown in Fig. 2A. There was no evidence of ascites or peritoneal dissemination. Laparoscopic ileocecal resection combined with D3 radical lymph node dissection was performed before the liver was resected. Laparoscopic ultrasonography revealed the presence of a hepatic metastasis measuring 5 mm in segment 7 of the liver. Laparoscopic left lateral segmentectomy was carried out for the hepatic metastasis in the left lobe of the liver, and partial resection of the liver was conducted for the hepatic metastasis in segment 6 of the liver (Fig. 2B). The remaining hepatic metastasis in segment 7 of the liver was treated with hand-assisted radiofrequency ablation (RFA) because the tumor was tiny, and it was difficult to approach it (Fig. 2B). The total operative time was 470 min, and 340 g of intraoperative blood loss occurred.
Fig. 2.
(A) The surgical trocar sites. The dotted line indicates the incision line used for the hand-assisted laparoscopic procedure, which was 7-cm long. (B) Liver schema. Arrowhead, a tumor measuring 5 mm was found in the right hepatic lobe (segment 7); Double arrowhead, another tumor was detected in the right hepatic lobe (segment 6); Arrow, a third metastatic tumor was observed in the left hepatic lobe (segments 2/3).
The patient’s disease was classified as stage IV (pT4apN2apM1a) according to the TNM classification.
Her postoperative course was uneventful, and the postoperative hospital stay was 23 days.
3. Presentation of case 2
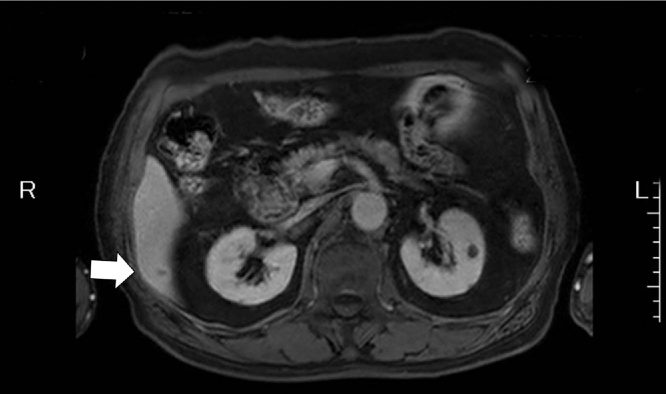
A 78-year-old male was diagnosed with hypertension, hyperlipidemia, and bronchial asthma at a local hospital. He saw a doctor regularly and was treated with oral drugs. He was subsequently diagnosed with anemia. A physical examination demonstrated the following characteristics: height, 166 cm; weight, 72.8 kg; blood pressure, 115/79 mmHg; and pulse rate, 65 beats/min. His PS was 0. No lymph nodes or tumors were palpable, nor was the liver. A laboratory examination detected anemia (RBC: 384 × 104/μl, Hb: 11.6 g/dl, Ht: 35.1%). The patient’s serum CEA and CA19-9 levels were normal. A colonoscopy demonstrated a type 2 tumor in the ascending colon. An abdominal computed tomography scan showed thickening of the ascending colonic wall. Abdominal magnetic resonance imaging (MRI) detected a hepatic metastasis measuring 10 mm in segment 6 of the liver (Fig. 3).
Fig. 3.
Abdominal MRI detected a hepatic metastasis measuring 10 mm in the right lobe of the liver (segment 6) (arrow).
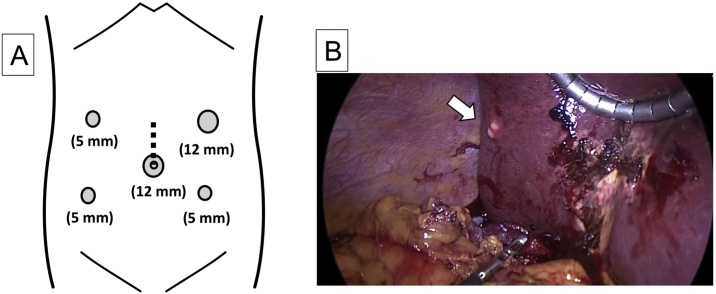
With the patient in the dorsosacral position, pneumoperitoneum was established at 10 mmHg. Trocars were inserted at the locations shown in Fig. 4A. There was no evidence of ascites or peritoneal dissemination. Laparoscopic right colectomy combined with D3 radical lymph node dissection was performed. Then, laparoscopic partial resection of the liver was conducted for the hepatic metastasis in segment 6 of the liver (Fig. 4B). The total operative time was 471 min, and 240 g of intraoperative blood loss occurred.
Fig. 4.
(A) The surgical trocar sites. Dotted line, an incision measuring 4.5 cm. (B) A tumor in the right hepatic lobe (segment 6) measuring 10 mm (arrow).
The patient’s disease was classified as stage IV (pT3pN0pM1a) according to the TNM classification.
His postoperative course was uneventful, and the postoperative hospital stay was 17 days.
4. Discussion
The simultaneous resection of CRC and SLM is considered to be associated with several risks: (i) intraoperative bacterial contamination of the surface of the resected liver with bacteria from the resected colorectum and (ii) postoperative impairment of the liver might influence the risk of postoperative anastomotic leakage [13]. However, it was reported that the simultaneous resection of CRC and SLM is desirable, except in patients (1) in which it is necessary to resect multiple hepatic sections, (2) that are aged ≥70 years, or (3) have undifferentiated adenocarcinoma. In addition, it was suggested that the main benefits of this procedure are that it results in a shorter hospital stay and is less expensive than open surgery [13].
In 2006, two cases in which CRC and SLM were treated with simultaneous laparoscopic resection were reported [14], [15]. In 2011, Huh et al. demonstrated that the simultaneous resection of CRC and SLM produces similar outcomes to the open approach and results in less intraoperative blood loss and earlier postoperative bowel movement [16]. Furthermore, in 2015 it was reported that at experienced centers the simultaneous laparoscopic resection of CRC and SLM is technically feasible, safe, and results in good oncological outcomes [12]. This particular study involved 142 retrospectively enrolled CRC patients with SLM with a median age of 66 years (range: 32–85) [12]. Hence, the feasibility of performing simultaneous laparoscopic procedures for CRC and SLM in elderly patients has not been studied sufficiently.
Gastroenterological surgeons are performing surgery in elderly patients with increasing frequency. A decade ago, it was reported considered that age itself is a risk factor for postoperative complications [17]. However, in 2006 it was demonstrated that laparoscopic resection for CRC is feasible and effective in elderly patients [18]. In a multicenter case-control study of laparoscopic surgery for CRC in patients aged ≥80 years with PS scores of ≥2, it was found that laparoscopic surgery is safe and produces similar survival outcomes to open surgery [19].
In the present two cases, the patients were aged 83 and 78 years, respectively, but they both exhibited a PS score of 0. Furthermore, both patients had coexisting disorders, including bronchial asthma, hypertension, and hyperlipidemia; however, their comorbidities were treated appropriately. Patient 1 had multiple liver metastases from ascending colon cancer. The largest metastatic tumor measuring 45 mm was located in the left hepatic lobe (segments 2/3). Another metastatic tumor measuring 17 mm was located in segment 6 of the liver. The consensus guidelines outlined in the 2008 Louisville Statement on laparoscopic liver surgery state that laparoscopic liver resection is indicated for patients with (1) solitary lesions, (2) tumors measuring ≤5 cm in diameter, and (3) tumors located in the periphery of the liver (segments 2–6) [20]. In case 1, although the patient had multiple liver tumors, preoperatively we considered that these tumors could be safely resected via laparoscopic resection because the biggest tumor was located in segments 2/3, and the tumor in segment 6 was small. A hepatic metastasis measuring 5 mm was subsequently detected in the right hepatic lobe (segment 7) using laparoscopic ultrasonography. In this case, laparoscopic left lateral segmentectomy for the hepatic metastasis in the left lobe of the liver, partial resection of the liver for the hepatic metastasis in segment 6 of the liver, and RFA for the hepatic metastasis in segment 7 of the liver were performed safely. On the other hand, laparoscopic ileocecal resection combined with D3 radical lymph node dissection was carried out uneventfully and safely due to the absence of obesity. In the other case (patient 2), the hepatic tumor was located in segment 6 and was small (10 mm), and the colon cancer was located in the ascending colon. The total operative time was 471 min due to the presence of large amounts of intra-abdominal fat. However, partial resection of the liver was performed uneventfully and safely for the hepatic metastasis. Neither of the patients suffered postoperative complications.
5. Conclusions
Our results indicate that the simultaneous laparoscopic resection of CRC and SLM is feasible and safe in elderly patients. However, further studies involving large numbers of elderly patients who undergo simultaneous laparoscopic resection of CRC and SLM are needed to establish guidelines for such surgical procedures.
Conflicts of interest
We have no conflict of interest.
Funding
We have no source of funding to declare.
Ethical approval
This case report is not research study, therefore approval was not given.
Consent
Written informed consent was obtained from the patient.
Author contribution
Both procedures were performed by Tomoaki Ito, Tomoyuki Kushida, Mutsumi Sakurada, Konomi Mizuguchi and Koichi Sato. Tomoaki Ito collected data and wrote the manuscript. Hiroshi Maekawa and Hajime Orita revised the manuscript.
Guarantor
Koichi Sato and Hiroshi Maekawa.
References
- 1.J. Ferlay, I. Soerjomataram, M. Ervik, et al., GLOBOCAN 2012 v1.0, Cancer incidence and mortality worldwide. IARC CancerBase No 11 [Internet] Lyon: International Agency for Research on Cancer, 2013. Available from: http://globocan.iarc.fr/.
- 2.Steele G., Jr., Ravikumar T.S. Resection of hepatic metastases from colorectal cancer. Biologic perspective. Ann. Surg. 1989;210(2):127–138. doi: 10.1097/00000658-198908000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Scheele J., Stangl R., Altendorf-Hofmann A. Hepatic metastases from colorectal carcinoma: impact of surgical resection on the natural history. Br. J. Surg. 1990;77(11):1241–1246. doi: 10.1002/bjs.1800771115. [DOI] [PubMed] [Google Scholar]
- 4.Leporrier J., Maurel J., Chiche L., Bara S., Segol P., Launoy G. A population-based study of the incidence, management and prognosis of hepatic metastases from colorectal cancer. Br. J. Surg. 2006;93(4):465–474. doi: 10.1002/bjs.5278. [DOI] [PubMed] [Google Scholar]
- 5.Andres A., Mentha G., Adam R., Gerstel E., Skipenko O.G., Barroso E. Surgical management of patients with colorectal cancer and simultaneous liver and lung metastases. Br. J. Surg. 2015;102(6):691–699. doi: 10.1002/bjs.9783. [DOI] [PubMed] [Google Scholar]
- 6.A. comparison of laparoscopically assisted and open colectomy for colon cancer. N. Engl. J. Med. 2004;350(20):2050–2059. doi: 10.1056/NEJMoa032651. [DOI] [PubMed] [Google Scholar]
- 7.Weeks J.C., Nelson H., Gelber S., Sargent D., Schroeder G. Short-term quality-of-life outcomes following laparoscopic-assisted colectomy vs open colectomy for colon cancer: a randomized trial. JAMA. 2002;287(3):321–328. doi: 10.1001/jama.287.3.321. [DOI] [PubMed] [Google Scholar]
- 8.Lacy A.M., Garcia-Valdecasas J.C., Delgado S., Castells A., Taura P., Pique J.M. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet. 2002;359(9325):2224–2229. doi: 10.1016/S0140-6736(02)09290-5. [DOI] [PubMed] [Google Scholar]
- 9.Lacy A.M., Delgado S., Castells A., Prins H.A., Arroyo V., Ibarzabal A. The long-term results of a randomized clinical trial of laparoscopy-assisted versus open surgery for colon cancer. Ann. Surg. 2008;248(1):1–7. doi: 10.1097/SLA.0b013e31816a9d65. [DOI] [PubMed] [Google Scholar]
- 10.Nguyen K.T., Gamblin T.C., Geller D.A. World review of laparoscopic liver resection-2,804 patients. Ann. Surg. 2009;250(5):831–841. doi: 10.1097/SLA.0b013e3181b0c4df. [DOI] [PubMed] [Google Scholar]
- 11.Belli G., Gayet B., Han H.S., Wakabayashi G., Kim K.H., Cannon R. Laparoscopic left hemihepatectomy a consideration for acceptance as standard of care. Surg. Endosc. 2013;27(8):2721–2726. doi: 10.1007/s00464-013-2840-8. [DOI] [PubMed] [Google Scholar]
- 12.Ferretti S., Tranchart H., Buell J.F., Eretta C., Patriti A., Spampinato M.G. Laparoscopic simultaneous resection of colorectal primary tumor and liver metastases: results of a multicenter international study. World J. Surg. 2015;39(8):2052–2060. doi: 10.1007/s00268-015-3034-4. [DOI] [PubMed] [Google Scholar]
- 13.Tanaka K., Shimada H., Matsuo K., Nagano Y., Endo I., Sekido H. Outcome after simultaneous colorectal and hepatic resection for colorectal cancer with synchronous metastases. Surgery. 2004;136(3):650–659. doi: 10.1016/j.surg.2004.02.012. [DOI] [PubMed] [Google Scholar]
- 14.Leung K.L., Lee J.F., Yiu R.Y., Ng S.S., Li J.C. Simultaneous laparoscopic resection of rectal cancer and liver metastasis. J. Laparoendosc. Adv. Surg. Tech. A. 2006;16(5):486–488. doi: 10.1089/lap.2006.16.486. [DOI] [PubMed] [Google Scholar]
- 15.Geiger T.M., Tebb Z.D., Sato E., Miedema B.W., Awad Z.T. Laparoscopic resection of colon cancer and synchronous liver metastasis. J. Laparoendosc. Adv. Surg. Tech. A. 2006;16(1):51–53. doi: 10.1089/lap.2006.16.51. [DOI] [PubMed] [Google Scholar]
- 16.Huh J.W., Koh Y.S., Kim H.R., Cho C.K., Kim Y.J. Comparison of laparoscopic and open colorectal resections for patients undergoing simultaneous R0 resection for liver metastases. Surg. Endosc. 2011;25(1):193–198. doi: 10.1007/s00464-010-1158-z. [DOI] [PubMed] [Google Scholar]
- 17.Lee L., Jannapureddy M., Albo D., Awad S.S., Farrow B., Bellows C.C. Outcomes of veterans affairs patients older than age 80 after surgical procedures for colon malignancies. Am. J. Surg. 2007;194(5):646–651. doi: 10.1016/j.amjsurg.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 18.Kannan U., Reddy V.S., Mukerji A.N., Parithivel V.S., Shah A.K., Gilchrist B.F. Laparoscopic vs open partial colectomy in elderly patients: insights from the American College of Surgeons – National Surgical Quality Improvement Program database. World J. Gastroenterol. 2015;21(45):12843–12850. doi: 10.3748/wjg.v21.i45.12843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Niitsu H., Hinoi T., Kawaguchi Y., Ohdan H., Hasegawa H., Suzuka I. Laparoscopic surgery for colorectal cancer is safe and has survival outcomes similar to those of open surgery in elderly patients with a poor performance status: subanalysis of a large multicenter case-control study in Japan. J. Gastroenterol. 2016;51(1):43–54. doi: 10.1007/s00535-015-1083-y. [DOI] [PubMed] [Google Scholar]
- 20.Buell J.F., Cherqui D., Geller D.A., O’Rourke N., Iannitti D., Dagher I. The international position on laparoscopic liver surgery: the Louisville Statement, 2008. Ann. Surg. 2009;250(5):825–830. doi: 10.1097/sla.0b013e3181b3b2d8. [DOI] [PubMed] [Google Scholar]