Abstract
This study explored the steps of food preparation, related handwashing opportunities, current practices, and community perceptions regarding foods at high-risk of contamination such as mashed foods and salads. In three rural Bangladeshi villages, we collected qualitative and observational data. Food preparation was a complex and multistep process. Food preparation was interrupted by tasks that could contaminate the preparers' hands, after which they continued food preparation without washing hands. Community members typically ate hand-mixed, uncooked mashed food and salad as accompaniments to curry and rice at meals. Hand-mixed dried foods were mostly consumed as a snack. Observers recorded handwashing during preparation of these foods. Among 24 observed caregivers, of 85 opportunities to wash hands with soap during food preparation, washing hands with soap occurred twice, both times after cutting fish, whereas washing hands with water alone was common. A simple and feasible approach is promotion of handwashing with soap upon entering and re-entering the food preparation area, and ensuring that everything needed for handwashing should be within easy reach.
Introduction
Diarrheal disease among children under 5 years of age causes considerable morbidity and contributes to child mortality in Bangladesh.1,2 Many diarrheal episodes can be attributed to contaminated food in low- and high-income countries.3–6
Hands that are not washed after fecal contact can act as a source of diarrhea pathogens, and foods can be contaminated through contact with unwashed hands.6–11 Raw vegetables are commonly contaminated with pathogens.12,13 Cross-contamination, the transfer of pathogens from a contaminated food via hands (or other vehicles such as utensils) to uncontaminated food is a further pathway for pathogen transmission. When contaminated foods are not consumed immediately or are stored without refrigeration, pathogenic bacteria can multiply exponentially.14,15
In rural Bangladesh, children living in households in which caregivers were observed to wash at least one hand with soap during food preparation had significantly fewer days of diarrhea (3.7%) than children whose caregivers were observed not washing hands at all during food preparation (12.5%), suggesting the importance of handwashing at this event.16 But handwashing during food preparation is rare in rural Bangladesh. One study identified that only 1% of food preparers in the home were observed washing their hands with soap during food preparation.16 Similarly, in northeast Brazil, most mothers had poor hand hygiene behaviors during food preparation, with the potential to introduce pathogens to the foods.17
Complexity of instructions, especially for behaviors consisting of multiple steps like food preparation–related handwashing, can hamper adherence to the recommended behaviors.18–21 To formulate appropriate behavioral recommendations that are both feasible and acceptable under local conditions, we must build upon a good understanding of all the steps in following these recommendations. A study conducted in India showed that interventions that were based on understanding local context and drivers of handwashing behavior significantly increased handwashing with soap at key event times (1% in baseline to 37% in 6-month follow-up visit) including during food preparation.22 One study that we could identified, conducted in Mali, described the process of preparation for two food items and related hygiene practices.23 However, generally, there are limited data on food preparation steps and related handwashing practices that can inform behavior change interventions and pinpoint when hands should be washed during food preparation, especially from low-income contexts where easy access to running water is uncommon.24
We examined community practices, related perceptions, and constraints to washing hands with soap during food preparation to aid development of an acceptable and feasible food preparation component to integrate into hand hygiene interventions. We focused on foods that carry increased risk for pathogen transfer, particularly those prepared with bare hands and were not further cooked.
Materials and Methods
Definitions.
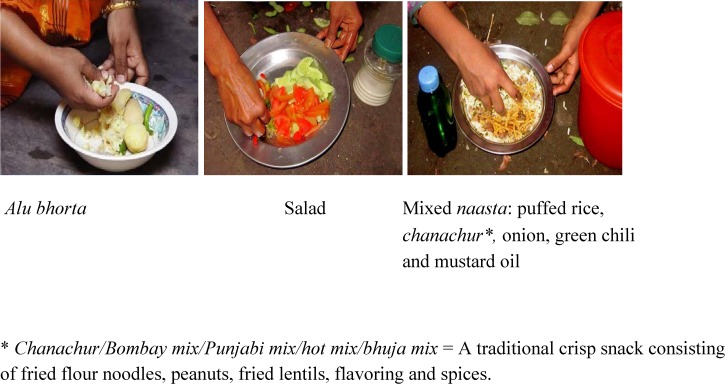
We developed a definition of high-risk foods before conducting field work. High-risk foods included mashed and mixed foods, which were likely to have the greatest risk for pathogen transmission, since their preparation involved manipulation with bare hands, after which the foods were not further cooked. In assessing level of risk, we also considered the moisture content of foods, which was assessed based on our familiarity with the way of preparation rather than measuring quantitatively, as moisture provides a favorable environment for rapid pathogen growth.5,25 We looked at three types of foods: bhortas, salads, and naasta. “Bhortas” are dishes made from hand-mashed vegetables, fish, or fruit. Salads typically consist of dishes made from hand-mixed raw vegetables with other ingredients like onion and chili. Under the salad category, we looked at “paan” (betel quid), a recreational substance for chewing, prepared with betel leaf combined with areca nut and/or cured tobacco using hands.26 “Naasta” are preparations made from dry snacks hand-mixed with other ingredients like onion and chili (Figure 1 ).
Figure 1.
Types of food prepared with bare hands and not further cooked: (A) alu bhorta, (B) salad, and (C) mixed naasta: puffed rice, chanachur, onion, green chili, and mustard oil.
We specified handwashing opportunities before high-risk food contact: 1) when foods came into direct contact with hands and were not further cooked, for example, mashing foods, mixing salad, mixing dried foods and 2) when cutting or peeling raw vegetables, fish, or meat immediately before preparing high-risk foods. We defined hand rinsing with water as washing hand(s) using only water with minimal rubbing. We defined hand contact with water when hand(s) were dipped into a bowl of water or water was simply poured over the hand(s) without any rubbing.
Study sites and population.
This formative research study was conducted in three rural villages of Kishorganj District, in central Bangladesh. We selected the sites to represent a typical rural area of Bangladesh in terms of water points and latrine facilities (i.e., shared tube wells with hand pump and shared latrines, both situated outside of the household) in which no handwashing intervention had been implemented. Most study participants were caregivers of children less than 3 years of age who prepared food for the child as well as for the household. We also included heads of households, the elder person of the family, for example, father, grandfather, or grandmother of the child, as in the Bangladeshi context elders are important family decision makers. Household heads decide how to manage household issues, including funding and arranging water, sanitation and hygiene facilities, for example, buying soap.
Data collection methods.
From November 2011 to January 2012, the data collection team sequentially used semi-structured observations, video observations, in-depth interviews, and focus group discussions.
Semi-structured observations and video observations recorded food preparation activities, which focused on the steps of preparing each category of high-risk food and the related handwashing opportunities and practices. In-depth interviews and focus groups explored the various types of each category of food that community members prepared and consumed, the foods given to children, the perceptions regarding hand hygiene around food preparation, and the barriers to washing hands with soap at these events. In addition, focus groups identified the broader community norms on food preparation–related handwashing. In exploring such factors with the study participants, we were guided by the Integrated Behavioral Model for Water, Sanitation and Hygiene (IBM-WASH),27 a theoretical framework that integrates the multilevel factors influencing water, sanitation, and hygiene behavior, in three dimensions: contextual, psychosocial, and technological.
A sociologist (Fosiul A. Nizame) led the data collection. Four experienced anthropologists conducted the semi-structured observations, in-depth interviews, and focus group discussions, while women from the study communities who had completed at least their secondary school certificate examination conducted video recordings of household activities. Experienced anthropologists trained the women to use the video camera and explained the activities to record during video sessions. Each woman made a short trial film to ensure that she had acquired the skills.
Sampling and data collection.
The data collection team selected study participants purposively. Only one caregiver was included from a compound, a group of houses surrounding a yard with occupants who share a familial relationship and typically share access to water and latrines. During enrollment, the data collection team included approximately the same number of child caregivers from each child age category: 0–12, 12–24, and 24–36 months, as there were likely different feeding practices and food types for each. The data collection team conducted 12 semi-structured observations, 12 video observations, and 12 in-depth interviews; six in-depth interviewees had also participated in the semi-structured or the video observations, while 24 enrollees participated in only one data collection activity. Anthropologists found data saturation after analyzing 12 in-depth interviews and did not proceed further to enroll in-depth informants.
For video observations, with the help of village residents, the field team identified the main entry point of each of three villages, as a starting point to include eligible caregivers, and selected four households per village, each household coming from four different adjacent compounds, for a total of 12 video observations. For semi-structured observations, the field team started the enrollment of eligible caregivers from the end point of each of the three villages, as identified by villagers. Four semi-structured observations per village were conducted in households coming from each of four different adjacent compounds for a total of 12 semi-structured observations. Although the objectives for video and semi-structured observations were the same, the video provided the study team with a visual record, which could be reviewed after leaving study sites, to aid data analysis. Each household was visited to take informed consent, to enroll the participants, collect basic demographic and socioeconomic information, and for an informal discussion on daily household activities to fix a feasible time and day for data collection activities. During this visit, anthropologists asked caregivers when they would next prepare and consume mashed and mixed foods, and the data collection team scheduled the observation to take place at that time. The team conducted semi-structured observations during two different periods in each household: from 7:30 am to 11:30 am and 6:00 pm to 8:00 pm, whereas video observation was conducted only during the morning period as there was insufficient lighting in the evening in study sites with no electricity.
The data collection team enrolled in-depth interview participants commencing from the compound immediately adjacent to the one included in the most recent video observation and proceeding with the next adjacent compound. Two caregivers who had not been previously observed or video recorded were enrolled from each of the three villages. Data collectors conducted six in-depth interviews with caregivers in this way. For the remaining six in-depth interviews, the data collection team included three caregivers who had participated in the semi-structured observations and three from the video observations; the team purposively selected one observed and one video-recorded caregiver from each village.
In each of the three different villages, anthropologists conducted one focus group discussion with household heads, three in total, selecting heads of households that had not been part of any other data collection activity. The team aimed to achieve a mix of household heads, representative of all three child age categories in each focus group discussion.
Data analysis.
Although our observations recorded the preparation steps of all foods prepared during the data collection period, the semi-structured and video observation data were analyzed by examining the preparation steps of bhorta, salad, and mixed dried naasta only. In the analysis, anthropologists counted handwashing opportunities, when soap was used to wash hand(s), when hand(s) were rinsed with water only, or when hand(s) came into contact with water.
Investigators determined the level of risk for each high-risk food type observed, based on the number of hand contact opportunities, food preparation interruptions and cross-contamination opportunities that occurred, estimated level of food moisture, and time between preparation and consumption.
Audio recordings of in-depth interviews and focus group discussions were transcribed verbatim in Bengali. On the basis of the thematic content, anthropologists coded the transcripts using Atlas.ti software (version 5.2; Scientific Software Development GmbH, Berlin, Germany), prepared a summary of codes for each interview and focus group discussion, and identified suitable quotes. Summary codes were translated into English, and individual summaries were compiled into a master summary report, followed by thematic analysis. As with data collection, we were guided by IBM-WASH to design codes, conduct thematic analysis, and organize emerging themes according to levels and dimensions in the framework. Where applicable, we analyzed the results according to the contextual, psychosocial, and technological dimensions, at the habitual, individual, household, and community levels, related to behavior in infrastructure-restricted settings.
Ethical considerations.
Data collectors explained clearly to the participants why and what types of data we were interested to collect by stating “as we are working on health issue, we will collect domestic hygiene–related data including the process of food preparation.” Before taking part in the study, all participants provided written informed consent. The study received the International Centre for Diarrhoeal Disease Research, Bangladesh Ethical Review Committee clearance.
Results
Sociodemographic characteristics.
Of the 30 caregivers enrolled across the three villages for observations and in-depth interviews, all were female. Among them more than half (17) were between 18 and 25 years of age, almost half (14) had no formal education, and almost all (28) considered themselves homemakers (Table 1). A total of 29 heads of households participated in the focus group discussions, all were males, and most were farmers (Table 1). Despite purposively enrolling participants from households with children from three different age categories, we found similar responses among all age categories, and therefore present the combined data.
Table 1.
Demographic characteristics of participants
| Characteristics | Caregivers (N = 30) | Household heads (N = 29) |
|---|---|---|
| n (%) | n (%) | |
| Age | ||
| 18–28 years | 19 (63) | 6 (21) |
| 28–38 years | 7 (23) | 12 (41) |
| > 38 years | 4 (14) | 11 (38) |
| Education | ||
| No formal education | 14 (47) | 11 (38) |
| Primary | 10 (33) | 11 (38) |
| Secondary | 4 (13) | 6 (21) |
| Above secondary | 2 (7) | 1 (3) |
| Occupation | ||
| Homemaker | 28 (93) | 0 (0) |
| Farmer | 0 (0) | 18 (62) |
| Business | 0 (0) | 3 (10) |
| Teacher/tutor | 2 (7) | 0 (0) |
| Fisherman | 0 (0) | 2 (7) |
| Driver | 0 (0) | 2 (7) |
| Skilled worker | 0 (0) | 2 (7) |
| Village doctor | 0 (0) | 1 (3) |
| Shopkeeper | 0 (0) | 1 (3) |
Preparation, level of risk, and consumption patterns: bhorta, salad, and mixed dried naasta.
We were able to observe preparation for seven types of high-risk foods: four bhortas, two salads, and one type of mixed dried snack, totaling 43 observed preparation events, all of which were prepared with bare hands and not further cooked. But during interviews, caregivers reported frequent preparation of an additional 24 similar types of foods, bringing the total number of types of high-risk foods to 31. Of the 31 foods, caregivers reported 15 that were consumed by children, and we were able to observe the preparation of 5/15 (Table 2). Community members reported typically eating mashed food and salad as accompaniments to curry and rice at meals; they ate mixed dried naasta as a snack between meals or if guests visited. Study participants always used bare hands when preparing these foods. None wore gloves or used utensils to prepare these foods.
Table 2.
Preparation and consumption of hand-prepared foods: reported and observed
| Types of food local name (English name) | High-risk foods reported by participants | No. of events of food prepared (observed) | Consumed by children (reported) | |
|---|---|---|---|---|
| English name | Bengali/local name | |||
| Bhortas | ||||
| Shobji bhortas (mashed vegetables) | Mashed potatoes | Alu/gula bhorta | 9 | Yes |
| Mashed eggplant | Begun bhorta | 5 | Yes | |
| Mashed bean | Sheem/uri bhorta | 3 | Yes | |
| Mashed tomato | Tomato bhorta | 0 | Yes | |
| Mashed mustard seeds | Shorisha bhorta | 0 | No | |
| Mashed gourd leaf | Lau pata bhorta | 0 | Yes | |
| Mashed jute leaves* | Paat/nailly shak bhorta | 0 | No | |
| Maacher bhortas (mashed fish) | Mashed spotted snake head fish | Taki/ladi maach bhorta | 0 | No |
| Mashed prawns | Chingri/iccha maach bhorta | 0 | No | |
| Mashed yellow tail cat fish | Pangas maach bhorta | 0 | No | |
| Mashed dried fish | Shutki/shidol/chepa bhorta | 10 | No | |
| Fholer bortas (mashed fruit)* | Mashed baby jack fruit | Kathal er muji bhorta | 0 | Yes |
| Mashed Indian jujube | Boroi bhorta | 0 | No | |
| Mashed olive | Jolpai bhorta | 0 | No | |
| Mashed unripened (green) mango | Kacha aam bhorta | 0 | No | |
| Mashed green banana | Kancha kola bhorta | 0 | No | |
| Mashed shaddock/pomelo | Jambura bhorta | 0 | No | |
| Mashed blackberry | Jaam bhorta | 0 | No | |
| Mashed star fruit | Kamranga bhorta | 0 | No | |
| Mashed guava | Peyara bhorta | 0 | No | |
| Mashed tamarind | Tetul bhorta | 0 | No | |
| Mashed pineapple | Anaros bhorta | 0 | Yes | |
| Salads | ||||
| Salads | Radish salad | Mula er salad | 3 | Yes |
| Carrot salad | Gajor er salad | 0 | Yes | |
| Cucumber/tomato salad† | Shosha/tomato er salad | 0 | Yes | |
| Paan | Betel quid‡ | Paan | 11 | No |
| Mixed dried naastas (snacks)* | ||||
| Mixed puffed rice | Muri/khoi makha | 2 | Yes | |
| Mixed puffed rice with snack like chanachur | Muri-chanachur makha | 0 | Yes | |
| Sweetened flattened rice mixed with shredded coconut | Chira makha | 0 | Yes | |
| Mixed roasted rice | Chaal vaja makha | 0 | Yes | |
| Mixed rice flour§ | Chaaler gura makha | 0 | Yes | |
| Total 31 | Total 43 | Total yes 15 | ||
Consumed as a snack.
Vegetables served as salads either mixed together or served separately.
Referred to as “paan.” This is stimulating, psychoactive preparation of betel leaf combined with areca nut and/or cured tobacco (source: Wikipedia).
A locally made dried snack that includes rice flour, shredded coconut, and jiggery or sugar.
We have organized food preparation data by level of risk from highest to lowest (Table 3). In deciding whether a certain dish represents a higher or lower risk, we considered the following events.
Table 3.
Analysis of the level of risk from higher to lower for high-risk food preparation and consumption (total number of preparations observed: N = 43)
| Type of foods | Item/main ingredients | Preparation process (sequentially followed according to the arrows) | No. of hand contact opportunities* (per preparation) | Observed handwashing opportunities | Level of moisture | Time between preparation and consumption (minutes) |
|---|---|---|---|---|---|---|
| Bhortas | Potato or bean or tomato or gourd leaf or mustard seeds or green banana | Boil → peel using both hands, when necessary → chop onions and green chilies → mix chopped onions, green chilies, mustard oil, and salt → mash all together with bare hand | 3–5 | Interruptions occurred within a preparation:0–2 times | Wet to very wet | 30–60 |
| No. of preparations observed: 12 | ||||||
| Eggplant | Scorch → peel using both hands → fry green chilies/onions with soya bean/mustard oil → mix these ingredients with salt | Cross-contamination opportunities observed within a single preparation: 1–3 times | ||||
| No. of preparations observed: 5 | ||||||
| Fish/dry fish | Fry/boil the fish → blend on slab-stone with raw green chilies, onions, garlic using both hands → mix with salt | |||||
| No. of preparations observed: 10 | ||||||
| Fruit (mango/berry/black berry/baby jack fruit/olive/tamarind/star fruit/guava/green banana, grapefruit) | Peel → chop → chop onion, green chili → add salt and sometimes mustard oil/ginger/coriander powder/coriander leaves → mixed and mash all together with bare hand | |||||
| No. of preparations observed: 0 | ||||||
| Salads | Vegetables (cucumber, tomato, radish, carrots) | Wash cucumber/tomato/ radish/carrot → peel/cut → chop green chili, onion → add salt/coriander leaves/mustard oil → mix all together with bare hands | 1–3 | Interruptions occurred within a preparation: 0 time | Wet | 30–60 |
| No. of preparations observed: 3 | Cross-contamination opportunities observed within a single preparation: 1–3 times | |||||
| Paan | Betel quid | Take a betel leaf → wash it with water → apply lime on the leaf → put areca nuts → wrap the leaf to serve | 1–3 | Interruptions occurred within a preparation: 0–2 times | Dry/damp | < 10 |
| No. of preparations observed: 11 | Cross-contamination opportunities observed within a single preparation: 0 times | |||||
| Mixed dried naastas | Puffed rice or different forms of rice or dried snacks | Mix puffed rice or dried snack → chop onion, green chili → add salt, mustard oil → mix all together with bare hands | 1–3 | Interruptions occurred within a preparation: 0–2 times | Dry/damp | < 10 |
| No. of preparations observed: 2 | Cross-contamination opportunities observed within a single preparation: 1 time |
Data from video and semi-structured observations.
Bhortas were prepared from boiled or raw vegetables, fruit, and/or fish in a process with multiple steps and frequent direct manipulation with hands (27 observed events; Table 3). No further cooking occurred after hand manipulation. In the risk analysis, we observed three to five events when the preparer used only hands to mix different ingredients to prepare a bhorta, that is, peel/cut/blend/boiled vegetable/fish, chopped onions/green chilies, mash and mixed all together with bare hands. Within a single preparation, we found one to three cross-contamination opportunities between cutting/peeling several raw ingredients (e.g., onion, green chili) and blending or mixing those ingredients with mashed vegetables/fish (e.g., boiled potato) and there was no further cooking. Moreover, most bhortas have high moisture content (Table 3).
Bhortas were prepared for all family members. Sometimes caregivers provided mashed foods as side dishes in meals for their children. Most commonly children eat bhortas made from mashed potatoes, beans, or eggplant but not those that are prepared with large quantities of chilies (Table 2).
Salads were prepared with different vegetables (e.g., tomato, cucumber, carrot, and radish) and mixed with other ingredients such as green chili, onion, mustard oil, and salt (14 observed events). Salad preparation also involved a multistep process, though direct hand mixing was less frequent than for bhortas (one to three hand contact events; Table 3). In the risk analysis, similar to bhorta, salad preparation included hand contact events, cross-contamination opportunities, and moderate to high levels of moisture (Table 3). Respondents reported that sometimes they provide pieces of salad vegetables to their child before mixing the vegetables with other ingredients, especially spices (Table 2; final column).
Mixed dried naasta (Table 2) preparation and consumption also involved direct hand contact (two observed events; Table 3). In the risk analysis, mixed dried naasta preparation had a low contamination risk compared with mashed food and salad. Low moisture content and shorter (10 minutes) storage time between preparation and consumption makes naasta less likely to support microbial multiplication (Table 3). According to most of the respondents, children eat mixed dried naastas, especially those prepared with little or no spice (Table 2).
Existing handwashing habits.
The current practice of handwashing during food preparation was influenced by psychosocial factors at the habitual level of the IBM-WASH framework, such as bad smell or visible dirt, or lack thereof. During observations of the 24 caregivers, of 85 opportunities to wash hands with soap during food preparation, participants washed hands with soap on two opportunities, rinsed with water alone on 11 opportunities, hands came into contact with water in a bowl on 34 opportunities, and they did not wash hands on 38 opportunities (Table 4). Both of the opportunities on which food preparers washed hands with soap occurred after cutting fish. In all events related to bhorta and salad preparations, cross-contamination risk occurred, for example, preparers peeled or cut boiled or non-boiled vegetables/fish/fruit, chopped other ingredients like chilies/onions, and then mashed or blended (for mashed foods) vegetables/fish/fruit and finally mixed all together. Food preparation was sometimes interrupted by other events or tasks during which contamination was likely, including their own defecation, cleaning child feces, or adding cow dung fuel sticks or firewood to the stove. After completing these tasks they continued food preparation without washing hands (Table 5).
Table 4.
Observed handwashing practices
| Types of handwashing opportunities | No. of opportunities by observation method | Caregivers washed/rinsed hands with | Water available at food preparation place | Soap (any form) available at food preparation place | ||||
|---|---|---|---|---|---|---|---|---|
| Soap (any form) | Water | Hands came into contact with water | Not washed | |||||
| After cutting fish | Semi-structured | 3 | 2 | 1 | 0 | 0 | 3 | 0 |
| Video | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Before mashing foods | Semi-structured | 17 | 0 | 2 | 10 | 5 | 17 | 1 |
| Video | 13 | 0 | 5 | 5 | 3 | 12 | 1 | |
| Before cutting vegetables | Semi-structured | 6 | 0 | 0 | 0 | 6 | 4 | 0 |
| Video | 9 | 0 | 0 | 0 | 9 | 5 | 1 | |
| Before preparing salad | Semi-structured | 1 | 0 | 0 | 0 | 1 | 1 | 0 |
| Video | 2 | 0 | 0 | 2 | 0 | 2 | 0 | |
| After cutting vegetables | Semi-structured | 6 | 0 | 2 | 4 | 0 | 6 | 0 |
| Video | 9 | 0 | 0 | 9 | 0 | 9 | 1 | |
| Before mixing dried foods | Semi-structured | 2 | 0 | 0 | 0 | 2 | 2 | 0 |
| Video | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Before preparing betel quid | Semi-structured | 10 | 0 | 0 | 1 | 9 | 1 | 0 |
| Video | 1 | 0 | 0 | 0 | 1 | 1 | 0 | |
| After interruptions | Semi-structured | 1 | 0 | 0 | 0 | 1 | 1 | 0 |
| Video | 5 | 0 | 1 | 3 | 1 | 4 | 0 | |
| Total observed occasions | Total semi-structured | 46 | 2 | 5 | 15 | 24 | 33 | 1 |
| Total video | 39 | 0 | 6 | 19 | 14 | 33 | 3 | |
Table 5.
Interruptions observed* during food preparation
| Type of interruption (a characteristic situation) | Details of actions that food preparer took during interruption | No. of interruption(s) occurred |
|---|---|---|
| Food preparer went to toilet | Food preparer was cutting vegetables for cooking. There was also rice boiling on the burner. From time to time food, preparer added firewood to the burner with same hands used to cut vegetables. After completing some of the vegetable cutting, she went to the toilet. After returning from the toilet, she washed her left hands with water only and then she started preparing spice ingredients as well as cutting another type of vegetable by using both hands | Occurred 1 time |
| Cleaned child feces/anus | Food preparer was cutting vegetables. In the meantime, her baby defecated on the floor in the household. She cleaned feces with pieces of cloth by using her left hand and then threw them in an open place beside a latrine situated outside the household. She cleaned her child's anus in the courtyard with water only by using her left hand and then just poured a small amount of water on her left hand. She went into the household and fed dry food to the baby using her bare right hand. Then she returned back to the cooking area and pushed fire wood into the stove with right hand. She peeled an onion and dipped it into bowl with water along with both of her hands, shook her hands with the water falling into the bowl of water used for washing the onion. She chopped the onion, then mashed it along with boiled beans and green chilies with bare hands | Occurred 1 time |
| Added cow dung fuel stick to the stove | Food preparer was cutting vegetables. When cutting, she added fuel sticks made with cow dung into the stove several times by using both hands, and she continued cutting vegetables without washing hands | Occurred 2 times |
| Performed by two different caregivers | ||
| Added firewood to the stove | After peeling a boiled egg, food preparer put it in a bowl. She added firewood to the burner using her right hand. She dipped her right hand into a bowl of water. She broke a portion of the boiled egg, mashed a little with her bare right hand and fed mashed egg to her child | Occurred 2 times |
| Performed by two different caregivers |
Data from video and semi-structured observations.
Qualitative data were compatible with the observation data. The majority of interviewed informants mentioned that they wash their hands with only water as part of the food preparation process, not as a separate task. They also thought that when they wash utensils, their hands are simultaneously washed in the water. Focus group discussions support this finding. A caregiver said,
Before eating or serving foods, when I washed the plates and bowls with water my hands also got washed.
Half explained that before mixing salads and mashing foods, they washed hands with soap if hands were visibly dirty. Otherwise they washed with water only and not as part of a distinct handwashing event but while washing or rinsing ingredients. A caregiver said,
Before preparing salad, we wash our hands along with ingredients in a water bowl. If hands are covered with dirt, then we wash hands with detergent or soap.
Some caregivers stated that they used soap to wash hands after cutting fish, meat, or chicken to remove the smell. Some caregivers said they washed hands with water alone before cutting vegetables, and some reported this practice after cutting vegetables.
Identified barriers to handwashing with soap.
The reported barriers to wash hands with soap during food preparation corresponded well to the contextual, psychosocial, and technological dimensions of the IBM-WASH framework at community, household, individual, or habitual level.
Video and semi-structured observations confirmed that none of the households were observed to have handwashing stations at the food preparation or any other area of the household, and no household had running water in the food preparation area (contextual dimension at the household level/technological dimension at the community level). Most households had water present in bowls or pots, which the food preparers brought to the food preparation area for washing utensils, washing hands, and cooking and drinking purposes. Few households had soap at their food preparation area (Table 4). A few informants from in-depth interviews and participants from all focus groups mentioned that not having soap and water together at the handwashing place is a barrier to washing hands with soap in general, including during food preparation. One caregiver stated,
I cannot keep the soap near the tube well because children waste it and I have to bring soap from my room to wash hands. I don't feel motivated to bring soap and my household work is also delayed because of this.
Most informants thought that hand contact with water alone during food preparation was adequate, and this was their normal practice. Household heads from all three focus groups stated that community members were not aware of the recommendation of handwashing with soap during food preparation to prevent disease transmission, and that this lack of knowledge was an important barrier to washing hands with soap at this key event (IBM-WASH psychosocial dimension at the individual level).
During focus group discussions with household heads, some participants mentioned soap cost as a barrier to wash hands (contextual dimension at the individual level). A household head cited,
We are so poor that we cannot afford to buy food, so how can we buy soap to wash our hands!
A few informants and participants from two focus groups mentioned that lack of time, combined with the pressure to complete other household chores (contextual dimension at the individual level), was another barrier for caregivers to wash hands with soap. Chores included sweeping rooms and yards, washing dishes and clothes. Another demand on time was child care tasks like helping children to defecate and cleaning them up afterward. In that context, as soap is kept far from the water, handwashing with soap therefore takes extra time, which also acts as a barrier to wash hands with soap during food preparation. A caregiver cited,
It takes time to wash hands with soap. Rubbing hands with soap and then washing with water takes lots of time, but when preparing food, we have a short time to do that. Every family member wants food from mother. To serve food and satisfy all, we have no time to wash hands with soap.
Discussion
Many foods consumed in rural Bangladeshi communities are good vehicles for pathogens, because they are prepared with bare hands and are not further cooked. Communities from other low-income countries also practiced similar food preparation processes with direct hand contact.9,23,28 Unwashed hands, contaminated from contact with other foods (cross-contamination) during cooking or through fecal contact (e.g., defecation, handling cow dung, cleaning the household) that occurred during cooking, can be sources of enteric pathogens. On the basis of frequency of hand contact, cross-contamination opportunities, and level of moisture content, bhorta dishes and salad were assessed to have moderate to high moisture content and, since they are not consumed immediately after preparation, provide a suitable environment for pathogen growth.5,14,25 A study conducted in Bangladesh recorded high rate of pathogen growth in mashed food.29
Study participants' handwashing habits, related perceptions, and other barriers to using soap at the food preparation area could be explained more clearly by using the IBM-WASH framework. The psychosocial dimension at the habitual level was key; almost none of the participants washed hands with soap and few with water during food preparation events. The psychosocial dimension at individual level explained the related perceptions; informants reported that their hands are simultaneously washed in the water during washing of utensils.
Though half of the informants stated the need to wash hands with soap before preparation of some foods, such as salads and bhortas, they only recognized this as important when there was visible dirt on hands, as reported for handwashing in general in previous studies from Bangladesh30,31 and elsewhere.32,33 Both types of observation methods confirmed that community members did not wash hands with soap during food preparation. Studies conducted in Bangladesh have detected that handwashing with water only is the most common practice, and the prevalence of handwashing with soap around food-related events is considerably lower than for post-feces contact.16,34 However, obvious handwashing with water was not commonly detected during food preparation in this study, likely due to common hand contact with water during the food preparation processes.
Participants stating that “lack of time due to household chores” was a reason for not washing hands at key food preparation events may reflect a low priority assigned to handwashing or insufficient motivation or lack of the amenities needed in the food preparation area to make handwashing quicker. Most hand hygiene interventions previously conducted in Bangladesh have focused on handwashing with soap after defecation and before eating but have not mentioned nor facilitated the importance of handwashing during food preparation.35
The Centers for Disease Control and Prevention (CDC) recommend washing hands before, during, and after food preparation.36 As shown here, food preparation involves many steps and processes. If food preparers in Bangladesh wish to comply with this recommendation, they may need to wash hands with soap around 10 times to prepare a typical meal, which may include a meat/fish dish, a vegetable dish, and a bhorta and rice. Preparation of a bhorta dish alone may need handwashing around five times (Table 3), that is, before cutting vegetables, before and after peeling, before cutting ingredients like onion/chili, and before mashing and mixing all ingredients with bare hands. Expecting busy caregivers in rural Bangladesh to wash hands at every CDC-recommended opportunity in the preparation of foods that are not further cooked is unrealistic. Washing hands at every CDC-recommended opportunity, translating to 29 times per hour for restaurant workers and to 11 times per hour for school food preparers was also found unrealistic elsewhere.37 Giving unrealistic recommendations in general, may undermine the credibility of the recommender.38 Studies found that simple rules to change behaviors were associated with better adherence than those that had complex rules.18–20 To provide simple and feasible recommendations, we suggest promoting handwashing with soap upon entering and re-entering the food preparation area to prepare foods, since home kitchens are common sources for domestic foodborne outbreaks.39–42 Moreover, we suggest further research to evaluate whether food preparers in low-resource settings are able to follow this recommendation, and whether an intervention built around this recommendation could reduce diseases risk.
The contextual and technological dimensions of IBM-WASH explained the commonly reported barriers to wash hands with soap. Soap cost was a barrier to washing hands with soap in this study. The absence of soap and water together at a handwashing place conveniently located for food preparation may have been another barrier to handwashing with soap during food preparation, as found previously.43 In rural Bangladesh, the water source is usually located away from food preparation areas.30 Installation of a conveniently located handwashing station could enhance regular practice of handwashing with soap. A handwashing station should be a dedicated device that stores water, preferably with a tap that allows water to flow and a location somewhere to place a handwashing agent such as soap or a bottle of soapy water. A model with these characteristics has been found acceptable in both rural and urban communities in Bangladesh.44 Thus, creating an enabling environment in favor of recommended behaviors may help people to overcome their cited barriers to washing hands with soap. A recent example of creating such an enabling environment was during the Ebola outbreak in west Africa where plastic buckets with taps installed almost everywhere have helped keep school classrooms free from Ebola infection.45,46
We collected data in only one geographical site. However, we included three different villages from this site, which were typical of Bangladeshi rural communities in terms of water points and latrine facilities. Findings on hygiene practices, related perceptions, constraints to washing hands with soap during food preparation, and intervention suggestions were similar among all three villages, and so likely captured the context of high-risk food preparation in rural water-constrained settings in Bangladesh.
The physical presence of an observer can influence hygiene practices.47,48 Moreover, our supposition was that the video observation might create a positive courtesy bias. To minimize reactivity, we hired and trained women from the study site to conduct the video recording. Despite the possibility that participants practiced better than normal handwashing behaviors while under observation, we found that most people did not wash hands at the overwhelming majority of the observed handwashing opportunities.
This investigation did not rely on risk modeling strategies such as Hazard Analysis of Critical Control Points.49 Instead, we adopted an approach that examined specific foods that we considered potentially at high risk for contamination from unwashed hands or from cross-contamination, because of manipulation with bare hands and the fact that they are not further cooked.
It is important to raise the profile of handwashing with soap during food preparation. Messages on handwashing during food preparation that are integrated into a handwashing intervention should avoid promoting impractically high rates of handwashing. Participants cited low awareness of the potential for handwashing during food preparation. Messages should aim to increase this awareness, as creating awareness is a first step toward behavior change.50 Communication messages should clarify that hand contact with water alone during food preparation might not be adequate to remove germs and therefore to reduce diarrhea. On the contrary, hand contact with water that was used to wash vegetables and other ingredients might increase the risk of hand contamination. To initiate and to form handwashing habits related to food preparation, the intervention might consider encouraging people, in the absence of soap, to wash/rub/scrub hands at least with water alone, as opposed to no handwashing at all or just dipping hands in water during food washing. Handwashing with water alone (but not simply water contact) during food preparation was associated with reduced childhood diarrhea.16 Interventions could include a message such as “when preparing food, handwashing with water is good and handwashing with soap is better” as suggested elsewhere.16 Thus, the negotiation of a less ideal behavior may lead to realistic, feasible, and acceptable practice.51,52
An intervention should encourage people to make soap and water available in the food preparation area; behavior change theory stresses the importance of environmental support to adapt a behavior.27,53,54 Participants' concern regarding soap cost could be addressed by demonstrating the simplicity and utility of soapy water, the low cost, US$0.038 for a 1.5-L bottle of soapy water that lasted longer than a bar of soap (∼US$0.40) (F. Sultana, F. A. Nizame, N. C. Dutta, L. Unicomb, P. K. Ram, S. P. Luby, P. J. Winch, manuscript in preparation), and convenient alternative found to be as microbiologically effective as soap to reduce pathogens on hands,55 and to be acceptable elsewhere in Bangladesh.44 Soapy water likely has application to other low-income settings.56 To develop an effective handwashing intervention, we suggest integrating these recommendations. The PRECEDE/PROCEED model pulls together three types of behavioral change strategies: cognitive/informational, social support/reinforcement, and enabling factors/resources. We suggest integrating all the three types into a single behavior change strategy.57 We also suggest iteratively piloting and revising the integrated intervention based on evaluation.
Acknowledgments
icddr,b acknowledges with gratitude the commitment of Bill & Melinda Gates Foundation to its research efforts. Moreover, icddr,b is thankful to the governments of Australia, Bangladesh, Canada, Sweden, and the United Kingdom for providing core/unrestricted support. We thank all the anthropologists and women from the study community who collected, videoed and processed the data, and Meghan L. Scott and Diana Diaz Granados for writing support. Finally, we like to thank the community members who gave their time and opinions.
Footnotes
Financial support: The study was funded by the Bill & Melinda Gates Foundation.
Authors' addresses: Fosiul A. Nizame, Md. Nuruzzaman, Shahana Parveen, and Leanne Unicomb, Centre for Communicable Diseases, icddr,b, Dhaka, Bangladesh, E-mails: fosiul@icddrb.org, nuruzzaman@icddrb.org, shahana@icddrb.org, and leanne@icddrb.org. Elli Leontsini and Peter J. Winch, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, E-mails: eleontsi@jhu.edu and pwinch@jhu.edu. Stephen P. Luby, Woods Institute of the Environment, Stanford University, Stanford, CA, E-mail: sluby@stanford.edu. Pavani K. Ram, University at Buffalo, State University of New York, Buffalo, NY, E-mail: pkram@buffalo.edu.
References
- 1.National Institute of Population Research and Training (NIPORT) Bangladesh Demographic and Health Survey 2011. Dhaka, Bangladesh: NIPORT and Mitra and Associates and Calverton, MD: MEASURE DHS, ICF International; 2013. [Google Scholar]
- 2.Liu L, Li Q, Lee RA, Friberg IK, Perin J, Walker N, Black RE. Trends in causes of death among children under 5 in Bangladesh, 1993–2004: an exercise applying a standardized computer algorithm to assign causes of death using verbal autopsy data. Popul Health Metr. 2011;9:43. doi: 10.1186/1478-7954-9-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kaferstein F. Foodborne diseases in developing countries: aetiology, epidemiology and strategies for prevention. Int J Environ Health Res. 2003;13((Suppl 1)):S161–S168. doi: 10.1080/0960312031000102949. [DOI] [PubMed] [Google Scholar]
- 4.Esrey SA, Feachem RG, Hughes JM. Interventions for the control of diarrhoeal diseases among young children: improving water supplies and excreta disposal facilities. Bull World Health Organ. 1985;63:757–772. [PMC free article] [PubMed] [Google Scholar]
- 5.Esrey SA. Food contamination and diarrhoea. World Health January–February. 1990:19–23. [Google Scholar]
- 6.Motarjemi Y, Kaferstein F, Moy G, Quevedo F. Contaminated weaning food: a major risk factor for diarrhoea and associated malnutrition. Bull World Health Organ. 1993;71:79–92. [PMC free article] [PubMed] [Google Scholar]
- 7.Curtis V, Cairncross S. Effect of washing hands with soap on diarrhoea risk in the community: a systematic review. Lancet Infect Dis. 2003;3:275–281. doi: 10.1016/s1473-3099(03)00606-6. [DOI] [PubMed] [Google Scholar]
- 8.Curtis V, Biran A, Deverell K, Hughes C, Bellamy K, Drasar B. Hygiene in the home: relating bugs and behaviour. Soc Sci Med. 2003;57:657–672. doi: 10.1016/s0277-9536(02)00409-4. [DOI] [PubMed] [Google Scholar]
- 9.Ehiri JE, Azubuike MC, Ubbaonu CN, Anyanwu EC, Ibe KM, Ogbonna MO. Critical control points of complementary food preparation and handling in eastern Nigeria. Bull World Health Organ. 2001;79:423–433. [PMC free article] [PubMed] [Google Scholar]
- 10.Devamani C, Norman G, Schmidt WP. A simple microbiological tool to evaluate the effect of environmental health interventions on hand contamination. Int J Environ Res Public Health. 2014;11:11846–11859. doi: 10.3390/ijerph111111846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Agustina R, Sari TP, Satroamidjojo S, Bovee-Oudenhoven IM, Feskens EJ, Kok FJ. Association of food-hygiene practices and diarrhea prevalence among Indonesian young children from low socioeconomic urban areas. BMC Public Health. 2013;13:977. doi: 10.1186/1471-2458-13-977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lynch MF, Tauxe RV, Hedberg CW. The growing burden of foodborne outbreaks due to contaminated fresh produce: risks and opportunities. Epidemiol Infect. 2009;137:307–315. doi: 10.1017/S0950268808001969. [DOI] [PubMed] [Google Scholar]
- 13.Sivapalasingam S, Friedman CR, Cohen L, Tauxe RV. Fresh produce: a growing cause of outbreaks of foodborne illness in the United States, 1973 through 1997. J Food Prot. 2004;67:2342–2353. doi: 10.4315/0362-028x-67.10.2342. [DOI] [PubMed] [Google Scholar]
- 14.Islam MS, Hasan MK, Khan SI. Growth and survival of Shigella flexneri in common Bangladeshi foods under various conditions of time and temperature. Appl Environ Microbiol. 1993;59:652–654. doi: 10.1128/aem.59.2.652-654.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kolvin JL, Roberts D. Studies on the growth of Vibrio cholerae biotype eltor and biotype classical in foods. J Hyg (Lond) 1982;89:243–252. doi: 10.1017/s0022172400070777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Luby SP, Halder AK, Huda T, Unicomb L, Johnston RB. The effect of handwashing at recommended times with water alone and with soap on child diarrhea in rural Bangladesh: an observational study. PLoS Med. 2011;8:e1001052. doi: 10.1371/journal.pmed.1001052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Monte CM, Ashworth A, Nations MK, Lima AA, Barreto A, Huttly SR. Designing educational messages to improve weaning food hygiene practices of families living in poverty. Soc Sci Med. 1997;44:1453–1464. doi: 10.1016/s0277-9536(96)00241-9. [DOI] [PubMed] [Google Scholar]
- 18.Stone VE, Hogan JW, Schuman P, Rompalo AM, Howard AA, Korkontzelou C, Smith DK, Hers S. Antiretroviral regimen complexity, self-reported adherence, and HIV patients' understanding of their regimens: survey of women in the her study. J Acquir Immune Defic Syndr. 2001;28:124–131. doi: 10.1097/00042560-200110010-00003. [DOI] [PubMed] [Google Scholar]
- 19.Martin S, Wolters PL, Calabrese SK, Toledo-Tamula MA, Wood LV, Roby G, Elliott-DeSorbo DK. Antiretroviral Regimen Complexity Index. A novel method of quantifying regimen complexity. J Acquir Immune Defic Syndr. 2007;45:535–544. doi: 10.1097/QAI.0b013e31811ed1f1. [DOI] [PubMed] [Google Scholar]
- 20.Mata J, Todd PM, Lippke S. When weight management lasts. Lower perceived rule complexity increases adherence. Appetite. 2010;54:37–43. doi: 10.1016/j.appet.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 21.Rogers EM. Diffusion of Innovations. 5th edition. New York, NY: Free Press; 2003. p. 16. [Google Scholar]
- 22.Biran A, Schmidt WP, Varadharajan KS, Rajaraman D, Kumar R, Greenland K, Gopalan B, Aunger R, Curtis V. Effect of a behaviour-change intervention on handwashing with soap in India (SuperAmma): a cluster-randomised trial. Lancet Glob Health. 2014;2:e145–e154. doi: 10.1016/S2214-109X(13)70160-8. [DOI] [PubMed] [Google Scholar]
- 23.Toure O, Coulibaly S, Arby A, Maiga F, Cairncross S. Piloting an intervention to improve microbiological food safety in peri-urban Mali. Int J Hyg Environ Health. 2013;216:138–145. doi: 10.1016/j.ijheh.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 24.Tumwine J, Katui-Katua M, Munguti K. Drawers of Water. II: 30 Years of Change in Domestic Use and Environmental Health in East Africa. London, United Kingdom: International Institute for Environment and Development; 2002. [Google Scholar]
- 25.Henry FJ, Patwary Y, Huttly SR, Aziz KM. Bacterial contamination of weaning foods and drinking water in rural Bangladesh. Epidemiol Infect. 1990;104:79–85. doi: 10.1017/s0950268800054558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mack TM. The new pan-Asian paan problem. Lancet. 2001;357:1638–1639. doi: 10.1016/s0140-6736(00)04860-1. [DOI] [PubMed] [Google Scholar]
- 27.Dreibelbis R, Winch PJ, Leontsini E, Hulland KR, Ram PK, Unicomb L, Luby SP. The Integrated Behavioural Model for Water, Sanitation, and Hygiene: a systematic review of behavioural models and a framework for designing and evaluating behaviour change interventions in infrastructure-restricted settings. BMC Public Health. 2013;13:1015. doi: 10.1186/1471-2458-13-1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sheth M, Patel J, Sharma S, Seshadri S. Hazard analysis and critical control points of weaning foods. Indian J Pediatr. 2000;67:405–410. doi: 10.1007/BF02859455. [DOI] [PubMed] [Google Scholar]
- 29.Khan M, Shahidullah M. Contrasting epidemiology of shigellae dysenteriae and shigellae flexneri, Dacca. Trans R Soc Trop Med Hyg. 1980;74:528–533. doi: 10.1016/0035-9203(80)90071-1. [DOI] [PubMed] [Google Scholar]
- 30.Nizame FA, Unicomb L, Sanghvi T, Roy S, Nuruzzaman M, Ghosh PK, Winch PJ, Luby SP. Handwashing before food preparation and child feeding: a missed opportunity for hygiene promotion. Am J Trop Med Hyg. 2013;89:1179–1185. doi: 10.4269/ajtmh.13-0434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nizame FA, Nasreen S, Halder AK, Arman S, Winch PJ, Unicomb L, Luby SP. Observed practices and perceived advantages of different hand cleansing agents in rural Bangladesh: ash, soil, and soap. Am J Trop Med Hyg. 2015;92:1111–1116. doi: 10.4269/ajtmh.14-0378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Curtis VA, Danquah LO, Aunger RV. Planned, motivated and habitual hygiene behaviour: an eleven country review. Health Educ Res. 2009;24:655–673. doi: 10.1093/her/cyp002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Whitby M, Pessoa-Silva CL, McLaws ML, Allegranzi B, Sax H, Larson E, Seto WH, Donaldson L, Pittet D. Behavioural considerations for hand hygiene practices: the basic building blocks. J Hosp Infect. 2007;65:1–8. doi: 10.1016/j.jhin.2006.09.026. [DOI] [PubMed] [Google Scholar]
- 34.Halder AK, Tronchet C, Akhter S, Bhuiya A, Johnston R, Luby SP. Observed hand cleanliness and other measures of handwashing behavior in rural Bangladesh. BMC Public Health. 2010;10:545. doi: 10.1186/1471-2458-10-545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rabbi SE, Dey NC. Exploring the gap between hand washing knowledge and practices in Bangladesh: a cross-sectional comparative study. BMC Public Health. 2013;13:89. doi: 10.1186/1471-2458-13-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Centers for Disease Control and Prevention (CDC) Wash Your Hands. 2014. http://www.cdc.gov/features/handwashing Available at. Accessed November 24, 2014.
- 37.Strohbehn C, Sneed J, Paez P, Meyer J. Hand washing frequencies and procedures used in retail food services. J Food Prot. 2008;71:1641–1650. doi: 10.4315/0362-028x-71.8.1641. [DOI] [PubMed] [Google Scholar]
- 38.Young KD, Aarde RJV. Science and elephant management decisions in South Africa. Biol Conserv. 2011;144:876–885. [Google Scholar]
- 39.Surujlal M, Badrie N. Household consumer food safety in Trinidad, West Indies. Internet J Food Saf. 2004;3:8–14. [Google Scholar]
- 40.Gorman R, Bloomfield S, Adley CC. A study of cross-contamination of food-borne pathogens in the domestic kitchen in the Republic of Ireland. Int J Food Microbiol. 2002;76:143–150. doi: 10.1016/s0168-1605(02)00028-4. [DOI] [PubMed] [Google Scholar]
- 41.Rangel JM, Sparling PH, Crowe C, Griffin PM, Swerdlow DL. Epidemiology of Escherichia coli O157:H7 outbreaks, United States, 1982–2002. Emerg Infect Dis. 2005;11:603–609. doi: 10.3201/eid1104.040739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ryan MJ, Wall PG, Gilbert RJ, Griffin M, Rowe B. Risk factors for outbreaks of infectious intestinal disease linked to domestic catering. Commun Dis Rep CDR Rev. 1996;6:R179–R183. [PubMed] [Google Scholar]
- 43.Luby SP, Halder AK, Tronchet C, Akhter S, Bhuiya A, Johnston RB. Household characteristics associated with handwashing with soap in rural Bangladesh. Am J Trop Med Hyg. 2009;81:882–887. doi: 10.4269/ajtmh.2009.09-0031. [DOI] [PubMed] [Google Scholar]
- 44.Hulland KR, Leontsini E, Dreibelbis R, Unicomb L, Afroz A, Dutta NC, Nizame FA, Luby SP, Ram PK, Winch PJ. Designing a handwashing station for infrastructure-restricted communities in Bangladesh using the integrated behavioural model for water, sanitation and hygiene interventions (IBM-WASH) BMC Public Health. 2013;13:877. doi: 10.1186/1471-2458-13-877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.UNICEF Hygiene Practices Have Helped Keep Ebola Out of the Classroom. 2015. http://www.unicef.org/media/media_82875.html Available at. Accessed February 13, 2016.
- 46.Ilesanmi OS, Alele FO. The effect of Ebola virus disease outbreak on hand washing among secondary school students in Ondo State Nigeria, October, 2014. Pan Afr Med J. 2015;22((Suppl 1)):24. doi: 10.11694/pamj.supp.2015.22.1.6614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cousens S, Kanki B, Toure S, Diallo I, Curtis V. Reactivity and repeatability of hygiene behaviour: structured observations from Burkina Faso. Soc Sci Med. 1996;43:1299–1308. doi: 10.1016/0277-9536(95)00380-0. [DOI] [PubMed] [Google Scholar]
- 48.Ram PK, Halder AK, Granger SP, Jones T, Hall P, Hitchcock D, Wright R, Nygren B, Islam MS, Molyneaux JW, Luby SP. Is structured observation a valid technique to measure handwashing behavior? Use of acceleration sensors embedded in soap to assess reactivity to structured observation. Am J Trop Med Hyg. 2010;83:1070–1076. doi: 10.4269/ajtmh.2010.09-0763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Touré O, Coulibaly S, Arby A, Maiga F, Cairncross S. Improving microbiological food safety in peri-urban Mali: an experimental study. Food Contr. 2011;22:1565–1572. [Google Scholar]
- 50.Weinstein ND, Rothman AJ, Sutton SR. Stage theories of health behavior: conceptual and methodological issues. Health Psychol. 1998;17:290–299. doi: 10.1037//0278-6133.17.3.290. [DOI] [PubMed] [Google Scholar]
- 51.Leontsini E, Rosenbaum J, Báez C, Solís A, Valera C, Gonzálvez G. NEgociación de PRÁcticas Mejoradas—NEPRÁM (Negotiation of Improved Practices): the development of a national behaviour change strategy for community-based prevention of dengue fever in the Dominican Republic. Dengue Bull. 2004;28((Suppl)):22–25. [Google Scholar]
- 52.Harvey SA, Paredes Olortegui M, Leontsini E, Ramal Asayag C, Scott K, Winch PJ. Trials of improved practices (TIPs): a strategy for making long-lasting nets last longer? Am J Trop Med Hyg. 2013;88:1109–1115. doi: 10.4269/ajtmh.12-0641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Story M, Neumark-Sztainer D, French S. Individual and environmental influences on adolescent eating behaviors. J Am Diet Assoc. 2002;102:S40–S51. doi: 10.1016/s0002-8223(02)90421-9. [DOI] [PubMed] [Google Scholar]
- 54.Gielen AC, Sleet D. Application of behavior-change theories and methods to injury prevention. Epidemiol Rev. 2003;25:65–76. doi: 10.1093/epirev/mxg004. [DOI] [PubMed] [Google Scholar]
- 55.Amin N, Pickering AJ, Ram PK, Unicomb L, Najnin N, Homaira N, Ashraf S, Abedin J, Islam MS, Luby SP. Microbiological evaluation of the efficacy of soapy water to clean hands: a randomized, non-inferiority field trial. Am J Trop Med Hyg. 2014;91:415–423. doi: 10.4269/ajtmh.13-0475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Saboori S, Mwaki A, Rheingans R. Is soapy water a viable solution for handwashing in schools? Waterlines. 2010;29:329–336. [Google Scholar]
- 57.Green LW. Health Program Planning: An Educational and Ecological Approach. 4th edition. New York, NY: McGraw-Hill; 2005. [Google Scholar]