Abstract
Cystic echinococcosis (CE) is a globally distributed zoonosis caused by the Echinococcus granulosus sensu lato species complex. Four approaches are available for treatment of abdominal CE: surgery, percutaneous aspiration, chemotherapy with albendazole, and watch-and-wait. Allocation of patients to these different treatment options mainly depends on the stage of the cystic lesion. However, as available guidelines are not widely followed, surgery is often applied even without the correct indication outside referral centers. This is not only a disadvantage for the patient, but also a waste of money. In this study, we evaluated the cost of the surgical approach for abdominal CE by analyzing hospitalization costs for 14 patients admitted to the General Surgery Ward at the “San Matteo” Hospital Foundation in Pavia, Italy, from 2008 through 2014. We found that the total cost of a single hospitalization, including hospital stay, surgical intervention, personnel, drugs, and administrative costs ranged from €5,874 to 23,077 (median €11,033) per patient. Our findings confirm that surgery can be an expensive option. Therefore, surgical intervention should be limited to cyst types that do not benefit from nonsurgical therapies and appropriate case management can best be accomplished by using a cyst stage-specific approach.
Introduction
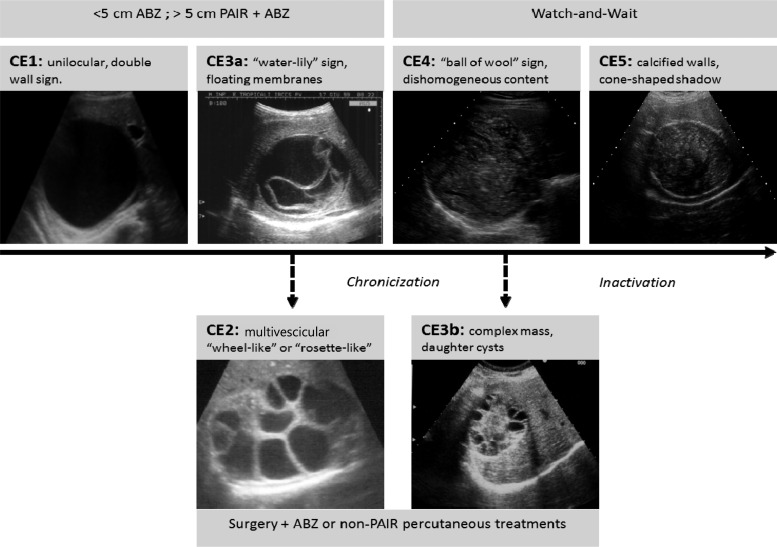
Cystic echinococcosis (CE) is a complex, chronic, and neglected disease with a cosmopolitan distribution.1 In humans, echinococcal cysts mainly form in the liver and lungs, and the clinical spectrum of infection ranges from asymptomatic to severe and rarely even fatal disease.2,3 Cysts are classified into six stages according to the World Health Organization Informal Working Group on Echinococcosis (WHO-IWGE) classification scheme (Figure 1 ).4 Four management options currently exist for uncomplicated abdominal CE: surgery, percutaneous techniques, and chemotherapy for active cysts, and a watch-and-wait approach for inactive cysts. Allocation of patients to these management options should be based on cyst stage, size, and location along with the presence of comorbidities and available clinical expertise.4 However, clinical decision algorithms, case management effectiveness, relapse rates, and costs associated with disease diagnosis and treatment have never been thoroughly evaluated.5
Figure 1.
Ultrasound classification and stage-specific approach to cystic echinococcosis (CE) cysts according to the World Health Organization Informal Working Group on Echinococcosis Expert Consensus4 modified from Rinaldi and others, 2014.8 ABZ = albendazole; PAIR = puncture, aspiration, injection, reaspiration.
There has been limited information published on the costs associated with CE in Italy. Mastrandrea and others analyzed CE-associated costs in Sardinia based on Diagnosis-Related Group (DRG) reimbursements.6 DRGs are used to classify patients into groups based on age, sex, principal diagnosis, type of treatment, discharge status, and the presence of complications or comorbidities. Under the prospective payment system, hospitals are paid a fixed fee for treating patients in a specific DRG category, regardless of the actual costs.7 To our knowledge, no data are available on detailed per-patient costs associated with the treatment of surgically managed abdominal CE cases in Italy. Such data would be helpful for comparison of different treatment options in the same clinical context, as well as for promoting a rational stage-specific treatment approach. This would encourage physicians to avoid overtreatment (e.g., to not recommend surgical management when drug therapy or watch-and-wait are more appropriate), thereby preventing the expenditure of unnecessary resources and funds. This study presents the findings of a detailed analysis of surgical costs for patients with abdominal CE treated in the same Italian center, by the same surgical team, over a period of 6 years.
Aim
The aim of this study was to provide a detailed evaluation of the costs of surgical interventions performed for abdominal CE cases at the “San Matteo” Hospital Foundation in Pavia, Italy, from 2008 through 2014.
Materials and Methods
Patient selection and management.
Patients with abdominal CE, who were admitted to the surgery ward of the “San Matteo” Hospital Foundation in Pavia, Italy, from January 2008 through November 2014, were included in the study. Clinical history and hospitalization information were collected from medical records and the database of the WHO Collaborating Center for Clinical Management of CE in Pavia, Italy, where these patients were managed postoperatively. Hepatic cysts were classified according to the WHO-IWGE classification of CE (Figure 1).
Every patient received routine preoperative blood tests, serology for viral hepatitis B and C and HIV, a urine analysis, an electrocardiogram (EKG), and thoracic radiographs. A subset of patients also received an abdominal computed tomography scan and/or additional laboratory tests. During all surgical interventions, patients were intubated and maintained on inhalant anesthesia. Peripheral and central vascular catheters, a bladder catheter, and a stomach probe were inserted and vital signs were monitored (EKG, heart rate, systolic pressure, oxygen saturation, and end-tidal carbon dioxide) throughout the procedure. In eight cases, an intraoperative ultrasound examination was performed. All patients received prophylaxis with albendazole and antibiotics.
Data collection.
Data collected included number and size of cysts, indications for the surgical intervention, complications (if any), duration of hospital stay, number and type of perioperative diagnostic tests performed, type and duration of the surgical intervention, diagnostic imaging performed, drugs administered during hospitalization, and clinical personnel involved in case management.
Cost analysis.
Itemized per-patient procedural data were compiled in a spreadsheet where costs were allocated to each item. The daily cost of hospitalization was calculated as the sum of direct and indirect costs associated with a stay in the general surgery ward. Direct costs included costs associated with healthcare personnel and the hospital room. Indirect costs included the cost of hospital maintenance, cooking and laundry services, electricity and heating for the hospital, patient transportation while hospitalized, and instrument sterilization. Surgical theatre costs included the hourly rate for the operating room and hourly wages for members of the surgical team, including anesthesiologists and nurses. Hospital administration costs (administrative personnel, bookkeeping, etc.) were assessed at 20% of the total cost for the patient. The most recent cost schedule (2013) for hospitalization-related expenses was obtained from the Management Control Service of the “San Matteo” Hospital Foundation. Laboratory and other diagnostic testing were priced using an Italian regional cost schedule for the year 2014. For surgical materials and prescribed medications, a year 2014 weighted price schedule was used based on the quantity of material used or drugs administered to an individual patient.
Results
Patients.
In total, 15 patients were surgically managed for abdominal CE during 2008–2014. One patient was excluded from the study because he also underwent a non-CE-related nephrectomy during the surgical intervention for CE. Out of the 19 cysts surgically removed, 13 were classified as CE3b, a stage known to be poorly responsive to other types of treatment.8,9 Demographic and clinical information for the 14 study patients is summarized in Table 1 . Information regarding treatment duration and medical personnel used per case is summarized in Table 2 . The median time for pericystectomy was 212 minutes, the median time for marsupialization was 182 minutes, and the median time for lobectomy was 197 minutes.
Table 1.
Summary of patient demographic and clinical information
| Demographic and clinical details | ||
|---|---|---|
| Sex | M | 12 |
| F | 2 | |
| Age (years) | Range; median value | 28–71; 44.5 |
| Country of birth | Italy | 7 |
| Other countries* | 7 | |
| No. of patients with extrahepatic (peritoneal and splenic) cysts | 1 | |
| No. of patients with multiple hepatic cysts | 4 | |
| Total number of cysts | 22 | |
| No. of hepatic cysts | 18 surgically removed; two inactive cysts not removed | |
| No. of extra-hepatic cysts | One surgically removed (splenic); one inactive peritoneal cyst not removed | |
| Size of hepatic cysts | Range; median value (mm) | 25–160; 100 |
| Location of surgically removed hepatic cysts | Left lobe (number of cysts) | 3 |
| Right lobe (number of cysts) | 15 | |
| No. of cysts per stage (WHO-IWGE) | CE3b | 13 (13 surgically removed) |
| CE3a | 1 (one surgically removed) | |
| CE4 | 8 (4 + 1† surgically removed) | |
| No. of patients with previous treatments for CE | Albendazole alone | 8 |
| Percutaneous | 1 | |
| Surgery + albendazole | 1 | |
| Percutaneous + albendazole | 2 | |
| None | 2 | |
| No. of patients with indication for surgery | Infection | 1 |
| Cystobiliary fistula | 2 | |
| Compression symptoms | 7 | |
| Unresponsiveness to albendazole | 4 | |
| No. of interventions per type | Marsupialization | 4 |
| Pericystectomy | 8 + 1‡ | |
| Lobectomy | 2 | |
| No. of patients with postsurgical complications | Early (during hospitalization) | 2 |
| Late (after discharge) | 1 | |
| None | 11 | |
CE = cystic echinococcosis; WHO-IWGE = World Health Organization Informal Working Group on Echinococcosis.
Other countries: Morocco (N = 3), Egypt (N = 1), Albania (N = 1), Macedonia (N = 1), and Moldova (N = 1).
Four CE4 cysts were hepatic, one splenic.
The patient with extra-hepatic cysts underwent a pericystectomy for the splenic cyst, and marsupialization for the liver cysts.
Table 2.
Treatment duration and number of medical personnel associated with surgical interventions
| Minimum | Maximum | Median | |
|---|---|---|---|
| Days of hospitalization (N) | 6 | 25 | 9 |
| Intervention | |||
| Intervention time (minutes) | 140 | 340 | 202 |
| Anesthesia time (minutes) | 165 | 400 | 228 |
| Operating room time (minutes) | 195 | 405 | 258 |
| Medical personnel (N) | |||
| Surgeons | 3 | 4 | 3.5 |
| Anesthesiologists | 1 | 3 | 2 |
| Nurses | 1 | 2 | 1.5 |
| Support | 1 | 2 | 1 |
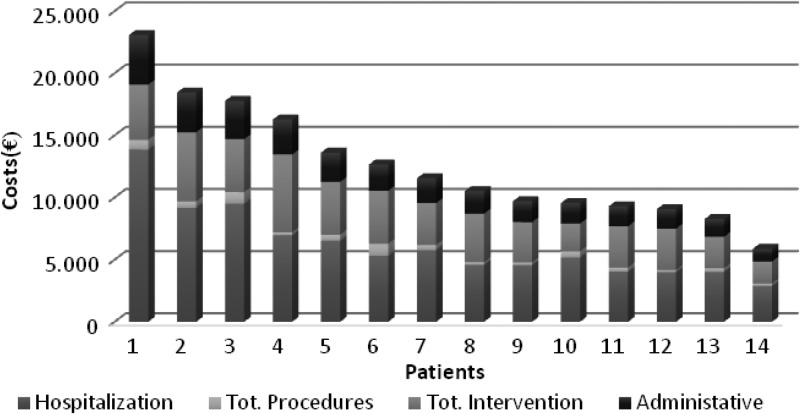
Costs.
Total surgical intervention-related costs ranged from €5,874 to 23,077 (median €11,033) per patient (Figure 2 ). The median cost for patients who underwent the marsupialization procedure was €2,525 (range: €2,224–4,262) and included two patients with CE3b cysts and one patient with a CE4 cyst. The median cost for patients who underwent a pericystectomy was €3,367 (range: €3,131–6,260) and included eight patients with CE3b cysts, one of whom had a second CE4 cyst, and one patient with a CE3a cyst. Finally, the median cost for patients who underwent a radical intervention was €4,085 (range: €3,906–4,264) and included two patients with CE3b cysts.
Figure 2.
Distribution of hospitalization and surgical intervention-related costs for each patient in decreasing order of cost. Administrative = administrative costs, fixed at the 20% of the total cost; hospitalization = cost per day × length of hospital stay; total intervention = cost of surgical intervention; total procedures = cost of all examinations performed during the hospital stay.
Time in the operating room and number of surgeons and nurses required during the procedure were the main determinants of the cost of a surgical intervention, with surgery costs ranging from €1,768 to 6,265. The patient with the highest overall cost (€13,855) had one CE3b cyst with a diameter of 14 cm and two CE4 cysts in the liver. He was the only patient with extra-hepatic cysts: one CE4 cyst in the spleen, with a diameter of 16 cm, and two in the peritoneal cavity. The liver cysts were drained and the splenic cyst was treated with a partial pericystectomy, whereas the peritoneal cyst was not treated, as it was relatively small and had been inactive from the time of the patient's first visit to the hospital in 2001. This patient was hospitalized again 5 months postsurgery due to the development of abscesses in the residual hepatic cavity and around the spleen. The second hospitalization event lasted over 40 days, with a resulting total cost of €36,105, including both procedural and hospitalization costs. None of the other 13 patients have required additional hospitalization or surgical interventions to date.
Discussion
This study presents additional details compared with previous studies that assessed the cost of CE case management using DRG related expenditures, where no or limited information was provided on the type of surgery performed, cyst(s) stage, cyst(s) location, or complications.10–12 Furthermore, all interventions in our cohort were performed in a single center with the same surgical team, minimizing differences in surgical approach and patient management. Mastrandrea and colleagues carried out a retrospective assessment of costs related to the treatment of CE in Sardinia in 2001–2009, calculating the expenses associated with diagnosis, hospitalization, and treatment.6 They analyzed a total of 1,409 hospital discharge records with a diagnosis of CE and found that over €4,500,000 were spent on the surgical treatment of the 515 patients that these records represented, resulting in an average cost of €8,738 per patient.6 Direct costs were calculated using price lists provided by the Sardinian regional government. Unfortunately, no information can be gleaned from this type of study regarding the costs of different surgical techniques or the impact of complications on the total expenditures. Providing these details makes comparisons with other viable treatment options, such as percutaneous approaches, easier.
Another weakness of studies that rely on hospital discharge records is that there is no information on the possible surgical overtreatment of inactive cysts.13 In the present study, considering the median values of each cost item (hospitalization, intervention, procedures, and administrative cost), the largest contributors to a patient's total cost were the duration of the hospital stay and the length of the surgical intervention, equating to 47% and 32% of the total cost, respectively. The patient with the highest overall cost had a prolonged hospital stay (25 days) due to the presence of extra-hepatic cysts and the need for a longer observation period. This same patient required a further hospitalization, resulting in a final total cost of over €36,000. Unexpected complications, therefore, can have a very large impact on hospitalization expenditures related to CE.
A limitation of this study is the small number of cases included, which reduces the generalizability of the findings to other national or international centers. However, this cohort encompasses the full range of abdominal CE presentations that are surgically managed at our center and we are currently prospectively collecting data on additional patients undergoing surgery for CE to expand the existing data set. Another limitation is that data about the costs of other approaches were not included, because only preliminary information about estimated costs is currently available. However, we plan to conduct similar studies on the cost of albendazole treatment, percutaneous interventions, and watch-and-wait, to compare expenditures for different management options and ultimately calculate the costs associated with treatment misallocation (e.g., treating asymptomatic inactive cysts with surgery as opposed to taking a watch-and-wait approach).
Conclusion
For the first time, this study provides detailed costs for the surgical management of patients with abdominal CE treated by the same team in a single center in Italy. We found that the largest contributors to a patient's total cost were the duration of the hospital stay and the length of the surgical intervention. We believe that studies on larger patient cohorts in different countries should be carried out to facilitate comparisons with other available treatment options and to better standardize the treatment of abdominal CE.
ACKNOWLEDGMENTS
We are grateful to Anna Obici, from the Management Control Service of the “San Matteo” Hospital Foundation for her contribution to the cost analysis.
Footnotes
Financial Support: This study was partly funded by the FP7 Human Cystic Echinococcosis ReseArch in CentraL and Eastern Societies (HERACLES) project (to Enrico Brunetti).
Authors' addresses: Roberta Narra, Francesca Tamarozzi, Mara Mariconti, Giovanni J. Nicoletti, and Francesca Rinaldi, Department of Clinical-Surgical, Diagnostic and Pediatric Sciences, University of Pavia, Pavia, Italy, and WHO Collaborating Centre for Clinical Management of Cystic Echinococcosis, Pavia, Italy, E-mails: roberta.narra1989@gmail.com, f_tamarozzi@yahoo.com, maramariconti@libero.it, jacopo.nicoletti@yahoo.it, and francescarinaldi16@yahoo.it. Marcello Maestri, Division of General Surgery, IRCCS San Matteo Hospital Foundation, Pavia, Italy, E-mail: mmaestri@smatteo.pv.it. Christine M. Budke, Department of Veterinary Integrative Biosciences, Texas A&M University, College Station, TX, E-mail: cbudke@cvm.tamu.edu. Enrico Brunetti, Department of Clinical-Surgical, Diagnostic and Pediatric Sciences, University of Pavia, Pavia, Italy, and WHO Collaborating Centre for Clinical Management of Cystic Echinococcosis, Pavia, Italy, Department of Clinical-Surgical, Diagnostic and Pediatric Sciences, University of Pavia, Pavia, Italy, and Division of Infectious and Tropical Diseases, IRCCS San Matteo Hospital Foundation, Pavia, Italy, E-mail: enrico.brunetti@unipv.it.
References
- 1.Craig PS, Budke CM, Schantz PM, Li T, Qiu J, Yang Y, Zeyhle E, Rogan MT, Ito A. Human echinococcosis: a neglected disease? Trop Med Health. 2007;35:283–292. [Google Scholar]
- 2.McManus DP, Thompson RCA. Molecular epidemiology of cystic echinococcosis. Parasitology. 2003;127:S37–S51. doi: 10.1017/s0031182003003524. [DOI] [PubMed] [Google Scholar]
- 3.Pawłowski ZS, Eckert J, Vuitton DA, Ammann RW, Kern P, Craig PS, Dar KF, De Rosa F, Filice C, Gottstein B, Grimm F, Macpherson CNL, Sato N, Todorov T, Uchino J, von Sinner W, Wen H. Echinococcosis in humans: clinical aspects, diagnosis and treatment. In: Eckert J, Gemmell MA, Meslin F-X, Pawłowski ZS, editors. WHO/OIE Manual on Echinococcosis in Humans and Animals: A Public Health Problem of Global Concern. Paris, France: World Organisation for Animal Health; 2001. pp. 20–66. [Google Scholar]
- 4.Brunetti E, Kern P, Vuitton DA. Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans. Acta Trop. 2010;114:1–16. doi: 10.1016/j.actatropica.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 5.Brunetti E, Garci HH, Junghanss T. Cystic echinococcosis: chronic, complex, and still neglected. PLoS Negl Trop Dis. 2011;5:e1146. doi: 10.1371/journal.pntd.0001146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mastrandrea S, Stegel G, Piseddu T, Ledda S, Masala G. A retrospective study on burden of human echinococcosis based on hospital discharge records from 2001 to 2009 in Sardinia, Italy. Acta Trop. 2012;123:184–189. doi: 10.1016/j.actatropica.2012.05.004. [DOI] [PubMed] [Google Scholar]
- 7.Beaty L. Understanding diagnostic related groups (DRGs) and inpatient hospital reimbursement. Gastroenterol Nurs. 2005;28:363–368. doi: 10.1097/00001610-200509000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Rinaldi F, Brunetti E, Neumayr A, Maestri M, Goblirsch S, Tamarozzi F. Cystic echinococcosis of the liver: a primer for hepatologists. World J Hepatol. 2014;6:293. doi: 10.4254/wjh.v6.i5.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Golemanov B, Grigorov N, Mitova R, Genov J, Vuchev D, Tamarozzi F, Brunetti E. Efficacy and safety of PAIR for cystic echinococcosis: experience on a large series of patients from Bulgaria. Am J Trop Med Hyg. 2011;84:48–51. doi: 10.4269/ajtmh.2011.10-0312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Benner C, Carabin H, Sánchez-Serrano LP, Budke CM, Carmena D. Analysis of the economic impact of cystic echinococcosis in Spain. Bull World Health Organ. 2010;88:49–57. doi: 10.2471/BLT.09.066795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Budke CM, Deplazes P, Torgerson PR. Global socioeconomic impact of cystic echinococcosis. Emerg Infect Dis. 2006;12:296–303. doi: 10.3201/eid1202.050499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carabin H, Budke CM, Cowan LD, Willingham AL, Torgerson PR. Methods for assessing the burden of parasitic zoonoses: echinococcosis and cysticercosis. Trends Parasitol. 2005;21:327–333. doi: 10.1016/j.pt.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 13.Piccoli L, Tamarozzi F, Cattaneo F, Mariconti M, Filice C, Bruno A, Brunetti E. Long-term sonographic and serological follow-up of inactive echinococcal cysts of the liver: hints for a “watch-and-wait” approach. PLoS Negl Trop Dis. 2014;8:e3057. doi: 10.1371/journal.pntd.0003057. [DOI] [PMC free article] [PubMed] [Google Scholar]