Abstract
Murine typhus is an acute undifferentiated febrile illness caused by Rickettsia typhi. The classic reservoir (Rattus spp.) and flea vector (Xenopsylla cheopis) were once culprits of murine typhus in the United States. Vector and rodent control efforts have drastically decreased the prevalence of disease, except in a few endemic foci where opossums and cat fleas play a role in transmission. Since 2012, there has been a reemergence of murine typhus in Galveston, TX. We hypothesize that opossums and cat fleas are involved in the transmission of R. typhi in Galveston. To explore this, we sought to find the seroprevalence of typhus group antibodies from opossums. We also sought to find the prevalence of R. typhi in fleas parasitizing these animals. We collected blood from 12 opossums and found that eight (66.7%) had the presence of anti-R. typhi antibodies. All opossums were infested with fleas; a total of 250 Ctenocephalides felis fleas were collected from these animals. Seven opossums (53.8%) were infested with fleas that had molecular evidence of R. typhi infection, while six (46.2%) were infested with fleas that contained Candidatus Rickettsia senegalensis, an organism closely related to R. felis. The minimum flea infection rate for R. typhi was 7.0%. The minimum infection rate for Candidatus R. senegalensis was 6.1%. Our study demonstrates that fleas infected with R. typhi parasitize opossums in Galveston. It is therefore likely that opossums and their fleas play a role in the city's recent reemergence of murine typhus.
Introduction
Murine typhus is an illness caused by Rickettsia typhi, a gram-negative obligate intracellular bacterium. The disease is most prevalent in tropical and subtropical coastal regions throughout the world where the primary reservoir (Rattus spp.) and the flea vector (Xenopsylla cheopis) thrive.1 The disease presents as an acute undifferentiated febrile illness. It is often clinically indistinguishable from other causes of fever, especially those prevalent in the tropics (e.g., malaria, dengue, leptospirosis, scrub typhus, and spotted fever group rickettsioses).2 Confirmation of diagnosis is difficult, as it usually requires the serologic detection of antibodies, which are often not present in the first week of illness. For these reasons, murine typhus is mostly underdiagnosed and is often not appreciated as a cause of disease.3 Although often ignored or deemed irrelevant as a cause of febrile illness, murine typhus continues to emerge as a cause of illness in communities in the United States.4–6 It has also been increasingly recognized as a cause of fever in returning travelers.2
In 1944, the number of murine typhus cases in the United States reached a peak of 5,401 and experienced a precipitous decline in the years following. This decline has been attributed to measures to control the proliferation of rats as well as the broad use of dichlorodiphenyltrichloroethane (DDT) in the mid to late 1940s, which dramatically decreased the burden of ectoparasites, such as X. cheopis, infesting rats. By 1956, only 98 cases were reported in the United States.7 In Galveston, a small city on the upper Texas coast, murine typhus was once a prevalent infectious disease. Like other parts of the United States, the incidence of disease took a remarkable decline after the initiation of DDT-driven vector control programs.8 As the disease became a rarity in most parts of the country, endemic foci in southern California and in South Texas remained. In these areas, there exists an alternate cycle of transmission thought to involve opossums and the cat flea (Ctenocephalides felis).9,10
In Galveston, after decades of apparent disease quiescence following the control of rat fleas with DDT,11,12 two cases of murine typhus were diagnosed in 2012 with an additional 12 patients in 2013.4 Since this reemergence, murine typhus has continued to affect residents of Galveston County (L. Blanton, unpublished data). We hypothesize that in Galveston, opossums play a role in the transmission of R. typhi, as they do in the southernmost counties of Texas and in southern California. To explore this hypothesis, we sought to find the prevalence of rickettsial antibodies in reservoir animals that have been implicated in the infectious cycle of R. typhi, and the presence of the bacterium within fleas parasitizing these animals.
Materials and Methods
Opossum trapping.
The Galveston Police Department Animal Services Unit provides Tomahawk cage traps (Tomahawk Live Trap, Hazelhurst, WI) to those who wish to have nuisance opossums removed from their premises. This study was conducted as part of the normal animal control efforts of the city. The traps were baited with wet canned cat food, set in the evening, and checked the following morning. Opossums successfully trapped were removed from the property for further study. To collect material for analysis, the opossums were removed from the traps and manually restrained by investigators. The opossums were combed for fleas using a commercial flea comb for pets (Sentry, Omaha, NE). Blood was collected from peripheral venous sites (external jugular or saphenous veins) via a 23-gauge needle and 3-mL syringe. Blood was placed in ethylenediaminetetraacetic acid and serum separating tubes for DNA extraction and indirect immunofluorescence assay (IFA) analysis, respectively. After sample collection, the animals were relocated to a rural island as normally performed by the employees of the Animal Services Unit. Rat trapping was also performed, but was unsuccessful (Supplemental Information).
Flea processing.
Collected fleas were transferred from the field to the laboratory, examined via a dissecting microscope, and identified using a taxonomic key.13 The fleas underwent surface decontamination by washing them in 5% bleach solution for 5 minutes, then in 70% ethanol for 5 minutes, and then in three subsequent 1 minute phosphate-buffered saline (PBS) rinses. The washed fleas were pooled in groups of two to five and in some cases processed individually. Flea pools were placed in a microcentrifuge tubes with 100 μL PBS and then homogenized using a micropestle. DNA was extracted from these homogenates using the DNeasy Blood and Tissue Kit (QIAGEN, Valencia, CA).
Molecular techniques.
DNA was extracted from 100 μL of opossum blood using the DNeasy Blood and Tissue Kit (QIAGEN). Real-time polymerase chain reaction (PCR) using primers to amplify a conserved region of the rickettsial citrate synthase gene was used to screen opossum blood and fleas for the presence of rickettsial DNA.14 Flea pools amplified by real-time PCR were then subjected to conventional PCR using primers to amplify a larger 383 base pair (bp) region of the citrate synthase gene,15 and a nested reaction to amplify a 231-bp region of the 17-kD antigen gene.10,16
Amplified PCR products of the aforementioned conventional and nested reactions were used for restriction fragment length polymorphism (RFLP) analysis. Two RFLP techniques were used to ensure consistency of results. The citrate synthase amplicons were digested using AluI (New England BioLabs, Ipswich, MA), and the nested 17-kD antigen gene amplicons were digested using XbaI (New England BioLabs) as described elsewhere.10,17 Restriction enzyme digestion of amplified PCR products from cell culture–propagated R. typhi and R. felis DNA were used as positive controls. The digested products were analyzed by separation on 8% precast polyacrylamide gels (Life Technologies, Grand Island, NY), stained with ethidium bromide as per the manufacturer's instructions, and visualized using a Gel Doc System (Bio-Rad, Hercules, CA). Samples were considered positive for the presence of a rickettsial species if the digestion products from both the citrate synthase and 17-kD gene amplicons were available for analysis.
To confirm the results of the RFLP analysis, DNA from six flea pools (three with RFLP results corresponding to R. typhi and three with RFLP results corresponding to R. felis) were subjected to conventional PCR using primers to amplify portions of the 17 kD,16 outer membrane protein B (OmpB),18 and citrate synthase genes15 as previously described. PCR products were then cloned in chemically competent Escherichia coli cells using the TOPO TA Cloning Kit (Life Technologies). Plasmid DNA was purified with the PureLink Plasmid Miniprep Kit (Life Technologies). To ensure an accurate sequence, plasmid DNA extracted from each clone was sequenced in triplicate using a 3130xl Genetic Analyzer (Life Technologies).
Immunofluorescence assays.
Opossum serum was tested for antibodies against R. typhi, R. felis, and Rickettsia rickettsii using IFA. Rickettsia typhi and R. rickettsii were grown in Vero cells and used as whole cell antigen with assays performed as previously described.19 Rickettsia felis Pedreira strain, kindly provided by Marcelo Labruna, was grown in S2 cells as described elsewhere20 and used to prepare antigen slides as similar to those for R. typhi and R. rickettsii. The secondary antibody used in these assays was fluorescein isothiocyanate–conjugated rabbit anti-opossum IgG–h+l (Bethyl Laboratories, Montgomery, TX) used at a dilution of 1:400. Sera from human cases of murine typhus and spotted fever rickettsiosis were used as positive controls on R. typhi and R. rickettsii IFA slides, respectively. Secondary antibody used for these positive controls was Alexa Fluor 488-conjugated goat anti-human IgG (γ-chain specific) at a dilution of 1:400 (Jackson ImmunoResearch Laboratories, West Grove, PA). Serum from an R. felis-infected guinea pig, collected 4 weeks after intraperitoneal inoculation, was used as a positive control for the R. felis antigen slides. Secondary antibody used for this control was Alexa Fluor 488-conjugated goat anti-guinea pig IgG (H+L) at a dilution of 1:1,000 (Life Technologies). Slides were examined on an Olympus BX61 fluorescence microscope (Olympus Scientific Solutions, Waltham, MA) at a magnification of 400×.
Analysis.
An estimation of the minimum infection rate (MIR) of pooled flea samples was performed using computational methods described by Biggerstaff21 with downloadable software for use in Microsoft Excel 2010 (Redmond, WA).22 This calculation was used to estimate the MIR of flea pools collected from individual opossums and from the total pools collected from all opossums. In cases where all pools were positive (a scenario in which the abovementioned software is unable to make its calculated estimate), the analysis was performed with the assumption that each pool contained one positive flea.
Results
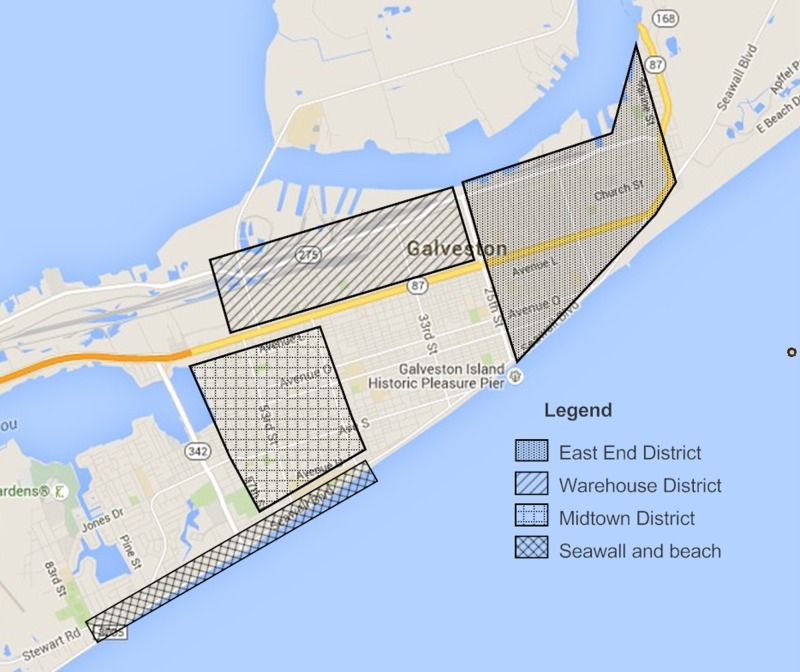
Of opossums trapped by the Galveston Police Department Animal Services Unit during the summer and fall of 2014, 12 were analyzed for the purposes of this study. Material from an additional opossum, caught during attempts to trap rats in July 2015 (Supplemental Information), was also used for analysis. The trapped opossums were caught from properties spread throughout the city (Figure 1 ). Seven (53.8%) were female, and six (46.2%) were male. Seven (53.8%) were adults, and the remaining six (46.2%) were juveniles. Of these opossums, blood for serologic and molecular analysis was obtained in 12 (in one animal, attempts to collect blood were unsuccessful). Quantitative real-time PCR screening of blood from these opossums was negative for the amplification of rickettsial DNA. IFA of available sera revealed the presence of antibodies reactive against R. typhi in eight (66.7%), R. felis in two (16.7%), and R. rickettsii in three (25.0%) (Table 1). Of those with reactive sera by IFA, the geometric mean reciprocal titers were 1,448, 256, and 203 for R. typhi, R. felis, and R. rickettsii, respectively.
Figure 1.
Locations of opossums collected for analysis.
Table 1.
Seroreactivity of opossums against Rickettsia typhi, Rickettsia felis, and Rickettsia rickettsii antigens
| Opossum | Reciprocal IFA titer |
||
|---|---|---|---|
| R. typhi | R. felis | R. rickettsii | |
| 1 | 256 | NR | NR |
| 2 | 8,192 | 512 | 256 |
| 3 | NR | NR | NR |
| 4 | 4,096 | 128 | 256 |
| 5 | NR | NR | NR |
| 6 | NR | NR | NR |
| 7 | 1,024 | NR | 128 |
| 8 | 1,024 | NR | NR |
| 9 | NA | NA | NA |
| 10 | 1,024 | NR | NR |
| 11 | 2,048 | NR | NR |
| 12 | NR | NR | NR |
| 13 | 1,024 | NR | NR |
| 1,448* | 256* | 203* | |
IFA = immunofluorescence assay; NA = not available; NR = nonreactive at a titer of 1:128.
Geometric mean of the reciprocal titer for reactive samples.
All 13 opossums included in this study were infested with fleas (Table 2). A total of 250 C. felis fleas were collected and grouped into 68 pools. Thirty-eight (55.9%) flea pools contained rickettsial DNA amplified by real-time PCR. Of these, 33 and 29 were amplified by conventional PCR for the citrate synthase and 17-kD antigen genes, respectively. The resultant amplicon bands were intense enough for interpretation of RFLP analysis in 27 citrate synthase and 17-kD gene pairs, which represent 39.7% of the total pools of fleas. Of these, 13 (19.1%), 11 (16.2%), and three (4.4%) had an RFLP banding pattern for R. typhi, R. felis, and coinfection with both agents, respectively. The estimated MIR for R. typhi was 7.0% (95% confidential interval [CI], 4.2–10.9%). The MIR of fleas with DNA similar to R. felis was 6.1% (95% CI, 3.5–9.8%). Seven opossums (53.8%) were infested with fleas that contained DNA of R. typhi. Six opossums (46.2%) were infested with fleas that contained DNA, consistent with those previously reported for R. felis by RFLP analysis.10,17
Table 2.
Molecular evidence of rickettsiae infecting fleas collected from opossums
| Opossum | No. of flea pools (total fleas) | No. of positive pools |
MIR % (95% CI) |
|||
|---|---|---|---|---|---|---|
| Rickettsia typhi | Rickettsia felis-like | R. typhi and R. felis-like | R. typhi | R. felis-like | ||
| 1 | 3 (7) | 0 | 0 | 0 | 0 | 0 |
| 2 | 3 (8) | 1 | 0 | 0 | 12.7 (0.8–52.3) | 0 |
| 3 | 6 (17) | 2 | 0 | 0 | 12.6 (2.4–37.2) | 0 |
| 4 | 8 (35) | 1 | 2 | 3 | 13.9 (4.8–32.0) | 19.2 (7.8–41.2) |
| 5 | 16 (83) | 3 | 0 | 0 | 3.8 (1.0–10.1) | 0 |
| 6 | 2 (4) | 0 | 1 | 0 | 0 | 24.9 (1.6–82.0) |
| 7 | 5 (25) | 0 | 2 | 0 | 0 | 8.8 (1.7–27.9) |
| 8 | 3 (7) | 3 | 0 | 0 | 42.9* | 0 |
| 9 | 2 (4) | 0 | 0 | 0 | 0 | 0 |
| 10 | 6 (24) | 2 | 1 | 0 | 8.9 (1.7–27.6) | 4.2 (0.3–19.2) |
| 11 | 7 (19) | 0 | 1 | 0 | 0 | 5.3 (0.3–23.7) |
| 12 | 5 (15) | 0 | 4 | 0 | 0 | 36.3 (13.5–77.1) |
| 13 | 2 (2) | 1 | 0 | 0 | 50.0* | 0 |
| Total | 68 (250) | 13 | 11 | 3 | 7.0 (4.4–10.9) | 6.1% (3.5–9.8) |
CI = confidential interval; MIR = minimum infection rate.
When all pools are positive or fleas are tested individually, the likelihood methods for the estimated MIR fail. In these cases, the calculation was performed with the assumption that there is only one infected flea per positive pool.
Amplification by conventional PCR and subsequent sequencing confirmed the results of the RFLP analysis, which had demonstrated R. typhi. When compared with the R. typhi prototype strain Wilmington, Basic Local Alignment Search Tool (BLAST) analysis of the DNA sequences of the citrate synthase (GenBank accession numbers KU167053 [342/342 bp], KU167055 [342/342 bp], KU167056 [341/342 bp]), 17-kD antigen gene (KU167047 [394/394 bp], KU167049 [394/394 bp], KU167050 [394/394 bp]), and OmpB gene amplicons (KU167059 [766/770 bp], KU167061 [770/770 bp], KU167062 [769/770 bp]) were very similar. These sequences were also very similar to the sequenced portions of an R. typhi isolate collected from a Galvestonian patient with murine typhus in 2013.4
Sequencing of samples with RFLP patterns suggestive of R. felis demonstrated the presence of DNA with close homology to sequences of organisms closely related to R. felis. BLAST analysis of the citrate synthase (KU167054 [342/342 bp], KU167057 [342/342 bp], and KU167058 [342/342 bp]) and OmpB (KU167060 [770/770 bp], KU167063 [768/770 bp], and KU167064 [769/770 bp]) gene amplicons revealed closest homology to Candidatus Rickettsia senegalensis. The 17-kD antigen gene sequences (KU167048 [393/394 bp], KU167051 [394/394 bp], and KU167052 [394/394 bp]) showed closest homology to a previously reported sequence generated from C. felis fleas collected in South Carolina.
Discussion
After the DDT-related reduction of X. cheopis on rats, the incidence of murine typhus in the United States was greatly reduced.7 Despite the dramatic effect of DDT, endemic foci of murine typhus have remained in southern California and in South Texas, where there exists an apparent alternate reservoir–vector cycle of transmission.23 This alternate cycle of transmission, involving opossums and their fleas, was first noted during a study to elucidate the cause of murine typhus occurring in suburban Los Angeles, away from the traditional urban focus of disease.9 Since then, opossums and their fleas (C. felis) have been implicated as a presumed reservoir–vector source, which fuels the remaining foci of endemicity in the United States.5,9,10,24,25
In Galveston, as in the rest of the country, the incidence of murine typhus sharply decreased with the dusting of rat runs with DDT.8 Even after discontinuation of the pesticide due to environmental concerns, the disruption of the disease cycle seemed to have lasting effects. When murine typhus made an apparent reappearance in Galveston, we could not help but wonder if the alternate cycle of transmission had a role in its reemergence. After all, opossums and C. felis fleas have been linked to cases of murine typhus in a city with longstanding endemicity (Corpus Christi, TX)11,12 and in a city with a recent outbreak (Austin, TX)5—both of which are only 220 miles from Galveston.
The reported prevalence of antibodies to R. typhi in opossums has varied depending on the location, year, and methods used to detect anti-R. typhi antibodies. Studies in Corpus Christi have found the R. typhi seroprevalence in opossums to be 60%, 25%, and 8% by latex agglutination, enzyme-linked immunoassay, and IFA, respectively.25,26 In the investigation, which described an outbreak of murine typhus in Austin, 70.6%, 47.1%, and 29.4% of opossums were reported to be seropositive at minimum reciprocal IFA IgG titers of 32, 64, and 128, respectively.5 In California, the seroprevalence rates in opossums trapped in the vicinity of human murine typhus cases have varied. The aforementioned study by Adams and others, which first implicated opossums and their fleas as a potential culprit, found 10.7% of opossums were seropositive for typhus group antibodies.9 Subsequent studies have reported 0% and 42% seropositivity.24,27 In our study, two-thirds of opossums were seropositive for anti-R. typhi antibodies at a conservative cutoff titer (1:128).
In this study, the estimated MIR of R. typhi in C. felis fleas was 7.0% (95% CI, 4.2–10.9%). This is likely an underestimate, considering the lower sensitivity of conventional PCR used for the RFLP analysis, compared with the initial screening real-time PCR, but is still a relatively high prevalence of R. typhi among fleas compared with other areas of the United States where murine typhus is endemic. The presence of R. typhi within C. felis fleas collected from opossums in Corpus Christi has been reported to range from 0.6% to 0.8%.10,25 In southern California, an MIR of 1.7% for R. typhi has been found in pools of fleas collected from Orange County and Los Angeles County opossums.27 In contrast, fleas collected from opossums in San Bernardino County, an area with fewer reported human cases than Orange and Los Angeles counties, showed no evidence of infection with R. typhi.28
None of the opossums analyzed had evidence of rickettsemia by PCR. Although the kinetics of circulating rickettsiae within opossums is unknown, the absence of rickettsemia in these opossums is not entirely surprising, as our analysis only represents a snapshot in time. Even in humans acutely ill with rickettsioses, detected rickettsemia seems to be an event that occurs late in the course of severe illness, limiting the use of PCR as a sensitive diagnostic tool during acute illness. Furthermore, the detection of anti-rickettsial antibodies via serologic assays during the later stages of acute illness correlates with the clearance of DNA in the bloodstream and inability to cultivate the organism from peripheral blood.29
In this study, we were unable to capture rats for analysis. This certainly does not mean there is an absence of rats in the city of Galveston, but this may indicate a relatively small population compared with that in decades past. Although trapping was performed over several parts of the island, including areas with reported sightings by residents, rat infestations may be localized to individual homes or buildings in which trappings were not performed.
Interestingly, in our study, we found no evidence of R. felis DNA from our sequencing analysis. Rather, these fleas demonstrated the presence of another rickettsial organism with close relation to R. felis. The amplified OmpB and citrate synthase genes showed close homology to the organism termed Candidatus R. senegalensis (isolated from C. felis fleas obtained from a cat in Dakar, Senegal).30 The 17-kD antigen gene was homologous to a sequence generated from a C. felis flea collected from a dog in South Carolina.31 Like R. felis, Candidatus R. senegalensis and Candidatus Rickettsia asemboensis (another closely related rickettsiae) have been identified in C. felis fleas.30,32,33 The pathogenic potential of these two rickettsiae for humans is unknown; they may simply play a role as a symbiont or commensal in fleas. In our study, two opossums had antibodies reactive against both spotted fever and transitional group rickettsial antigens (R. rickettsii and R. felis, respectively), but these same opossums also had much higher antibody titers to R. typhi. Therefore, these low titers against R. rickettsii and R. felis may be explained by cross-reactivity to non-lipopolysaccharide-related antigens common within all rickettsial groups.19,34 Although we cannot exclude the possibility that Candidatus R. senegalensis was responsible for the induction of antibodies reactive against R. felis and R. rickettsii, we speculate that this agent does not cause a robust antibody response in opossums, as R. typhi does.
The apparent eradication of murine typhus after the use of DDT is a remarkable example of vector control as a means of controlling human disease. With the resurgence of murine typhus in Galveston, its appearance in other communities, and the potential of R. typhi to spread to areas where non-classical reservoirs (i.e., opossums) thrive, it is important to understand the dynamics of potential reservoirs and vectors in respect to human disease. It is also imperative to recognize murine typhus as a cause of febrile illness and consider vector/reservoir control as a means of curbing its reemergence.
Supplementary Material
ACKNOWLEDGMENTS
We thank the Galveston Police Department Animal Services Unit and the Galveston Island Humane Society for their cooperation and assistance in the collection of samples from opossums.
Footnotes
Financial support: This work was supported by the Carnage and Martha Walls Distinguished University Chair in Tropical Diseases Endowment.
Authors' addresses: Lucas S. Blanton, Division of Infectious Diseases, Department of Internal Medicine, University of Texas Medical Branch, Galveston, TX, E-mail: lsblanto@utmb.edu. Boluwatife M. Idowu and Tyler N. Tatsch, School of Medicine, University of Texas Medical Branch, Galveston, TX, E-mails: mbidowu@utmb.edu and tntatsch@utmb.edu. Joshua M. Henderson, Galveston Police Department Animal Services Unit, Galveston, TX, E-mail: jhenderson@cityofgalveston.org. Donald H. Bouyer and David H. Walker, Department of Pathology, University of Texas Medical Branch, Galveston, TX, E-mails: dobouyer@utmb.edu and dwalker@utmb.edu.
References
- 1.Civen R, Ngo V. Murine typhus: an unrecognized suburban vectorborne disease. Clin Infect Dis. 2008;46:913–918. doi: 10.1086/527443. [DOI] [PubMed] [Google Scholar]
- 2.Walter G, Botelho-Nevers E, Socolovschi C, Raoult D, Parola P. Murine typhus in returned travelers: a report of thirty-two cases. Am J Trop Med Hyg. 2012;86:1049–1053. doi: 10.4269/ajtmh.2012.11-0794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chikeka I, Dumler JS. Neglected bacterial zoonoses. Clin Microbiol Infect. 2015;21:404–415. doi: 10.1016/j.cmi.2015.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blanton LS, Vohra RF, Bouyer DH, Walker DH. Reemergence of murine typhus in Galveston, Texas, USA, 2013. Emerg Infect Dis. 2015;21:484–486. doi: 10.3201/eid2103.140716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Adjemian J, Parks S, McElroy K, Campbell J, Eremeeva ME, Nicholson WL, McQuiston J, Taylor J. Murine typhus in Austin, Texas, USA, 2008. Emerg Infect Dis. 2010;16:412–417. doi: 10.3201/eid1603.091028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention Murine typhus—Hawaii, 2002. MMWR. 2003;52:1224–1226. [PubMed] [Google Scholar]
- 7.Pratt HD. The changing picture of murine typhus in the United States. Ann N Y Acad Sci. 1958;70:516–527. doi: 10.1111/j.1749-6632.1958.tb35408.x. [DOI] [PubMed] [Google Scholar]
- 8.Strandtmann RW, Eben DJ. A survey of typhus in rats and rat ectoparasites in Galveston, Texas. Tex Rep Biol Med. 1953;11:144–151. [PubMed] [Google Scholar]
- 9.Adams WH, Emmons RW, Brooks JE. The changing ecology of murine (endemic) typhus in southern California. Am J Trop Med Hyg. 1970;19:311–318. doi: 10.4269/ajtmh.1970.19.311. [DOI] [PubMed] [Google Scholar]
- 10.Schriefer ME, Sacci JB, Jr, Taylor JP, Higgins JA, Azad AF. Murine typhus: updated roles of multiple urban components and a second typhus like Rickettsia. J Med Entomol. 1994;31:681–685. doi: 10.1093/jmedent/31.5.681. [DOI] [PubMed] [Google Scholar]
- 11.Older JJ. The epidemiology of murine typhus in Texas, 1969. JAMA. 1970;214:2011–2017. [PubMed] [Google Scholar]
- 12.Taylor JP, Betz TG, Rawlings JA. Epidemiology of murine typhus in Texas: 1980 through 1984. JAMA. 1986;255:2173–2176. [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention Pictorial Key to Arthropods, Reptiles, Birds, and Mammals of Public Health Significance. 2006. http://www.cdc.gov/nceh/ehs/publications/pictorial_keys.htm Available at. Accessed November 19, 2015.
- 14.Labruna MB, Whitworth T, Horta MC, Bouyer DH, McBride JW, Pinter A, Popov V, Gennari SM, Walker DH. Rickettsia species infecting Amblyomma cooperi ticks from an area in the state of Sao Paulo, Brazil, where Brazilian spotted fever is endemic. J Clin Microbiol. 2004;42:90–98. doi: 10.1128/JCM.42.1.90-98.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Regnery RL, Spruill CL, Plikaytis BD. Genotypic identification of rickettsiae and estimation of intraspecies sequence divergence for portions of two rickettsial genes. J Bacteriol. 1991;173:1576–1589. doi: 10.1128/jb.173.5.1576-1589.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Webb L, Carl M, Malloy DC, Dasch GA, Azad AF. Detection of murine typhus infection in fleas by using the polymerase chain reaction. J Clin Microbiol. 1990;28:530–534. doi: 10.1128/jcm.28.3.530-534.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zavala-Velazquez JE, Zavala-Castro JE, Vado-Solis I, Ruiz-Sosa JA, Moron CG, Bouyer DH, Walker DH. Identification of Ctenocephalides felis fleas as a host of Rickettsia felis, the agent of a spotted fever rickettsiosis in Yucatan, Mexico. Vector Borne Zoonotic Dis. 2002;2:69–75. doi: 10.1089/153036602321131869. [DOI] [PubMed] [Google Scholar]
- 18.Roux V, Raoult D. Phylogenetic analysis of members of the genus Rickettsia using the gene encoding the outer-membrane protein rOmpB (ompB) Int J Syst Evol Microbiol. 2000;50:1449–1455. doi: 10.1099/00207713-50-4-1449. [DOI] [PubMed] [Google Scholar]
- 19.Philip RN, Casper EA, Ormsbee RA, Peacock MG, Burgdorfer W. Microimmunofluorescence test for the serological study of Rocky Mountain spotted fever and typhus. J Clin Microbiol. 1976;3:51–61. doi: 10.1128/jcm.3.1.51-61.1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Luce-Fedrow A, Macaluso KR, Richards AL. Growth of Rickettsia felis in Drosophila melanogaster S2 cells. Vector Borne Zoonotic Dis. 2014;14:101–110. doi: 10.1089/vbz.2013.1370. [DOI] [PubMed] [Google Scholar]
- 21.Biggerstaff BJ. Confidence intervals for the difference of two proportions estimated from pooled samples. J Agric Biol Environ Stat. 2008;13:478–496. [Google Scholar]
- 22.Centers for Disease Control and Prevention Mosquito Surveillance Software. 2015. http://www.cdc.gov/westnile/resourcepages/mosqsurvsoft.html Available at. Accessed April 8, 2016.
- 23.Azad AF, Radulovic S, Higgins JA, Noden BH, Troyer JM. Flea-borne rickettsioses: ecologic considerations. Emerg Infect Dis. 1997;3:319–327. doi: 10.3201/eid0303.970308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sorvillo FJ, Gondo B, Emmons R, Ryan P, Waterman SH, Tilzer A, Andersen EM, Murray RA, Barr R. A suburban focus of endemic typhus in Los Angeles County: association with seropositive domestic cats and opossums. Am J Trop Med Hyg. 1993;48:269–273. doi: 10.4269/ajtmh.1993.48.269. [DOI] [PubMed] [Google Scholar]
- 25.Boostrom A, Beier MS, Macaluso JA, Macaluso KR, Sprenger D, Hayes J, Radulovic S, Azad AF. Geographic association of Rickettsia felis-infected opossums with human murine typhus, Texas. Emerg Infect Dis. 2002;8:549–554. doi: 10.3201/eid0806.010350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Buttery CM, Magnuson LW, McLerran G, Villarreal T. Endemic (murine) typhus in Corpus Christi. Tex Med. 1984;80:53–54. [PubMed] [Google Scholar]
- 27.Eremeeva ME, Karpathy SE, Krueger L, Hayes EK, Williams AM, Zaldivar Y, Bennett S, Cummings R, Tilzer A, Velten RK, Kerr N, Dasch GA, Hu R. Two pathogens and one disease: detection and identification of flea-borne rickettsiae in areas endemic for murine typhus in California. J Med Entomol. 2012;49:1485–1494. doi: 10.1603/me11291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abramowicz KF, Wekesa JW, Nwadike CN, Zambrano ML, Karpathy SE, Cecil D, Burns J, Hu R, Eremeeva ME. Rickettsia felis in cat fleas, Ctenocephalides felis parasitizing opossums, San Bernardino County, California. Med Vet Entomol. 2012;26:458–462. doi: 10.1111/j.1365-2915.2012.01017.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.La Scola B, Raoult D. Diagnosis of Mediterranean spotted fever by cultivation of Rickettsia conorii from blood and skin samples using the centrifugation-shell vial technique and by detection of R. conorii in circulating endothelial cells: a 6-year follow-up. J Clin Microbiol. 1996;34:2722–2727. doi: 10.1128/jcm.34.11.2722-2727.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mediannikov O, Aubadie-Ladrix M, Raoult D. Candidatus ‘Rickettsia senegalensis' in cat fleas in Senegal. New Microbes New Infect. 2015;3:24–28. doi: 10.1016/j.nmni.2014.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reeves WK, Nelder MP, Korecki JA. Bartonella and Rickettsia in fleas and lice from mammals in South Carolina, USA. J Vector Ecol. 2005;30:310–315. [PubMed] [Google Scholar]
- 32.Luce-Fedrow A, Maina AN, Otiang E, Ade F, Omulo S, Ogola E, Ochieng L, Njenga MK, Richards AL. Isolation of Candidatus Rickettsia asemboensis from Ctenocephalides fleas. Vector Borne Zoonotic Dis. 2015;15:268–277. doi: 10.1089/vbz.2014.1744. [DOI] [PubMed] [Google Scholar]
- 33.Jiang J, Maina AN, Knobel DL, Cleaveland S, Laudisoit A, Wamburu K, Ogola E, Parola P, Breiman RF, Njenga MK, Richards AL. Molecular detection of Rickettsia felis and Candidatus Rickettsia asemboensis in fleas from human habitats, Asembo, Kenya. Vector Borne Zoonotic Dis. 2013;13:550–558. doi: 10.1089/vbz.2012.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vishwanath S. Antigenic relationships among the rickettsiae of the spotted fever and typhus groups. FEMS Microbiol Lett. 1991;65:341–344. doi: 10.1016/0378-1097(91)90238-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.