Abstract
Objectives
Radical trachelectomy has enabled select women with stage I cervical cancer to maintain fertility after treatment. Tumor size ≥2 cm has been considered a contraindication and those patients denied trachelectomy. We report our trachelectomy experience with tumors measuring 2–4 cm.
Methods
We retrospectively reviewed the medical records of all patients planned for fertility-sparing radical trachelectomy. Largest tumor dimension was determined by physical exam, preoperative MRI, or pathology. No patient received neoadjuvant chemotherapy.
Results
Twenty-nine of 110 (26%) patients had stage IB1 disease with tumors 2–4 cm. Median age was 31 years (range, 22–40) and 83% were nulliparous. Thirteen (45%) had squamous cell carcinoma, 12 (41%) adenocarcinoma, and 4 (14%) adenosquamous. Thirteen of 29 (45%) patients had positive pelvic nodes. All paraortic nodes were negative. Due to intraoperative frozen section, 13 (45%) patients underwent immediate hysterectomy and 1 (3%) definitive chemoradiation. Due to high-risk features on final pathology, 6 (21%) patients who had retained their uterus received chemoradiation. Nine (31%) patients underwent a fertility-sparing procedure. At median follow-up 44 months (range, 1–90) there was one recurrence.
Conclusions
Expanding radical trachelectomy inclusion criteria to women with 2–4 cm tumors allows for a fertility-sparing procedure in 30% of patients who would otherwise have been denied the option, with no compromise in oncologic outcome.
Introduction
There has been a dramatic shift from skepticism to acceptance of radical trachelectomy as a treatment option for early stage cervical cancer in young women who seek to preserve fertility since the first reports were published by Eugen Aburel and Daniel Dargent (1–3). The National Comprehensive Cancer Network’s cervical cancer guidelines now include radical trachelectomy as an option for young women who wish to preserve fertility and have tumors that are stage IA1 with lymph vascular space invasion, stage IA2, or stage IB1. Dargent initially described the radical trachelectomy as a vaginal procedure and it has typically been considered for patients with less than 2 cm lesions due to a high recurrence rate in those patients with larger lesions. The introduction of an abdominal technique (type C1 resection), and more recently a robotic approach mimicking the abdominal approach, has greatly expanded the availability of the procedure as a more radical resection can be attained compared to a vaginal approach. More than 1,000 cases of radical trachelectomy have been reported in over 200 publications (2,3,5). Key to acceptance of the radical trachelectomy has been the fact that the oncologic outcomes are maintained. Eligibility criteria were initially limited to those with no more than stage IB1 tumors of favorable histology and size less than 2 cm due to concerns regarding oncologic safety in cases with larger tumors. Adhering to these inclusion criteria, the vaginal approach, a type B resection (comparable to a modified radical hysterectomy), results in a recurrence rate of less than 5%, which is equivalent to that seen with radical hysterectomy (5, 6).
The abdominal radical trachelectomy is a wider resection (comparable to a type C1 radical hysterectomy) that captures a larger portion of the parametria (7). The introduction of the abdominal radical trachelectomy was initially met with hesitation. The procedure involves interruption in the uterine vasculature at the origin from the hypogastric, and there was concern about the effect this may have on future pregnancies. However, this procedure has been shown to maintain oncologic and fertility outcomes and has now been adopted at an ever increasing number of centers (8–12). As a result of the wider resection margins, some have advocated expanding the selection criteria of radical trachelectomy to include those women with stage IB1 tumors measuring 2 to 4 cm in size. This is an area of ongoing controversy with significant variability in outcomes noted among the available publications. Here we present a single institution series of patients with stage IB1 cervical cancer measuring 2 to 4 cm in size, with a focus on oncologic outcomes.
Materials and Methods
Institutional Review Board approval was obtained to identify and review the records of all patients planned for radical trachelectomy. Clinical databases at Memorial Sloan-Kettering Cancer Center, New York, NY were queried to identify patients with cervical cancer who were planned for radical trachelectomy between January 2001 and July 2011 and insure all cases were captured. This is a consecutive set of patients. Pediatric and adolescent patients were excluded. Patients with high-risk histology (eg, neuroendocrine, adenoma malignum) or stage IIA-IVB were not considered eligible for attempt at radical trachelectomy. Tumor size measurements were based on exam, magnetic resonance imaging (MRI), loop electrosurgical excisional procedure (LEEP), cone or trachelectomy pathology, or on the sum of dimensions measured on LEEP/cone and trachelectomy specimens. In some cases size determinations were discrepant amongst the three methodologies and the largest size was used. Additionally, in certain cases the final pathology revealed a larger tumor than identified on preoperative assessment. All patients had preoperative imaging (MRI or PET/CT) to confirm no evidence of locally advanced or metastatic disease.
All patients were consented for a radical trachelectomy with lymph node dissection and/or sentinel lymph node mapping, as well as possible radical hysterectomy based on intraoperative findings. The surgical techniques utilized have been described previously (14–16). The surgical approach (laparotomy, laparoscopy, or robotic assisted laparoscopy) and the decision of whether to include sentinel lymph node mapping were based on surgeon and patient preferences. Pelvic node dissection (with or without sentinel lymph node mapping) was completed, with frozen-section of suspicious nodes. Frozen-section of uterine curettings and a shaved margin of the cervix were performed. Patients with pathology-confirmed metastasis to the nodes, and/or tumor in the uterine curettings or shaved margin underwent immediate radical hysterectomy. Cerclage placement was performed at the surgeon’s discretion. Recommendations for postoperative chemotherapy or radiation were based on pathologic high-risk features, such as nodal metastasis or parametrial involvement, as well as for those with intermediate risk factors. Specific treatment recommendations were at the discretion of the gynecologic oncologist and radiation oncologist.
Demographic and clinical data were extracted from the medical records including information on past medical and obstetric history, pathology findings, surgical procedure details, adjuvant therapy and clinical outcomes. Standard descriptive statistics were used.
Results
We identified 110 patients planned for fertility-sparing radical trachelectomy. Twenty-nine (26%) of these patients had stage IB1 tumors 2–4 centimeters in size: 15 of the 29 (52%) were 2–2.9 cm and 14 of the 29 (48%) were 3–4 cm. The size of the tumor was determined by preoperative assessment (exam, MRI, and/or cone/LEEP pathology) for 18 (62%) patients and postoperative assessment (trachelectomy or summation of LEEP/cone and trachelectomy specimens) for 11 (38%). No patient had a tumor greater than 4 centimeters on exam, MRI or pathology. No patient received neoadjuvant chemotherapy. Fourteen patients (48%) had a biopsy as the only method of preoperative diagnosis; 15 (42%) had a LEEP or cold knife cone, in addition to biopsy. Five surgeons performed the 29 procedures. Twenty-two (76%) cases were approached abdominally, 6 (21%) vaginally with laparoscopic assistance for the nodal assessment, and 1 (3%) with a robotic platform. All 6 patients who underwent a vaginal/laparoscopic procedure had tumors 2–2.8 cm in size identified by pathology specimen, and not physical exam or MRI. The first attempt at radical trachelectomy for a tumor 2–4 cm was in 2002; 22 of the 29 patients had their procedure after May 2005, when the abdominal approach became more utilized in our group and we expanded the inclusion criteria to include IB1 lesions 2–4 cm in size. The 29 patients had a median age of 31 years (range, 22–40 years). Twenty-four (83%) were nulliparous, 4 (14%) had one child and 1 (3%) had 2 children [Table 1].
Table 1.
Patient characteristics
| Patients | 29 | |
|
| ||
| Median Followup | 44 (range 1–90) | |
|
| ||
| Median age | 31 years (range 22–40) | |
|
| ||
| Number of prior children | ||
|
| ||
| 0 | 24 (83%) | |
| 1 | 4 (14%) | |
| 2 | 1 (3%) | |
|
| ||
| Stage | ||
|
| ||
| IB1 | 29 (100%) | |
|
| ||
| Histology | ||
|
| ||
| Squamous | 13 (45%) | |
| Adenosquamous | 4 (14%) | |
| Adenocarcinoma | 12 (41%) | |
|
| ||
| Method of diagnosis | ||
|
| ||
| Biopsy only | 14 (48%) | |
| Cone | 9 (31%) | |
| LEEP | 6 (21%) | |
|
| ||
| Cone/LEEP margin | ||
|
| ||
| Positive | 13 (45%) | |
| Negative | 2 (7%) | |
| N/A | 14 (48%) | |
|
| ||
| LVSI | ||
|
| ||
| Positive | 8 (28%) | |
| Negative | 7 (24%) | |
| N/A | 14 (48%) | |
|
| ||
| Size of tumor | ||
|
| ||
| 2 – 2.9 cm | 15 (52%) | |
| 3 – 4 cm | 14 (48%) | |
Based on the International Federation of Gynecology and Obstetrics (FIGO) clinical staging system, all 29 patients had IB1 disease. To confirm no clinical evidence of disease spread, all patients had assessment with PET/CT or MRI preoperatively, in addition to physical exam. In the preoperative (LEEP/cone or cervical biopsy) tumor specimens lymph vascular space invasion was present in 53% and specimen margins were positive in 87%. Tumor histology was consistent with squamous (45%), adenosquamous (14%), and adenocarcinoma (41%).
A median of 26 lymph nodes (range, 7–57) were removed. Eleven (38%) patients had paraaortic lymph node sampling (0–11 nodes). Twenty-three (79%) patients had sentinel lymph node mapping. In all, 45% of patients had positive nodes. Three patients had benign assessment of lymph nodes at the time of frozen section but microscopic metastatic disease identified through sentinel lymph node ultrastaging. One patient had 4 positive nodes, 1 had 3 positive nodes, 6 had 2 positive nodes, and 5 had 1 positive node. All positive nodes were pelvic nodes. All patients with benign intraoperative lymph node assessment (n=22) had frozen section of the trachelectomy endocervical margin and curettage of the uterine fundus to determine whether to remove the fundus. Fifteen (68%) had negative uterine endocervical margins and curettage; 7 (32%) had positive lower uterine endocervical margins or positive curettage leading to immediate completion hysterectomy. At the time of radical trachelectomy, 2 (7%) patients had no residual cancer identified in the cervix.
Following intraoperative assessment for the extent of disease, 15 (52%) patients underwent radical trachelectomy and 13 (45%) radical hysterectomy. The reasons for radical hysterectomy were positive lower uterine margins (24%) and positive nodes (21%). One patient with a 3–4 cm tumor had bilateral positive nodes (common iliac and external iliac) identified on frozen-section. The decision was made to abort the procedure and treat with chemoradiation. Among the 15 patients who underwent radical trachelectomy, 6 required postoperative chemoradiation: 4 (27%) for positive nodes on final pathology and 2 (13%) for intermediate risk criteria (Sedlis criteria of LVSI, tumor diameter, and deep stromal invasion). In summary, 1 (3%) patient received definitive chemoradiation, 6 (21%) patients underwent radical trachelectomy followed by chemoradiation, 9 (31%) patients were treated with radical hysterectomy and chemoradiation, and 4 (14%) required radical hysterectomy alone. Thus, 9 of 29 (31%) patients underwent a successful radical trachelectomy and preserved the uterine fundus and the possibility of future pregnancy [Table 2].
Table 2.
Procedure details
| Surgical procedure | |
|
| |
| Radical Trachelectomy | 15 (52%) |
| Radical Hysterectomy | 13 (45%) |
| Aborted procedure | 1 (3%) |
|
| |
| Surgical approch | |
|
| |
| Abdominal | 22 (76%) |
| Vaginal | 6 (21%) |
| Robotic | 1 (3%) |
|
| |
| Median # lymph nodes removed | 26 (range 7–57) |
|
| |
| Paraaortic lymph nodes sampled | |
|
| |
| Yes | 11 (38%) |
| No | 18 (62%) |
|
| |
| Sentinel lymph nodes sampled | |
|
| |
| Yes | 23 (79%) |
| No | 6 (21%) |
|
| |
| Number of positive Nodes | |
|
| |
| 0 | 16 (55%) |
| 1 | 5 (17%) |
| 2 | 6 (21%) |
| 3 | 1 (3%) |
| 4 | 1 (3%) |
|
| |
| Residual cancer on final pathology | |
|
| |
| Yes | 27 (93%) |
| No | 2 (7%) |
|
| |
| Frozen section results | |
|
| |
| Positive Endocervical Margin | 7 (24%) |
| Positive Node | 8 (28%) |
|
| |
| Indication for chemoradiation | |
|
| |
| Positive Margin | 3 (10%) |
| Positive Node | 13 (45%) |
| Recurrence | 1 (3%) |
| None | 12 (41%) |
|
| |
| Summary of primary treatment | |
|
| |
| Trachelectomy | 9 (31%) |
| Trachelectomy, Chemoradiation | 6 (21%) |
| Hysterectomy | 4 (14%) |
| Hysterectomy, Chemoradiation | 9 (31%) |
| Definitive chemoradiation | 1 (3%) |
|
| |
| Disease Status | |
|
| |
| NED | 28 (97%) |
| Alive with disease | 1 (3%) |
Median follow-up was 44 months (range, 1–90 months). There was 1 (3%) recurrence. In this case, a 22-year old patient was found on office exam to have an exophytic 3 cm cervical mass that on biopsy was a moderately differentiated squamous cell carcinoma. She underwent a robotically assisted radical trachelectomy with pelvic lymph node dissection (23 negative nodes). Final pathology demonstrated a 2.8 × 2.2cm tumor, no LVSI, stromal invasion of 6mm out of 18mm (33%), and negative uterine margins of at least 1 cm. The patient received no further treatment. She was diagnosed with a recurrence 9 months later in the right adnexa, iliac nodes and peritoneum. She is currently receiving treatment 18 months following the radical trachelectomy.
Of the 9 patients who preserved fertility, only two have tried to conceive. Both are actively seeking the assistance of a reproductive endocrinologist and final outcomes are pending. One patient experienced an unintended pregnancy and underwent a first trimester termination.
Discussion
Fertility-sparing radical trachelectomy was a revolutionary procedure when it was first introduced. This procedure now allows patients to both survive their cancer and preserve the uterus for future childbearing. Originally, it was approached as a vaginal procedure with laparoscopic assessment of the nodal basins (Dargent operation). This approach is comparable to a type B, or modified radical hysterectomy, with a more limited resection of the parametria. Many surgeons therefore limited the use of this approach to patients with smaller (<2 cm) tumors due to the concerns over oncologic outcomes. Abdominal radical trachelectomy recently has been gaining more acceptance as a procedure with satisfactory oncologic and fertility outcomes. The abdominal approach permits a wider, nerve-sparing resection of the parametria consistent with a type C1 resection and, therefore, the potential to resect larger tumors. Thus, it has become necessary to determine whether the capability to perform the procedure for larger tumors is also met with an oncologic outcome equivalent to that of the radical abdominal hysterectomy or definitive chemoradiation. The data presented in this publication demonstrate that patients with stage IB1 tumors measuring 2–4 cm and with favorable histology (squamous cell carcinoma, adenosquamous or adenocarcinoma) are acceptable candidates for attempt at radical trachelectomy.
The population in this series is remarkably high-risk in comparison to the majority of stage I cervical cancer patients. Ninety-three percent of patients had residual carcinoma in the cervix (compared to nearly 50% in prior series), pelvic nodal metastases were seen in 45% of cases (compared to 10–20% commonly reported in other trachelectomy series), and final pathology findings required hysterectomy in 45% of patients and chemoradiation in 55%. All of these characteristics are reflective of high-risk lesions. Despite the high-risk nature of this cohort, 31% of all-comers had treatment which preserved the uterus for future childbearing. Our data may be interpreted in more than one way. First, the relatively low rate of successful fertility preservation serves as proof the procedure should not be offered to women with tumors 2cm or greater in size. The focus of this interpretation is frequency of fertility preservation and not on a key outcome: oncologic safety. Alternatively, the preservation of oncologic outcomes demonstrates the safety of offering women with 2–4 cm tumors the option of radical trachelectomy. These patients must be clearly informed of all the possibilities if they are to consider an attempt at fertility preservation. Given the preservation of oncologic outcomes for the 31% of women who are able to maintain the potential for future childbearing, we feel that it is quite reasonable to consider radical trachelectomy in these cases. We are continuing to investigate and refine our preoperative imaging strategies, such as pelvic MRI, to better estimate cervical tumor burden, lower uterine segment involvement, and deep stromal invasion so as to provide improved preoperative assessment of eligibility for trachelectomy.
The reported recurrence rates for patients with tumors 2cm or larger in size vary tremendously ranging from 0% to 38% (4, 5, 9–11,16–22). The disparate recurrence rates could be attributed to: differences in patient population, surgical approach (vaginal versus abdominal), utilization of intraoperative frozen section, and frequency of postoperative therapy. A basic summary of key publications on the topic estimates recurrence rates with a vaginal approach at 16% and with an abdominal approach of 9% [Table 3]. The frequency of parametrial nodes identified in pathology specimens reflects the extent of the resection margins obtained with vaginal and abdominal radical trachelectomy. In a previously published cohort, 7% of vaginal radical trachelectomies specimens contained parametrial nodes (23). We identified parametrial nodes in 40% of the abdominal radical trachelectomies cases included here. There is emerging literature on the use of the robotic platform in the treatment of cervical cancers. The available literature on robotic radical hysterectomy primarily focuses on feasibility and immediate surgical complications, and less on long-term oncologic outcomes (24–29). Nick and colleagues reported their outcomes comparing robotic radical trachelectomy to abdominal radical trachelectomy among 12 patients who underwent robotic radical trachelectomy and 25 patients who underwent open radical trachelectomy (30). At a median followup of 17 months there were no recurrences, a reassuring result. Their cases appeared to be well selected to be at low risk for recurrence, 58% were stage IA1 with LVSI or IA2, and only 42% had residual carcinoma identified in the trachelectomy specimen.
Table 3.
Recurrence following radical trachelectomy for tumors 2 centimeters or greater: Summary of key prior publications.
| Author | Number of Patients | Surgical Approach | Recurrence (%) |
|---|---|---|---|
| Pahisa | 4 | vaginal | 1 (25) |
| Lanowska | 6 | vaginal | 1 (17) |
| Chen | 7 | vaginal | 0 (0) |
| Covens | 8 | vaginal | 1 (13) |
| Plante | 19 | vaginal | 3 (16) |
| Marchiole | 27 | vaginal | 6 (22) |
| Ungar | 4 | abdominal | 0 (0) |
| Nishio | 13 | abdominal | 5 (38) |
| Li | 14 | abdominal | 0 (0) |
| Cibula | 6 | abdominal | 0 (0) |
| Karateke | 5 | abdominal | 0 (0) |
| Saso | 5 | abdominal | 1 (20) |
| Current series | 29 | mix | 1 (3) |
| Vaginal approach | 77 | vaginal | 12 (16) |
| Abdominal approach | 69 | abdominal | 6 (9) |
| Total | 147 | *** | 19 (13) |
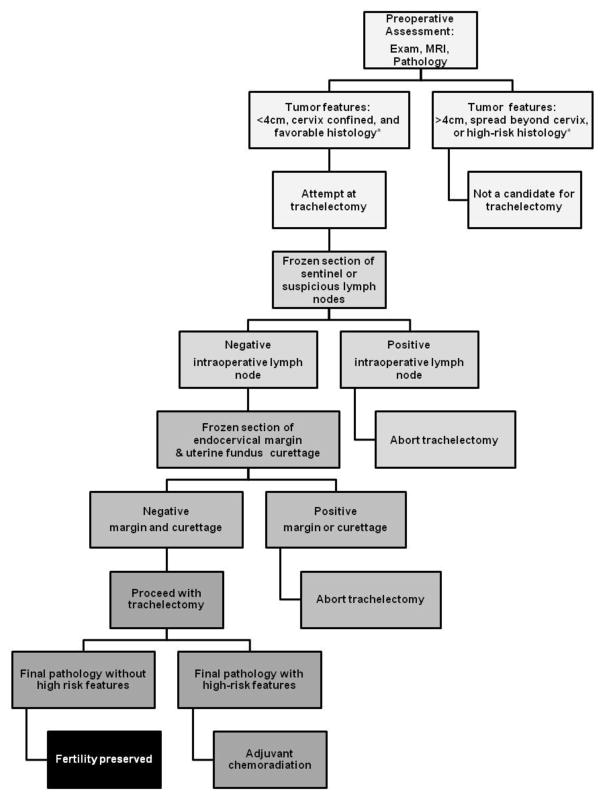
Preservation of oncologic outcome following trachelectomy is highly dependent on strict adherence to an assessment algorithm [Figure 1]. Counseling of patients with 2–4cm tumors must include information on the high likelihood (69%) of finding metastatic or high-risk disease, which would require radical hysterectomy and/or chemoradiation, as well the potential for pregnancy complications if fertility is successfully preserved. The radical trachelectomy algorithm should include preoperative assessment with imaging (MRI or PET), pathology confirmation of low-risk histology, and reproductive endocrinology consultation to discuss alternative options, such as surrogacy. For women with tumors 2–4 cm in size, squamous, adenocarcinoma, or adenosquamous histology, and a strong desire to maintain fertility, attempt at radical trachelectomy is a reasonable option. Intraoperative procedures should include frozen section of suspicious pelvic lymph nodes (complete lymphadenectomy or sentinel lymph node mapping), a shaved endocervical margin, and endometrial curettage. In the event that any of the frozen section specimens is positive for carcinoma, radical trachelectomy should not be performed. Patients with high-risk features should be counseled regarding treatment options once complete pathologic information is available.
Figure 1.
Protocol for attempt at radical trachelectomy
*High-risk histology includes adenoma malignum and neuroendocrine tumors.
Acceptance of radical trachelectomy as an appropriate standard of care for patients with cervical cancer who wish to preserve fertility has been achieved with the inclusion of this procedure in the National Comprehensive Cancer Network guidelines. Continued investigation is needed to further refine the indications and the best surgical approaches. Our data demonstrate that oncologic outcomes appear to be maintained for patients with 2–4 cm tumors. The role of neoadjuvant chemotherapy in these patients to improve long-term outcomes or to extend the possibility of fertility preservation to an increased number of patients is of great interest and merits further investigation. Obstetrical outcomes for patients with stage IB1, 2–4 cm lesions who undergo a successful trachelectomy will also require long-term follow-up data.
Footnotes
There are no funding disclosures.
References
- 1.Aburel E. Proceedings: Extended abdominal exstirpation of cervix and isthmus in early stages of cervix carcinoma (carcinoma in situ and microcarcinoma) Archiv fur Gynakologie. 1973;214:106–8. doi: 10.1007/BF00671074. [DOI] [PubMed] [Google Scholar]
- 2.Dargent D, Mathevet P. Schauta’s vaginal hysterectomy combined with laparoscopic lymphadenectomy. Bailliere’s clinical obstetrics and gynaecology. 1995;9:691–705. doi: 10.1016/s0950-3552(05)80392-x. [DOI] [PubMed] [Google Scholar]
- 3.Rob L, Skapa P, Robova H. Fertility-sparing surgery in patients with cervical cancer. Lancet Oncology. 2011;12:192–200. doi: 10.1016/S1470-2045(10)70084-X. [DOI] [PubMed] [Google Scholar]
- 4.Marchiole P, Benchaib M, Buenerd A, Lazlo E, Dargent D, Mathevet P. Oncological safety of laparoscopic-assisted vaginal radical trachelectomy (LARVT or Dargent’s operation): a comparative study with laparoscopic-assisted vaginal radical hysterectomy (LARVH) Gynecol Oncol. 2007;106:132–41. doi: 10.1016/j.ygyno.2007.03.009. [DOI] [PubMed] [Google Scholar]
- 5.Plante M, Gregoire J, Renaud MC, Roy M. The vaginal radical trachelectomy: an update of a series of 125 cases and 106 pregnancies. Gynecol Oncol. 2011;121:290–7. doi: 10.1016/j.ygyno.2010.12.345. [DOI] [PubMed] [Google Scholar]
- 6.Diaz JP, Sonoda Y, Leitao MM, et al. Oncologic outcome of fertility-sparing radical trachelectomy versus radical hysterectomy for stage IB1 cervical carcinoma. Gynecol Oncol. 2008;111:255–60. doi: 10.1016/j.ygyno.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 7.Einstein MH, Park KJ, Sonoda Y, et al. Radical vaginal versus abdominal trachelectomy for stage IB1 cervical cancer: a comparison of surgical and pathologic outcomes. Gynecol Oncol. 2009;112:73–7. doi: 10.1016/j.ygyno.2008.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pareja FR, Ramirez PT, Borrero FM, Angel CG. Abdominal radical trachelectomy for invasive cervical cancer: a case series and literature review. Gynecol Oncol. 2008;111:555–60. doi: 10.1016/j.ygyno.2008.07.019. [DOI] [PubMed] [Google Scholar]
- 9.Cibula D, Slama J, Svarovsky J, et al. Abdominal radical trachelectomy in fertility-sparing treatment of early-stage cervical cancer. Int J Gynecol Cancer. 2009;19:1407–11. doi: 10.1111/IGC.0b013e3181b9549a. [DOI] [PubMed] [Google Scholar]
- 10.Karateke A, Kabaca C. Radical abdominal trachelectomy is a safe and fertility preserving option for women with early stage cervical cancer. Eur J Gynaecol Oncol. 2012;33:200–3. [PubMed] [Google Scholar]
- 11.Saso S, Ghaem-Maghami S, Chatterjee J, et al. Abdominal radical trachelectomy in West London. BJOG. 2012;119:187–93. doi: 10.1111/j.1471-0528.2011.03213.x. [DOI] [PubMed] [Google Scholar]
- 12.Wethington SL, Cibula D, Duska LR, et al. An international series on abdominal radical trachelectomy: 101 patients and 28 pregnancies. Int J Gynecol Cancer. 2012;22:1251–7. doi: 10.1097/IGC.0b013e318263eee2. [DOI] [PubMed] [Google Scholar]
- 13.Abu-Rustum NR, Sonoda Y, Black D, Levine DA, Chi DS, Barakat RR. Fertility-sparing radical abdominal trachelectomy for cervical carcinoma: technique and review of the literature. Gynecol Oncol. 2006;103:807–13. doi: 10.1016/j.ygyno.2006.05.044. [DOI] [PubMed] [Google Scholar]
- 14.Abu-Rustum NR, Sonoda Y. Fertility-sparing radical abdominal trachelectomy for cervical carcinoma. Gynecol Oncol. 2007;104:56–9. doi: 10.1016/j.ygyno.2006.10.036. [DOI] [PubMed] [Google Scholar]
- 15.Sonoda Y, Abu-Rustum NR. Radical vaginal trachelectomy and laparoscopic pelvic lymphadenectomy for early-stage cervical cancer in patients who desire to preserve fertility. Gynecol Oncol. 2007;104:50–5. doi: 10.1016/j.ygyno.2006.10.035. [DOI] [PubMed] [Google Scholar]
- 16.Ungar L, Palfalvi L, Hogg R, et al. Abdominal radical trachelectomy: a fertility-preserving option for women with early cervical cancer. BJOG. 2005;112:366–9. doi: 10.1111/j.1471-0528.2004.00421.x. [DOI] [PubMed] [Google Scholar]
- 17.Nishio H, Fujii T, Kameyama K, et al. Abdominal radical trachelectomy as a fertility-sparing procedure in women with early-stage cervical cancer in a series of 61 women. Gynecol Oncol. 2009;115:51–5. doi: 10.1016/j.ygyno.2009.06.036. [DOI] [PubMed] [Google Scholar]
- 18.Li J, Li Z, Wang H, et al. Radical abdominal trachelectomy for cervical malignancies: surgical, oncological and fertility outcomes in 62 patients. Gynecol Oncol. 2011;121:565–70. doi: 10.1016/j.ygyno.2011.01.032. [DOI] [PubMed] [Google Scholar]
- 19.Pahisa J, Alonso I, Torne A. Vaginal approaches to fertility-sparing surgery in invasive cervical cancer. Gynecol Oncol. 2008;110:S29–32. doi: 10.1016/j.ygyno.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 20.Lanowska M, Mangler M, Spek A, et al. Radical vaginal Trachelectomy (RVT) combined with laparoscopic lymphadenectomy: prospective study of 225 patients with early-stage cervical cancer. Int J Gynecol Cancer. 2011;21:1458–64. doi: 10.1097/IGC.0b013e3182216aa7. [DOI] [PubMed] [Google Scholar]
- 21.Chen Y, Xu H, Zhang Q, Li Y, Wang D, Liang Z. A fertility-preserving option in early cervical carcinoma: laparoscopy-assisted vaginal radical trachelectomy and pelvic lymphadenectomy. Eur J Obstet Gynecol Reprod Biol. 2008;136:90–3. doi: 10.1016/j.ejogrb.2006.10.014. [DOI] [PubMed] [Google Scholar]
- 22.Beiner ME, Covens A. Surgery insight: radical vaginal trachelectomy as a method of fertility preservation for cervical cancer. Nat Clin Practi Oncol. 2007;4:353–61. doi: 10.1038/ncponc0822. [DOI] [PubMed] [Google Scholar]
- 23.Lanowska M, Morawietz L, Sikora A, et al. Prevalence of lymph nodes in the parametrium of radical vaginal trachelectomy (RVT) specimen. Gynecol Oncol. 2011;121:298–302. doi: 10.1016/j.ygyno.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 24.Cantrell LA, Mendivil A, Gehrig PA, Boggess JF. Survival outcomes for women undergoing type III robotic radical hysterectomy for cervical cancer: a 3-year experience. Gynecol Oncol. 2010;117:260–5. doi: 10.1016/j.ygyno.2010.01.012. [DOI] [PubMed] [Google Scholar]
- 25.Estape R, Lambrou N, Diaz R, Estape E, Dunkin N, Rivera A. A case matched analysis of robotic radical hysterectomy with lymphadenectomy compared with laparoscopy and laparotomy. Gynecol Oncol. 2009;113:357–61. doi: 10.1016/j.ygyno.2009.03.009. [DOI] [PubMed] [Google Scholar]
- 26.Fanning J, Hojat R, Johnson J, Fenton B. Robotic radical hysterectomy. Minerva Ginecologica. 2009;61:53–5. [PubMed] [Google Scholar]
- 27.Maggioni A, Bocciolone L, Peiretti M, et al. Robotic modified radical hysterectomy with pelvic lymphadenectomy. E-cancer Medical Science. 2007;1:55. doi: 10.3332/ecancer.2008.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Magrina JF, Pawlina W, Kho RM, Magtibay PM. Robotic nerve-sparing radical hysterectomy: feasibility and technique. Gynecol Oncol. 2011;121:605–9. doi: 10.1016/j.ygyno.2011.02.034. [DOI] [PubMed] [Google Scholar]
- 29.Tinelli R, Malzoni M, Cosentino F, Perone C, Fusco A, Cicinelli E, et al. Robotics versus laparoscopic radical hysterectomy with lymphadenectomy in patients with early cervical cancer: a multicenter study. Ann Surg Oncol. 2011;18:2622–8. doi: 10.1245/s10434-011-1611-9. [DOI] [PubMed] [Google Scholar]
- 30.Nick AM, Frumovitz MM, Soliman PT, Schmeler KM, Ramirez PT. Fertility sparing surgery for treatment of early-stage cervical cancer: open vs robotic radical trachelectomy. Gynecol Oncol. 2012;124:276–80. doi: 10.1016/j.ygyno.2011.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]