Abstract
Patients going home after a hospitalization face many challenges. This transition period exposes patients to unnecessary risks related to inadequate preparation prior to leaving the hospital, potentially leading to errors and patient harm. Although patients engaging in self-management have better health outcomes and increased self-efficacy, little is known about the processes in place to support and develop these skills for patients leaving the hospital. Through qualitative interviews and observations of 28 patients during and after their hospitalizations, we explore the challenges they face transitioning from hospital care to self-management. We identify three key elements in this process: knowledge, resources, and self-efficacy. We describe how both system and individual factors contribute to breakdowns leading to ineffective patient management. This work expands our understanding of the unique challenges faced by patients during this difficult transition and uncovers important design opportunities for supporting crucial yet unmet patient needs.
Author Keywords: Health informatics, pediatric, hospital, medical informatics, self-efficacy, self-management, discharge
ACM Classification Keywords: J.3 Life and Medical Sciences, Health, Medical Information Systems, H.5.m. Information interfaces and presentation
INTRODUCTION
Hospitals provide acute management for both new and chronic medical conditions with the goal of treating and stabilizing patients so they can return to their life outside the hospital. However, patients face many risks and challenges after leaving the hospital. Re-hospitalization, one such risk, has been identified as a major issue within the United States health care system, impacting 1 out of 5 Medicare beneficiaries, leading to $17.4 billion each year in unnecessary spending [35]. Although some hospital readmissions are unavoidable, many are preventable and result from inadequate patient preparation prior to leaving the hospital (i.e. discharge) [11]. Discharge planning, a common component of many health care systems, allows for the development of individualized plans provided to a patient prior to leaving the hospital, with the goal of improving patient outcomes and reducing unnecessary re-hospitalizations. Yet, it has had mixed results [53]. Key remaining challenges include patients having a poor understanding of their medical condition or low health literacy in general [2,34] as well as patients not being able to access the health resources they need after discharge [37,39].
June, a 16-year-old competitive soccer player, recently returned home from a three-day hospitalization after being newly diagnosed with Type 1 diabetes. In addition to receiving the medical care necessary to treat and manage her new condition, hospital staff also provided intensive education designed to teach June and her family about what diabetes is and how to manage this chronic condition. Eager to leave the hospital and return to a normal life, June and her family felt empowered with their newly acquired knowledge, confident that they had the tools to face whatever challenges lay ahead. However, their feelings of confidence quickly transitioned to feeling overwhelmed and unprepared. Previously simple tasks for June, like grabbing a snack to bring to soccer practice, now required that she read food labels, count carbs, and plan insulin injections. Should she tell her coach or her teammates about her diabetes in case the disease caused her to get ill during an away game, even though she did not want any special treatment? What would she do if she did not have a place at school to take injections in private or to dispose of needles?
Once discharged, patients and their caregivers need to possess, or know how to obtain, the knowledge (e.g. including both technical/clinical facts as well as patient expertise [58]) and resources (enablers that help individuals manage their illness including social support, access to pharmacies, etc.) required to provide care at home, and respond appropriately to the routine as well as unfamiliar challenges, referred to as self-management [46]. As a result, patients like June (whose scenario is based on a teenaged patient from our study) face a number of challenges immediately after leaving the hospital.
Using human-computer interaction (HCI) methods to redesign technology for use after hospital discharge has the potential to bridge the resource and knowledge gaps faced by patients and caregivers. By designing better tools that consider the holistic needs of patients, clinicians can support patients through their transition to self-management. Although abundant research in HCI and Health Informatics has explored how to best support patients with chronic diseases [12,21,28], we have less understanding of how technology could support patients as they transition to life after an acute hospitalization.
To better understand how information technology could support patients and prepare them as they move from hospital to home, we conducted an interview and observation study with 28 hospitalized patients and their family caregivers, prior to and just after discharge. Through our analysis, we show that many challenges the patients face arise from deficiencies in three key areas: (1) medical Knowledge, (2) Resources to manage their health (including social support), or (3) Self-efficacy. We describe how these three key areas, referred to as the KRS framework, have the potential to help guide design opportunities for HCI and patient-centered information technology to support patients as they transition from hospital-based management to self-management. Based on multiple in-depth interviews, we describe the challenges faced by patients and their families during such a hospital to home transition. We explore how gaps in medical knowledge, in resources needed to care for one’s health, and in self-efficacy prevent effective self-management when patients leave the hospital setting. Finally, we outline design recommendations for technologies that could help address these unmet needs and ease the burden of this difficult and fragile transition for patients.
BACKGROUND AND RELATED WORK
With the increasing life expectancy of individuals around the world, the number living with a chronic condition has correspondingly increased [10]. This situation has led individuals to self manage and integrate their health conditions into their daily routine, through self-care [8]. Recently, researchers in the fields of HCI and CSCW have explored broadly how technology supports those living with a chronic illness and have provided suggestions on how to advance both research and design to support individuals living with a chronic illness [24,48].
Although low-tech solutions have shown benefit in reducing undesirable events after discharge (e.g. readmission or no follow-up with their primary physician) [4], they often did not assess the innate skills required for self-management at home.
Given that behavior change is a key component of self-management as individuals need to learn how to adapt their lifestyle as a result living with a chronic illness, Social Cognitive Theory [6] provides a useful lens to help understand and guide the patients’ actions post-discharge. SCT has been applied to health promotion interventions [5], and includes the key determinants of the KRS framework. However, SCT alone cannot account for all challenges and constraints faced by individuals self-managing their illness. Therefore, new frameworks are needed in order to understand and design for the needs of this unique population. In the sections that follow, we describe patients’ knowledge, resources, and self-efficacy in the context of clinical care and related work.
Knowledge
Traditionally, hospital staff take the primary role in managing patients during the course of a hospitalization. After discharge, patients and their caregivers must take over this management task. Staff try to prepare patients for this transition by providing the appropriate knowledge and resources to ensure a smooth and seamless transition. Interventions that provide patients with medical education at and beyond the time of discharge, facilitate access to needed resources, or support self-efficacy have been successful in improving patient health and quality of life and decreasing readmission rates [13,57,62]. However, not all interventions have been reliably successful, suggesting additional studies are needed to identify useful strategies to reduce readmissions [29].
Despite the education currently provided, patients continue to face many challenges after discharge from the hospital. It has been estimated that up to 20% of patients discharged from US hospitals suffer some type of adverse event leading to re-hospitalization within 90 days, one third of which are preventable [25]. Lack of knowledge is a key factor in these events related to: low health literacy [3,34], and a poor understanding of medication regimens [45]. These knowledge deficits lead to a gap in effective care after discharge.
Some have explored technological solutions to address these gaps in knowledge. For example, researchers have developed relational agents to act as a virtual nurse who helps disseminate information prior to discharge [64] or as a virtual pharmacist who helps detect and resolve issues that arise post-hospitalization [50]. The patients preferred receiving their virtual discharge nurse over their human nurse or doctor and expressed high levels of satisfaction with the virtual agent.
Resources
To successfully manage health and disease outside the hospital setting, patients must also have access to resources that support their transition to home care. Patients face many impediments needed to mange health outside the hospital setting. These impediments include inadequate social and family support [54], challenges with transportation and obtaining medication [40]. These barriers to resources can be particularly exacerbated among vulnerable populations. For example, children and adolescents are often dependent on their families and communities for health-related resources [15], and individuals of low socioeconomic status often lack resources to access health care or engage in healthy behaviors [9,36].
Self-efficacy
Self-efficacy refers to a person’s confidence in their ability to accomplish a specific goal [5,6,12]. Lorig and Holman describe that in addition to understanding and managing the medical components of illness, people need to manage their behaviors as well as the emotional sequelea and self-efficacy associated with their illness [43]. Although education programs focusing just on medical aspects of the disease are not sufficient to improve health outcomes in adults [27], those focusing on medical management, self-efficacy, and emotional support, the three tasks required for self-management, have demonstrated benefits in a variety of chronic conditions [44].
Goal setting, a key component of self-efficacy, also plays an important role in helping patients manage their illnesses. Bodenheimer and colleagues describe how these goals help with the creation of action plans, developed by patients through the use of problem solving skills [12]. The creation and successful completion of patient-derived action plans, (which take into account knowledge and resources), support self-efficacy, and provides patients with the confidence to manage their own illness. This results in increased motivation leading to self-management success. In addition, coaching has shown to be effective in enhancing self-management especially during times of transition [49].
Although self-directed goal formation is important for patients, patients often also turn to others with similar conditions for information as well as guidance and support in the goal-forming process. Peers help through informational [18], emotional [51], and instrumental forms of support [32]. With the explosion of online health communities there are many opportunities for individuals to obtain support beyond their immediate social network. Hartzler and colleagues describe how experienced patients do not serve as just “amateur doctors,” but rather offer valuable personal information that clinicians often cannot provide [30]. Patient expertise explores “strategies [used] for coping with day-to-day personal health issues gained through trial and error of the lived experience [30].” Integrating patient expertise and promoting social support resources in times of transition should therefore help inexperienced patients with finding and setting realistic goals.
With realistic goals, patients then require decision-making and problem solving skills to support goal attainment. These key skills of self-management require individuals to have access to, gather and interpret data (i.e. sensemaking). Mamykina and colleagues have proposed a sensemaking framework for chronic-disease self-management [46]. With patients in one of two modes based on the familiarity of an experience, they utilize different skills to navigate these experiences.
Recognizing the benefits of self-management, hospitals have an opportunity to integrate knowledge, facilitate access to resources, and support self-efficacy, to aid patients as they transition from hospital care to self care.
METHODS
Our work is part of a larger study, which was approved by the authors’ institutional review board and the participating hospitals, exploring how to increase patient engagement in preventing hospital-based errors. We conducted interviews and observations with 28 adult and pediatric (i.e. child and adolescent) patients and their caregivers hospitalized at two different hospitals in Seattle, Washington, United States. One is an adult hospital that serves local patients from various socioeconomic and ethnic backgrounds. The other is a children’s hospital that serves pediatric patients from urban and rural areas from various regional states. We chose these two sites because of the different challenges faced by adult and pediatric patients in the discharge process. While adult patients may have a caregiver assisting them post-discharge, pediatric patients almost always rely on the support of adult caregivers because of their minor status and may not be developmentally capable of caring for themselves. Thus pediatric patients are dependent on caregivers who have their own goals and needs to aid in the patients’ self-management. Therefore we sought to understand and include multiple populations to understand the range of complexities and associated with and similarities across self-care strategies.
Study Procedures
Patients were recruited over a four-month period between February 2015 and May 2015. For each patient, we conducted three semi-structured interview or observation sessions that occurred pre- and post-discharge. First, while the patient was in the hospital, the initial sessions with both patients and their caregivers lasted 40–60 minutes. Next we observed the patient while he/she was still in the hospital for 60–90 minutes. Typically, these interviews and observations occurred 1–2 days prior to the patient’s discharge. Finally, we carried out a follow-up phone interview within 1–2 weeks after the patient was discharged from the hospital. Follow-up interviews lasted up to 30 minutes and were guided and informed by the initial interviews and allowed us to determine if the patients’ needs and expectations were met after discharge.
In the interviews, participants (both patients and caregivers) were asked about their current hospital visit, exploring their experiences in providing and receiving information related to their care. The follow up interviews occurred shortly after discharge and followed up on items discussed and events that occurred after the first interview. All interviews were audio-recorded and transcribed prior to analysis.
We also conducted bedside observations with all the participants, typically after the initial interview. During the observation period, a member of the research team sat in the hospital room and took notes. We focused on discussions regarding the patient’s care, communications between patients, caregivers, and providers, and finally the use of technology or other information artifacts in the room.
Study Sites
Our study took place at one adult and one pediatric hospital in a large urban area, Seattle, WA, in the United States. Each hospital serves as a tertiary referral center for a large geographic region. The adult hospital admits over 16,000 patients each year, and the pediatric hospital admits over 15,000 patients each year. Patients at the adult hospital have similar demographics with the local area’s population, and two-thirds of the patients are covered by private insurance. The pediatric hospital has a slightly more diverse patient population then the surrounding area, and less than half have private insurance.
Participants
Due to our site selection and sampling methods we had the opportunity to recruit patients with a wide variety of ages and medical conditions. This allowed us to see whether themes were common across age and medical condition. We recruited a total of 48 people to participate: 28 patients and 20 caregivers across both sites. Our methodology utilized a purposeful sampling framework focusing on age, gender, ethnicity, medical service, and disease complexity. Research coordinators employed by each hospital recruited and consented participants on behalf of the research team.
Patient participants had diverse reasons for being in the hospital, which represented varying levels of complexity and medical needs. Fifty percent of the patients, were in the hospital on the surgical service after undergoing different procedures such as a heart or kidney transplant, hip repair, gall stone removal, cleft lip repair, and infection drainage. The other 50% of patients were cared for on medical teams for problems such as a blood infection, diabetes, Chron’s disease, chronic obstructive pulmonary disease, kidney failure, pneumonia, and heart disease. Otherwise, patients were equally divided in the following categories: pediatric vs adult, chronic vs. non-chronic conditions, and male vs. female. Though, of the 28 patients, 20 had previously been hospitalized for some reason that could have been related to the current condition for which they were receiving care. Patients’ ages ranged between 7 and 76. In the pediatric hospital (14 patients), half of the patients were age 7–13 years and half age 13–17 years. In the adult hospital (14 patients), patients were evenly split between ages 18–39, 40–59, and 60–76 years. Patients were more ethnically diverse than the American population: 18 were White/Caucasian, 6 Black/African American, 3 Hispanic, 2 Asian, and 1 American Indian/Alaska Native. Adult patients had a range of educational levels, with most having had at least some college.
In addition, we enrolled 20 caregivers who were present when patients were recruited. Half were 18–39 and the other half were 40–59. Caregivers were predominantly female, especially at the pediatric hospital. Of the 20 caregivers that participated, 16 were parents of pediatric patients and 4 were caregivers of adult patients.
Analysis
Throughout the interviews and observations, the research team met regularly to discuss preliminary findings and identify themes in the data to identify the gaps associated with discharge preparation. Transcripts were reviewed and coded by three members of the research team using AtlasTi. Initial coding was developed through an iterative process and not guided by a theory or framework identified a priori.
FINDINGS
Throughout our analysis, it became clear that the challenges patients experienced during their time of transition to self-management related to three areas: Knowledge, Resources, and Self-efficacy (KRS). Below we show how the KRS areas frame two key themes: (1) Gaps in System-based Self-Management support and (2) Elements of individual self-management. Gaps in system-based self-management support relate to the importance of hospital-based practices in supporting individuals as they transition from hospital management to self-management. Elements of individual self-management relate to the various states of individuals in their journey towards effective self-management. Below we describe findings by theme and provide quotations to illustrate each theme. We identify participants with a code: The first letter indicates the site as adult (A) or pediatric (P), the second letter designates patient (P) or caregiver (C), and the number is a unique identification provided by the research team.
Gaps in System-based Self-Management Support
Despite the large amounts of knowledge patients gain during a hospitalization, many patients are still unprepared to successfully self-manage their illness at home. This finding was present in both adult and pediatric populations and across different medical conditions. The gap between hospital management and self-management is related to three key factors: (1) most information transferred to patients occurs verbally, which makes it difficult for patients to process and remember, (2) patients lack the necessary patient expertise to adequately integrate the knowledge back into their lives, and (3) patients and caregivers often have low self-efficacy, preventing them from accomplishing specific tasks. Although the later two items are individual in nature, we identify how all three factors relate back to fundamental system failures.
Challenges with verbal information transfer
Although most hospitals utilize electronic health records (EHR) to document, order, and organize the care provided to patients in the hospital, these systems support the information needs of clinicians rather than patients. Despite the fact that patients are legally entitled to their medical information contained within the EHR, most hospitals do not provide easy or timely access [33,47]. Instead, patients obtain most of their results and the reasoning behind the care they receive verbally from nurses and physicians. However, without a concrete record for patients to refer to, their ability to retain it for future use is called into question. Not to mention the overwhelming volume of information presented over the course of a hospitalization:
I didn’t understand and they were talking so fast and I didn’t know what was important and what wasn’t. Like I wasn’t able to tell my family what was going on because there was just so much information. (PC04)
In addition to the lack of tangible information available to patients after a verbal exchange, another important barrier relates to the physical and mental state of patients while in the hospital. Often patients are not capable of interacting with the medical team in a way conducive to effective information transfer.
I really was out of it, I was not the best advocate for myself while I was there, because I was at such diminished capacity that I wasn’t advocating for myself like I normally would when I’m in my normal state. (AP06)
Despite the strong efforts of hospitals to educate their patients in preparation for discharge, patients continue to have large gaps in the information or knowledge needed to support them in self-management due to communication challenges stemming from a lack of understanding of complex medical information and being unprepared or unable to process this information.
Lack of patient expertise
Although some discharge information provides a basic framework for re-introduction into life outside of the hospital, many patients are not completely prepared for this transition. Because patient-expertise requires some degree of trial and error through real experiences, it is not surprising that patients are unprepared after discharge. In the controlled setting of the hospital, patients are not exposed to the variety or spontaneity of interactions they are likely to experience once they leave the hospital.
I mean for her, she’s like “Am I still going to be able to do my sport?” Even though they keep saying that, she won’t believe it until she does. (PC06)
So I felt like I was prepared to take care of him, it was just a matter of taking care of him in our environment that we were going to. That I wasn’t sure about - and am still not sure, we’re still figuring it out. (PC04)
However, for many, discovering a lack of expertise only occurs after getting back home. Often, the lack of expertise relates to the ability to track important metrics or parameters required for self-management.
If I can’t keep track, I forgot and then usually I need my parents to help me keep track of some things, because if I don’t keep track of it I lose information. (PP05)
When patients lack expertise they feel overwhelmed or helpless, and not knowing where to turn for help. In this situation patients clearly lack both knowledge and self-efficacy to manager their illness.
Sometimes she’ll get sad or she’ll feel like she’s alone. (PC14)
Fortunately, instead of taking the time to develop their own expertise, patients turn to others for help. Although many have discussed the importance of online patient communities [18,26,52] as well as in-person patient support groups [32] that support the needs of patients with a chronic illness, little is known about how a resource of peer expertise might help people in the hospital prepare for self management. Nonetheless, we found that patients are clearly interested in such a resource.
We haven’t [found any other families who need to deal with the same condition]. It’s something I would definitely like to do - being that we live in a smaller area, our options are pretty small. (PC14)
Although we know that patient expertise does exist in the hospital, the ability for non expert patients to obtain this form of support from those more experienced while in the hospital is constrained because of privacy concerns or physical constraints related to an illness.
Due to gaps in knowledge, specifically understanding how to integrate their illness into their daily routines after leaving the hospital, as well as poor self-efficacy, patients clearly lack the expertise or confidence necessary to engage in self-management before leaving the hospital.
Low self-efficacy
Many patients feel completely overwhelmed by their illness, and this feeling leads to the inability to effectively self-manage.
It’s been overwhelming, one day at a time. Just trying to - I mean it’s just reorganization of your entire life. (PC06)
However, providing patients and their caregivers with simple support tools, allows them to escape the cycle of despair and hopelessness. Support can come in the form of informational, emotional, or instrumental (i.e. providing additional resources) [32].
When I’m really, really worried, I get really stressed out and no one helps me, and I overstress and I get just - but when someone helps me, I stop stressing (PC05)
Although hospital-based systems provide significant and diverse forms of support to patients in the hospital, this support does not adequately prepare all patients for successful self-management after leaving the hospital. We identified specific challenges in ensuring that patients have the necessary knowledge, resources, and self-efficacy to support successful self management. However, ensuring patients have the emotional and physical support throughout their hospitalization, should help foster self-efficacy earlier which in turn should help facilitate knowledge acquisition and ultimately the development of patient expertise easing the transition to self-management.
Elements of Individual Self-Management
We found that both adult and pediatric patients and their caregivers discussed knowledge, resources, and self-efficacy as important issues to support self-management. Based on these findings, we developed the Knowledge, Resources, and Self-efficacy (KRS) Framework of Hospital Discharge to describe how these elements intersect to support self-management (Figure 1). We propose this framework because while SCT includes these concepts, it may be limited in the hospital setting where sociocultural influences may be constrained. Also, individuals have less control over their health because they may not (1) be physically or mentally capable of engaging in or have control of their care or (2) have access to key knowledge or resources because of clinician- and system-level issues.
Figure 1.
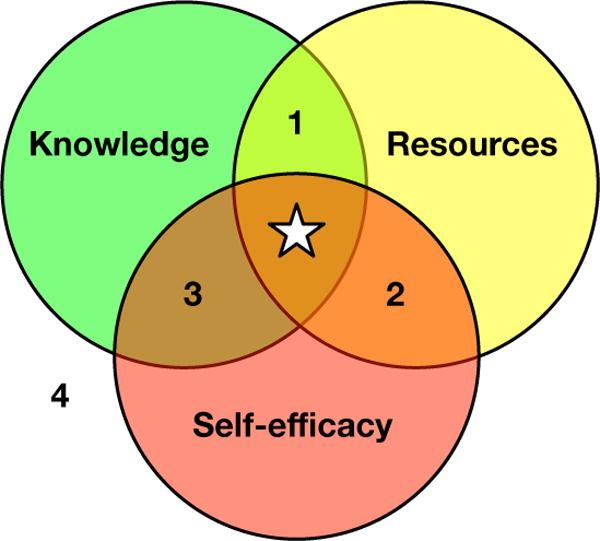
The Knowledge, Resources, and Self-efficacy (KRS) Framework of Hospital Discharge. Self-management (star). When lacking the complete set, patients may posses a combination of elements (1–3), a single element (knowledge, resources, or self-efficacy), or no elements (4).
In reality, patients might have two, one, or none of the elements, which can hamper efforts to engage in self-management. We will describe each of the combinations of knowledge, resources, and self-efficacy and illustrate them using quotes from the study.
Knowledge only
Patients could have only knowledge without resources or self-efficacy. This situation is seen often in current hospital discharge practice in which patients are provided information about medications, future appointments, and the plan for managing their health. However, hospital staff do not (1) assess which resources patients have or (2) provide time for patients to learn and practice skills that are needed to carry out the plans.
We saw an example of this in an adult patient (AP02). He had been admitted for Chronic Obstructive Pulmonary Disease (COPD). Although he had been living with the disease before being admitted and knew what medications he needed to take. However, due to financial reasons he had to stop taking the medication, which exacerbated his symptoms and lead to being admitted to the hospital.
I was off for a couple of weeks for financial reasons why I didn’t get it refilled and stuff…My condition just became deteriorated. I had trouble breathing and I was real fatigued all the time, and that brought me here.
He also stated that previously he did not have the motivation to adequately care for his health, including proper use of the oxygen tank he had been prescribed. While he had always cared for himself, he did not have the motivation to listen and learn from the clinicians on how to best manage his health. Ultimately, he appeared to be gaining motivation to support the full development of self-efficacy.
I was just really ready to listen to what they were telling me because I knew there was something that was out of my control, something that I needed to let somebody else take care of and listen to what they were saying … this was my health, because I didn’t like the way I was feeling. So I was ready to listen … I kind of felt it was time to, like they say, put the cotton in your mouth and open the ears, because I’ve always taken care of myself, and listen to myself, and make my own decisions based on myself. I never – but I thought it was time to listen to others.
Resources only
Some patients have resources but not knowledge or self-efficacy. These patients have access to social and physical resources (e.g., family caregivers, access to health insurance and a pharmacy to obtain medication). However, the hospital staff did not provide them all the information needed to successfully manage their care because the information was not tailored to their individual needs. Often, the materials that hospital staff utilize are created for a general population, such as exercise and diet pamphlets that do not take into account cultural dimensions. Also, the patients do not have the confidence to perform new tasks because they did not have the opportunity to be taught and practice the skills under the guidance of health professionals at the hospital.
PC04 provides an example of having only resources. The pediatric patient and his caregiver had access to the medications that the pediatric patient needed post-discharge. However, the caregiver did not have the information and skills needed to prepare the medication properly.
… they kept preparing me for the fact that this [medication] would have to be given a certain way until he starts eating and then we can sprinkle it. It’s a tab that has the little sprinkles inside of it. Well, when I went to the pharmacy to get his medications, they didn’t give me that version of it. They gave me a like a horse pill that I have to crush, and so they spent so much time preparing me for one thing and then I got a completely different version of the medication … I kind of wish I would have gotten the medication maybe a couple of days before discharge, so I could have done them in the hospital, like with the nurses, just so I would have had a better idea of that. Because that first night it took me about two hours to do his medications.
Self-efficacy only
Patients with only self-efficacy represent few patients at discharge but could still exist and be impacted by the current discharge practices. These patients have the confidence to manage their health but lack the knowledge and resources to carry out self-management. AP13 provides an illustration of self-efficacy only. She had been living with Crohn’s Disease for over 10 years so she had the skills and confidence on how to manage her health. However, she had been admitted to the hospital for a new kidney condition.
It’s kind of a habit I’ve cultivated over the last 13 years with Crohn’s, I make sure I have everything – everybody’s questions in a row and I get them all answered … I’m kind of used to all my research being about guts and stuff, and all of a sudden I’ve got kidneys to deal with…
She didn’t posses the knowledge about this new condition because the clinicians did not know what was causing the problem and the patient did not know much about kidney disease. Also, she was having problems accessing adequate medical care where she lived.
Trying to get information from here to [Medical clinic] and [Medical clinic] to here, because my insurance company wanted me to have my primary a little closer to home, but I think that’s just not going to be a workable thing. We’re going to have to figure something out.
Knowledge and Resources (Figure 1, area 1)
The patients who would benefit the most from a restructuring of hospital discharge are patients who have knowledge and resources, even though they lack self-efficacy. These patients have an understanding of their disease and its management and have the resources to mange their health; however, they are in need of motivation or confidence in their ability to manage their health.
Pediatric participant PP09 is an example of someone who has knowledge and resources but lacks self-efficacy. The hospital provided the parent with information about post-discharge care. The pediatric patient also had social support – their parent – and access to medical care including on-call help via phone when needed.
I needed to know for the care of my son and they gave me everything what I need, all the numbers, if I had any questions. They gave me my follow up appointment. I mean, basically it was good. They gave me all the information I needed … I did call them … because for his blood pressure - I’ve been doing at home so I did call them on Monday just to make sure that his blood pressure and his pulse was in the right range.
However, the patient did not have the self-efficacy to take their medications. The parent was in the process of providing him the confidence in his ability to take medications through teaching.
Right now, yes, it’s just me [the parent giving him the medications], but I’m also training him. I’m telling him you need to know and now I’ve been training him so he could look at the pills and knows what pill is what.
Resources and self-efficacy (Figure 1, area 2)
There may be patients who have the resources and self-efficacy but lack knowledge needed to engage in self-management. It is possible to easily address this by providing tailored information to patients before discharge, which can be facilitated by clinical and/or personal technologies. These patients are likely to have resources, including tangible and informational, available after discharge. In addition, these patients typically have high levels of motivation to get their health back on track.
Caregiver PC05 of a pediatric patient is an example of having resources and self-efficacy but lacking knowledge. This parent was caring for her child and had the resources and self-efficacy to learn about the medications her son was taking and she had resources to purchase these medications. She also had some knowledge about what to expect after discharge.
…we looked up some of the medications like on Google that he’s on now … we talked about what appointments he was going to need after he was out, what appointments we had to come back for … and following up with the kidney doctor or the urology [doctor].
However, she lacked important knowledge about her son’s treatment plan, specifically what medications he needed to take after discharge.
… so like when we left [the hospital] I wasn’t sure if I was still supposed to give him the [medication] when we got home, I realized they had been giving him an anti-acid in the hospital but there wasn’t anywhere on the form about whether or not we should take them. So I think there was a slight gap in how everything - information passing over.
Knowledge and Self-efficacy (Figure 1, area 3)
The situation in which patients have knowledge and self-efficacy but not resources may occur frequently, in particular in areas where there may be system or structural barriers to resources. An illustrative patient could include a patient admitted to a hospital related to their diabetes. They have had the disease for many years so they know about the disease and how to manage it. However, they live in an area with frequent power outages so it is difficult to keep critical medication stored in their refrigerator at the proper temperature.
AP12 exemplifies this scenario. She was admitted for a planned orthopedic surgery and had been given information before being admitted and while in the hospital. She also had the confidence to take her medications and understand much about the medical system and her care specifically because she worked in healthcare.
I had kind of picked her [the surgeon’s] brain before on my pre-op appointment, and I did a little research … she has actually a documentary, like a short four-minute thing on her website, it talks about what they do and what to expect and then six or eight months down the road I should be going back to a more regular routine.
However, she lacked the needed resources when the hospital, her health insurance, and her military benefits did not coordinate, resulting in billing concerns.
…when I had called to schedule I had been told from my insurance company that I had approval and I called scheduling, they said they didn’t have anything and because I had military stuff pending on my surgery, she said “well, I can send you a bill, but it’s going to be $60,000,” but they didn’t since then. And I called financial aid and all that, they haven’t said “well, your patient portion is going to be this, and this is how much,” so I have no idea what my bill looks like. And that bothered me a little bit going into this, not knowing if I owe $10,000 or $10.
No knowledge, resources, or self-efficacy (Figure 1, area 4)
These patients lack the knowledge, resources, and self-efficacy to engage in self-management. They may be the most challenging at discharge but potentially have the most to gain from any support. Since all of the subjects in our study had access to healthcare, by the very nature of being in the hospital, we have no such examples to describe. However, here we provide a hypothetical example to illustrate this case. Imagine a teenager who is a very recent immigrant, admitted to the emergency department because of injuries from a sexual assault. They come from a culture where sexual assault is not discussed so they do not know about what constitutes sexual assault and consequences of being sexually assaulted. Because of the psychological consequences of being assaulted and being in a new country, they lack confidence in their ability to manage their health or social interactions. Also, because they are not a citizen and in a country with a medical system that they are not familiar with, they may lack the resources to medical care after they leave the emergency department.
DESIGN OPPORTUNITIES
Our analysis at the time of transition after a hospitalization has highlighted the presence of a gap between hospital based care and individual-driven care at home for both adult and pediatric populations and across different medical conditions. This gap leads to challenges for patients recovering from an illness to engage in self-management because often there are not opportunities to (1) support health knowledge, (2) to access resources, and (3) promote self-efficacy, each of which contribute to successful self-management outside the hospital. In addition, hospital-based system challenges and individual personal traits contribute to this problem. With understanding the contributing factors to this gap, designers have an opportunity to focus on specific patient needs that provide support to patients during this risky time of transition from hospital to home. Based on findings regarding expectations and experiences post discharge, we first focus on system support issues ripe for potential design improvements, then discuss the opportunities available to support individual patients who are missing one or more elements required for effective self-management. We focused on the opportunities that take place prior to discharge in preparation for self-management after discharge to address pre-discharge expectations and prevent adverse experiences post-discharge.
System Support
Traditionally, hospitals expect patients to begin self-management only at the time of discharge. Although they provide resources to support this transition, we have shown that, in reality, patients still struggle. Given the importance of the knowledge gained from patient expertise and self-efficacy in supporting self-management, it is unrealistic to expect that these elements will be present immediately at the time of discharge. Ideally, a system should support their progressive development over the transition period, culminating with patients completely engaging in their own self-management at the time of discharge (Figure 2). This strategy supports patients as they develop the necessary skills, without having to worry about failure, since they remain supported by the hospital.
Figure 2.
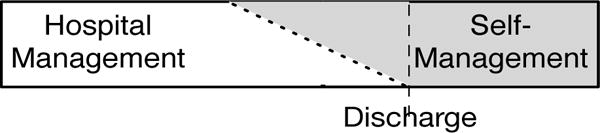
Ideally patients should have the opportunity to develop the necessary self-management elements over time while under the support and guidance of the hospital and its resources prior to discharge.
Through the KRS framework, we can beging to understand the unique and varying needs of patients throughout their hospitalization and morre importantly how these needs change overtime. The framework will allow tools to be tailored to meet the individual needs of patients in an early yet gradual and supported transition to self-management, taking into consideration the unique constraints (both physical and cognitive placed on patients as a result of their illness. In the following sections, we discuss technology opportunities to allow hospitals to realize this goal.
Capturing and Retaining Verbal Information
We have described multiple issues with information exchange to patients due to communication challenges for hospitalized patients that in turn can impact patients’ health knowledge and self-efficacy. These include excessive amounts of information, unfamiliar or confusing medical terms, an inability to process information in real time, and an inability to receive information in the first place, due to altered states of cognition resulting from a patient’s illness. Not only is the volume and content of information overwhelming for patients, but so is the speed at which it is delivered, resulting in misunderstandings and errors [60].
In the outpatient setting, others have recommended an automated approach to capturing verbal information [60], and in a cancer consultation setting, simple audio recordings have improved patients recall of the information [61] and been rated highly by patients [1]. However, simple audiotapes provide limited search and retrieval capability. Capturing verbal content during rounds and other hospital based clinician interactions could build on research from the field of ubiquitous computing to go beyond simple audio recordings.
Although embedded capture and access technologies have the potential to encourage the review of recorded conversations [38], further contextualization of this information has the potential to improve its comprehension. For example, medication names, laboratory tests, and even medical problems or diagnoses could be associated with relevant links or InfoButtons (i.e., tailored medical information) [7,17] providing patients the ability to obtain this critical information on demand at a time of their choosing.
Finding Expertise in the Hospital
To gain clinical knowledge and patient expertise, patients, including the patients in this study, are spending more time online searching for health related information, including other patients’ experiences, to address various gaps [26,52]. In addition, we know that patient expertise is obtainable from both online communities as well as in-person support groups, but these venues typically support patients outside of the hospital [18,32]. Although preliminary work explores how social interactions support children and adolescents with chronic disease in the hospital setting [59], more work is needed to understand how this technology can support both children and adults during the times of transition at the end of a hospitalization. Work is also needed to explore how hospitals and patients can address the knowledge needs of patients who may not have reliable or any access to online resources (e.g., lack of consistent internet access because they live in a rural area or lack a steady income to pay each internet bill).
Besides directing patients to external resources, hospital-based support has the potential to also fill the patient-expertise gap. Preliminary work [31,41] has shown the potential in cataloging and archiving previous patients’ personal histories, experiences, challenges, and solutions in a variety of different formats (e.g. written or video biographies), allowing current patients to obtain this information from a trusted source with minimal effort. At the very least hospitals need to enable patient access to expertise from their peers, and provide ways for them to locate it within the hospital [19].
Supporting Self-Efficacy
Although we have described how gaps in clinical knowledge and patient expertise can lead to low self-efficacy, systems supporting self-efficacy also support self-management, at least in the outpatient setting [12,14]. Preliminary work in hospitals have shown that technology supports patient engagement leading to self-efficacy through contextualized information and communication portals [22,23,63]. Although these systems focus on care planning, goal setting, and medication tracking—all important for improving self-efficacy—our results demonstrate the need for additional support tools.
We have reported patients’ challenges in understanding their capabilities and limits related to physical activity and diet. In addition, patients commented on their ability to understand how their actions impact certain clinical parameters—such as blood tests, changes in body weight, or just their overall well being. Therefore, providing patients with the ability to track a variety of parameters, outcomes or actions may help provide them with a better understanding of (1) how their ability to meet specific goals has changed over the course of their hospitalization and (2) how their behaviors and actions directly impact their clinical course. Work outside the hospital has explored the benefits of self tracking related to general wellness [20] and chronic disease management [55], but little is known about how this technology can influence patients in the hospital. In addition, we need to develop technological solutions that support the integration of self-tracking tools and electronic health records so patients can see this data in context with the rest of their medical information. These tools must minimize the burden of tracking personal information [42], especially in light of the physical and mental constraints faced by hospitalized patients. Finally, we need to expand our understanding how individuals utilize this type of information [16], specifically focusing on how to frame the data to support patient goals and self-efficacy, which are likely different from those needed to support general wellness or chronic disease tracking activities outside the hospital.
Identifying Patients’ Needs to Provide Tailored Individual Support
The common thread across the design recommendations we have discussed thus far is that to support patient self-management, hospitals and patients need to work together to identify which of the three elements that patients possess. With this understanding, using the KRS framework, systems can better tailor resources to meet the individual needs of patients. To identify these needs requires both individual- and system-level considerations.
At the individual level, we need to ensure patients have the necessary skills required for self-management (e.g. decision making and problem solving) [43]. By identifying individual deficiencies in one or more of the three elements—knowledge, resources, and self-efficacy—hospital staff can tailor specific strategies to fit the underlying needs. Most often this work will rely on a combination of technologies we just described. However, to ensure resources are allocated efficiently and effectively, understanding individual patient needs will be key. In addition, these tools should support short- and long-term self-management tailored to a specific type or class of medical conditions. Individuals with an acute medical condition, such as a broken bone, and a chronic medical condition, such as diabetes, will need knowledge, resources, and self-efficacy to engage in self-management. The difference lies in how long self-management needs to be sustained. In particular, for individuals with chronic diseases, their knowledge, resources, and self-efficacy needs may change over time and disease progression, and therefore the self-management strategies may need to adjust to those changes requiring the use of flexible tools and strategies.
At the system level, hospitals need to support patients as they transition from hospital management to self-management. This will require multiple changes to existing hospital-based practices. Hospitals and clinicians need to improve how they educate patients about their medical condition, remove the emphasis on verbal lines of transmission, support additional patient-expertise searching, and ensure patients have the confidence necessary to provide their own care without direct medical supervision. Finally, utilization of one or more of these systems will require that hospital staff understand the individual patient and his or her needs.
For both individual- and system-level design recommendations, consideration of the KRS framework and how it supports self-management requires appropriate patient training and education. Knowledge, the most straightforward, requires that patients gain clinical knowledge and patient expertise required to engage in self-management of their illness. Self-efficacy requires that patients gain the confidence and motivation required to change their behaviors and for realistic goal setting. Finally, learning appropriate problem-solving and decision-making skills, both key tasks in self-management [43,46], help individuals find and access social and structural resources needed to mange their health.
Traditional hospital educational programs that only transmit information, which is usually the same across all patients, should be replaced with tailored information that is appropriate for their cognitive development (e.g., toddler vs. older adult) to support active learning. Therefore, designers should explore how the key learning principles of growth, diversity, cognitive development, and motivation [56], support the cultivation of self-management skills. Hospital educational resources should therefore support methods that incorporate these principles to support patients as they prepare for hospital discharge.
Limitations and future work
Although our work provides insight into the challenges facing patients around the time of discharge from a hospitalization, we need to recognize its limitations. Our sample represents the patients from only two different institutions in a single metropolitan area in the United States. Although both institutions provide care to patients from a wide geographic area and diverse sociocultural and medical backgrounds, our findings may not be generalizable and therefore should be validated at additional institutions and locations within and beyond the United States. In future work, we would like to follow patients throughout their hospitalization to understand how best to begin fostering self-management. Finally, our data focused exclusively on patients and caregivers, using their own perspectives and stories. Given the significant role hospital staff play in these issues, they should be included in future studies, not just obtaining their perspective on the challenges related to transitioning to self-management, but more importantly on the development and validation of future technological resources.
CONCLUSION
In this paper, we describe how patients discharged from the hospital often are unprepared as they transition from hospitals managing their illness to their own self-management. We make three primary contributions. First, we show that—despite their best efforts—hospital systems do not utilize their resources in ways that adequately support patients during the transition period. In addition, we describe how patients lack the key elements of knowledge, resources, and self-efficacy required for self-management outside the hospital. Finally, we outline design opportunities for new systems to support patients in their self-management journey. These technological opportunities have the potential to empower patients, affording them the opportunity to focus less on living with an illness, and just living.
Acknowledgments
We thank our participants, who graciously gave us their time and attention during their hospital stay. We thank the Patients as Safeguards team, including Barry Aaronson, Shefali Haldar, Alex Filipkowski, Kelsey Aiello, and Cory Brown. We also thank Virginia Mason and Seattle Children’s hospitals. This project was primarily supported by grant #1R01HS022894 from the Agency for Healthcare Research and Quality (AHRQ), with additional funding from the NIH National Library of Medicine Training Grant #T15LM007442.
Footnotes
- ACM copyright: ACM holds the copyright on the work. This is the historical approach.
- License: The author(s) retain copyright, but ACM receives an exclusive publication license.
- Open Access: The author(s) wish to pay for the work to be open access. The additional fee must be paid to ACM.
This text field is large enough to hold the appropriate release statement assuming it is single-spaced in Times New Roman 8-point font. Please do not change or modify the size of this text box.
Each submission will be assigned a DOI string to be included here.
Contributor Information
Ari H Pollack, Email: apollack@uw.edu.
Uba Backonja, Email: backonja@uw.edu.
Andrew D. Miller, Email: millerad@uw.edu.
Sonali R. Mishra, Email: srmishra@uw.edu.
Maher Khelifi, Email: khelifi@uw.edu.
Logan Kendall, Email: kendall5@uw.edu.
Wanda Pratt, Email: wpratt@uw.edu.
References
- 1.Abowd Gregory D, Mynatt Elizabeth D. Charting past, present, and future research in ubiquitous computing. Transactions on Computer-Human Interaction (TOCHI. 2000;7(1):29–58. http://doi.org/10.1145/344949.344988. [Google Scholar]
- 2.Baker David W, Gazmararian Julie A, Williams Mark V, et al. Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. American journal of public health. 2002;92(8):1278–1283. doi: 10.2105/ajph.92.8.1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baker David W, Parker Ruth M, Williams Mark V, Scott Clark W. Health literacy and the risk of hospital admission. Journal of general internal medicine. 1998;13(12):791–798. doi: 10.1046/j.1525-1497.1998.00242.x. http://doi.org/10.1046/j.1525-1497.1998.00242.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Balaban Richard B, Weissman Joel S, Samuel Peter A, Woolhandler Stephanie. Redefining and redesigning hospital discharge to enhance patient care: a randomized controlled study. Journal of general internal medicine. 2008;23(8):1228–1233. doi: 10.1007/s11606-008-0618-9. http://doi.org/10.1007/s11606-008-0618-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bandura Albert. Self-efficacy: toward a unifying theory of behavioral change. Psychological review. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. http://doi.org/10.1016/0146-6402(78)90002-4. [DOI] [PubMed] [Google Scholar]
- 6.Bandura Albert. Health Promotion by Social Cognitive Means. Health Education & Behavior. 2004;31(2):143–164. doi: 10.1177/1090198104263660. http://doi.org/10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 7.Baorto David M, Cimino James J. An “infobutton”for enabling patients to interpret online Pap smear reports. Proceedings/AMIA … Annual Symposium. AMIA Symposium. 2000:47–50. [PMC free article] [PubMed] [Google Scholar]
- 8.Barlow Julie, Wright Chris, Sheasby Janice, Turner Andy, Hainsworth Jenny. Self-management approaches for people with chronic conditions: a review. Patient education and counseling. 2002;48(2):177–187. doi: 10.1016/s0738-3991(02)00032-0. [DOI] [PubMed] [Google Scholar]
- 9.Barnes Priscilla, Caine Kelly, Connelly Kay, Siek Katie. Understanding the needs of low SES patients with type 2 diabetes. ICST (Institute for Computer Sciences, Social-Informatics and Telecommunications Engineering); 2013. http://doi.org/10.4108/icst.pervasivehealth.2013.252153. [Google Scholar]
- 10.Ben-Shlomo Yoav, Kuh Diana. A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. International journal of epidemiology. 2002;31(2):285–293. [PubMed] [Google Scholar]
- 11.Benbassat Jochanan, Taragin Mark. Hospital readmissions as a measure of quality of health care: advantages and limitations. Archives of internal medicine. 2000;160(8):1074–1081. doi: 10.1001/archinte.160.8.1074. [DOI] [PubMed] [Google Scholar]
- 12.Bodenheimer Thomas, Lorig Kate, Holman Halsted, Grumbach Kevin. Patient self-management of chronic disease in primary care. JAMA. 2002;288(19):2469–2475. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 13.Burke Robert E, Ruixin Guo, Prochazka Allan V, Misky Gregory J. Identifying keys to success in reducing readmissions using the ideal transitions in care framework. BMC health services research. 2014;14(1):423. doi: 10.1186/1472-6963-14-423. http://doi.org/10.1186/1472-6963-14-423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carman Kristin L, Dardess Pam, Maurer Maureen, et al. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health affairs (Project Hope) 2013;32(2):223–231. doi: 10.1377/hlthaff.2012.1133. http://doi.org/10.1377/hlthaff.2012.1133. [DOI] [PubMed] [Google Scholar]
- 15.Charlton Richard, Gravenor Michael B, Rees Anwen, et al. Factors associated with low fitness in adolescents - a mixed methods study. BMC public health. 2014;14(1):764. doi: 10.1186/1471-2458-14-764. http://doi.org/10.1186/1471-2458-14-764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Choe Eun Kyoung, Lee Nicole B, Lee Bonghin, Pratt Wanda, Kientz Julie A. Understanding quantified-selfers’ practices in collecting and exploring personal data. 2014 http://doi.org/10.1145/2556288.2557372.
- 17.Cimino James J, Elhanan G, Zeng Q. Supporting infobuttons with terminological knowledge. AMIA Annual Symposium Proceedings. 1997:528–532. [PMC free article] [PubMed] [Google Scholar]
- 18.Civan Andrea, Pratt Wanda. Threading together patient expertise. AMIA Annual Symposium Proceedings. 2007:140–144. [PMC free article] [PubMed] [Google Scholar]
- 19.Civan-Hartzler Andrea, McDonald David W, Powell Chris, Skeels Meredith M, Mukai Marlee, Pratt Wanda. Bringing the field into focus: user-centered design of a patient expertise locator. ACM Request Permissions. 2010:1675–1684. doi: 10.1145/1753326.1753577. http://doi.org/10.1145/1753326.1753577. [DOI] [PMC free article] [PubMed]
- 20.Consolvo Sunny, Everitt Katherine, Smith Ian, Landay James A. Design requirements for technologies that encourage physical activity. 2006 http://doi.org/10.1145/1124772.1124840.
- 21.Corbin Juliet M, Strauss Anselm. Unending work and care: managing chronic illness at home. Jossey-Bass; 1988. [Google Scholar]
- 22.Dalal Anuj K, Dykes Patricia C, Collins Sarah, et al. A web-based, patient-centered toolkit to engage patients and caregivers in the acute care setting: a preliminary evaluation. Journal of the American Medical Informatics Association: JAMIA. 2015:ocv093. doi: 10.1093/jamia/ocv093. http://doi.org/10.1093/jamia/ocv093. [DOI] [PMC free article] [PubMed]
- 23.Dykes Patricia C, Stade Diana, Chang Frank, et al. Participatory Design and Development of a Patient-centered Toolkit to Engage Hospitalized Patients and Care Partners in their Plan of Care. Proceedings of the AMIA Symposium. 2014;2014:486–495. [PMC free article] [PubMed] [Google Scholar]
- 24.Fitzpatrick Geraldine, Ellingsen Gunnar. A Review of 25 Years of CSCW Research in Healthcare: Contributions, Challenges and Future Agendas. Computer Supported Cooperative Work (CSCW) 2013;22(4–6):609–665. http://doi.org/10.1007/s10606-012-9168-0. [Google Scholar]
- 25.Forster Alan J, Murff Harvey J, Peterson Josh F, Gandhi Tejal K, Bates David W. The incidence and severity of adverse events affecting patients after discharge from the hospital. Annals of Internal Medicine. 2003;138(3):161–167. doi: 10.7326/0003-4819-138-3-200302040-00007. [DOI] [PubMed] [Google Scholar]
- 26.Fox Susannah. The social life of health information, 2011. Pew internet & American life project. 2011 Retrieved from http://pewinternet.org/Reports/2011/Social-Life-of-Health-Info.aspx.
- 27.Gibson Peter G, Powell Heather, Wilson Amanda J, et al. Limited (information only) patient education programs for adults with asthma. The Cochrane database of systematic reviews. 2002;2:CD001005. doi: 10.1002/14651858.CD001005. http://doi.org/10.1002/14651858.CD001005. [DOI] [PubMed] [Google Scholar]
- 28.Glasziou Paul, Irwig Les, Mant David. Monitoring in chronic disease: a rational approach. BMJ (Clinical research ed) 2005;330(7492):644–648. doi: 10.1136/bmj.330.7492.644. http://doi.org/10.1136/bmj.330.7492.644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hansen Luke O, Young Robert S, Hinami Keiki, Leung Alicia, Williams Mark V. Interventions to reduce 30-day rehospitalization: a systematic review. Annals of Internal Medicine. 2011;155(8):520–528. doi: 10.7326/0003-4819-155-8-201110180-00008. http://doi.org/10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 30.Hartzler Andrea, Pratt Wanda. Managing the personal side of health: how patient expertise differs from the expertise of clinicians. Journal of medical Internet research. 2011;13(3):e62. doi: 10.2196/jmir.1728. http://doi.org/10.2196/jmir.1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hartzler Andrea L, Chaudhuri Shomir, Fey Brett C, Flum David R, Lavallee Danielle. Integrating Patient-Reported Outcomes into Spine Surgical Care through Visual Dashboards: Lessons Learned from Human-Centered Design. eGEMs. 2015;3(2):1133. doi: 10.13063/2327-9214.1133. http://doi.org/10.13063/2327-9214.1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Helgeson Vicki S, Cohen Sheldon. Social support and adjustment to cancer: reconciling descriptive, correlational, and intervention research. Health psychology: official journal of the Division of Health Psychology, American Psychological Association. 1996;15(2):135–148. doi: 10.1037//0278-6133.15.2.135. [DOI] [PubMed] [Google Scholar]
- 33.Hodge James G, Gostin Lawrence O, Jacobson Peter D. Legal issues concerning electronic health information: privacy, quality, and liability. JAMA. 1999;282(15):1466–1471. doi: 10.1001/jama.282.15.1466. [DOI] [PubMed] [Google Scholar]
- 34.Horwitz Leora I, Moriarty John P, Chen Christine, et al. Quality of discharge practices and patient understanding at an academic medical center. JAMA internal medicine. 2013;173(18):1715–1722. doi: 10.1001/jamainternmed.2013.9318. http://doi.org/10.1001/jamainternmed.2013.9318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jencks Stephen F, Williams Mark V, Coleman Eric A. Rehospitalizations among patients in the Medicare fee-for-service program. The New England journal of medicine. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. http://doi.org/10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 36.Johnson Amber E, Ebony Boulware L, Anderson Cheryl AM, et al. Perceived barriers and facilitators of using dietary modification for CKD prevention among African Americans of low socioeconomic status: a qualitative study. BMC nephrology. 2014;15(1):194. doi: 10.1186/1471-2369-15-194. http://doi.org/10.1186/1471-2369-15-194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shreya Kangovi, Barg Frances K, Carter Tamala, et al. Challenges faced by patients with low socioeconomic status during the post-hospital transition. Journal of general internal medicine. 2014;29(2):283–289. doi: 10.1007/s11606-013-2571-5. http://doi.org/10.1007/s11606-013-2571-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kientz Julie A. Embedded capture and access: encouraging recording and reviewing of data in the caregiving domain. 2012;16:2. [Google Scholar]
- 39.Kind Amy JH, Jencks Steve, Brock Jane, et al. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: a retrospective cohort study. Annals of Internal Medicine. 2014;161(11):765–774. doi: 10.7326/M13-2946. http://doi.org/10.7326/M13-2946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gina Koch, Wakefield Bonnie J, Wakefield Douglas S. Barriers and facilitators to managing multiple chronic conditions: a systematic literature review. Western journal of nursing research. 2015;37(4):498–516. doi: 10.1177/0193945914549058. http://doi.org/10.1177/0193945914549058. [DOI] [PubMed] [Google Scholar]
- 41.Lavallee Danielle C, Wicks Paul, Cristancho Rafael Alfonso, Daniel Mullins C. Stakeholder engagement in patient-centered outcomes research: high-touch or high-tech? Expert review of pharmacoeconomics & outcomes research. 2014;14(3):335–344. doi: 10.1586/14737167.2014.901890. http://doi.org/10.1586/14737167.2014.901890. [DOI] [PubMed] [Google Scholar]
- 42.Ian Li, Anind Dey, Forlizzi Jodi. A stage-based model of personal informatics systems. ACM; New York, USA: 2010. http://doi.org/10.1145/1753326.1753409. [Google Scholar]
- 43.Lorig Kate R, Holman Halsted R. Self-management education: History, definition, outcomes, and mechanisms. Annals of Behavioral Medicine. 2003;26(1):1–7. doi: 10.1207/S15324796ABM2601_01. http://doi.org/10.1207/S15324796ABM2601_01. [DOI] [PubMed] [Google Scholar]
- 44.Lorig Kate R, Ritter Philip, Stewart Anita L, et al. Chronic disease self-management program: 2-year health status and health care utilization outcomes. Medical care. 2001;39(11):1217–1223. doi: 10.1097/00005650-200111000-00008. [DOI] [PubMed] [Google Scholar]
- 45.Makaryus Amgad N, Friedman Eli A. Patients’ understanding of their treatment plans and diagnosis at discharge. Mayo Clinic Proceedings. 2005;80(8):991–994. doi: 10.4065/80.8.991. http://doi.org/10.4065/80.8.991. [DOI] [PubMed] [Google Scholar]
- 46.Lena Mamykina, Smaldone Arlene M, Bakken Suzanne R. Adopting the sensemaking perspective for chronic disease self-management. Journal of Biomedical Informatics. 2015;56(C):406–417. doi: 10.1016/j.jbi.2015.06.006. http://doi.org/10.1016/j.jbi.2015.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mandl Kenneth D, Szolovits Peter, Kohane Isaac S. Public standards and patients’ control: how to keep electronic medical records accessible but private. BMJ (Clinical research ed) 2001;322(7281):283–287. doi: 10.1136/bmj.322.7281.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nunes Francisco, Verdezoto Nervo, Fitzpatrick Geraldine, Kyng Morten, Grönvall Erik, Storni Cristiano. Self-Care Technologies in HCI: Trends, Tensions, and Opportunities. ACM Transactions on Computer-Human Interaction (TOCHI) 2015;22(6):33–45. http://doi.org/10.1145/2803173. [Google Scholar]
- 49.Carla Parry, Kramer Heidi M, Coleman Eric A. A qualitative exploration of a patient-centered coaching intervention to improve care transitions in chronically ill older adults. Home health care services quarterly. 2006;25(3–4):39–53. doi: 10.1300/J027v25n03_03. http://doi.org/10.1300/J027v25n03_03. [DOI] [PubMed] [Google Scholar]
- 50.Pfeifer Laura M, Bickmore Timothy W. Longitudinal Remote Follow-Up by Intelligent Conversational Agents for Post-Hospitalization Care. AAAI Spring Symposium: AI and Health … 2011 [Google Scholar]
- 51.Preece Jenny. Empathic communities: reaching out across the Web. interactions. 1998 http://doi.org/10.1145/274430.274435.
- 52.Sarasohn-Kahn Jane. The wisdom of patients: Health care meets online social media. California HealthCare Foundation 2008. 2012 Retrieved from http://www.chcf.org/publications/2008/04/the-wisdom-of-patients-health-care-meets-online-social-media.
- 53.Sasha Shepperd, Lannin Natasha A, Clemson Lindy M, McCluskey Annie, Cameron Ian D, Barras Sarah L. Discharge planning from hospital to home. The Cochrane database of systematic reviews. 2013;1:CD000313. doi: 10.1002/14651858.CD000313.pub4. http://doi.org/10.1002/14651858.CD000313.pub4. [DOI] [PubMed] [Google Scholar]
- 54.Skeels Meredith M, Kenton Unruh T, Powell Christopher, Pratt Wanda. Catalyzing Social Support for Breast Cancer Patients. CHI … conference proceedings/Conference on Human Factors in Computing Systems. CHI Conference. 2010:173–182. doi: 10.1145/1753326.1753353. http://doi.org/10.1145/1753326.1753353. [DOI] [PMC free article] [PubMed]
- 55.Smith Brian K, Frost Jeanna, Albayrak Meltem, Sudhakar Rajneesh. Integrating glucometers and digital photography as experience capture tools to enhance patient understanding and communication of diabetes self-management …. Personal and Ubiquitous … 2007 [Google Scholar]
- 56.Elliot Soloway, Jackson Shari L, Klein Jonathan, et al. Learning theory in practice: case studies of learner-centered design. ACM; New York, USA: 1996. http://doi.org/10.1145/238386.238476. [Google Scholar]
- 57.Stamp Kelly D, Machado Monique A, Allen Nancy A. Transitional care programs improve outcomes for heart failure patients: an integrative review. The Journal of cardiovascular nursing. 2014;29(2):140–154. doi: 10.1097/JCN.0b013e31827db560. http://doi.org/10.1097/JCN.0b013e31827db560. [DOI] [PubMed] [Google Scholar]
- 58.Storni Cristiano. Patients’ lay expertise in chronic self-care: a case study in type 1 diabetes. Health expectations: an international journal of public participation in health care and health policy. 2015;18(5):1439–1450. doi: 10.1111/hex.12124. http://doi.org/10.1111/hex.12124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Third Amanda, Richardson Ingrid. Connecting, supporting and empowering young people living with chronic illness and disability: the livewire online community. 2010 Report prepared for the Starlight Children’s Foundation …. Retrieved from https://starlight.org.au/sites/all/tmp/files/200-programs/Livewire-Online-Community-Research-Project.pdf.
- 60.Unruh Kenton T, Skeels Meredith, Civan-Hartzler Andrea, Pratt Wanda. Transforming Clinic Environments into Information Workspaces for Patients. CHI … conference proceedings/Conference on Human Factors in Computing Systems. CHI Conference. 2010:183–192. doi: 10.1145/1753326.1753354. http://doi.org/10.1145/1753326.1753354. [DOI] [PMC free article] [PubMed]
- 61.van der Meulen Nienke, Jansen Jesse, van Dulmen Sandra, Bensing Jozien, van Weert Julia. Interventions to improve recall of medical information in cancer patients: a systematic review of the literature. Psycho-oncology. 2008;17(9):857–868. doi: 10.1002/pon.1290. http://doi.org/10.1002/pon.1290. [DOI] [PubMed] [Google Scholar]
- 62.Vigod Simone N, Kurdyak Paul A, Dennis Cindy-Lee, et al. Transitional interventions to reduce early psychiatric readmissions in adults: systematic review. The British journal of psychiatry: the journal of mental science. 2013;202(3):187–194. doi: 10.1192/bjp.bp.112.115030. http://doi.org/10.1192/bjp.bp.112.115030. [DOI] [PubMed] [Google Scholar]
- 63.Lauren Wilcox, Janet Woollen, Jennifer Prey, et al. Interactive Tools for Inpatient Medication Tracking: A Multi-Phase Study with Cardiothoracic Surgery Patients. Journal of the American Medical Informatics Association: JAMIA. 2015 doi: 10.1093/jamia/ocv160. http://doi.org/http://dx.doi.org/10.1093/jamia/ocv160. [DOI] [PMC free article] [PubMed]
- 64.Shuo Zhou, Timothy Bickmore, Michael Paasche-Orlow, Jack Brian. Agent-User Concordance and Satisfaction with a Virtual Hospital Discharge Nurse. Intelligent Virtual Agents 2014 [Google Scholar]


