Abstract
The biokinetics of radon in the body has previously been studied with the assumption that its absorption through the skin is negligibly small. This assumption would be acceptable except in specific situations, such as bathing in a radon hot spring where the radon concentration in thermal water is far higher than that in air. The present study focused on such a situation in order to better understand the biokinetics of radon. To mathematically express the entry of radon through the skin into the body, we first modified the latest sophisticated biokinetic model for noble gases. Values of an important parameter for the model—the skin permeability coefficient K (m s−1)—were derived using data from previous human studies. The analysis of such empirical data, which corresponded to radon concentrations in the air exhaled by subjects during and following bathing in radon-rich thermal water, revealed that the estimated K values had a log-normal distribution. The validity of the K values and the characteristics of the present model are then discussed. Furthermore, the impact of the intake of radon or its progeny via inhalation or skin absorption on radiation dose was also assessed for possible exposure scenarios in a radon hot spring. It was concluded that, depending on the radon concentration in thermal water, there might be situations in which the dose contribution resulting from skin absorption of radon is comparable to that resulting from inhalation of radon and its progeny. This conclusion can also apply to other therapeutic situations (e.g. staying in the pool for a longer period).
Keywords: Radon, Biokinetic model, Skin absorption, Radon hot spring, Thermal water
INTRODUCTION
Radon gas can be absorbed into the bloodstream following inhalation, and it will then be distributed to the systemic tissues. This results in a dose of radiation to the tissues, although the effective dose from radon gas inhalation is generally about 20 times less than that resulting from radon progeny inhalation [1, 2]. The biokinetics of inhaled radon has been studied both numerically [3–8] and experimentally [9, 10]. Different biokinetic models for radon have been developed with regard to the systemic compartments and relevant parameters such as a tissue/blood partition coefficient. The latest model, which was developed as a generic biokinetic model framework for inhaled (and ingested) noble gases, was reported by Leggett et al. [3]. The predictions generated when this model was applied to radon were shown to be consistent with measured data from earlier human studies.
The majority of radon biokinetic models assume that inhalation is the only route of exposure to radon, and that no entry occurs through the skin. Only the model calculation by Peterman and Perkins explained that gas exchange of xenon through skin is much lower (about 0.6%) than that occurring by inhalation, suggesting the assumption that uptake through the skin could be ignored was valid [8]. In response to this report, the question arose as to whether this observation was still true for a person taking a bath in a radon hot spring, as the radon concentration in thermal water is much higher than that in air (maybe by at least three orders of magnitude). In such a situation, it is possible that skin exposure may be a significant contributor to the radiation dose.
The water that gives rise to natural spas rises through major faults or large fissures in the earth, and may come from deep underground zones to reach the surface at moderate temperatures. This underground water may contain high concentrations of radon as a result of passing through cracks or pores that are surrounded by materials containing high levels of radium, such as rocks and radium deposits. It has been reported that water with a radon concentration between hundreds and thousands of becquerels per liter may be used for therapeutic purposes [11]. Depending on the ratio of the radon concentration in thermal water to that present in the surrounding air, the amount of radon absorbed via the skin would be expected to be less significant than, similar to or more significant than the dose obtained by inhalation. However, the dermal absorption rate of radon from water and its subsequent systemic modeling have not been elucidated in detail.
The aim of the present study was to evaluate quantitatively the skin absorption of radon that takes place during taking a bath using published data from human subjects. The most recent biokinetic model for radon was first modified to account for skin absorption as an intake route [3]. Values of the unknown parameter, i.e. the skin permeability coefficient, were estimated from human data; the variability and validity of the estimated values are then discussed. Lastly, radiation doses due to the intake of radon or its progeny via inhalation or skin absorption are simply assessed for a possible exposure scenario in a radon hot spring to better understand the impact of each exposure route. Here it should be noted that in this paper, the terms ‘radon’ and ‘radon progeny’ are clearly differentiated, and the units ‘Bq l−1’ and ‘Bq m−3’ are used for water and air, respectively, according to the convention.
MATERIALS AND METHODS
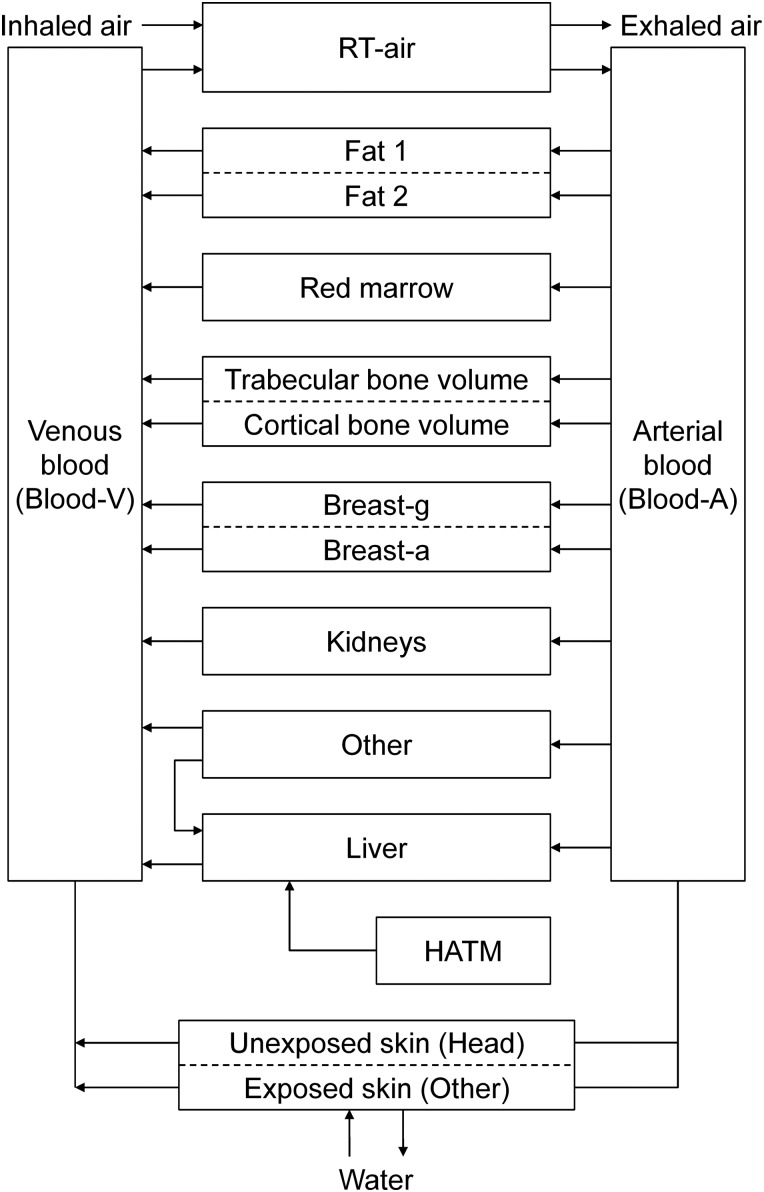
Figure 1 shows the biokinetic model used in the present work. This model was developed by incorporating skin compartments into the model previously published by Leggett et al. [3]. In their original model, the only routes of radon intake that were considered were inhalation and ingestion, because the purpose of their study was to develop a generic model from the viewpoint of radiation protection from inert gas exposure by inhalation and ingestion. Our fundamental mathematical descriptions for the kinetics of radon in tissues, and the values of the introduced parameters (e.g. the transfer coefficient between compartments and tissue mass) are derived from those reported in the paper of Leggett et al. and ICRP Publ. 89 [3, 12]. Based on the rationale behind this biokinetic modeling, the rate of change in the radon activity in a tissue (compartment), Qi (Bq), is expressed as:
| (1) |
Fig. 1.
Schematic diagram of the biokinetic model for inhaled, ingested or skin absorbed radon. RT-air, respiratory air; Breast-g, glandular tissue of breast; Breast-a, adipose tissue of breast; HATM, Human alimentary tract model.
Where Fi (m3 s−1) is the blood flow rate, CA (Bq m−3) is the radon concentration in non-pulmonary arterial blood, CV (Bq m−3) is the radon concentration in non-pulmonary venous blood and λ (s−1) is the decay constant of radon. This equation can be rewritten as:
| (2) |
Where VA (m3) is the volume of the non-pulmonary arterial blood, QA (Bq) is the activity of radon in the non-pulmonary arterial blood, Pi (−) is the tissue/blood partition coefficient of radon and Vi (m3) is the volume of the tissue. The terms Fi/VA and Fi/(PiVi) are called the transfer coefficients from arterial blood to tissue, and from tissue to venous blood, respectively.
Equations (1) and (2) are also applicable to the compartment ‘Unexposed skin (Head),’ since the head does not touch the thermal water. On the other hand, for the compartment ‘Exposed skin (Other),’ a new term describing the exchange of radon via skin must be added to Eq. (1):
| (3) |
Where the subscript ES stands for the exposed skin, K (m s−1) is the permeability coefficient of radon in skin, A (m2) is the surface area, Cw (Bq m−3) is the radon concentration in water and PS/W (−) is the skin/water partition coefficient of radon. This kind of treatment has been widely employed as a first approach in previous studies of the dermal uptake of substances (e.g. [13]). In a manner similar to the rearrangement of Eq. (1) to yield Eq. (2), Eq. (3) can be rewritten as:
| (4) |
Where PS (−) is the skin/blood partition coefficient of radon.
Parameters related to the two skin compartments (i.e. blood flow rate, tissue volume and the skin/blood partition coefficient) were determined as follows. The blood flow rate was assumed to be simply proportional to the surface area. According to ICRP Publ. 89, the total surface areas of the human body are 1.90 m2 for adult males and 1.66 m2 for adult females, and the skin on the head accounts for 7.5% of the total area of the body for both sexes [12]. In addition, regional blood flow rates in adults are given as 5.0% of the cardiac output for both sexes. Consequently, the blood flow rates were estimated to be 0.4% (= 5.0% × 0.075) of the cardiac output for the skin on the head, and 4.6% (= 5.0% × (1 − 0.075)) for the remaining skin. For the estimation of the volumes of the two skin compartments, epidermal and dermal masses of 0.005 and 0.22 g cm−2, respectively, were used [12]. The volumes (or masses) of skin on the head and the remaining parts of the body were subsequently calculated to be 0.292 l (321 g) and 2.71 l (2979 g), respectively, for adult males; and 0.255 l (280 g) and 1.84 l (2020g), respectively, for adult females. A tissue/blood partition coefficient of 0.4 was assigned to both skin compartments, as this value was applied to the compartment ‘Other,’ which included skin, in the paper of Leggett et al. [3].
To evaluate values of K and their range, our model calculation was fitted to human data from three previous studies [14–16]. The experimental conditions and results are briefly summarized in Table 1. During each experiment, the subject's body (except the head) was supposed to be kept in thermal water. Exhaled air samples were taken from the subjects during and/or after bathing, and their radon concentrations were measured. The study of Nagy used radon-free air, meaning that subjects were only exposed to radon through their skin [14]. The experimental conditions in the studies of Tempfer et al. and Furuno were similar, although the radon concentrations in both water and air were different by an order of magnitude [15, 16].
Table 1.
Summary of human volunteer experiments and values of K·AES estimated by the present model
| Reference | Experimental condition |
K·AES (m s−1) | ||||||
|---|---|---|---|---|---|---|---|---|
| Number of subjects | Radon concentration (Bq m−3) |
Water temperature (°C) | Bath time (min) |
Breath sampling for radon measurement |
||||
| Water | Air | |||||||
| Nagy [14]a | 17 (Male 8; Female 9) | Average: 73 × 103 Range: (65–86) × 103 | <1.9b | 31 | 60 | Once immediately after bathing. | 5th percentile Mode GM (median) AM 95th percentile | 5.4 × 10−8
9.5 × 10−8 3.7 × 10−7 7.3 × 10−7 2.7 × 10−6 |
| Tempfer et al. [15] | 1 (Female) | 950 × 103 | 3000 | 37 | 20 | Eleven times during and after bathing. | Best estimate | 7.4 × 10−8 |
| Furuno [16] | 1 (Unknown) | 58 × 103 | 274 | 36 | 60 | Five times during bathing. | Best estimate | 6.9 × 10−7 |
aSince it was impossible to identify which data corresponded to male or female subjects, the analyses were performed individually assuming that the subjects were all male or female. The sex-averaged K·AES is represented here; in fact, the values were almost the same between the assumed male and female groups.
bRadon-free air was used for breathing.
RESULTS
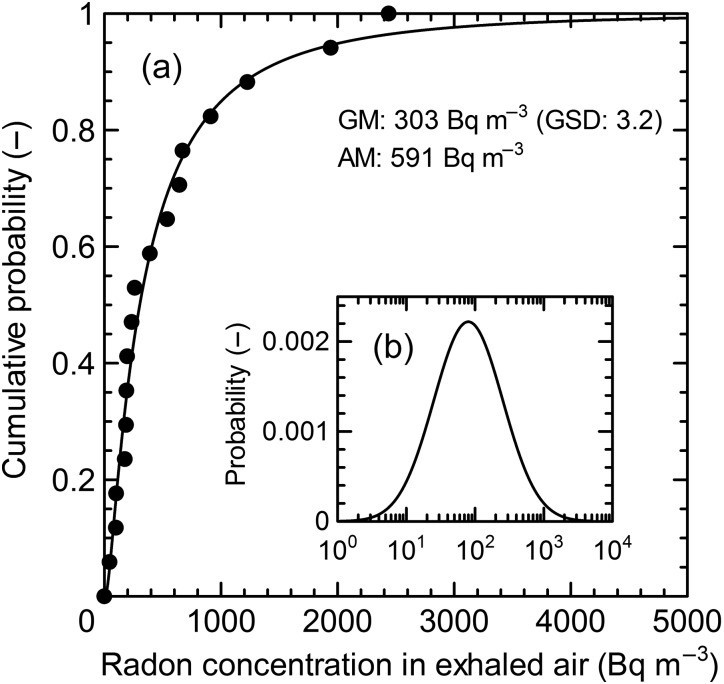
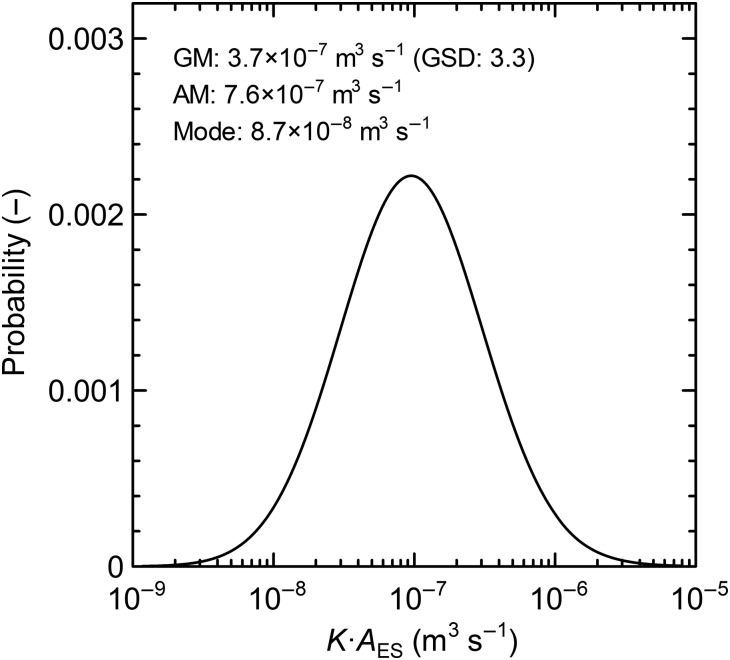
For the evaluation of K, we relied heavily on empirical data reported in the study of Nagy, which included a large ensemble of volunteers (Table 1) [14]. The radon concentration in the exhaled air samples from the original data were normalized to a radon concentration of 100 Bq l−1 in thermal water (Fig. 2). It is apparent that the data are comparable to a log-normal distribution with a geometric mean (GM) of 303 Bq m−3 and a geometric standard deviation (GSD) of 3.2. Based on the experimental data in Fig. 2, the distributions of K and K·AES were evaluated, and the results are shown in Table 2 and Fig. 3, respectively. It is worth noting that the cohort of volunteers participating in Nagy's study was composed of different sexes and ages, and individuals could not be uniquely identified in the corresponding plots in Fig. 2(a). In our analysis, we therefore assumed that all experimental data were obtained either from male or female adults. As shown in Table 2, the values of K between the 5th and 95th percentiles ranged over two orders of magnitude, while different skin surface areas resulted in small differences in K between males and females. In fact, the values of K·AES were almost the same for both sexes, leading to overlapping of the two curves shown in Fig. 3.
Fig. 2.
Distributions of radon concentrations in exhaled air (Bq m−3) immediately after a 60-min bathing session in thermal water. (a) Cumulative probability distribution. (b) Probability density distribution. The closed circles are experimental data reported by Nagy, which were normalized to a radon concentration of 100 Bq l−1 in thermal water [14]. The solid lines are curves fitted with a log-normal distribution function. GM stands for geometric mean, GSD for geometric standard deviation and AM for arithmetic mean.
Table 2.
Skin permeability estimated by fitting the present model calculation to the experimental data provided by Nagy [14]
| Skin permeability K (m s−1) | Male | Female |
|---|---|---|
| K5th – 5th percentile | 3.1 × 10−8 | 3.5 × 10−8 |
| KMode – Mode | 5.4 × 10−8 | 6.2 × 10−8 |
| KGM – Geometric mean (median) | 2.1 × 10−7 | 2.4 × 10−7 |
| KAM – Arithmetic mean | 4.1 × 10−7 | 4.8 × 10−7 |
| K95th – 95th percentile | 1.5 × 10−6 | 1.8 × 10−6 |
Note: Since it was impossible to identify which data corresponded to male or female subjects, the analyses were individually done assuming that the subjects were all male or female.
Fig. 3.
Skin permeability coefficient K estimated from the experimental data in Fig. 2. The curves for both sexes overlap over the entire range of K·AES. GM stands for geometric mean, GSD for geometric standard deviation and AM for arithmetic mean.
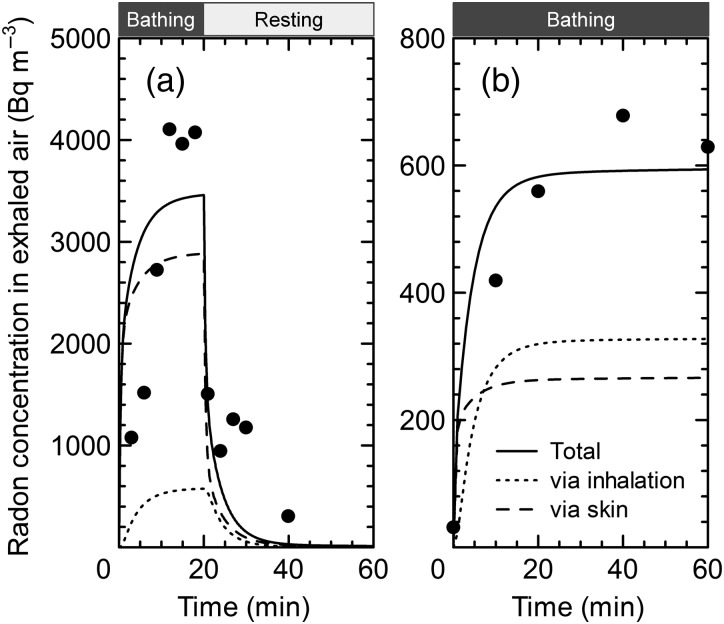
In the studies of Tempfer et al. and Furuno, the time dependence of radon concentration in exhaled air during (and after) bathing was investigated [15, 16]. In Fig. 4, measured data are compared to least-squares-fitted data, and the best estimated K values (KBest) were obtained. They are listed as KBest·AES in Table 1. Both values of KBest·AES (7.4 × 10−8 and 6.9 × 10−7 m s−1) were found to fall between K5th (5.4 × 10−8 m s−1) and K95th (2.7 × 10−6 m s−1), which were determined from the empirical data of Nagy [14]. The curve ‘Total’ represents the best fit between the calculated values and the experimental data. The curve ‘Total’ was then separated according to the contribution of each exposure route into the parts ‘via inhalation’ and ‘via skin.’
Fig. 4.
Comparisons between the model calculations and human studies of radon concentrations in exhaled air during and after bathing in thermal water. Experimental data: (a) Tempfer et al. and (b) Furuno [15, 16]. The exposure conditions are summarized in Table 1. The solid curves were obtained by the use of the best estimated K values (KBest), which were determined by fitting the experimental data. Taking into account the contribution of each exposure route, the curves (‘Total’) were then separated into inhalation and skin uptake.
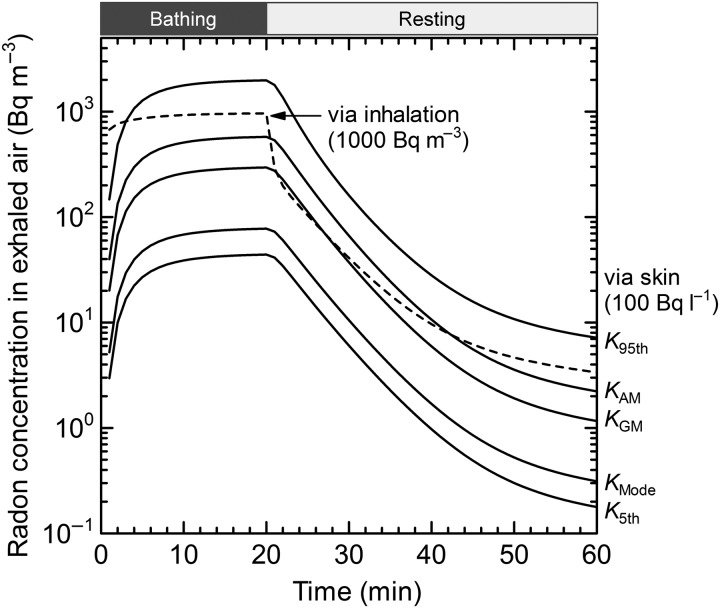
Two scenarios were tested to illustrate the influences of both the permeability coefficient K and the different exposure routes on the radon concentration in exhaled air during and after bathing. In the first, it was assumed that the bathing time was 20 min and the radon concentrations were 100 Bq l−1 in the thermal water and 0 Bq m−3 in the surrounding air (i.e. only skin exposure was considered). Secondly, a scenario of only inhalation exposure with a concentration of 1000 Bq m−3 in air was considered. As shown in Fig. 5, the rates of increase and decrease in radon concentration during and after exposure are different between the two exposure routes. The impact of K can therefore be understood.
Fig. 5.
Model predictions of radon concentrations in exhaled air during and after bathing in thermal water, for several values of K. First, only skin exposure was assumed, with the following conditions: bathing time 20 min and radon concentration 100 Bq l−1 in water. For comparison, only inhalation exposure was assumed with a bathing time of 20 min and a radon concentration of 1000 Bq m−3.
DISCUSSION
From Table 1, it can be concluded that the values of K·AES (i.e. K) estimated from the three human studies were reasonably consistent. In addition, the time trends indicated in Fig. 4 show an agreement between the calculated and measured results. These facts suggest that the present biokinetic model is accurate and represents a useful tool to predict the rate of radon intake through skin from thermal water, and its subsequent behavior in the body. According to Kety and Krogh [17, 18], the increase in the diffusion coefficient of an inert gas is approximately 1% °C−1 in the temperature range between 0 and 36°C. The range of the results obtained for K·AES allowed us to conclude that the degree of radon absorption through the skin is more strongly influenced by individual variability than the water temperature. Thus, the values of K·AES obtained here could also be applicable to the entry of radon through skin from the air. This argument will also be used later in regard to radiation dose.
However, it is also clear from Fig. 4 that the calculated data (solid lines) change more abruptly with time than the empirical data (closed plots); for example, a relatively large difference can be found just after starting the test. The fast increase or decrease in radon concentration observed immediately after starting or finishing the bath, respectively, is mainly due to the assumption made in the model that the concentration of exhaled radon that originated from inhalation could rapidly reach equilibrium with that in the environment. Figure 5 is helpful to better understand this issue. In the case of the compartment ‘RT-air’ (see Fig. 1), our modeling and relevant parameters were in accordance with those reported by Leggett et al. [3]. We must emphasize that their original modeling concept (or assumption) was appropriate in terms of continuous inhalation and dose assessment in the area of radiation protection. A half-time of 23 s, corresponding to a transfer coefficient of 2600 d−1, was assumed for ‘Environment → RT-air’ and ‘RT-air → Environment,’ which was based on measured half-times (e.g. [9]). This short half-time was estimated from data observed during the rapid phase of noble gas exhalation by human subjects, which occurs immediately after a period of continuous inhalation (8.5 h). The model of Leggett et al. did not pay particular attention to brief inhalation periods, such as those that would occur during bathing (at the longest 60 min), and this may account for the differences observed between the prediction and measurement in Fig. 4 [3]. In fact, another measurement by Furuno demonstrated that, in the case of exposure resulting solely from inhalation, it took a few tens of minutes to reach an equilibrium between the radon concentrations in exhaled air and those in the environment [16]. In addition, it should be noted that it has not been empirically validated that our model with a single skin compartment correctly represents the radon transport and storage properties of the actual skin layers (stratum corneum, viable epidermis and dermis). This validation is important if the model is to realistically reproduce the behavior of radon in skin. For the assessment of radiation dose, however, validation may not necessarily be required because overestimation or underestimation of the predicted radon concentrations in skin is expected to be counterbalanced when the periods during and after bathing are considered together.
The present work is not the first attempt that has been made to incorporate the skin absorption of radon into a biokinetic model. The first model was reported by Peterman and Perkins, and described the uptake of radon from air into skin [8]. Hofmann and Winkler-Heil have recently reported that this model was capable of making reasonable predictions [19]. The modeling by Peterman and Perkins assumed that radon diffusing through surface skin layers was dissolved in subcutaneous fat (i.e. there was no absorption above the subcutaneous fat), and that radon absorption into the bloodstream occurred from this area [8]. Interestingly, they did not rely on experimental data from radon exposure tests with subjects to derive a parameter associated with that process; this parameter was determined using four pieces of information—the diffusion coefficient of radon in tissue, the thickness of the surface skin layers, the skin surface area and the volume of subcutaneous fat. In contrast, in a manner similar to that used for many common substances, our skin modeling was based on dermal absorption [8], and it is difficult to theoretically acquire a value for the permeability coefficient K.
Our rationale for modeling the intake of radon via skin is different from that of Peterman and Perkins, although it is evident that both models can reproduce the observed data to some degree [8]. As it was not possible to directly compare the estimated skin parameters of both models, we made an attempt to compare them from the standpoint of the contribution of the skin to the total uptake of radon. Peterman and Perkins noted that the contribution of skin to xenon absorption was about 0.6% when compared with the respiratory route; radon may also have a similar value [8]. Our model calculation quantified corresponding values for radon of 0.1% for K5th, 0.2% for KMode, 0.7% for KGM, 1.1% for KAM and 2.5% for K95th. In our calculation (Eqs (3) and (4)), CW and PS/W were replaced by radon concentration in air (CAir) and PS/A (the skin/air partition coefficient of radon), respectively, because in this case, the surrounding medium was air only. It is obvious that our values are in the same range as those given by Peterman and Perkins, regardless of the difference between the models [8]. At the moment, it cannot be concluded which concept is better used when considering the intake of radon via skin, and this should be studied further.
Based on the calculation of radon distribution in the body, doses to tissues were evaluated for a scenario in which radon exposure occurred during a 20-min bathing session with radon concentrations of 100 Bq l−1 in thermal water and 1000 Bq m−3 in air, followed by a resting period in which radon concentrations of 0 Bq m−3 were assumed in both mediums. The activities of radon in the body were followed until they became negligibly small. In the dosimetry, it was assumed for simplicity that equilibrium between radon and its progeny (218Po, 214Pb, 214Bi and 214Po) was established anytime and anywhere. This means that the biokinetics of each progeny was not individually considered. Only energy deposition from alpha particles was considered because the energies of beta particles and gamma rays emitted by radon progeny are significantly lower. Table 3 shows a comparison of equivalent and effective doses, calculated using various values of K. The doses for red marrow and breast, which have higher tissue/blood partition coefficients, are reasonably higher. It is also obvious that the skin dose increases with increasing K, as expected. In the case of the scenario studied, the effective dose from radon progeny inhalation exposure, which was calculated with the dose conversion factor suggested by the United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR), is still more important than the dose resulting from radon exposure, even for K95th [1]. The effective dose from radon exposure accounts for, at most, 8% of the total dose from all exposures. It is worth noting that, if the radon concentration in water is 10 times higher (i.e. 1000 Bq l−1), the dose contribution from the radon exposure can reach approximately 40% in the case of K95th. This high concentration level has occasionally been observed in real hot springs [11, 20].
Table 3.
Calculated doses for radon exposure following a 20-min bath in radon-rich thermal water (1000 Bq m−3 in air and 100 Bq l−1 in water) and subsequent resting (0 Bq m−3 in both water and air)
| Tissue | Radon exposure (summed dose from inhalation and skin absorption exposures) |
Radon progeny inhalation exposure |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male |
Female |
||||||||||||
| Kzero (=0)a | K5th | KMode | KGM | KAM | K95th | Kzero (=0)a | K5th | KMode | KGM | KAM | K95th | ||
| Equivalent dose (nSv) | |||||||||||||
| Kidneys | 21 | 22 | 23 | 28 | 34 | 64 | 21 | 22 | 23 | 28 | 34 | 64 | - |
| Liver | 21 | 22 | 23 | 28 | 34 | 64 | 21 | 22 | 23 | 28 | 34 | 64 | - |
| Bone surface | 3 | 3 | 3 | 4 | 4 | 8 | 2 | 2 | 2 | 3 | 3 | 6 | - |
| Red marrow | 145 | 151 | 156 | 189 | 231 | 432 | 145 | 152 | 157 | 190 | 232 | 439 | - |
| Breast | 45 | 48 | 49 | 59 | 73 | 136 | 46 | 48 | 49 | 60 | 73 | 138 | - |
| Skin | 11 | 38 | 58 | 187 | 352 | 1149 | 11 | 40 | 62 | 202 | 380 | 1251 | - |
| Other | 12 | 13 | 13 | 16 | 19 | 36 | 12 | 13 | 13 | 16 | 19 | 37 | - |
| Effective dose (nSv) | 32 | 34 | 35 | 44 | 55 | 108 | 32 | 34 | 36 | 44 | 56 | 110 | 1200b |
aThis means only inhalation of radon (i.e. without accounting for its exchange through skin).
bThe dose from radon progeny inhalation was calculated using a dose conversion factor of 9 nSv (Bq h m−3) −1 and an equilibrium factor of 0.4 [1].
A trial assessment of doses from radon in a natural environment (not a bathing situation) was also attempted using various K values. The application of our estimated K to the air-to-skin exchange of radon may be valid as discussed above. The effective doses from both inhalation and skin absorption exposures are estimated to be 97–98 pSv (Bq h m−3) −1 for both sexes for Kzero (i.e. exposure only by inhalation) and any K value given in Table 2. This result leads to the conclusion that skin uptake is negligible compared with the inhalation of radon, even when the inhalation of radon progeny is not considered.
CONCLUSION
In this study, a biokinetic model of radon is introduced in which the exchange of radon between skin and the environment was incorporated into the latest sophisticated model. This permits a better understanding of the behavior of radon in the body. The skin permeability, K, which is necessarily implemented in the presented model, was determined, and found to have a log-normal distribution among individuals. The estimated values of K were validated for the skin-to-water exchange of radon, and based on their temperature-dependent behavior, were inferred also to be applicable to skin-to-air exchange. The changes in radon concentration in exhaled air during and after bathing, as an index of its dynamics after intake into the body, were compared. In general, there was an agreement between the model predictions and real-world observations.
The need to consider the dose contribution of radon absorbed via the skin was also discussed by comparison with the contribution made by radon and its progeny following inhalation. It was shown that this depends on the ratio of the radon concentration in thermal water to that present in air. For typical indoor and outdoor exposures, the intake of not only radon progeny, but also radon, through the skin is negligible in comparison with the intake via inhalation. In situations involving immersion in radon-rich thermal water, however, it might be better to consider the impact of skin absorption; our calculation demonstrated that skin absorption might reach a few tens of a percent of the total dose when the radon concentration is 1000 Bq m−3 in air and 1000 Bq l−1 in water. This result provides a new insight into the existing approach for radon exposure assessment, although the relevance of these findings may be limited to this kind of special case.
FUNDING
Funding to pay the Open Access publication charges for this article was provided by Japan Atomic Energy Agency.
ACKNOWLEDGMENTS
The authors are grateful to Drs K. Nagy (Markhot Ferenc County Hospital in Hungary), K. Tibor (University of Pannonia, Hungary) and N. Kavasi (National Institute of Radiological Sciences, Japan) for sharing information on their human studies. We also thank Drs W. Hofmann and H. Lettner (University of Salzburg, Austria) for the discussion on biokinetic modeling and their human studies, and Dr W.B. Li (Helmholtz Zentrum München, Germany) for the discussion on dosimetry.
REFERENCES
- 1.United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR). Sources and Effects of Ionizing Radiation. UNSCEAR 2000 Report to the General Assembly, with Scientific Annexes. New York: United Nations, 2000. [Google Scholar]
- 2.United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR). Sources and Effects of Ionizing Radiation. UNSCEAR 2006 Report to the General Assembly, with Scientific Annexes. New York: United Nations, 2008. [Google Scholar]
- 3.Leggett R, Marsh J, Gregoratto D et al. A generic biokinetic model for noble gases with supplication to radon. J Radiol Prot 2013;33:413–32. [DOI] [PubMed] [Google Scholar]
- 4.Sakoda A, Ishimori Y, Kawabe A et al. Physiologically based pharmacokinetic modeling of inhaled radon to calculate absorbed doses in mice, rats, and humans. J Nucl Sci Technol 2010;47:731–8. [Google Scholar]
- 5.Yu D, Kim JK. A physiologically based assessment of human exposure to radon released from groundwater. Chemosphere 2004;54:639–45. [DOI] [PubMed] [Google Scholar]
- 6.Khursheed A. Doses to systemic tissues from radon gas. Radiat Protect Dosim 2000;88:171–81. [Google Scholar]
- 7.National Academy Sciences (NAS). Risk Assessment of Radon in Drinking Water. Washington DC: National Academy Press, 1999. [PubMed] [Google Scholar]
- 8.Peterman BF, Perkins CJ. Dynamics of radioactive chemically inert gases in the human body. Radiat Protect Dosim 1988;22:5–12. [Google Scholar]
- 9.Harley JH, Jetter ES, Nelson N. Elimination of radon from the body. Environ Int 1994;20:573–84. [Google Scholar]
- 10.Nussbaum E, Hursh JB. Radon solubility in rat tissues. Science 1957;125:552–3. [DOI] [PubMed] [Google Scholar]
- 11.Voronov AN. Radon-rich waters in Russia. Environ Geol 2004;46:630–4. [Google Scholar]
- 12.International Commission on Radiological Protection (ICRP). Basic anatomical and physiological data for use in radiological protection reference values. ICRP Publication 89. Ann ICRP 2002;32. [PubMed] [Google Scholar]
- 13.Roy A, Georgopoulos PG. Mechanistic Modeling of Transport and Metabolism in Physiological Systems. Technical report CCL/EDMAS-02 Piscataway, NJ: Environmental and Occupational Health Sciences Institute, 1997. www.ccl.rutgers.edu/ccl-files/reports/EDMAS/T-11_CCL-EDMAS-02.pdf (26 Oct 2015, date last accessed). [Google Scholar]
- 14.Nagy K. Clinical and Experimental Tests Carried Out with Medicinal Water and Medicinal Caves Containing Radon. Dissertation, University of Szeged, 2008. http://doktori.bibl.u-szeged.hu/1174 (26 October 2015, date last accessed).
- 15.Tempfer H, Schober A, Hofmann W et al. Biophysical mechanisms and radiation doses in radon therapy. In: McLaughlin JP, Simopoulos SE, Steinhäusler F (eds). Radiactivity in the Environment. Amsterdam: Elsevier, 2005;7:640–8. [Google Scholar]
- 16.Furuno K. Studies on trace elements in the field of balneology (II) Determination of radon contents in the air of radioactive spa areas, and excretion of radon in expiratory air after using spring water. J Jpn Soc Balneol Climatol Phys Med 1982;45:49–67 (in Japanese with English abstract). [Google Scholar]
- 17.Kety SS. The theory and applications of the exchange of inert gas at the lungs and tissues. Pharmacol Rev 1951;3:1–41. [PubMed] [Google Scholar]
- 18.Krogh A. The rate of diffusion of gases through animal tissues, with some remarks on the coefficient of invasion. J Physiol 1919;52:391–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hofmann W, Winkler-Heil R. Mathematische Simulation der Aufnahme, Verteilung und Ausscheidung von Radon in der Radontherapie. Proceedings of the 5th Biophysics Workshop—Biologische Wirkungen niedriger Strahlendosen—Natürliche Strahlenexposition, Radon-Balneotherapie und Strahlenschutz. Bad Schlema, July 2010, 77–82, ISBN 3–9811258–7–8 (in German with English abstract).
- 20.Tempfer H, Hofmann W, Schober A et al. Deposition of radon progeny on skin surfaces and resulting radiation doses in radon therapy. Radiat Environ Biophys 2010;49:249–259. [DOI] [PubMed] [Google Scholar]