Abstract
Background
Evidence is emerging that indoor air pollution (IAP) from use of solid fuels for cooking and heating may be an important risk factor for coronary heart disease (CHD).
Sources of data
We searched the Ovid Medline, Embase Classic, Embase and Web of Science databases from inception through to June 12, 2015, to identify reports of primary epidemiological research concerning the relationship of CHD to IAP from solid fuel, the likely magnitude of any increase in risk, and potential pathogenic mechanisms.
Areas of agreement
The current balance of epidemiological evidence points to an increased risk of CHD from IAP as a consequence of using solid, and especially biomass, fuels for cooking and heating. Relative risks from long-term exposure could be 2- to 4-fold.
Areas of controversy
The evidence base is still limited, and although an association of CHD with such IAP from solid fuel is consistent with the known hazards from smoking, environmental tobacco smoke and ambient air pollution, and supported by evidence of effects on inflammatory processes, atherosclerosis and blood pressure, it requires confirmation by larger and more robust studies.
Growing points
The completion of two relatively small case-control studies on CHD and IAP from use of biomass fuel demonstrates the feasibility of such research, and is an encouragement to further, larger studies using similar methods.
Areas timely for developing research
The need for such research is particularly pressing because the incidence of CHD in developing countries is rising, and IAP may interact synergistically with the risk factors that are driving that increase. Furthermore, relatively cheap methods are available to reduce IAP from use of solid fuels, and there are indications from intervention studies that these may impact beneficially on CHD as well as other diseases caused by such pollution.
Keywords: solid fuel, biomass, indoor air pollution, household air pollution, coronary heart disease, cardiovascular disease
Introduction
Coronary heart disease (CHD) is the leading cause of death worldwide, with a rapidly increasing incidence in developing countries.1 In addition to well-established risk factors such as smoking, an important contributor to the burden of CHD in developing countries may be indoor air pollution (IAP) from use of solid fuel (principally biomass) for cooking and heating. In 2010, some 40% of households across the world used solid fuel for cooking or heating, with the highest prevalence in Africa, followed by Asian countries.2
Major air pollutants produced by combustion of solid fuels include fine particulate matter (PM) and carbon monoxide (CO), both of which have been linked to CHD. They are present in tobacco smoke, and may in part explain the increased risks of CHD from both active3,4 and passive smoking.5,6 Furthermore, PM in ambient air is an established risk factor for CHD, as demonstrated in time-series and cohort studies.7,8
Combustion of solid fuel for cooking can generate concentrations of pollutants in kitchens 100–200 times higher than current ambient air standards.9 Thus, it is highly plausible that IAP from use of solid fuel could importantly increase the risk of CHD. However, until recently the relationship of CHD to IAP has been much less investigated than its links with ambient air pollution. In 2008, Fullerton and colleagues published a non-systematic review of research on the health effects of IAP from biomass fuel, including on cardiovascular disease (CVD), and found a paucity of relevant data.10 More recently, Yamamoto et al. 11 carried out a systematic review of the impacts of air pollution, both ambient and indoor, on CVDs, but restricted their attention to research carried out in eight lower income countries in South Asia. In total they identified nine relevant studies, of which four related to IAP from biomass fuels.
Over the last 10 years, epidemiological research on use of biomass fuel and CHD has been expanding, and it is therefore timely to review the published literature more comprehensively, as a guide both to policy and to priorities for further research. To this end, we undertook a narrative evaluation of systematically identified epidemiological reports, our aim being to assess the strength of evidence for an association of CHD with IAP from use of solid fuel, and the likely magnitude of any increase in risk.
Methods
To address our study question, we sought to identify all reports in peer-reviewed journals, which had at least an abstract in English, and which described primary epidemiological research concerning the relationship of IAP from use of biomass fuel to heart disease (particularly CHD) or to pathogenic mechanisms relevant to CHD.
We first interrogated four electronic databases (Ovid Medline, Embase Classic, Embase and Web of Science) from inception through to June 12, 2015, using the combination of search terms set out in Table 1. Potentially relevant references (with their abstracts) were imported into a single Endnote file, and after removal of duplicates, each was reviewed. Those that were clearly irrelevant were discarded, and full text copies of the remainder were obtained and scrutinized. Those that met our inclusion criteria were abstracted and summarized using a standardized form. In addition we searched their reference lists for further papers that might have been missed. Each stage of the process after the initial electronic search was carried out independently by the two authors, and their decisions and abstracted summaries were compared, with resolution of discrepancies by discussion.
Table 1.
Search terms used to identify relevant studies
| Exposure terms |
|
| Outcome terms | |
| Combination terms |
In evaluating the publications that were eligible for review, we grouped findings by health outcome, and considered the conclusions that could be drawn given the strengths and limitations of each study.
Results
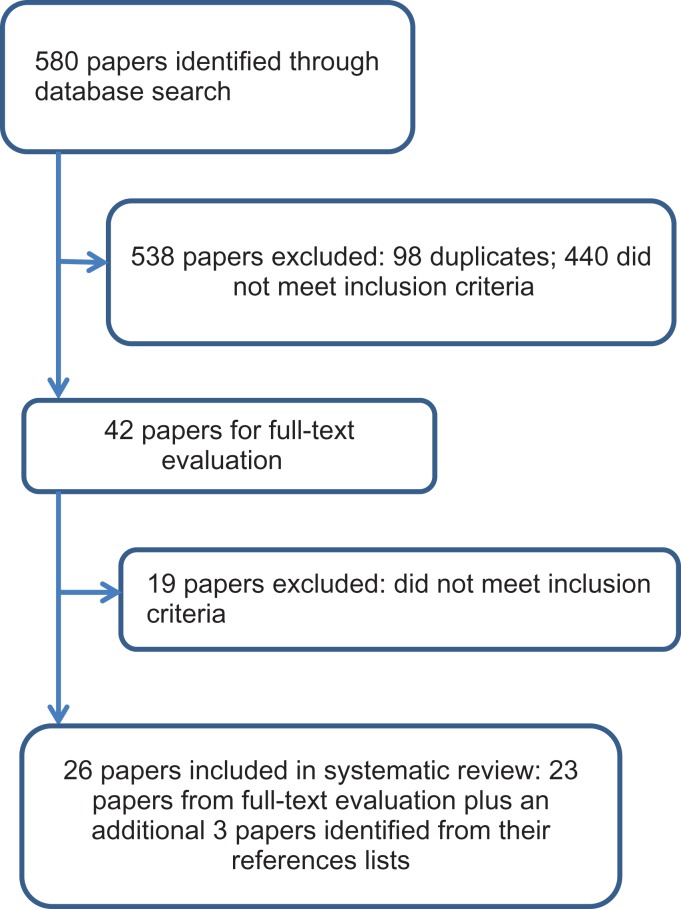
Our initial search identified 202 potentially relevant reports through Ovid Medline and Embase, and 378 in the Web of Science database. After removal of 98 duplicates, the titles and abstracts of the remaining 482 papers were read, and 440 that did not meet the specified inclusion criteria were discarded. Full copies of the other 42 references were retrieved, and following detailed scrutiny, 23 were judged eligible for inclusion. In addition, three further publications were identified from the reference lists of those papers, giving a final total of 26 reports that were included in the review (Fig. 1).
Fig. 1.
Flow chart summarizing the identification and selection of papers for review.
The 26 articles (Table 2) had all been published since 2005, including 22 since 2010. They described 25 studies (two papers12,13 related to the same study) conducted in South Asia (10), China (4), Turkey (2), Iran (1) and Central and South America (8). Five studies were reported only as abstracts. Eight provided information about risk of CHD or heart disease more generally, 3 about heart rate or its variability, 4 about measures of vascular pathology, 6 about oxidative stress and/or biomarkers of inflammation, 13 about blood pressure (BP), and 1 about lipid profile. Most compared use of biomass with non-use or with use of cleaner fuels, but four assessed the impact of biomass stoves with improved design, three compared different levels of exposure to PM, CO or black carbon and one assessed associations with occupational exposure to indoor barbecues. Sixteen were cross-sectional in design, four assessed interventions, two were case-control investigations and three were cohort studies. Potential for confounding was addressed by various combinations of restriction (e.g. to women or non-smokers), matching and statistical adjustment. However, in two studies there was no documented control for possible confounding. As indicated in the comments in Table 2, some of the studies had important limitations.
Table 2.
Epidemiological studies bearing on the relationship of coronary heart disease to IAP from use of solid fuel
| Country and reference | Design | Study sample | Exposures compared | Outcome | Association | Confounders addressed | Comments |
|---|---|---|---|---|---|---|---|
| India (Ray et al. 14) | Cross-sectional | 165 non-smoking women who cooked regularly with biomass and 155 non-smoking controls who cooked with liquefied petroleum gas (LPG) | Cooking with biomass vs. LPG | Hypertension, CD11b and CD18 expression on circulating neutrophils and monocytes, P-selectin expression on platelets, and count of activated platelet–neutrophil and platelet–monocyte aggregates | Hypertension in 6.0% biomass users vs. 3.2% LPG users | Age, smoking, tobacco-chewing and environmental tobacco smoke | Methods of statistical analysis not fully described |
| Activation of leucocytes and formation of leucocyte-platelet aggregates significantly more common in women using biomass, but differences reduced after adjustment for tobacco-chewing and exposure to environmental tobacco smoke | |||||||
| Guatemala (McCracken et al. 15) | Controlled intervention with intervention subsequently offered to control group | 120 women aged >38 who cooked daily and lived in households participating in a randomized controlled trial of an improved woodstove (49 intervention and 71 controls) | Use vs. non-use of improved stove | Systolic and diastolic blood pressure (SBP and DBP) | Differences in blood pressure (BP): | Age, body mass index, ambient temperature, rainy season, day of week, time of day, use of wood-heated sauna, having household electricity, an asset index, ever smoked and environmental tobacco smoke | Personal 24 h PM2.5 exposures during trial period were 264 vs. 102 μg/m3 |
Intervention vs control group:
| |||||||
| intervention vs. control group | |||||||
| After vs. before intervention in controls who subsequenly received it | |||||||
| Control group after vs. before: SBP: −3.1 (95% CI: −5.3 to −0.8) mm Hg DBP: −1.9 (95% CI: −3.5 to −0.4) mm Hg | |||||||
| Turkey (Davutoglu et al. 16) | Cross-sectional | 40 non-smoking male indoor barbecue workers using charcoal and 48 non-smoking age-matched healthy controls | Barbecue work vs. control | Carotid intima media thickness (CIMT), high-sensitivity C-reactive protein (hs-CRP), blood pressure (BP) and lipid profile |
|
Sex, age and body mass index well matched | Mean carboxy-haemoglobin was higher in exposed group (6.4% vs. 2.0%) |
| Turkey (Butarak et al. 17) | Cross-sectional | 47 healthy, non-smoking subjects exposed to biomass smoke since birth and 32 healthy, non-smoking controls with no exposure to biomass | Lifelong exposure to biomass vs. no exposure | CIMT, flow associated dilatation (FAD %) and endothelium independent vasodilatation (GTN %) assessed by ultrasound |
|
Smoking | No adjustment for age (on average, controls were 3.7 years younger than exposed) or other potential confounders such as body mass index |
| India (Dutta et al. 18) | Cross-sectional | 244 healthy, non-smoking women aged 22–41, using biomass for cooking and 236 healthy, non-smoking women aged 23–40, using LPG for cooking | Use of biomass vs. LPG for cooking | Hypertension, expression of platelet P-selectin, platelet aggregation to collagen, generation of reactive oxygen species (ROS) in leucocytes, serum oxidized low density lipoprotein (oxLDL) and serum anticarbiolipin antibody (aCL) |
|
Smoking and age | Women using biomass were less educated and had lower family income. 8 h mean PM2.5 concentration in cooking areas 156 vs. 52 μg/m3
Statistical methods are poorly described |
| Nicaragua (Clark et al. 19) | Cross-sectional | 123 non-smoking women aged 11–80, who cooked using traditional biomass stoves | Increase by inter-quartile range in 48 hr indoor PM2.5 (1212 μg/m3), indoor CO (24 ppm) and personal CO (2 ppm) | Difference in SBP, DBP and heart rate (assessed by pulse oximeter) |
|
Smoking, age, body mass index, environmental tobacco smoke and education | |
| China (Baumgartner et al. 12; Baumgartner et al. 13) | Cross-sectional | 280 non-smoking women aged ≥ 25 in rural households using biomass fuels (mainly wood or charcoal) | Levels of personal 24-hr average exposure to PM2.5, black carbon and water-soluble organic mass | SBP and DBP | A 1-log-μg/m3 increase in PM2.5 exposures was associated with 2.2 (95% CI: 0.8 to 3.7) mm Hg higher SBP and 0.5 (95% CI: −0.4 to 1.3) mm Hg higher DBP | Age, waist circumference, physical activity, socio-economic status, salt intake, day of week, time of day and average ambient temperature | |
| Among different measures of particulate air pollution, associations with SBP and DBP were strongest and most robust for black carbon. | |||||||
| India (Firdaus et al. 20) | Cross-sectional | 5949 households selected by partially random multi-stage sampling | Use of traditional fuels vs. non-use | Cardiovascular disease the most frequently occurring disease faced by at least one household member in last 3 months | Odds ratio 1.22 (95% CI: 1.09 to 1.35) | Crude analysis with poorly specified health outcome and no control for potential confounders | |
| Guatemala (McCracken et al. 21) | Controlled intervention with intervention subsequently offered to control group | 119 women aged >38 who cooked daily and lived in households participating in a randomized controlled trial of an improved woodstove (49 intervention and 70 controls) | Use vs. non-use of improved stove – | Heart rate variability (HRV) and ST-segment depression (defined as average below −1 mm) | Intervention vs. control group:
|
Age (quadratic), body mass index (quadratic), asset index, ever smoked, environmental tobacco smoke, owning a wood-fired sauna, recent use of wood-fired sauna, time of day, season (wet/dry), ambient temperature and humidity, daily rainfall, and interactions of weather variable with season | Adjustment for potential confounders differed according to comparison Personal 24-h PM2.5 exposures during trial period were 266 vs. 102 μg/m3 |
| Intervention vs. control group | Control group after vs. before:
|
||||||
| After vs. before intervention in controls who subsequently received it | |||||||
| India (Dutta et al. 22) | Cross-sectional | 635 healthy, non-smoking women aged 24–44, using biomass for cooking and 452 healthy, non-smoking women aged 25–44, using LPG for cooking | Use of biomass vs. LPG for cooking | Hypertension, tachycardia (>100 beats per minute), serum C-reactive protein (CRP), tumour necrosis factor-alpha (TNF-α), interleukin-8 (IL-8), IL-6, generation of ROS in leucocytes, and erythrocyte superoxide dismutase (SOD) |
|
Smoking Groups well matched for age, body mass index and smokers in family |
Women using biomass were less educated and had lower family income. |
| 8-h mean PM2.5 concentration in cooking areas 158 v 51 μg/m3 | |||||||
| Statistical methods are poorly described | |||||||
| Unclear whether there is overlap with Dutta et al. (2011) 18 | |||||||
| Nicaragua (Clark et al. 23) | Intervention with before and after comparison | 98 women who cooked using biomass stoves | Provision of cleaner burning cookstove | Change in CRP measured in dried blood spot samples | Reduction of 25% (95% CI: 2 to 49) among obese women. | Reported only as abstract | |
| Sri Lanka (Sathiakumar24) | Case-control | 50 women aged 40–70 years treated in hospital for acute coronary syndrome and 50 controls | Use of biomass fuel vs. LPG | Acute coronary syndrome | Odds ratio = 2.57 (95% CI 1.07 to 6.13) | Not specified | Reported only as an abstract. |
| Biomass included kerosene | |||||||
| China (Baumgartner et al. 25) | Cross-sectional | 240 children aged 5–14 in rural households cooking with biomass | Levels of personal 24-hr average exposure to PM2.5 | SBP and DBP | A 1-log-μg/m3 increase in PM2.5 exposures was associated with a −1.8 (95% CI: −3.6 to 0.1) mm Hg difference in SBP and a −0.5 (95% CI: −2.1 to 1.2) mm Hg difference in DBP | Sex, age, height, body mass index, passive smoking, socioeconomic status, salt intake, monosodium glutamate use, physical activity, day of week and time of day of blood pressure measurement | |
| China (Lee et al. 26) | Cross-sectional | 13 438 adults randomly selected from census data | Ever vs. never use of solid fuel (coal or biomass) | Self-report of doctor-diagnosed CHD, hypertension | CHD odds ratio = 2.58 (95% CI: 1.53 to 4.32)Hypertension odds ratio = 1.70 (95% CI: 1.40 to 2.07) | Age, gender, educational level, smoking, environmental tobacco smoke, pack-years smoked, body mass index and waist circumference | Risk of hypertension increased with duration of solid fuel use, but CHD did not show a consistent exposure–response relationship |
| Iran (Mitter et al. 27) | Cohort | 50 045 men | Years used wood and other biomass for cooking and heating | Mortality from heart disease | HR for death from heart disease for each additional year of use:Cooking:
Heating:
|
Age, sex, rural living, socioeconomic status, body mass index, smoking, use of opiates, diabetes and hypertension. | Reported only as abstract. |
| Bangladesh (Alam et al. 28) | Cohort | 22 337 adult residents of 11 villages (20 757 using solid fuel and 1580 using natural gas) followed for 10 years | Use of solid fuel for cooking or heating vs. use of natural gas | Mortality from ischaemic heart disease (IHD) determined by verbal autopsy | Incidence rate ratios for IHD:
|
Sex | It is unclear whether there was any adjustment for age |
| India (Banerjee et al. 29) | Cross-sectional | 142 women aged 23–40 who had never smoked and had cooked exclusively with biomass for ≥5 years, and 126 age-matched, non-smoking controls who cooked with LPG | Use of biomass vs. LPG for cooking | Surface expression of CD35, CD16 and CD11b/CD18 on circulating neutrophils | Among users of biomass fuel:
|
Age, body mass index, years of cooking, hours of cooking per day, environmental tobacco smoke, food habits and use of mosquito repellants | Education, family income and prevalence of homes with separate kitchens were lower in biomass users. |
| Plasma concentrations of tumour necrosis factor-alpha (TNF-α), interleulin-6 (IL-6), IL-8, IL-12 and nitric oxide (NO) | |||||||
| The published report is unclear in places, and the methods of statistical analysis are not adequately explained | |||||||
| Myeloperoxidase activity in circulating neutrophils | |||||||
| Erythrocyte level of SOD | |||||||
| Peru (Painschab et al. 30) | Cross-sectional | 266 adults aged ≥ 35 including 154 using biomass fuel and 112 using clean fuel (based on rural or urban residence) | Chronic exposure to biomass smoke vs. use of clean fuel | CIMT and prevalence of carotid plaque (assessed by ultrasound) and blood pressure (BP) | Increase in mean CIMT: 0.03 (95% CI: 0.01 to 0.06) mm | Age, sex, low density lipoprotein, high density lipoprotein, body mass index, homeostasis model of assessment-insulin resistance, use of anti-hypertensives | |
| Increase in maximum CIMT: 0.03 (95% CI: 0.01 to 0.06) mm | |||||||
| Increase in systolic BP: 9.2 (95% CI: 5.4 to 13.0) mm Hg | |||||||
| Increase in diastolic BP: 6.5 (95% CI: 4.1 to 8.9) mm Hg | |||||||
| Odds ratio for carotid plaque: 2.55 (95% CI: 1.08 to 5.98) | |||||||
| Pakistan (Fatmi et al. 31) | Case-control | 73 non-smoking women admitted to hospital with acute coronary syndrome and 73 non-smoking controls admitted for other reasons | Current use of biomass vs. natural gas for cooking | Acute coronary syndrome | Odds ratio: 4.8 (95% CI: 1.5 to 14.8) | Age, smoking, body mass index, educational status, type of kitchen, type of house, use of ghee and consumption of meat | Risk was lowest among women who had not used biomass fuel in past 15 years |
| Nepal (Pratali and Cogo32) | Cross-sectional | 82 men and women without established CVD | Use vs. non-use of biomass fuels | Endothelial function in brachial artery evaluated by flow-mediated dilation (FMD) | FMD tended to be lower in people using biomass fuels | Reported only as abstract | |
| China (Kim et al. 33) | Cohort study | 73 363 women | Use of coal in home for >30 years vs. never use. | Mortality from CVD and myocardial infarction (MI) | HRs CVD: 1.32 (95% CI: 1.11 to 1.57) MI: 1.62 (95% CI: 1.01 to 2.63) |
Smoking status, family income, environmental tobacco smoke, occupational history, shift work, body mass index, hormone therapy and parity. | Reported only as abstract. |
| Duration of follow-up not mentioned. | |||||||
| Peru (Caravedo et al. 34) | Cross-sectional | 519 adults aged ≥35 | Long-term use of biomass (n = 275) vs. clean fuels (n = 244) for cooking | Serum N-terminal pro-B-type natriuretic peptide (NT-pro-BNP) Pulmonary artery systolic pressure (PASP) in subset of 159 | No significant difference in NT-pro-BNP or PASP | Sex, age, height, body mass index, systolic blood pressure, hypertension, CVD, diabetes, asthma and others | |
| Peru (Burroughs Peña et al. 35) | Cross-sectional | 1004 adults aged ≥35 | Daily use of biomass for cooking or heating for >6 months at any time in life (n = 509) vs. not so exposed (n = 495) | SBP and DBP | SBP overall higher by 7.0 (95% CI: 4.4 to 9.6) mm Hg:
|
Sex, age, body mass index, height, wealth, education years, depressive symptoms, smoking (pack-years), alcohol abuse and low physical activity | |
DBP overall higher by 5.9 (95% CI: 4.2 to 7.6) mm Hg:
| |||||||
| Bolivia (Alexander et al. 36) | Intervention with before and after comparison | 28 non-smoking women from a rural community | Use vs. non-use of improved cookstove | SDP and DBP | Following intervention SBP fell by 5.5 mm Hg (p = 0.01) and DBP by 1.1 mm Hg (p = 0.5) (stratified data showed significant decrease only for >50 years age women). | ||
| In random subset of 13 women, reductions in SBP and DBP correlated with reductions in concentrations of PM during cooking (p = 0.01 for both) | |||||||
| Nepal (Neupane et al. 37) | Cross-sectional | 519 women aged 30–83 in rural location | Cooked for ≥10 years primarily with biomass (n = 300) vs. biogas (n = 219) | SBP and DBP | Differences in blood pressure (mm Hg) at age 30–50:
|
Sex, age, body mass index, socio-economic status, smoking, kitchen characteristics, ventilation and additional fuel use | |
Differences in blood pressure (mm Hg) at age>50:
|
ns = not significant.
Heart disease
Two case-control studies assessed the association of hospital treatment for acute coronary syndrome with use of biomass fuel as compared with natural or liquefied petroleum gas (LPG).24,31 Although they were relatively small, both found significantly elevated odds ratios (2.57 and 4.8). However, one was reported only as an abstract, and apart from age, it is unclear exactly which potential confounders were taken into account.24 Furthermore, it grouped kerosene with biomass fuels, which may have biased risk estimates towards the null.
In Iran, Mitter et al. 27 examined hazard ratios (HRs) for death from heart disease in a cohort of more than 50 000 men and women, according to years of using wood or other biomass fuel for cooking and heating. Positive associations were found with use of biomass other than wood, but they were weak and not statistically significant (HRs of 1.003 for each additional year of use). Again, the study was reported only as an abstract, making it difficult to be confident about the validity of the methods. Adjustment for hypertension could have caused the effects of biomass to be underestimated if effects on BP lay on a causal pathway to heart disease.
In a cohort study of 73 363 women in China, use of coal in the home for >30 years carried a HR of 1.62 (95% CI: 1.01 to 2.63) for death from myocardial infarction in comparison with never use33. However, the investigation was reported only as an abstract, and the duration of follow-up was not described.
Alam et al. 28 ascertained deaths from ischaemic heart disease (IHD) by verbal autopsy during follow-up over 10 years of a cohort comprising 20 757 rural residents from Bangladesh who used solid fuel for cooking or heating and 1 589 who used natural gas. Incidence rate ratios for use of solid fuel were below one, but the reduction in risk was not statistically significant. It is unclear whether and how potential confounders were taken into account.
Lee and colleagues26 asked about use of solid fuel and history of doctor-diagnosed CHD, as part of a cross-sectional survey of 13 438 adults in China. They found a positive association (OR 2.58, 95% CI: 1.53 to 4.32), but there was no consistent trend in risk with longer duration of using solid fuel. Moreover, the use of self-report to collect information about both exposure and disease may have led to bias (either inflationary because of differential reporting, or towards the null if there were non-differential errors in recall).
Another cross-sectional study collected information from 5949 households in India.20 It found a significant association between use of traditional fuels and CVD being ‘the most frequently occurring disease that was reported by at least one household member in the last three months’ (OR 1.39, 95% CI: 1.24 to 1.55). However, the health outcome and exact method of statistical analysis were poorly specified. It is unclear whether the adjustment for age took into account the ages of all household members, or just that of the individual who responded on behalf of the household, and whether and how allowance was made for differing sizes of households.
Complementing these findings from observational studies, McCracken et al. 21 reported a significantly lower prevalence of ST segment depression in electrocardiograms with use of an improved stove in an intervention study.
Heart rate
Three studies considered heart rate or its variability as an outcome. In a cross-sectional survey of 123 non-smoking women in Nicaragua, who were using traditional biomass stoves, heart rate was significantly higher among those with higher personal exposures to CO, and non-significantly elevated with higher indoor concentrations of PM2.5.19 In India, Dutta et al. 22 found a significantly higher prevalence of tachycardia (>100 beats per minute) in non-smoking women using biomass as compared with LPG for cooking (6.6% vs. 1.3%). On the other hand, McCracken and colleagues21 found no significant differences in heart rate variability with use of an improved stove in an intervention study in Guatemala.
Vascular pathology
Four cross-sectional studies have related IAP from biomass fuels to abnormalities of vascular structure or function. Two showed significant associations with higher carotid intima media thickness (CIMT),16,30 and one also with the prevalence of carotid plaque ascertained by ultrasound (OR 2.55, 95% CI: 1.08 to 5.98).30 Against this, a third study found no association with CIMT, although exposure was significantly related to reduced flow-associated dilatation and lower endothelium-independent vasodilatation of the brachial artery.17 In the fourth study, reported only as an abstract, flow-mediated dilatation of the brachial artery again tended to be lower in people using biomass fuels, especially if there was no chimney in the kitchen.32 However, only 9 of the total of 81 subjects were in the control group used for comparison.
Oxidative stress and inflammatory markers
Cross-sectional studies have also indicated that use of biomass fuel is associated with: increased generation of reactive oxygen species by leucocytes;18,22 reduction in erythrocyte superoxide dismutase;22,29 elevations in serum levels of interleukin-6,22,29 interleukin-822,29 and tumour necrosis factor-alpha;22,29 increases in platelet aggregation and expression of P-selectin by platelets;18 and higher serum concentrations of C-reactive protein (CRP).16,22 The last finding is supported by an intervention study in Nicaragua, in which change to a cleaner burning stove for cooking was associated with a significant reduction in CRP among obese women.23
Blood pressure
Blood pressure has been the most frequently studied cardiovascular outcome in research on IAP from solid fuels. Eight cross-sectional studies have found significant positive associations with higher BP12,30,35,37 or prevalence of hypertension14,18,22,26 (it is unclear whether there was overlap between the study samples for two of the reports18,22). Another found higher systolic and diastolic BPs in non-smoking indoor barbecue workers as compared with controls, although the differences (about 4mm Hg) were not significant.16 Furthermore, there was a significant reduction in BP with use of improved stoves in two intervention studies, one in Guatemala15 and the other in Bolivia.36 Against this, two cross-sectional surveys19,25 (one in children25) have failed to demonstrate significant associations with BP.
Lipid profile
The only study that examined lipid profiles found no significant associations with use of biomass fuel.16
Discussion
Our review confirms that the epidemiological literature on the relationship between IAP from solid fuel and CHD is limited but growing. Moreover, the research that has been conducted, although not yet conclusive, points to an effect that could be of major public health importance, given the continuing widespread use of biomass fuel in developing countries for cooking and heating, and their increasing incidence of CHD.
In conducting our review, we searched systematically for all papers that were relevant to our study question, and that met our specified inclusion criteria. For each report that was found, we identified any major limitations that were relevant to interpretation, but we did not attempt to score quality according a pre-specified scheme. The evidence base was limited and heterogeneous, and most relevant was not the quality of each study per se, but its implications for interpretation of the study's findings. The heterogeneity of studies—in the exposures compared, outcomes investigated and potentials for bias—meant also that there was no basis for any form of meta-analysis.
Most studies classified exposure according to whether solid (or biomass) fuel was used, or the time for which it had been used. However, others assessed risks in relation to measured exposures to specific pollutants, or following the introduction of stoves designed to reduce IAP. The merits of these alternative approaches will depend on the mechanisms (if any) by which IAP causes the outcomes under investigation. Among users of biomass fuels, there may be wide variations in personal exposures to pollutants, depending on, for example, the time for which a fire or stove is burning, the time spent on cooking and in the room where a fire is burning, and the design of the stove and house. Such distinctions will be lost when exposure is classified simply according to use of biomass fuel, such that risk estimates represent only a crude average. On the other hand, direct measurements of personal exposures to, or environmental concentrations of, pollutants may be misleading if levels vary over time and risk depends on longer term cumulative exposures. For the same reason, studies investigating short-term changes following the introduction of improved stoves will only detect impacts on outcome measures that are driven importantly by recent exposures.
We found only five studies that examined associations with CHD specifically. Two were relatively small case-control studies,24,31 one of which was reported only as an abstract.24 However, both found significant associations between use of biomass fuels and acute coronary syndrome in women, with adjusted odds ratios of 2.57 and 4.8. Another was a large cross-sectional survey in China, which relied on self-report of a doctor's diagnosis of CHD as its measure of outcome, and as a consequence may have been subject to inflationary bias.26 Nevertheless, it too indicated a positive association, with an odds ratio of 2.58. This was supported by the findings from a cohort study of mortality from myocardial infarction in China, which found a hazard ratio of 1.62 for prolonged use of coal as a fuel, but was reported only as an abstract.33 Against this, a cohort study in Bangladesh found no significant association between use of solid fuel for cooking or heating and mortality from IHD. However, cause of death was assessed by verbal autopsy, which although validated, is unlikely to have been completely accurate.28
A large cohort study in Iran found no significant associations between years of using biomass fuels for cooking or heating and death from heart disease more generally.27 As CHD accounts for a large proportion of deaths from heart disease, the broader case definition would not be expected to dilute risks substantially. However, from the limited abstract that was published, it is unclear how durations of exposure to different categories of fuel were related, and what proportion of the exposed subjects were still using biomass fuels at the time of recruitment to the study. It may be that recent exposures are a more important determinant of risk than those that occurred many years in the past.
Evidence for short-term effects on risk comes from the intervention study by McCracken and colleagues,21 which found differences in the prevalence of ST depression on the electrocardiogram at a relatively short interval after improved stoves were introduced.
A further investigation was also reported as indicating an association between use of traditional fuels and CVD,20 but the outcome measure was poorly specified, and the method of analysis inadequately described, making it difficult to draw any useful conclusions.
If IAP from combustion of solid fuel does cause CHD, then one mechanism could be through the stimulation of inflammatory processes that promote atherogenesis or susceptibility to thrombosis. In addition to the studies that have assessed risk of CHD or heart disease more generally, others have explored associations with inflammatory biomarkers, indicators of atherosclerosis or its early development (e.g. CIMT and flow-mediated dilatation), and measures of platelet aggregation. For the most part, these too have given positive results, and while there is a possibility of publication bias, such that positive results are preferentially reported, the balance of published evidence supports the generation of inflammation as a plausible mechanism for a hazard of CHD.
There is also a notable consistency of evidence for an association of IAP from biomass fuels with higher BP, which is a well-established risk factor for CHD. Ten studies have found significant positive associations,12,14,15,18,22,26,30,35–37 and another indicated a relationship, which although not significant, was of comparable magnitude.16 Only two studies have failed to find associations with BP,19,25 and one of them was in children.25
Conclusions
The current balance of epidemiological evidence points to an increased risk of CHD from IAP as a consequence of using solid, and especially biomass, fuels for cooking and heating. Relative risks from long-term exposure could be two- to fourfold. However, the evidence base is still limited, and although such an association is consistent with the known hazards from smoking, environmental tobacco smoke and ambient air pollution, and supported by evidence of effects on inflammatory processes, atherosclerosis and BP, it requires confirmation by larger and more robust studies. The need for such research is particularly pressing because the incidence of CHD in developing countries is rising, and IAP may interact synergistically with the risk factors that are driving that increase. Furthermore, relatively cheap methods are available to reduce IAP from use of solid fuels, and there are indications from intervention studies that these may impact beneficially on CHD as well as on other diseases caused by such pollution.
Acknowledgements
We thank Dr Clare Harris for her help in designing the strategy for the literature search. The study was conducted as part of the work for a PhD thesis by Dr Fatmi, who was funded through a fellowship provided by the Colt Foundation, UK.
References
- 1.Murray CJ, Vos T, Lozano R, et al. . Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2197–223. [DOI] [PubMed] [Google Scholar]
- 2.Bonjour S, Adair-Rohani H, Wolf J, et al. . Solid fuel use for household cooking: country and regional estimates for 1980–2010. Environ Health Perspect 2013;121:784–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Teo KK, Ounpuu S, Hawken S, et al. . Tobacco use and risk of myocardial infarction in 52 countries in the INTERHEART study: a case-control study. Lancet 2006;368:647–58. [DOI] [PubMed] [Google Scholar]
- 4.Yusuf S, Hawken S, Ounpuu S, et al. . Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004;364:937–52. [DOI] [PubMed] [Google Scholar]
- 5.Howard G, Thun MJ.. Why is environmental tobacco smoke more strongly associated with coronary heart disease than expected? A review of potential biases and experimental data. Environ Health Perspect 1999;107:853–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaur S, Cohen A, Dolor R, et al. . The impact of environmental tobacco smoke on women's risk of dying from heart disease: a meta-analysis. J Womens Health 2004;13:888–97. [DOI] [PubMed] [Google Scholar]
- 7.Dockery DW, Pope CA, Xu X, et al. . An association between air pollution and mortality in six US cities. N Engl J Med 1993;329:1753–9. [DOI] [PubMed] [Google Scholar]
- 8.Pope CA, Thun MJ, Namboodiri MM, et al. . Particulate air pollution as a predictor of mortality in a prospective study of US adults. Am J Respir Crit Care Med 1995;151:669–74. [DOI] [PubMed] [Google Scholar]
- 9.Clark ML, Peel JL, Balakrishnan K, et al. . Health and household air pollution from solid fuel use: the need for improved exposure assessment. Environ Health Perspect 2013;121:1120–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fullerton DG, Bruce N, Gordon SB.. Indoor air pollution from biomass fuel smoke is a major health concern in the developing world. Trans R Soc Trop Med Hyg 2008;102:843–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yamamoto SS, Phalkey R, Malik AA.. A systematic review of air pollution as a risk factor for cardiovascular disease in South Asia: limited evidence from India and Pakistan. Int J Hyg Environ Health 2014;217:133–44. [DOI] [PubMed] [Google Scholar]
- 12.Baumgartner J, Schauer JJ, Ezzati M, et al. . Indoor air pollution and blood pressure in adult women living in rural China. Environ Health Perspect 2011;119:1390–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baumgartner J, Zhang Y, Schauer JJ, et al. . Highway proximity and black carbon from cookstoves as a risk factor for higher blood pressure in rural China. PNAS 2014;111:13229–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ray MR, Mukherjee S, Roychoudhury S, et al. . Platelet activation, upregulation of CD11b/CD18 expression on leukocytes and increase in circulating leukocyte-platelet aggregates in Indian women chronically exposed to biomass smoke. Hum Exp Toxicol 2006;25:627–35. [DOI] [PubMed] [Google Scholar]
- 15.McCracken JP, Smith KR, Díaz A, et al. . Chimney stove intervention to reduce long-term wood smoke exposure lowers blood pressure among Guatemalan women. Environ Health Perspect 2007;115:996–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Davutoglu V, Zengin S, Sari I, et al. . Chronic carbon monoxide exposure is associated with the increases in carotid intima-media thickness and C-reactive protein level. Tohoku J Exp Med 2009;219:201–6. [DOI] [PubMed] [Google Scholar]
- 17.Buturak A, Genç A, Ulus ÖS, et al. . Evaluation of the effects of chronic biomass fuel smoke exposure on peripheral endothelial functions: an observational study. Anadolu Kardiyol Derg 2011;11:492–7. [DOI] [PubMed] [Google Scholar]
- 18.Dutta A, Mukherjee B, Das D, et al. . Hypertension with elevated levels of oxidized low-density lipoprotein and anticardiolipin antibody in the circulation of premenopausal Indian women chronically exposed to biomass smoke during cooking. Indoor Air 2011;21:165–76. [DOI] [PubMed] [Google Scholar]
- 19.Clark ML, Bazemore H, Reynolds SJ, et al. . A baseline evaluation of traditional cook stove smoke exposures and indicators of cardiovascular and respiratory health among Nicaraguan women. Int J Occup Environ Health 2011;17:113–21. [DOI] [PubMed] [Google Scholar]
- 20.Firdaus G, Ahmad A.. Indoor air pollution and self-reported diseases – a case study of NCT of Delhi. Indoor Air 2011;21:410–16. [DOI] [PubMed] [Google Scholar]
- 21.McCracken J, Smith KR, Stone P, et al. . Intervention to lower household wood smoke exposure in Guatemala reduces ST-segment depression on electrocardiograms. Environ Health Perspect 2011;119:1562–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dutta A, Ray MR, Banerjee A.. Systemic inflammatory changes and increased oxidative stress in rural Indian women cooking with biomass fuels. Toxicol Appl Pharmacol 2012;261:255–62. [DOI] [PubMed] [Google Scholar]
- 23.Clark ML, Bachand AM, Heiderscheidt JM, et al. . Use of dried blood spots to measure the impact of an indoor cookstove intervention on changes in systemic inflammation. Epidemiology 2012;23:S280. [Google Scholar]
- 24.Sathiakumar N. Indoor air pollution due to biomass fuel use and acute coronary syndrome among Sri Lankan women. Epidemiology 2012;23:S224. [Google Scholar]
- 25.Baumgartner J, Zhang Y, Schauer JJ, et al. . Household air pollution and children's blood pressure. Epidemiology 2012;23:641–642. [DOI] [PubMed] [Google Scholar]
- 26.Lee M-S, Hang J-Q, Zhang F-Y, et al. . In-home solid fuel use and cardiovascular disease: a cross-sectional analysis of the Shanghai Putuo study. Environ Health 2012;11:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mitter SS, Islami F, Pourshams A, et al. . Use of biomass fuels for cooking and heating is associated with increased non-communicable disease mortality: Golestan cohort study. Circulation 2012;125:AP042. [Google Scholar]
- 28.Alam DS, Chowdhury MAH, Siddiquee AT, et al. . Adult cardiopulmonary mortality and indoor air pollution: a10-year retrospective cohort study in a low-income rural setting. Glob Heart 2012;7:215–21. [DOI] [PubMed] [Google Scholar]
- 29.Banerjee A, Mondal NK, Das D, et al. . Neutrophilic inflammatory response and oxidative stress in premenopausal women chronically exposed to indoor air pollution from biomass burning. Inflammation 2012;35:671–83. [DOI] [PubMed] [Google Scholar]
- 30.Painschab MS, Davila-Roman VG, Gilman RH, et al. . Chronic exposure to biomass fuel is associated with increased carotid artery intima-media thickness and a higher prevalence of atherosclerotic plaque. Heart 2013;99:984–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fatmi Z, Coggon D, Kazi A, et al. . Solid fuel use is a major risk factor for acute coronary syndromes among rural women: a matched case control study. Public Health 2014;128:77–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pratali L, Cogo A.. Exposure to indoor air pollution induces endothelial dysfunction in Nepalese high altitude dwellers. High Alt Med Biol 2014;15:A241–2. [Google Scholar]
- 33.Kim C, Shu X-O, Hosgood HD, et al. . Past use of coal for cooking is associated with all-cause mortality in the prospective Shanghai women's health study. Cancer Res 2014;74:Abstract nr 2184. [Google Scholar]
- 34.Caravedo MA, Painschab MS, Davila-Roman VG, et al. . Lack of association between chronic exposure to biomass fuel smoke and markers of right ventricular pressure overload at high altitude. Am Heart J 2014;168:731–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Burroughs Peña M, Romero KM, Velazquez EJ, et al. . Relationship between daily exposure to biomass fuel smoke and blood pressure in high-altitude Peru. Hypertension 2015;65:1134–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alexander D, Larson T, Bolton S, et al. . Systolic blood pressure changes in indigenous Bolivian women associated with an improved cookstove intervention. Air Qual Atmos Health 2015;8:47–53. [Google Scholar]
- 37.Neupane M, Basnyat B, Fischer R, et al. . Sustained use of biogas fuel and blood pressure among women in rural Nepal. Environ Res 2015;136: 343–51. [DOI] [PMC free article] [PubMed] [Google Scholar]