Abstract
Background
Many details of the negative relationship between perceived racial/ethnic discrimination and health are poorly understood.
Purpose
The purpose of this study was to examine racial/ ethnic differences in the relationship between perceived discrimination and self-reported health, identify dimensions of discrimination that drive this relationship, and explore psychological mediators.
Methods
Asian, Black, and Latino(a) adults (N=734) completed measures of perceived racial/ethnic discrimination, self-reported health, depression, anxiety, and cynical hostility.
Results
The association between perceived discrimination and poor self-reported health was significant and did not differ across racial/ethnic subgroups. Race-related social exclusion and threat/harassment uniquely contributed to poor health for all groups. Depression, anxiety, and cynical hostility fully mediated the effect of social exclusion on health, but did not fully explain the effect of threat.
Conclusions
Our results suggest that noxious effects of race-related exclusion and threat transcend between-group differences in discriminatory experiences. The effects of race-related exclusion and threat on health, however, may operate through different mechanisms.
Keywords: Racism, Ethnic discrimination, Self-reported health, Health, Social exclusion, Meditation, Depression
Introduction
Racial or ethnic discrimination, defined as unfair treatment received because of one’s racial or ethnic characteristics [1–3], has been associated with a remarkable variety of negative mental and physical health outcomes, as well as negative health behaviors [4–7]. One of the most common physical health outcomes examined in this literature is self-reported general health status, or the overall appraisal of one’s physical health status. Self-reported health is of interest given its strong association with objective indices of physical health such as diagnoses of chronic disorders (e.g., diabetes [8], hypertension [9], and chronic respiratory diseases [10]) and the occurrence of acute life-threatening conditions (e.g., myocardial infarction and stroke) [9, 11].
The focus of this paper is on the health effects of perceived or self-reported racial or ethnic discrimination, which refers to race- or ethnicity-related maltreatment which the individual acknowledges and reports [4, 12–15]. In a search of Medline and PsycInfo conducted in June of 2009, we located 43 studies that examined the relationship between perceived racial or ethnic discrimination and self-reported health [14–56]. The findings across studies are fairly robust, with half the studies reporting a significant negative association between perceived discrimination and self-reported health [14, 18, 22–24, 28, 32–35, 37, 38, 40–42, 44, 46, 49, 51, 53, 56] and another 16 reporting partial or mixed evidence of such a relationship [15, 16, 19, 21, 26, 29–31, 36, 39, 43, 47, 48, 52, 54, 55]. Of the studies reporting partial support, nine found a significant negative relationship for a subset of demographic groups [16, 19, 21, 26, 29, 31, 36, 43, 52], and in three others the relationship was significant for only a subset of discrimination measures that were examined [39, 47, 54]. An additional four studies found a negative correlation between perceived discrimination and health, but reported that the effects did not remain significant when potential confounding or mediating variables (e.g., demographic characteristics, psychological distress, general stress) were controlled [15, 30, 48, 55]. Only five studies reported no relationship between perceived discrimination and self-reported health status [20, 25, 27, 45, 50].
Despite substantial supportive literature, three significant gaps remain in our understanding of the influence of perceived discrimination on self-reported general health. First, the extent to which the effects of perceived discrimination on self-reported health generalize across race/ethnic groups is not well understood. Variations in the health effects of perceived discrimination might be expected given sociocultural and historical differences among racial and ethnic groups. For example, the context in which discrimination is experienced for a given group is likely to be influenced by the forces driving immigration and affecting acculturation [57]. Many Black Americans, for instance, are the descendants of involuntary immigrants brought to the USA as slaves. Black Americans arguably remain the most stigmatized racial group in the USA and experience considerable residential segregation [6, 37, 58, 59]. Such segregation likely has a negative impact on health as communities with high concentrations of Black individuals tend to be more crowded, be located in lower income areas, have housing of a poorer quality, and to have fewer resources to support a healthy lifestyle [6, 60–62]. In contrast, many Latino and Asian Americans are voluntary immigrants or descendants of voluntary immigrants. Factors associated with the choice to migrate, including socioeconomic resources and sufficient emotional and physical health to meet the challenges of migration, may serve as unmeasured buffers of the effects of a social stressor, such as discrimination, on perceived health [63–65]. For some Latino individuals, particularly those from Puerto Rico, the ability to return to a place in which they form the majority may also offset the burden of discrimination in mainland USA. There are also significant differences in the types of stereotypical beliefs held about Black, Latino vs. Asian Americans [66], and this may translate into subtle differences in the discrimination experienced by members of these groups.
Although one might expect differences across groups in the health effects of discrimination for the reasons described, the existence of such differences has not been well studied. Most studies of discrimination and health have either examined the health effects of perceived discrimination for a single minority group [14, 15, 19, 21, 23, 25, 27, 39, 44, 45] or for multiple racial and ethnic groups combined into one sample [20, 22, 24, 30, 37, 40, 46, 47, 51, 55, 56]. Only a few studies have examined racial and ethnic differences in the relationship of perceived discrimination to self-reported health, and these have found the relationship to be non-significant or attenuated among Latino(a)s compared to Blacks, Whites, and/or other racial/ethnic groups [26, 29, 42, 52]. Three of these studies, however, used limited measures of discrimination consisting of only one to three items. In addition, Asian Americans, one of the fastest growing immigrant groups in the USA [67], have generally not been included in these comparative studies, so it is unknown how the experiences of this group compare to those of other groups.
Second, we do not have a full understanding of the types of perceived discrimination that are most closely associated with negative health outcomes. The type of discrimination, the context in which it occurs, and the degree to which it involves a socio-emotional vs. a physical threat can influence how one reacts to discrimination. For example, social exclusion of any type is well known to be depressogenic [68]. In contrast, physical threat and harassment may elicit anxiety or anger, producing a “fight or flight” response. In our prior work, we have demonstrated that different types of race/ethnicity-related discrimination were associated with different patterns of coping responses and with different indices of physical and mental health [13, 69–71]. For instance, individuals exposed to workplace discrimination reported suppressing anger in new situations, whereas those who were exposed to race/ethnicity-based social exclusion or harassment reported confronting others and aggressively expressing their feelings [71]. These findings suggest that different types of discrimination may produce different psychophysiological responses, which may ultimately result in different overall effects on health.
In the broader literature, however, the potential health effects of different types of perceived discrimination have not been well documented, in part because perceived discrimination has typically been treated as a single-dimensional construct. For example, among the studies of discrimination and self-reported health reviewed for this paper, ten used a single-item measure of perceived discrimination [20, 26, 29, 30, 34, 37, 38, 40, 49, 51] and 23 combined multiple items into overall perceived discrimination scores [14, 16–19, 21, 23–25, 27, 32, 36, 41–46, 48, 50, 52, 53, 56]. Some studies have found that particular types of perceived discrimination such as verbal abuse, physical attacks, and discrimination encountered in specific settings (i.e., work, the military, or medical settings) are negatively associated with self-reported health [28, 31, 35, 47, 72]. However, most of the research which has focused on differential effects associated with specific dimensions of racial discrimination has been done outside of the USA [28, 31, 35, 72], so it is unknown which particular types of discrimination are associated with health among minority groups in the USA.
Third, the psychophysiological mechanisms through which perceived discrimination influences self-reported health are not fully understood. There is substantial evidence that perceived discrimination is related to symptoms of depression and anxiety [5, 14, 19, 23, 31, 41, 44, 49, 54, 69, 73–78], both of which have negative implications for physical health [79–83]. The relationship between perceived discrimination and overall health is sometimes reduced or eliminated after controlling for measures of psychological distress [14, 15, 49]. Therefore, it is possible that greater perceived discrimination leads to decrements in self-reported physical health by increasing depression and anxiety and the psychophysiological changes that accompany such psychological distress. It is also possible that the stressors associated with discrimination or other adverse social conditions may exert effects on health through the development of underlying schemas about the world and the self. For example, exposure to discrimination may cultivate the tendency to interpret the behaviors of others as intentionally harmful, deceitful, and/or selfish (i.e., hostile attributions) and reinforce the belief that one’s efforts to change one’s circumstances are likely to be ineffective (i.e., cynicism) [69]. Cynicism and hostility have been independently associated with health status, particularly with indices of cardiovascular disease [84, 85]. Prior studies of perceived discrimination, including our own, have typically treated personality traits such as cynicism or hostility as confounding variables rather than as potential mediators [13, 69, 73, 86, 87]. However, given that adult levels of cynicism and hostility are at least partly shaped by childhood environmental circumstances [88], experiences of discrimination over one’s life could also cultivate these personality traits, which are then associated with poor health. Studies have shown that controlling for cynical hostility reduces, but does not eliminate, the association of perceived discrimination with nocturnal ambulatory blood pressure [87], negative affect [69], anger [73], and appraisals of social interactions [73]. Whether cynical hostility influences the association between perceived discrimination and self-reported health has not been previously examined.
In this study, we address existing gaps in the literature by examining racial/ethnic variation in the relationship between perceived discrimination and self-reported health in a community sample of Asian, Black, and Latino(a) adults. Second, we examine the types of race-related maltreatment associated with self-reported health by employing a multidimensional measure of perceived discrimination that assesses experiences of race- or ethnicity-based social exclusion, discrimination at work/ school, stigmatization, and threat or harassment [13]. Third, we examine whether the symptoms of depression, anxiety, and cynical hostility act independently or jointly as mediators of the relationship of perceived discrimination to health.
Method
Participants and Procedure
English-speaking individuals 18 years of age or older who self-identified as Asian, Black, or Latino(a) were recruited from a variety of locations in New York City, including a large urban university, community health facilities, community recreational centers, community health fairs, and religious organizations. Black and Latino(a) participants were drawn from a study of strategies used to cope with discrimination, and Asian participants were drawn from a study designed to validate the Perceived Ethnic Discrimination Questionnaire—Community Version (PEDQ-CV) in an Asian sample. The same types of recruitment sites and recruitment strategies were used for both studies, with the exception that more of the Asian participants were drawn from the university and from community health fairs. Both studies were reviewed and approved by the Institutional Review Boards of St. John’s University, Jamaica Hospital Medical Center, and Flushing Hospital Medical Center. No exclusion criteria were employed, with the exception that participants were asked if they were able to read and write English at a level that would permit them to complete the survey, which was written at an eighth grade reading level. After providing written consent, participants completed a questionnaire packet that contained measures of self-reported health status, perceived discrimination, depressive symptoms, anxiety, cynical hostility, and socio-demographic characteristics. Other measures were also included, but are not the focus of the current analysis. Participants received $10 and a St. John’s University mug as compensation for their participation.
Measures
Self-Reported General Health Status
Self-reported health was assessed with the MOS SF-36 general health scale (eight items) [89]. The items ask about perceptions of overall health, risk for future illness, and health in comparison to others. The scale is widely used in studies of perceived or self-reported general health [90]. The alpha in this sample was 0.80.
Perceived Discrimination
Perceived racial or ethnic discrimination was assessed with the PEDQ-CV Lifetime Exposure to Discrimination Scale [13]. This scale consists of 34 items that can be combined into a total score assessing lifetime exposure to discrimination. The PEDQ-CV Lifetime Exposure Scale also includes four subscales that assess different dimensions of discrimination, including experiences of social exclusion, stigmatization, discrimination at work/school, and threat/ harassment. Participants are asked how often they have had the experiences described in the items because of their ethnicity or race. Response options are presented on a five-point Likert scale, ranging from 1 (never) to 5 (very often). For the full sample, the alpha for the PEDQ-CV Lifetimes Exposure Scale was 0.95 and exceeded 0.94 for every group. Sample items (and alphas across the full sample for each subscale include: “How often have you been kept out of a public place or group?” (Social Exclusion, eight items, α=0.87); “How often have you been treated unfairly by co-workers or classmates?” (Workplace/School Discrimination, four items, α=0.76); “How often have others hinted that you must be violent or dangerous?” (Stigmatization, six items, α=0.84); “How often have others threatened to damage your property?” (Threat, four items, α=0.82). Alphas for the subscales exceeded 0.76 when examined by ethnic group. The PEDQ-CV has yielded evidence of reliability and validity in samples of Black and Latino adults, as well as in multi-ethnic samples of Asians [91, 92].
Depression and Anxiety
Symptoms of depression and anxiety were assessed with the SCL-90-R [93] depression and anxiety subscales. Items are presented on a five-point scale, ranging from 1 (not at all) to 5 (extremely). The SCL-90-R has been found to be a valid and reliable instrument for use with diverse populations that are represented in this study, including African Americans, Latino(a)s, Koreans, Chinese, and Filipinos [94, 95]. Alphas in this sample exceeded 0.91.
Cynical Hostility
We used 25 items from the MMPI-based Cook and Medley Hostility Scale (Ho) to measure cynical hostility. Specifically, we included the Hostile Attribution (12 items) and Cynicism (13 items) subscales developed by Barefoot et al. [96] who demonstrated the convergent and discriminant validity of these subsets [97]. These two scales reflect schemas likely to be affected by discrimination and have been shown to be related to perceived discrimination in our prior work [87]. The hostile attributions subscale tends to interpret the behavior of others as intended to harm the respondent, as reflected in suspicion, paranoia, and fear of threat to the self. The cynicism subscale represents a general negative view of the world and of people as being unworthy, deceitful, and selfish. Participants rate their agreement or disagreement with each of the items on a six-point scale as recommended by Weidner et al. [98]. To provide an index of cynical hostility, we combined responses to these two measures into a single score (α=0.86).
Socio-demographics
Participants were asked to respond to items regarding their gender; age (in years); student status (yes or no); highest level of education completed (less than high school diploma, high school diploma or GED, or college degree); marital status (single or not); employment status (not working vs. working full-time or part-time); and place of birth (US-born or foreign-born). Participants who self-identified as Black or African American, Asian, or Latino (a) on a measure of ethnicity were included in this analysis. Participants also provided a response to an open-ended question about their specific racial or ethnic group, and these responses were used to identify the specific ethnic subgroups that comprised the larger groups of Black/ African Americans, Asians, or Latino(a)s.
Analyses
Race and ethnic differences in socio-demographic characteristics were tested using chi-square analyses for categorical variables and analysis of variance (ANOVA) for continuous variables. A series of ANOVAs were then conducted to examine whether there were socio-demographic variations in the total perceived discrimination score and self-reported health for the purpose of identifying covariates to include in subsequent analyses. Based on those analyses, subsequent analyses were conducted both with and without age, gender, student status, employment status, education level, and place of birth as covariates.
Race and ethnic differences in the total lifetime exposure to discrimination score, the four subscales, the psychological mediators, and self-reported health were examined using ANOVA. Post hoc Scheffe analyses were conducted to determine whether Asian–Black, Asian–Latino(a), and Black–Latino(a) differences were significant.
We used linear regression to examine the association of perceived discrimination with self-reported health and to evaluate any racial/ethnic differences in these effects. When testing interactions between race/ethnic group and perceived discrimination, discrimination scores were centered and race/ethnicity was dummy coded. Latino(a)s were chosen as the reference group given that prior studies have found the relationship between perceived discrimination and health to be attenuated for this group [26, 29, 42, 52]. To determine whether specific aspects of perceived discrimination were associated with self-reported health, we repeated the analyses described above, but replaced the lifetime exposure score with the set of four subscale scores (i.e., social exclusion, workplace discrimination, stigmatization, and threat/harassment).
To test whether depression, anxiety, and/or cynicism mediated the relation of perceived discrimination to self-reported health, we conducted a test of multiple mediation using bootstrapping procedures recommended by Preacher and Hayes [99]. This multiple mediator approach permits examination of the combined effects of the mediators as well as the unique effects of each mediator, controlling for the contributions of the others. It also allows the magnitude of the effects of each mediator to be compared through pairwise comparisons. This analytic approach reduces the likelihood of potentially important variables being omitted from a test of any given mediator. The bootstrap method does not assume that sampling distributions for direct and mediated (i.e., indirect) effects of variables are normal. Instead, the bootstrap method involves drawing a specified number of samples from the original sample (with replacement) so that the sampling distributions of the effects can be approximated. Point estimates and percentile bootstrap confidence intervals for the effects of interest are then derived from the bootstrap analyses. Calculating the confidence intervals using two methods designed to correct for potential bias (i.e., bias-corrected and bias-corrected accelerated) yielded equivalent results, so we report the original percentile bootstrap confidence intervals in this paper.
Using the bootstrap method, we examined the total direct effect of lifetime exposure to discrimination on self-reported health, as well as the indirect (i.e., mediated) effects through each of the proposed mediators (i.e., depression, anxiety, and cynical hostility), separately and in combination. We also conducted pairwise comparisons of the mediated effects to determine whether there were significant differences in the extent to which depression, anxiety, and/or cynical hostility mediated the effect of perceived discrimination on health. We conducted these analyses with and without the covariates to determine whether adding the covariates changed the results. In addition, because the SCL90-R subscales were skewed, we subjected the scores to a square root transformation which improved skewedness. We ran analyses using both transformed and untransformed scores. Since the results did not change in substance using untransformed scores, we report those here. Finally, we repeated all analyses for each of the discrimination subscales that were found to be independently associated with self-reported health. These analyses were performed using algorithms provided by Preacher and Hayes [100] and using SAS (SAS Institute). To determine whether there were race/ethnicity differences in the mediating effects of these psychological variables, we employed the tests of moderated mediation recommended by Preacher et al. [101] in which race/ethnicity (Asian, Black, or Latino(a) served as the moderator. We employed the algorithms available from http://www.quantpsy.org using SPSS and conducted additional follow-up analyses employing SAS GLM procedures.
Results
Sample Characteristics
The sample included 341 Asian (46%), 260 Black (35%), and 133 Latino(a) (18%) participants over the age of 18 (Table 1). The largest Asian subgroups included individuals of Chinese (n=107, 31%), Indian (n=119, 35%), Filipino (n=38, 11%), and Korean (n=28, 8%) descent; the largest Black subgroups included individuals who identified African American (n=82, 32%), Black (n=22, 8%), Jamaican (n=56, 21%), and Haitian (n=40, 15%); and the largest Latino(a) subgroups included individuals of Puerto Rican (n=53, 50%), Dominican (n=25, 19%), and Ecuadorian (n=9, 7%) descent. Participants ranged in age from 18 to 84 years (mean=28.40, SD=12.70), and 529 (72%) were women. More than half of the participants (n=446, 61%) were students. Overall, 95% of the sample had at least a high school education. Most (n=481, 66%) were currently employed full- or part-time. Among students, 60% (n=267) were employed either full- or part-time. A total of 56% (n=408) of the sample was born in the USA.
Table 1.
Demographic characteristics, perceived discrimination, self-reported health, and psychological mediators for the full sample and by racial/ethnic group
| Variable | Full sample (n=734) | Asian (n=341) | Black (n=260) | Latino(a) (n=133) | p valuea |
|---|---|---|---|---|---|
| Gender (women), n (%) | 529 (72.07) | 234 (68.6) | 197 (75.77) | 98 (73.68) | <0.14 |
| Student, n (%) | 446 (60.76) | 258 (75.66)a | 122 (46.92)b | 66 (49.62)b | <0.001 |
| Education, n (%) | <0.001 | ||||
| Less than high school | 39 (5.31) | 5 (1.47)a | 21 (8.08)b | 13 (9.77)b | |
| High school diploma | 499 (67.98) | 224 (65.69) | 183 (70.38) | 92 (69.17) | |
| College degree or better | 196 (26.70) | 112 (32.84) | 56 (21.54) | 28 (21.05) | |
| Full- or part-time employed, n (%) | 481(66.34) | 212(63.10) | 174(67.18) | 95(73.08) | <0.12 |
| Married, n (%) | 149 (20.55) | 64 (18.99) | 54 (21.01) | 31 (23.66) | <0.52 |
| Born in the USA, n (%) | 408 (55.59) | 157 (46.04)a | 158 (60.77)b | 93 (69.92)b | <0.001 |
| Mean age (SD) | 28.40 (12.70) | 25.62(11.52)a | 31.43(13.41)b | 29.57(12.72)b | <.001 |
| Lifetime exposure | 1.81 (0.63) | 1.66 (0.55)a | 1.98 (0.67)b | 1.85 (0.63)b | <0.001 |
| PEDQ subscales | |||||
| Social exclusion | 2.17 (0.76) | 2.00 (0.69)a | 2.37 (0.78)b | 2.23 (0.77)b | <0.001 |
| Workplace/school discrimination | 1.88 (0.82) | 1.70 (0.71)a | 2.06 (0.89)b | 1.99 (0.85)b | <0.001 |
| Stigmatization | 1.58 (0.69) | 1.46 (0.59)a | 1.69 (0.75)b | 1.66 (0.76)b | <0.001 |
| Threat/harassment | 1.50 (0.69) | 1.48 (0.66) | 1.54 (0.72) | 1.44 (0.72) | <0.33 |
| MOS self-reported health | 3.84 (0.76) | 3.81 (0.73) | 3.83 (0.80) | 3.95 (0.79) | <0.55 |
| Depressive symptoms | 1.94 (0.78) | 1.94 (0.72) | 1.95 (0.82) | 1.94 (0.85) | <0.99 |
| Anxiety symptoms | 1.76 (0.78) | 1.78 (0.73) | 1.70 (0.81) | 1.80 (0.87) | <0.37 |
| Cynical hostility | 0.50 (0.21) | 0.47 (0.21)a | 0.54 (0.20)b | 0.49 (0.20)a,b | <0.001 |
Different letters indicate significant (p<0.05) between-group differences identified using post hoc contrasts PEDQ-CV Perceived Ethnic Discrimination Questionnaire—Community Version
p values are for comparisons across race and ethnic groups using analysis of variance of continuous measures and χ2 for categorical variables
As shown in Table 1, there were no differences among the three race/ethnicity groups in gender, employment status, or marital status. However, there were significant racial/ethnic group differences in age, student status, education, and place of birth. Compared to Black or Latino(s) participants, Asian participants were more likely to be students, had more education, were less likely to be born in the USA, and were significantly younger. These socio-demographic differences were in part a function of ethnicity-related differences in recruitment as more Asians were recruited at the university site than the community or medical center sites.
Socio-demographic Variations in Perceived Discrimination and Self-Reported Health
Analyses on total lifetime exposure to perceived discrimination revealed significant effects of gender (F(1,732)=25.62, p< 0.001), education level (F(2,731)=12.39, p<0.0001), and place of birth (F(1,732)=17.98, p<0.0001). In comparison to women (mean=1.74), men (mean=1.99) reported more lifetime discrimination. Those with a college degree (mean= 1.63) reported significantly less discrimination than those with either a high school diploma (mean=1.86) or less than a high school education (mean=2.02). Participants born outside the USA (mean=1.70) reported less discrimination than those born in the USA (mean=1.90). Perceived discrimination did not differ for students and non-students (p>0.44) or for employed vs. unemployed individuals (p>0.59) and was not correlated with age (p>0.12).
Analyses of self-reported health revealed significant education-level differences (F(2,731)=11.28, p<0.001), such that those with a college degree (mean=4.03) reported significantly better health than either those with a high school diploma (mean=3.79) or less than a high school education (mean=3.50). Those who were employed full- or part-time reported better health (mean=3.91) than those who were unemployed (mean=3.70; F(1,723)=11.78, p<0.001). There were no effects of gender (p>0.90), age (p>0.48), student status (p>0.44), or place of birth (p>0.11) on self-reported health.
Race/Ethnicity Differences in Perceived Discrimination, Self-Reported General Health, and Psychological Mediators
Table 1 displays the uncorrected mean scores on the lifetime exposure to discrimination measure, the four discrimination subscales, and self-reported health for the full sample and for each race/ethnic group. There were significant racial/ethnic group differences in total lifetime exposure, as well as in social exclusion, workplace/school discrimination, and stigmatization subscale scores. Specifically, Asian participants reported significantly less lifetime exposure than did either Black or Latino(a) participants. These differences persisted even when controlling for age, gender, education level, student status, employment status, and place of birth. There were no racial/ethnic group differences in scores on the threat subscale. It is worth noting that although the mean levels of threat were relatively low overall, 53% of the Asian participants, 54% of the Black participants, and 44% of the Latino(a) participants had experienced race-related threat and harassment over the course of their lifetimes at least occasionally.
There were no racial/ethnic group differences in self-reported health (see Table 1). Controlling for age, gender, education level, student status, employment status, and place of birth did not change these results.
There were no significant racial/ethnic group differences in symptoms of depression or anxiety. There were significant differences in cynical hostility, with post hoc analyses indicating that Black individuals obtained significantly higher scores than Asians (p<0.001) and tended to have higher scores than Latino(a)s (p<0.06). These results were unchanged when controlling for the covariates.
Associations of Perceived Discrimination with Self-Reported Health
Lifetime Exposure to Discrimination
As shown in Table 2, there was a significant association of lifetime exposure to discrimination with overall self-reported health in the full sample, with perceived discrimination explaining 7% of the variance. The effect of perceived discrimination remained significant when race, age, gender, place of birth, student status, employment status, and education level were controlled. In analyses stratified by race/ethnic group, the relationship of perceived discrimination to self-reported health was significant for every group, both with and without adjustment for the covariates (see Table 2). Interactions between race/ethnic group and perceived discrimination tested in the full sample were not significant, indicating that the association of perceived discrimination with health did not differ significantly among Asians, Blacks, and Latino(a)s. The coefficients for the interactions were quite small (−0.09 and −0.14), as shown in Table 2.
Table 2.
Regression analyses testing relationship of perceived lifetime exposure to discrimination to self-reported health for the full group and for each racial/ethnic group
| Unadjusted models
|
Adjusted models
|
|||||||
|---|---|---|---|---|---|---|---|---|
| B | SE | Beta | Partial R2 | B | SE | Beta | Partial R2 | |
| Full sample, no race interactions | ||||||||
| Lifetime exposure to discrimination | −0.33 | 0.04 | −0.27*** | 0.07 | −0.34 | 0.05 | −0.28*** | 0.07 |
| Full sample, with race interactions | ||||||||
| Lifetime exposure to discrimination | −0.26 | 0.10 | −0.21** | 0.01 | −0.25 | 0.10 | 0.20** | 0.01 |
| L-A contrast | −0.15 | 0.08 | −0.10* | 0.01 | −0.21 | 0.08 | −0.14** | 0.01 |
| L-B contrast | −0.02 | 0.08 | −0.01 | 0.00 | −0.04 | 0.08 | −0.02 | 0.00 |
| Discrimination × L-A | −0.14 | 0.12 | −0.07 | 0.00 | −0.14 | 0.12 | −0.07 | 0.00 |
| Discrimination × L-B | −0.09 | 0.12 | −0.05 | 0.00 | −0.11 | 0.12 | −0.06 | 0.00 |
| Lifetime exposure to discrimination in models stratified by racial/ethnic group | ||||||||
| Asian | −0.40 | 0.08 | −0.30*** | .09 | −0.38 | 0.07 | −0.29*** | 0.08 |
| Black | −0.36 | 0.07 | −0.30*** | .09 | −0.34 | 0.07 | −0.29*** | 0.08 |
| Latino(a) | −0.26 | 0.11 | −0.21* | .04 | −0.24 | 0.11 | −0.19* | 0.03 |
Adjusted models included race, age, gender, place of birth, education, employment status, and student status
L-A Latino–Asian contrast, L-B Latino–Black contrast, Discrimination × L-A interaction term between lifetime exposure to discrimination and the Latino–Asian contrast, Discrimination × L-B interaction term between lifetime exposure to discrimination and the Latino–Black contrast
p<.05,
p<.01,
p<.001
Potential Moderators
Employment, student status, and place of birth may all affect the context in which discrimination is experienced and consequently affect the association of perceived discrimination to health. Although we included these variables as covariates in our previous analyses, we also tested them as potential moderators of the association of perceived discrimination to health. Tests of the interaction of employment status (p>0.67), student status (p>0.79), and age (a variable closely associated with student status) with perceived discrimination on health were not significant (p>0.20). The interaction of place of birth with perceived discrimination also failed to reach significance (B=0.17, SE=0.09, t=1.91, p<0.06).
Types of Discrimination
Analyses examining the association of discrimination subscales with self-reported health are reported in Table 3. Analyses indicated that social exclusion and threat contributed unique variance to the prediction of self-reported health, even when all covariates were added to the equation. The remaining two subscales, workplace/school discrimination and stigmatization, were not significantly associated with self-reported health. None of the interactions between racial/ethnic group and each of the subscales were significant (analyses not shown; betas for the interactions ranged from −0.08 to 0.02, p values ranged from 0.19 to 0.89), suggesting that the effects of each subscale on self-reported health did not differ significantly among Asians, Blacks, and Latino(a)s.
Table 3.
Regression analyses testing relationship of discrimination subscales to self-reported health for the full sample, all subscales entered simultaneously
| Unadjusted models
|
Adjusted models
|
|||||||
|---|---|---|---|---|---|---|---|---|
| B | SE | Beta | Partial R2 | B | SE | Beta | Partial R2 | |
| Social exclusion | −0.14 | 0.06 | −0.14* | 0.01 | −0.14 | 0.06 | −0.14* | 0.01 |
| Workplace/school discrimination | −0.04 | 0.05 | −0.04 | 0.00 | −0.06 | 0.05 | −0.06 | 0.00 |
| Stigmatization | −0.00 | 0.06 | −0.00 | 0.00 | −0.01 | 0.06 | −0.01 | 0.00 |
| Threat/harassment | −0.15 | 0.05 | −0.14* | 0.01 | −0.14 | 0.05 | −0.13* | 0.01 |
Adjusted models included race, age, gender, place of birth, education, employment status, and student status. None of the interactions of race/ ethnicity by subscale were significant (all p>0.19)
p<.05,
p<.01,
p<.001
Mediation Analyses
In these analyses, we are testing the degree to which symptoms of depression, symptoms of anxiety, and cynical hostility serve as mediators of the relationship of perceived discrimination to health. The three mediators are intercorrelated. Depressive and anxious symptoms are highly correlated (r=0.84, p<0.0001). Cynical hostility is moderately correlated with both symptoms of depression (r=0.34, p<0.001) and anxiety (r=0.36, p< 0.001). Given potential concerns about multicollinearity, we examined the effects of each mediator both separately and jointly to aid interpretability.
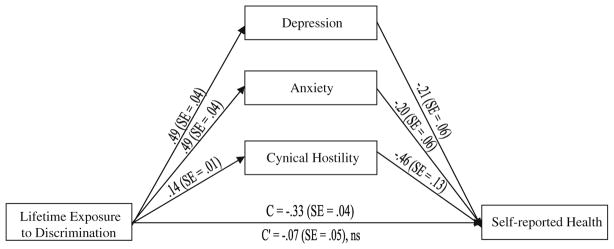
Including the covariates in the multiple mediation models did not change the outcome of the analyses, so we report only the results from models that excluded the covariates. As shown in Fig. 1, the total effect of lifetime exposure to discrimination on self-reported health (C=−0.33, SE=0.04, p<0.001) was reduced to non-significance (C'=−0.07, SE= 0.05, p<0.14) after accounting for the combined meditational effects of depression, anxiety, and cynical hostility. Depression, anxiety, and cynical hostility were all positively associated with discrimination and negatively associated with self-reported health. Estimates of the indirect effects of discrimination on self-reported health through each of the mediators are provided in Table 4. The total indirect effect is significant, indicating that, together, depressive symptoms, anxiety, and cynical hostility mediate the effect of perceived discrimination on general health. The combination of mediators accounts for about 79% of the variance in the relationship between total lifetime exposure to discrimination and self-reported health. An examination of the indirect effects of lifetime discrimination through each of the specific mediators indicates that depressive symptoms, anxiety symptoms, and cynical hostility all serve as mediators. None of the pairwise contrasts of the indirect effects (i.e., depression vs. anxiety; depression vs. cynical hostility, and anxiety vs. cynical hostility) were significant, suggesting that there are no significant differences in the mediating effects of depression, anxiety, and cynical hostility in the relationship of lifetime discrimination to self-reported health.
Fig. 1.
Model testing depression, anxiety, and cynical hostility as multiple mediators of the association between lifetime exposure to discrimination and self-reported health. The numbers provided for each path are regression coefficients and standard errors (SE) derived from a bootstrap procedure. C represents the total effect of lifetime exposure to discrimination on self-reported health. C' represents the direct effect of lifetime exposure to discrimination on self-reported health after accounting for the effects of the mediators. All paths are significant at p<0.001, except C' which is non-significant (ns)
Table 4.
Mediation of the effect of perceived discrimination (total lifetime exposure, social exclusion, and threat/harassment) on self-reported health through depression, anxiety, and cynical hostility
| Point estimate | Product of coefficients
|
Percentile 95% CI
|
|||
|---|---|---|---|---|---|
| SE | Z | Lower | Upper | ||
| Lifetime exposure | |||||
| Indirect effects | |||||
| Depression | −0.1036 | 0.0302 | −3.4303 | −0.1696 | −0.0455 |
| Anxiety | −0.0973 | 0.0304 | −3.2036 | −0.1627 | −0.0364 |
| Cynical hostility | −0.0647 | 0.0195 | −3.3172 | −0.1032 | −0.0271 |
| Total | −0.2656 | 0.0294 | −9.0395 | −0.3346 | −0.2125 |
| Contrasts | |||||
| Depression vs. anxiety | −0.0064 | 0.0555 | −0.1147 | −0.1324 | 0.0992 |
| Depression vs. cynical hostility | −0.0390 | 0.0363 | −1.0752 | −0.1173 | 0.0355 |
| Anxiety vs. cynical hostility | −0.0326 | 0.0374 | −0.8723 | −0.1129 | 0.0443 |
| Social exclusion | |||||
| Indirect effects | |||||
| Depression | −0.0864 | 0.0252 | −3.4337 | −0.1505 | −0.0388 |
| Anxiety | −0.0796 | 0.0245 | −3.2537 | −0.1355 | −0.0274 |
| Cynical hostility | −0.0546 | 0.0159 | −3.4411 | −0.0874 | −0.0260 |
| Total | −0.2205 | 0.0242 | −9.1020 | −0.2713 | −0.1746 |
| Contrasts | |||||
| Depression vs. anxiety | −0.0068 | 0.0453 | −0.1492 | −0.1111 | 0.0928 |
| Depression vs. cynical hostility | −0.0318 | 0.0299 | −1.0647 | −0.0989 | 0.0275 |
| Anxiety vs. cynical hostility | −0.0251 | 0.0303 | −0.8272 | −0.0964 | 0.0424 |
| Threat/harassment | |||||
| Indirect effects | |||||
| Depression | −0.0647 | 0.0194 | −3.3329 | −0.1115 | −0.0245 |
| Anxiety | −0.0626 | 0.0213 | −2.9333 | −0.1109 | −0.0218 |
| Cynical hostility | −0.0376 | 0.0117 | −3.2164 | −0.0609 | −0.0141 |
| Total | −0.1648 | 0.0218 | −7.5626 | −0.2160 | −0.1192 |
| Contrasts | |||||
| Depression vs. anxiety | −0.0022 | 0.0360 | −0.0600 | −0.0868 | 0.0767 |
| Depression vs. cynical hostility | −0.0271 | 0.0227 | −1.1942 | −0.0812 | 0.0207 |
| Anxiety vs. cynical hostility | −0.0250 | 0.0249 | −1.0037 | −0.0828 | 0.0268 |
CI confidence intervals generated based on 1,000 bootstrap samples
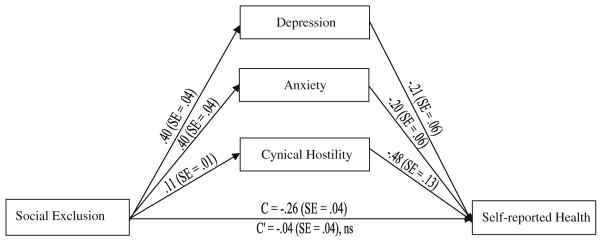
We conducted tests of multiple mediation for the social exclusion and threat subscales as these were both found to be associated with self-reported health in the regression analyses. As shown in Fig. 2, the total effect of social exclusion on self-reported health (C=−0.26, SE=0.04, p< 0.001) was reduced to non-significance (C'=−0.04, SE= 0.04, p<0.28) after accounting for the combined meditational effects of depression, anxiety, and cynical hostility. Depression, anxiety, and cynical hostility were all positively associated with social exclusion and negatively associated with self-reported health. The total indirect effect was significant (see Table 4), indicating that the combination of depression, anxiety, and cynical hostility mediates the effect of social exclusion on self-reported health, and the indirect effects of depressive symptoms, anxiety, and cynical hostility were each significant. Together, the three mediators account for about 84% of the relationship of social exclusion to self-reported health, and the pairwise contrasts of the indirect effects were not significant.
Fig. 2.
Model testing depression, anxiety, and cynical hostility as multiple mediators of the association between the social exclusion dimension of discrimination and self-reported health. The numbers provided for each path are regression coefficients and standard errors (SE) derived from a bootstrap procedure. C represents the total effect of exclusion on self-reported health. C' represents the direct effect of exclusion on self-reported health after accounting for the effects of the mediators. All paths are significant at p<0.001, except C' which is non-significant (ns)
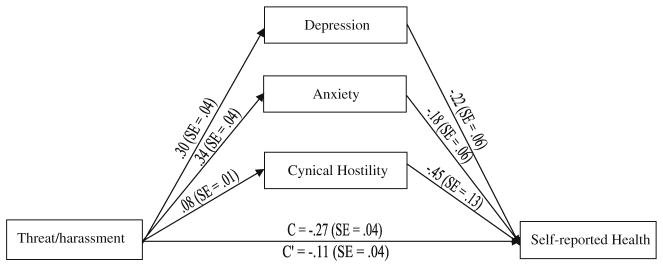
A similar pattern of results was observed when race-related threat served as the independent variable. However, the mediators did not fully account for the relationship between threat and self-reported health. As shown in Fig. 3, the total effect of threat on self-reported health was still significant (C'=−0.11, SE=0.04, p<0.01) after accounting for the combined meditational effects of depression, anxiety, and cynical hostility. The significant total indirect effect of the combined mediators (see Table 4) indicates that depression, anxiety, and cynical hostility partially mediate the relationship, with the combined mediators accounting for about 62% of the variance in the relationship. Each indirect effect was significant, and none of the contrasts among the mediators was significant.
Fig. 3.
Model testing depression, anxiety, and cynical hostility as multiple mediators of the association between threat/harassment dimension of discrimination and self-reported health. The numbers provided for each path are regression coefficients and standard errors (SE) derived from a bootstrap procedure. C represents the total effect of threat/harassment on self-reported health. C' represents the direct effect of threat/harassment on self-reported health after accounting for the effects of the mediators. All paths are significant at p<0.001
Finally, we tested the degree to which racial/ethnic group moderated the mediating role of depression, anxiety, and cynical hostility on perceived health. In these analyses, the mediators were tested individually. We performed the analyses as specified by Preacher and Hayes [100] to determine whether race/ethnicity moderated the path from the independent variable (i.e., lifetime exposure or one of the subscales) to any of the mediators and/or from the mediators to the dependent variable (i.e., general health). Race/ethnicity did not moderate the mediating effects of depression or anxiety or cynicism (all CI included 0) when lifetime exposure or race-related social exclusion was the independent variable.
When the results were repeated with race-related threat serving as the independent variable, race/ethnicity significantly moderated the relationship of race-related threat to depression, but not to anxiety or cynical hostility; the relationship is twice as strong for Latinos (B=0.51) as it is for Asians (B=0.24) and Blacks (B=0.25; F(2,727)=3.77, p<0.04). This, in turn, made the mediated effect, through depression, of race-based threat on general health twice as strong for Latinos as for the other two groups, with depression accounting for almost 100% of the association between race-based threat and general health in Latinos, 44% in Asians, and only 30% in Blacks (a non-significantly smaller percentage for Blacks than Asians because the overall association between race-based threat and general health is non-significantly larger for Blacks than Asians).
Discussion
The goal of this study was to clarify the nature of the relationship between perceived racial or ethnic discrimination and self-reported health. First, we examined variations by race/ethnicity in the association between perceived discrimination and self-reported health in a sample of Asian, Black, and Latino(a) individuals. Few prior studies have directly compared the association of perceived discrimination with health across multiple race and ethnic groups, and Asians have not been included in such comparative studies [26, 29, 42, 52]. We found that perceived discrimination was significantly associated with self-reported health in the overall sample and accounted for 7% of the variance. The magnitude of the association did not differ significantly across Asian, Black, and Latino(a) subgroups. The size of the effect we observed is comparable to or larger than the size of effects reported in studies in which we could make direct comparisons between standardized estimates or correlation coefficients [14, 30, 31, 42, 44, 49, 54].
A handful of studies have found smaller effects of perceived discrimination on health for Latino(a)s than for Blacks [26, 29, 42, 52]. In our study, the effects in the Latino(a) sample, although smaller, were not statistically different from those seen in the other groups. The finding of racial and ethnic variations in the health effects of perceived discrimination found in prior studies may be due, in part, to the use of measures that are less sensitive to the experiences of some groups over others. Williams and Mohammed [6] have highlighted the importance of using measures of discrimination that accurately and completely assess discrimination as it is likely to be experienced by a given group, or differences in responses may reflect measurement error rather than actual differences in discrimination experiences. We assessed perceived discrimination using the PEDQ-CV, a multidimensional measure that is appropriate for making comparisons across groups, as there is evidence of its reliability and validity in Asian, Black, and Latino(a) samples [13, 92, 93] and among college students and community-dwelling adults [13].
Our use of the PEDQ-CV allowed us to examine how specific dimensions of discrimination, including race/ ethnicity-based social exclusion, workplace/school discrimination, stigmatization, and threat or harassment, were related to self-reported health. To our knowledge, this is the first study that has examined the effects of these dimensions of discrimination on the self-reported health of racial and ethnic minority groups in the USA. Across all racial/ethnic groups in this study, social exclusion and threat/harassment were the two dimensions of discrimination that made unique contributions to poor self-reported health, while stigmatization and workplace/school discrimination were not uniquely associated with health when all four subscales are entered simultaneously.
These findings are consistent with a study by Jaskinkaja-Lahti et al. [31] of individuals from different ethnic groups living in Finland. They report that measures of everyday discrimination were negatively associated with perceived health across their sample, and the size of the relationship was similar to that seen in our sample. The everyday discrimination measure included items assessing experiences of social exclusion, stigmatization, and threat. In analyses conducted using a separate measure of workplace discrimination, the authors found a much smaller, or depending on the ethnic subgroup, an inverse relationship with a measure of perceived health.
In the current study, the specific effects of workplace discrimination on self-reported health were not significant after controlling for the effects of social exclusion, stigmatization, and threat. It may be the case that the harm specifically associated with experiences of discrimination at work is offset by the social and economic benefits of employment. The coping strategies used to manage different types of discriminatory experiences may also vary and therefore account for different patterns of psychophysiological response to threats to achievement (i.e., discrimination at work) vs. threats to belonging (i.e., race-related social exclusion) or safety (i.e., race-related threat) [71].
The results of our mediational analyses provide evidence that different dimensions of discrimination may affect health through multiple pathways. As expected, the effects of race-related social exclusion on self-reported health were fully mediated by depression, anxiety, and cynical hostility. These findings are consistent with research on the psychological effects of all types of social exclusion/ostracism [102]. However, these psychological variables did not fully mediate the effects of race-related threat on self-reported health and suggest that additional biobehavioral mechanisms may be at work. One possibility is that race-related threat evokes compensatory behaviors (e.g., remaining indoors, avoiding public places) that have an independent effect on health-related behaviors (e.g., participation in recreational activities). This notion is consistent with other data suggesting that perceptions of neighborhood safety are associated with participation in physical activity [103]. Further research will be required to test this and related hypotheses.
Finally, we examined in this study whether race/ethnicity moderated the relationships of perceived discrimination to self-reported health or moderated the mediating effects of depression, anxiety, and/or cynical hostility. We found that race/ethnicity did not moderate the overall relationship of lifetime exposure or race-related social exclusion or threat to self-reported health. Specifically, although the estimates of the effects of perceived discrimination on health appeared to be somewhat smaller for Latino(a)s in analyses stratified by racial/ethnic group, tests of the interactions of race/ethnicity with perceived discrimination (or social exclusion) revealed that race/ethnicity differences among groups were not significant. Post hoc analyses to determine whether we had sufficient power to detect race/ethnicity differences in our study sample indicated that we had 80% power to detect an interaction effect of 0.34 or larger. If the magnitude of the interaction effect in the population was the size of the interaction effects obtained in the present study, we estimate that we would need a sample size of over 4,500 individuals in order to have 80% power to detect significant differences across race and ethnic groups (at p< 0.05). This suggests that the magnitude of any observed effects is very small and that similarities among groups in their response to race- and ethnicity-related maltreatment is more important than the variations among groups. We interpret this to mean that the noxious elements of perceived discrimination have generalized effects across racial/ethnic groups.
We also found in our study that race/ethnicity did not moderate the mediating effects of depression, anxiety, and cynical hostility in the relationship of either lifetime perceived discrimination or social exclusion to self-reported health. However, we did find some evidence that race/ethnicity moderates the mediating role of depression in the relationship of race-related threat to general health. Depression partly mediates the relationship of race-related threat to general health for all groups, but the effects are stronger for Latino(a) than for Black or Asian individuals. It is important to note that our Latino(a) sample was largely composed of individuals of Puerto Rican and Dominican descent. Our findings may not generalize across other ethnic subgroups within the Latino(a) population. A larger and more ethnically diverse sample would permit clarification of subtle group differences in the effects of discrimination on self-reported health. Future research, including qualitative studies, will also be needed to understand the circumstances in which individuals are experiencing race-related threat to understand racial/ethnic differences in the psychological sequelae of these exposures.
Several limitations of the study should be noted. Most importantly, we employed convenience sampling and not population-based recruitment. Consequently, we cannot determine if between-group differences in levels of exposure to racial or ethnic discrimination or in the relationship of discrimination to health would also emerge in population-based samples. We recruited from a wide variety of locations, but our Asian sample was more likely to be recruited from university vs. community settings. Overall, slightly more than half the sample was recruited from university settings. This resulted in the oversampling of young people and students and limits the generalizability of the findings. However, despite the diverse methods of recruitment, the relationship of perceived racial or ethnic discrimination to self-reported health held across ethnic groups and in both student and community samples. In addition, the findings remained significant even when controlling for factors potentially related to the variations in recruitment sites, such as education level.
Another limitation is that the predictor, mediators, and outcome of interest in this study were measured via self-report, which could lead to inflated estimates of their association. This would not explain, however, why certain elements of discrimination (i.e., social exclusion and threat) were uniquely associated with self-reported health or why the psychological mediators fully accounted for the effects of social exclusion but not threat. The three mediators are significantly correlated, raising concerns about multicollinearity. However, all three were independently linked to self-reported health. This suggests that multicollinearity is unlikely to have unduly influenced the outcomes.
In addition, although self-reported health has been widely established as a good indicator of objective health measures [9–11], it is not clear whether our results would generalize to objective measures of overall health or specific health conditions. Finally, the cross-sectional nature of the study does not allow conclusions about the causal relationships among perceived discrimination, psychological mediators, and self-reported health. Although we have argued that depression, anxiety, and cynical hostility mediate the relationship between perceived discrimination and health, it is also possible that these variables make individuals more sensitive to the effects of race-related maltreatment.
Despite its limitations, this study advances our understanding of the effects of perceived discrimination on health by demonstrating that race/ethnicity-based social exclusion and threat are associated with poor self-reported health for Asians, Blacks, and Latino(a)s and that these associations are due at least in part to the impact of social exclusion and threat on psychological functioning. The similar effects of discrimination observed across diverse race/ethnic groups suggest that there is a particularly noxious element associated with race-related exclusion and threat that degrades health by promoting depression, anxiety, and cynical hostility. The findings of this study underscore the importance of recognizing and treating mental health concerns in racial and ethnic minority patients, particularly in the context of routine medical care. Addressing the symptoms of depression and anxiety may help offset some of the effects of racial or ethnic discrimination on health. In future work, it will be necessary to develop and disseminate strategies that can be used in clinical settings to efficiently and appropriately assess the overall stress burden imposed by racial or ethnic discrimination. Furthermore, it will be valuable to determine whether different dimensions of discrimination elicit different patterns of psychophysiological response or different coping responses and investigate whether these responses influence health outcomes. Understanding the mechanisms through which race/ethnicity-related maltreatment affect a range of health outcomes can permit the development of more targeted and effective interventions.
Acknowledgments
This study was funded in part by seed grants from St. John's University and by minority supplements from NHLBI grant no. R01 HL065890 to the first author. This material is the result of work partially supported by resources and the use of facilities at the Veterans Affairs Pittsburgh Healthcare System in Pittsburgh, PA. Dr. Hausmann was supported by VA Health Services Research and Development Career Development Awards (RCD 06-287 & ER 0280-1).
Footnotes
Conflict of Interest Statement The authors have no conflicts of interest to disclose.
Contributor Information
Elizabeth Brondolo, Email: brondole@stjohns.edu, Department of Psychology, St. John’s University, Jamaica, NY, USA
Leslie R. M. Hausmann, Research Health Science Specialist, Health Services Research & Development Service, Veterans Affairs Pittsburgh Health Care System, Center for Health Equity Research and Promotion, Pittsburgh, PA, USA
Juhee Jhalani, Department of Psychology, St. John’s University, Jamaica, NY, USA
Melissa Pencille, Department of Psychology, St. John’s University, Jamaica, NY, USA
Jennifer Atencio-Bacayon, Department of Psychology, St. John’s University, Jamaica, NY, USA
Asha Kumar, Department of Psychology, St. John’s University, Jamaica, NY, USA
Jasmin Kwok, Department of Psychology, St. John’s University, Jamaica, NY, USA
Jahanara Ullah, Department of Psychology, St. John’s University, Jamaica, NY, USA
Alan Roth, Jamaica Hospital Medical Center, Jamaica, NY, USA
Daniel Chen, Flushing Hospital Medical Center, Flushing, NY, USA
Robert Crupi, Flushing Hospital Medical Center, Flushing, NY, USA
Joseph Schwartz, Flushing Hospital Medical Center, Flushing, NY, USA
References
- 1.Contrada RJ, Ashmore RD, Gary ML, et al. Ethnicity-related sources of stress and their effects on well-being. Current Directions in Psychological Science. 2000;9:136–139. [Google Scholar]
- 2.Contrada RJ, Ashmore RD, Gary ML, et al. Measures of ethnicity-related stress: Psychometric properties, ethnic group differences, and associations with well-being. Journal of Applied Social Psychology. 2001;31:1775–1820. [Google Scholar]
- 3.Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans: A biopsychosocial model. American Psychologist. 1999;54:805–816. doi: 10.1037//0003-066x.54.10.805. [DOI] [PubMed] [Google Scholar]
- 4.Paradies Y. A systematic review of empirical research on self-reported racism and health. International Journal of Epidemiology. 2006;35:888–901. doi: 10.1093/ije/dyl056. [DOI] [PubMed] [Google Scholar]
- 5.Mays VM, Cochran SD, Barnes NW. Race, race-based discrimination, and health outcomes among African Americans. Annu Rev Psychol. 2007;58:201–225. doi: 10.1146/annurev.psych.57.102904.190212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Williams DR, Mohammed SA. Discrimination and racial disparities in health: Evidence and needed research. Journal Of Behavioral Medicine. 2009;32:20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychol Bull. 2009;135:531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pietz K, Petersen LA. Comparing self-reported health status and diagnosis-based risk adjustment to predict 1- and 2 to 5-year mortality. Health Serv Res. 2007;42:629–643. doi: 10.1111/j.1475-6773.2006.00622.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Okura Y, Urban LH, Mahoney DW, Jacobsen SJ, Rodeheffer RJ. Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. J Clin Epidemiol. 2004;57:1096–1103. doi: 10.1016/j.jclinepi.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 10.Iversen L, Hannaford PC, Godden DJ, Price D. Do people self-reporting information about chronic respiratory disease have corroborative evidence in their general practice medical records? A study of intermethod reliability. Prim Care Respir J. 2007;16:162–168. doi: 10.3132/pcrj.2007.00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haapanen N, Miilunpalo S, Pasanen M, Oja P, Vuori I. Agreement between questionnaire data and medical records of chronic diseases in middle-aged and elderly Finnish men and women. Am J Epidemiol. 1997;145:762–769. doi: 10.1093/aje/145.8.762. [DOI] [PubMed] [Google Scholar]
- 12.Krieger N. Embodying inequality: A review of concepts, measures, and methods for studying health consequences of discrimination. International Journal of Health Services. 1999;29:295–352. doi: 10.2190/M11W-VWXE-KQM9-G97Q. [DOI] [PubMed] [Google Scholar]
- 13.Brondolo E, Kelly KP, Coakley V, et al. The Perceived Ethnic Discrimination Questionnaire: Development and preliminary validation of a community version. Journal of Applied Social Psychology. 2005;35:335–365. [Google Scholar]
- 14.Finch BK, Hummer RA, Kolody B, Vega WA. The role of discrimination and acculturative stress in the physical health of Mexican-origin adults. Hispanic Journal of Behavioral Sciences. 2001;23:399–429. [Google Scholar]
- 15.Kwate NOA, Valdimarsdottir HB, Guevarra JS, Bovbjerg DH. Experiences of racist events are associated with negative health consequences for African American women. Journal of the National Medical Association. 2003;96:450–460. [PMC free article] [PubMed] [Google Scholar]
- 16.Asakura T, Gee GC, Nakayama K, Niwa S. Returning to the 'homeland': Work-related ethnic discrimination and the health of Japanese Brazilians in Japan. American Journal of Public Health. 2008;98:743–750. doi: 10.2105/AJPH.2007.117309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bahm A, Forchuk C. Interlocking oppressions: The effect of a comorbid physical disability on percevied stigma and discrimination among mental health consumers in Canada. Health and Social Care in the Community. 2009;17:63–70. doi: 10.1111/j.1365-2524.2008.00799.x. [DOI] [PubMed] [Google Scholar]
- 18.Becares L, Nazroo J, Stafford M. The buffering effects of ethnic density on experienced racism and health. Health & Place. 2009;15:670–678. doi: 10.1016/j.healthplace.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 19.Borrell LN, Kiefe CI, Williams DR, Diez-Roux AV, Gordon-Larsen P. Self-reported health, perceived racial discrimination, and skin color in African Americans in the CARDIA study. Soc Sci Med. 2006;63:1415–1427. doi: 10.1016/j.socscimed.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 20.Caputo RK. The effects of socioeconomic status, perceived discrimination and mastery on health status in a youth cohort. Social Work in Health Care. 2003;37:17–42. doi: 10.1300/J010v37n02_02. [DOI] [PubMed] [Google Scholar]
- 21.Chae DH, Walters KL. Racial discrimination and racial identity attitudes in relation to self-rated health and physical pain and impairment among two-spirit American Indians/Alaska Natives. American Journal of Public Health. 2009;99:S144–S151. doi: 10.2105/AJPH.2007.126003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Edwards RR. The association of perceived discrimination with low back pain. Journal of Behavioral Medicine. 2008;31:379–389. doi: 10.1007/s10865-008-9160-9. [DOI] [PubMed] [Google Scholar]
- 23.Flores E, Tschann JM, Dimas JM, et al. Perceived discrimination, perceived stress, and mental and physical health among Mexican-origin adults. Hispanic Journal of Behavioral Sciences. 2008;30:401–424. [Google Scholar]
- 24.Franzini L, Caughy M, Spears W, Fernandez-Esquer ME. Neighborhood economic conditions, social processes, and self-rated health in low-income neighborhoods in Texas: A multilevel latent variables model. Social Science & Medicine. 2005;61:1135–1150. doi: 10.1016/j.socscimed.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 25.Franzini L, Fernandez-Esquer ME. Socioeconomic, cultural, and personal influences on health outcomes in low income Mexican-origin individuals in Texas. Social Science & Medicine. 2004;59:1629–1646. doi: 10.1016/j.socscimed.2004.02.014. [DOI] [PubMed] [Google Scholar]
- 26.Fujishiro K. Is perceived racial privilege associated with health? Findings from the Behavioral Risk Factor Surveillance System. Soc Sci Med. 2009;68:840–844. doi: 10.1016/j.socscimed.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 27.Gee GC. A multilevel analysis of the relationship between institutional and individual racial discrimination and health status. Am J Public Health. 2002;92:615–623. doi: 10.2105/ajph.92.4.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harris R, Tobias M, Jeffreys M, et al. Racism and health: The relationship between experience of racial discrimination and health in New Zealand. Soc Sci Med. 2006;63:1428–1441. doi: 10.1016/j.socscimed.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 29.Hausmann LR, Jeong K, Bost JE, Ibrahim SA. Perceived discrimination in health care and health status in a racially diverse sample. Med Care. 2008;46:905–914. doi: 10.1097/MLR.0b013e3181792562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hong TB, Oddone EZ, Weinfurt KP, et al. The relationship between perceived barriers to healthcare and self-rated health. Psychology, Health & Medicine. 2004;9:476–481. [Google Scholar]
- 31.Jasinskaja-Lahti I, Liebkind K, Perhoniemi R. Perceived discrimination and well-being: A victim study of different immigrant groups. Journal of Community & Applied Social Psychology. 2006;16:267–284. [Google Scholar]
- 32.Jasinskaja-Lahti I, Liebkind K, Perhoniemi R. Perceived ethnic discrimination at work and well-being of immigrants in Finland: The moderating role of employment status and work-specific group-level control beliefs. International Journal of Intercultural Relations. 2007;31:223–242. [Google Scholar]
- 33.Karlsen S, Nazroo J. Agency and structure: The impact of ethnic identity and racism on the health of ethnic minority people. Sociology of Health & Illness. 2002;24:1–20. [Google Scholar]
- 34.Karlsen S, Nazroo JY. Fear of racism and health. J Epidemiol Community Health. 2004;58:1017–1018. doi: 10.1136/jech.2004.020479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Karlsen S, Nazroo JY. Relation between racial discrimination, social class, and health among ethnic minority groups. Am J Public Health. 2002;92:624–631. doi: 10.2105/ajph.92.4.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Larson A, Gillies M, Howard PJ, Coffin J. It's enough to make you sick: The impact of racism on the health of Aboriginal Australians. Australian and New Zealand Journal of Public Health. 2007;31:322–329. doi: 10.1111/j.1753-6405.2007.00079.x. [DOI] [PubMed] [Google Scholar]
- 37.Laveist TA. Racial segregation and longevity among African Americans: An individual-level analysis. Health Services Research. 2003;38:1719–1734. doi: 10.1111/j.1475-6773.2003.00199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mohseni M, Lindstron M. Ethnic differences in anticipated discrimination, generalized trust in other people and self-rated health: A population-based study in Sweden. Ethnicity & Health. 2008;13:417–434. doi: 10.1080/13557850802009603. [DOI] [PubMed] [Google Scholar]
- 39.Moody-Ayers SY, Stewart AL, Covinsky KE, Inouye SK. Prevalence and correlates of perceived societal racism in older African-American adults with type 2 diabetes mellitus. Journal of the American Geriatric Society. 2005;53:2202–2208. doi: 10.1111/j.1532-5415.2005.00501.x. [DOI] [PubMed] [Google Scholar]
- 40.Piette JD, Bibbins-Domingo K, Schillinger D. Health care discrimination, processes of care, and diabetes patients' health status. Patient Educ Couns. 2006;60:41–48. doi: 10.1016/j.pec.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 41.Ren XS, Amick BC, Williams DR. Racial/ethnic disparities in health: The interplay between discrimination and socioeconomic status. Ethn Dis. 1999;9:151–165. [PubMed] [Google Scholar]
- 42.Ryan AM, Gee GC, Laflamme DF. The association between self-reported discrimination, physical health and blood pressure: Findings from African Americans, Black immigrants, and Latino immigrants in New Hampshire. Journal of Health Care for the Poor and Underserved. 2006;17:116–132. doi: 10.1353/hpu.2006.0092. [DOI] [PubMed] [Google Scholar]
- 43.Schulz A, Israel B, Williams D, et al. Social inequalities, stressors and self reported health status among African American and White women in the Detroit metropolitan area. Social Science & Medicine. 2000;51:1639–1653. doi: 10.1016/s0277-9536(00)00084-8. [DOI] [PubMed] [Google Scholar]
- 44.Schulz AJ, Gravlee CC, Williams DR, et al. Discrimination, symptoms of depression, and self-rated health among African American women in Detroit: Results from a longitudinal analysis. American Journal of Public Health. 2006;96:1265–1270. doi: 10.2105/AJPH.2005.064543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sellers SL, Bonham V, Neighbors HW, Amell JW. Effects of racial discrimination and health behaviors on mental and physical health of middle-class African American men. Health Education & Behavior. 2009;36:31–44. doi: 10.1177/1090198106293526. [DOI] [PubMed] [Google Scholar]
- 46.Sohler N, Li X, Cunningham C. Perceived discrimination among severely disadvantaged people with HIV infection. Public Health Rep. 2007;122:347–355. doi: 10.1177/003335490712200308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sohn L, Harada ND. Effects of racial/ethnic discrimination on the health status of minority veterans. Military Medicine. 2008;173:331–338. doi: 10.7205/milmed.173.4.331. [DOI] [PubMed] [Google Scholar]
- 48.Stepanikova I, Cook KS. Effects of poverty and lack of insurance on perceptions of racial and ethnic bias in health care. Health Serv Res. 2008;43:915–930. doi: 10.1111/j.1475-6773.2007.00816.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sujoldzic A, Peternel L, Kulenovic T, Terzic R. Social determinants of health: A comparative study of Bosnian adolescents in different cultural contexts. Collegium Antropologicum. 2006;30:703–711. [PubMed] [Google Scholar]
- 50.Taloyan M, Johansson LM, Johansson SE, Sundquist J, Kocturk TO. Poor self-reported health and sleeping difficulties among Kurdish immigrant men in Sweden. Transcultural Psychiatry. 2006;43:445–461. doi: 10.1177/1363461506066988. [DOI] [PubMed] [Google Scholar]
- 51.Trivedi AN, Ayanian JZ. Perceived discrimination and use of preventive health services. J Gen Intern Med. 2006;21:553–558. doi: 10.1111/j.1525-1497.2006.00413.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Watson JM, Logan HL, Tomar SL. The influence of active coping and perceived stress on health disparities in a multi-ethnic low income sample. BMC Public Health. 2008;8:41. doi: 10.1186/1471-2458-8-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wiking E, Johansson SE, Sundquist J. Ethnicity, acculturation, and self reported health: A population based study among immigrants from Poland, Turkey, and Iran in Sweden. Journal of Epidemiology & Community Health. 2004;58:574–582. doi: 10.1136/jech.2003.011387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Williams DR, Gonzalez HM, Williams SL, et al. Perceived discrimination, race and health in South Africa. Social Science & Medicine. 2008;67:12p. doi: 10.1016/j.socscimed.2008.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: Socio-economic status, stress and discrimination. J Health Psychol. 1997;2:335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 56.Bird ST, Bogart LM, Delahanty DL. Health-related correlates of perceived discrimination in HIV care. AIDS Patient Care and STDs. 2004;18:19–26. doi: 10.1089/108729104322740884. [DOI] [PubMed] [Google Scholar]
- 57.Ogbu JU. Cultural amplifiers of intelligence: IQ and minority status in cross-cultural perspective. In: Fish JM, editor. Race and intelligence: Separating science from myth. Mahwah, NJ: Lawrence Erlbaum Associates; 2002. pp. 241–278. [Google Scholar]
- 58.Emerson MO, Yancey G, Chai KJ. Does race matter in residential segregation? Exploring the preferences of White Americans. American Social Review. 2001;66:922–935. [Google Scholar]
- 59.Brezina T, Winder K. Economic disadvantage, status generalization and negative racial stereotyping by White Americans. Social Psychology Quarterly. 2003;66:402–418. [Google Scholar]
- 60.Schlundt DG, Hargreaves MK, McClellan L. Geographic clustering of obesity, diabetes, and hypertension in Nashville, Tennessee. Journal of Ambulatory Care Management. 2006;29:125–152. doi: 10.1097/00004479-200604000-00005. [DOI] [PubMed] [Google Scholar]
- 61.Williams DR, Jackson PB. Social sources of racial disparities in health. Health Affairs. 2005;24:325–334. doi: 10.1377/hlthaff.24.2.325. [DOI] [PubMed] [Google Scholar]
- 62.Kwate NOA. Fried chicken and fresh apples: Racial segregation as a fundamental cause of fast food density in black neighborhoods. Health & Place. 2008;14:32–44. doi: 10.1016/j.healthplace.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 63.McDonald JT, Kennedy S. Insights into the ‘healthy immigrant effect’: Health status and health service use of immigrants to Canada. Social Science & Medicine. 2004;59:1613–1627. doi: 10.1016/j.socscimed.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 64.Gushulak B. Healthier on arrival? Further insight into the “healthy immigrant effect”. CMAJ: Canadian Medical Association Journal Supplement. 2007;176:1439–1440. doi: 10.1503/cmaj.070395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sanders AE. A Latino advantage in oral health-related quality of life is modified by nativity status. Social Science & Medicine. 2010;71:205–211. doi: 10.1016/j.socscimed.2010.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Alba R, Rumbaut RG, Marotz K. A distorted nation: Perceptions of racial/ethnic group sizes and attitudes toward immigrants and other minorities. Social Forces. 2005;84:901–919. [Google Scholar]
- 67.Bureau USC. http://www.census.gov/population/www/projections/usinterimproj/.2008.
- 68.Brondolo E, Brady N, Beatty DL, Pencille M, Contrada R. Coping with racism: A selective review and theoretical and methodological critique. Journal of Behavioral Medicine. 2009;32:64–88. doi: 10.1007/s10865-008-9193-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Brondolo E, Brady N, Thompson S, et al. Perceived racism and negative affect: Analyses of trait and state measures of affect in a community sample. Journal of Social & Clinical Psychology. 2008;27:150–173. doi: 10.1521/jscp.2008.27.2.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Brondolo E, Brady Ver Halen N, Pencille M, Beatty DL, Contrada RJ. Coping with racism: A selective review of the literature and a theoretical and methodological critique. Journal Of Behavioral Medicine. 2009;32:64–88. doi: 10.1007/s10865-008-9193-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Brondolo E, Thompson S, Brady N, et al. The relationship of racism to appraisals and coping in a community sample. Ethnicity & Disease. 2005;15:S5-14–19. [PubMed] [Google Scholar]
- 72.Karlsen S, Nazroo JY, Stephenson R. Ethnicity, environment and health: Putting ethnic inequalities in health in their place. Soc Sci Med. 2002;55:1647–1661. doi: 10.1016/s0277-9536(01)00297-0. [DOI] [PubMed] [Google Scholar]
- 73.Broudy R, Brondolo E, Coakley V, et al. Perceived ethnic discrimination in relation to daily moods and negative social interactions. J Behav Med. 2007;30:31–43. doi: 10.1007/s10865-006-9081-4. [DOI] [PubMed] [Google Scholar]
- 74.Finch BK, Kolody B, Vega WA. Perceived discrimination and depression among Mexican-origin adults in California. J Health Soc Behav. 2000;41:295–313. [PubMed] [Google Scholar]
- 75.Banks KH, Kohn-Wood LP, Spencer M. An examination of the african american experience of everyday discrimination and symptoms of psychological distress. Community Ment Health J. 2006;42:555–570. doi: 10.1007/s10597-006-9052-9. [DOI] [PubMed] [Google Scholar]
- 76.Noh S, Kaspar V, Wickrama KA. Overt and subtle racial discrimination and mental health: Preliminary findings for Korean immigrants. Am J Public Health. 2007;97:1269–1274. doi: 10.2105/AJPH.2005.085316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Jackson JS, Brown TN, Williams DR, et al. Racism and the physical and mental health status of African Americans: A thirteen year national panel study. Ethn Dis. 1996;6:132–147. [PubMed] [Google Scholar]
- 78.Hwang WC, Goto S. The impact of perceived racial discrimination on the mental health of Asian American and Latino college students. Cultur Divers Ethnic Minor Psychol. 2008;14:326–335. doi: 10.1037/1099-9809.14.4.326. [DOI] [PubMed] [Google Scholar]
- 79.McGrady A, McGinnis R, Badenhop D, Bentle M, Rajput M. Effects of depression and anxiety on adherence to cardiac rehabilitation. J Cardiopulm Rehabil Prev. 2009;29:358–364. doi: 10.1097/HCR.0b013e3181be7a8f. [DOI] [PubMed] [Google Scholar]
- 80.Kaup BA, Loreck D, Gruber-Baldini AL, et al. Depression and its relationship to function and medical status, by dementia status, in nursing home admissions. Am J Geriatr Psychiatry. 2007;15:438–442. doi: 10.1097/JGP.0b013e31803c54f7. [DOI] [PubMed] [Google Scholar]
- 81.Larson C, Belue R, Schlundt DG, McClellan L. Relationship between symptoms of depression, functional health status, and chronic disease among a residential sample of African Ameri-cans. J Ambul Care Manage. 2006;29:133–140. doi: 10.1097/00004479-200604000-00006. [DOI] [PubMed] [Google Scholar]
- 82.Husaini BA, Hull PC, Sherkat DE, et al. Diabetes, depression, and healthcare utilization among African Americans in primary care. J Natl Med Assoc. 2004;96:476–484. [PMC free article] [PubMed] [Google Scholar]
- 83.Bromberger JT, Kravitz HM, Wei HL, et al. History of depression and women's current health and functioning during midlife. Gen Hosp Psychiatry. 2005;27:200–208. doi: 10.1016/j.genhosppsych.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 84.Miller TQ, Smith TW, Turner CW, et al. A meta-analytic review of research on hostility and physical health. Psychological Bulletin. 1996;119:322–348. doi: 10.1037/0033-2909.119.2.322. [DOI] [PubMed] [Google Scholar]
- 85.Smith TW, Ruiz JM. Psychosocial influences on the development and course of coronary hart disease: Current status and implications for research and practice. Journal of Consulting and Clinical Psychology. 2002;70:548–568. doi: 10.1037//0022-006x.70.3.548. [DOI] [PubMed] [Google Scholar]
- 86.Taylor TR, Kamarck TW, Shiffman S. Validation of the Detroit Area Study Discrimination Scale in a community sample of older African American adults: The Pittsburgh healthy heart project. Int J Behav Med. 2004;11:88–94. doi: 10.1207/s15327558ijbm1102_4. [DOI] [PubMed] [Google Scholar]
- 87.Brondolo E, Libby DJ, Denton E, et al. Racism and ambulatory blood pressure in a community sample. Psychosomatic Medicine. 2008;70:49–56. doi: 10.1097/PSY.0b013e31815ff3bd. [DOI] [PubMed] [Google Scholar]
- 88.Nabi H, Singh-Manoux A, Ferrie JE, et al. Hostility and depressive mood: Results from the Whitehall II prospective cohort study. Psychol Med. 2010;40:405–413. doi: 10.1017/S0033291709990432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.McHorney CA, Ware JE, Jr, Lu JF, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Medical Care. 1994;32:40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 90.Ware JE, Jr, Sherbourne CD. The MOS 36-Item Short-Form Health Survey (SF-36): I. Conceptual framework and item selection. Medical Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 91.Kwok J, Atencio J, Ullah J, et al. The Perceived Ethnic Discrimination Questionnaire – Community Version: Validation in a Multi-Ethnic Asian Sample. 2008. [DOI] [PubMed] [Google Scholar]
- 92.Kwok J, Kumar A, Jhalani J, et al. Preliminary Validation of the Perceived Ethnic Discrimination Questionnaire in an Asian Sample. Annual Meeting of the Society for Behavioral Medicine; San Diego, CA. 2008; March. [Google Scholar]
- 93.Deragotis LR. Symptom Checklist-90-R: Administration, scoring and procedures manual. 3. Minneapolis, MN: National Computer Systems, Inc; 1994. [Google Scholar]
- 94.Martinez S, Stillerman L, Waldo M. Reliability and validity of the SCL-90-R with Hispanic college students. Hispanic Journal of Behavioral Sciences. 2005;27:254–264. [Google Scholar]
- 95.Noh S, Kasper V, Chen X. Measuring depression in Korean Immigrants: Assessing validity of the translated Korean version of the CES-D scale. Cross-Cultural Research: The Journal of Comparative Social Science. 1998;32:358–377. [Google Scholar]
- 96.Barefoot JC, Dodge KA, Peterson BL, Dahlstrom WG. The Cook-Medley Hostility Scale: Item content and ability to predict survival. Psychosomatic Medicine. 1989;51:46–57. doi: 10.1097/00006842-198901000-00005. [DOI] [PubMed] [Google Scholar]
- 97.Contrada RJ, Jussim L. What does the Cook-Medley hostility scale measure? In search of an adequate measurement model. Journal of Applied Social Psychology. 1992;22:615–627. [Google Scholar]
- 98.Weidner G, Friend R, Ficarrotto TJ, Mendell NR. Hostility and cardiovascular reactivity to stress in women and men. Psychosomatic Medicine. 1989;51:36–45. doi: 10.1097/00006842-198901000-00004. [DOI] [PubMed] [Google Scholar]
- 99.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 100.Preacher KJ, Hayes AF. Available from: http://www.comm.ohio-state.edu/ahayes/spss%20programs/indirect.htm.
- 101.Preacher KJ, Rucker DD, Hayes AF. Assessing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivariate Behavioral Research. 2007;42:185–227. doi: 10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- 102.Eisenberger NI, Inagaki TK, Mashal NM, Irwin MR. Inflammation and social experience: An inflammatory challenge induces feelings of social disconnection in addition to depressed mood. Brain, Behavior & Immunity. 2010;24:558–563. doi: 10.1016/j.bbi.2009.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Lopez R. Black-white residential segregation and physical activity. Ethnicity & Disease. 2006;16:495–502. [PubMed] [Google Scholar]