Abstract
Background
Fecal microbiota therapy is increasingly being used to treat patients with Clostridium difficile infection. This health technology assessment primarily evaluated the effectiveness and cost-effectiveness of fecal microbiota therapy compared with the usual treatment (antibiotic therapy).
Methods
We performed a literature search using Ovid MEDLINE, Embase, Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects, CRD Health Technology Assessment Database, Cochrane Central Register of Controlled Trials, and NHS Economic Evaluation Database. For the economic review, we applied economic filters to these search results. We also searched the websites of agencies for other health technology assessments.
We conducted a meta-analysis to analyze effectiveness. The quality of the body of evidence for each outcome was examined according to the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) Working Group criteria. Using a step-wise, structural methodology, we determined the overall quality to be high, moderate, low, or very low.
We used a survey to examine physicians’ perception of patients’ lived experience, and a modified grounded theory method to analyze information from the survey.
Results
For the review of clinical effectiveness, 16 of 1,173 citations met the inclusion criteria. A meta-analysis of two randomized controlled trials found that fecal microbiota therapy significantly improved diarrhea associated with recurrent C. difficile infection versus treatment with vancomycin (relative risk 3.24, 95% confidence interval [CI] 1.85–5.68) (GRADE: moderate). While fecal microbiota therapy is not associated with a significant decrease in mortality compared with antibiotic therapy (relative risk 0.69, 95% CI 0.14–3.39) (GRADE: low), it is associated with a significant increase in adverse events (e.g., short-term diarrhea, relative risk 30.76, 95% CI 4.46–212.44; abdominal cramping, relative risk 14.81, 95% CI 2.07–105.97) (GRADE: low).
For the value-for-money component, two of 151 economic evaluations met the inclusion criteria. One reported that fecal microbiota therapy was dominant (more effective and less expensive) compared with vancomycin; the other reported an incremental cost-effectiveness ratio of $17,016 USD per quality-adjusted life-year for fecal microbiota therapy compared with vancomycin. This ratio for the second study indicated that there would be additional cost associated with each recurrent C. difficile infection resolved. In Ontario, if fecal microbiota therapy were adopted to treat recurrent C. difficile infection, considering it from the perspective of the Ministry of Health and Long-Term Care as the payer, an estimated $1.5 million would be saved after the first year of adoption and $2.9 million after 3 years. The contradiction between the second economic evaluation and the savings we estimated may be a result of the lower cost of fecal microbiota therapy and hospitalization in Ontario compared with the cost of therapy used in the US model.
Physicians reported that C. difficile infection significantly reduced patients’ quality of life. Physicians saw fecal microbiota therapy as improving patients’ quality of life because patients could resume daily activities. Physicians reported that their patients were happy with the procedures required to receive fecal microbiota therapy.
Conclusions
In patients with recurrent C. difficile infection, fecal microbiota therapy improves outcomes that are important to patients and provides good value for money.
BACKGROUND
Clinical Need and Target Population
The incidence of Clostridium difficile infection has increased by about 20 times over the past 10 years, and rates are about 20 per 100,000 population.1 Risk factors for infection include antibiotic use, inflammatory bowel disease, comorbidity, and increasing age.1 About 20% to 30% of patients treated for an initial episode have a recurrence, and 40% to 60% of those patients have subsequent (second or later) recurrences.2 In severe cases, C. difficile infection can result in bowel perforation and, rarely, death.2
Antibiotics used for C. difficile infection are metronidazole as first-line and vancomycin as second-line therapies.1 In some cases, patients unresponsive to medical management are treated by surgical colectomy.3
Technology
Fecal microbiota therapy is increasingly used as a treatment for C. difficile infection in the belief that importing the colonic microbiome of a healthy person is a simple way to reconstitute the normal colonic flora (microorganisms that live in the gut).3
The routes of fecal microbiota administration vary in the literature (e.g., enema, upper gastrointestinal tract route, colonoscopy). The timing and frequency of fecal microbiota therapy also vary, from a single session to serial administration over several days.3
Regulatory Information
A Health Canada Guidance document (March 2015)4 considers fecal microbiota therapy a biologic drug and states the following:
Health Canada is notifying stakeholders of its risk based, provisional interpretation regarding the Clinical Trial Application (CTA) requirements in the Food and Drug Regulations for the use of Fecal Microbiota Therapy (FMT) by health care practitioners to treat patients with recurrent CDI [C. difficile infection] not responsive to conventional therapies … This interim policy allows health care practitioners to treat patients suffering from CDI not responsive to conventional therapies with FMT without a clinical trial where the conditions in this guidance document are followed … Effective immediately, this provisional interpretation regarding the CTA requirements will be applied on an interim basis while the Department continues to explore future policy options for regulating FMT.
Health Canada's 2015 guidance for fecal microbiota therapy4 replicates the United States Food and Drug Administration's 2013 enforcement policy5 regarding investigational new drug requirements for the use of fecal microbiota therapy to treat C. difficile infection that is unresponsive to standard therapies.
Context
At least three centres in Ontario perform fecal microbiota therapy for C. difficile infection (University Health Network, St. Joseph's Healthcare Hamilton, and Toronto East General Hospital).
Based on referral experience, an expert estimated that about 500 to 1,000 patients per year in Ontario would be eligible to receive fecal microbiota therapy for recurrent C. difficile infection (C. Lee, written communication, October 27, 2015).
Research Question
What are the effectiveness, cost-effectiveness, and budgetary impact of fecal microbiota therapy compared with antibiotics in adults with initial, recurrent, or refractory C. difficile infections?
CLINICAL EVIDENCE REVIEW
Objective
The clinical evidence section of the health technology assessment reviewed the effectiveness of fecal microbiota therapy compared with antibiotics in adults with initial or recurrent C. difficile infection.
Methods
Research questions are developed by Health Quality Ontario in consultation with experts and applicants in the topic area.
Sources
We performed a literature search on July 30, 2015, using Ovid MEDLINE, Embase, Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects, Centre for Reviews and Dissemination Health Technology Assessment Database, Cochrane Central Register of Controlled Trials, and National Health Service (NHS) Economic Evaluation Database, for studies published from January 1, 2013, to July 30, 2015. A 2-year search was chosen because a recent, comprehensive systematic review was published in 2015.
Search strategies were developed by medical librarians using medical subject headings (MeSH). See Appendix 1 for full details, including all search terms.
Literature Screening
A single reviewer reviewed the abstracts, and we obtained full-text articles for studies meeting the eligibility criteria. We also examined reference lists for any additional relevant studies not identified through the search.
Inclusion Criteria
English-language full-text publications
Studies published between January 1, 2013, and July 30, 2015
Randomized controlled trials, observational studies, systematic reviews, and meta-analyses
Studies of fecal microbiota therapy (via variable routes of administration and variable timing and frequency) for C. difficile infection
Studies involving patients with initial, recurrent, or refractory C. difficile infection. Initial infection is defined as the first occurrence, recurrent infection as an episode occurring after one previous episode of treatment with a favourable response, and refractory infection as an episode that did not respond to treatment
Studies where the comparators were antibiotics
Exclusion Criteria
Animal and in vitro studies
Editorials, case reports, or commentaries
Studies of fecal microbiota therapy for indications other than C. difficile infection
Outcomes of Interest
Resolution of symptoms
Quality of life
Mortality
Adverse events
Data Extraction
We extracted relevant data on study characteristics, risk of bias items, and PICO (population, intervention, comparison, and outcome) using a standardized data form. The form collected information about:
Source (i.e., citation information, contact details, study type)
Methods (i.e., study design, study duration and years, participant allocation, allocation sequence concealment, blinding, reporting of missing data, reporting of outcomes, and whether the study compared two or more groups)
Outcomes (i.e., outcomes measured, number of participants for each outcome, number of participants missing for each outcome, outcome definition and source of information, unit of measurement, upper and lower limits [for scales], and time points at which the outcome was assessed)
We contacted the authors of the studies to provide unpublished data when required for comparisons and meta-analysis.
Statistical Analysis
An analysis of individual studies was performed using Review Manager, version 5.6 Summary measures were expressed as the mean difference for continuous data and risk difference for dichotomous data using the Mantel-Haenszel method. Statistical heterogeneity was assessed using the chi-square test. A P value ≤ .10 associated with a chi-square statistic was considered substantial heterogeneity, and a random effects model was used. In the case of zero events, 1.0 was added to both groups. Graphic display of the forest plots was also examined. A P value ≤ .05 was considered statistically significant for overall effect estimate.
Quality of Evidence
We used the Assessment of Multiple Systematic Reviews (AMSTAR) measurement tool to assess the methodologic quality of systematic reviews.7 See Appendix 2 for details of the AMSTAR analysis.
The quality of the body of evidence for each outcome was examined according to the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) Working Group criteria.8 The overall quality was determined to be high, moderate, low, or very low using a step-wise, structural methodology.
Results
Literature Search
The database search yielded 1,173 citations published between January 1, 2013, and July 30, 2015. After removing duplicates, we reviewed titles and abstracts to identify potentially relevant articles. We obtained the full texts of these articles for further assessment. Sixteen studies (nine systematic reviews, six observational studies, and one randomized controlled trial [RCT]) met the inclusion criteria. We hand-searched reference lists of the included studies, along with health technology assessment websites and other sources, to identify additional relevant studies. No further citations were added.
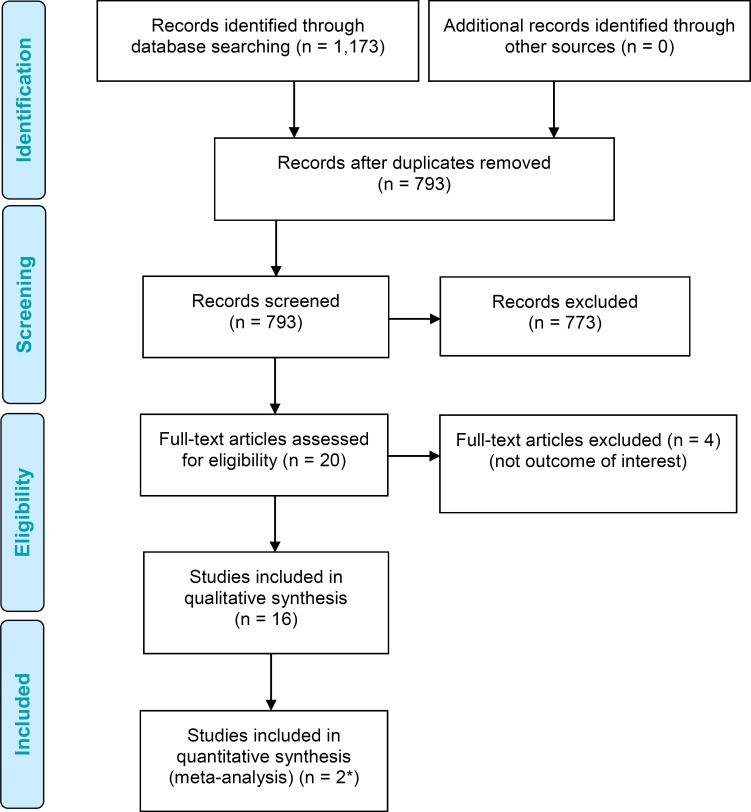
Figure 1 presents the flow diagram for the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA).
Figure 1: Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) Flow Diagram.
*Incorporates one study that was already included in the systematic review by Drekonja et al.3
Source: Adapted from Moher et al.9
Methodologic Quality of Included Studies
Results of the methodology checklist for included studies are presented in Appendix 2.
The AMSTAR scores for the nine systematic reviews are shown in Table A1.
One RCT10 and six observational studies11–16 were published after the literature search cut-off date (January 2015) used in the most recent systematic review by Drekonja et al.3
Systematic Review
The most recent (2015) systematic review by Drekonja et al3 defined initial infection as the first occurrence, recurrent infection as an episode occurring after one previous episode of treatment with a favourable response, and refractory infection as an episode that does not respond to treatment. The primary outcome of interest was the resolution of symptoms after a single treatment of fecal microbiota, or after a single prespecified series of treatments.3 Drekonja et al3 identified two RCTs and 28 case series for recurrent C. difficile infection. A meta-analysis was not completed, and results were reported narratively. The overall quality of the available evidence evaluating fecal microbiota therapy is low.3
Results of the systematic review are reported in Appendix 4. In summary, the authors concluded that, for recurrent C. difficile infection,3 fecal microbiota therapy could have a substantial effect with few short-term adverse events. However, evidence was insufficient about the use of fecal microbiota therapy for refractory or initial C. difficile treatment, and about whether effects vary by donor, preparation, or delivery method.3 Transient adverse events attributed to fecal microbiota therapy—including diarrhea, cramping, belching, nausea, abdominal pain, bloating, fever, and dizziness—were reported in the RCTs and case series reports.17,18 Possible procedure-related harms (including microperforation with colonoscopy19 and gastrointestinal bleeding,20 peritonitis,21 and pneumonia21 with use of the upper gastrointestinal tract route) were rarely reported. Mortality was not specifically reported as an outcome.3
There are several limitations to this systematic review. First, Drekonja et al3 classified patients into recurrent, refractory, or initial C. difficile infection. However, after reviewing the primary studies, it is unclear how classifications were defined within those studies, and importantly how recurrent and refractory infections were distinguished. Second, most studies reported a primary outcome that combined the resolution of symptoms and recurrence of infection, such as “cure without relapse” or “resolution of diarrhea without recurrence.” This combined outcome makes it difficult to assess the effectiveness of the treatment. Future studies of fecal microbiota therapy should carefully consider using discrete outcomes of symptom resolution and recurrence prevention to evaluate the effectiveness of this treatment. Third, the optimal source of donor feces, amount and processing method of donor stool, and timing of the procedure relative to antimicrobial use were unclear.
Randomized Controlled Trials
One new RCT was published after the systematic review by Drekonja et al.3 Cammarota et al10 studied the effect of fecal microbiota therapy via colonoscopy in patients with recurrent C. difficile infection compared with the standard vancomycin regimen. Details about the RCT by Cammarota et al10 are outlined in Table A6 (Appendix 3). To assess the results of all three RCTs together, the previously published RCTs that were included in the systematic review by Drekonja et al are also summarized in Table A6.
The open-label RCT by Cammarota et al10 (N = 39 patients) has inclusion criteria (recurrent C. difficile infection), comparison groups (fresh fecal microbiota therapy vs. vancomycin), and a primary end point (resolution of diarrhea associated with C. difficile infection without relapse after 10 weeks) similar to those of the previously published open-label RCT by Van Nood et al (N = 29 patients).17 Both RCTs reported a priori cases involving patients who developed recurrent C. difficile infection after the first donor feces infusion and were given a second infusion of feces.10,17 For patients in the infusion groups who required a second infusion of donor feces, follow-up was extended to 10 weeks after the second infusion.10,17 The main difference between the studies was the route of administration; the RCT by Cammarota et al10 used colonoscopy and the RCT by Van Nood et al17 used a nasogastric tube.
The open-label RCT by Youngster et al18 compared nasogastric tube versus colonoscopic delivery of previously frozen fecal microbiota in patients with recurrent and refractory C. difficile infection.
Resolution of Clostridium difficile Infection
In the study by Cammarota et al,10 fecal microbiota therapy via colonoscopy achieved significantly higher resolution rates of diarrhea associated with C. difficile infection than vancomycin treatment alone (18/20 [90%] vs. 5/19 [26%], P < .0001).
Initially, 13 of 20 (65%) patients were cured after their first fecal microbiota infusion.10 The seven remaining patients were also diagnosed with pseudomembranous colitis. Six of these patients received multiple infusions (four received two infusions, one patient received three infusions, and one underwent four infusions), and one patient received one infusion.10
Five of the seven patients with pseudomembranous colitis were cured of diarrhea associated with C. difficile infection; two patients still had symptoms and received one or two fecal microbiota infusions but died of C. difficile–related complications.10 All five of the seven patients with pseudomembranous colitis received a fecal microbiota infusion every 3 days until the colitis resolved.10
In the vancomycin group, 5 of 19 (26%) patients were cured of diarrhea associated with C. difficile infection.10 In two cases that were refractory to antibiotic treatment, patients died of C. difficile–related complications. Twelve patients had a recurrence of C. difficile. Median time to recurrence was 10 days (range 4–21 days). At the time of recurrence, these patients had been discharged home, and the authors were not able to offer them fecal infusion.10
Cammarota et al10 noted that no patient refused the proposed treatment or expressed concerns about any aspect of fecal microbiota therapy.
Van Nood et al17 reported that, in 13 of 16 (81%) patients receiving fecal microbiota therapy, C. difficile–associated diarrhea resolved after the first infusion. When the three remaining patients received a second infusion, two of the three achieved resolution of symptoms. In the group receiving vancomycin alone, symptoms of C. difficile resolved in 4 of the 13 (31%) patients. Clostridium difficile symptoms resolved in 3 of the 13 (23%) patients receiving vancomycin and lavage (P < .001 in overall cure rates for both comparisons with the group receiving fecal microbiota therapy).17
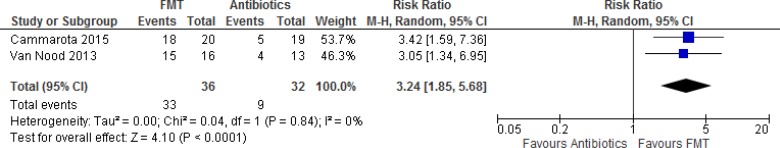
With inclusion criteria, comparison groups, follow-up duration, and primary end points similar to those in the RCTs by Cammarota et al10 and Van Nood et al,17 a meta-analysis was conducted to determine overall resolution of diarrhea associated with C. difficile infection between patients who received fecal microbiota versus vancomycin (Figure 2). In the study by Van Nood et al,17 the group receiving vancomycin alone was used as the control group for the meta-analysis. Fecal microbiota therapy significantly improved overall resolution of diarrhea associated with C. difficile infection in patients with recurrent C. difficile infection compared with treatment with vancomycin (summary risk ratio 3.24, 95% confidence interval [CI] 1.85–5.68). Patients who received fecal microbiota therapy were three times as likely as patients receiving antibiotics to have their diarrhea symptoms successfully treated. The GRADE quality of evidence is moderate.
Figure 2: Meta-analysis of Overall Resolution of Diarrhea Associated With CDI in Randomized Controlled Trials Comparing FMT With Vancomycin.
Abbreviations: CDI, Clostridium difficile infection; CI, confidence interval; df, degrees of freedom; FMT, fecal microbiota therapy; M-H, Mantel-Haenszel test.
Youngster et al18 reported symptoms resolved in 8 of 10 patients in the colonoscopy group and in 6 of 10 patients in the nasogastric group (P = .628). One patient in the nasogastric group refused subsequent retreatment. The remaining five patients were given a second fecal microbiota infusion at a mean of 4.9 days (standard deviation 2.1 days) after first fecal microbiota treatment.18 All five patients requested fecal microbiota be delivered via the nasogastric route. Subsequently, four of the five patients were cured of diarrhea associated with C. difficile infection. Overall, 8 of 10 (80%) patients in the nasogastric group and 10 of 10 (100%) patients in the colonoscopy group were cured of diarrhea associated with C. difficile infection (P = .53).18
Quality of Life
None of the RCTs reported outcomes for quality of life.
Youngster et al18 found that the self-reported heath rating using a 10-point standardized questionnaire (1 was lowest and 10 was “best recent health baseline”) increased over the study period from a median of 5 (interquartile range 3–6) and 4 (interquartile range 2–5) in the colonoscopy and nasogastric groups, respectively, the day before fecal microbiota therapy (P = .44) to 8 (interquartile range 7–10) and 7 (interquartile range 5–8), respectively, 8 weeks after infusion. No statistical test compared self-reported health rating before fecal microbiota therapy with that 8 weeks after fecal microbiota treatment for either route of administration. The colonoscopy group had higher health scores accounted for by a higher reported score the day before fecal microbiota therapy. The groups did not differ regarding absolute change in scores (P = .51).18
Mortality
In the RCT by Cammarota et al, the first two patients in the fecal microbiota therapy group had pseudomembranous colitis.10 The first patient had a recurrence of C. difficile infection and received a second fecal microbiota infusion. The patient underwent another recurrence of C. difficile infection and started vancomycin but died of sepsis after 1 week. The second patient with pseudomembranous colitis was affected by severe cardiopathy and had a recurrence of C. difficile infection. Given the patient's deterioration, the authors could not offer a second fecal microbiota infusion. The patient received vancomycin but died 15 days later.10
In the vancomycin group, 2 of the 19 patients did not benefit from antibiotic treatment and died of C. difficile–related complications.10
In the RCT by Van Nood et al,17 the death of one patient from severe heart failure and chronic obstructive pulmonary disease in the vancomycin-only group was considered to be unrelated to the study drug. No patients died in the fecal microbiota therapy group.17
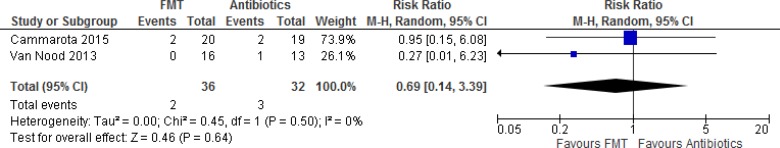
A meta-analysis was conducted to determine mortality in patients who received fecal microbiota compared with vancomycin therapy for the treatment of recurrent C. difficile infection (Figure 3). Overall, there was no significant difference in mortality between patients who received fecal microbiota therapy and those who received vancomycin (summary risk ratio 0.69, 95% CI 0.14–3.39). The GRADE quality of evidence was low.
Figure 3: Meta-analysis of Mortality in Randomized Controlled Trials Comparing Fecal Microbiota Therapy With Vancomycin.
Abbreviations: CI, confidence interval; df, degrees of freedom; FMT, fecal microbiota therapy; M-H, Mantel-Haenszel test.
In the RCT by Youngster et al,18 one patient died 12 weeks after the procedure while hospitalized secondary to acute exacerbation of chronic obstructive pulmonary disease, including bleb (air sac) rupture requiring intubation and a chest tube. Although she was treated for several weeks with parenteral broad-spectrum antimicrobials, her C. difficile infection did not recur. Another patient died of metastatic laryngeal cancer 21 weeks after the procedure. A third patient was diagnosed with adenocarcinoma of the esophagus.18 A fourth patient, treated by the upper gastrointestinal route, was hospitalized for Fournier gangrene (necrotizing fasciitis or gangrene usually affecting the perineum).18
Adverse Events
In the study by Cammarota et al,10 19 of 20 patients who received fecal microbiota therapy (95%) had diarrhea immediately after fecal infusion and 12 of 20 (60%) patients had bloating and abdominal cramping (symptoms resolved within 12 hours in all patients). No adverse events were reported in the vancomycin group.10
Van Nood et al17 reported that, immediately after fecal microbiota therapy, 15 of 16 patients had diarrhea (94%). Cramping in 5 of 16 (31%) patients and belching in 3 of 16 (19%) patients were also reported. In all patients, these symptoms resolved within 3 hours. No other adverse events related to study treatment were reported. No adverse events were reported in the vancomycin group.
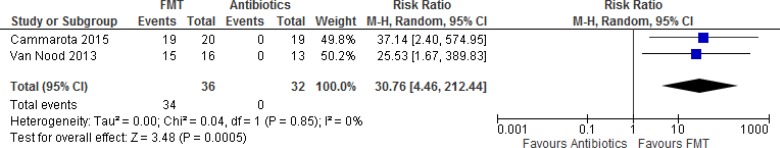
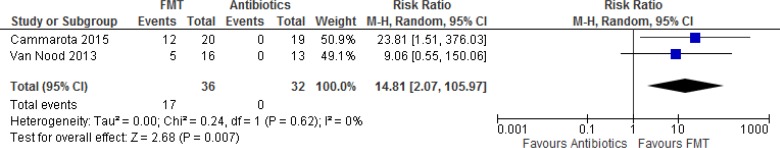
A meta-analysis was conducted to assess adverse events in patients who received fecal microbiota therapy compared with vancomycin for the treatment of recurrent C. difficile infection (Figure 3). Overall, there were significant differences in treatment-related diarrhea and abdominal cramps between patients who received fecal microbiota therapy compared with vancomycin (summary risk ratios 30.76, 95% CI 4.46–212.44, and 14.81, 95% CI 2.07–105.97, respectively) (Figures 4 and 5). Patients treated with fecal microbiota therapy were 30 times more likely to have treatment-related diarrhea and abdominal cramping than those receiving vancomycin. The GRADE quality of evidence was low.
Figure 4: Meta-analysis of Adverse Event of Treatment-Related Diarrhea in Randomized Controlled Trials Comparing Fecal Microbiota Therapy With Vancomycin.
Abbreviations: CI, confidence interval; df, degrees of freedom; FMT, fecal microbiota therapy; M-H, Mantel-Haenszel test.
Figure 5: Meta-analysis of Adverse Event Abdominal Cramps in Randomized Controlled Trials Comparing Fecal Microbiota Therapy With Vancomycin.
Abbreviations: CI, confidence interval; df, degrees of freedom; FMT, fecal microbiota therapy; M-H, Mantel-Haenszel test.
Youngster et al18 reported that adverse events likely to be related to fecal microbiota therapy included mild abdominal discomfort and bloating in 4 of 20 patients (20%).
Limitations of and Comments About the Randomized Controlled Trials
The randomized controlled trials had several limitations.
In the study by Cammarota et al, pseudomembranous colitis was present in 35% of patients with recurrent C. difficile infection.10 According to the authors, patients with pseudomembranous colitis required multiple fecal microbiota infusions to be cured.10 Patients in the vancomycin group did not undergo colonoscopy, and it is unknown how many patients treated with vancomycin had pseudomembranous colitis.10
All RCTs had small sample sizes, and meta-analyses generally yielded large confidence intervals for the summary estimates. The power calculation in the RCT by Van Nood et al17 was based on the efficacy of vancomycin for a first recurrence of C. difficile infection. Most patients had several relapses before inclusion. Therefore, the efficacy of vancomycin was lower than expected, which could have contributed to the findings. Cammarota et al10 confirmed the low response rate of a vancomycin regimen in curing patients with recurrent C. difficile infection (26% vs. the 31% reported by van Nood et al). Before their inclusion in the study, most patients had had relapses after previous vancomycin-based treatments. This exposure most likely contributed to the poor results of the vancomycin regimen in both studies.
The RCT by Youngster et al18 was a small feasibility study and not powered to detect a difference between the nasogastric versus colonoscopic administration of fecal microbiota.
It is unclear what standardized questionnaire was used to assess self-reported health in the RCT by Youngster et al (no reference was provided).18
Observational Studies
Details of the six observational studies are summarized in Table A8.11–16 All studies were uncontrolled, retrospective case series with sample sizes ranging from 6 to 61 patients. Patients received fecal microbiota therapy because of recurrent C. difficile infection in all six studies.11–16 Three studies specifically reported patients as having recurrent and refractory C. difficile infection.13,15,16 In terms of route of administration of fecal microbiota therapy, four studies used colonoscopy,12,13,15,16 one study used orally administered capsules,11 and one study used nasogastric tubing.14
Resolution of Clostridium difficile Infection
Overall, resolution or cure rates of C. difficile–associated diarrhea ranged from 89% to 100%.11–16
For most patients in the case series, C. difficile infection–associated diarrhea resolved after the first fecal microbiota treatment was administered (range 55%–100%).11–16 The total number of times fecal microbiota were administered for complete resolution of C. difficile infection–associated diarrhea in the studies ranged from one to three.11–13,16
Quality of Life
Quality of life was not reported in any of the case series.
Mortality
Hirsch et al reported one death in the case series of 19 patients.11 This 84-year-old man had dementia, coronary artery disease, congestive heart failure, arthritis, and non-Hodgkin's lymphoma. He had recurrent symptoms consistent with C. difficile within 2 to 4 weeks of each of four fecal microbiota therapy attempts.11 He required hospitalization for diarrhea, dehydration, and acute kidney injury. The diarrhea resolved with oral vancomycin and rifaximin. He developed health care–acquired pneumonia, which was treated with systemic antimicrobial therapy. Oral vancomycin was continued. He did not develop recurrent diarrhea, but died of respiratory failure. His death was considered unrelated to the fecal microbiota therapy.11
Two case series did not report any deaths in patients who received fecal microbiota therapy.12,13
Satokari et al reported that a nonresponder in the group receiving fresh feces transplantation developed C. difficile infection after ciprofloxacin administration for urinary tract infection.15 She had atherosclerosis and was receiving long-term dialysis. Despite C. difficile treatment with antibiotics, the patient died of multiple medical problems 2 months after fecal microbiota treatment.15
During the year after fecal microbiota therapy, one patient in the fresh fecal microbiota therapy group died of unrelated illnesses.15 In the group receiving frozen fecal microbiota transplants, two patients had a relapse of C. difficile infection.15 In these cases, C. difficile infections were subsequently treated with antibiotics. Both patients died, one of arterial thrombosis in the lower limb and the other one of the C. difficile infection.15
Fischer et al reported three deaths associated with C. difficile infection: (1) death of sepsis within 24 hours of the first fecal microbiota treatment; (2) death of a patient who failed to benefit from three courses of fecal microbiota therapy following colectomy 6 weeks after orthotopic liver transplantation; and (3) death of sepsis after being treated with antibiotics for a urinary tract infection 92 days following the first fecal microbiota treatment.16 Five patients died of causes unrelated to C. difficile infection.16
The overall cumulative survival after the first fecal microbiota treatment was 93% (95% CI 84–100) at 1 month and 76% (95% CI 62–93) at 3 months.16
Lagier et al reported global and 1-month mortality in elderly patients (mean age 84 years, range 66–101 years) who received fecal microbiota therapy.14 Patients were divided into two groups: antibiotics plus late fecal microbiota therapy (patients were treated with antibiotics; fecal microbiota therapy was used only in cases of a least three treatment failures or relapses) and antibiotics plus early fecal microbiota therapy (antibiotics and fecal microbiota therapy were offered early during the first week following diagnosis).14 Most patients in the late fecal microbiota therapy group received only antibiotics; three patients were also treated with fecal microbiota therapy.14
There was a significant difference in global mortality between the two patient groups: 3 of 16 (19%) who received early fecal microbiota therapy versus 29 of 45 (64%) who received late fecal microbiota therapy (P < .001).14 There was also a significant difference in 1-month mortality between the groups: 1 of 16 (6%) who received early fecal microbiota therapy versus 24 of 43 (56%) who received late fecal microbiota therapy (P < .0003).14
Of the 40 patients treated only by antibiotics in the group receiving late fecal microbiota therapy, 23 died before 1 month (58%).14 Among these 23 patients, 17 patients (74%) died during the first week following diagnosis. Among the three patients treated by antibiotics and late fecal microbiota therapy, 1-month mortality was one of three (33%).14
Lagier et al14 reported that antibiotics and early fecal microbiota therapy was associated with a significant decrease in mortality compared with antibiotics and late fecal microbiota therapy (log-rank test P < .001).
Adverse Events
Adverse events reported in the studies included abdominal pain that was reported in 5 of 19 patients from Hirsch et al (mild and transient in four patients and moderate to severe in one patient who also had irritable bowel syndrome, but pain subsided 3 days after fecal microbiota treatment).11
Ray et al12 reported adverse events in 5 of 20 patients during an 8-month follow-up:
One had pain or nausea after colonoscopy
One continued to have diarrhea (but results for C. difficile remained negative during 8 months of follow-up)
One had bloating or cramps daily “consistent with her pre-existent inflammatory bowel disease symptoms. The patient stated that the symptoms did not worsen after the procedure”
One had flatulence and nausea for a few weeks after fecal microbiota therapy but noted an improvement in the symptoms of diarrhea
One reported, more than a month later, that she suffered a cerebrovascular accident at another hospital and had complications, including persistent nausea and vomiting with abdominal pain” after eating that eventually resolved
Lagier et al14 reported that, of 33 elderly patients treated with fecal microbiota procedures (including those treated with successive fecal microbiota treatments), 24 patients (73%) had treatment-related diarrhea that resolved on the next day. For adverse events, Lagier et al also reported that one patient refused the nasogastric tube on the day of transplantation, one patient had uncontrollable nausea caused by the nasogastric tube, and one patient presented with acute heart failure.
Limitations of and Comments About the Observational Studies
The observational studies had limitations.
All studies were retrospective case series. Primary outcomes were reported as a combination of resolution of symptoms and prevention of recurrence.11–16
The use of antibiotics for treatment of recurrent C. difficile infection around the time of fecal microbiota administration varied across studies. Some studies11,13,15,16 discontinued antibiotics 24 to 48 hours before fecal microbiota treatment. Several studies resumed antibiotic and repeat fecal microbiota therapy if patients experienced recurring C. difficile symptoms.11,16 Ray et al12 stated that all patients received antibiotic treatment (vancomycin, metronidazole, or fidaxomicin) for C. difficile infection before fecal microbiota treatment; however, it is unclear whether patients continued antibiotic therapy during and after fecal microbiota therapy. Lagier et al14 reported outcomes of patients who received antibiotics (vancomycin, metronidazole, or fidaxomicin) and fecal microbiota therapy simultaneously.
Discussion
Beyond the six patients in the case series identified by Drekonja et al,3 no additional studies of patients treated with fecal microbiota for initial C. difficile infection were identified in the updated literature search. All studies in this systematic review included patients with recurrent C. difficile infection. However, a few studies explicitly stated that patients were included if they had recurrent or refractory C. difficile infection.13,15,16 International guidelines (Appendix 5) on the use of fecal microbiota therapy all specifically refer to patients with recurrent C. difficile infections.1,22–24 Health Canada currently provides a provisional interpretation that allows fecal microbiota to be used to treat patients with recurrent C. difficile infection unresponsive to conventional therapies.4
Overall, results of observational studies were generally consistent with results from RCTs. The resolution of diarrhea associated with recurrent C. difficile infection was the primary outcome for all studies. Adverse events associated with fecal microbiota therapy were generally minimal and short term (diarrhea, abdominal cramping). Quality of life was not reported as an outcome in any of the studies in this systematic review.
The route of administration for fecal microbiota varied across studies. The only study included in this systematic review that compared different routes of administration was a small RCT.18 Youngster et al found no significant difference in resolution rates for administration of fecal microbiota therapy via nasogastric tube versus colonoscopy; however, the RCT was considered a feasibility study and not statistically powered to detect a difference between the two routes of administration.18
An expert consultant stated that anecdotal evidence increasingly indicates that multiple administrations are required for most cases of recurrent C. difficile infection to fully resolve (Dr. Susy Hota, written communication, October 19, 2015). The frequency and timing of repeat fecal microbiota treatment is unclear and could need to be tailored to individual cases (Dr. Susy Hota, written communication, October 19, 2015). It is also unclear whether different donors should be used for repeat administration of fecal microbiota (in hopes of eventually getting the right “microbiome match”) (Dr. Susy Hota, written communication, October 19, 2015).
Conclusions
In patients with recurrent C. difficile infection:
Fecal microbiota therapy is effective in resolving diarrhea associated with C. difficile infection compared with antibiotics (GRADE: moderate)
There is insufficient evidence to conclude that fecal microbiota therapy reduces mortality compared with antibiotics (GRADE: low)
Fecal microbiota therapy is associated with a significant increase in adverse events, specifically treatment-related diarrhea and abdominal cramping compared with antibiotics (GRADE: low). In the studies, these adverse events were short lived and resolved successfully
ECONOMIC EVIDENCE REVIEW
Objectives
This economic section of the health technology assessment reviewed the literature for the cost-effectiveness of fecal microbiota therapy compared with antibiotic treatment in adults with recurrent C. difficile infection.
Methods
Sources
We performed an economic literature search on August 4, 2015, using Ovid MEDLINE, Ovid MEDLINE In-Process, Ovid Embase, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects (DARE), Centre for Reviews and Dissemination (CRD) Health Technology Assessment Database, and National Health Service (NHS) Economic Evaluation Database, for studies published from January 1, 2000, to August 4, 2015. We also extracted economic evaluation reports developed by health technology assessment agencies by searching the websites of the Canadian Agency for Drugs and Technologies in Health, Institute of Health Economics, Institut national d'excellence en sante et en services, McGill University Health Centre Health Technology Assessment Unit, and Cost-Effectiveness Analysis (CEA) Registry (available at https://research.tufts-nemc.org/cear4). Finally, we reviewed reference lists of included economic literature for any additional relevant studies not identified through the systematic search.
Literature Screening
We based our search terms on those used in the clinical evidence review of this health technology assessment and applied economic filters to the search results. Study eligibility criteria for the literature search are listed below. A single reviewer reviewed titles and abstracts and, for those studies meeting the inclusion and exclusion criteria, we obtained full-text articles.
Inclusion Criteria
English-language full-text publications
Studies published between January 1, 2000, and August 4, 2015
Studies in adults who had initial, recurrent or refractory C. difficile infection
Studies of fecal microbiota therapy (via variable routes of administration and variable timing and frequency) for C. difficile infection and recurrent C. difficile infection
Studies where the comparators were standard antibiotic treatment
Exclusion Criteria
Animal and in vitro studies
Editorials, case reports, or commentaries
Studies of fecal microbiota therapy for indications other than C. difficile infection or recurrent C. difficile infection
Outcomes of Interest
Full economic evaluations: cost-utility analyses, cost-effectiveness analyses, cost-benefit analyses
Data Extraction
We extracted relevant data on the following:
Source (i.e., name, location, year)
Study design (perspective, time horizon) and population
Indications, interventions, and comparators
Results: outcomes (i.e., health outcomes, costs, and cost-effectiveness)
Limitations
The review was conducted by a single reviewer, and the search was limited to 15 years.
Results
Literature Search
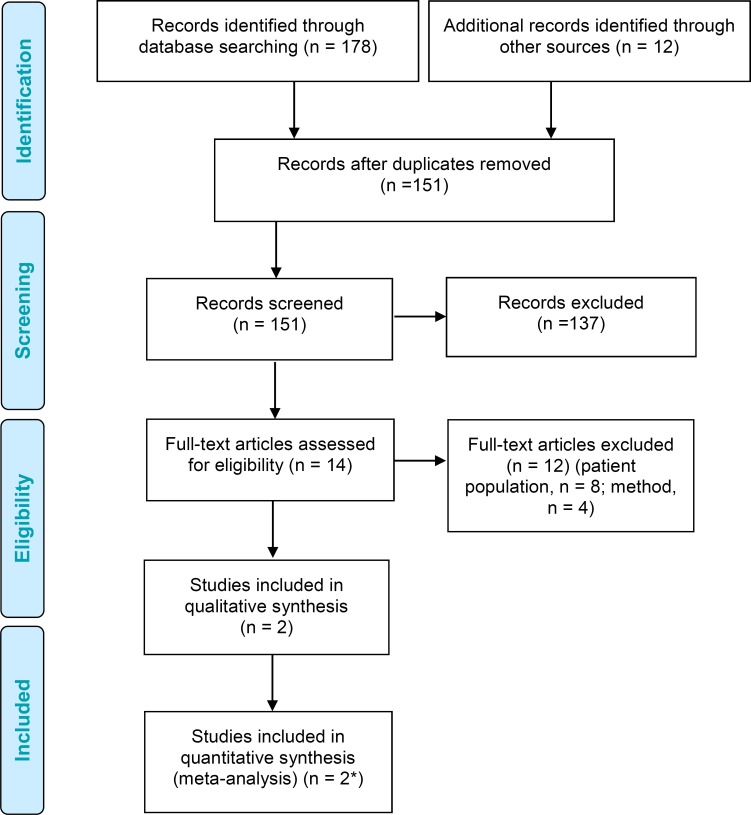
The database search yielded 151 citations published between January 1, 2000, and August 4, 2015 (with duplicates removed). A longer (15-year) time horizon was used in the literature search to ensure that all relevant economic evaluations were captured based on the scoping phase. We excluded a total of 137 articles from information in the title, abstract, and full text. We then examined the full texts of 14 potentially relevant articles for further assessment. Figure 6 presents the flow diagram for the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) adapted for this economic review.
Figure 6: Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) Flow Diagram.
*Incorporates same studies included in qualitative synthesis.
Source: Adapted from Moher et al.9
Two studies met the inclusion criteria. We hand-searched the reference lists of the included studies and health technology assessment websites to identify other relevant studies, and no additional citations were included.
Critical Review
The two economic evaluations meeting the inclusion criteria are summarized and appraised in Table 1.
Table 1:
Results of Economic Literature Review for Fecal Microbial Therapy—Summary
| Name, Year, Location | Study Design, Time Horizon, and Perspective | Population and Indication | Interventions and Comparators | Results | ||
|---|---|---|---|---|---|---|
| Health Outcomes QALYs, Cure Rates | Costs | Cost-Effectiveness | ||||
| Varier et al, 201525 United States |
Design Decision-analytic model Time horizon 90 days Perspective Third-party payer |
Population RCDI patients Indication FMT for first-line treatment of RCDI patients |
Interventions FMT colonoscopy Comparator Vancomycin |
FMT 0.242 83%–100% Vancomycin 0.235 59%–75% |
FMT $1,669 vs. vancomycin $3,788 Discount No discounting necessary because simulated patients in model were followed for 90 days |
Dominant |
| Konijeti et al, 201426 United States |
Design Decision-analytic model comparing 4 treatment strategies for first-line treatment of RCDI Time horizon 1 year Perspective Societal |
Population RCDI patients Indication FMT for first-line treatment of RCDI in hypothetical cohort |
Interventions FMT colonoscopy Comparators Metronidazole, vancomycin, fidaxomicin |
FMT 0.8719, 94.5% Vancomycin 0.8580, 91.6% Metronidazole 0.8292, 71% Fidaxomicin 0.8653, 93.7% |
Cost FMT $3,149 Vancomycin $2,912 Metronidazole $3,941 Fidaxomicin $4,261 Discount No discounting necessary because simulated patients in model were followed for 1 year |
FMT compared with vancomycin: ICER $17,016 per QALY FMT vs. metronidazole Dominant FMT vs. fidaxomicin Dominant |
Abbreviations: FMT, fecal microbiota transplant; ICER, incremental cost-effectiveness ratio; QALY, quality-adjusted life-year; RCDI, recurrent Clostridium difficile infection.
Methodologic Quality of Included Studies
The two studies were directly applicable or partially applicable to the research question and were deemed relevant to the eligible patient population.
Discussion
Varier et al25 constructed a decision-analytic model using inputs from the published literature to compare standard vancomycin treatment with fecal microbiota therapy for recurrent C. difficile infection. This analysis was completed from a third-party payer perspective. The effectiveness measure was quality-adjusted life-years (QALYs). Fecal microbiota therapy was less costly ($1,669 vs. $3,788 USD) and more effective (0.242 vs. 0.235 QALYs) than vancomycin for recurrent C. difficile infection (Table 1). Sensitivity analyses showed that fecal microbiota therapy was the dominant treatment strategy if the cure rate for fecal microbiota therapy was higher than 70% and for vancomycin was higher than 91%, and if the cost of fecal microbiota therapy was lower than $3,206 USD. The results of this study suggest that using fecal microbiota therapy to manage recurrent C. difficile infection can save money and help reduce the economic burden on the health care system.25
Konijeti et al26 demonstrated that fecal microbiota therapy via colonoscopy is a cost-effective strategy for recurrent C. difficile infection, with an incremental cost-effectiveness ratio of $17,016 USD per QALY (Table 1) compared with antibiotic treatment (vancomycin). Fecal microbiota therapy was also dominant—less costly and more effective—than metronidazole and fidaxomicin for recurrent C. difficile infection. The decision model constructed for this analysis suggested that treatment with fecal microbiota via colonoscopy would have cure rates of 88% or higher and recurrence rates of less than 15%; this is consistent with findings from the study performed by Brandt et al,27 which reported fecal microbiota therapy cure rates to be greater than 90%. Considering the costs and training required to perform fecal microbiota transplant, the analysis strongly suggested a need for standardized routes of administration for fecal microbiota if the treatment is to be used frequently for recurrent C. difficile infection.
After reviewing these two studies and the existing clinical studies, we decided against developing a full economic model. The data would have been similar to the data in these two evaluated economic studies, and the evidence presented about the cost-effectiveness of fecal microbiota therapy in these studies was sufficient for the Ontario context.
Conclusions
One of the two economic evaluations concluded that fecal microbiota therapy can save money compared with standard (vancomycin) treatment. The study showed that fecal microbiota therapy is dominant (less expensive, more effective) over metronidazole and fidaxomicin because of the higher observed cure rates.25 The second economic evaluation concluded fecal microbiota therapy is a cost-effective strategy for managing recurrent C. difficile infection.26
BUDGET IMPACT ANALYSIS
We conducted a budget impact analysis from the perspective of the Ontario Ministry of Health and Long-Term Care to determine the estimated cost burden of C. difficile infection for 1 year (2015) and the potential costs of fecal microbiota therapy for recurrent C. difficile infection over the next 3 years. All costs are reported in 2015 Canadian dollars. Clostridium difficile infection includes both initial and recurrent infections, and recurrent C. difficile infection refers to one or more episodes after an initial infection with C. difficile.
Objectives
Our objectives were to estimate:
The 1-year cost to the Ministry of Health and Long-Term Care of C. difficile infections and the corresponding 1-year cost of treating these infections with fecal microbiota therapy
The potential costs to the Ministry of Health and Long-Term Care over the next 3 years of using fecal microbiota therapy for recurrent C. difficile infection among eligible patients
Methods
Target Population
We created a budget impact model to address the 1-year (2015) impact of C. difficile infection on the Ontario health care system using the reported volume of episodes multiplied by the cost of treatment to patients. The total number of C. difficile cases (both initial and recurrent) was reported to be 5,810 in 2014/2015; this was used as the prevalent year. Data were obtained by Health Quality Ontario from the Ministry of Health and Long-Term Care (Health Analytics Branch, written communication, October 27, 2015).
Next, we determined the potential impact to the ministry of fecal microbiota therapy for recurrent C. difficile infections currently treated with standard antibiotics (vancomycin and metronidazole). It is estimated that recurrent C. difficile infections account for 27% of total C. difficile cases.28 The impact of fecal microbiota therapy on the ministry's budget was calculated for a fixed number of procedures on the basis of expert opinion.
Canadian Costs
Cost parameters were calculated from several sources (Tables 2 and A10):
Table 2:
Average Cost Associated With CDI and RCDI Treatment per Episode
| Cost Parameter | Cost, $ | Source/Notes |
|---|---|---|
| Community-Based Treatment | ||
| FMT colonoscopy | 1,429 | Varier et al, 2015,25 Biltaji et al, 2014, and Guo et al, 201132 |
| Total cost per patient with CDI | 542 | Assumed that all patients receive vancomycin |
| Total cost per RCDI episode | 574 | Assumed that all patients receive vancomycin |
| Average cost per FMT treatment of RCDI | 1,866 | Calculated from Levy et al, 2015,28 Varier et al, 2015,25 Biltaji et al, 2014,33 and Guo et al, 201132 |
| Hospital-Based Treatment | ||
| Total cost per patient with RCDI | 16,096 | Calculated from Levy et al, 2015,28 Varier et al, 2015,25 Biltaji et al, 2014,33 and Guo et al, 201132 |
| Cost per RCDI FMT treatment | 9,422 | Calculated from Levy et al, 2015,28 Varier et al, 2015,25 Biltaji et al, 2014,33 and Guo et al, 201132 |
Abbreviations: CDI, Clostridium difficile infection; FMT, fecal microbiota therapy; RCDI, recurrent Clostridium difficile infection.
Analysis
The 1-year (2015) cost impact of the 5,810 episodes (2014/2015) of C. difficile infection (initial and recurrent) on the Ontario care system was calculated. This cost included both hospital- and community-based treatments in Ontario. It is estimated that 53% of total C. difficile infections receive hospital-based treatment and 47% receive community-based treatment.28 The 1-year cost impact was calculated from the product of the number of C. difficile infection episodes (initial and recurrent), the percentage of cases per treatment location (hospital versus community), and the cost associated with both the place and type of infection (initial versus recurrent).
The base case for fecal microbiota treatment of recurrent C. difficile infection was calculated based on an expert estimate of about 500 to 1,000 procedures being performed per year in Ontario (C. Lee, written communication, October 27, 2015). The analysis assumed that 500 fecal microbiota procedures will be performed in year 1 of introduction, with a 50% annual increase, reaching a maximum of 1,000 fecal microbiota procedures in year 3 (Table 4). Patients with recurrent C. difficile infection are usually treated with standard antibiotics (vancomycin and metronidazole) in the hospital or community.28 For community-based treatment, we assumed that all patients are treated with a standard regimen of 10 to 14 days of vancomycin. All antibiotic treatments were assumed to be publicly funded. The budget impact was calculated from the difference in the total cost of treating recurrent C. difficile infection with standard antibiotic therapy and the total cost of treating these patients with fecal microbiota therapy in hospitals and communities.
Table 4:
Three-Year Budget Impact of FMT for RCDI in Ontario
| Year | Number of Patients Receiving FMT | Estimated Total Cost, $ in Millionsa |
|---|---|---|
| 1 | 500 | −1.5 |
| 2 | 750 | −2.2 |
| 3 | 1,000 | −2.9 |
| Total | 2,250 |
Abbreviations: CB, community based; FMT, fecal microbiota therapy; HB, hospital based; RCDI, recurrent Clostridium difficile infection.
[(RCDITotal × 53%) × Cost FMThb] + [(RCDIcb × 47%) × Cost FMTcb].
Sensitivity analyses were performed on two key parameters in the budget impact model: the proportion of infections treated in the hospital (70%) versus the community (30%). This proportion was based on that in the published literature.28 The cost of fecal microbiota procedures was discounted by 25%. In Ontario, the fecal transplant is generally administered via enema, which is less costly than colonoscopy (C. Lee, oral communication, August 5, 2015); colonoscopy accounts for about 25% (20%–30%) of the fecal microbiota therapy costs.
Results
Base Case
In 2014/2015, our model suggested that C. difficile infection in Ontario was associated with costs of about $47.8 million dollars. If all cases of recurrent C. difficile infection had been eligible for and treated with fecal microbiota therapy, there would have been a potential reduction of about $5.2 million in the overall treatment cost (Table 3).
Table 3:
Cost to Ontario of CDI Antibiotic Treatment in 2014/2015 and Potential Total Yearly Cost of FMT
| Treatment Subgroups | Target Population | Estimated Total Cost, $ in Millions |
|---|---|---|
| Current standard treatment (antibiotics) in Ontario (HB + CB) | 5,810a | 47.8c |
| Standard treatment (antibiotics) for recurrent CDIs (HB + CB) in patients eligible for FMT | 1,575b | 13.9d |
| FMT treatment (HB + CB) for recurrent CDIs in eligible patients | 1,575 | 8.7e |
| Net budget impact of FMT for recurrent CDIs | –5.2f |
Abbreviations: CB, community based; CDI, Clostridium difficile infection; FMT, fecal microbiota therapy; HB, hospital based; RCDI, recurrent Clostridium difficile infection.
Total C. difficile infections (initial and recurrent) in 2014/2015: Health Analytics Branch, Ministry of Health and Long-Term Care.
Recurrent C. difficile infections (27.1% of 5,810).
[(CDITotal × 53%) × Cost CDIhb] + [(CDITotal × 47%) × Cost CDIcb] + [(RCDITotal × 53%) × Cost RCDIhb] + [(RCDIcb × 47%) × Cost RCDIcb].
[(RCDITotal × 53%) × Cost RCDIhb] + [(RCDIcb × 47%) × Cost RCDIcb].
[(RCDITotal × 53%) × Cost FMThb] + [(RCDIcb × 47%) × Cost FMTcb].
Difference between e and d.
Over the next 3 years, an estimated total of 2,250 (Σ Year 1+Year 2+ Year 3) fecal microbiota procedures could be performed in Ontario for recurrent C. difficile infection. If fecal microbiota therapy were adopted in Ontario to treat recurrent C. difficile infection, and considering it from the perspective of the Ministry of Health and Long-Term Care as the payer, an estimated $1.5 million would be saved after the first year of adoption and $2.9 million after 3 years (Table 4).
Sensitivity Analysis
The budget impact is sensitive to the proportion of patients treated in the hospital (Table 5) and the cost of fecal microbiota therapy (Table 6). Whether we increase the proportion of patients treated in the hospital to 70% or decreased the cost of fecal microbiota treatment by 25%, the impact to the Ministry of Health and Long-Term Care is potentially net savings (Tables 5 and 6).
Table 5:
Three-Year Budget Impact of FMT for RCDI in Ontario: Number of Patients Treated in Hospital Increased to 70%
| Year | Number of Patients Receiving FMT | Estimated Total Cost, $ in Millionsa |
|---|---|---|
| 1 | 500 | −2.1 |
| 2 | 750 | −3.2 |
| 3 | 1,000 | −4.3 |
| Total | 2,250 |
Abbreviations: CB, community based; FMT, fecal microbiota therapy; HB, hospital based; RCDI, recurrent Clostridium difficile infection.
[(RCDlTotal × 70%) × Cost FMThb] + [(RCDIcb × 30%) × Cost FMTcb].
Table 6:
Three-Year Budget Impact of FMT for RCDI: Cost of FMT Decreased by 25%
| Year | Number of Patients Receiving FMT | Estimated Total Cost, $ in Millionsa |
|---|---|---|
| 1 | 500 | −1.6 |
| 2 | 750 | −2.5 |
| 3 | 1,000 | −3.3 |
| Total | 2,250 |
Abbreviations: CB, community based; FMT, fecal microbiota therapy; HB, hospital based; RCDI, recurrent Clostridium difficile infection.
[(RCDlTotal × 53%) × 75% × Cost FMThb] + [(RCDIcb × 47%) × 75% × Cost FMTcb].
Limitations
The number of C. difficile infections in Ontario is based on 2014/2015 numbers and includes both the initial and recurrent cases. This might underestimate costs as some experts believe symptoms might resolve in some patients before an actual diagnosis of C. difficile infection is made.
Presently the distribution of recurrent C. difficile infections treated in hospital versus the community is difficult to estimate because there is no consistency in reporting.28 Hence, we assumed that treatment of recurrent C. difficile infections has the same distribution as treatment of initial C. difficile infections: 53% in hospital and 47% in the community.
We assumed that all patients treated in the community received a standard regimen of 10 to 14 days of vancomycin, and we included this as a cost to the Ministry of Health and Long-Term Care. This assumption may present an overestimation of the cost associated with these cases.
The Ontario cost for vancomycin was not available at the time of this writing, so we used the published price from Quebec. The cost in Ontario and Quebec is assumed to be equivalent because the prices for patented medicines, like vancomycin, are regulated by the Patented Medicine Prices Review Board. Therefore, the use of Quebec costs may not significantly impact the results.
The number of fecal microbiota procedures is based on expert opinion (C. Lee, written communication, October 27, 2015).
Discussion and Conclusions
Based on our analysis, C. difficile infection (both initial and recurrent episodes) in Ontario was estimated to cost $48 million in 2014/2015. We found that most of Ontario's cost (96%) is attributed to hospital-based treatment (53%) of the total initial and recurrent C. difficile episodes. Recurrent C. difficile infections account for almost half (49.4%) of the cost of treating this disease.
Some hospital centres in Ontario have championed fecal microbiota therapy for recurrent C. difficile infection. Although the number of fecal microbiota procedures performed per year is still unknown, experts estimate that 500 to 1,000 fecal microbiota transplantation procedures can be performed every year. Our analysis predicts a cost savings over the next 3 years if fecal microbiota therapy is used instead of standard antibiotic therapy to treat recurrent C. difficile infection. We increased the number of fecal microbiota procedures performed in the hospital and also decreased the price of the fecal microbiota procedure; both scenarios found cost savings if fecal microbiota therapy becomes the standard treatment for recurrent C. difficile infection.
PUBLIC AND PATIENT ENGAGEMENT ANALYSIS
Background
The primary aim of public and patient engagement in the context of health technology assessment is to “ensure that assessments and decisions are informed by the unique perspectives of those with the lived experience of a health condition and its management.”34
Patient and caregiver input can serve as a unique source of evidence about the personal impact of a disease or condition and how technology can make a difference in people's lives. It can also identify gaps or limitations in the published research (e.g., outcome measures that do not reflect what is important to patients and caregivers).35–37 Patient, caregiver, and public input can provide additional information or perspectives on the more general ethical and social-values implications of technology and treatments.
Dealing with C. difficile infection is perceived as directly affecting patients’ quality of life. To understand how fecal microbiota therapy might affect an individual's quality of life, we spoke directly with physicians who had a close relationship with the patients under their care and their families and caregivers. Our preferred approach is to speak directly with patients themselves; however, resource limitations precluded this level of engagement for this health technology assessment. Understanding and appreciating day-to-day functioning in this population helps to place the potential value of the intervention into context.
Methods
Activity and Rationale
The engagement typology we selected for this health technology assessment was a consultation.38 Consultation refers to the process of gathering information (e.g., social values, experiential input) from the public, patients, and caregivers.39
We chose to examine lived experience through physicians’ perceptions because of resourcing and staffing considerations. Having two physicians with close proximity and familiarity with the relevant patient population provided rationale for soliciting their perceptions of patients’ lived experience in this project.
Recruitment
We relied on two physicians who were clinical experts caring for individuals and families with personal experience of the infection.
Interview Questions
For the purposes of this assessment, a member of the Patient, Caregiver, and Public Engagement office at Health Quality Ontario surveyed physicians about their perceptions of their patients through a series of open-ended questions. Questions for the interview were based on a list developed by the Health Technology Assessment international Interest Group on Patient and Citizen Involvement in Health Technology Assessment to elicit responses specific to how health technology affects lived experience and quality of life.40
Survey questions focused on how C. difficile infection affects quality of life and on patients’ experiences with other health interventions, including other ongoing treatments, that are intended to manage the condition. The questions focused on patient experiences with the fecal microbiota procedure itself, any follow-up required, and any perceived benefits or limitations of the intervention. The survey is attached as Appendix 6.
Analysis
We selected a modified version of a grounded-theory method to analyze information from the surveys by coding responses and comparing themes.41,42 This approach allowed us to identify and interpret patterns in the survey data about the meaning and implications of the condition and intervention for participants’ quality of life.43
Results
Clostridium difficile and Quality of Life
Physicians perceived that all patients with C. difficile infection have lower quality of life regardless of whether the infection is a first episode or recurrent. This reduced quality of life is exacerbated if diagnosis is delayed. Examples of how C. difficile infection affects quality of life include preventing patients and their families from going to work, travelling, hosting social gatherings, and seeing other family and grandchildren.
Most patients with C. difficile infection do not leave their house during an acute episode as they experience extreme urgency and incontinence with diarrhea. Many feel socially isolated and are concerned about becoming a burden on their families. Some patients require emergency or ambulatory care, and some require hospitalization.
Many patients with recurrent C. difficile infection report feeling as though they are walking on eggshells between episodes and being extremely anxious about recurrence. They are also very concerned about transmitting the infection to loved ones.
Experiences With Other Medical Treatment
Physicians reported that most patients have little success with two antibiotic medications: metronidazole and fidaxomicin. Physicians said that many patients reported feeling better with vancomycin and indicated that this medication acts within a few days and ensures a good quality of life.
Fecal Microbiota Therapy
Generally speaking, physicians perceived that patients were happy with the processes needed to receive fecal microbiota therapy. The most cumbersome part of the experience was described as aligning the timing of donor screening with the appropriate time for intervention. A few patients reported some reservations because of an “ick” factor, relating to general unsureness about receiving feces from another person, although most were receptive to the procedure itself. Physicians reported few patients experienced discomfort during the procedure, aside from a very mild temporary cramping during the infusion.
Impact on Quality of Life
Physicians perceived that, within 2 weeks of fecal microbiota treatment, most patients were able to resume daily activities. Some patients reported a little trepidation about embarking on longer-term activities, such as travel or longer periods away from home. Some patients required multiple fecal microbiota treatments or antibiotic follow-up therapy, but for many, no follow-up therapies were required.
Discussion
Several important themes emerged from physician surveys about their perceptions of their patients and families.
One of the most important themes described by physicians was how greatly C. difficile infection influences day-to-day functioning of patients, especially for any activity that involves being away from their own homes. These activities include integral activities (such as going to work), other important daily life activities (like hosting family and friends), and even simple tasks requiring patients to leave their house (such as running errands and going to appointments). The social isolation felt by patients with recurrent C. difficile infection can be overwhelming.
While some success was described after using standard therapies, the two physicians surveyed believed that the fecal microbiota procedure seemed to restore quality of life for patients with recurrent C. difficile infection. The procedure itself did not come across as difficult or onerous to patients, with an overall perceived benefit of patients and their families being able to return to normal activities of daily living.
Conclusion
The two physicians surveyed reported that recurrent C. difficile infection seemed to significantly reduce their patients’ quality of life. The fecal microbiota procedure seemed to improve their patients’ quality of life, which speaks to the value of this intervention from the lived experience.
Acknowledgments
the medical editor was Elizabeth Jean Betsch. Others involved in the development and production of this report were Irfan Dhalla, Nancy Sikich, Andrêe Mitchell, Kellee Kaulback, Anne Sleeman, Claude Soulodre, Kristan Chamberlain, Susan Harrison, and Jessica Verhey.
We are grateful to Drs. Susy Hota and Christine Lee for their expert consultations.
Glossary
ABBREVIATIONS
- AMSTAR
Assessment of Multiple Systematic Reviews
- CI
Confidence interval
- GRADE
Grading of Recommendations Assessment, Development, and Evaluation
- PICO
Population, intervention, comparison, outcome
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-analyses
- QALY
Quality-adjusted life-year
- RCT
Randomized controlled trial
APPENDICES
Appendix 1: Literature Search Strategies
Clinical Literature Search
Search date: July 30, 2015
Databases searched: All Ovid MEDLINE, Embase, Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects, CRD Health Technology Assessment Database, Cochrane Central Register of Controlled Trials, and NHS Economic Evaluation Database
Database: EBM Reviews - Cochrane Central Register of Controlled Trials <June 2015>, EBM Reviews - Cochrane Database of Systematic Reviews <2005 to June 2015>, EBM Reviews - Database of Abstracts of Reviews of Effects <2nd Quarter 2015>, EBM Reviews - Health Technology Assessment <2nd Quarter 2015>, EBM Reviews - NHS Economic Evaluation Database <2nd Quarter 2015>, Embase <1980 to 2015 Week 30>, All Ovid MEDLINE(R) <1946 to Present>
Search Strategy:
| 1 | Clostridium difficile/ (17125) |
| 2 | Enterocolitis, Pseudomembranous/ (11518) |
| 3 | Clostridium Infections/ (6438) |
| 4 | (clostridium difficile or c difficile or c diff or clostridium enterocolitis or ((pseudomembranous or antibiotic associated) adj2 (enteritis or colitis or enterocolitis)) or clostridium infection*).tw. (26393) |
| 5 | or/1–4 (37418) |
| 6 | exp Feces/ (125351) |
| 7 | Microbiota/ (12252) |
| 8 | (((fecal or faecal or feces or faeces or stool or stools or microbiota*) adj4 (transplant* or transfus* or transfer* or infusion* or donor* or donation* or therap* or suspension)) or FMT or bacteriotherap* or human probiotic infus* or intestinal microbiome restorat*).tw. (5960) |
| 9 | or/6–8 (141077) |
| 10 | Diarrhea/th [Therapy] (6332) |
| 11 | or/9–10 (147039) |
| 12 | 5 and 11 (4285) |
| 13 | exp Animals/ not (exp Animals/ and Humans/) (8226588) |
| 14 | 12 not 13 (3967) |
| 15 | limit 14 to english language [Limit not valid in CDSR,DARE; records were retained] (3475) |
| 16 | limit 15 to yr=“2013 -Current” [Limit not valid in DARE; records were retained] (1098) |
| 17 | 16 use pmoz,cctr,coch,dare,clhta,cleed (524) |
| 18 | peptoclostridium difficile/ (773) |
| 19 | Clostridium difficile infection/ (6827) |
| 20 | Clostridium infection/ (6531) |
| 21 | pseudomembranous colitis/ (11692) |
| 22 | (clostridium difficile or c difficile or c diff or clostridium enterocolitis or ((pseudomembranous or antibiotic associated) adj2 (enteritis or colitis or enterocolitis)) or clostridium infection*).tw. (26393) |
| 23 | or/18–22 (37100) |
| 24 | feces/ (120531) |
| 25 | feces microflora/ (4066) |
| 26 | (((fecal or faecal or feces or faeces or stool or stools or microbiota*) adj4 (transplant* or transfus* or transfer* or infusion* or donor* or donation* or therap* or suspension)) or FMT or bacteriotherap* or human probiotic infus* or intestinal microbiome restorat*).tw. (5960) |
| 27 | or/24–26 (128618) |
| 28 | diarrhea/th [Therapy] (6332) |
| 29 | or/27–28 (134579) |
| 30 | 23 and 29 (4275) |
| 31 | (exp animal/ or nonhuman/) not exp human/ (9402331) |
| 32 | 30 not 31 (3929) |
| 33 | limit 32 to english language [Limit not valid in CDSR,DARE; records were retained] (3452) |
| 34 | limit 33 to yr=“2013 -Current” [Limit not valid in DARE; records were retained] (1143) |
| 35 | 34 use emez (649) |
| 36 | 17 or 35 (1173) |
| 37 | 36 use pmoz (507) |
| 38 | 36 use emez (649) |
| 39 | 36 use cctr (8) |
| 40 | 36 use coch (0) |
| 41 | 36 use dare (3) |
| 42 | 36 use clhta (4) |
| 43 | 36 use cleed (2) |
| 44 | remove duplicates from 36 (829) |
Economic Literature Search
Search date: August 4, 2015
Databases searched: Ovid MEDLINE, Ovid MEDLINE In-Process, Ovid Embase, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects (DARE), Centre for Reviews and Dissemination (CRD) Health Technology Assessment Database and National Health Service (NHS) Economic Evaluation Database
Database: EBM Reviews - Cochrane Central Register of Controlled Trials <June 2015>, EBM Reviews - Cochrane Database of Systematic Reviews <2005 to June 2015>, EBM Reviews - Database of Abstracts of Reviews of Effects <2nd Quarter 2015>, EBM Reviews - Health Technology Assessment <2nd Quarter 2015>, EBM Reviews - NHS Economic Evaluation Database <2nd Quarter 2015>, Embase <1980 to 2015 Week 31>, All Ovid MEDLINE(R) <1946 to Present>
Search Strategy:
| 1 | Clostridium difficile/ (17125) |
| 2 | Enterocolitis, Pseudomembranous/ (11520) |
| 3 | Clostridium Infections/ (6439) |
| 4 | (clostridium difficile or c difficile or c diff or clostridium enterocolitis or ((pseudomembranous or antibiotic associated) adj2 (enteritis or colitis or enterocolitis)) or clostridium infection*).tw. (26426) |
| 5 | or/1–4 (37451) |
| 6 | exp Feces/ (125412) |
| 7 | Microbiota/ (12302) |
| 8 | (((fecal or faecal or feces or faeces or stool or stools or microbiota*) adj4 (transplant* or transfus* or transfer* or infusion* or donor* or donation* or therap* or suspension)) or FMT or bacteriotherap* or human probiotic infus* or intestinal microbiome restorat*).tw. (5976) |
| 9 | or/6–8 (141194) |
| 10 | Diarrhea/th [Therapy] (6333) |
| 11 | or/9–10 (147157) |
| 12 | 5 and 11 (4290) |
| 13 | exp Animals/ not (exp Animals/ and Humans/) (8230594) |
| 14 | 12 not 13 (3972) |
| 15 | economics/ (247193) |
| 16 | economics, medical/ or economics, pharmaceutical/ or exp economics, hospital/ or economics, nursing/ or economics, dental/ (697761) |
| 17 | economics.fs. (369069) |
| 18 | (econom* or price or prices or pricing or priced or discount* or expenditure* or budget* or pharmacoeconomic* or pharmaco-economic*).tw. (636474) |
| 19 | exp “costs and cost analysis”/ (485810) |
| 20 | cost*.ti. (219098) |
| 21 | cost effective*.tw. (228512) |
| 22 | (cost* adj2 (util* or efficacy* or benefit* or minimi* or analy* or saving* or estimate* or allocation or control or sharing or instrument* or technolog*)).ab. (142978) |
| 23 | models, economic/ (127076) |
| 24 | markov chains/ or monte carlo method/ (116078) |
| 25 | (decision adj1 (tree* or analy* or model*)).tw. (31046) |
| 26 | (markov or markow or monte carlo).tw. (92331) |
| 27 | quality-adjusted life years/ (26021) |
| 28 | (QOLY or QOLYs or HRQOL or HRQOLs or QALY or QALYs or QALE or QALEs).tw. (44560) |
| 29 | ((adjusted adj (quality or life)) or (willing* adj2 pay) or sensitivity analys*s).tw. (87840) |
| 30 | or/15–29 (2151007) |
| 31 | 14 and 30 (196) |
| 32 | limit 31 to english language [Limit not valid in CDSR,DARE; records were retained] (187) |
| 33 | 32 use pmoz,cctr,coch,dare,clhta (76) |
| 34 | 14 use cleed (4) |
| 35 | or/33–34 (80) |
| 36 | peptoclostridium difficile/ (792) |
| 37 | Clostridium difficile infection/ (6854) |
| 38 | Clostridium infection/ (6534) |
| 39 | pseudomembranous colitis/ (11699) |
| 40 | (clostridium difficile or c difficile or c diff or clostridium enterocolitis or ((pseudomembranous or antibiotic associated) adj2 (enteritis or colitis or enterocolitis)) or clostridium infection*).tw. (26426) |
| 41 | or/36–40 (37153) |
| 42 | feces/ (120591) |
| 43 | feces microflora/ (4077) |
| 44 | (((fecal or faecal or feces or faeces or stool or stools or microbiota*) adj4 (transplant* or transfus* or transfer* or infusion* or donor* or donation* or therap* or suspension)) or FMT or bacteriotherap* or human probiotic infus* or intestinal microbiome restorat*).tw. (5976) |
| 45 | or/42–44 (128701) |
| 46 | diarrhea/th [Therapy] (6333) |
| 47 | or/45–46 (134663) |
| 48 | 41 and 47 (4281) |
| 49 | (exp animal/ or nonhuman/) not exp human/ (9407210) |
| 50 | 48 not 49 (3934) |
| 51 | Economics/ (247193) |
| 52 | Health Economics/ or exp Pharmacoeconomics/ (209005) |
| 53 | Economic Aspect/ or exp Economic Evaluation/ (375018) |
| 54 | (econom* or price or prices or pricing or priced or discount* or expenditure* or budget* or pharmacoeconomic* or pharmaco-economic*).tw. (636474) |
| 55 | exp “Cost”/ (485810) |
| 56 | cost*.ti. (219098) |
| 57 | cost effective*.tw. (228512) |
| 58 | (cost* adj2 (util* or efficacy* or benefit* or minimi* or analy* or saving* or estimate* or allocation or control or sharing or instrument* or technolog*)).ab. (142978) |
| 59 | Monte Carlo Method/ (47283) |
| 60 | (decision adj1 (tree* or analy* or model*)).tw. (31046) |
| 61 | (markov or markow or monte carlo).tw. (92331) |
| 62 | Quality-Adjusted Life Years/ (26021) |
| 63 | (QOLY or QOLYs or HRQOL or HRQOLs or QALY or QALYs or QALE or QALEs).tw. (44560) |
| 64 | ((adjusted adj (quality or life)) or (willing* adj2 pay) or sensitivity analys*s).tw. (87840) |
| 65 | or/51–64 (1759792) |
| 66 | 50 and 65 (171) |
| 67 | limit 66 to english language [Limit not valid in CDSR,DARE; records were retained] (162) |
| 68 | 67 use emez (98) |
| 69 | 35 or 68 (178) |
| 70 | remove duplicates from 69 (152) |
| 71 | 69 use pmoz (72) |
| 72 | 69 use emez (98) |
| 73 | 69 use cctr (0) |
| 74 | 69 use coch (2) |
| 75 | 69 use dare (1) |
| 76 | 69 use clhta (1) |
| 77 | 69 use cleed (4) |
Appendix 2: Evidence Quality Assessment
Table A1:
AMSTAR Scores of Included Systematic Reviews
| Author, Year | AMSTAR Scorea | (1) Provided Study Design | (2) Duplicate Study Selection | (3) Broad Literature Search | (4) Considered Status of Publication | (5) Listed Excluded Studies | (6) Provided Characteristics of Studies | (7) Assessed Scientific Quality | (8) Considered Quality in Report | (9) Methods to Combine Appropriate | (10) Assessed Publication Bias | (11) Stated Conflict of Interest |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Drekonja et al, 20153 | 7 | ✓ | ✓ | ✓ | ✗ | ✗ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ |
| Bagdasarian et al, 201544 | 2 | ✓ | ✗ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| NICE, 201422 | 1 | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| O'Horo et al, 201445 | 5 | ✓ | ✗ | ✓ | ✗ | ✗ | ✓ | ✓ | ✗ | ✓ | ✗ | ✗ |
| Sha et al, 201446 | 5 | ✓ | ✓ | ✓ | ✗ | ✗ | ✓ | ✗ | ✗ | ✓ | ✗ | ✗ |
| Cammarota et al, 201447 | 6 | ✓ | ✓ | ✓ | ✗ | ✗ | ✓ | ✓ | ✗ | ✓ | ✗ | ✗ |
| Kassam et al, 201348 | 7 | ✓ | ✓ | ✓ | ✗ | ✗ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ |
| Dodin and Katz, 201449 | 1 | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Sofi et al, 201350 | 4 | ✓ | ✓ | ✓ | ✗ | ✗ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ |
Abbreviations: AMSTAR, Assessment of Multiple Systematic Reviews; NICE, National Institute for Health and Care Excellence.
Maximum possible score is 11. Details of AMSTAR score are described in Shea et al.7
Our first consideration was study design; we started with the assumption that randomized controlled trials (RCTs) are high quality, whereas observational studies are low quality. We then took into account five additional factors—risk of bias, inconsistency, indirectness, imprecision, and publication bias. Limitations in these areas resulted in downgrading the quality of evidence. Finally, we considered three main factors that may raise the quality of evidence: the large magnitude of effect, the dose-response gradient, and any residual confounding factors.8 For more detailed information, please refer to the latest series of GRADE articles.8
As stated by the GRADE Working Group, the final quality score can be interpreted using the following definitions:
| High | We are very confident that the true prognosis (probability of future events) lies close to that of the estimate |
| Moderate | We are moderately confident that the true prognosis (probability of future events) is likely to be close to the estimate, but there is a possibility that it is substantially different |
| Low | Our confidence in the estimate is limited: the true prognosis (probability of future events) may be substantially different from the estimate |
| Very Low | We have very little confidence in the estimate: the true prognosis (probability of future events) is likely to be substantially different from the estimate |
Table A2:
GRADE Evidence Profile for Comparison of Fecal Microbiota Therapy to Antibiotics
| Number of Studies (Design) | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Upgrade Considerations | Quality |
|---|---|---|---|---|---|---|---|
| 2 RCTs | No serious limitations | No serious limitations | No serious limitations | No serious limitations | Undetected Likely (−1) | Large magnitude of effect (+1) | ⊕⊕⊕⊕ High ⊕⊕⊕ Moderate |
| 40 observational case series | Serious limitations (−1) | Serious limitations (−1) | Serious limitations (−1) | Serious limitations (−1) | Very likely (−2) | Dose-response gradient (+1) | ⊕⊕ Low ⊕ Very Low |
| Very serious limitations (−2) | Very serious limitations (−2) | Very serious limitations (−2) | Very serious limitations (−2) | All plausible confounding increases confidence in estimate (+1) Other considerations (+1) |
|||
| Resolution | |||||||
| 2 RCTs | No serious limitations | No serious limitations | Serious limitations (−1)b | No serious limitations | Undetected | – | ⊕⊕⊕ Moderate |
| 40 observational case series | Serious limitations (−1)a | No serious limitations | No serious limitations | No serious limitations | Undetected | – | ⊕⊕ Low |
| Quality of life | |||||||
| 0 studies | – | – | – | – | – | – | – |
| Mortality | |||||||
| 2 RCTs | No serious limitations | No serious limitations | No serious limitations | Very serious limitations (−2)c | Undetected | ⊕⊕ Low | |
| 40 observational case series | Serious limitations (−1)a | No serious limitations | No serious limitations | No serious limitations | Undetected | – | ⊕⊕ Low |
| Adverse events | |||||||
| 2 RCTs | Serious limitations (−1)d | No serious limitations | No serious limitations | Serious limitations (−1)c | Undetected | – | ⊕⊕ Low |
| 40 observational case series | Serious limitations (−1)a | No serious limitations | No serious limitations | No serious limitations | Undetected | – | ⊕⊕ Low |
Abbreviations: GRADE, Grading of Recommendations Assessment, Development, and Evaluation; RCT, randomized controlled trial.
Observational uncontrolled, mostly retrospective case series.
Most fecal microbiota therapy in Ontario is via enema. Studies published to date mostly use colonoscopy and nasoduodenal or nasogastric tube.
Optimal information size not met. Wide confidence intervals.
Lack of long-term follow-up in RCTs (up to 10 weeks).
Table A3:
Risk of Bias Among Randomized Controlled Trials for Fecal Microbiota Therapy
| Author, Year | Allocation Concealment | Blinding | Complete Accounting of Patients and Outcome Events | Selective Reporting Bias | Other Limitations |
|---|---|---|---|---|---|
| Cammarota et al, 201510 | No limitations | No limitationsa | No limitations | No limitations | Limitationsb |
| Van Nood et al, 201317 | No limitations | No limitationsa | No limitations | No limitations | Limitationsb |
| Youngster et al, 201418 | No limitations | No limitationsa | No limitations | No limitations | Limitationsc |
Because of intrinsic difference between the two treatments, neither physicians nor patients were blinded to randomization groups.
Trials ended early. Potential overestimation of treatment effect. Both randomized controlled trials confirmed an extremely low cure rate of a vancomycin regimen (26% reported by Cammarota et al10 and 31% reported by van Nood et al17). Before their inclusion, most patients had relapses after previous vancomycin-based treatments; this most likely contributed to poor results of vancomycin regimen in both studies.
Feasibility study was not adequately powered to detect clinically significant differences in outcomes.
Table A4:
Risk of Bias Among Observational Trials for Fecal Microbiota Therapy
| Author, Year | Appropriate Eligibility Criteria | Appropriate Measurement of Exposure | Appropriate Measurement of Outcome | Adequate Control for Confounding | Complete Follow-Up |
|---|---|---|---|---|---|
| Hirsch et al, 201511 | No limitations | No limitations | No limitations | No limitations | No limitations |
| Ray et al, 201412 | No limitations | No limitations | No limitations | No limitations | No limitations |
| Pierog et al, 201413 | No limitations | No limitations | No limitations | No limitations | No limitations |
| Lagier et al, 201514 | No limitations | No limitations | No limitations | Limitationsa | No limitations |
| Satokari et al, 201515 | No limitations | No limitations | No limitations | No limitations | Limitationsb |
| Fischer et al, 201516 | Limitationsc | No limitations | No limitations | No limitations | No limitations |
Concomitant use of antimicrobials during administration of fecal microbiota therapy.
42/49 patients followed up at 1 year.
Concomitant use of vancomycin during administration of fecal microbiota therapy if pseudomembranes were present in patient.
Appendix 3: Evidence Base
Table A5:
Studies Included in 2015 Systematic Review by Drekonja et al
| Author, Year | Study Design and Methods | N | Average Patient Age (Years) | Number of CDI Recurrences, N (Range) | Number of Donors and Relationship to Fecal Donor | Reported Length of Follow-Up (Range) | Resolution of Symptoms after FMT, n/N (%) |
|---|---|---|---|---|---|---|---|
| Recurrent CDI; FMT via upper GI tract (7 studies; n = 214 patients [187 patients received FMT]) | |||||||
| Youngster et al, 201451 | Prospective case series | 16 | 60 | 2 (1–5) | 4; not related | 6 months | 13/16 (81) |
| Youngster et al 201418 | RCT | 10 | 55 (among 20 enrolled) | 4.5 (2.0–16.0) | 5; not related | 6 months | 6/10 (60) |
| Van Nood et al, 201317 | RCT | 43 (16 FMT) | 70 (among 43 enrolled) | 3 (1–5) FMT group | 15; NR | 10 weeks | 13/16 (81) |
| Rubin et al, 201352 | Retrospective case series | 74 (72 adults) | 63 (median) | NR | NR; healthy close household member | 60 days | 58/72 (81) |
| Garborg et al, 201053 | Retrospective case series | 40 | 75 | NR | NR; close relative or other household member | 80 days | 29/40 (73) |
| MacConnachie et al, 200920 | Retrospective case series | 15 | 82 | 4 (3–7) | NR; related | 16 weeks (4–24 weeks) | 11/15 (73) |
| Aas et al, 200321 | Retrospective case series | 18 | 73 | 3.6 (2.0–7.0) | 16; spouse, partner, household family member | 90 days | 15/18 (83) |
| Recurrent CDI; FMT via colonoscopy (11 studies; n = 257) | |||||||
| Khan et al, 201454 | Retrospective case series | 20 | 66 | 5.1 | 20; spouse, partner, first-degree relative, not related | 6 months | 18/20 (90) |
| Youngster et al, 201418 | RCT | 10 | 55 (among 20 enrolled) | 4.5 (2.0–16.0) | 5; not related | 6 months | 8/10 (80) |
| Cammarota et al, 201455 | Retrospective case series | 3 | 67 | 1–5 | 3; child sibling, not specified | 4–5 months | 3/3 (100) |
| Pathak et al, 201356 | Retrospective case series | 12 (11 via colonoscopy) | 72 | NR | 12; spouse, child sibling, niece | 2–29 months | 11/12 (92) |
| Patel et al, 201319 | Retrospective case series | 31 | 61 | 4 (2–7) | 33; spouse, child sibling, parent, niece, friend | 1 week–1 year | 22/30 (73) |
| Hamilton et al, 201257 | Retrospective case series | 43 | 59 | 5.9 | 12; parent, child, spouse, friend, volunteer | 2 months | 37/43 (86) |
| Kelly et al, 201258 | Retrospective case series | 26 | 59 | ≥ 3 | 26; partner, sibling, spouse, child, cousin, friend | 11 months (2–30 months) | 25/26 (96) |
| Mattila et al, 201259 | Retrospective case series | 70 | 73 | 3.5 (1.0–12.0) | 62; relative or household contact, volunteer | 12 months | 66/70 (94) |
| Mellow and Kanatzar, 201160 | Retrospective case series | 13 (12 recurrent) | 67 | 4 (3–7) | NR; chosen by patient | 5 months (1–10 months) | 11/12 (92) |
| Rohlke et al, 201061 | Retrospective case series | 19 | 49 | NR | 19; partner, family member, housemate | 27 months (6 months–5 years) | 18/19 (95) |
| Yoon and Brandt, 201062 | Retrospective case series | 12 | 66 | NR | 12; spouse, partner, child/grandchild | 3 weeks–8 years | 12/12 (100) |
| Recurrent CDI; FMT via enema (5 studies; n = 45) | |||||||
| Emanuelsson et al, 201463 | Retrospective case series | 23 | 67 | 3 (1–5) | NR; spouse or close relative | 18 months (birth-courses of antibiotics 21 months) | 15/23 (65) |
| Silverman et al, 201064 | Retrospective case series | 7 | 72 | NR | 7; child/grandchild, spouse, sibling | 8.6 months (4–14 months) | 7/7 (100) |
| Gustafsson et al, 199965 | Retrospective case series | 6 | 61 | NR | 1; not related | 18 months | 5/6 (83) |
| Paterson et al, 199466 | Retrospective case series | 7 | 56 | 3 (1–4) | NR; relative | NR | 7/7 (100) |
| Tvede and Rask-Madsen, 198967 | Retrospective case series | 2 | 60 | 3 (2–4) | 2; spouse, child | 12 months | 1/2 (50) |
| Recurrent CDI; FMT via upper GI tract and colonoscopy (1 study; n = 27) | |||||||
| Dutta et al, 201468 | Prospective case series | 27 | 65 | 4.6 (3.0–5.0) | 27; spouse, child, parent | 21 months (10–34 months) | 27/27 (100) |
| Refractory CDI; FMT via upper GI tract (2 studies; n = 12) | |||||||
| Youngster et al, 201451 | Prospective case series | 4 | 72 | 3 (1–5) | 3; not related | 6 months | 1/4 (25) |
| Zainah et al, 201569 | Retrospective case series | 8 | 74 | 3.3 (2.0–5.0) | NR; family member or unrelated | 100 days | 8/8 (100) |
| Refractory CDI; FMT via colonoscopy (2 studies; n = 5) | |||||||
| Weingarden et al, 201370 | Retrospective case series | 4 | 73 | NR | 1; not related | Up to 12 months | 0/4 (0) |
| Mellow and Kanatzar, 201160 | Retrospective case series | 1 (from series) | NR | 1 | 1; chosen by patient | 9 months | 1/1 (100) |
| Refractory CDI; FMT via enema (3 studies; n = 112) | |||||||
| Lee et al, 201471 | Retrospective case series | 94 | 72 | 2.1 (courses of antibiotics) | NR; not related | 6–24 months | 45/94 (48) |
| Bowden et al, 198172 | Retrospective case series | 16 (15 adults) | 59 | NR | NR; household relative, volunteer | NR | 13/15 (87) |
| Eiseman et al, 195873 | Retrospective case series | 3 (patients 1, 2, and 4) | 52 | NR | NR; NR | 2–10 days | 3/3 (100) |
| Initial therapy for CDI; FMT via upper GI tract (1 study; n = 6) | |||||||
| Zainah et al, 201569 | Retrospective case series | 6 | 72 | 0 | NR; family member or unrelated | 100 days | 1/6 (17) |
| Initial therapy for CDI; FMT via enema (1 study; n = 1) | |||||||
| Eiseman et al, 195873 | Retrospective case series | 1 (patient 3) | 68 | NR | NR; NR | 5 days | 1/1 (100) |
Abbreviations: CDI, Clostridium difficile infection; FMT, fecal microbiota therapy; GI, gastrointestinal; NR, not reported; RCT, randomized controlled trial.
Source: Adapted from Drekonja et al.3
Table A6:
Summary of Randomized Controlled Trials
| Author, Year | Study Design | Study Group | Control Group | Outcome | Feces Donor | Results | Comments |
|---|---|---|---|---|---|---|---|
| Cammarota et al, 201510 | Open-label RCT (neither physicians nor patients were blinded to treatment) At enrolment recurrent CDI defined as diarrhea (at least 3 loose or watery stools per day for 2 or more consecutive days or at least 8 loose stools in 48 hours) and positive results from C. difficile toxin stool test within 10 weeks from end of previous antibiotic treatment. To obtain homogeneity in both study arms, only patients the authors believed were able to undergo colonoscopy were enrolled |
N = 20 Patients ≥ 18 years old with recurrent CDI after one or more courses of specific antibiotic therapy (at least 10 days of vancomycin at a dose of at least 125 mg 4 times daily or at least 10 days of metronidazole at a dose of 500 mg 3 times a day) received a short regimen of vancomycin (125 mg 4 times a day for 3 days), followed by ≥ 1 infusions of feces via colonoscopy Patients in whom recurrent CDI developed after the first fecal infusion were given a second infusion of feces within 1 week. However, after enrolment of the first 2 patients who underwent FMT, this part of the study protocol was amended. Thereafter, all subsequent patients with PMC underwent repeated infusions every 3 days until colitis resolved |
N = 19 Patients ≥ 18 years old with recurrent CDI received vancomycin 125 mg 4 times daily for 10 days, followed by 125–500 mg/day every 2–3 days for at least 3 weeks. No colonoscopy was performed |
Primary End Point Resolution of diarrhea related to CDI 10 weeks after end of treatment For patients in FMT group who required more than 1 infusion of feces, follow-up was extended to 10 weeks after last infusion Cure was defined as disappearance of diarrhea or persistent diarrhea explicable by other causes with 2 stool tests negative for C. difficile toxin Recurrence after treatment was defined as diarrhea (at least 3 loose or watery stools per day for 2 or more consecutive days or at least 8 loose stools in 48 hours) unexplainable by other causes with or without positive results for stool toxin within 10 weeks from end of therapy Secondary End Point Toxin negative without recurrent CDI 5 and 10 weeks after end of treatment Stool diary was kept by patients, by family members, or by medical and nursing staff Patients, family members, and referring physicians were also questioned about stool frequency and consistency, medication use, and adverse events within 7 days after end of treatment and on weeks 2–10 post-treatment Stool tests for C. difficile toxin performed on weeks 5, 10, and whenever diarrhea occurred |
Healthy volunteers (preferably patients’ relatives or intimates) | No significant differences in baseline characteristics between patient groups First 2 patients in FMT group had PMC. The first patient had a recurrence of CDI and received a second fecal infusion. The patient underwent another recurrence of CDI and started vancomycin but died of sepsis after 1 week. The second patient with PMC was affected by severe cardiopathy and had a recurrence of CDI. The patient's deteriorating condition prevented a second fecal infusion. The patient received vancomycin but died 15 days later. Based on both ITT and PP analysis, FMT was considered to have failed in these first 2 patients At planned 1-year interim analysis, FMT showed a significantly higher efficacy than vancomycin. Study was stopped at 39 patients (originally planned 50 patients per group) Primary End Point Overall, FMT via colonoscopy achieved significantly higher remission rates of recurrent CDI than vancomycin treatment (90% vs. 26%, P < .0001 for both ITT and PP analysis) Overall odds ratio of the cure rates was 25.2 (99.9% CI, 1.26–502.30) Secondary End Point At 5 and 10 weeks post-treatment, 18/20 FMT patients had no discernible C. difficile stool toxins; 2 patients had positive results for stool toxin within 1 week post-treatment. In the vancomycin group, 3 patients had negative results for stool toxin after 5 weeks, and 5 patients had negative results after 10 weeks Adverse Events 19/20 (95%) FMT patients had diarrhea immediately after fecal infusion, and 12/20 (60%) patients had bloating and abdominal cramping (symptoms resolved within 12 hours in all patients). No adverse events were reported in the vancomycin group |
3-day vancomycin regimen was offered before FMT to avoid leaving patients uncovered by medical treatment during time required for donor screening No patient refused treatment or expressed concerns about any aspect of FMT Findings are consistent with previous success rate (81%) obtained in a Dutch RCT using nasoduodenal tube for fecal infusion.17 PMC was present in 35% of patients with recurrent CDI. PMC patients seemed to require multiple fecal infusions to be cured.10 Patients receiving vancomycin did not undergo colonoscopy, and it is unknown how many of them had PMC FMT Group Overall, 18/20 patients were cured 13/20 (65%) patients cured after first fecal infusion. None of 13 patients were diagnosed with PMC. The 7 remaining patients were diagnosed with PMC: 6 of these patients received multiple infusions (4 received 2 infusions, 1 received 3 infusions, and 1 underwent 4 infusions), and 1 patient received 1 infusion 5/7 patients with PMC were cured; 2 had a recurrence, received 1 or 2 fecal infusions, and died of C. difficile–related complications. All 5/7 patients with PMC received a fecal infusion every 3 days until colitis resolved Vancomycin Group 5/19 (26%) patients were cured 2 patients did not benefit from antibiotic treatment and died of C. difficile–related complications. 12 patients had a CDI recurrence. Median time to recurrence was 10 days (range 4–21 days). At time of recurrence, these patients had been discharged home, and researchers were unable to offer them fecal infusion |
| Van Nood et al, 201317 | Open-label RCT (neither physicians nor patients were blinded to treatment) Patients > 18 years of age and had a relapse of CDI after at least 1 course of adequate antibiotics (vancomycin or metronidazole) CDI defined as diarrhea (≥ 3 loose or watery stools per day for at least 2 consecutive days or ≥ 8 loose stools in 48 hours) and positive results from stool test for C. difficile toxin |
n = 16 Initial vancomycin regimen (500 mg orally 4 times daily for 4 days), followed by bowel lavage and subsequent infusion of feces via nasoduodenal tube Patients in whom recurrent CDI developed after first donor feces infusion were given second infusion with feces from a different donor |
n = 13 Standard vancomycin regimen (500 mg orally four times per day for 14 days). n = 13 Standard vancomycin regimen with bowel lavage Patients in whom antibiotic therapy failed were offered treatment with donor feces off protocol |
Primary End Point Resolution of diarrhea associated with CDI without relapse after 10 weeks For patients in FMT group who needed a second infusion, follow-up was extended to 10 weeks after second infusion Secondary End Point Cure without relapse after 5 weeks Cure defined as absence of diarrhea or persistent diarrhea that could be explained by other causes with 3 consecutive negative results from stool tests for C. difficile toxin Relapse was defined as diarrhea with positive results from stool test for C. difficile toxin Adjudication committee whose members were unaware of study group assignments decided which patients were cured Patients kept a stool diary and were questioned about stool frequency and consistency, medication use, and adverse effects on days 7, 14, 21, 35, and 70 and at initiation of vancomycin Stool tests for C. difficile toxin were performed on days 14, 21, 35, and 70 and whenever diarrhea occurred |
Volunteers | Initially, 40 patients per study group was planned. Because most patients in both control groups relapsed, the monitoring board advised termination of trial All analyses were performed on modified ITT basis, excluding 1 patient, who required high-dose prednisolone after randomization but before study treatment was initiated Primary End Point 13/16 (81%) of FMT patients had resolution of CDI-associated diarrhea after first infusion 3 remaining patients received a second infusion; 2/3 cases resolved 4/13 (31%) patients who received vancomycin alone had resolution 3/13 (23%) patients who received vancomycin and lavage had resolution P < .001 in overall cure rates for both comparisons with FMT group 5 weeks after initiation of therapy, infection recurred in 1/16 (6%) FMT patients, 8/13 (62%) in vancomycin-only group, and 7/13 (54%) in vancomycin and bowel lavage group Adverse Events No significant differences in adverse events among 3 study groups were observed except for mild diarrhea and abdominal cramping in the FMT group on infusion day |
Mainly elderly patients Power calculation was based on efficacy of vancomycin for a first recurrence of CDI. Most patients had several relapses before inclusion; therefore, efficacy of vancomycin was lower than expected, which could have contributed to findings Patients were pretreated with vancomycin and bowel lavage following protocol that was effective in previously published case series by the authors74 |
| Youngster et al, 201418 | Open-label RCT (neither physicians nor patients were blinded to treatment) Relapsing/refractory CDI was defined by relapse of CDI after having at least 3 episodes of mild to moderate CDI and failure of 6- to 8-week taper with vancomycin with or without an alternative antibiotic, or at least 2 episodes of severe CDI resulting in hospitalization and associated with serious morbidity Patients were required to discontinue antibiotics at least 48 hours before procedure Patients in both study arms who showed no improvement in diarrheal symptoms were offered second FMT by their preferred route of administration Patients in both groups were followed with questionnaires on days 1, 2, 3, 7, 14, and 21 and at 2 and 6 months via telephone Questionnaires recorded stool frequency, general well-being, rating of symptoms, drug use, and adverse events Recipients provided stool samples before FMT, weekly for 3 weeks, and then at 2 and 6 months |
N = 10 Colonoscopy Patients with relapsing/refractory CDI |
N = 10 Nasogastric tube Patients with relapsing/refractory CDI |
Primary End Point Clinical resolution of diarrhea when antibiotics for CDI were discontinued without relapse after 8 weeks For patients who required second dose, follow-up was calculated as starting at time of second administration Resolution of diarrhea defined as < 3 bowel movements per 24 hours Secondary End Point Self-reported well-being and adverse events |
Volunteers (unrelated donors) Frozen fecal sample |
Primary End Point Colonoscopy: 8/10 cured Nasogastric: 6/10 cured, P = .628 1 patient in nasogastric group refused subsequent retreatment Remaining 5 patients were given second infusion at mean of 4.9 days (SD 2.1 days) after first procedure. All 5 patients requested nasogastric route. 4/5 patients were cured. Overall, 80% in nasogastric group and 100% in colonoscopy group were cured, P = .53 Secondary End Points Self-reported heath rating using a standardized questionnaire scale of 1–10 (1 lowest and 10 being “best recent health baseline”) increased over study period from median of 5 (IQR, 3–6) and 4 (IQR 2–5) in colonoscopy and nasogastric groups, respectively, on day before FMT (P = .44) to 8 (IQR 7–10) and 7 (IQR 5–8), respectively, 8 weeks after infusion. Colonoscopy group had higher health scores accounted for by higher reported score on day before FMT. Groups did not differ regarding absolute increment in scores (P = .51) Adverse events likely to be related included mild abdominal discomfort and bloating in 4 patients (20%) |
Small feasibility study Study not powered to detect difference between nasogastric route vs. colonoscopy Unclear what standardized questionnaire was used in study (no reference provided) Mean age of patients was 54; however 3 children were included in study Optimal shelf life for frozen feces is unknown |
Abbreviations: CDI, Clostridium difficile infection; CI, confidence interval; FMT, fecal microbiota therapy; IQR, interquartile range; ITT, intent to treat; PMC, pseudomembranous colitis; PP, per protocol; RCT, randomized controlled trial; SD, standard deviation.
Table A7.
Adverse Events in Fecal Microbiota Therapy Group
| Adverse Event | On Day of Fecal Microbiota Therapy (Number of Events) | During Follow-Up (Number of Events) |
|---|---|---|
| Belching | 3 | 0 |
| Nausea | 1 | 0 |
| Vomiting | 0 | 0 |
| Abdominal cramps | 5 | 0 |
| Diarrhea | 15 | 0 |
| Constipation | 0 | 3 |
| Abdominal pain | 2 (associated with cramping) | 0 |
| Infection | 0 | 2 |
| Hospital admission | Not applicable | 1 |
| Death | 0 | 0 |
| Other | 1 | 1 |
Table A8:
Summary of Observational Studies
| Author, Year | N | Route of Administration | Recurrent, Refractory or Initial CDI | Inclusion Criteria | Antimicrobial Use Peri-FMT | Study Design and Methods | Donor | Results | Limitations/Comments |
|---|---|---|---|---|---|---|---|---|---|
| Hirsch et al, 201511 | 19 | Orally administered capsules (previously cryopreserved) | Recurrent | All patients (April 2013–February 2014) with ≥ 2 prolonged, severe, or recurrent episodes of CDI after therapy with metronidazole, vancomycin, or fidaxomicin ≥ 18 years of age |
Antimicrobial treatment was discontinued day before FMT Patients who had persistent or recurring CDI were instructed to resume CDI antimicrobial therapy immediately and were offered repeat FMT Repeat FMT treatments were administered about 6 weeks after previous FMT treatment |
Retrospective chart review Primary Outcome Resolution of CDI-associated diarrhea without relapse after 90 days Recurrence was defined as diarrhea with positive results from stool test for C. difficile toxin B by PCR Outpatients ingested 6–22 capsules (average 10 ± 3 SD) Patients were followed up by phone interview at 2 days, 3 weeks, and 90 days post-treatment After each repeat FMT administration, follow-up was extended for additional 90 days |
3 unrelated volunteers |
Mean age 61 years (range 26–92 years). Patients had average of 4 CDI recurrences (range 2–8) before study Primary Outcome 13 (68%) patients had resolution after single FMT treatment 4/6 cases that did not respond to initial FMT went on to resolution after 1 more FMT (cumulative cure rate of 89%) 1 patient had 4 FMT treatments without resolution of diarrhea In successful courses, clinical improvement was noted within 3 days of FMT; in most cases, symptoms gradually improved over 2 weeks Adverse Events Abdominal pain was reported post-procedure by 5 patients (mild and transient in 4 patients; moderate to severe in 1 patient who also had irritable bowel syndrome but pain subsided after 3 days) |
Retrospective case series Patients’ self-reports Incomplete understanding of dose-response characteristics of capsules |
| Ray et al, 201412 | 20 | Colonoscopy | Recurrent or “severe” | All patients who underwent FMT for CDI at authors’ institution between August 2012 and November 2013 Patients were candidates if they had 2 recurrences of CDI defined by continued diarrhea or positive results from C. difficile stool sample after finishing courses of antibiotics, or if they had life-threatening illness from CDI requiring hospitalization or admission to intensive care unit |
All patients received antibiotic treatment for CDI before FMT | Retrospective chart review | Relative or spouse or unrelated | Mean age 62 years (range 27–89 years) Average follow-up post-treatment was 3.175 months (range 0–10 months) No recurrence of CDI was documented after 1 course of FMT Adverse Events (all resolved after treatment) Abdominal cramping Bloating Flatulence Nausea |
Retrospective case series No explicit objective was stated |
| Pierog et al, 201413 | 6 (pediatric) | Colonoscopy | Recurrent and refractory | History of recurrent and refractory CDI, defined as at least 34 CDIs that failed to resolve with therapy or relapsed within 2 weeks after withdrawal of antibiotic therapy 4/6 patients had other gastrointestinal disorders (e.g., inflammatory bowel disease, Hirschsprung disease, and gastrostomy tube dependence) |
Patients discontinued anti-CDI antimicrobials 24 hours before FMT | Retrospective chart review Cure was defined as clinical resolution of patient's symptoms (diarrhea, pain, failure to gain weight) attributed to CDI without further dependence on anti-CDI antimicrobials |
Parent | All patients were cured of CDI following FMT | Retrospective case series No explicit objective was stated |
| Lagier et al, 201514 | 61 (elderly) | Nasogastric | Recurrent | Patients who had positive results from stool sample during C. difficile outbreak that started in March 2013 |
Antibiotics and Late FMT Patients treated only with antimicrobials (vancomycin, metronidazole, or fidaxomicin). In cases of at least 3 failures or relapses, patients received FMT Antibiotics and Early FMT Antibiotics and FMT offered early during first week following diagnosis |
Case series Patients excluded from FMT if immunity was compromised or prolonged or if patients had been treated by antibiotics for infections other than CDI on day of FMT Primary Outcomes Global mortality rate, mortality in month following diagnosis Relapse was defined as diarrhea (> 3 liquid stool daily) and positive results for C. difficile Length of study and how patients were followed up was not reported |
Relatives or unrelated |
Overall Mean age 84 years (range 66–101 years). Global mortality: 31/61 (50.8%) 1-month mortality: 26/60 (43.3%) Antibiotics and late FMT includes 3 patients treated by FMT after at least 2 relapses 6/16 (37.5%) patients treated using antibiotics and early FMT required second FMT owing to relapse in first month. Second FMT plus antibiotics resolved symptoms in all 6 patients Global Mortality Early FMT (n = 16): 3/16 (18.8%) Late FMT (n = 45): 29/45 (64.4%) P < .001 1-Month Mortality Early FMT (n = 16): 1/16 (6%) Late FMT (n = 43): 24/43* (56%) *Excluding 2 patients who were unavailable at follow-up P < .0003 Of 40 patients treated only by antibiotics, 23 patients died before 1 month (57.5%). Among these 23 patients, 17 patients (74%) died during first week following diagnosis. Among 3 patients treated by antibiotics and late FMT, 1-month mortality was 1/3 (33%) Survival Analysis Antibiotics and early FMT was associated with significant mortality decrease, log-rank test, P < .001. Length of follow-up from graph is about 250 days Cox Regression Included age, sex, antibiotics, and early FMT Antibiotics and early FMT was only independent predictor of survival (hazard ratio 0.18, 95% CI 0.05–0.61, P = .006) Adverse Events Authors stated that 33 FMT procedures were conducted (including patients treated with successive FMTs). 24 patients (73%) had diarrhea that resolved by next day |
Case series. Unclear if consecutive and prospective or retrospective Unclear length of follow-up Study not designed to compare early vs. late FMT Unclear how many relapses occurred in which patients (33 FMTs undertaken in total) Authors consider study to be “preliminary” Authors propose “concomitant use of antibiotics to reduce the bacterial load and transplantation to rehabilitate the fecal flora. Waiting for the third episode before considering transplantation as recommended by current literature will inevitably lead to further preventable deaths” |
| Satokari et al, 201515 | 49 | Colonoscopy | Recurrent and refractory | All patients treated by FMT for CDI through colonoscopy at authors’ hospital from December 2007 to February 2014 without any further inclusion or exclusion criteria | Patients were receiving vancomycin treatment until discontinued at average of 36 hours before FMT | Retrospective chart review FMT used for patients with laboratory-confirmed recurrent CDI (positive results from culture and toxin) despite antimicrobial treatment for CDI FMT not used for patients with contraindications for colonic lavage or colonoscopy, who needed antibiotic treatment for indication other than CDI, or who were unable to understand treatment (e.g., dementia) Failure was defined as persistent or recurrent symptoms with positive results from C. difficile toxin stool test and need for new therapy Patients were advised to contact hospital if diarrhea or other symptoms recurred post-FMT Most patients were scheduled to visit clinic or were contacted by telephone 12 weeks post-FMT Patients who received frozen FMT were contacted 2–4 times during year post-FMT |
Relatives or unrelated | No patients refused FMT 42/49 patients were followed up at 1 year Mean Age (range) Fresh: n = 26, 52 (22–81) Frozen: n = 23, 61 (20–88) Mean Number of CDI Relapses Before FMT (range) Fresh: 4.6 (2–12) Frozen: 4.0 (1–6) Mean Days From First CDI to FMT (range) Fresh: 147 (60–360) Frozen: 148 (42–312) Success Rate of FMT in Resolving CDI at 12 Weeks (%) Fresh: 25/26 (96) Frozen: 22/23 (96) Success Rate of FMT in Resolving CDI at 1 Year (%) Fresh: 22/25 (88) Frozen: 15/17 (88) |
Retrospective review Loss to follow-up |
| Fischer et al, 201516 | 29 | Colonoscopy | Refractory “Severe CDI” or “severe/complicated CDI” |
Consecutive patients with severe and severe or complicated CDI refractory to antimicrobial therapy (vancomycin, fidaxomicin, metronidazole). All patients were evaluated for colectomy Severe CDI was defined as serum albumin < 3 g/dL plus either WBC ≥ 15,000 cells/mm3 or abdominal tenderness. Severe or complicated CDI was defined as any of the following:
|
Antibiotics were discontinued 12–24 hours before FMT | Retrospective case series Oral vancomycin resumed 24–48 hours after FMT for minimum 5 days if pseudomembranes were present. For patients not improving by days 6–7, vancomycin was stopped and FMT was repeated next day. If pseudomembranes were still present, vancomycin therapy was resumed for additional 5 days If a patient could not be discharged because of ongoing CDI symptoms, vancomycin was stopped on day 12–13 and third FMT performed on day 13–14 Treatment success was defined as complete resolution of diarrhea, no further need of anti-CDI therapy, avoidance of colectomy, and discharge from hospital |
Relatives or unrelated | Mean age 65.2 years (range 25–92 years) Median follow-up: 4.5 months Mean number of FMT doses administered: 1.5 (range 1–3) Severe CDI: n = 10 (Table A9) Severe or complicated CDI: n = 19 (Table A9) Overall cumulative survival after FMT was 93% (95% CI 84–100) at 1 month and 76% (95% CI 62–93) at 3 months 3 patients died of CDI-related and 5 from non–CDI-related causes in follow-up period |
Retrospective review Five patients had inflammatory bowel disease |
Abbreviations: CDI, Clostridium difficile infection; CI, confidence interval; FMT, fecal microbiota therapy; ICU, intensive care unit; PCR, polymerase chain reaction; SD, standard deviation; WBC, white blood cell.
Table A9.
Results of FMT from Fischer et al
| Study Parameters | Severe CDI, N = 10 | Severe or Complicated CDI, N = 19 |
|---|---|---|
| Number of patients receiving 1 FMT treatment, N (%) | 7 (70) | 9 (4) |
| Number of patients receiving 2 FMT treatments, N (%) | 3 (30) | 8 (42) |
| Number of patients receiving 3 FMT treatments, N (%) | 0 | 2 (11) |
| Median length of hospital stay (days) | 9 | 11.5 |
| Overall success rate at 30 days (%) | 10 (100) | 17 (89) |
Abbreviations: CDI, Clostridium difficile infection; FMT, fecal microbiota therapy.
Source: Adapted from Fischer et al.16
Table A10:
Average Cost Associated With CDI and RCDI Treatment per Episode
| Cost Parameter | Cost, $ | Derivation of Cost | Sources/Notes |
|---|---|---|---|
| Community-Based Treatment | |||
| Total cost of diagnostic testing | 49.50 | Ontario MOHLTC schedule of benefits | Levy et al, 201528 |
| FMT colonoscopy | 1,429 | Varier et al, 2015,25 Biltaji et al, 2014,33 and Guo et al, 201132 | |
| Physician visit | 203 | Levy et al, 201528 | |
| Physician visit for RCDI | 284 | Levy et al, 201528 | |
| Vancomycin 125 mg QID | 20.72 | $5.18 per pill | RAMQ cost30 |
| Metronidazole 500 mg TID | 2.11 | $0.703 per pill | ODB cost29 |
| Total cost per CDI patient | 542 | Includes diagnostic testing, physician visit for RCDI, metronidazole, and vancomycin treatment for CDI | Assumed that all CB patients receive vancomycin |
| Total cost per RCDI episode | 574 | Includes diagnostic testing, physician visit for RCDI, and vancomycin treatment for RCDI | Assumed that all CB patients receive vancomycin |
| Average cost per FMT treatment of RCDI | 1,866 | Includes diagnostic testing, FMT, physician visit for RCDI, and vancomycin treatment for RCDI | Calculated from Levy et al, 2015,28 Varier et al, 2015,25 Biltaji et al, 2014,33 and Guo et al, 201132 |
| Hospital-Based Treatment | |||
| Hospitalization cost associated with CDI | 11,930 | Length of stay = 13.6 days | Levy et al, 201528 (low estimation) |
| Hospitalization cost associated with RCDI | 15,330 | Length of stay = 13.6 days | Levy et al, 201528 (low estimation) |
| Physician visits | 284 | Levy et al, 201528 | |
| Physician visits per RCDI | 476 | Levy et al, 201528 | |
| Total per CDI (mild to moderate) | 12,243 | Levy et al, 201528 | |
| Total per CDI (severe) | 12,504 | Levy et al, 201528 | |
| Total per failed initial therapy for CDI patient | 12,514 | Levy et al, 201528 | |
| Total cost per RCDI patient | 16,096 | Includes the hospitalization cost associated with RCDI, physician visit for RCDI, and vancomycin treatment for RCDI | Calculated from Levy et al, 2015,28 Varier et al, 2015,25 Biltaji et al, 2014,33 and Guo et al, 201132 |
| Cost per RCDI FMT | 9,422 | Includes FMT, hospitalization cost associated with RCDI, physician visit for RCDI, and vancomycin treatment for RCDI | Calculated from Levy et al, 2015,28 Varier et al, 2015,25 Biltaji et al, 2014,33 and Guo et al, 201132 |
Abbreviations: CB, community based; CDI, Clostridium difficile infection; FMT, fecal microbiota therapy; MOHLTC, Ministry of Health and Long-Term Care; ODB, Ontario Drug Benefit; QID, four times daily; RAMQ, Régie de l'assurance maladie du Québec; RCDI, recurrent Clostridium difficile infection; TID, three times daily.
Appendix 4: Results of the Systematic Review
Recurrent Clostridium difficile Infections
One small (n = 43; 16 fecal microbiota therapy), unblinded RCT by van Nood et al from the Netherlands compared fecal microbiota therapy via nasoduodenal tube versus control groups who had vancomycin alone and vancomycin plus bowel lavage17:
Symptoms resolved in 81% of cases involving fecal microbiota therapy within 3 months compared with 31% and 23% for vancomycin and vancomycin plus bowel lavage control groups, respectively (P < .001 for fecal microbiota therapy vs. both control groups)
The study was terminated after the authors saw “extremely low” response rates in the control groups, which differed substantially from the 60% rate used for calculations of sample sizes
Although control groups received the same dose of vancomycin for 14 days, fecal microbiota therapy was administered after 4 to 5 days of oral vancomycin treatment
One small (n = 20), unblinded RCT from the United States compared two fecal microbiota treatment approaches: nasogastric tube versus colonoscopy18:
Overall, symptoms resolved in 70% of patients; the difference between treatment approaches was not significant (60% in nasogastric vs. 80% in colonoscopy, P = .63)
There was no non–fecal microbiota therapy control group
Fecal microbiota therapy was administered 3 days after stopping the antibiotic treatment of C. difficile infection
This RCT was a feasibility study and was not adequately powered to detect clinically significant differences in outcomes
We found 21 case series of recurrent C. difficile infections19–21,51–68:
Fecal microbiota therapy was delivered by various methods
Outcome reporting was variable, especially regarding the resolution of symptoms. Many studies reported a primary outcome that combined the resolution of symptoms and recurrence3
Authors commonly reported that antibiotics for C. difficile infection were given before fecal microbiota therapy to ensure that patients were asymptomatic or had a “reduction in symptoms” at the time of fecal microbiota administration.3 Therefore, fecal microbiota therapy was administered when patients were largely asymptomatic. Fecal microbiota therapy possibly contributed to further symptom resolution, recurrence prevention, or both3
Although stated outcomes included an element of symptom resolution, in most cases fecal microbiota therapy seemed to be given with the intent to prevent recurrence after antibiotic treatment had resolved all or most C. difficile symptoms3
Overall, in case-series studies, 85% of cases treated with fecal microbiota remained without recurrence3
Refractory Clostridium difficile Infection
We found seven case series of refractory C. difficile infection51,60,69,71–73,75:
Fecal microbiota therapy was delivered by various methods
No study compared fecal microbiota therapy with standard therapy or different methods of administration3
The reported resolution rate varied widely (0% to 100%). The overall resolution rate from the seven case series was calculated to be 55%3
Initial Clostridium difficile Infection
For initial C. difficile infection, we found one case series (n = 6)69 and one case report from 1953, which predated the discovery of C difficile and reported few details.73 For the case series of six patients, one patient was reported to be cured after fecal microbiota treatment.69
Appendix 5: International Guidelines
National Institute for Health and Care Excellence (NICE)
In March 2014, NICE recommended22:
Current evidence on the efficacy and safety of faecal microbiota transplant for recurrent Clostridium difficile infection is adequate to support the use of this procedure provided that normal arrangements are in place for clinical governance, consent and audit.
This procedure should only be considered for patients with recurrent C. difficile infections that have failed to respond to antibiotics and other treatments.
Clinicians should ensure that a confidential record is kept of the donor and recipient of each faecal microbiota transplant.
NICE encourages further research into faecal microbiota transplant for C. difficile infection, specifically to investigate optimal dosage, mode of administration and choice of donor.
Canadian Association of Gastroenterology
The 2014 position statement advised the following1:
Currently, there is sufficient evidence to recommend FMT in patients with C. difficile infection that have failed or had recurrent infection after 2 rounds of different antibiotics (usually metronidazole and vancomycin).
European Society of Clinical Microbiology and Infectious Diseases
In 2014 the following recommendation was reported for multiple recurrent C. difficile infections23:
For multiple recurrent C. difficile infections unresponsive to repeated antibiotic treatment, FMT in combination with oral antibiotic treatment is strongly recommended.
This quality of evidence was based on “evidence from at least one properly designed randomized controlled trial,” and the strength of recommendation “strongly supports a recommendation for use.”
American College of Gastroenterology
In 2013, the following recommendation was reported for the treatment of ≥ 3 C. difficile infection recurrences24:
If there is a third recurrence after a pulsed vancomycin regimen, FMT should be considered. (Conditional recommendation, moderate-quality evidence).
The strength of evidence was graded as “conditional” when uncertainty exists about the risk-benefit ratio. The quality of the evidence was graded as “moderate” if further research is likely to have an important impact and may change the estimate.
Appendix 6. Questions to Understand Lived Experience of Clostridium Difficile Infection and Fecal Microbiota Therapy
If Patient Has Undergone Fecal Microbiota Therapy
What is the impact of Clostridium difficile infection on your life? How does the condition affect your quality of life and the quality of life for your loved ones or caregivers?
What were your experiences of health interventions before fecal microbiota therapy (FMT)? For example, could you manage your condition with available therapies before FMT? Did you have any treatment for C. difficile infection before FMT? If yes, what kind of health care services did you require? Was there any associated cost?
What were your experiences with FMT? For example, what difference does it make to your quality of life? Are there any activities that you once enjoyed but couldn't do before the implant, and can do now? What was it like to go through FMT?
Did you have any post-procedure experiences? How long after FMT did you regain function in your day-to-day life?
After FMT, do you need any follow-up therapies for C. difficile infection? Does the follow-up therapy have any associated costs?
What expectations did you have of FMT? Were there any drawbacks or limitations?
If a Patient Has Not Undergone Fecal Microbiota Therapy
What is the impact of Clostridium difficile infection on your life? How does the condition affect your quality of life and the quality of life for your loved ones or caregivers?
What are your experiences of current health interventions aside from FMT? For example, can you manage your condition with available therapies aside from FMT? Are there any associated costs?
What expectations might you have of FMT? Do you have any perceived sense of positive aspects or drawbacks and limitations?
Author contributions
This report was developed by a multidisciplinary team from Health Quality Ontario. The lead clinical epidemiologist was Kristen McMartin, the lead health economist was Amar Chadee, and the senior program analyst in patient, caregiver, and public engagement was Mark Weir. The medical librarians were Corinne Holubowich and Caroline Higgins.
KEY MESSAGES
In patients who had recurrent Clostridium difficile infection, fecal microbiota therapy reduced diarrhea associated with C. difficile infection better than antibiotics. Treatment-related adverse events (such as short-term diarrhea or abdominal cramping) were more frequent in patients treated with fecal microbiota therapy than in patients treated with antibiotics.
Fecal microbiota therapy is cost-effective when compared with antibiotics in patients with recurrent C. difficile infection. If Ontario uses fecal microbiota therapy to treat patients with recurrent C. difficile infection, the health care system could save money.
This review did not find evidence about using fecal microbiota therapy in people infected with C. difficile for the first time or in people who have refractory infection.
This report was developed by a multidisciplinary team from Health Quality Ontario. The lead clinical epidemiologist was Kristen McMartin, the lead health economist was Amar Chadee, and the senior program analyst in patient, caregiver, and public engagement was Mark Weir. The medical librarians were Corinne Holubowich and Caroline Higgins, and the medical editor was Elizabeth Jean Betsch. Others involved in the development and production of this report were Irfan Dhalla, Nancy Sikich, Andrée Mitchell, Kellee Kaulback, Anne Sleeman, Claude Soulodre, Kristan Chamberlain, Susan Harrison, and Jessica Verhey.
About Health Quality Ontario
Health Quality Ontario is the provincial advisor on the quality of health care. We are motivated by a single-minded purpose: Better health for all Ontarians.
Who We Are
We are a scientifically rigorous group with diverse areas of expertise. We strive for complete objectivity, and look at things from a vantage point that allows us to see the forest and the trees. We work in partnership with health care providers and organizations across the system, and engage with patients themselves, to help initiate substantial and sustainable change to the province's complex health system.
What We Do
We define the meaning of quality as it pertains to health care, and provide strategic advice so all the parts of the system can improve. We also analyze virtually all aspects of Ontario's health care. This includes looking at the overall health of Ontarians, how well different areas of the system are working together, and most importantly, patient experience. We then produce comprehensive, objective reports based on data, facts and the voice of patients, caregivers and those who work each day in the health system. As well, we make recommendations on how to improve care using the best evidence. Finally, we support large scale quality improvements by working with our partners to facilitate ways for health care providers to learn from each other and share innovative approaches.
Why It Matters
We recognize that, as a system, we have much to be proud of, but also that it often falls short of being the best it can be. Plus certain vulnerable segments of the population are not receiving acceptable levels of attention. Our intent at Health Quality Ontario is to continuously improve the quality of health care in this province regardless of who you are or where you live. We are driven by the desire to make the system better, and by the inarguable fact that better has no limit.
REFERENCES
- (1).Moayyedi P, Marshall J, Yuan Y, Hunt R. Canadian Association of Gastroenterology position statement: fecal microbiota transplant therapy. Can J Gastroenterol Hepatol. 2014; 28(2): 66–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (2).Leong C, Zelenitsky S. Treatment strategies for recurrent Clostridium difficile infection. Can J Hosp Pharm. 2013; 66(6): 361–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (3).Drekonja D, Reich J, Gezahegn S, Greer N, Shaukat A, MacDonald R, et al. Fecal microbiota transplantation for Clostridium difficile infection: a systematic review. Ann Intern Med. 2015; 162(9): 630–8. [DOI] [PubMed] [Google Scholar]
- (4).Health Canada. Guidance document: regulation of fecal microbiota therapy for the treatment of C. difficile infections [Internet]. Ottawa (ON): Health Canada; 2015. Mar [cited 2015 Aug 20]. Available from: http://www.hc-sc.gc.ca/dhp-mps/consultation/biolog/fecal_microbiota-bacterio_fecale-eng.php [Google Scholar]
- (5).US Food and Drug Administration. Enforcement policy regarding investigational new drug requirements for use of fecal microbiota for transplantation to treat Clostridium difficile infection not responsive to standard therapies [Internet]. Silver Spring (MD): The Administration; 2013. Jul [cited 2015 Aug 20]. Available from: http://www.fda.gov/BiologicsBloodVaccines/GuidanceComplianceRegulatoryInformation/Guidances/Vaccines/ucm361379.htm [Google Scholar]
- (6).Review Manager (RevMan) [computer program]. Version 5.0. Copenhagen (DK): The Nordic Cochrane Centre, The Cochrane Collaboration; 2008. [Google Scholar]
- (7).Shea BJ, Grimshaw JM, Wells GAMB, Andersson N, Hamel C, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007; 7(10): 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (8).Guyatt GH, Oxman AD, Schunemann HJ, Tugwell P, Knottnerus A. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol. 2011; 64(4): 380–2. [DOI] [PubMed] [Google Scholar]
- (9).Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009; 6(6): e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (10).Cammarota G, Masucci L, Ianiro G, Bibbo S, Dinoi G, Costamagna G, et al. Randomised clinical trial: faecal microbiota transplantation by colonoscopy vs. vancomycin for the treatment of recurrent Clostridium difficile infection. Aliment Pharmacol Ther. 2015; 41(9): 835–43. [DOI] [PubMed] [Google Scholar]
- (11).Hirsch BE, Saraiya N, Poeth K, Schwartz RM, Epstein ME, Honig G. Effectiveness of fecal-derived microbiota transfer using orally administered capsules for recurrent Clostridium difficile infection. BMC Infect Dis. 2015; 15:191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (12).Ray A, Smith R, Breaux J. Fecal microbiota transplantation for clostridium difficile infection: the Ochsner experience. Ochsner J. 2014; 14(4): 538–44. [PMC free article] [PubMed] [Google Scholar]
- (13).Pierog A, Mencin A, Reilly NR. Fecal microbiota transplantation in children with recurrent Clostridium difficile infection. Pediatr Infect Dis J. 2014; 33(11): 1198–200. [DOI] [PubMed] [Google Scholar]
- (14).Lagier JC, Delord M, Million M, Parola P, Stein A, Brouqui P, et al. Dramatic reduction in Clostridium difficile ribotype 027-associated mortality with early fecal transplantation by the nasogastric route: a preliminary report. Eur J Clin Microbiol Infect Dis. 2015; 34(8): 1597–601. [DOI] [PubMed] [Google Scholar]
- (15).Satokari R, Mattila E, Kainulainen V, Arkkila PET. Simple faecal preparation and efficacy of frozen inoculum in faecal microbiota transplantation for recurrent Clostridium difficile infection - an observational cohort study. Aliment Pharmacol Ther. 2015; 41(1): 46–53. [DOI] [PubMed] [Google Scholar]
- (16).Fischer M, Sipe BW, Rogers NA, Cook GK, Robb BW, Vuppalanchi R, et al. Faecal microbiota transplantation plus selected use of vancomycin for severe-complicated Clostridium difficile infection: description of a protocol with high success rate. Aliment Pharmacol Ther. 2015; 42(4): 470–6. [DOI] [PubMed] [Google Scholar]
- (17).Van Nood E, Vrieze A, Nieuwdorp M, Fuentes S, Zoetendal EG, De Vos WM, et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med. 2013; 368(5): 407–15. [DOI] [PubMed] [Google Scholar]
- (18).Youngster I, Sauk J, Pindar C, Wilson RG, Kaplan JL, Smith MB, et al. Fecal microbiota transplant for relapsing Clostridium difficile infection using a frozen inoculum from unrelated donors: a randomized, open-label, controlled pilot study. Clin Infect Dis. 2014; 58(11): 1515–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (19).Patel NC, Griesbach CL, DiBaise JK, Orenstein R. Fecal microbiota transplant for recurrent Clostridium difficile infection: Mayo Clinic in Arizona experience. Mayo Clin Proc. 2013; 88(8): 799–805. [DOI] [PubMed] [Google Scholar]
- (20).MacConnachie AA, Fox R, Kennedy DR, Seaton RA. Faecal transplant for recurrent Clostridium difficile-associated diarrhoea: a UK case series. Q J Med. 2009; 102(11): 781–4. [DOI] [PubMed] [Google Scholar]
- (21).Aas J, Gessert CE, Bakken JS. Recurrent Clostridium difficile colitis: case series involving 18 patients treated with donor stool administered via a nasogastric tube. Clin Infect Dis. 2003; 36(5): 580–5. [DOI] [PubMed] [Google Scholar]
- (22).National Institute for Health and Care Excellence. Faecal microbiota transplant for recurrent Clostridium difficile infection: NICE interventional procedure guidance 485 [Internet]. London, UK: The Institute; 2014. [cited 2015 Aug 20]. Available from: http://www.nice.org.uk/guidance/ipg485 [Google Scholar]
- (23).Debast SB, Bauer MP, Kuijper EJ, European Society of Clinical Microbiology and Infectious Diseases. European Society of Clinical Microbiology and Infectious Diseases: update of the treatment guidance document for Clostridium difficile infection. Clin Microbial Infect. 2014; 20 Suppl 2:1–26. [DOI] [PubMed] [Google Scholar]
- (24).Surawicz CM, Brandt LJ, Binion DG, Ananthakrishnan AN, Curry SR, Gilligan PH, et al. Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infections. Am J Gastroenterol. 2013; 108(4): 478–98. [DOI] [PubMed] [Google Scholar]
- (25).Varier RU, Biltaji E, Smith KJ, Roberts MS, Kyle Jensen M, LaFleur J, et al. Cost-effectiveness analysis of fecal microbiota transplantation for recurrent Clostridium difficile infection. Infect Control Hosp Epidemiol. 2015; 36 (4): 438–44. [DOI] [PubMed] [Google Scholar]
- (26).Konijeti GG, Sauk J, Shrime MG, Gupta M, Ananthakrishnan AN. Cost-effectiveness of competing strategies for management of recurrent Clostridium difficile infection: a decision analysis. Clin Infect Dis. 2014; 58(11): 1507–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (27).Brandt LJ, Borody TJ, Campbell J. Endoscopic fecal microbiota transplantation: “first-line” treatment for severe Clostridium difficile infection? J Clin Gastroenterol. 2011; 45(8): 655–7. [DOI] [PubMed] [Google Scholar]
- (28).Levy AR, Szabo SM, Lozano-Ortega G, Lloyd-Smith E, Leung V, Lawrence R, et al. Incidence and costs of Clostridium difficile infections in Canada. Open Forum Infect Dis. 2015; 2(3): ofv076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (29).Ministry of Health and Long-Term Care. Ontario drug benefit formulary/comparative drug index [Internet]. Toronto (ON): The Ministry; 2015. [cited 2015 Oct 10]. Available from: http://www.health.gov.on.ca/en/pro/programs/drugs/formulary42/edition_42.pdf [Google Scholar]
- (30).Régie de l'assurance maladie du Québec. List of Medications: Régie de l'assurance maladie du Québec [Internet]. Quebec (QC): Ministry of Health and Social Services; [cited 2015 Oct 10]. Available from: https://www.prod.ramq.gouv.qc.ca/DPI/PO/Commun/PDF/Liste_Med/Liste_Med/liste_med_2015_11_20_en.pdf [Google Scholar]
- (31).Ministry of Health and Long-Term Care. Schedule of benefits physician services under the Health Insurance Act [Internet]. Toronto (ON): The Ministry; 2015. [cited 2015 Oct 31]. Available from: http://www.health.gov.on.ca/english/providers/program/ohip/sob/physserv/sob_master11062015.pdf [Google Scholar]
- (32).Guo B, Harstall C, Nguyen T, Ohinmaa A. Fecal transplantation for the treatment of Clostridium difficile-associated disease or ulcerative colitis. Edmonton (AB): Institute of Health Economics; 2011. [PubMed] [Google Scholar]
- (33).Biltaji E, Varier R, Smith K, Roberts M, Lafleur J, Nelson RE. Cost-effectiveness analysis of treatment strategies for initial Clostridium difficile infection. Value Health. 2014; 17 (3): A38. [DOI] [PubMed] [Google Scholar]
- (34).Health Technology Assessment international Interest Group on Patient and Citizen Involvement in HTA. FAQ for HTA agencies and policy makers [Internet]. Edmonton (AB): Health Technology Assessment international; 2015. [updated 2015; cited 2015 Aug 5]. Available from: http://www.htai.org/interest-groups/patient-and-citizen-involvement/resources/for-hta-agencies-and-policy-makers/faq-for-hta-agencies-and-policy-makers.html#c3229 [Google Scholar]
- (35).Barham L. Public and patient involvement at the UK National Institute for Health and Clinical Excellence. Patient. 2011; 4(1): 1–10. [DOI] [PubMed] [Google Scholar]
- (36).Messina J, Grainger DL. A pilot study to identify areas for further improvements in patient and public involvement in health technology assessments for medicines. Patient. 2012; 5(3): 199–211. [DOI] [PubMed] [Google Scholar]
- (37).Tjornhoj-Thomsen T, Hansen HP. Knowledge in health technology assessment: who, what, how? Int J Technol Assess Health Care. 2011; 27(4): 324–9. [DOI] [PubMed] [Google Scholar]
- (38).Rowe G, Frewer LJ. A typology of public engagement mechanisms. Sci Technol Hum Val. 2005; 30(2): 251–90. [Google Scholar]
- (39).Brundisini F, Giacomini M, DeJean D, Vanstone M, Winsor S, Smith A. Chronic disease patients’ experiences with accessing health care in rural and remote areas: a systematic review and qualitative meta-synthesis. Ont Health Technol Assess Ser. 2013; 13(15): 1–33. [PMC free article] [PubMed] [Google Scholar]
- (40).Health Technology Assessment international Interest Group on Patient and Citizen Involvement in HTA. Introduction to health technology assessment [Internet]. 2015. [updated 2015]. Available from: http://www.htai.org/fileadmin/HTAi_Files/ISG/PatientInvolvement/v2_files/Resource/PCISG-Resource-Intro_to_HTA__KFacey__Jun13.pdf
- (41).Strauss AL, Corbin JM. Basics of qualitative research: techniques and procedures of developing a grounded theory. 2nd ed. Thousand Oaks (CA): Sage Publications; 1998. [Google Scholar]
- (42).Strauss AL, Corbin JM. Grounded theory methodology: an overview. In: Denzin NK, Lincoln YS, editors. Handbook of qualitative research. Thousand Oaks (CA): Sage Publications; 1994. p. 273–85. [Google Scholar]
- (43).Strauss AL, Corbin JM. Grounded theory research: procedures, canons, and evaluative criteria. Qual Sociol. 1990; 13(1): 3–21. [Google Scholar]
- (44).Bagdasarian N, Rao K, Malani PN. Diagnosis and treatment of Clostridium difficile in adults: a systematic review. JAMA. 2015; 313(4): 398–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (45).O'Horo JC, Jindai K, Kunzer B, Safdar N. Treatment of recurrent Clostridium difficile infection: a systematic review. Infection. 2014; 42(1): 43–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (46).Sha S, Liang J, Chen M, Xu B, Liang C, Wei N, et al. Systematic review: Faecal microbiota transplantation therapy for digestive and nondigestive disorders in adults and children. Aliment Pharmacol Ther. 2014; 39(10): 1003–32. [DOI] [PubMed] [Google Scholar]
- (47).Cammarota G, laniro G, Gasbarrini A. Fecal microbiota transplantation for the treatment of Clostridium difficile infection: a systematic review. J Clin Gastroenterol. 2014; 48(8): 693–702. [DOI] [PubMed] [Google Scholar]
- (48).Kassam Z, Lee CH, Yuan Y, Hunt RH. Fecal microbiota transplantation for Clostridium difficile infection: systematic review and meta-analysis. Am J Gastroenterol. 2013; 108(4): 500–8. [DOI] [PubMed] [Google Scholar]
- (49).Dodin M, Katz DE. Faecal microbiota transplantation for Clostridium difficile infection. Int J Clin Pract. 2014; 68(3): 363–8. [DOI] [PubMed] [Google Scholar]
- (50).Sofi AA, Silverman AL, Khuder S, Garborg K, Westerink JMA, Nawras A. Relationship of symptom duration and fecal bacteriotherapy in Clostridium difficile infection-pooled data analysis and a systematic review. Scand J Gastroenterol. 2013; 48(3): 266–73. [DOI] [PubMed] [Google Scholar]
- (51).Youngster I, Russell GH, Pindar C, Ziv-Baran T, Sauk J, Hohmann EL. Oral, capsulized, frozen fecal microbiota transplantation for relapsing Clostridium difficile infection. JAMA. 2014; 312(17): 1772–8. [DOI] [PubMed] [Google Scholar]
- (52).Rubin TA, Gessert CE, Aas J, Bakken JS. Fecal microbiome transplantation for recurrent Clostridium difficile infection: report on a case series. Anaerobe. 2013; 19(1): 22–6. [DOI] [PubMed] [Google Scholar]
- (53).Garborg K, Waagsbo B, Stallemo A, Matre J, Sundoy A. Results of faecal donor instillation therapy for recurent Clostridium difficile-associated diarrhoea. Scand J Infect Dis. 2010; 42 (11–12): 857–61. [DOI] [PubMed] [Google Scholar]
- (54).Khan MA, Sofi AA, Ahmad U, Alaradi O, Khan AR, Hammad T, et al. Efficacy and safety of, and patient satisfaction with, colonoscopic-administered fecal microbiota transplantation in relapsing and refractory community- and hospital-acquired Clostridium difficile infection. Can J Gastroenterol Hepatol. 2014; 28(8): 434–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (55).Cammarota G, Ianiro G, Gasbarrini A, Masucci L, Sanguinetti M. Faecal transplantation for Clostridium difficile infection: three cases treated in Italy. Dig Liver Dis. 2014; 46(5): 475. [DOI] [PubMed] [Google Scholar]
- (56).Pathak R, Enuh HA, Patel A, Wickremesinghe P. Treatment of relapsing Clostridium difficile infection using fecal microbiota transplantation. Clin Exp Gastroenterol. 2013; 7(1): 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (57).Hamilton MJ, Weingarden AR, Sadowsky MJ, Khoruts A. Standardized frozen preparation for transplantation of fecal microbiota for recurrent Clostridium difficile infection. Am J Gastroenterol. 2012; 107(5): 761–7. [DOI] [PubMed] [Google Scholar]
- (58).Kelly CR, De Leon L, Jasutkar N. Fecal microbiota transplantation for relapsing Clostridium difficile infection in 26 patients: methodology and results. J Clin Gastroenterol. 2012; 46(2): 145–9. [DOI] [PubMed] [Google Scholar]
- (59).Mattila E, Uusitalo-Seppala R, Wuorela M, Lehtola L, Nurmi H, Ristikankare M, et al. Fecal transplantation through colonoscopy is effective therapy for recurent Clostridium difficile infection. Gastroenterology. 2012; 142(3): 490–6. [DOI] [PubMed] [Google Scholar]
- (60).Mellow MH, Kanatzar A. Colonoscopic fecal bacteriotherapy in the treatment of recurrent Clostridium difficile infection: results and follow-up. J Okla State Med Assoc. 2011; 104(3): 89–91. [PubMed] [Google Scholar]
- (61).Rohlke F, Surawicz CM, Stollman N. Fecal flora reconstitution for recurrent Clostridium difficile infection: results and methodology. J Clin Gastroenterol. 2010; 44(8): 567–70. [DOI] [PubMed] [Google Scholar]
- (62).Yoon SS, Brandt LJ. Treatment of refractory/recurrent C. difficile-associated disease by donated stool transplanted via colonoscopy: a case series of 12 patients. J Clin Gastroenterol. 2010; 44(8): 562–6. [DOI] [PubMed] [Google Scholar]
- (63).Emanuelsson F, Claesson BEB, Ljungstrom L, Tvede M, Ung KA. Faecal microbiota transplantation and bacteriotherapy for recurrent Clostridium difficile infection: a retrospective evaluation of 31 patients. Scand J Infect Dis. 2014; 46(2): 89–97. [DOI] [PubMed] [Google Scholar]
- (64).Silverman MS, Davis I, Pillai DR. Success of self-administered home fecal transplantation for chronic Clostridium difficile infection. Clin Gastroenterol Hepatol. 2010; 8(5): 471–3. [DOI] [PubMed] [Google Scholar]
- (65).Gustafsson A, Berstad A, Lund-Tonnesen S, Midtvedt T, Norin E. The effect of faecal enema on five microflora-associated characteristics in patients with antibiotic-associated diarrhoea. Scand J Gastroenterol. 1999; 34(6): 580–6. [DOI] [PubMed] [Google Scholar]
- (66).Paterson DL, Iredell J, Whitby M. Putting back the bugs: bacterial treatment relieves chronic diarrhoea. Med J Aust. 1994; 160(4): 232–3. [PubMed] [Google Scholar]
- (67).Tvede M, Rask-Madsen J. Bacteriotherapy for chronic relapsing Clostridium difficile diarrhoea in six patients. Lancet. 1989; 1(8648): 1156–60. [DOI] [PubMed] [Google Scholar]
- (68).Dutta SK, Girotra M, Garg S, Dutta A, von Rosenvinge EC, Maddox C, et al. Efficacy of combined jejunal and colonic fecal microbiota transplantation for recurrent Clostridium difficile infection. Clin Gastroenterol Hepatol. 2014; 12(9): 1572–6. [DOI] [PubMed] [Google Scholar]
- (69).Zainah H, Hassan M, Shiekh-Sroujieh L, Hassan S, Alangaden G, Ramesh M. Intestinal microbiota transplantation, a simple and effective treatment for severe and refractory Clostridium difficile infection. Dig Dis Sci. 2015; 60(1): 181–5. [DOI] [PubMed] [Google Scholar]
- (70).Weingarden AR, Hamilton MJ, Sadowsky MJ, Khoruts A. Resolution of severe Clostridium difficile infection following sequential fecal microbiota transplantation. J Clin Gastroenterol. 2013; 47(8): 735–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (71).Lee CH, Belanger JE, Kassam Z, Smieja M, Higgins D, Broukhanski G, et al. The outcome and long-term follow-up of 94 patients with recurrent and refractory Clostridium difficile infection using single to multiple fecal microbiota transplantation via retention enema. Eur J Clin Microbiol Infect Dis. 2014; 33(8): 1425–8. [DOI] [PubMed] [Google Scholar]
- (72).Bowden TA, Mansberger AR, Lykins LE. Pseudomembraneous enterocolitis: mechanism for restoring floral homeostasis. Am Surg. 1981; 47(4): 178–83. [PubMed] [Google Scholar]
- (73).Eiseman B, Silen W, Bascom GS, Kauvar AJ. Fecal enema as an adjunct in the treatment of pseudomembranous enterocolitis. Surgery. 1958; 44(5): 854–9. [PubMed] [Google Scholar]
- (74).Van Nood E, Speelman P, Kuijper E, Keller J. Struggling with recurrent Clostridium difficile infections: is donor faeces the solution? Euro Surveill. 2009; 14(34):pii: 19316. [DOI] [PubMed] [Google Scholar]
- (75).Weingarden A, Hamilton MJ, Sadowsky MJ, Khoruts A. Changes in bacterial composition following fecal microbiota transplantation for severe Clostridium difficile infection. Gastroenterology. 2013; 1):S829. [DOI] [PMC free article] [PubMed] [Google Scholar]