Abstract
Background
As Bangladesh, India and Nepal progress towards visceral leishmaniasis (VL) elimination, it is important to understand the role of asymptomatic Leishmania infection (ALI), VL treatment relapse and post kala-azar dermal leishmaniasis (PKDL) in transmission.
Methodology/ Principal Finding
We reviewed evidence systematically on ALI, relapse and PKDL. We searched multiple databases to include studies on burden, risk factors, biomarkers, natural history, and infectiveness of ALI, PKDL and relapse. After screening 292 papers, 98 were included covering the years 1942 through 2016. ALI, PKDL and relapse studies lacked a reference standard and appropriate biomarker. The prevalence of ALI was 4–17-fold that of VL. The risk of ALI was higher in VL case contacts. Most infections remained asymptomatic or resolved spontaneously. The proportion of ALI that progressed to VL disease within a year was 1.5–23%, and was higher amongst those with high antibody titres. The natural history of PKDL showed variability; 3.8–28.6% had no past history of VL treatment. The infectiveness of PKDL was 32–53%. The risk of VL relapse was higher with HIV co-infection. Modelling studies predicted a range of scenarios. One model predicted VL elimination was unlikely in the long term with early diagnosis. Another model estimated that ALI contributed to 82% of the overall transmission, VL to 10% and PKDL to 8%. Another model predicted that VL cases were the main driver for transmission. Different models predicted VL elimination if the sandfly density was reduced by 67% by killing the sandfly or by 79% by reducing their breeding sites, or with 4–6y of optimal IRS or 10y of sub-optimal IRS and only in low endemic setting.
Conclusion/ Significance
There is a need for xenodiagnostic and longitudinal studies to understand the potential of ALI and PKDL as reservoirs of infection.
Author Summary
The role of asymptomatic Leishmania infection (ALI), PKDL and VL relapse in transmission is unclear as VL elimination is achieved in the Indian subcontinent. ALI, PKDL and relapse studies lacked a reference standard and appropriate biomarker. ALI was 4–17-fold more prevalent than VL. The risk of ALI was higher in VL case contacts. Most infections remained asymptomatic or resolved spontaneously. The natural history of PKDL showed variability. Twenty nine percent had no past history of VL treatment. The risk of VL relapse was higher with HIV co-infection. Modelling studies predicted different effects. Early diagnosis was unlikely to eliminate VL in the long term. ALI was predicted to contribute to 82% of the overall transmission, VL to 10% and PKDL to 8%. Another model predicted that VL cases were the main driver for transmission. VL elimination was predicted if the sandfly density was reduced by 67% by killing the sandfly or by 79% by reducing their breeding sites, or with 4–6y of optimal IRS or 10y of sub-optimal IRS and only in low endemic setting. There is a need for more studies to fully understand the potential of ALI and PKDL as reservoirs of infection.
Introduction
The concomitance of anthroponotic transmission of visceral leishmaniasis (VL), a single species of sandfly as the only known vector for transmission, the largely localized geographic endemicity of the disease, the availability of field-based diagnostic tests and highly effective drugs for treating VL, together, favour the elimination of the disease as a public health problem in the Indian subcontinent through effective surveillance, early detection and treatment, and integrated vector control strategies [1]. Furthermore, historical evidence of near-eradication of VL in the 1970s following insecticide spraying for malaria control in the 1950s and 1960s in India supports the rationale for VL elimination in the Indian subcontinent [2]. In 2005, the Governments of Bangladesh, India and Nepal signed a memorandum of understanding to eliminate VL and set the target to reduce its annual incidence to less than 1 per 10,000 population (at the upazila level in Bangladesh, block level in India and district level in Nepal) by 2015 [3]. This political commitment was recently reinforced at a meeting of the Ministers of Health in September 2014 with the aim to make the Southeast Asia region including Bhutan and Thailand free of VL by 2017 or earlier [4]. Substantial progress has been made towards the elimination target in Bangladesh with only two out of 98 endemic upazilas reporting a incidence rate greater than 1 per 10,000 in 2015 (Table A in S1 Text). An external assessment of the national VL control program in Nepal conducted in 2015 indicated that all the 12 previously endemic districts have achieved the elimination target (Table B in S1 Text). On the other hand, despite a declining trend in the number of reported VL cases, 90 out of 456 blocks continue to report an annual incidence of more than 1 per 10,000 in India (Table C in S1 Text). Despite substantial progress, a major challenge evident from recent outbreak investigations and surveillance data has been the increasing emergence of new ecological niches of indigenous transmission in previously non-endemic regions of Bangladesh and Nepal [5–9].
Research on VL and post Kala-azar dermal leishmaniasis (PKDL) has focused largely on the clinical and epidemiology aspects of the disease. A large body of research has evaluated diagnostics [10–13], potential biomarkers for treatment response of VL and PKDL [14], treatment options [15], and vector control [16,17]. The parasite, vector species and alternative animal reservoirs for VL infection in Africa differ from that in the Indian subcontinent and research findings cannot be simply applied from one to the other [18]. Many questions remain about the natural history, the progression of asymptomatic Leishmania infection (ALI) to symptomatic VL disease, development of PKDL, the pathogenesis, the immune response to infection and disease [19]. Moreover, data on transmission dynamics, infectiveness and vector bionomics, role and duration of acquired immunity after infection are scarce, which limits the use of mathematical modelling to predict and inform treatment and vector control strategies for VL elimination [20]. Furthermore, the complex interactions of co-infection with HIV alters the transmission dynamics and increases the vulnerability of both infections to treatment failure and relapse and has the potential to thwart elimination efforts [21–25]. The emergence of parasite resistance to antimonials that led to a sharp increase of up to 65% treatment failure in a case series [26–28] seen in Bihar, India between 1980 and 1997, also suggested the potential for development of resistance to miltefosine [29–31] and liposomal amphotericin B [32,33]. This could further alter the transmission dynamics and is a major concern for elimination efforts [34,35].
As countries progress towards the elimination target using current strategies of early detection and treatment of clinical disease and vector control, it is necessary to understand the consequences of under-reporting on planning and evaluating VL elimination strategies, the contribution of ALI to sustain transmission and emergence of new hotspots for infection [36]. It is equally important to understand the contribution of PKDL to transmission and its potential role as a reservoir of infection, to inform how long elimination efforts need to be continued and how they should be targeted to prevent recrudescence of new VL epidemics in the future [1]. The objective of this systematic review was to synthesize existing literature on transmission dynamics and relapse rates of VL caused by L donovani in the Indian subcontinent. In particular, the review focused on the role of ALI and PKDL as potential reservoirs for transmission so as to inform current strategies for achieving and maintaining VL elimination in the Indian subcontinent.
Methods
The Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) statement was used to guide the process and reporting of this review (Table D in S1 Text) [37]. The broader outcome of interest was to systematically review information related to and affecting transmission dynamics of visceral leishmaniasis from the perspective of elimination. Primary outcomes reviewed were the role of ALI and PKDL as potential reservoirs and their contribution to transmission. Secondary outcomes of interest included the potential of HIV co-infection and relapse in altering the transmission dynamics, and vector bionomics related to transmission (Fig 1).
Fig 1. Conceptual framework for the systematic review of transmission dynamics of visceral leishmaniasis in the Indian subcontinent.
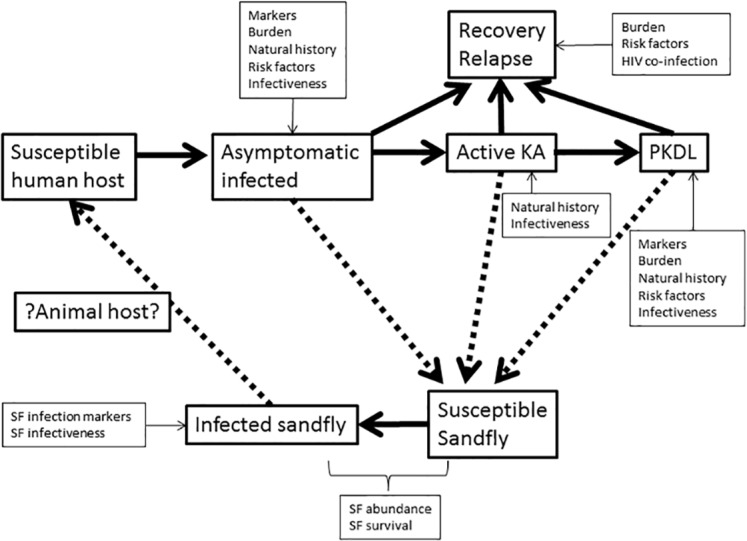
For simplicity, the relapse and recovery stages are shown together and the infectiveness of the relapse stage to the sandfly is omitted.
We searched multiple databases (United States National Library of Medicine, Cochrane Library, WHO Library Information System, National Database of Indian Medical Journals) using different combinations of MeSH terms (with synonyms and closely related words) such as ‘Leishmaniasis, Visceral’, ‘Disease transmission, Infectious’, ‘risk factors’, ‘relapse’, ‘recurrence’, ‘asymptomatic infections’, ‘Basic reproduction number’, ‘disease outbreaks’, ‘contact tracing’, and text words such as ‘transmission risk’, ‘disease progression’, ‘surveillance’ etc. with and without restriction to MeSH terms ‘Bangladesh OR India OR Nepal’. An example of a search query is shown in Table E in S1 Text. Duplicates were removed and two reviewers (SH, SQ) independently screened the title and abstract of all articles and determined eligibility. We also screened articles that showed up as related during the search. The full text of all eligible articles was further assessed by SH and SQ independently for inclusion. We also screened the references of all included articles to identify any new articles hitherto missed. We reviewed all the earlier reviews and the individual studies that were included in the past reviews. Articles were included based on consensus between SH and SQ. For multiple articles referring to the same study, we included the article with the most recent finding. However, we included all articles that referred to different aspects of the same study. The research community involved in visceral leishmaniasis research in the Indian subcontinent is small and well-networked. We requested researchers for information on ongoing studies and share preliminary findings or manuscripts in preparation or submission. We accessed meeting reports of the Regional Technical Advisory Group (RTAG) for Kala-azar elimination, research study findings that were presented at recent conferences and presentations made by country program managers at a WHO TDR meeting for the most recent update on VL status on the Indian subcontinent. We could not assess the extent of publication bias if any.
The scope and eligibility criteria for the review are given in Box 1.
Box 1
We included studies on VL and PKDL:
from Bangladesh, Bhutan, India and Nepal
articles in the English language
articles related to the burden of ALI and PKDL–their markers (excluding genetic markers) and risk factors
related to the natural history and transmission dynamics of VL–the infectiveness of the ALI and PKDL
on co-infection with HIV and relapse following VL and PKDL
We excluded studies on VL and PKDL that focused solely on:
burden, clinical aspects and epidemiology of VL and outbreak investigations
evaluated diagnostics
clinical drug trials (except to estimate relapse rate)
evaluated early detection, treatment and vector control program strategies
The following topics were beyond the scope of this systematic review:
pathogenesis and immunogenicity of VL and PKDL
bionomics of the Ph. argentipes vector
mother to child transmission and transmission through blood transfusion
Mathematical modelling of VL transmission
Data was extracted from the full text articles directly into a structured table under variables such as diagnostic used, seroprevalence, negative sero-conversion, asymptomatic to symptomatic ratio, risk factors / markers for ALI, progression to symptomatic VL disease, relapse, risk factors for relapse, infectiveness, etc.
Simple proportions and risks (hazard ratio, risk ratio, odds ratio) as applicable and their range across different studies were used to describe the outcome variables of interest. We also compared the different mathematical models used for quantifying transmission dynamics with respect to their structures, data sources, assumptions, limitations, and predictions. We did not attempt a meta-analysis as the number of studies that focused on transmission dynamics, infectiveness were limited in the context of the Indian subcontinent. The risk of bias was ascertained using the Newcastle-Ottawa bias assessment scale for observational studies [38] and the Cochrane risk of bias assessment tool for trials [39].
Results
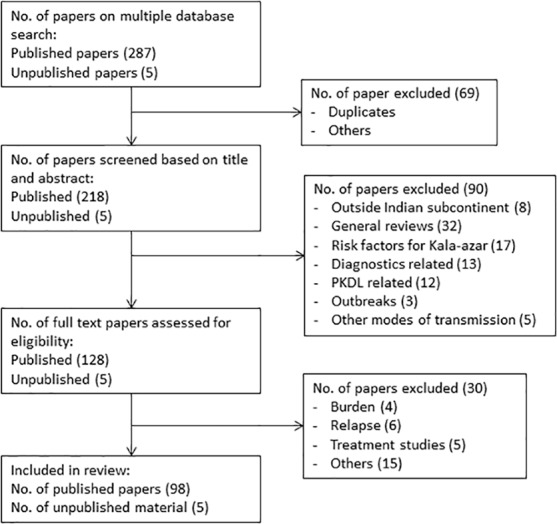
The review covers Bangladesh, Bhutan, India and Nepal representing more than 73% of the global burden of VL in 2012 [40]. A total of 292 papers (including 5 meeting reports) were identified based on the multiple database searches as of 01 March 2016 of which 69 were excluded as duplicates or for other reasons. A further 90 papers were excluded (32 general reviews, 8 papers from outside the Indian subcontinent, 17 papers on risk factors for VL etc.) based on screening of the title and abstract. Another 30 papers were excluded (four were related to disease burden, six related to relapse etc.) after a full text appraisal. A total of 98 published and 5 meeting reports from 1942 to 2016 were included in the final review (Fig 2). The assessment of the risk of bias in the included studies is shown in Tables F to I in S1 Text. Most cross-sectional surveys did not justify sample size or demonstrated comparability of non-respondents or comparability of the different outcome groups. The risk of bias due to loss to follow up was high from most cohort studies. Case-control studies did not report on the non-response rates.
Fig 2. PRISMA flowchart of inclusion and exclusion of articles for the review.
Asymptomatic Leishmania infection–burden, risk factors, natural history, infectiveness
A total of 31 articles including two reviews were identified. ALI lacked a reference standard and appropriate biomarker. It was variably ascertained by a positive serology test (rk39 ICT, rk39 ELISA or DAT), PCR, qPCR or LST in an otherwise healthy individual from an endemic area [41,42]. Only one study established the specificity of the assay on non-endemic controls [43]. Individuals with past history of VL were often but not always excluded from serological surveys. Table 1 gives the prevalence and incidence of ALI by country and by the different tests and thresholds used to ascertain infection. The majority of studies from which prevalence was estimated were not population based. Seropositivity among endemic healthy controls in diagnostic evaluation studies were also included for estimating prevalence of ALI. The seropositivity as measured by antibody response to rk39 antigen was 7.4% [44]. The seropositivity as measured by antibody response to the saliva antigen of the sandfly vector ranged between 43.5–63.2%; this is a proxy for human exposure to sandfly but not necessarily infection [45]. The prevalence of ALI was 34.8% and 3.8% for a parasitaemia of >0 and >1 parasite genome/mL on qPCR respectively [46]. The prevalent ALI cases outnumbered that of prevalent symptomatic VL cases by a factor of 4.0 in Bangladesh, 13 in Nepal and ranging from 7.6 to 17 in India [47,48]. The ratio of incident asymptomatic infection to incident clinical disease increased with decreasing incidence rates of VL (Table J in S1 Text). However, more standardized and validated tests are needed to establish more accurately the prevalence of ALIs [46,49]. The risk of ALI was significantly higher (OR ranging from 1.25–5.5) in individuals in close contact (household member) with a known VL case [50,51] or with the presence of other seropositive or recently sero-converted individuals in the household (OR 1.37–2.22) [52] indicative of spatial and temporal clustering of infections [49,53]. Livestock ownership was associated with a lower risk for infection (OR 0.4–1.0) [54] in Nepal but a significantly higher risk (OR 1.16–2.1) in India [55,56]. In contrast, a higher cattle density in the community had a protective effect against infection in Bangladesh (OR 0.97) and Nepal (OR 0.63) [47,51]. Risk factors associated with VL such as poverty, low socioeconomic status, malnutrition, poor housing conditions, damp floors, mud walls, sleeping on the floor, sleeping outside and proximity to water bodies, also significantly increased the risk for ALI [51,52,55,57].
Table 1. ALI as a potential reservoir for transmission in the Indian subcontinent.
| Reference | Bangladesh | India | Nepal | |
|---|---|---|---|---|
| Prevalence of ALI | ||||
| - rk39 ICT | [50,58–62] | 0.25% | 5.6–13.8% | |
| - rk39 ELISA | [41,42,44,47,49,63,64] | 10–14% | 5.4–26.3% | 6.4–12.6% |
| - DAT | [41,42,44,50,51,54,56,61–63,65–72] | 3.02% | 3.1–26.4% | 4.4–16.2% |
| - LST | [47,54,73,74] | 19–35% | 19–23.1% | 13.2% |
| - PCR | [42,53,58,62,65,71,75,76] | 7.2–36.9% | 5.1–17.9% | |
| Prevalence among healthy contacts of current or past VL cases | ||||
| - rk39 ICT | [60] | 0.08% | ||
| - rk39 ELISA | [42,77] | 19.5–43.6% | ||
| - DAT | [42,65,66,69] | 14.4–100% | 20.8% | |
| - IFAT | [78] | 17.5% | ||
| - LST | [78] | 5% | ||
| - PCR | [42,65] | 20.6% | 12.5% | |
| Incidence (1y) | ||||
| - rk39 ICT | [60] | 0% (6mo) | ||
| - rk39 ELISA | [41,44,46,47] | 6.31% | 1.3–27.3% | |
| - DAT | [41,44,46,48,55,72] | 2.5–27.3% | 2.9–7.2% | |
| - qPCR (parasite/ml) | [46] | 34.8% (>0); 3.8% (>1p/ml); 1.36% (>5p/ml); | ||
| -rKRP42 ELISA (at 30mo) | [79] | 23.4% | ||
| ALI to VL ratio | [47,48] | 4:1 | 7.6:1 | 9.6:1 |
| Risk factors for ALI | ||||
| - contact of VL (cf non-contact of VL) OR | [47,50–52,57,65] | 1.37–1.85 | 1.25–3.71 | 1.66–5.5 |
| - presence of other seropositive or sero-converter in house OR | [52] | 1.37–2.22 | 1.37–2.22 | |
| - family size OR | [54] | 4.4 | ||
| - damp floor OR | [55] | 2.4 | ||
| - mud walls OR | [54,55] | 28.9 | 4.3 | 3.0 |
| - proximity to pond OR | [54,55] | 2.1 | 3.7 | |
| - proximity to forest OR | [57] | 3.67 | ||
| - livestock ownership OR | [54–56] | 1.16–2.1 | 0.4–1.0 | |
| - cattle density OR | [47,51] | 0.97 | 0.63 | |
| - spatial clustering of PCR+ human with PCR+ animals | [53] | significant | ||
| - Risk of spatial clustering of PCR+ or sero+ human for transmission | [49,53] | High risk | No effect | |
| - sleeping covered/inside OR | [55] | 0.5–0.6 | ||
| - age OR | [41,47,51,52,54,56] | 1.12 | 1.57–3.68 | 1.57–7.29 |
| - highest (cf lowest) SES OR | [52] | 0.63 | 0.63 | |
| - poverty OR | [51] | 3.86 | ||
| - indoor residual spraying OR | [55] | No effect | ||
| - IRS more than 18mo ago OR | [52] | 1.53 | 1.53 | |
| - use of bednet OR | [47,52,55] | No effect– 0.82 (ns) | 0.7–1.09 (ns) | 0.66 (ns) |
| Proportion asymptomatic with spontaneous resolution at 1y | ||||
| - rk39 ELISA | [41,47,62] | 50.21% | 59–60% | |
| - DAT | [41,48,62,66] | 33–86.7% | 86.7% | |
| Progression of ALI to VL within 1y | ||||
| - rk39 ICT | [58,62] | 12.5–23.1% | ||
| - rk39 ELISA | [44,47,49] | 5.4–25% (6mo– 2y) | 1.8–23.3% | 7.7% |
| - DAT | [44,48,50,68] | 5.4% (2y) | 1.5–16.6% | 1.681 – 9.8% |
| - PCR | [46,58] | 2.5–17.9% | ||
| -rKRP42 ELISA | [79] | 29.2% | ||
| - Contacts of VL case | [58,66,77] | 24.1–69.1% | ||
| - Contacts of active VL case | [66] | 18.8% | ||
| - Contacts of cured VL case | [66] | 30.8% | ||
| - Non-contacts | [58,66] | 5–38% | ||
| Risk factors for progression of ALI to VL | ||||
| - contact of VL (cf non-contact) OR | [47,62,66] | 2.85 | 3.36–4.82 | |
| - contact of cured VL (cf contact of active VL) OR | [66] | 1.64 | ||
| - Risk of spatial clustering of PCR+ or sero+ for progression to VL | [49] | Highest risk | ||
| - age (10y increment) OR | [47] | 0.74 | ||
| - beef, goat consumption OR | [47] | 0.49 | ||
| Biomarkers for progression of ALI to VL | ||||
| - rk39 titres HR | [44,80] | |||
| Negative | reference | reference | reference | |
| Mod positive | 1.6 | 1.6–4.9 | -- | |
| Strongly positive | 17.7 | 7.7–39.6 | 26.9 | |
| - rk39 titres among contacts of VL (positive predictive value) | [77] | 44% at 3mo, 56.6% at 6mo; | ||
| - rk39 / DAT titres high | [46] | 60% | ||
| - Sero-converters rk39 titres HR | [44,80] | |||
| Negative | reference | reference | ||
| Mod positive | 4.7 | 0.9 (ns) | ||
| Strongly positive | 165 | 15.9–123.9 | ||
| - DAT titres HR | [44] | |||
| <1:1600 | reference | reference | ||
| 1600 - <25600 | 1.0–3.8 | -- | ||
| >1:25600 | 7.9–26.6 | 35.6 | ||
| - Sero-converters DAT titres HR | [44] | |||
| <1:1600 | reference | reference | ||
| 1600 - <25600 | 6.6–9.0 | 10.1 | ||
| >1:25600 | 44.5–111.0 | 99.2 | ||
| DAT+ve (cf DAT-ve) RR at 1y | [48] | 3.42 | 3.42 | |
| Recent DAT sero-converter (cf EHC) RR at 1y | [48] | 11.5 | 11.5 | |
| Immune and other markers | ||||
| - IFN- γ, NO, CRP | [47,81] | Raised | Raised | |
| - TNF –α, IL-2, IL-4 | [81] | Low | ||
| - Serum retinol, zinc | [47] | Low | ||
| Parasite markers | ||||
| - parasite load (>5genome equivalent/mL) | [46,76] | 80% | ||
1: at 6mo follow up
Note: cf (compared from); CRP (C-reactive protein); DAT (Direct agglutination test); EHC (Endemic healthy controls); ELISA (Enzyme linked immunosorbent assay); HR (Hazard ratio); IFN- γ (Interferon gamma); IL-2 (Interleukin 2), IL-4 (Interleukin 4); LST (Leishmanin skin test); NO (Nitric oxides); OR (Odds ratio); PCR (Polymerase chain reaction); qPCR (quantitative polymerase chain reaction); rk39 (recombinant kinetoplast 39); RR (Relative risk); TNF –α (Tumor necrosis factor alpha)
Most infections remained asymptomatic [42]. Spontaneous resolution (sero-reverting from positive to negative status) was seen in 33–86.7% of ALI within a year [41,48,62,66]. The proportion recovering spontaneously was lower for ALI with higher antibody titres [47]. On the other hand, the proportion of ALI that progressed to symptomatic disease within one year ranged between 1.5–23% [44,48–50,58,62,68]. It was higher (18.8–69.1%) amongst seropositive contacts of VL compared to seropositive non-contacts (5–38%) [58,66,77]. Seropositive contacts were 1.64–4.82-fold more likely to progress to clinical disease compared to seropositive non-contacts of a known VL case [47,49,62]. Anti-leishmania antibody titres were strong predictors of progression of ALI to symptomatic VL disease. Healthy but seropositive individuals with moderate antibody titres as measured by DAT were up to 5-times, and those with high titres were 8–40-times more likely to progress to symptomatic disease than those who were seronegative [44,46]. The risk for progression to symptomatic disease was significantly greater (up to 9 and 111-fold for moderate and high titres respectively) despite the small numbers amongst sero-converters [44,48]. Raised levels of immune cytokines and chemokines such as interferon-γ, nitric oxides, C-reactive protein and lowered levels of TNF-α, interleukin-2 and interleukin-4 were other potential markers for progression of ALI to clinical disease [47,81]. Parasitaemia levels were 500-fold lower in ALI than in active VL disease; individuals with a parasitaemia >5 parasite genome / mL were at higher risk of developing clinical VL [46,76].
Xenodiagnostic studies or artificial feeding experiments were limited in scale and number. In one study, 5.3% of a total of 258 laboratory-bred Ph argentipes became infected when fed on active VL patients [82]. There were no studies from the Indian subcontinent that quantified the infectiveness potential of infected asymptomatic individuals. Mathematical transmission models estimated the infectiveness of an early (PCR+, DAT-) and late asymptomatic infected (PCR+, DAT+) individual to be 2.5 and 3.3% assuming that a VL patient would infect 100% of sand flies feeding on them [83,84]. The model further assumed that the relative infectiveness of an early asymptomatic infected (PCR+ but seronegative) individual was half of that of a late asymptomatic infected individual.
PKDL–a reservoir for infection?
PKDL is hypothesized to be the reservoir for the Leishmania parasite and was incriminated in the resurgence of VL in West Bengal, India in the 1990s following discontinuation of insecticide spraying [85]. A total of 35 studies on PKDL including 6 reviews were identified. Except for one longitudinal study each in Nepal and India, most studies were cross-sectional surveys or based on surveillance data. There was no standard case definition for PKDL diagnosis, though operational case definitions are available from the WHO since 2010 [86]. All rk39 positive cases, with or without a past history of VL, with skin lesions suggestive of PKDL were considered probable PKDL by most studies. Confirmed PKDL required the demonstration of parasite in the skin lesion. Table 2 summarizes the findings of burden, natural history, risk factors and infectiveness of PKDL. The prevalence of confirmed PKDL ranged between 4.4–4.8 per 10,000 population in Bangladesh and India [87–89]. The incidence of PKDL has been estimated to be 0.1 per 10,000 (Table K in S1 Text). The development and natural history of PKDL showed wide variability. The proportion of PKDL without a preceding history of VL was between 3.8–28.6% [90–94]. The proportion of treated VL cases who developed PKDL within a year averaged 1–3% [95,96]. The mean period from VL treatment to development of PKDL was 1–4 years. The duration to development of PKDL did not differ by the drug used for VL treatment. The duration was slightly longer for nodular PKDL (34mo) compared to macular or papular PKDL (22.8–23.8mo). Active surveillance of a population of 24,814 individuals in Bangladesh between 2002 and 2010 identified 98 untreated PKDL patients, 48 (about 49%) of whom resolved spontaneously with a median time of 19 months [91]. The younger age group was more likely (17.1%) to develop PKDL compared to older VL cases (12.5%). They also developed PKDL earlier (27mo compared to 50mo) [87]. Family history of VL and clustering was a significant risk factor for development of PKDL [88,94]. Inadequate treatment of VL with antimonials was associated with a 11.6-fold higher risk of developing PKDL [96].
Table 2. PKDL as a potential reservoir of infection in the Indian subcontinent.
| Reference | Bangladesh | India | Nepal | |
|---|---|---|---|---|
| Burden | ||||
| Prevalence (per 10000 pop) | [87–89] | 6.28 (probable); 4.4 (confirmed) | 7.8 (probable); 4.4–4.82 (confirmed) | |
| Incidence (per 10000 pop) | [90] | 1–21 | ||
| Incident PKDL per 100 VL cases | [90,91,96] | 3–9.7% (1y); 10% (2y); 17% (3y) | 1.4% (2y); 2.5% (2 – 4y); 3.6% (4 – 8y); | |
| Natural history | ||||
| Prop PKDL without a past h/o VL | [90–94,97–100] | 9.2% | 3.85–20% | 28.6% |
| Prop of VL developing PKDL post-VL treatment | [95,96,100] | 0.29–15% (5y) | 1.4% (1y); 2.5% (4y); 2.9% (5y); 3.6% (8y) | |
| VL treatment–PKDL duration | [87,88,90,92–96,98–100] | 3y (2 –4y); | 12mo– 3.13y (range 1mo– 20y); 23mo (post-antimonial); 29mo (post-amphotericin); 9mo (post-liposomal amphotericin); 31mo (post-miltefosine); 25mo (post-paramomycin) | 23–26.9mo (range 6mo– 5y); 22.8mo (macular); 23.8mo (papular); 34mo (nodular); |
| Prop of PKDL by VL–PKDL duration | [93,95,97] | 33.0–36.4% (1y); 68.2% (2y); 19.3–82% (<5y); 18–70.5% (>5y); Post-liposomal amphotericin: 1.2y; Post-antimonial: 2.9y (1.5–5.5y); | ||
| Prop PKDL resolved without treatment | [91] | 49%; | ||
| Duration to PKDL resolution | [91] | 19mo | ||
| Onset–treatment time lag for PKDL | [93,98] | 2y (range 1 – 12y); Onset–treatment duration varied with type of PKDL lesion; | 28.4mo (macular); 26.1mo (papular); 39.5mo (nodular); | |
| Risk factors | ||||
| - Young age at VL (cf older age) | [87,88,90,91] | OR: 1.36 | Higher risk | |
| - clustering | [88] | Higher risk | ||
| - inadequate VL treatment | [96] | OR: 11.68 | ||
| Infectiveness of PKDL to SF | ||||
| - SF infected after feeding on PKDL | [101,102] | 32–53% |
Note: cf (compared from); h/o (history of); SF (sandfly); OR (Odds ratio)
We identified two xenodiagnostic studies done on PKDL patients from the Indian subcontinent. The proportion of sandfly getting infected after feeding on PKDL patients in an experimental setting ranged from 32–53% with the highest rate of infection of the sandfly seen on the 4th day post-feed [101,102]. For lack of data, transmission dynamics modelling studies assumed the infectiveness of PKDL to be either 50 or 100% in order to estimate other parameters of interest such as infectiveness of the asymptomatic stage of infection [84]. One of the model variants was structured in a way to assume that only VL and PKDL (but not ALI) contributed to transmission. With this and other assumptions of sandfly density, biting rate, life expectancy etc., the infectiveness of PKDL relative to VL was estimated by this model variant to range between 2.32–2.72 [83].
Relapse–a potential threat to VL elimination?
A total of 20 studies relevant to relapse including eight drug trials and six cohort studies were identified from the Indian subcontinent. There was no standard case definition for relapse. Most studies required demonstration of the parasite to confirm a relapse following either a clinical cure or parasite cure at the end of treatment for VL or PKDL.
VL relapse
The 1 year cumulative incidence of VL relapse following VL treatment with antimonials ranged from 0.14–1.67% [103–106]. A relapse rate of up to 3.7% and up to 20% was seen following treatment with liposomal amphotericin and miltefosine respectively (Table 3). The relapse incidence was higher (8.1–67%) for HIV-co-infected individuals [103,107]. The mean duration from VL treatment to relapse ranged from 3.75 to 10 months with 68% relapsing within a year following treatment with liposomal amphotericin [29,32,108]. The risk of relapse was higher (OR 1.94–3.54) in children, and those who presented with a shorter duration of symptoms prior to VL treatment [108,109]. The risk of relapse was higher (16% at 1y, 20% at 2y and 26% at 4y) for individuals with HIV co-infection [9,21,110]. L donovani antigen-specific IgG1 levels were significantly elevated in treatment failure and relapsed cases compared to cured VL patients [111]. Similarly, a rise in anti-rk39 antibody titres to levels higher than pre-treatment levels following treatment indicated treatment failure and relapse [64]. Quantitative PCR could potentially define thresholds for parasite load to predict relapse but there were no studies from the Indian subcontinent [21].
Table 3. Relapse following VL and PKDL in the Indian subcontinent.
| Reference | Bangladesh | India | Nepal | |
|---|---|---|---|---|
| VL relapse | ||||
| Incidence of VL relapse | ||||
| - post-antimonial VL treatment | [103–106] | 0.6% (1y) | 0.14–1.67% (1y); 67% (HIV co-infected– 1y); | |
| - post-miltefosine VL treatment | [29,31,109,112–118] | 1.6–11.1% (6mo); 7.6–12.8% (1y); | 6–10.8% (6mo); 12.8–20.0% (1y); | |
| - post liposomal amphotericin treatment | [9,32,33,107,108,110,116] | 3.6% | 0–0.26% (6mo); 1.39–3.7% (1y); 8.1% (HIV co-infected - 1y); 26.5% (HIV co-infected - 2y); 17–49.1% (HIV co-infected); | |
| Duration to relapse distribution (post-liposomal amphotericin treatment) | [108] | 15.1% (<6mo); 52.9% (6 – 12mo); 31.9% (>12mo); | ||
| Duration to relapse | [29,32,108,110] | 3.75–10.1mo; 10mo (HIV co-infected) | ||
| Risk factors for VL relapse following treatment with miltefosine or liposomal amphotericin | ||||
| - children (cf adults) OR | [31,108,109,113] | 1.94–3.54 | 3.19 | |
| - male (cf female) OR | [108,109] | 1.74–2.14 | 2.14 | |
| - decrease in spleen size < 0.5cm/day at discharge OR | [108,109] | 1.0–1.55 | 1.0 | |
| - longer duration of symptoms prior to treatment OR | [108,109] | 0.62–1.0 | 1.0 | |
| - Risk of relapse with HIV co-infection | [9,21,110] | 16% (1y); 20% (2y); 26% (4y); 6.4% (1y) (combination therapy) | ||
| - Anti-retroviral therapy for HIV co-infection after admission RR | [110] | 0.25 | ||
| Markers for VL relapse | ||||
| - rk39 ELISA titres | [64] | No correlation | ||
| - parasite genotype | [31] | No difference between cured VL and relapse; | ||
| - CD+4 count (in HIV-co-infected) | [103,107] | <200 /cmm | ||
| - promastigote morphology | [30] | Procyclic: Longer slender body; Metacyclic: shorter body; Increased metacyclogenesis; | ||
| - macrophages | [30] | Higher percentage of macrophages infected with parasite; | ||
| PKDL relapse | ||||
| Incidence of PKDL relapse following PKDL | [9,88,92,119,120] | 13% | 0–12.5% (post-miltefosine); 22%; | |
| Risk factors for PKDL relapse | ||||
| - drug dosage | [92] | No correlation; | ||
| - treatment duration | [121] | 43% (post-miltefosine for 3mo); 0% (post-miltefosine for 4mo); | ||
| Parasite resistance (drug susceptibility) | ||||
| - promastigote survival (IC50) | [122] | PKDL: 11.45 (SD: 4.19); VL: 2.58 (SD: 1.58) | ||
| - promastigote survival (IC50) (VL relapse following VL) | [31,122] | Pre-miltefosine: 1.86; Post-miltefosine cured: 2.43; Post-miltefosine relapse: 4.72; | No difference between cured VL and relapse; | |
| - promastigote survival (IC50) (PKDL relapse) | [122] | Pre-miltefosine: 8.63; Post-miltefosine relapse: 16.13; | ||
Note: IC50 (Inhibitory concentration 50%); SD (Standard deviation); cf (compared from); OR (Odds ratio); rk39 (recombinant kinetoplast 39); ELISA (Enzyme linked immunosorbent assay)
PKDL relapse
The cumulative incidence of a PKDL relapse following PKDL treatment ranged from 0–12.5% [9,92]. Two of the 9 (22%) PKDL patients detected in a house to house survey were relapsed cases of PKDL [88]. There was no correlation between the miltefosine dosage used for treating PKDL and PKDL relapse [92]. However, the proportion of PKDL relapse following a 3mo PKDL treatment with miltefosine was significantly higher (43%) compared to PKDL patients treated with 4mo of miltefosine [121]. There were two case reports of recurrence of VL following PKDL possibly triggered by immunosuppression due to concurrent infection [123]. A higher proportion of macrophages infected with the parasite was reported in relapse. There was no difference in the parasite genotype but some phenotype changes and increased meta-cyclogenesis was seen [30].
Parasite resistance to drugs has also been studied as a potential cause for relapse. Overall, promastigote survival was significantly higher in intracellular amastigote cultures obtained from PKDL compared to VL patients. More importantly, promastigote survival was significantly higher in isolates from relapse cases compared to pre-treatment isolates (Table 3) [122]. In contrast, there was no difference in parasite survival between cured VL and relapse cases [31]. One transmission modelling study that modelled the effect of drug-resistant parasites on treatment failure rates, simulated different scenarios where either disease-related factors, pathogenicity (resistant parasite would cause more VL cases compared to susceptible parasite) or virulence (symptomatic VL case with resistant parasite would infect more sandfly) or transmission-related factors (asymptomatic or symptomatic host will infect more sandfly or sandfly will infect more host) were varied to predict the effect of drug resistance on treatment failure rate. The study concluded that increased transmissibility of resistant parasites (and not antimonial resistance alone) was the most likely reason for the unusually high treatment failure up to 65% seen in India between 1980–97 [27,34].
Modelling transmission dynamics for planning and evaluation of VL elimination
We reviewed seven modelling studies that used data from the Indian subcontinent [34,80,83,84,124–127]. Transmission was modelled to quantify the levels and consequences of under-reporting, to quantify and predict the effect of different treatment or vector control strategies on VL incidence and / or prevalence and to ascertain the potential of ALI and PKDL as reservoirs of infection. All models were deterministic albeit with slightly varying compartments for the different transmission and clinical stages. The major differences in the model structure, data sources used to fit the model, assumptions, fixed and estimated parameters, scenarios simulated, main findings and limitations are summarized in Table L in S1 Text. Under-reporting can be a problem for planning and evaluation of elimination strategies. The first attempt at estimating under-reporting ratios was based on mathematical modelling that predicted a 90% under-reporting rate in 5 and 8 of the 21 endemic districts in Bihar, India in 2003 and 2005 respectively [124]. As a result, 3–5 districts were misclassified as high or low risk. Furthermore, the model predicted that the population density, health infrastructure, literacy level of the district had no effect on the extent of under-reporting which was sensitive to changes in VL endemicity levels. Community-based surveys reported an actual under-reporting of VL cases by a factor of 8.13 in 2003 [128] and 4.17 in 2005 in Bihar, India [129]. More than 85% of VL patients sought treatment from the public sector and was consistent with a downward trend in under-reporting, which was largely attributed to the free availability of VL drugs in government facilities under the elimination program [35]. Any attempt at interpreting the current reported disease trends should take into account this drastic change in underreporting ratio.
Assuming that clinical cases were responsible for the bulk of transmission, country-specific empirical data on health seeking behaviour was used to parameterize a transmission dynamics model to predict the effect of very early diagnosis (when non-specific symptoms such as fever appeared before the classical signs and symptoms of VL) and to characterize the profile of a potential diagnostic product [126]. Patients in Nepal, typically first presented with VL symptoms to the health system and had a shorter duration of onset of symptoms to diagnosis and treatment, whereas in India, patients sought care earlier at the stage of non-specific symptoms, and experienced delayed diagnosis and remained untreated for a longer duration [130]. The study shows the importance of earlier diagnosis and prompt therapy in VL elimination but also the risk that reduced transmission will expose the population to future epidemics, with waning herd immunity if vigilance is not maintained and diagnostic delays increase–a factor which might further delays the detection of an epidemic.
The models shows that the importance of novel diagnostics that can detect the infection in asymptomatic carries before they develop full VL, where high specificity is at a prime, even if sensitivity is relatively low. The reason is that the challenge of early testing with the intention of treating is to avoid false positives, especially with decreasing prevalence.
Transmission dynamics was modelled to predict the effect of treatment of VL and PKDL patients on VL elimination, simulating different scenarios of detection delays, varying duration of treatment regimens, varying rate of treatment failure and relapse [84]. The model was fitted to the KALANET data to predict a best-case treatment scenario (early case detection, shorter duration, and more efficacious treatment) to reduce VL prevalence but no effect on the prevalence of ALI. Such a scenario reduced PKDL incidence from 1 to 0.6 per 10,000 but had a minimal effect on VL incidence (the benchmark for the elimination program). The model predicted that transmission was predominantly driven by asymptomatic infected individuals and early case detection and treatment had no substantive effect on overall transmission. A variation of this model which tested the assumption of PKDL (as opposed to ALI infection) as the reservoir of infection predicted that ALI contributed to 82% of the overall transmission compared to 10% by symptomatic VL and 8% by PKDL patients [83].
Transmission dynamics was similarly modelled to predict the effect of different vector control strategies on VL elimination simulating different scenarios of optimal and sub-optimal IRS under varying endemicity levels and different assumptions of infection reservoirs. The transmission of the parasite between the host and sandfly was dependent on the infectiveness of the host or of the sandfly with a single bite, the mean biting rate and the sandfly density. The biting rate was assumed to be 0.25 / day (inverse of the feeding interval assumed to be 4 days [131]) and the latency period in the sandfly was assumed to be 5 days [132]. The elimination target could be achieved if the sandfly density was reduced from 5.27 to 1 per human, the life expectancy of the sandfly halved from 14 to 7 days, or the interval between blood feeds for the female sandfly doubled from 4 to 8 days or by a combination of any of these [84]. Entomology surveys estimated a prevalence of infected sandfly to range from 4.9–12% [64,71,133,134]. Table 4 gives details of sandfly abundance, distribution and feeding behaviour and risk factors affecting sandfly density. The effect of vector control on reducing PKDL prevalence would be delayed due to the latency between recovering from VL and developing PKDL. The same model estimated the basic reproduction number (R0) as 4.71 (95% CI: 4.1–5.4). The effective reproduction number (Re) was reduced non-linearly by IRS and LLINs and linearly by environmental management for vector control [125]. The model predicted that VL would be eliminated if the sandfly density was reduced by 67% (95% CI: 60–72%) by killing the sandfly with IRS or LLINs or if the sandfly density was reduced by 79% (95% CI: 75–82%) by reducing their breeding sites with environmental management for vector control or by a combination of these. Compared with these model predictions, the actual reduction in sandfly density of 24.9–43.7% with LLIN [135,136] and 42% with environmental management for vector control [136] seen in intervention trials (Table 4), would not be sufficient to reduce transmission to achieve the VL elimination target. However, the sandfly reduction of 72.4% seen in the intervention trial [136] with IRS would be adequate to reduce the transmission level (Re<1) to achieve elimination. A more recent model designed to test different scenarios of optimal and sub-optimal application of IRS (sandfly density reduced by 63% and 31.5% respectively) in varying endemicity settings predicted that optimal use of IRS reduced the VL incidence by 25% and 50% at 1y and 2y respectively at all endemicity levels [83]. VL incidence continued to decline as the burden of ALI became less. However, the decline in VL incidence was slower if PKDL (not ALI) was assumed to be the main reservoir of infection. The model predicted VL elimination with 4 – 6y of optimal IRS or 10y of sub-optimal IRS and only in low endemic (VL incidence < 5 / 10,000) setting whereas VL was not eliminated even with 12y of optimal IRS if PKDL were assumed to be the main reservoir of infection. A longer period to development of PKDL, a longer PKDL duration increased the transmission pressure to slow down the decline in VL incidence. Model predictions of VL elimination by IRS depended on the assumptions about the main reservoir for infection (ALI or PKDL) and were sensitive to other model assumptions such as the proportion of ALI progressing to symptomatic disease and the proportion of VL developing PKDL. However these predictions were robust to assumptions of infectiveness of early asymptomatic relative to that of late asymptomatic stage.
Table 4. Sandfly abundance, infectiveness, risk factors and effects of vector control strategies.
| Reference | Bangladesh | India | Nepal | |
|---|---|---|---|---|
| SF abundance | ||||
| SF distribution | [137,138] | Vegetation (30.6%), mixed dwelling (26.7%), cattle shed (18.6%), human dwelling (12.1%), chicken coop (12%); Cattle shed, mixed dwelling (77%); | ||
| SF density | [139–141] | Human dwelling: 10.22 SF/MH; Mixed dwelling: 17.09 SF/MH | Human dwelling: 25 SF/MH Cattle shed: 100 SF/MH; Peak: 5.60 SF/MH | 4.4 female SF/MH; |
| SF saliva antibody titres in human | [45,142] | 43.5–63.2% Positive correlation with female SF density; | 43.5–63.2% | |
| Prevalence of infected SF | [71,133,134,143] | Microscopy: 0.1%; PCR+: 4.9–17.37%; PCR+: 1.5% (annual), 2.84% (winter), 1.04% (summer), 0.85% (monsoon); | PCR+: 12% | |
| Prop SF infected after feeding on infected host | [82,143] [144] | 2.43–5.33%; 100% | ||
| SF feeding preference | [145] | Cattle: 68%; human: 17.9%; birds: 4%; | ||
| Factors affecting SF density | ||||
| - seasonality | [134,137,140,146–150] | Peak: Mar; Blood-fed SF peak: May; | 5.60–13.0 SF/MH (peak season); 2.13–8 SF/MH (lean season); 10.09–11.14 SF/trap (Sept–Oct); 0.28–0.37 SF/trap (Jan–Feb); | Peak: Mar, Sept; |
| - indoor temperature | [148,151] | 29–32°C (peak season); 20–24°C (lean season); | ||
| - relative humidity | [151] | Predicts SF abundance | ||
| - soil pH, soil moisture | [150,151] | Alluvial soil; | ||
| - vegetation | [146,151] | Inversely correlation | ||
| - land use, land cover suitability for SF habitat | [151,152] | High suitability: water bodies, sandy area, moist fallow area, weeds, grassland, near water body, marshy land, dry fallow, settlement; Low suitability: plantation; | ||
| - VL prevalence | [134,146] | No correlation | ||
| Effect of SF control | ||||
| - IRS effect and duration | [5,136,147,153–155] | Rebound at 11mo; 94% reduction at 6mo; | Rebound at 3mo; 124% reduction at 6mo; Human dwelling: 4.5 SF/MH at 1mo; Mixed dwelling: 5 SF/MH at 1mo; Cattle shed: 6 SF/MH at 1mo; No SF after 2nd IRS at 1.5mo interval; | Reduced from 11 to 0.6 SF/trap; 52–53% reduction at 6mo; |
| - LLIN effect and duration | [136,141,147,154] | 60% lower at 11mo; 68% reduction at 6mo; | 298%1 reduction at 6mo; | Reduced from 7.9 to 0.9 SF/trap; 16–22% (NS) reduction at 6mo; |
| - EVM effect and duration | [136,154,156] | 9% reduction at 6mo; | 108%1 reduction at 6mo; | Reduced from 8.2 to 2.6 SF/trap; 4–51% reduction at 6mo; |
1 Larger than 100% as the SF density decreased in intervention group but increased in control group at 6mo
Note: SF (Sandfly); SF/MH (Sandfly per man-hour); PCR+ (Polymerase Chain Reaction positive); NS (not significant); EVM (environmental management for vector control); IRS (Indoor residual spraying); LLIN (Long lasting insecticide nets)
Discussion
We identified eight systematic reviews including two Cochrane reviews–five reviews were on diagnostic tests and biomarkers, and one review each on treatment options, risk factors, and vector control. This is the first systematic review of transmission dynamics from the perspective of VL elimination in the Indian subcontinent.
The burden of ALI relative to active VL disease was high in the Indian subcontinent. The thresholds for serodiagnosis were originally defined for active VL disease and need to be validated for diagnosis of ALI. Studies of ALI were hampered by lack of a reference standard and appropriate biomarker which also hampers the evaluation of any new assay. However, any assay used could at least be evaluated to be 100% specific in a sufficiently large group of non-endemic controls. Molecular techniques such as PCR and q-PCR are now increasingly used to diagnose early ALI with parasitaemia levels as low as less than one parasite genome per mL of blood. At such low levels, it would be important to know whether the parasite DNA detected by PCR was from a metabolically-active parasite and not just a residual DNA from a dead parasite. The parasite load in ALI was reported to be 500-fold lower than that in active VL disease [76]. A study from Ethiopia that modelled the L donovani parasite load in the blood of asymptomatic and symptomatic individuals to estimate their infectiveness to the sandfly species Ph orientalis predicted that 3.2% of the most heavily-infected individuals (parasitaemia levels greater than 500 parasites genomes / mL) were responsible for 62% (95% CI: 53–79%) of the infected sandfly population [157]. Based on the parasite load threshold of <5 per mL for ALI [76], this implied that symptomatic infection was the predominant driver for transmission and by implication treatment of symptomatic VL cases would be most effective to reduce transmission. Nevertheless, AVL may continue to act as a hidden reservoir of infection which will build up to eventually lead to another epidemic outbreak in the presence of vector abundance. The infectiveness of HIV–Leishmania co-infected patients maybe higher due to higher parasitaemia levels [158]. Laboratory studies from Ethiopia suggest a L donovani parasite load of 20,000 per mL of blood in the host is required to infect the sandfly species Ph orientalis [159]. Infectiousness was seen to be correlated with parasite loads in dogs exposed to natural L infantum infection [160]. The threshold for parasitaemia at which a sandfly that ingests less than 1 μL of blood during a feed on an infected host can get infected needs to be defined through xenodiagnostic studies or artificial feeding experiments. Studies using different modelling approaches, assumptions and data sets gave contradictory results–one study predicted that ALI contributed to 82% of the overall transmission whereas another study predicted that 3.2% of infected human VL cases with the highest parasitemia were responsible for 62% of all the infections in sandfly [83,157]. It seems likely that only those persons with very high parasitaemia would serve as effective reservoirs infecting the sandfly [161]. Nevertheless, even if the transmission potential for ALI is relatively low compared to active VL or PKDL when prevalence is high, their potential should not be underestimated as they represent a large reservoir of infection [162]. There is now evidence from outbreak investigations in new eco-niches that suggest that local transmission can be maintained in isolated communities in the absence of VL or PKDL cases [8,163]. Further research is needed to define markers and thresholds for defining ALI, for infectiveness to the sandfly and to predict the potential for progression of ALI to symptomatic VL disease.
PKDL is a poorly understood sequelae of VL. Most of the evidence on the natural history of PKDL came from epidemiological and clinical studies. Given the long and variable duration to the development of PKDL, it is logistically difficult to conduct longitudinal studies. Research on PKDL is also hampered by a lack of a validated definition, appropriate biomarkers, and standardized definition for treatment end-point and cure. Some case definitions biased the selection of PKDL cases to only those with a past history of VL treatment. Nevertheless, the burden of PKDL in the Indian subcontinent was considerable. It was suggested that as few as 0.5% of PKDL cases during a VL epidemic can potentially sustain transmission to make VL endemic [164]. Differences in methodology to detect PKDL cases (active case detection in Bangladesh, passive surveillance based on patients with the more severe nodular form of PKDL reporting to health facilities in India), differences in treatment practices for VL (antimonial treatment for 3 weeks in Bangladesh compared to 4 weeks in India and Nepal), and treatment compliance may partly explain the higher PKDL burden seen in Bangladesh compared to India and Nepal. Further research is needed to understand differences in pathogenesis of PKDL within the Indian subcontinent. It has been presumed that PKDL is a potential reservoir for infection that may trigger a recrudescence of the disease post-elimination as was seen in the 1990s in India. On the other hand, PKDL has not been identified as the source of outbreaks in previously non-endemic areas in the last two decades. There are many unresolved issues for PKDL. The continental differences in the pathogenesis, immune response and transmission of PKDL prevent extrapolation of findings from Africa to the Indian subcontinent [165,166]. The potential role of qPCR in predicting the development of PKDL needs to be studied. The parasitaemia threshold for infectiveness of PKDL needs to be defined as parasites are more likely to be in the skin lesions relative to their presence in blood. Moreover, the infectiveness thresholds are likely to differ for the nodular form of PKDL compared to the maculo-papular form which is far more frequent in the Indian subcontinent. Experimental studies have shown that 32–53% of laboratory bred sandfly were infected after feeding on PKDL patients [101,102]. Modelling studies have assumed the infectiveness of PKDL to be the same or half of that of an active VL case. Further research is needed to define markers and thresholds for the development of PKDL and their infectiveness to the sandfly to better understand the role of PKDL as a potential reservoir especially in the maintenance phase of VL elimination.
The demonstration of parasite in the blood of domestic animals and the significant spatial clustering of PCR-positive animals and humans suggests domestic animals as an alternate reservoir for an infection thought to be only anthroponotic in transmission on the Indian subcontinent [53]. In mixed dwellings where cattle sheds are attached to the house, 66% of the blood meals of the sandfly was of bovine origin whereas 19% of the sandfly fed on human [145]. In contrast, 81–92% of the blood meals were of bovine origin from cattle sheds compared to 49–100% blood meals of human origin in human dwellings [145,167,168]. Domestic animals could increase transmission pressure by virtue of being an untreated reservoir for the parasite. Proximity to domestic animals may also increase sandfly density, and as a result transmission, due to increased availability of blood meals for the sandfly as well as organic manure for breeding of larvae and resting. On the other hand, proximity to domestic animals may lower transmission by altering sandfly feeding behaviour and lessen the human exposure to sandfly [36,47,51]. Even in the scenario where domestic animals are just reservoirs for infection without zoonotic transmission, they could be a potential threat to VL elimination unless they alter sandfly feeding behaviour and lower human exposure to sandfly bite. Further research is needed to understand the potential of domestic animals as a reservoir for infection and its complex effect on VL transmission.
Though the burden of relapse is relatively low following treatment with miltefosine or liposomal amphotericin, it is important in the context of transmission dynamics. First, relapse contributes to the overall infective pool of parasite in the host that is available for transmission to the sandfly. Second, in HIV positive individuals who are not on antiretroviral therapy, VL relapse increases the risk of transmission because of the suppressed immunity and higher parasite load and unresponsiveness to drug treatment [21]. Third, the possibility of parasite resistance to anti-Leishmania drugs seen in patients with HIV co-infection experiencing relapse may be an important reservoir for drug-resistant parasite by being parasitaemic for longer periods or for their increased risk to develop PKDL [169].
Treatment outcome measures should be standardised; the case definition of relapse varied among studies. Initial cure was assessed on clinical resolution and / or parasitological cure at intervals ranging from 1–2 months post-treatment [112,113]. Final definitive cure was assessed clinically at intervals ranging from 6–12 months post-treatment [32,108]. Most studies were hospital-based and could not differentiate between reinfection, reactivation and relapse [31]. They were not powered or designed to follow up patients post-treatment long enough to estimate relapse rates. Though the burden of VL–HIV co-infection is relatively lower on the Indian subcontinent than in Africa, the importance for monitoring for relapse and emergence of drug-resistant parasites cannot be overemphasized.
The interest in modelling VL transmission to inform VL elimination program strategies is recent and comes primarily from two groups of modellers from the Neglected Tropical Diseases Modelling Consortium. The proportion and progression of the various infective stages in transmission cycle, the persistence of antibodies and acquired immunity following infection, the host and vector infectiveness profile need to be based on large well-designed and powered longitudinal field trials so as to better parameterize the model [20]. Models on vector control measures do not consider the duration of the post-intervention effects relative to the duration of infectiveness by individuals (whether VL, ALI or PKDL) if not ‘removed’. Current models need to be further refined to allow for stochastic variation, factor-in the effect of temporal and spatial clustering of cases, and the effect of acquired immunity on transmission dynamics. Further research is needed on vector bionomics, the potential role of an alternate animal reservoir for infection and its complex effect on transmission dynamics.
Our review, though systematic, was subject to several methodological and substantive limitations. First, we restricted our review to literature in the English language. However, we were aware that the majority of the research work on VL in the Indian subcontinent has come from a relatively small community of researchers and institutes historically and as we contacted the key persons in this network for additional information, it is unlikely that we may have missed out on any substantive evidence. Second, as we restricted the scope of our systematic review to the Indian subcontinent, we may have missed out on some lessons learnt from VL studies in other continents, lessons that could be partly or wholly extrapolated to the Indian subcontinent. Third, we did not do a systematic review of the sandfly biology component of the transmission cycle. We hope this component will be covered in a separate systematic review. Fourth, we did not cover other reported modes of transmission such as through blood transfusion [170], organ transplant [171,172], laboratory accidents [173] and the occasional reports of mother to child transmission [174]. These transmission routes are very rare. The mechanical transmission of the Leishmania parasite through syringes used by intravenous drug users is probably more relevant [175]. Though currently not yet problematic, the rising number of HIV–Leishmania co-infections is gaining importance in the region as also in the risk group of IV drug users is present in more urban communities.
As progress towards VL elimination gains momentum, there are many ongoing and planned research efforts aimed at improving treatment and vector control strategies [9]. Research is ongoing for improved diagnostics and identifying biomarkers for ALI. A longitudinal study in Bihar, India is following a cohort of asymptomatic cases in households with and without current or past VL case using q-PCR to assess the parasite load thresholds for progression of ALI to VL disease. Another longitudinal study of VL and PKDL patients in Bangladesh is ongoing to estimate relapse rates and risk factors. The role of treating livestock to interrupt transmission is being investigated. A transmission dynamics study and evaluation of the impact of disease elimination is being planned in endemic villages of Bihar in India. Research is now focused on investigating new outbreaks in hitherto non-endemic areas to understand the source and risk factors for the indigenous transmission dynamics. Modelling groups are working towards refining their models to simulate the effects of scenarios that could be a potential threat to elimination efforts. All these and other planned and ongoing research are urgently needed to help national programs to achieve and maintain elimination of VL in the Indian subcontinent.
Conclusion
The burden of ALI is considerable. Longitudinal studies are necessary to identify biomarkers for infectiveness and for progression of ALI to symptomatic VL disease. More research is needed on the immune response to VL and PKDL to identify biomarkers for development of PKDL. Xenodiagnostic studies are necessary to quantify the infectiveness of ALI and PKDL to sandfly relative to symptomatic VL, and their contribution to overall transmission. Even though domestic animals are seen to be infected, there is no evidence of their role in anthroponotic transmission in the Indian subcontinent. Relapse rates need to be monitored for their potential to contribute to transmission and for the emergence of drug-resistant parasites in the context of HIV co-infection. Availability of better data from large well-designed longitudinal studies for modelling would contribute to a better understanding of the impact of treatment and vector control strategies and potential threats to VL elimination in the Indian subcontinent.
Supporting Information
Supplementary information containing unpublished information (Tables A, B, C, J and K), PRISMA statement (Table D), Strategies and keywords used for literature search (Table E), Potential risk of bias in studies (Tables F to I), and Modelling transmission of Leishmania donovani infection in the Indian subcontinent (Table L).
(DOCX)
Acknowledgments
The authors would like to thank M Mamun Huda of the International Center for Diarrheal Diseases Research, Bangladesh, Pradeep Das of Rajendra Memorial Research Institute of Medical Sciences, Patna, India, Shyam Sundar of Kala-azar Medical Research Center, Muzaffarpur, India, Megha Raj Banjara of Public Health and Infectious Disease Research Center, Kathmandu, Nepal, Keshav Kumar Yogi of the WHO country office, Nepal, and Suman Rijal of the Drugs for Neglected Diseases Initiative and the National Kala-azar elimination program managers of Bangladesh, India and Nepal for sharing information for the review. We also thank Graham Medley of the London School of Hygiene and Tropical Medicine and Lloyd Chapman of the University of Warwick for their comments on the review of the transmission modelling studies. Finally, the authors thank Saba Qasmieh of George Washington University for the independent screening of literature for eligibility of the studies included in the review. Disclaimer: SH, AK and PO work for the World Health Organization. The authors alone are responsible for the views expressed in this publication and they do not necessarily represent the decisions, policy or views of the World Health Organization.
Data Availability
All relevant data are within the paper and its Supporting Information file.
Funding Statement
The study was supported by the Special Program for Research and Training in Tropical Diseases, World Health Organization through an APW contract no. 2015/572330 with SH. AK and PO from WHO TDR contributed to the design of the study, data analysis and preparation of the manuscript. SH is a staff member of WHO, Global Influenza Programme; AK is at the Center for Medicine and Society, University of Freiburg, Germany and also a consultant to WHO TDR, TDR programme; PO is a staff member of WHO, TDR programme. WHO/TDR funded SH to conduct the systematic review, (ii) defined the objectives and terms of the review; (iii) funded a workshop of experts where the results were reviewed; (iv) both TDR and the experts participated in the interpretation of results and writing up of the paper.
References
- 1.Chappuis F, Sundar S, Hailu A, Ghalib H, Rijal S, et al. (2007) Visceral leishmaniasis: what are the needs for diagnosis, treatment and control? Nat Rev Microbiol 5: 873–882. [DOI] [PubMed] [Google Scholar]
- 2.Muniaraj M (2014) The lost hope of elimination of Kala-azar (visceral leishmaniasis) by 2010 and cyclic occurrence of its outbreak in India, blame falls on vector control practices or co-infection with human immunodeficiency virus or therapeutic modalities? Trop Parasitol 4: 10–19. 10.4103/2229-5070.129143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization (2005) Regional strategic framework for elimination of kala-azar from the South-East Asia region (2005–2015) New Delhi: WHO Regional Office for South-East Asia. [Google Scholar]
- 4.World Health Organization (2015) Meeting of Ministers of Health of the WHO South-East Asia Region: report of the thirty-second meeting, Dhaka, Bangladesh, 9 Sept 2014.
- 5.Kesari S, Kumar V, Palit A, Kishore K, Das VN, et al. (2009) A localized foci of kala-azar in a village of Chandi PHC (Nalnda district). J Commun Dis 41: 211–214. [PubMed] [Google Scholar]
- 6.Khan AM, Dutta P, Khan SA, Baruah SK, Raja D, et al. (2014) Kala-azar and post-kala-azar dermal leishmaniasis, Assam, India. Emerg Infect Dis 20: 487–489. 10.3201/eid2003.130260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pandey BD, Pun SB, Kaneko O, Pandey K, Hirayama K (2011) Case report: Expansion of visceral leishmaniasis to the western hilly part of Nepal. Am J Trop Med Hyg 84: 107–108. 10.4269/ajtmh.2011.10-0291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Uranw S, Hasker E, Roy L, Meheus F, Das ML, et al. (2013) An outbreak investigation of visceral leishmaniasis among residents of Dharan town, eastern Nepal, evidence for urban transmission of Leishmania donovani. BMC Infect Dis 13: 21 10.1186/1471-2334-13-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization (2015) Kala-Azar elimination programme: report of a WHO consultation of partners, Geneva, Switzerland, 10–11 February 2015: World Health Organization. [Google Scholar]
- 10.Boelaert M, Verdonck K, Menten J, Sunyoto T, van Griensven J, et al. (2014) Rapid tests for the diagnosis of visceral leishmaniasis in patients with suspected disease. Cochrane Database Syst Rev 6: CD009135 10.1002/14651858.CD009135.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maia Z, Lirio M, Mistro S, Mendes CM, Mehta SR, et al. (2012) Comparative study of rK39 Leishmania antigen for serodiagnosis of visceral leishmaniasis: systematic review with meta-analysis. PLoS Negl Trop Dis 6: e1484 10.1371/journal.pntd.0001484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Ruiter CM, van der Veer C, Leeflang MM, Deborggraeve S, Lucas C, et al. (2014) Molecular tools for diagnosis of visceral leishmaniasis: systematic review and meta-analysis of diagnostic test accuracy. J Clin Microbiol 52: 3147–3155. 10.1128/JCM.00372-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adams ER, Versteeg I, Leeflang MM (2013) Systematic Review into Diagnostics for Post-Kala-Azar Dermal Leishmaniasis (PKDL). J Trop Med 2013: 150746 10.1155/2013/150746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kip AE, Balasegaram M, Beijnen JH, Schellens JH, de Vries PJ, et al. (2015) Systematic review of biomarkers to monitor therapeutic response in leishmaniasis. Antimicrob Agents Chemother 59: 1–14. 10.1128/AAC.04298-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Olliaro PL, Guerin PJ, Gerstl S, Haaskjold AA, Rottingen JA, et al. (2005) Treatment options for visceral leishmaniasis: a systematic review of clinical studies done in India, 1980–2004. Lancet Infect Dis 5: 763–774. [DOI] [PubMed] [Google Scholar]
- 16.Gonzalez U, Pinart M, Sinclair D, Firooz A, Enk C, et al. (2015) Vector and reservoir control for preventing leishmaniasis. Cochrane Database Syst Rev 8: CD008736 10.1002/14651858.CD008736.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ostyn B, Vanlerberghe V, Picado A, Dinesh DS, Sundar S, et al. (2008) Vector control by insecticide-treated nets in the fight against visceral leishmaniasis in the Indian subcontinent, what is the evidence? Trop Med Int Health 13: 1073–1085. 10.1111/j.1365-3156.2008.02110.x [DOI] [PubMed] [Google Scholar]
- 18.Ready PD (2014) Epidemiology of visceral leishmaniasis. Clin Epidemiol 6: 147–154. 10.2147/CLEP.S44267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mukhopadhyay D, Dalton JE, Kaye PM, Chatterjee M (2014) Post kala-azar dermal leishmaniasis: an unresolved mystery. Trends Parasitol 30: 65–74. 10.1016/j.pt.2013.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rock KS, le Rutte EA, de Vlas SJ, Adams ER, Medley GF, et al. (2015) Uniting mathematics and biology for control of visceral leishmaniasis. Trends Parasitol 31: 251–259. 10.1016/j.pt.2015.03.007 [DOI] [PubMed] [Google Scholar]
- 21.van Griensven J, Carrillo E, Lopez-Velez R, Lynen L, Moreno J (2014) Leishmaniasis in immunosuppressed individuals. Clin Microbiol Infect 20: 286–299. 10.1111/1469-0691.12556 [DOI] [PubMed] [Google Scholar]
- 22.Singh S (2014) Changing trends in the epidemiology, clinical presentation, and diagnosis of Leishmania-HIV co-infection in India. Int J Infect Dis 29: 103–112. 10.1016/j.ijid.2014.07.011 [DOI] [PubMed] [Google Scholar]
- 23.Burza S, Mahajan R, Sanz MG, Sunyoto T, Kumar R, et al. (2014) HIV and visceral leishmaniasis coinfection in Bihar, India: an underrecognized and underdiagnosed threat against elimination. Clin Infect Dis 59: 552–555. 10.1093/cid/ciu333 [DOI] [PubMed] [Google Scholar]
- 24.Cota GF, de Sousa MR, Rabello A (2011) Predictors of visceral leishmaniasis relapse in HIV-infected patients: a systematic review. PLoS Negl Trop Dis 5: e1153 10.1371/journal.pntd.0001153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Patole S, Burza S, Varghese GM (2014) Multiple relapses of visceral leishmaniasis in a patient with HIV in India: a treatment challenge. Int J Infect Dis 25: 204–206. 10.1016/j.ijid.2014.02.015 [DOI] [PubMed] [Google Scholar]
- 26.Sundar S, More DK, Singh MK, Singh VP, Sharma S, et al. (2000) Failure of pentavalent antimony in visceral leishmaniasis in India: report from the center of the Indian epidemic. Clin Infect Dis 31: 1104–1107. [DOI] [PubMed] [Google Scholar]
- 27.Sundar S (2001) Drug resistance in Indian visceral leishmaniasis. Trop Med Int Health 6: 849–854. [DOI] [PubMed] [Google Scholar]
- 28.Alvar J, Croft S, Olliaro P (2006) Chemotherapy in the treatment and control of leishmaniasis. Adv Parasitol 61: 223–274. [DOI] [PubMed] [Google Scholar]
- 29.Burza S, Nabi E, Mahajan R, Mitra G, Lima MA (2013) One-year follow-up of immunocompetent male patients treated with miltefosine for primary visceral leishmaniasis in Bihar, India. Clin Infect Dis 57: 1363–1364. 10.1093/cid/cit508 [DOI] [PubMed] [Google Scholar]
- 30.Rai K, Cuypers B, Bhattarai NR, Uranw S, Berg M, et al. (2013) Relapse after treatment with miltefosine for visceral leishmaniasis is associated with increased infectivity of the infecting Leishmania donovani strain. MBio 4: e00611–00613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rijal S, Ostyn B, Uranw S, Rai K, Bhattarai NR, et al. (2013) Increasing failure of miltefosine in the treatment of Kala-azar in Nepal and the potential role of parasite drug resistance, reinfection, or noncompliance. Clin Infect Dis 56: 1530–1538. 10.1093/cid/cit102 [DOI] [PubMed] [Google Scholar]
- 32.Burza S, Sinha PK, Mahajan R, Lima MA, Mitra G, et al. (2014) Five-year field results and long-term effectiveness of 20 mg/kg liposomal amphotericin B (Ambisome) for visceral leishmaniasis in Bihar, India. PLoS Negl Trop Dis 8: e2603 10.1371/journal.pntd.0002603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sinha PK, Roddy P, Palma PP, Kociejowski A, Lima MA, et al. (2010) Effectiveness and safety of liposomal amphotericin B for visceral leishmaniasis under routine program conditions in Bihar, India. Am J Trop Med Hyg 83: 357–364. 10.4269/ajtmh.2010.10-0156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stauch A, Duerr HP, Dujardin JC, Vanaerschot M, Sundar S, et al. (2012) Treatment of visceral leishmaniasis: model-based analyses on the spread of antimony-resistant L. donovani in Bihar, India. PLoS Negl Trop Dis 6: e1973 10.1371/journal.pntd.0001973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.World Health Organization ROfS-EA (2016) Regional Strategic Framework for Elimination of Kala-azar from South-East Asia Region (2016–2020)—draft report Delhi, India: World Health Organization. [Google Scholar]
- 36.Bern C, Courtenay O, Alvar J (2010) Of cattle, sand flies and men: a systematic review of risk factor analyses for South Asian visceral leishmaniasis and implications for elimination. PLoS Negl Trop Dis 4: e599 10.1371/journal.pntd.0000599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Open Med 3: e123–130. [PMC free article] [PubMed] [Google Scholar]
- 38.Wells GA, Shea B, O'Connell D, Peterson J, Welch V, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses.
- 39.Cochrane Collaboration (2011) Part 2: General methods for Cochrane reviews. In: Higgins JP, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions.
- 40.Alvar J, Velez ID, Bern C, Herrero M, Desjeux P, et al. (2012) Leishmaniasis worldwide and global estimates of its incidence. PLoS One 7: e35671 10.1371/journal.pone.0035671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hasker E, Kansal S, Malaviya P, Gidwani K, Picado A, et al. (2013) Latent infection with Leishmania donovani in highly endemic villages in Bihar, India. PLoS Negl Trop Dis 7: e2053 10.1371/journal.pntd.0002053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Srivastava P, Gidwani K, Picado A, Van der Auwera G, Tiwary P, et al. (2013) Molecular and serological markers of Leishmania donovani infection in healthy individuals from endemic areas of Bihar, India. Trop Med Int Health 18: 548–554. 10.1111/tmi.12085 [DOI] [PubMed] [Google Scholar]
- 43.Sundar S, Singh RK, Maurya R, Kumar B, Chhabra A, et al. (2006) Serological diagnosis of Indian visceral leishmaniasis: direct agglutination test versus rK39 strip test. Trans R Soc Trop Med Hyg 100: 533–537. [DOI] [PubMed] [Google Scholar]
- 44.Hasker E, Malaviya P, Gidwani K, Picado A, Ostyn B, et al. (2014) Strong association between serological status and probability of progression to clinical visceral leishmaniasis in prospective cohort studies in India and Nepal. PLoS Negl Trop Dis 8: e2657 10.1371/journal.pntd.0002657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gidwani K, Picado A, Rijal S, Singh SP, Roy L, et al. (2011) Serological markers of sand fly exposure to evaluate insecticidal nets against visceral leishmaniasis in India and Nepal: a cluster-randomized trial. PLoS Negl Trop Dis 5: e1296 10.1371/journal.pntd.0001296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sudarshan M, Singh T, Singh AK, Chourasia A, Singh B, et al. (2014) Quantitative PCR in epidemiology for early detection of visceral leishmaniasis cases in India. PLoS Negl Trop Dis 8: e3366 10.1371/journal.pntd.0003366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bern C, Haque R, Chowdhury R, Ali M, Kurkjian KM, et al. (2007) The epidemiology of visceral leishmaniasis and asymptomatic leishmanial infection in a highly endemic Bangladeshi village. Am J Trop Med Hyg 76: 909–914. [PubMed] [Google Scholar]
- 48.Ostyn B, Gidwani K, Khanal B, Picado A, Chappuis F, et al. (2011) Incidence of symptomatic and asymptomatic Leishmania donovani infections in high-endemic foci in India and Nepal: a prospective study. PLoS Negl Trop Dis 5: e1284 10.1371/journal.pntd.0001284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Vallur AC, Duthie MS, Reinhart C, Tutterrow Y, Hamano S, et al. (2014) Biomarkers for intracellular pathogens: establishing tools as vaccine and therapeutic endpoints for visceral leishmaniasis. Clin Microbiol Infect 20: O374–383. 10.1111/1469-0691.12421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gidwani K, Kumar R, Rai M, Sundar S (2009) Longitudinal seroepidemiologic study of visceral leishmaniasis in hyperendemic regions of Bihar, India. Am J Trop Med Hyg 80: 345–346. [PubMed] [Google Scholar]
- 51.Rijal S, Uranw S, Chappuis F, Picado A, Khanal B, et al. (2010) Epidemiology of Leishmania donovani infection in high-transmission foci in Nepal. Trop Med Int Health 15 Suppl 2: 21–28. 10.1111/j.1365-3156.2010.02518.x [DOI] [PubMed] [Google Scholar]
- 52.Picado A, Ostyn B, Singh SP, Uranw S, Hasker E, et al. (2014) Risk factors for visceral leishmaniasis and asymptomatic Leishmania donovani infection in India and Nepal. PLoS One 9: e87641 10.1371/journal.pone.0087641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bhattarai NR, Van der Auwera G, Rijal S, Picado A, Speybroeck N, et al. (2010) Domestic animals and epidemiology of visceral leishmaniasis, Nepal. Emerg Infect Dis 16: 231–237. 10.3201/eid1602.090623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schenkel K, Rijal S, Koirala S, Koirala S, Vanlerberghe V, et al. (2006) Visceral leishmaniasis in southeastern Nepal: a cross-sectional survey on Leishmania donovani infection and its risk factors. Trop Med Int Health 11: 1792–1799. [DOI] [PubMed] [Google Scholar]
- 55.Saha S, Ramachandran R, Hutin YJ, Gupte MD (2009) Visceral leishmaniasis is preventable in a highly endemic village in West Bengal, India. Trans R Soc Trop Med Hyg 103: 737–742. 10.1016/j.trstmh.2008.10.006 [DOI] [PubMed] [Google Scholar]
- 56.Singh SP, Picado A, Boelaert M, Gidwani K, Andersen EW, et al. (2010) The epidemiology of Leishmania donovani infection in high transmission foci in India. Trop Med Int Health 15 Suppl 2: 12–20. 10.1111/j.1365-3156.2010.02519.x [DOI] [PubMed] [Google Scholar]
- 57.Khanal B, Picado A, Bhattarai NR, Van Der Auwera G, Das ML, et al. (2010) Spatial analysis of Leishmania donovani exposure in humans and domestic animals in a recent kala azar focus in Nepal. Parasitology 137: 1597–1603. 10.1017/S0031182010000521 [DOI] [PubMed] [Google Scholar]
- 58.Das VN, Siddiqui NA, Verma RB, Topno RK, Singh D, et al. (2011) Asymptomatic infection of visceral leishmaniasis in hyperendemic areas of Vaishali district, Bihar, India: a challenge to kala-azar elimination programmes. Trans R Soc Trop Med Hyg 105: 661–666. 10.1016/j.trstmh.2011.08.005 [DOI] [PubMed] [Google Scholar]
- 59.Goswami RP, Bairagi B, Kundu PK (2003) K39 strip test—easy, reliable and cost-effective field diagnosis for visceral leishmaniasis in India. J Assoc Physicians India 51: 759–761. [PubMed] [Google Scholar]
- 60.Huda MM, Rudra S, Ghosh D, Bhaskar KR, Chowdhury R, et al. (2013) Low prevalence of Leishmania donovani infection among the blood donors in kala-azar endemic areas of Bangladesh. BMC Infect Dis 13: 62 10.1186/1471-2334-13-62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Singh DP, Goyal RK, Singh RK, Sundar S, Mohapatra TM (2010) In search of an ideal test for diagnosis and prognosis of kala-azar. J Health Popul Nutr 28: 281–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Topno RK, Das VN, Ranjan A, Pandey K, Singh D, et al. (2010) Asymptomatic infection with visceral leishmaniasis in a disease-endemic area in bihar, India. Am J Trop Med Hyg 83: 502–506. 10.4269/ajtmh.2010.09-0345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Khanal B, Rijal S, Ostyn B, Picado A, Gidwani K, et al. (2010) Serological markers for leishmania donovani infection in Nepal: Agreement between direct agglutination test and rK39 ELISA. Trop Med Int Health 15: 1390–1394. [DOI] [PubMed] [Google Scholar]
- 64.Kumar R, Pai K, Pathak K, Sundar S (2001) Enzyme-linked immunosorbent assay for recombinant K39 antigen in diagnosis and prognosis of Indian visceral leishmaniasis. Clin Diagn Lab Immunol 8: 1220–1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bhattarai NR, Van der Auwera G, Khanal B, De Doncker S, Rijal S, et al. (2009) PCR and direct agglutination as Leishmania infection markers among healthy Nepalese subjects living in areas endemic for Kala-Azar. Trop Med Int Health 14: 404–411. 10.1111/j.1365-3156.2009.02242.x [DOI] [PubMed] [Google Scholar]
- 66.Bimal S, Das VN, Sinha PK, Gupta AK, Verma N, et al. (2005) Usefulness of the direct agglutination test in the early detection of subclinical Leishmania donovani infection: a community-based study. Ann Trop Med Parasitol 99: 743–749. [DOI] [PubMed] [Google Scholar]
- 67.Chowdhury MS, el Harith A, al Massum A, al Karim E, al Rahman A (1993) Prevalence of agglutinating anti-Leishmania antibodies in two multi-thousand Bengoli communities. Parasitol Res 79: 444–450. [DOI] [PubMed] [Google Scholar]
- 68.Koirala S, Karki P, Das ML, Parija SC, Karki BM (2004) Epidemiological study of kala-azar by direct agglutination test in two rural communities of eastern Nepal. Trop Med Int Health 9: 533–537. [DOI] [PubMed] [Google Scholar]
- 69.Sinha PK, Bimal S, Pandey K, Singh SK, Ranjan A, et al. (2008) A community-based, comparative evaluation of direct agglutination and rK39 strip tests in the early detection of subclinical Leishmania donovani infection. Ann Trop Med Parasitol 102: 119–125. 10.1179/136485908X252278 [DOI] [PubMed] [Google Scholar]
- 70.Kumar R, Pai K, Kumar P, Pandey HP, Sundar S (2006) Sero-epidemiological study of kala-azar in a village of Varanasi district, India. Trop Med Int Health 11: 41–48. [DOI] [PubMed] [Google Scholar]
- 71.Ostyn B, Uranw S, Bhattarai NR, Das ML, Rai K, et al. (2015) Transmission of Leishmania donovani in the Hills of Eastern Nepal, an Outbreak Investigation in Okhaldhunga and Bhojpur Districts. PLoS Negl Trop Dis 9: e0003966 10.1371/journal.pntd.0003966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Picado A, Singh SP, Rijal S, Sundar S, Ostyn B, et al. (2010) Longlasting insecticidal nets for prevention of Leishmania donovani infection in India and Nepal: paired cluster randomised trial. BMJ 341: c6760 10.1136/bmj.c6760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Nandy A, Neogy AB, Chowdhury AB (1987) Leishmanin test survey in an endemic village of Indian kala-azar near Calcutta. Ann Trop Med Parasitol 81: 693–699. [DOI] [PubMed] [Google Scholar]
- 74.Bern C, Amann J, Haque R, Chowdhury R, Ali M, et al. (2006) Loss of leishmanin skin test antigen sensitivity and potency in a longitudinal study of visceral leishmaniasis in Bangladesh. Am J Trop Med Hyg 75: 744–748. [PubMed] [Google Scholar]
- 75.Salotra P, Sreenivas G, Pogue GP, Lee N, Nakhasi HL, et al. (2001) Development of a species-specific PCR assay for detection of Leishmania donovani in clinical samples from patients with kala-azar and post-kala-azar dermal leishmaniasis. J Clin Microbiol 39: 849–854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sudarshan M, Sundar S (2014) Parasite load estimation by qPCR differentiates between asymptomatic and symptomatic infection in Indian visceral leishmaniasis. Diagn Microbiol Infect Dis 80: 40–42. 10.1016/j.diagmicrobio.2014.01.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Singh S, Kumari V, Singh N (2002) Predicting kala-azar disease manifestations in asymptomatic patients with latent Leishmania donovani infection by detection of antibody against recombinant K39 antigen. Clin Diagn Lab Immunol 9: 568–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Saran R, Gupta AK, Sharma MC (1992) Evidence of Leishmania donovani infection in household members residing with visceral leishmaniasis patients. J Commun Dis 24: 242–244. [PubMed] [Google Scholar]
- 79.Islam MZ, Itoh M, Ul Islam MA, Saifuddin Ekram AR, Rahman MA, et al. (2012) ELISA with recombinant rKRP42 antigen using urine samples: a tool for predicting clinical visceral leishmaniasis cases and its outbreak. Am J Trop Med Hyg 87: 658–662. 10.4269/ajtmh.2012.12-0168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chapman LA, Dyson L, Courtenay O, Chowdhury R, Bern C, et al. (2015) Quantification of the natural history of visceral leishmaniasis and consequences for control. Parasit Vectors 8: 521 10.1186/s13071-015-1136-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ansari NA, Sharma P, Salotra P (2007) Circulating nitric oxide and C-reactive protein levels in Indian kala azar patients: correlation with clinical outcome. Clin Immunol 122: 343–348. [DOI] [PubMed] [Google Scholar]
- 82.Mukhopadhyay AK, Mishra RN (1991) Development of Leishmania donovani in Phlebotomus argentipes & Ph. papatasi fed on kala-azar patients in Bihar. Indian J Med Res 93: 152–154. [PubMed] [Google Scholar]
- 83.Le Rutte EA, Coffeng LE, Bontje DM, Hasker EC, Ruiz Postigo JA, et al. (2016) Feasibility of eliminating visceral leishmaniasis from the Indian subcontinent: explorations with a set of deterministic age-structured transmission models. Parasit Vectors 9: 24 10.1186/s13071-016-1292-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Stauch A, Sarkar RR, Picado A, Ostyn B, Sundar S, et al. (2011) Visceral leishmaniasis in the Indian subcontinent: modelling epidemiology and control. PLoS Negl Trop Dis 5: e1405 10.1371/journal.pntd.0001405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Thakur CP, Kumar K (1992) Post kala-azar dermal leishmaniasis: a neglected aspect of kala-azar control programmes. Ann Trop Med Parasitol 86: 355–359. [DOI] [PubMed] [Google Scholar]
- 86.World Health Organization (2010) Indicators for monitoring and evaluation of the kala-azar elimination programme Kala-azar elimination in Bangladesh, India and Nepal. Geneva: World Health Organization. [Google Scholar]
- 87.Mondal D, Nasrin KN, Huda MM, Kabir M, Hossain MS, et al. (2010) Enhanced case detection and improved diagnosis of PKDL in a Kala-azar-endemic area of Bangladesh. PLoS Negl Trop Dis 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Singh RP, Picado A, Alam S, Hasker E, Singh SP, et al. (2012) Post-kala-azar dermal leishmaniasis (PKDL) in visceral leishmaniasis-endemic communities in Bihar, India. Trop Med Int Health. [DOI] [PubMed] [Google Scholar]
- 89.Rai RN, Kumar M, Srivastava A, Joshi RD, Asthana AK, et al. (1989) Clinico-epidemiological profiles of post-kala-azar dermal leishmaniasis in Varanasi. J Commun Dis 21: 214–217. [PubMed] [Google Scholar]
- 90.Rahman KM, Islam S, Rahman MW, Kenah E, Ghalib CM, et al. (2010) Increasing incidence of post-kala-azar dermal leishmaniasis in a population-based study in Bangladesh. Clin Infect Dis 50: 73–76. 10.1086/648727 [DOI] [PubMed] [Google Scholar]
- 91.Islam S, Kenah E, Bhuiyan MA, Rahman KM, Goodhew B, et al. (2013) Clinical and immunological aspects of post-kala-azar dermal leishmaniasis in Bangladesh. Am J Trop Med Hyg 89: 345–353. 10.4269/ajtmh.12-0711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ganguly S, Saha P, Chatterjee M, Roy S, Ghosh TK, et al. (2015) PKDL—A Silent Parasite Pool for Transmission of Leishmaniasis in Kala-azar Endemic Areas of Malda District, West Bengal, India. PLoS Negl Trop Dis 9: e0004138 10.1371/journal.pntd.0004138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Das VN, Ranjan A, Pandey K, Singh D, Verma N, et al. (2012) Clinical epidemiologic profile of a cohort of post-kala-azar dermal leishmaniasis patients in Bihar, India. Am J Trop Med Hyg 86: 959–961. 10.4269/ajtmh.2012.11-0467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Garg VK, Agrawal S, Rani S, Joshi A, Agarwalla A, et al. (2001) Post-kala-azar dermal leishmaniasis in Nepal. Int J Dermatol 40: 179–184. [DOI] [PubMed] [Google Scholar]
- 95.Burza S, Sinha PK, Mahajan R, Sanz MG, Lima MA, et al. (2014) Post Kala-Azar dermal leishmaniasis following treatment with 20 mg/kg liposomal amphotericin B (Ambisome) for primary visceral leishmaniasis in Bihar, India. PLoS Negl Trop Dis 8: e2611 10.1371/journal.pntd.0002611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Uranw S, Ostyn B, Rijal A, Devkota S, Khanal B, et al. (2011) Post-kala-azar dermal leishmaniasis in Nepal: a retrospective cohort study (2000–2010). PLoS Negl Trop Dis 5: e1433 10.1371/journal.pntd.0001433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Salotra P, Sreenivas G, Nasim AA, Subba Raju BV, Ramesh V (2002) Evaluation of enzyme-linked immunosorbent assay for diagnosis of post-kala-azar dermal leishmaniasis with crude or recombinant k39 antigen. Clin Diagn Lab Immunol 9: 370–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Das ML, Deb M, Karki BM, Sarif M, Khanal B, et al. (2007) Use of rK39 for diagnosis of post kala-azar dermal leishmaniasis in Nepal. Southeast Asian J Trop Med Public Health 38: 619–625. [PubMed] [Google Scholar]
- 99.Singh R, Subba Raju BV, Jain RK, Salotra P (2005) Potential of direct agglutination test based on promastigote and amastigote antigens for serodiagnosis of post-kala-azar dermal leishmaniasis. Clin Diagn Lab Immunol 12: 1191–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Ramesh V, Mukherjee A (1995) Post-kala-azar dermal leishmaniasis. Int J Dermatol 34: 85–91. [DOI] [PubMed] [Google Scholar]
- 101.Addy M, Nandy A (1992) Ten years of kala-azar in west Bengal, Part I. Did post-kala-azar dermal leishmaniasis initiate the outbreak in 24-Parganas? Bull World Health Organ 70: 341–346. [PMC free article] [PubMed] [Google Scholar]
- 102.Dinesh DS, Kar SK, Kishore K, Palit A, Verma N, et al. (2000) Screening sandflies for natural infection with Leishmania donovani, using a non-radioactive probe based on the total DNA of the parasite. Ann Trop Med Parasitol 94: 447–451. [DOI] [PubMed] [Google Scholar]
- 103.Mathur P, Samantaray JC, Vajpayee M, Samanta P (2006) Visceral leishmaniasis/human immunodeficiency virus co-infection in India: the focus of two epidemics. J Med Microbiol 55: 919–922. [DOI] [PubMed] [Google Scholar]
- 104.Bern C, Hightower AW, Chowdhury R, Ali M, Amann J, et al. (2005) Risk factors for kala-azar in Bangladesh. Emerg Infect Dis 11: 655–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Maurya R, Singh RK, Kumar B, Salotra P, Rai M, et al. (2005) Evaluation of PCR for diagnosis of Indian kala-azar and assessment of cure. J Clin Microbiol 43: 3038–3041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sen Gupta PC, Mukherjee AM (1968) Recurrence of kala-azar associated with post-kala-azar dermal leishmaniasis. J Indian Med Assoc 50: 1–5 passim. [PubMed] [Google Scholar]
- 107.Sinha PK, van Griensven J, Pandey K, Kumar N, Verma N, et al. (2011) Liposomal amphotericin B for visceral leishmaniasis in human immunodeficiency virus-coinfected patients: 2-year treatment outcomes in Bihar, India. Clin Infect Dis 53: e91–98. 10.1093/cid/cir521 [DOI] [PubMed] [Google Scholar]
- 108.Burza S, Sinha PK, Mahajan R, Lima MA, Mitra G, et al. (2014) Risk factors for visceral leishmaniasis relapse in immunocompetent patients following treatment with 20 mg/kg liposomal amphotericin B (Ambisome) in Bihar, India. PLoS Negl Trop Dis 8: e2536 10.1371/journal.pntd.0002536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ostyn B, Hasker E, Dorlo TP, Rijal S, Sundar S, et al. (2014) Failure of miltefosine treatment for visceral leishmaniasis in children and men in South-East Asia. PLoS One 9: e100220 10.1371/journal.pone.0100220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Burza S, Mahajan R, Sinha PK, van Griensven J, Pandey K, et al. (2014) Visceral leishmaniasis and HIV co-infection in Bihar, India: long-term effectiveness and treatment outcomes with liposomal amphotericin B (AmBisome). PLoS Negl Trop Dis 8: e3053 10.1371/journal.pntd.0003053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Bhattacharyya T, Ayandeh A, Falconar AK, Sundar S, El-Safi S, et al. (2014) IgG1 as a potential biomarker of post-chemotherapeutic relapse in visceral leishmaniasis, and adaptation to a rapid diagnostic test. PLoS Negl Trop Dis 8: e3273 10.1371/journal.pntd.0003273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Bhattacharya SK, Jha TK, Sundar S, Thakur CP, Engel J, et al. (2004) Efficacy and tolerability of miltefosine for childhood visceral leishmaniasis in India. Clin Infect Dis 38: 217–221. [DOI] [PubMed] [Google Scholar]
- 113.Bhattacharya SK, Sinha PK, Sundar S, Thakur CP, Jha TK, et al. (2007) Phase 4 trial of miltefosine for the treatment of Indian visceral leishmaniasis. J Infect Dis 196: 591–598. [DOI] [PubMed] [Google Scholar]
- 114.Jha TK, Sundar S, Thakur CP, Bachmann P, Karbwang J, et al. (1999) Miltefosine, an oral agent, for the treatment of Indian visceral leishmaniasis. N Engl J Med 341: 1795–1800. [DOI] [PubMed] [Google Scholar]
- 115.Singh UK, Prasad R, Mishra OP, Jayswal BP (2006) Miltefosine in children with visceral leishmaniasis: a prospective, multicentric, cross-sectional study. Indian J Pediatr 73: 1077–1080. [DOI] [PubMed] [Google Scholar]
- 116.Sundar S, Jha TK, Thakur CP, Engel J, Sindermann H, et al. (2002) Oral miltefosine for Indian visceral leishmaniasis. N Engl J Med 347: 1739–1746. [DOI] [PubMed] [Google Scholar]
- 117.Sundar S, Jha TK, Sindermann H, Junge K, Bachmann P, et al. (2003) Oral miltefosine treatment in children with mild to moderate Indian visceral leishmaniasis. Pediatr Infect Dis J 22: 434–438. [DOI] [PubMed] [Google Scholar]
- 118.Sundar S, Singh A, Rai M, Prajapati VK, Singh AK, et al. (2012) Efficacy of miltefosine in the treatment of visceral leishmaniasis in India after a decade of use. Clin Infect Dis 55: 543–550. 10.1093/cid/cis474 [DOI] [PubMed] [Google Scholar]
- 119.Ramesh V, Katara GK, Verma S, Salotra P (2011) Miltefosine as an effective choice in the treatment of post-kala-azar dermal leishmaniasis. Br J Dermatol 165: 411–414. 10.1111/j.1365-2133.2011.10402.x [DOI] [PubMed] [Google Scholar]
- 120.Sundar S, Singh A, Chakravarty J, Rai M (2015) Efficacy and safety of miltefosine in treatment of post-kala-azar dermal leishmaniasis. ScientificWorldJournal 2015: 414378 10.1155/2015/414378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Ghosh S, Das NK, Mukherjee S, Mukhopadhyay D, Barbhuiya JN, et al. (2015) Inadequacy of 12-Week Miltefosine Treatment for Indian Post-Kala-Azar Dermal Leishmaniasis. Am J Trop Med Hyg 93: 767–769. 10.4269/ajtmh.14-0721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Bhandari V, Kulshrestha A, Deep DK, Stark O, Prajapati VK, et al. (2012) Drug susceptibility in Leishmania isolates following miltefosine treatment in cases of visceral leishmaniasis and post kala-azar dermal leishmaniasis. PLoS Negl Trop Dis 6: e1657 10.1371/journal.pntd.0001657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Nandy A, Addy M, Maji AK, Guha SK, Banerjee D, et al. (1998) Recurrence of kala-azar after PKDL: role of co-factors. Trop Med Int Health 3: 76–78. [DOI] [PubMed] [Google Scholar]
- 124.Mubayi A, Castillo-Chavez C, Chowell G, Kribs-Zaleta C, Ali Siddiqui N, et al. (2010) Transmission dynamics and underreporting of Kala-azar in the Indian state of Bihar. J Theor Biol 262: 177–185. 10.1016/j.jtbi.2009.09.012 [DOI] [PubMed] [Google Scholar]
- 125.Stauch A, Duerr HP, Picado A, Ostyn B, Sundar S, et al. (2014) Model-based investigations of different vector-related intervention strategies to eliminate visceral leishmaniasis on the Indian subcontinent. PLoS Negl Trop Dis 8: e2810 10.1371/journal.pntd.0002810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Medley GF, Hollingsworth TD, Olliaro PL, Adams ER (2015) Health-seeking behaviour, diagnostics and transmission dynamics in the control of visceral leishmaniasis in the Indian subcontinent. Nature 528: S102–108. 10.1038/nature16042 [DOI] [PubMed] [Google Scholar]
- 127.Dye C, Wolpert DM (1988) Earthquakes, influenza and cycles of Indian kala-azar. Trans R Soc Trop Med Hyg 82: 843–850. [DOI] [PubMed] [Google Scholar]
- 128.Singh SP, Reddy DC, Rai M, Sundar S (2006) Serious underreporting of visceral leishmaniasis through passive case reporting in Bihar, India. Trop Med Int Health 11: 899–905. [DOI] [PubMed] [Google Scholar]
- 129.Singh VP, Ranjan A, Topno RK, Verma RB, Siddique NA, et al. (2010) Estimation of under-reporting of visceral leishmaniasis cases in Bihar, India. Am J Trop Med Hyg 82: 9–11. 10.4269/ajtmh.2010.09-0235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Boettcher JP, Siwakoti Y, Milojkovic A, Siddiqui NA, Gurung CK, et al. (2015) Visceral leishmaniasis diagnosis and reporting delays as an obstacle to timely response actions in Nepal and India. BMC Infect Dis 15: 43 10.1186/s12879-015-0767-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Hati AK, Sur S, De N, Dwivedi HN, Bhattacharyya J, et al. (1991) Longitudinal study on distribution of Phlebotomus argentipes sandflies at different heights in cattleshed. Indian J Med Res 93: 388–390. [PubMed] [Google Scholar]
- 132.Sacks DL, Perkins PV (1985) Development of infective stage Leishmania promastigotes within phlebotomine sand flies. Am J Trop Med Hyg 34: 456–459. [DOI] [PubMed] [Google Scholar]
- 133.Tiwary P, Kumar D, Mishra M, Singh RP, Rai M, et al. (2013) Seasonal variation in the prevalence of sand flies infected with Leishmania donovani. PLoS One 8: e61370 10.1371/journal.pone.0061370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Tiwary P, Kumar D, Singh RP, Rai M, Sundar S (2012) Prevalence of sand flies and Leishmania donovani infection in a natural population of female Phlebotomus argentipes in Bihar State, India. Vector Borne Zoonotic Dis 12: 467–472. 10.1089/vbz.2011.0808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Picado A, Das ML, Kumar V, Kesari S, Dinesh DS, et al. (2010) Effect of village-wide use of long-lasting insecticidal nets on visceral Leishmaniasis vectors in India and Nepal: a cluster randomized trial. PLoS Negl Trop Dis 4: e587 10.1371/journal.pntd.0000587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Joshi AB, Das ML, Akhter S, Chowdhury R, Mondal D, et al. (2009) Chemical and environmental vector control as a contribution to the elimination of visceral leishmaniasis on the Indian subcontinent: cluster randomized controlled trials in Bangladesh, India and Nepal. BMC Med 7: 54 10.1186/1741-7015-7-54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Poche D, Garlapati R, Ingenloff K, Remmers J, Poche R (2011) Bionomics of phlebotomine sand flies from three villages in Bihar, India. J Vector Ecol 36 Suppl 1: S106–117. [DOI] [PubMed] [Google Scholar]
- 138.Rao JS, Sharma SK, Bhattacharya D, Saxena NB (2001) Sandfly survey in Nainital and Almora districts of Uttaranchal with particular reference to Phlebotomus argentipes, vector of kala-azar. J Commun Dis 33: 7–11. [PubMed] [Google Scholar]
- 139.Hati AK, Nandy A, Mallik KK, Moitra SB, Choudhury AB (1984) A report on kala-azar cases in Malda district during 1980–81. J Indian Med Assoc 82: 1–4. [PubMed] [Google Scholar]
- 140.Joshi AB, Banjara MR, Pokhrel S, Jimba M, Singhasivanon P, et al. (2006) Elimination of visceral leishmaniasis in Nepal: pipe-dreams and possibilities. Kathmandu Univ Med J (KUMJ) 4: 488–496. [PubMed] [Google Scholar]
- 141.Mondal D, Chowdhury R, Huda MM, Maheswary NP, Akther S, et al. (2010) Insecticide-treated bed nets in rural Bangladesh: their potential role in the visceral leishmaniasis elimination programme. Trop Med Int Health 15: 1382–1389. 10.1111/j.1365-3156.2010.02635.x [DOI] [PubMed] [Google Scholar]
- 142.Clements MF, Gidwani K, Kumar R, Hostomska J, Dinesh DS, et al. (2010) Measurement of recent exposure to Phlebotomus argentipes, the vector of Indian visceral Leishmaniasis, by using human antibody responses to sand fly saliva. Am J Trop Med Hyg 82: 801–807. 10.4269/ajtmh.2010.09-0336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Kumar V, Kishore K, Palit A, Keshari S, Sharma MC, et al. (2001) Vectorial efficacy of Phlebotomus argentipes in Kala-azar endemic foci of Bihar (India) under natural and artificial conditions. J Commun Dis 33: 102–109. [PubMed] [Google Scholar]
- 144.Swaminath CS, Shortt HE, Anderson LA (1942) Transmission of Indian kala-azar to man by the bites of Phlebotomus argentipes, ann and brun. 1942. Indian J Med Res 123: 473–477. [PubMed] [Google Scholar]
- 145.Mukhopadhyay AK, Chakravarty AK (1987) Bloodmeal preference of Phlebotomus argentipes & Ph. papatasi of north Bihar, India. Indian J Med Res 86: 475–480. [PubMed] [Google Scholar]
- 146.Bhunia GS, Kesari S, Chatterjee N, Mandal R, Kumar V, et al. (2012) Seasonal relationship between normalized difference vegetation index and abundance of the Phlebotomus kala-azar vector in an endemic focus in Bihar, India. Geospat Health 7: 51–62. [DOI] [PubMed] [Google Scholar]
- 147.Chowdhury R, Dotson E, Blackstock AJ, McClintock S, Maheswary NP, et al. (2011) Comparison of insecticide-treated nets and indoor residual spraying to control the vector of visceral leishmaniasis in Mymensingh District, Bangladesh. Am J Trop Med Hyg 84: 662–667. 10.4269/ajtmh.2011.10-0682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Kesari S, Bhunia GS, Chatterjee N, Kumar V, Mandal R, et al. (2013) Appraisal of Phlebotomus argentipes habitat suitability using a remotely sensed index in the kala-azar endemic focus of Bihar, India. Mem Inst Oswaldo Cruz 108: 197–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Rao JS, Rahman SJ, Singh J, Singh SK (1992) Kala-azar in Ballia district, Uttar Pradesh. J Commun Dis 24: 116–120. [PubMed] [Google Scholar]
- 150.Pandya AP (1983) Geographical distribution & density of phlebotominae sandflies in Surat district, Gujarat. Indian J Med Res 77: 817–823. [PubMed] [Google Scholar]
- 151.Kesari S, Bhunia GS, Kumar V, Jeyaram A, Ranjan A, et al. (2011) A comparative evaluation of end-emic and non-endemic region of visceral leishmaniasis (Kala-azar) in India with ground survey and space technology. Mem Inst Oswaldo Cruz 106: 515–523. [DOI] [PubMed] [Google Scholar]
- 152.Bhunia GS, Kesari S, Chatterjee N, Kumar V, Das P (2012) Localization of kala-azar in the endemic region of Bihar, India based on land use/land cover assessment at different scales. Geospat Health 6: 177–193. [DOI] [PubMed] [Google Scholar]
- 153.Coleman M, Foster GM, Deb R, Pratap Singh R, Ismail HM, et al. (2015) DDT-based indoor residual spraying suboptimal for visceral leishmaniasis elimination in India. Proc Natl Acad Sci U S A 112: 8573–8578. 10.1073/pnas.1507782112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Das ML, Roy L, Rijal S, Paudel IS, Picado A, et al. (2010) Comparative study of kala-azar vector control measures in eastern Nepal. Acta Trop 113: 162–166. 10.1016/j.actatropica.2009.10.012 [DOI] [PubMed] [Google Scholar]
- 155.Mukhopadhyay AK, Hati AK, Chakraborty S, Saxena NB (1996) Effect of DDT on Phlebotomus sandflies in Kala-Azar endemic foci in West Bengal. J Commun Dis 28: 171–175. [PubMed] [Google Scholar]
- 156.Kumar V, Kesari SK, Sinha NK, Palit A, Ranjan A, et al. (1995) Field trial of an ecological approach for the control of Phlebotomus argentipes using mud & lime plaster. Indian J Med Res 101: 154–156. [PubMed] [Google Scholar]
- 157.Miller E, Warburg A, Novikov I, Hailu A, Volf P, et al. (2014) Quantifying the contribution of hosts with different parasite concentrations to the transmission of visceral leishmaniasis in Ethiopia. PLoS Negl Trop Dis 8: e3288 10.1371/journal.pntd.0003288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Molina R, Canavate C, Cercenado E, Laguna F, Lopez-Velez R, et al. (1994) Indirect xenodiagnosis of visceral leishmaniasis in 10 HIV-infected patients using colonized Phlebotomus perniciosus. AIDS 8: 277–279. [DOI] [PubMed] [Google Scholar]
- 159.Seblova V, Volfova V, Dvorak V, Pruzinova K, Votypka J, et al. (2013) Phlebotomus orientalis sand flies from two geographically distant Ethiopian localities: biology, genetic analyses and susceptibility to Leishmania donovani. PLoS Negl Trop Dis 7: e2187 10.1371/journal.pntd.0002187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Courtenay O, Quinnell RJ, Garcez LM, Shaw JJ, Dye C (2002) Infectiousness in a cohort of brazilian dogs: why culling fails to control visceral leishmaniasis in areas of high transmission. J Infect Dis 186: 1314–1320. [DOI] [PubMed] [Google Scholar]
- 161.Costa CH, Gomes RB, Silva MR, Garcez LM, Ramos PK, et al. (2000) Competence of the human host as a reservoir for Leishmania chagasi. J Infect Dis 182: 997–1000. [DOI] [PubMed] [Google Scholar]
- 162.Costa CH, Stewart JM, Gomes RB, Garcez LM, Ramos PK, et al. (2002) Asymptomatic human carriers of Leishmania chagasi. Am J Trop Med Hyg 66: 334–337. [DOI] [PubMed] [Google Scholar]
- 163.Yangzom T, Cruz I, Bern C, Argaw D, den Boer M, et al. (2012) Endemic transmission of visceral leishmaniasis in Bhutan. Am J Trop Med Hyg 87: 1028–1037. 10.4269/ajtmh.2012.12-0211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Ganguly S, Das NK, Barbhuiya JN, Chatterjee M (2010) Post-kala-azar dermal leishmaniasis—an overview. Int J Dermatol 49: 921–931. 10.1111/j.1365-4632.2010.04558.x [DOI] [PubMed] [Google Scholar]
- 165.Zijlstra EE, Musa AM, Khalil EA, el-Hassan IM, el-Hassan AM (2003) Post-kala-azar dermal leishmaniasis. Lancet Infect Dis 3: 87–98. [DOI] [PubMed] [Google Scholar]
- 166.Ramesh V, Singh R, Salotra P (2007) Short communication: post-kala-azar dermal leishmaniasis—an appraisal. Trop Med Int Health 12: 848–851. [DOI] [PubMed] [Google Scholar]
- 167.Ghosh KN, Bhattacharya A, Ghosh TN (1990) Blood meal analysis of Phlebotomus argentipes in eight districts of West Bengal. J Commun Dis 22: 67–71. [PubMed] [Google Scholar]
- 168.Palit A, Bhattacharya SK, Kundu SN (2005) Host preference of Phlebotomus argentipes and Phlebotomus papatasi in different biotopes of West Bengal, India. Int J Environ Health Res 15: 449–454. [DOI] [PubMed] [Google Scholar]
- 169.Ritmeijer K, Dejenie A, Assefa Y, Hundie TB, Mesure J, et al. (2006) A comparison of miltefosine and sodium stibogluconate for treatment of visceral leishmaniasis in an Ethiopian population with high prevalence of HIV infection. Clin Infect Dis 43: 357–364. [DOI] [PubMed] [Google Scholar]
- 170.Dey A, Singh S (2006) Transfusion transmitted leishmaniasis: a case report and review of literature. Indian J Med Microbiol 24: 165–170. [PubMed] [Google Scholar]
- 171.Basset D, Faraut F, Marty P, Dereure J, Rosenthal E, et al. (2005) Visceral leishmaniasis in organ transplant recipients: 11 new cases and a review of the literature. Microbes Infect 7: 1370–1375. [DOI] [PubMed] [Google Scholar]
- 172.Antinori S, Cascio A, Parravicini C, Bianchi R, Corbellino M (2008) Leishmaniasis among organ transplant recipients. Lancet Infect Dis 8: 191–199. 10.1016/S1473-3099(08)70043-4 [DOI] [PubMed] [Google Scholar]
- 173.Herwaldt BL (2001) Laboratory-acquired parasitic infections from accidental exposures. Clin Microbiol Rev 14: 659–688, table of contents. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Eltoum IA, Zijlstra EE, Ali MS, Ghalib HW, Satti MM, et al. (1992) Congenital kala-azar and leishmaniasis in the placenta. Am J Trop Med Hyg 46: 57–62. [DOI] [PubMed] [Google Scholar]
- 175.Cruz I, Morales MA, Noguer I, Rodriguez A, Alvar J (2002) Leishmania in discarded syringes from intravenous drug users. Lancet 359: 1124–1125. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary information containing unpublished information (Tables A, B, C, J and K), PRISMA statement (Table D), Strategies and keywords used for literature search (Table E), Potential risk of bias in studies (Tables F to I), and Modelling transmission of Leishmania donovani infection in the Indian subcontinent (Table L).
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information file.


