Abstract
The management of high-grade gliomas (hggs) is complex and ever-evolving. The standard of care for the treatment of hggs consists of surgery, chemotherapy, and radiotherapy. However, treatment options are influenced by multiple factors such as patient age and performance status, extent of tumour resection, biomarker profile, and tumour histology and grade. Follow-up cranial magnetic resonance imaging (mri) to differentiate treatment response from treatment effect can be challenging and affects clinical decision-making. An assortment of advanced radiologic techniques—including perfusion imaging with dynamic susceptibility contrast mri, dynamic contrast-enhanced mri, diffusion-weighted imaging, proton spectroscopy, mri subtraction imaging, and amino acid radiotracer imaging—can now incorporate novel physiologic data, providing new methods to help characterize tumour progression, pseudoprogression, and pseudoresponse. In the present review, we provide an overview of current treatment options for hgg and summarize recent advances and challenges in imaging technology.
Keywords: Gliomas, pseudoprogression, pseudoresponse, perfusion, diffusion
BACKGROUND
Gliomas are malignant tumours derived from glial cells or their precursors; in the United States, they constitute 80% of all primary intra-axial malignancies of the central nervous system and 28% of all cancers involving the central nervous system1. The current World Health Organization histologic classification system uses histopathologic changes of cellular atypia, mitotic activity, endothelial cell proliferation, and necrosis to classify gliomas as “low grade” (grades i and ii) and “high grade” (grades iii and iv)2. Common glioma subtypes include astrocytoma (including glioblastoma), oligodendroglioma, and oligoastrocytoma (or mixed glioma)3.
Predictive and Prognostic Factors
Important factors that predict positive outcomes are oligodendroglial cell line, extent of surgical resection, and age less than 50 years4. Furthermore, tumours with mgmt (O-6-methylguanine-dna methyltransferase) promoter methylation, chromosomal 1p and 19q co-deletion (seen in oligodendroglioma cell lineage), or isocitrate dehydrogenase 1 and 2 mutations have been shown to have more favourable outcomes5–8. The presence of mgmt promoter methylation and 1p/19q co-deletion can also affect treatment decisions, because either of those mutations predicts a better outcome in patients treated with alkylating chemotherapy5,9. In the case of mgmt promoter methylation, inferior outcomes have been reported in elderly patients (defined as >70 years of age) when such patients are treated with conventionally fractionated radiotherapy alone compared with chemotherapy8.
MANAGEMENT STRATEGIES
Maximal safe surgical resection is widely accepted as the standard of care for high-grade gliomas, although existing evidence is retrospective in nature10,11. Currently accepted adjuvant management, which is based on a trial by the European Organisation for Research and Treatment of Cancer (eortc) and the (then) ncic Clinical Trials Group12, includes maximal surgical resection or biopsy followed by concomitant temozolomide (tmz) and radiation (a total dose of 60 Gy administered in 30 fractions) followed by 6 cycles of adjuvant tmz. That regimen is based on trial results demonstrating improvement in survival outcomes with that protocol rather than with radiation therapy (rt) alone12. In the tmz arm of the trial, 27.2% of patients were alive at 2 years compared with 10.9% in the rt-alone arm. At 5 years, 9.8% of patients in the combined therapy group were alive compared with 1.9% of those who received rt alone. Median overall survival was also higher in the tmz-containing arm (14 months with tmz–rt plus adjuvant tmz vs. 12 months with rt-alone)12.
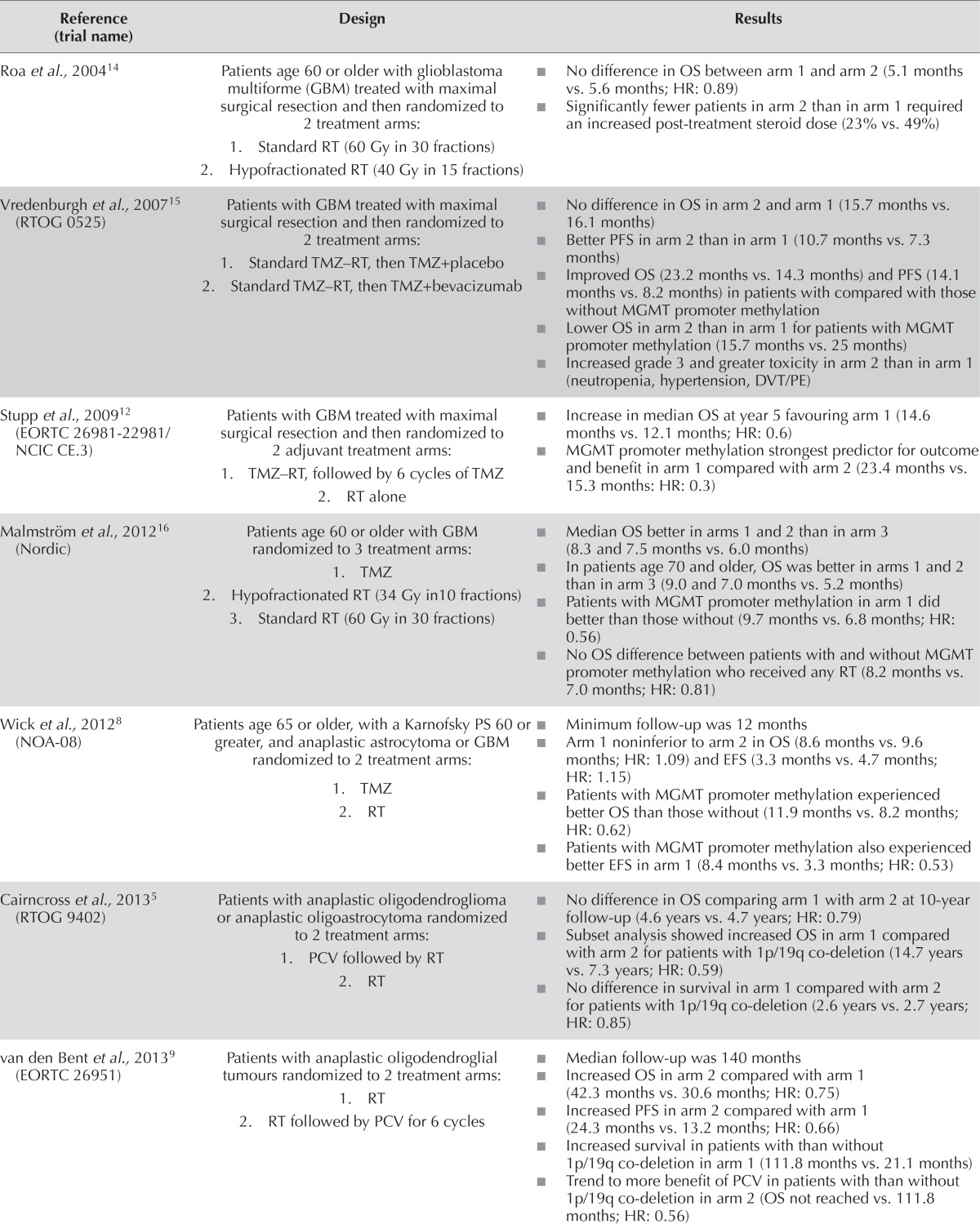
Given emerging data supporting the use of alternating electric fields with tmz after the rt–tmz phase of treatment13, the current standard of care is evolving. Other trials have yielded new insights into the management of specific glioma subpopulations (discussed in the subsections that follow). Table i summarizes the results of recent trials.
TABLE I.
Summary of landmark trials in the treatment of high-grade glioma
| Reference (trial name) | Design | Results |
|---|---|---|
| Roa et al., 200414 | Patients age 60 or older with glioblastoma multiforme (GBM) treated with maximal surgical resection and then randomized to 2 treatment arms:
|
|
| Vredenburgh et al., 200715 (RTOG 0525) | Patients with GBM treated with maximal surgical resection and then randomized to 2 treatment arms:
|
|
| Stupp et al., 200912 (EORTC26981-22981/NCIC CE.3) | Patients with GBM treated with maximal surgical resection and then randomized to 2 adjuvant treatment arms:
|
|
| Malmström et al., 201216 (Nordic) | Patients age 60 or older with GBM randomized to 3 treatment arms:
|
|
| Wick et al., 20128 (NOA-08) | Patients age 65 or older, with a Karnofsky PS 60 or greater, and anaplastic astrocytoma or GBM randomized to 2 treatment arms:
|
|
| Cairncross et al., 20135 (RTOG 9402) | Patients with anaplastic oligodendroglioma or anaplastic oligoastrocytoma randomized to 2 treatment arms:
|
|
| van den Bent et al., 20139 (EORTC 26951) | Patients with anaplastic oligodendroglial tumours randomized to 2 treatment arms:
|
|
| Chinot et al., 201417 (AVAglio) | Patients with GBM treated with maximal surgical resection and then randomized to 2 treatment arms:
|
|
| Roa et al., 201518 (IAEA) | Patients age 50 or older, a Karnofsky PS 50 or greater, with GBM treated with maximal surgical resection and then randomized to 2 treatment arms:
|
|
| Gilbert et al., 201319 (RTOG 0825) | Patients with GBM treated with maximal surgical resection and concurrent TMZ/RT before randomization to 2 treatment arms:
|
|
RT = radiotherapy; OS = overall survival; HR = hazard ratio; RTOG = Radiation Therapy Oncology Group; TMZ = temozolomide; PFS = progression-free survival; MGMT = O-6-methylguanine-DNA methyltransferase; DVT = deep vein thrombosis; PE = pulmonary embolism; EORTC = European Organisation for Research and Treatment of Cancer; NCIC = National Cancer Institute of Canada; QOL = quality of life; PS = performance status; EFS = event-free survival; PCV = chemotherapy regimen of procarbazine–lomustine–vincristine; IAEA = International Atomic Energy Agency; CI = confidence interval.
Elderly Patients
Evidence suggests that, compared with younger patients, elderly patients (60 years of age and older) tend to do poorly. Two large randomized controlled trials, noa-8 and the Nordic trial, indicated that, compared with using both tmz and rt, the use of tmz alone in patients with mgmt promoter methylation produced similar outcomes with less toxicity8,16. The noa-8 trial also demonstrated that, compared with the tmz group, the rt-alone group of patients without mgmt promoter methylation experienced superior event-free survival. Those trials suggest that treatment with tmz or rt alone in elderly patients is acceptable depending on mgmt status. The results of ce.6 (NCT00482677), a phase iii trial comparing rt plus tmz with rt alone in elderly patients is ongoing, and results are expected within the next year.
Age and poor performance status have also affected rt dose and fractionation schemes in elderly patients. For individuals more than 50 years of age with a Karnofsky performance status greater than 50, lower-dose radiotherapy is preferred because higher-dose radiotherapy demonstrates no survival advantage14,18.
Anaplastic Astrocytoma
The optimal management of patients with anaplastic astrocytoma is unknown. A few patients with anaplastic astrocytoma were included in the eortc–ncic trial12, and for that reason, the study treatment regimen is often used for patients with such tumours. The results of Radiation Therapy Oncology Group (rtog) 9813 (NCT00004259) and eortc 26053–22054 (NCT00626990) are pending and will provide the first prospective evidence for the management of anaplastic astrocytoma.
Anaplastic Oligodendroglioma
The management of anaplastic oligodendroglioma is based on evidence from two large phase iii trials that recently established a new standard of care5,9. In eortc 26951, a significant increase in median overall survival was shown in patients treated with rt and adjuvant procarbazine, lomustine, and vincristine (pcv) compared with rt alone (3.4 years vs. 2.6 years respectively). A similar survival benefit with the addition of pcv chemotherapy was observed in rtog 9402, but only in patients with 1p/19q co-deletion.
Although some available data support the use of tmz instead of pcv in this patient population, no phase iii trials have yet been completed. The results of the ongoing eortc 26081–22086 trial (NCT00887146) comparing rt followed by pcv with rt and concomitant and adjuvant tmz will hopefully add some clarity about the role of tmz in patients with anaplastic oligodendroglioma.
Recurrent Disease
Treatment options are more limited at the time of recurrence because patients who received radiotherapy often cannot be re-treated because of the risk of brain necrosis or radiation injury to critical structures. Patients are re-assessed for either or both of tumour resection and treatment with tmz, single-agent lomustine, etoposide, carboplatin with tamoxifen, or pcv. Alternating electric field therapy has also shown promise in the recurrent setting, although its use is not widespread20. Carmustine-impregnated wafers deliver chemotherapy locally at the time of resection and can confer a survival benefit21; however, few centres are currently using that method because of high complication rates and cost.
Bevacizumab has shown some promise in recurrent glioblastoma multiforme and can also be used to treat radiation necrosis. Bevacizumab inhibits vascular endothelial growth factor, thereby normalizing the integrity of the blood–brain barrier and changing imaging characteristics. Bevacizumab is not yet in wide use in publicly funded health systems because of high cost and a lack of an overall survival benefit15,22,23. There is some evidence of a potential survival advantage when lomustine is combined with bevacizumab, as in the phase ii belob trial24. However, the results of the phase iii extension of that trial (NCT01290939) reported no difference in overall survival between treatment arms.
Future Treatment Strategies
Despite treatment advances, outcomes remain poor in high-grade gliomas, and particularly in glioblastoma. Many promising treatment options are currently under investigation.
Vaccines act by boosting the body’s own immune defenses through immunologic memory and might play a role in combating malignant cells. Several vaccines are currently being investigated in early clinical trials. The dendritic cell–based DCVax-L (Northwest Biotherapeutics, Bethesda, MD, U.S.A.) has been shown to be effective and safe in phase i and ii clinical trials25–27, and research into its effectiveness is ongoing (NCT00045968, NCT02146066). The peptide-based synthetic vaccine rindopepimut (against epidermal growth factor receptor variant iii) was shown to increase overall survival in a phase ii trial28, and further studies are currently underway to confirm its efficacy and safety (NCT01498328, NCT01480479, NCT00458601).
Interest in the use of human pathogenic viruses to selectively destroy tumour cells has also been increasing. The therapeutic use of such “oncolytic viruses” has shown some promise in preclinical models, including glioma cell cultures29–32. The development of therapies that selectively target tumour cells would have clear advantages over conventional chemotherapy and rt, which exert toxic effects on both malignant and non-malignant tissues. Research is currently ongoing, studying the PVSRIPO polio virus (NCT01491893) and the retroviral replicating factor Toca 511 [Tocagen, San Diego, CA, U.S.A. (NCT02598011, NCT01985256, NCT02414165, NCT01470794)].
Immunotherapy has been successful in other disease sites and also shows preclinical promise in the treatment of brain tumours. Inhibition of PD-1, such as that seen with nivolumab, has been shown to be effective in mice implanted with glioblastoma cells33,34. Its use is also currently being explored in humans with glioblastoma (NCT02423343, NCT02529072). If the effect on glioma tissue is comparable to that in other malignancies such as non-small-cell lung cancer35, this form of therapy could play a significant role in the future management of high-grade gliomas.
Blockade of ctla4 by ipilimumab has been revolutionary in the treatment of melanoma36. It has also shown preclinical promise in high-grade gliomas37,38. Clinical trials are currently underway to test its efficacy and safety in humans (NCT02311920, NCT02017717).
RESPONSE ASSESSMENT
The Macdonald criteria were developed in 1990 to provide a means of accurately establishing tumour response to therapy based on the volume of enhancing tumour seen on computed tomography39. The method was later extrapolated to conventional magnetic resonance imaging (mri), in which tumour progression was defined according to increased volume of gadolinium-enhancing tumour. However, radiologic evaluation can be confounded by so-called pseudophenomena—imaging changes that do not reflect a true alteration in the burden of disease.
Pseudoprogression
Pseudoprogression refers to new areas of enhancement or edema that arise not from tumour progression, but from chemoradiotherapy-related inflammation, likely because of increased vessel permeability40. Recognized as early as 197941, pseudoprogression poses a clinical challenge because the imaging appearance is indistinguishable from true disease progression. Before the use of tmz chemoradiation, only approximately 1% of patients treated with focal fractional rt alone would develop treatment-related imaging changes42. However, with the current regimen, pseudoprogression been reported in up to 50% of patients, typically noted at the first follow-up mri obtained within 2–3 months after chemoradiation therapy43.
Failure to recognize pseudoprogression can lead to premature termination of an effective therapy, unnecessary surgical intervention, or additional chemotherapeutic agents. Because pseudoprogression resolves spontaneously, that resolution might be misinterpreted as evidence that the new treatment is effective, thus skewing the results of clinical trials44. On the other hand, successful recognition of pseudoprogression has been associated with improved prognosis, possibly because of the increased likelihood of mgmt promoter methylation in this population45.
Given the growing evidence surrounding pseudoprogression, the Response Assessment in Neuro-Oncology (rano) criteria provided an update in 2010 to account for the phenomenon of pseudoprogression46. The rano criteria specify that, within the first 12 weeks after completion of rt, tumour progression can be established only if most of the new enhancement occurs outside the radiation field or if histologic confirmation of progression is obtained. However, a diagnostic dilemma remains for enlarging enhancement and peritumoural edema that occurs within the radiation field during the initial 12 weeks. Biopsy samples can sometimes reveal either obvious tumour growth or therapy-induced changes, but in many instances, even histologic assessment fails to resolve the dilemma because of sampling errors, inconclusive specimens with mixed treatment and tumour histologic findings, inter-observer variability, and inconsistent definitions of residual and recurrent disease47.
Because of the diagnostic challenges, the current management practice for pseudoprogression in asymptomatic patients often involves observation and continuation of current therapy with radiologic follow-up in 2–3 months48. In the presence of clinical symptoms, surgical resection can be considered for therapeutic and diagnostic purposes40.
Pseudoresponse
Another phenomenon that confounds imaging interpretation in glioma patients is that of pseudoresponse. Pseudoresponse refers to an apparent improvement in disease severity on mri when, in reality, the changes are treatment-related. Antiangiogenic therapies such as bevacizumab or cediranib have shown early reduction in contrast enhancement on mri within days or even hours49. The rapidity of the change and the lack of an associated survival benefit50 indicate that these findings do not reflect a true improvement in tumour burden. This phenomenon can arise from normalization of the blood–brain barrier integrity. Patients placed on a “drug holiday” from antiangiogenic therapy because of toxicity have in fact demonstrated reversal of the effect and subsequent re-improvement when the drug is restarted44. Concern has arisen that antiangiogenic therapy might inadvertently select for a more invasive tumour phenotype that co-opts existing microvasculature rather than relying on neoangiogenesis51.
The rano criteria address pseudoresponse by requiring mri changes to persist for at least 4 weeks before being termed a true response. They also include clinical status as an indirect measure of worsening non-enhancing disease51. The lack of an objective imaging parameter for non-enhancing disease is clearly suboptimal; measurement of T2 or fluid attenuation inversion recovery signal abnormality in patients on antiangiogenic therapy has not been helpful in predicting survival50. Updates to the criteria are expected as work in this area develops.
Advanced Imaging and Pseudophenomena
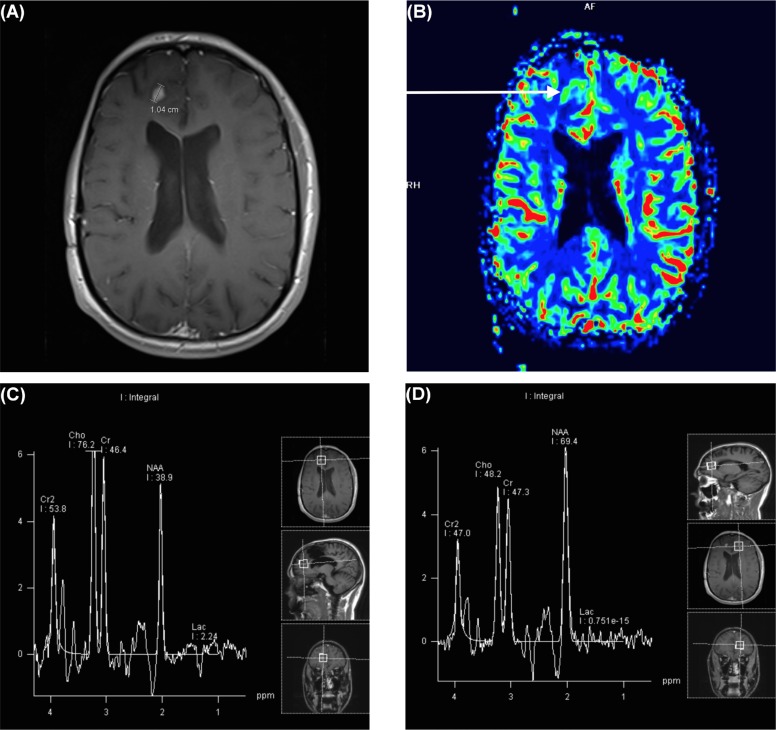
A number of preliminary investigations suggest that advanced mri techniques using physiologic and biochemical parameters might provide unique information valuable to discriminating pseudophenomena from true changes in tumour status (Figure 1).
FIGURE 1.
A 31-year-old male patient with prior resection of a right frontal glioblastoma multiforme presented later with a 1-cm enhancing nodule concerning for recurrence compared with pseudoprogression. (A) Magnetic resonance image of the new nodule. (B) Map of relative cerebral blood volume demonstrates increased flow in the nodule (arrow). (C) Spectroscopic imaging demonstrates an elevated choline peak compared with (D) the normal contralateral brain parenchyma in the same patient.
Perfusion Imaging
Perfusion imaging is an mri technique that can provide qualitative and quantitative assessment of the increased blood supply typically seen with neoangiogenesis, which accompanies neoplastic growth52. On the other hand, treatment-related changes increase vascular permeability without neoangiogenesis. Given this important distinction, perfusion imaging can help to differentiate gliomas from treatment-related pseudoprogression.
Dynamic susceptibility contrast–enhanced mri (dsc-mri) is the most commonly used perfusion imaging technique. It relies on a first-pass bolus of gadolinium contrast to generate parametric maps such as cerebral blood flow maps and cerebral blood volume maps. A quantitative analysis of the cerebral blood volume map can be used to generate relative cerebral blood volume ratios. In clinical investigations, such ratios derived from dsc-mri were shown to distinguish between true tumour progression and pseudoprogression with 82% sensitivity and 78% specificity53. In addition, dsc-mri has been used in the rtog 0625 multicentre trial to evaluate pseudoresponse with bevacizumab, noting shorter overall survival times for patients demonstrating increasing relative cerebral blood volume after initiation of bevacizumab54.
Another mri technique, dynamic contrast-enhanced mri, relies on the increased permeability of blood vessels in tumours, which manifests as an increased rate of capillary leakage of contrast into the interstitial space55. Dynamic contrast-enhanced mri parameters have been particularly useful in conjunction with parameters derived from dsc-mri. Multiparametric analysis from both dsc-mri and dynamic contrast-enhanced mri was used in a study of 108 patients, successfully discriminating pseudoprogression from true progression with a sensitivity of 87% and a specificity of 87.1%–90.3%56.
Diffusion Imaging
Diffusion-weighted imaging is a readily available mri technique that depicts the restriction of water molecule movement, relying on the apparent diffusion coefficients. Tumour growth involves increased cellularity and greater diffusion restriction, generating a lower apparent diffusion coefficient; in contrast, pseudoprogression has been found to have a higher apparent diffusion coefficient57,58. Diffusion-weighted imaging is also useful in cases of pseudoresponse, because treatment-induced permeability changes do not tend to affect diffusion restriction. Preliminary investigations have noted that a high b value (reflecting the strength and duration of the magnetic diffusion gradient) in diffusion-weighted imaging can identify some cases of pseudoresponse earlier than the Macdonald and rano criteria can59.
Magnetic Resonance Spectroscopy
Proton magnetic resonance spectroscopy is another promising technique that provides noninvasive characterization of cellular metabolites, determining changes in the proportions of choline, N-acetyl aspartate, and creatine60,61. Proliferating tumours demonstrate increased cell membrane turnover, which entails an elevation in choline relative to creatine, because of increased phospholipids in the cell membranes. These tumours also demonstrate diminished normal functional neuronal tissue, which entails a reduction in N-acetyl aspartate. Cerebral parenchyma involved in pseudoprogression does not exhibit the same metabolite profile62.
Recent advances have also highlighted the role of magnetic resonance spectroscopy in determining cases of pseudoresponse. An increased ratio of N-acetyl aspartate to choline indicates improvement in the patient’s tumour burden in keeping with true response to therapy63.
Subtraction Mapping
In patients on antiangiogenic therapy, invasive tumour can appear to be non-enhancing, given the improved integrity of the blood–brain barrier. However, with T1 subtraction mapping, true voxel-to-voxel subtraction measurements can detect subtle residual enhancement in tumour that might otherwise be inconspicuous to the eye. Using such a method in 160 patients, Ellingson et al.64 demonstrated improved visualization and quantification of tumour volume that was predictive of overall survival and progression-free survival. Similarly, T2 subtraction mapping has been used to quantify voxel-wise changes, allowing visualization of persistent abnormality in patients that appear improved in conventional imaging65.
Positron-Emission Tomography Imaging
Increased radiotracer accumulation in positron-emission tomography (pet) has been noted in cases of true progression compared with pseudoprogression. Of particular interest are the investigations that have gone beyond traditional pet using 18F–fluorodeoxyglucose, which is of limited utility in the normally high metabolic environment of the brain.
Brain tumours exhibit increased protein synthesis, making amino acid tracers an attractive imaging modality. In a study evaluating 72 patients with 11C–methionine pet, a threshold uptake index of 1.9 could distinguish between true tumour progression and pseudoprogression with 83.5% sensitivity and 97% specificity66. A smaller study using pet imaging with the amino acid tracer O-2-18F-fluoroethyl- l-tyrosine and a cut-off value of 2.3 demonstrated 100% sensitivity and 91% specificity in discriminating true tumour proliferation from pseudoprogression67.
FUTURE DIRECTIONS
Pseudoprogression has yet to be adequately described beyond the population of high-grade glioma patients on tmz. A small amount of research has described pseudo-progression in low-grade glioma pediatric subjects, most frequently manifesting as increasing mass effect rather than new enhancement68. Moreover, pseudoprogression has yet to be adequately studied in patients on other chemotherapeutic agents such as pcv (now fairly commonly used for grade iii gliomas in patients with 1p/19q co-deleted tumours). One case series has demonstrated mri findings of pseudoprogression in patients treated with lomustine and tmz combination therapy69. The time course of pseudoprogression also warrants better delineation. Traditionally, pseudoprogression has been described in the first 3 months and radiation-induced brain necrosis has been described after that period, but caution must be exercised in relying on such timelines because cases of non-classical “delayed” or “late” pseudoprogression have been noted after the 3-month period69.
The landscape of glioma management is changing rapidly given new advances in genetic and imaging markers. Because prospective data on some glioma subpopulations is lacking, ongoing clinical trials are expected to optimize therapeutic protocols for patients with anaplastic astrocytoma and anaplastic oligodendroglioma. Although response assessment continues to be a great challenge, preliminary investigations with functional techniques are quite promising. Such findings warrant replication in larger studies and the addition of imaging biomarkers to therapeutic trials to establish a new assessment algorithm for evaluating therapeutic response in patients with high-grade glioma.
CONFLICT OF INTEREST DISCLOSURES
We have read and understood Current Oncology’s policy on disclosing conflicts of interest, and we declare the following interests: ME is a speaker and consultant for Bayer Healthcare and a speaker for Siemens Healthcare.
REFERENCES
- 1.Ostrom QT, Gittleman H, Liao P, et al. cbtrus statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2007–2011. Neuro Oncol. 2014;16(suppl 4):iv, 1–63. doi: 10.1093/neuonc/nou223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Louis DN, Ohgaki H, Wiestler OD, et al. The 2007 who classification of tumours of the central nervous system. Acta Neuropathol. 2007;114:97–109. doi: 10.1007/s00401-007-0243-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kleihues P, Louis DN, Scheithauer BW, et al. The who classification of tumors of the nervous system. J Neuropathol Exp Neurol. 2002;61:215–25. doi: 10.1093/jnen/61.3.215. [DOI] [PubMed] [Google Scholar]
- 4.Wick W, Hartmann C, Engel C, et al. noa-04 randomized phase iii trial of sequential radiochemotherapy of anaplastic glioma with procarbazine, lomustine, and vincristine or temozolomide. J Clin Oncol. 2009;27:5874–80. doi: 10.1200/JCO.2009.23.6497. [DOI] [PubMed] [Google Scholar]
- 5.Cairncross G, Wang M, Shaw E, et al. Phase iii trial of chemoradiotherapy for anaplastic oligodendroglioma: long-term results of rtog 9402. J Clin Oncol. 2013;31:337–43. doi: 10.1200/JCO.2012.43.2674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hegi ME, Diserens AC, Gorlia T, et al. mgmt gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med. 2005;352:997–1003. doi: 10.1056/NEJMoa043331. [DOI] [PubMed] [Google Scholar]
- 7.Sanson M, Marie Y, Paris S, et al. Isocitrate dehydrogenase 1 codon 132 mutation is an important prognostic biomarker in gliomas. J Clin Oncol. 2009;27:4150–4. doi: 10.1200/JCO.2009.21.9832. [DOI] [PubMed] [Google Scholar]
- 8.Wick W, Platten M, Meisner C, et al. on behalf of the noa-08 Study Group of Neuro-oncology Working Group (noa) of the German Cancer Society Temozolomide chemotherapy alone versus radiotherapy alone for malignant astrocytoma in the elderly: the noa-08 randomised, phase 3 trial. Lancet Oncol. 2012;13:707–15. doi: 10.1016/S1470-2045(12)70164-X. [DOI] [PubMed] [Google Scholar]
- 9.van den Bent MJ, Brandes AA, Taphoorn MJB, et al. Adjuvant procarbazine, lomustine, and vincristine chemotherapy in newly diagnosed anaplastic oligodendroglioma: long-term follow-up of eortc Brain Tumor Group study 26951. J Clin Oncol. 2013;31:344–50. doi: 10.1200/JCO.2012.43.2229. [DOI] [PubMed] [Google Scholar]
- 10.Lacroix M, Abi-Said D, Fourney DR, et al. A multivariate analysis of 416 patients with glioblastoma multiforme: prognosis, extent of resection, and survival. J Neurosurg. 2001;95:190–8. doi: 10.3171/jns.2001.95.2.0190. [DOI] [PubMed] [Google Scholar]
- 11.Keles GE, Anderson B, Berger MS. The effect of extent of resection on time to tumor progression and survival in patients with glioblastoma multiforme of the cerebral hemisphere. Surg Neurol. 1999;52:371–9. doi: 10.1016/S0090-3019(99)00103-2. [DOI] [PubMed] [Google Scholar]
- 12.Stupp R, Hegi ME, Mason WP, et al. on behalf of the European Organisation for Research and Treatment of Cancer Brain Tumour and Radiation Oncology Groups and the ncic Clinical Trials Group Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase iii study: 5-year analysis of the eortc–ncic trial. Lancet Oncol. 2009;10:459–66. doi: 10.1016/S1470-2045(09)70025-7. [DOI] [PubMed] [Google Scholar]
- 13.Stupp R, Wong E, Scott C, et al. Interim analysis of the ef-14 trial: a prospective, multicenter trial of NovoTTF-100A together with temozolomide compared to temozolomide alone in patients with newly diagnosed gbm [abstract NT-40] Neuro Oncol. 2014;16(suppl 5):v167. doi: 10.1093/neuonc/nou265.40. [DOI] [Google Scholar]
- 14.Roa W, Brasher PMA, Bauman G, et al. Abbreviated course of radiation therapy in older patients with glioblastoma multiforme: a prospective randomized clinical trial. J Clin Oncol. 2004;22:1583–8. doi: 10.1200/JCO.2004.06.082. [DOI] [PubMed] [Google Scholar]
- 15.Vredenburgh JJ, Desjardins A, Herndon JE, 2nd, et al. Bevacizumab plus irinotecan in recurrent glioblastoma multiforme. J Clin Oncol. 2007;25:4722–9. doi: 10.1200/JCO.2007.12.2440. [DOI] [PubMed] [Google Scholar]
- 16.Malmström A, Grønberg BH, Marosi C, et al. on behalf of the Nordic Clinical Brain Tumour Study Group Temozolomide versus standard 6-week radiotherapy versus hypofractionated radiotherapy in patients older than 60 years with glioblastoma: the Nordic randomised, phase 3 trial. Lancet Oncol. 2012;13:916–26. doi: 10.1016/S1470-2045(12)70265-6. [DOI] [PubMed] [Google Scholar]
- 17.Chinot OL, Wick W, Mason W, et al. Bevacizumab plus radiotherapy–temozolomide for newly diagnosed glioblastoma. N Engl J Med. 2014;370:709–22. doi: 10.1056/NEJMoa1308345. [DOI] [PubMed] [Google Scholar]
- 18.Roa W, Kepka L, Kumar N, et al. International Atomic Energy Agency randomized phase iii study of radiation therapy in elderly and/or frail patients with newly diagnosed glioblastoma multiforme. J Clin Oncol. 2015;33:4145–50. doi: 10.1200/JCO.2015.62.6606. [DOI] [PubMed] [Google Scholar]
- 19.Gilbert MR, Wang M, Aldape KD, et al. Dose-dense temozolomide for newly diagnosed glioblastoma: a randomized phase iii clinical trial. J Clin Oncol. 2013;31:4085–91. doi: 10.1200/JCO.2013.49.6968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stupp R, Wong ET, Kanner AA, et al. NovoTTF-100A versus physician’s choice chemotherapy in recurrent glioblastoma: a randomised phase iii trial of a novel treatment modality. Eur J Cancer. 2012;48:2192–202. doi: 10.1016/j.ejca.2012.04.011. [DOI] [PubMed] [Google Scholar]
- 21.Bregy A, Shah AH, Diaz MV, et al. The role of Gliadel wafers in the treatment of high-grade gliomas. Expert Rev Anticancer Ther. 2013;13:1453–61. doi: 10.1586/14737140.2013.840090. [DOI] [PubMed] [Google Scholar]
- 22.Friedman HS, Prados MD, Wen PY, et al. Bevacizumab alone and in combination with irinotecan in recurrent glioblastoma. J Clin Oncol. 2009;27:4733–40. doi: 10.1200/JCO.2008.19.8721. [DOI] [PubMed] [Google Scholar]
- 23.Gilbert MR, Dignam JJ, Armstrong TS, et al. A randomized trial of bevacizumab for newly diagnosed glioblastoma. N Engl J Med. 2014;370:699–708. doi: 10.1056/NEJMoa1308573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Taal W, Oosterkamp HM, Walenkamp AM, et al. Single-agent bevacizumab or lomustine versus a combination of bevacizumab plus lomustine in patients with recurrent glioblastoma (belob trial): a randomised controlled phase 2 trial. Lancet Oncol. 2014;15:943–53. doi: 10.1016/S1470-2045(14)70314-6. [DOI] [PubMed] [Google Scholar]
- 25.Yu JS, Wheeler CJ, Zeltzer PM, et al. Vaccination of malignant glioma patients with peptide-pulsed dendritic cells elicits systemic cytotoxicity and intracranial T-cell infiltration. Cancer Res. 2001;61:842–7. [PubMed] [Google Scholar]
- 26.Kikuchi T, Akasaki Y, Irie M, Homma S, Abe T, Ohno T. Results of a phase i clinical trial of vaccination of glioma patients with fusions of dendritic and glioma cells. Cancer Immunol Immunother. 2001;50:337–44. doi: 10.1007/s002620100205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wheeler CJ, Black KL, Liu G, et al. Vaccination elicits correlated immune and clinical responses in glioblastoma multiforme patients. Cancer Res. 2008;68:5955–64. doi: 10.1158/0008-5472.CAN-07-5973. [DOI] [PubMed] [Google Scholar]
- 28.Schuster J, Lai RK, Recht LD, et al. A phase ii, multicenter trial of rindopepimut (CDX-110) in newly diagnosed glioblastoma: the act iii study. Neuro Oncol. 2015;17:854–61. doi: 10.1093/neuonc/nou348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dobrikova EY, Broadt T, Poiley-Nelson J, et al. Recombinant oncolytic poliovirus eliminates glioma in vivo without genetic adaptation to a pathogenic phenotype. Mol Ther. 2008;16:1865–72. doi: 10.1038/mt.2008.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Merrill MK, Bernhardt G, Sampson JH, Wikstrand CJ, Bigner DD, Gromeier M. Poliovirus receptor CD155-targeted oncolysis of glioma. Neuro Oncol. 2004;6:208–17. doi: 10.1215/S1152851703000577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Huang TT, Parab S, Burnett R, et al. Intravenous administration of retroviral replicating vector, Toca 511, demonstrates therapeutic efficacy in orthotopic immune-competent mouse glioma model. Hum Gene Ther. 2015;26:82–93. doi: 10.1089/hum.2014.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huang TT, Hlavaty J, Ostertag D, et al. Toca 511 genetransfer and 5-fluorocytosine in combination with temozolomide demonstrates synergistic therapeutic efficacy in a temozolomide-sensitive glioblastoma model. Cancer Gene Ther. 2013;20:544–51. doi: 10.1038/cgt.2013.51. [DOI] [PubMed] [Google Scholar]
- 33.Zeng J, See AP, Phallen J, et al. Anti–PD-1 blockade and stereo-tactic radiation produce long-term survival in mice with intracranial gliomas. Int J Radiat Oncol Biol Phys. 2013;86:343–9. doi: 10.1016/j.ijrobp.2012.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reardon DA, Gokhale P, Ligon K, et al. Immune checkpoint blockade for glioblastoma: preclinical activity of single agent and combinatorial therapy [abstract]. Neuro Oncol. 2014;16(suppl 3):iii, 11–12. [Google Scholar]
- 35.Borghaei H, Paz-Ares L, Horn L, et al. Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N Engl J Med. 2015;373:1627–39. doi: 10.1056/NEJMoa1507643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hodi FS, O’Day SJ, McDermott DF, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363:711–23. doi: 10.1056/NEJMoa1003466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fecci PE, Ochiai H, Mitchell DA, et al. Systemic ctla-4 blockade ameliorates glioma-induced changes to the CD4+ T cell compartment without affecting regulatory T-cell function. Clin Cancer Res. 2007;13:2158–67. doi: 10.1158/1078-0432.CCR-06-2070. [DOI] [PubMed] [Google Scholar]
- 38.Vom Berg J, Vrohlings M, Haller S, et al. Intratumoral il-12 combined with ctla-4 blockade elicits T cell–mediated glioma rejection. J Exp Med. 2013;210:2803–11. doi: 10.1084/jem.20130678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Macdonald DR, Cascino TL, Schold SC, Cairncross JG. Response criteria for phase ii studies of supratentorial malignant glioma. J Clin Oncol. 1990;8:1277–80. doi: 10.1200/JCO.1990.8.7.1277. [DOI] [PubMed] [Google Scholar]
- 40.Brandsma D, Stalpers L, Taal W, Sminia P, van den Bent MJ. Clinical features, mechanisms, and management of pseudoprogression in malignant gliomas. Lancet Oncol. 2008;9:453–61. doi: 10.1016/S1470-2045(08)70125-6. [DOI] [PubMed] [Google Scholar]
- 41.Hoffman WF, Levin VA, Wilson CB. Evaluation of malignant glioma patients during the postirradiation period. J Neurosurg. 1979;50:624–8. doi: 10.3171/jns.1979.50.5.0624. [DOI] [PubMed] [Google Scholar]
- 42.Chaskis C, Neyns B, Michotte A, De Ridder M, Everaert H. Pseudoprogression after radiotherapy with concurrent temozolomide for high-grade glioma: clinical observations and working recommendations. Surg Neurol. 2009;72:423–8. doi: 10.1016/j.surneu.2008.09.023. [DOI] [PubMed] [Google Scholar]
- 43.Taal W, Brandsma D, de Bruin HG, et al. Incidence of early pseudo-progression in a cohort of malignant glioma patients treated with chemoirradiation with temozolomide. Cancer. 2008;113:405–10. doi: 10.1002/cncr.23562. [DOI] [PubMed] [Google Scholar]
- 44.Clarke JL, Chang S. Pseudoprogression and pseudoresponse: challenges in brain tumor imaging. Curr Neurol Neurosci Rep. 2009;9:241–6. doi: 10.1007/s11910-009-0035-4. [DOI] [PubMed] [Google Scholar]
- 45.Gahramanov S, Varallyay C, Tyson RM, et al. Diagnosis of pseudoprogression using mri perfusion in patients with glioblastoma multiforme may predict improved survival. CNS Oncol. 2014;3:389–400. doi: 10.2217/cns.14.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wen PY, Macdonald DR, Reardon DA, et al. Updated response assessment criteria for high-grade gliomas: Response Assessment in Neuro-Oncology working group. J Clin Oncol. 2010;28:1963–72. doi: 10.1200/JCO.2009.26.3541. [DOI] [PubMed] [Google Scholar]
- 47.Melguizo-Gavilanes I, Bruner JM, Guha-Thakurta N, Hess KR, Puduvalli VK. Characterization of pseudoprogression in patients with glioblastoma: is histology the gold standard? J Neurooncol. 2015;123:141–50. doi: 10.1007/s11060-015-1774-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Knudsen-Baas KM, Moen G, Fluge Ø, Storstein A. Pseudo-progression in high-grade glioma. Acta Neurol Scand Suppl. 2013:31–7. doi: 10.1111/ane.12047. [DOI] [PubMed] [Google Scholar]
- 49.Telles BA, D’Amore F, Lerner A, Law M, Shiroishi MS. Imaging of the posttherapeutic brain. Top Magn Reson Imaging. 2015;24:147–54. doi: 10.1097/RMR.0000000000000051. [DOI] [PubMed] [Google Scholar]
- 50.Boxerman JL, Ellingson BM. Response assessment and magnetic resonance imaging issues for clinical trials involving high-grade gliomas. Top Magn Reson Imaging. 2015;24:127–36. doi: 10.1097/RMR.0000000000000054. [DOI] [PubMed] [Google Scholar]
- 51.Huang RY, Neagu MR, Reardon DA, Wen PY. Pitfalls in the neuroimaging of glioblastoma in the era of antiangiogenic and immuno/targeted therapy—detecting illusive disease, defining response. Front Neurol. 2015;6:33. doi: 10.3389/fneur.2015.00033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Essig M, Anzalone N, Combs SE, et al. mr imaging of neoplastic central nervous system lesions: review and recommendations for current practice. AJNR Am J Neuroradiol. 2012;33:803–17. doi: 10.3174/ajnr.A2640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kong DS, Kim ST, Kim EH, et al. Diagnostic dilemma of pseudoprogression in the treatment of newly diagnosed glioblastomas: the role of assessing relative cerebral blood flow volume and oxygen-6-methylguanine-dna methyltransferase promoter methylation status. AJNR Am J Neuroradiol. 2011;32:382–7. doi: 10.3174/ajnr.A2286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schmainda KM, Zhang Z, Prah M, et al. Dynamic susceptibility contrast mri measures of relative cerebral blood volume as a prognostic marker for overall survival in recurrent glioblastoma: results from the acrin 6677/rtog 0625 multicenter trial. Neuro Oncol. 2015;17:1148–56. doi: 10.1093/neuonc/nou364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jain R, Poisson L, Narang J, et al. Genomic mapping and survival prediction in glioblastoma: molecular subclassification strengthened by hemodynamic imaging biomarkers. Radiology. 2013;267:212–20. doi: 10.1148/radiol.12120846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Park JE, Kim HS, Goh MJ, Kim SJ, Kim JH. Pseudoprogression in patients with glioblastoma: assessment by using volume-weighted voxel-based multiparametric clustering of mr imaging data in an independent test set. Radiology. 2015;275:792–802. doi: 10.1148/radiol.14141414. [DOI] [PubMed] [Google Scholar]
- 57.Yang I, Huh NG, Smith ZA, Han SJ, Parsa AT. Distinguishing glioma recurrence from treatment effect after radiochemotherapy and immunotherapy. Neurosurg Clin N Am. 2010;21:181–6. doi: 10.1016/j.nec.2009.08.003. [DOI] [PubMed] [Google Scholar]
- 58.Prager AJ, Martinez N, Beal K, Omuro A, Zhang Z, Young RJ. Diffusion and perfusion mri to differentiate treatment- related changes including pseudoprogression from recurrent tumors in high-grade gliomas with histopathologic evidence. AJNR Am J Neuroradiol. 2015;36:877–85. doi: 10.3174/ajnr.A4218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yamasaki F, Kurisu K, Aoki T, et al. Advantages of high b-value diffusion-weighted imaging to diagnose pseudo-responses in patients with recurrent glioma after bevacizumab treatment. Eur J Radiol. 2012;81:2805–10. doi: 10.1016/j.ejrad.2011.10.018. [DOI] [PubMed] [Google Scholar]
- 60.Zonari P, Baraldi P, Crisi G. Multimodal mri in the characterization of glial neoplasms: the combined role of single-voxel mr spectroscopy, diffusion imaging and echo-planar perfusion imaging. Neuroradiology. 2007;49:795–803. doi: 10.1007/s00234-007-0253-x. [DOI] [PubMed] [Google Scholar]
- 61.Di Costanzo A, Scarabino T, Trojsi F, et al. Multiparametric 3T mr approach to the assessment of cerebral gliomas: tumor extent and malignancy. Neuroradiology. 2006;48:622–31. doi: 10.1007/s00234-006-0102-3. [DOI] [PubMed] [Google Scholar]
- 62.O’Brien BJ, Colen RR. Post-treatment imaging changes in primary brain tumors. Curr Oncol Rep. 2014;16:397. doi: 10.1007/s11912-014-0397-x. [DOI] [PubMed] [Google Scholar]
- 63.Ratai EM, Zhang Z, Snyder BS, et al. Magnetic resonance spectroscopy as an early indicator of response to antiangiogenic therapy in patients with recurrent glioblastoma: rtog 0625/acrin 6677. Neuro Oncol. 2013;15:936–44. doi: 10.1093/neuonc/not044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ellingson BM, Kim HJ, Woodworth DC, et al. Recurrent glioblastoma treated with bevacizumab: contrast-enhanced T1-weighted subtraction maps improve tumor delineation and aid prediction of survival in a multicenter clinical trial. Radiology. 2014;271:200–10. doi: 10.1148/radiol.13131305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ellingson BM, Cloughesy TF, Lai A, et al. Quantification of edema reduction using differential quantitative T2 (DQT2) relaxometry mapping in recurrent glioblastoma treated with bevacizumab. J Neurooncol. 2012;106:111–19. doi: 10.1007/s11060-011-0638-x. [DOI] [PubMed] [Google Scholar]
- 66.Skvortsova TY, Brodskaya ZL, Gurchin AF. pet using 11C–methionine in recognition of pseudoprogression in cerebral glioma after combined treatment [Russian] Zh Vopr Neirokhir Im N N Burdenko. 2014;78:50–8. doi: 10.17116/neiro201478650-54. [DOI] [PubMed] [Google Scholar]
- 67.Galldiks N, Dunkl V, Stoffels G, et al. Diagnosis of pseudo-progression in patients with glioblastoma using O-(2-[18F] fluoroethyl)-l-tyrosine pet. Eur J Nucl Med Mol Imaging. 2014;42:685–95. doi: 10.1007/s00259-014-2959-4. [DOI] [PubMed] [Google Scholar]
- 68.Naftel RP, Pollack IF, Zuccoli G, Deutsch M, Jakacki RI. Pseudoprogression of low-grade gliomas after radiotherapy. Pediatr Blood Cancer. 2015;62:35–9. doi: 10.1002/pbc.25179. [DOI] [PubMed] [Google Scholar]
- 69.Stuplich M, Hadizadeh DR, Kuchelmeister K, et al. Late and prolonged pseudoprogression in glioblastoma after treatment with lomustine and temozolomide. J Clin Oncol. 2012;30:e180–3. doi: 10.1200/JCO.2011.40.9565. [DOI] [PubMed] [Google Scholar]