Abstract
Pre-exposure prophylaxis (PrEP), the antiretroviral treatment regimen for HIV-negative people at high risk of acquiring HIV, has demonstrated efficacy across clinical trials in several patient populations. The Centers for Disease Control (CDC) have released detailed guidelines to aid providers in prescribing PrEP for their high-risk patients, including men who have sex with men (MSM), high-risk heterosexuals, and injection drug users. Given that much attention in PrEP has focused on MSM patients, the present study used an online survey to assess factors involved in HIV care providers’ (n=363) decisions about prescribing PrEP, along with their willingness to prescribe PrEP to patients from various risk populations (e.g., MSM, heterosexuals, injection drug users). The efficacy of PrEP was an important factor in provider’s decisions about prescribing PrEP, as were considerations about patients’ adherence to the regimen, regular follow-up for care, and medication costs. This survey’s findings also suggest that providers’ willingness to prescribe PrEP varies by patient group, with providers most willing to initiate the regimen with MSM who have an HIV-positive partner, and least willing to prescribe to high-risk heterosexuals or injection drug users. In the context of the current CDC recommendations for PrEP that include MSM, heterosexuals, and injection drug users, examining providers’ rationales for and barriers against supporting this HIV prevention strategy across patient groups merits further attention.
Keywords: Pre-exposure Prophylaxis (PrEP), HIV/AIDS, HIV Care Providers, Prevention
Over 30 years into the HIV/AIDS epidemic, significant advances in treatment have been made. With antiretroviral therapy, people living with HIV/AIDS can drastically reduce the risk of disease transmission. Still, the rate of new infections annually in the U.S. has remained steady (Centers for Disease Control and Prevention [CDC], 2012), highlighting the ongoing need for large-scale primary prevention approaches targeting HIV-negative persons.
Pre-exposure prophylaxis (PrEP), antiretroviral treatment as a prevention strategy for HIV-negative adults, gained worldwide attention (Baeten et al., 2012; Grant et al., 2010; Grant et al., 2014; Thigpen et al., 2012). In 2012, the US Food and Drug Administration approved once-daily Truvada (tenofovir + emtricitabine; Gilead) for PrEP. In light of evidence for its efficacy (Baeten et al., 2012; Grant et al., 2010; Grant et al., 2014; Thigpen et al., 2012), the CDC (2014) released detailed recommendations for PrEP. In these guidelines, the CDC recommends that PrEP be considered as one prevention strategy for HIV-negative patients at “substantial risk” for HIV infection within three groups: men who have sex with men (MSM), heterosexual adults, and injection drug users (IDUs).
The CDC recommends PrEP for persons with an HIV-positive sexual partner, recent sexually transmitted infection (STI), multiple sexual partners, inconsistent or no condom use, and/or history of commercial sex work (CDC, 2014). The recommendations for heterosexual men and women are identical to those for MSM, adding that PrEP be considered for heterosexual adults living in high-prevalence areas or belonging to high-prevalence networks. The CDC recommends that PrEP be considered for IDUs with an HIV-positive injecting partner, those sharing injection equipment, and those recently in drug treatment, but continue injecting drugs. Taken as a whole, the CDC’s (2014) message is clear: PrEP is a beneficial strategy for HIV prevention among MSM, heterosexual adults, and IDUs.
Most of the attention and research on PrEP (efficacy, effectiveness, feasibility, acceptability) has focused on MSM. Auerbach and colleagues (2015) found that less than 10% of women in a qualitative study were familiar with PrEP before study enrollment; others believed PrEP was only for men. Upon learning of the regimen, women expressed interest in PrEP, and anger that their medical providers had failed to inform them of it (Auerbach et al., 2015). In the few studies that have examined IDUs’ attitudes toward PrEP, knowledge has been low (Escudero et al., 2015; Stein, Thurmond, & Bailey, 2014).
Healthcare providers are an important source of information about health innovations for patients. However, evidence suggests that providers’ judgments about their patients can influence their treatment decisions. Studies using clinical vignettes have demonstrated that drug abuse history and race can affect providers’ willingness to prescribe antiretroviral treatment, even when all other information is identical (Bogart, Catz, Kelly, & Benotsch, 2001). Medical students have shown bias in their attitudes and willingness to prescribe PrEP to black versus white MSM (Calabrese et al., 2014). A recent study demonstrated that HIV care providers were comfortable prescribing PrEP to serodiscordant couples, especially when the HIV-positive partner is not on antiretroviral treatment (80%), but were less comfortable prescribing to IDUs (42%) (Krakower, Beekman, Polgreen, & Mayer, 2015). In the context of the CDC recommendations, we examined the current perceptions of front-line HIV care providers across the U.S. about PrEP and their likelihood of prescribing it to different patient groups.
Methods
Sample
Data were collected from a cross-sectional internet-based survey. Members of the American Academy of HIV Medicine (AAHVIM), a professional association of predominantly front-line HIV care providers, were invited via e-mail to complete the survey in June 2014. The e-mail was distributed to 3,484 AAHIVM members; providers were instructed to complete the survey only if they were licensed prescribers (e.g., M.D., D.O., N.P., P.A.) and currently seeing patients. No incentives for completing the survey were provided.
Survey
The survey consisted of 53 questions including providers’ demographic and practice-related features, practices towards patients’ sexual health, attitudes and beliefs about PrEP, and likelihood of prescribing PrEP to different patients (Adams, Balderson, Packett, Brown, & Catz, 2015). Survey completion time was approximately 10 minutes.
Measures
Providers reported their demographic characteristics, along with practice-related features (e.g., years in practice, caseload), and their frequency (Never, Rarely, Occasionally, Often, Always) of asking patients about their sexual practices and offering HIV and STI testing. Frequency items were dichotomized into “Infrequent” (collapsing Never, Rarely, Occasionally) and “Frequent” (collapsing Often, Always). Providers rated how important (Not At All, Somewhat, Very) several factors were in their decision to prescribe PrEP (e.g., adherence, cost, side effects). Providers also reported the likelihood (Not At All, Somewhat, Very) that they would prescribe PrEP to a variety of patient groups (e.g., MSM with an HIV-positive partner, high-risk heterosexual, injection drug user). Responses were dichotomized into “Unlikely” (collapsing Not At All and Somewhat Likely) and “Very Likely.”
Analysis
Analyses were conducted using SPSS version 22.0 (IBM Corp., 2013). Cochran’s Q statistic assessed whether providers differed in their likelihood of prescribing PrEP by patient group. McNemar’s chi-square tests determined where these differences existed. Given the large number of McNemar tests conducted (n=21), a Bonferonni correction was applied (p<.002 as statistically significant).
Results
Sample Description
The survey was completed by 363 providers, approximately 14% of those who were e-mailed and eligible based upon their prescription privileges. Ten providers were excluded because they were not authorized to prescribe (e.g., psychologists), 29 respondents outside of the U.S. were excluded, and an additional 64 providers were excluded because their caseload only included HIV-positive patients, precluding them from prescribing PrEP for prevention. The final analytic sample included 260 providers. Table 1 provides demographic and descriptive information. The efficacy of PrEP, along with concerns about adherence, follow-up, and cost were primary factors in providers’ decisions about prescribing.
Table 1.
Sample Descriptives
| Provider Demographics /Practice Characteristics | Percentage (n) |
|---|---|
| Gender | |
| Male | 52.3 (135) |
| Female | 47.3 (122) |
| Transgender | 0.4 (1) |
| Age | |
| Under 40 | 18.9 (49) |
| 40–49 | 26.6 (69) |
| 50–59 | 35.1 (91) |
| 60+ | 19.3 (50) |
| Years in Practice | |
| 0–5 | 13.2 (34) |
| 6–10 | 14.4 (37) |
| 11–15 | 14.0 (36) |
| 16–20 | 13.2 (34) |
| 21+ | 45.1 (116) |
| Race | |
| White | 76.4 (197) |
| Black | 9.3 (24) |
| Asian | 8.9 (23) |
| Other | 5.4 (14) |
| Primary Care Provider | |
| Yes | 79.3 (203) |
| No | 20.7 (53) |
| Physician Specialty | |
| Infectious Disease | 30.7 (79) |
| Family Medicine | 30.4 (78) |
| Internal Medicine | 28.8 (74) |
| Other | 10.1 (26) |
| Percentage of Caseload: HIV-Negative | |
| 1–24 | 31.9 (83) |
| 25–49 | 20.8 (54) |
| 50–74 | 27.3 (71) |
| 75–100 | 20.0 (52) |
|
Practices Toward Patients’ Sexual Health | |
| Asking About: | |
| Sexual Partners | |
| Infrequent | 9.8 (25) |
| Frequent | 90.2 (230) |
| Partners’ HIV Status | |
| Infrequent | 18.1 (46) |
| Frequent | 81.9 (208) |
| Condom Use | |
| Infrequent | 9.8 (25) |
| Frequent | 90.2 (229) |
| Offering: | |
| HIV Testing to “Low Risk” Patients | |
| Infrequent | 19.2 (49) |
| Frequent | 80.8 (206) |
| HIV Testing to “High Risk” Patients | |
| Infrequent | 4.0 (10) |
| Frequent | 96.0 (242) |
| STI Testing to “Low Risk” Patients | |
| Infrequent | 27.2 (69) |
| Frequent | 72.8 (185) |
| STI Testing to “High Risk” Patients | |
| Infrequent | 3.5 (9) |
| Frequent | 96.5 (245) |
|
Factors in Prescribing PrEP | |
| Importance of Taking PrEP Daily | |
| Not At All | 0.5 (1) |
| Somewhat | 3.6 (8) |
| Very | 95.9 (211) |
| Sex Risk Compensation (Increased Risk) | |
| Not At All | 23.5 (51) |
| Somewhat | 32.3 (70) |
| Very | 44.2 (96) |
| Side Effects of PrEP | |
| Not At All | 8.6 (19) |
| Somewhat | 39.1 (86) |
| Very | 52.3 (115) |
| Increased Chance of Drug Resistance | |
| Not At All | 16.3 (35) |
| Somewhat | 38.1 (82) |
| Very | 45.6 (98) |
| Decreased HIV Risk | |
| Not At All | 2.8 (6) |
| Somewhat | 16.7 (36) |
| Very | 80.5 (173) |
| Cost of Medication | |
| Not At All | 6.4 (14) |
| Somewhat | 32.1 (70) |
| Very | 61.5 (134) |
| Regular Follow-up Care/Monitoring | |
| Not At All | 0.0 (0) |
| Somewhat | 8.6 (19) |
| Very | 91.4 (202) |
Providers’ Likelihood to Prescribe PrEP Differs By Patient Group
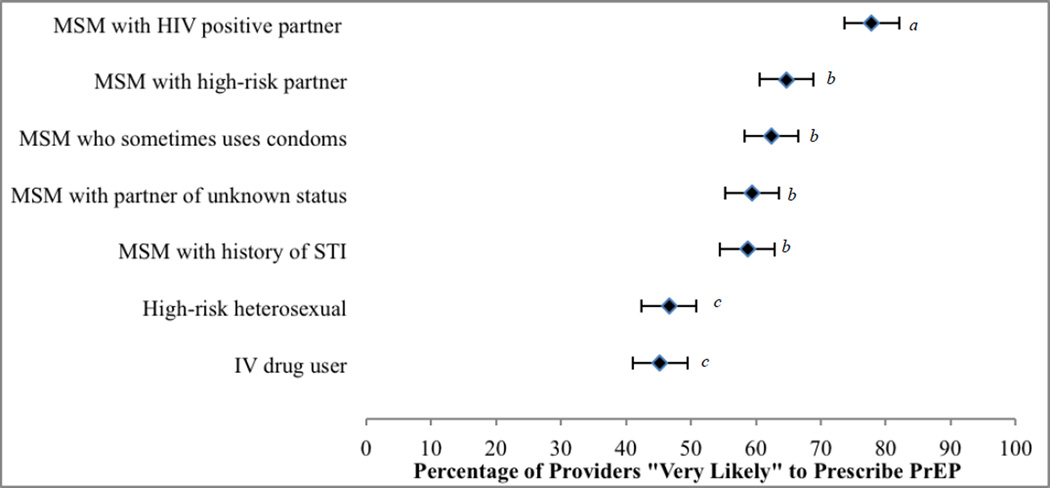
Providers’ likelihood to prescribe PrEP differed across patient types (Cochran’s Q = 130.60, p<.001, df=6). McNemar’s tests (Bonferroni-adjusted) revealed that providers were most likely to consider PrEP for MSM patients with an HIV positive partner (78%); the rate of endorsing prescribing to this group was significantly higher than any other group (Figure 1). Providers were equally likely to prescribe PrEP to all other MSM patients. Providers were least likely to consider prescribing PrEP to high-risk heterosexuals (47%) or to IV drug users (45%).
Figure 1.
Providers’ Likelihood to Prescribe PrEP Differs By Patient Type
Note. Error bars display 95% confidence interval. Patient types sharing subscripts (a,b,c) are not significantly different (p>.002; Bonferroni-corrected) according to McNemar’s chi-square tests for paired comparisons.
Discussion
Despite CDC guidelines recommending PrEP as a prevention strategy for MSM, high-risk heterosexuals, and IDUs, our findings suggest that HIV medication prescribers’ willingness to prescribe PrEP differs across patient types. Providers were most likely to prescribe PrEP to MSM with an HIV-positive partner, followed by all other MSM groups. They were least likely to prescribe to high-risk heterosexuals and IDUs. These findings align with prior research that demonstrated providers’ comfort with prescribing PrEP to serodiscordant couples, and discomfort prescribing it to IDUs (Krakower et al., 2015).
Notably, likelihood to prescribe PrEP did not reach 100% for any groups, suggesting an ongoing need to increase support in the medical community. Providers endorsed concerns about adherence, monitoring, and cost of treatment, which have been identified as important factors previously (Arnold et al., 2012; Karris et al., 2013; Krakower et al., 2014). Concerns about cost-effectiveness for lower-incidence groups (e.g., heterosexuals) may have tempered eagerness to prescribe a limited resource like PrEP to non-MSM patients. Providers’ reticence to prescribe PrEP to patients identified in the CDC guidelines as eligible suggests that there may be opportunity for differential prevention success for some groups. Given HIV treatment disparities among women, African-Americans, and IDUs, providers’ hesitance to prescribe PrEP could exacerbate the gap in HIV/AIDs care (Gebo et al., 2005; Fleishman, Yehia, Moore, Gebo, & Agwu, 2012).
The present study was exploratory in nature and has limitations. We did not assess providers’ knowledge about PrEP and CDC guidelines, their prescribing behaviors, or general attitudes about PrEP. Respondents were not given additional context for determining their willingness to prescribe across patients. For example, providers may be less willing to prescribe PrEP to MSM with an HIV-positive partner on antiretroviral treatment than to MSM with an HIV-positive partner who is untreated. Further, patient groups were not mutually exclusive (e.g., MSM vs. IDU) and there were fewer non-MSM patient categories than MSM sub-types, negating the opportunity to delve into further comparisons to determine reasons for different endorsement levels. Our convenience sample of AAHIVM members may not generalize to other providers who prescribe PrEP, and some providers who play an important role in health maintenance were excluded (e.g., pharmacists, psychologists). Our response rate was very low, and we cannot determine whether non-responders chose not to respond, never viewed the invitation, or self-excluded due to being out of practice.
Conclusions
Our findings suggest the need for further research to determine barriers to receiving complete PrEP endorsement across providers, along with exploration into factors that may prevent providers from prescribing PrEP to heterosexuals and IDUs. Future studies should link PrEP-related attitudes and behaviors, and should assess psychosocial concerns, along with structural and institutional barriers, to prescribing PrEP for patients at risk of acquiring HIV.
Acknowledgments
We thank Bruce J. Packett II, Kathy Brown, MD, FACP, AAHIVS, and Sheryl L. Catz, Ph.D. for their contributions to this project. Survey development was supported by the American Academy of HIV Medicine (AAHIVM) and Gilead Sciences, Inc. The contribution of Dr. Adams was supported by Grant T32 AG027677 from the National Institute on Aging.
Footnotes
The authors received no financial compensation from AAHIVM or Gilead Sciences, Inc. for their work on this project.
References
- Adams LM, Balderson B, Packett BJ, II, Brown K, Catz SL. Providers’ perspectives on prescribing pre-exposure prophylaxis (PrEP) for HIV prevention. The HIV Specialist: Magazine of the American Academy of HIV Medicine. 2015 Apr;:19–25. [Google Scholar]
- Arnold EA, Hazelton P, Lane T, Christopoulos KA, Galindo GR, Steward WT, Morin SF. A qualitative study of provider thoughts on implementing pre-exposure prophylaxis (PrEP) in clinical settings to prevent HIV infection. Plos One. 2012;7(7):1–8. doi: 10.1371/journal.pone.0040603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auerbach JD, Kinsky S, Brown G, Charles V. Knowledge, attitudes, and likelihood of Pre-Exposure Prophylaxis (PrEP) use among US women at risk of acquiring HIV. AIDS Patient Care & STDS. 2015;29(2):102–110. doi: 10.1089/apc.2014.0142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baeten JM, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, Celum C. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. New England Journal of Medicine. 2012;367(5):399–410. doi: 10.1056/NEJMoa1108524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogart LM, Catz SL, Kelly JA, Benotsch EG. Factors influencing physicians’ judgments of adherence and treatment decisions for patients with HIV disease. Medical Decision Making. 2001;21(1):28–36. doi: 10.1177/0272989X0102100104. [DOI] [PubMed] [Google Scholar]
- Calabrese SK, Earnshaw VA, Underhill K, Hansen NB, Dovidio JF. The impact of patient race on clinical decisions related to prescribing HIV Pre-Exposure Prophylaxis (PrEP): Assumptions about sexual risk compensation and implications for access. AIDS and Behavior. 2014;18(2):226–240. doi: 10.1007/s10461-013-0675-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Estimated HIV incidence in the United States, 2007–2010. HIV Surveillance Supplemental Report. 2012 Dec;17(4) Retrieved from http://www.cdc.gov/hiv/topics/surveillance/resources/reports/#supplemental. [Google Scholar]
- Centers for Disease Control and Prevention. Preexpsoure prophylaxis for the prevention of HIV infection in the United States – 2014 Clinical Practice Guideline. 2014 May 14; Retrieved from http://www.cdc.gov/hiv/pdf/prepguidelines2014.pdf.
- Escudero DJ, Kerr T, Wood E, Nguyen P, Lurie MN, Sued O, Marshall BDL. Acceptability of HIV Pre-Exposure Prophylaxis (PrEP) among people who inject drugs (PWID) in a Canadian setting. AIDS and Behavior. 2015;19(5):752–757. doi: 10.1007/s10461-014-0867-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleishman JA, Yehia BR, Moore RD, Gebo KA, Agwu AL. Disparities in receipt of antiretroviral therapy among HIV-infected adults (2002–2008) Medical Care. 2012;50(5):419–427. doi: 10.1097/MLR.0b013e31824e3356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gebo KA, Fleishman JA, Conviser R, Reilly ED, Korthuis PT, Moore RD, Mathews WC. Racial and gender disparities in receipt of highly active antiretroviral therapy persist in a multistate sample of HIV patients in 2001. JAIDS. 2005;38(1):96–103. doi: 10.1097/00126334-200501010-00017. [DOI] [PubMed] [Google Scholar]
- Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, Glidden DV. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. New England Journal of Medicine. 2010;363(27):2587–2599. doi: 10.1056/NEJMoa1011205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant RM, Anderson PL, McMahan V, Liu A, Amico KR, Mehrotra M, Glidden DV. Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: a cohort study. Lancet. 2014;14(9):820–829. doi: 10.1016/S1473-3099(14)70847-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karris MY, Beekmann SE, Mehta SR, Anderson CM, Polgreen PM. Are we prepped for preexposure prophylaxis (PrEP)? Provider opinions on the real-world use of PrEP in the United States and Canada. Clinical Infectious Diseases. 2013;58(5):704–712. doi: 10.1093/cid/cit796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krakower D, Ware N, Mitty JA, Maloney K, Mayer KH. HIV providers’ perceived barriers and facilitators to implementing pre-exposure prophylaxis in care settings: A qualitative study. AIDS and Behavior. 2014;18:1712–1721. doi: 10.1007/s10461-014-0839-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krakower DS, Beekman SE, Polgreen PM, Mayer KH. Diffusion of newer HIV prevention innovations: Variable practices of frontline infectious diseases physicians. Clinical Infectious Diseases. 2015 doi: 10.1093/cid/civ736. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein M, Thurmond P, Bailey G. Willingness to use HIV Pre-Exposure Prophylaxis among opiate users. AIDS and Behavior. 2015;18:1694–1700. doi: 10.1007/s10461-014-0778-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thigpen MC, Kebaabetswe PM, Paxton LA, Smith DK, Rose CE, Segolodi TM, Brooks JT. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. New England Journal of Medicine. 2012;367:423–434. doi: 10.1056/NEJMoa1110711. [DOI] [PubMed] [Google Scholar]